Abstract
Increased interest in the demarcation of catatonia from other conditions such as schizophrenia and autism is shown in the new DSM-5 category Catatonia Not Elsewhere Classified (NEC) encompassing catatonia of uncertain origin or associated with developmental conditions. Catatonia NEC is an imminently relevant diagnosis in patients who meet criteria for catatonia but without clearly defined associated psychotic, affective, or medical disorders. Catatonia NEC should be considered when catatonic symptoms present in patients with autism spectrum disorders, developmental disorders such as Prader-Willi Syndrome and Down Syndrome, tic disorders and Tourette Syndrome, Kleine-Levin Syndrome, aseptic encephalitis such as Anti-N-methyl-D-aspartate Receptor encephalitis, Pervasive Refusal Syndrome, or complex posttraumatic conditions.
Current experiences continue to support the use of benzodiazepines and ECT in catatonia as safe and effective treatments without the risk of worsening catatonia or precipitating Neuroleptic Malignant Syndrome as opposed to when antipsychotic medications are used as first-line or sole treatment
Historical and contemporary clinical and experimental catatonia models are available for future research, focusing on motor circuitry dysfunction, abnormal neurotransmitters, epileptic discharges, genetics, neuroendocrine and immune abnormalities, fear reactions akin to the animal defense strategy of tonic immobility, and developmental risk factors.
There have been advances in demarcating catatonia in a wide variety of patients as a treatable condition that requires prompt identification. Catatonia NEC in DSM-5 is likely to improve proper diagnosis and treatment of catatonia and to intensify research of this condition.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Catatonia
- Malignant
- Psychomotor abnormalities
- Movement disorders
- Schizophrenia
- Mood disorder
- Psychosis
- Autism spectrum disorders
- Developmental disorders
- Tourette syndrome
- Tics
- Self-injury
- Autism
- Kleine-Levin Syndrome
- Anti-N-methyl-D-aspartate Receptor encephalitis
- Posttraumatic stress disorder
- Neuroleptic Malignant Syndrome
- Toxic Serotonergic Syndrome
- Delirium
- Children and adolescents
- Benzodiazepines
- Electroconvulsive treatment (ECT)
- Autonomic symptoms
- Vagal nerve
And the more you really see mental patients and get to know their symptoms, the more you will be convinced that finally nothing else can be found and observed but movements and the whole pathology of mental patients consists of nothing else but the peculiarities of their motor behavior.
Carl Wernicke, 1900 (1)
It happens quite often that we fail to see something because it’s too big.
Multatuli (pseudonym of Eduard Douwes Dekker; Dutch writer; 1820–1887)
1 Introduction
Catatonia is a unique syndrome characterized by specific motor signs, at times life-threatening when aggravated by autonomic dysfunction and fever, but treatable with benzodiazepines and electroconvulsive therapy (ECT) if recognized early (2, 3). Identifiable motor signs are immobility sometimes alternating with excessive motor activity that is mostly purposeless and not influenced by external stimuli, extreme negativism, reduced speech or muteness, repetitive movements (stereotypy), echolalia, echopraxia, and other peculiarities of voluntary movement. Tics and other sudden and non-rhythmic movements, often with self-injury, occur commonly in catatonic patients and may qualify as additional catatonic symptoms (4, 5).
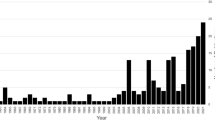
Since the publication of the first version of this chapter in 2008, catatonia has been further delineated across a wide range of disorders (6, 7). An update on symptoms, prevalence, evaluation, treatment, risk factors, and experimental models of catatonia is presented, through review of literature and case-reports since 2008, incorporating important changes in the classification of catatonia that have been made in DSM-5 (8) (Table 27.1).
2 Catatonia NEC: A Dark Horse in DSM-5
Catatonia was originally described in 1874 by Kahlbaum as a separate brain disorder with a cyclic, alternating, and ultimately progressive course (9). Kraepelin viewed catatonia as an exclusive subtype of dementia praecox or schizophrenia. In contrast, recent studies show the preponderance of underlying affective symptoms and syndromes, particularly mania, in adult catatonic patients (10–13) and comorbidity with an expanding list of adult and pediatric conditions (Table 27.2). Examples of catatonia are provided in Figs. 27.1–27.4.
In DSM-IV (44), catatonia was a specifier of Schizophrenia, Primary Mood Disorder, and Mental Disorder due to a General Medical Condition. However, major changes have been made in DSM-5 (8) including the deletion of catatonia as a type of schizophrenia, the creation of a new class of Catatonia Not Elsewhere Classified (NEC), and the addition of a catatonia specifier for 10 primary diagnoses. A uniform list of catatonia signs was adopted across all categories. Catatonia Secondary to a general Medical Condition created in 1994 has been retained.
The recommendation for catatonia as an independent syndrome in the form of a separate category Catatonia NEC is profound and finalizes the divorce between catatonia and schizophrenia, in order to allow experience to refine the place of catatonia in clinical care and to offer the recommended treatments for catatonia to a wider range of patients. The known experience finds about 80% of the patients with catatonia respond to the benzodiazepines, and almost universal response to ECT in those who fail benzodiazepines. Prompt recognition of catatonia and in some cases treatment with ECT is likely to prevent medical complications, such as deep vein thrombosis, pulmonary emboli (45, 46), dehydration, malnutrition, and physical exhaustion.
The designation of catatonia specifiers for 10 primary diagnoses and the retention of a Catatonia Secondary to a Medical Disorder sustain the secondary position of catatonia in the prior classifications and do not encourage the first-line use of benzodiazepines in patients who meet the criteria for catatonia thereby continuing to create treatment dilemmas.
For example, the distinction between Catatonia Secondary to a Medical Disorder and Catatonia NEC is unclear. A case-in-point is the patient who meets criteria for (malignant) catatonia and tests positive for anti-NMDA receptor antibodies. Is the patient suffering from the newly coined anti-NMDAR encephalitis (47) that should be treated with immune treatments? Or is the patient suffering from malignant catatonia that should be treated swiftly with benzodiazepines and ECT? The enthusiasm for the newly defined disorder of anti-NMDA receptor encephalitis should not be a barrier for treating the recognized catatonia vigorously (32). The immune treatments that are recommended for the newly proposed form of synaptic autoimmune encephalitis often yield equivocal results, especially in pediatric cases. The sharp increase in the number of reports of pediatric cases of anti-NMDA receptor encephalitis highlights that catatonia is common yet often unacknowledged in children and adolescents (6, 19). There are now a few reports that show the efficacy of treatment with high-dose benzodiazepine and ECT in anti-NMDA receptor encephalitis (36, 48, 49). Studies comparing benzodiazepines or ECT with immune therapies in children, adolescents, and adults who meet criteria for catatonia and who test positive for the anti-NMDA receptor antibody are warranted (Table 27.3).
3 Evaluation, Differential Diagnosis, and Treatment
Catatonia should be considered in any patient when there is a marked deterioration in psychomotor function and overall responsiveness. Observation and psychiatric interview will not suffice to detect the catatonic syndrome, since the most striking symptoms such as posturing, are present only in a minority of the cases. It is of importance to elicit specific catatonic signs (such as negativism, automatic obedience, passive obedience, gegenhalten, or grasp reflex) during a neuropsychiatric examination. A rating scale or checklist may aid the detection and quantification of catatonia. Up to date, 6 different catatonia rating scales have been published: the Rogers Catatonia Scale (51), the Bush-Francis Catatonia Rating Scale (52), the Northoff Catatonia Rating Scale (53), the Braunig Catatonia Rating Scale (54), the Bush-Francis Catatonia Rating Scale Revised Version (55) and the Kanner Scale (56). Characteristics of these scales are presented in Table 27.4.
Reflecting different underlying diagnostic concepts, current diagnostic rating scales differ substantially in the nature and number of the items included. The total number of items ranges from 18 to 40. Both sensitivity and specificity of current rating scales is high. With the exception of the MRS-C, all rating scales provide a threshold score for the diagnosis of catatonia, based on the total score of the scale or on the score of a screening instrument, as in the BFCRS and the Kanner scale. Probably, not all scales are suited for use in the divergent patient groups in which catatonia can be encountered: the RCS is designed to detect catatonia in depression, whereas the MRC may be better suited in schizophrenia. None of the scales have been applied to autistic populations. The BFCRS, the BCRS and the Kanner scale are completed during a semi-structured interview. A correct BCRS examination is time consuming, whereas completing the BFCRS is easily integrated in a psychiatric evaluation, making the BFCRS a practical screening tool for routine clinical practice. Current rating scales seem best suited for screening, offering the clinician a scheme to perform a neuropsychiatric examination and improving the detection of catatonic symptoms. These scales are less well suited for assessing severity and change, since they lack the sensitivity necessary to measure change (58).
Although different criteria for a diagnosis of catatonia are used, we find the criteria proposed by Fink & Taylor (3) relevant and practical (Table 27.5). In DSM-5, catatonia is diagnosed when three or more of a list of 12 catatonic symptoms are present (8). The 12 catatonic symptoms are: stupor, catalepsy, waxy flexibility, mutism, negativism, posturing, mannerism, stereotypy, agitation (non-influenced by external activity), grimacing, echolalia, and echopraxia.
3.1 Differential Diagnosis
A detailed history, clinical examination, and application of diagnostic criteria must be used to differentiate catatonia from other well-recognized conditions, syndromes, or disorders featuring psychomotor abnormalities that may overlap with the manifestations of catatonia. Making an adequate differential diagnosis of catatonia is complicated by the fact that there is no biologic marker diagnostic of catatonia. The differential diagnosis of catatonia when motor activity is increased or reduced is shown in Table 27.6.
Some motor manifestations of catatonia such as catatonic excitement, psychomotor retardation, or negativism may be mistaken for purposeful, oppositional and attention-seeking behaviors that are under full control of the patient and for secondary gain. Decreased speech, muteness, or posturing may be mistaken as indicative of conversion disorder especially when following stressful events or trauma. It may be very difficult in some instances to determine the origin of these behaviors and degree of control that the patient has on these behaviors, even during longer periods of observation. The catatonia benzodiazepine challenge test that will be discussed in the treatment section may be useful in such situations. A profoundly positive response would support a diagnosis of catatonia, although the therapeutic effects of anxiolytics including amytal and benzodiazepines as diagnostic tools and treatment are also known in conversion disorders (59–63). A negative challenge test is expected when motor abnormalities represent voluntary behaviors for secondary gain although there may be mild improvement due to specific sedative effects.
Epilepsy and status epilepticus are important differential diagnoses given the overlap of symptoms between psychomotor seizures and catatonia and the increased prevalence of seizures in catatonic patients (3). In his original description, Kahlbaum (Fig. 27.5) reported seizure-like symptoms in catatonia (9). Seizures are also frequent in children and adolescents with autism (64, 65) and catatonia (7, 20). Seizures and catatonia are not mutually exclusive in this population. However, frank epileptic activity is usually absent in EEG recordings in catatonic patients. Typical findings in catatonia include diffuse slowing in patients in catatonic stupor and a dysrhythmic EEG in catatonia. These findings are consistent with non-convulsive status epilepticus that resolves when catatonia remits and is consistent with the underlying theory (66, 67) of this disorder, that there is localized brain excitation in catatonic patients in specific deep brain structures that are not detected by current EEG techniques, which improves with anticonvulsant medications but especially with benzodiazepines and ECT.
3.2 Laboratory and Other Investigations
Various infectious, metabolic, endocrine, neurological, toxic and autoimmune conditions have been associated with catatonia and must therefore be assessed. Proposed basic investigations include a complete blood count and metabolic panel, erythrocyte sedimentation rate, magnetic resonance imaging, electroencephalogram, cerebrospinal fluid analysis, antinuclear antibodies, and urine and organic metabolic testing, with further testing based upon clinical findings (68) (Fig. 27.6).
A drug screen to detect common illicit and prescribed substances is necessary. Recreational drugs (phencyclidine, mescaline, psilocybin, cocaine, ecstasy, opiates and opioids), disulfiram, steroids, antibiotic agents (ciprofloxacin), baclofen and bupropion have been associated with the emergence of catatonia. Withdrawal of benzodiazepines, gabapentin and dopaminergic drugs, especially if done rapidly, has precipitated catatonia in some patients (3).
3.3 Medication Management
All prescribed medications should be evaluated for their potential to induce catatonic symptoms, since many medications can cause catatonia or catatonia-like conditions. Antipsychotic agents, especially of the first generation, should be discontinued as they are contraindicated in patients who exhibit the signs of catatonia because of the reported increased incidence of malignant catatonia or neuroleptic malignant syndrome (NMS) in patients with incipient signs of catatonia (69, 70). The symptoms of malignant catatonia or NMS are essentially the motor symptoms of catatonia compounded with autonomic symptoms (fever, blood pressure abnormalities, hypoventilation, excessive sweating). NMS is considered a toxic reaction to psychotropic medications, particularly antipsychotics.
Once catatonia is resolved, second generation antipsychotics with low D2 blockade (quetiapine, olanzapine) or with D2 partial agonism (aripiprazole) should be preferred for treatment of residual psychotic symptoms, if any (71).
3.4 Medical Management
Simultaneous treatment of catatonia and a drug-induced or medical condition, if any is detected, is generally recommended in addition to supportive measures. For instance, despite the withdrawal of the offending agent, treatment of an underlying infection or metabolic disease, or the removal of a malignancy, as the case may be, catatonia often persists and requires urgent intervention that should not be postponed for elaborate searches for ill-defined or poorly treatable medical conditions. This may be particularly relevant in recent cases of presumed autoimmune entities such as Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections (PANDAS) and anti-NMDA-receptor encephalitis where catatonic symptoms are evident, yet well documented anti-catatonic treatments are rejected in favor of novel immunological interventions of questionable benefit and possible danger (32, 72).
3.5 Lorazepam Test Validates Catatonia
As a first step, a benzodiazepine challenge test of 1 or 2 mg of lorazepam that can be administered per os, intramuscularly, or intravenously, should be used to verify the catatonia diagnosis (Fig. 27.6) (2, 3, 73). If intravenous lorazepam is used, any changes in the next two to five minutes are noted. If no change is observed, the second 1 or 2 mg lorazepam is injected, and the assessment is repeated. The interval for the repeat dose is longer for intramuscular (15’) and peroral (30’) administration. The use of the gamma-aminobutyric acid-A (GABA) receptor modulator zolpidem has also been developed as an alternative catatonia challenge test and implemented, particularly in Europe (74). Zolpidem is only available in oral form.
When a single dose of lorazepam improves catatonia, lorazepam can be prescribed at regular intervals to maintain improvement. Many catatonic patients require relatively high dosages of lorazepam, occasionally up to 24 mg daily, for symptom resolution. Our experience shows that in some patients with catatonia doses up to 24 mg daily are tolerated without ensuing sedation, especially when instituted using daily incremental dosages, and result in marked reduction of catatonic symptoms. This suggests that in some cases, catatonia may be associated with high tolerance to benzodiazepines. Careful monitoring in a medical setting for excessive sedation, respiratory compromise, and other side effects is required.
3.6 Pre-ECT Laboratory and Other Investigations
Routine laboratory tests and an anesthesia consult are required during the pre-ECT work-up. Routine brain imaging studies is not generally recommended prior to ECT, however, in some hospitals, pre-ECT brain CT or MRI is mandatory. Additional consultation may be required in selected cases to stabilize general medical issues such as risk of dehydration and hemodynamic abnormalities in catatonic patients before starting ECT (Fig. 27.6).
3.7 ECT Parameters
The relief of catatonia often seems to require more frequent seizures than those necessary for the relief of major depression. The UK standard practice of two seizures a week, although effective for major depression, may not be so for catatonia. In severe or malignant catatonia, daily (“en bloc”) treatment for three to five days may be necessary. Second, the efficacy of bilateral (bitemporal or bifrontal) electrode placement is better documented than is unilateral placement. Therefore, based on practical experience, the authors recommend bilateral electrode placement for catatonia. Furthermore, in our experience the number of treatments, before substantial and sustained improvement becomes obvious, cannot be predicted. Therefore, ECT treatment must be individually tailored and the duration and the frequency of treatment should be based on regular assessments, possibly after every 6–12 treatments.
3.8 ECT and Concurrent Medications
All psychiatric medications should be stopped prior to initiation of ECT, as well as any other non-psychiatric medications, if possible. An exception is when there was a partial response with benzodiazepine treatment, often administered in a high dose; in these instances, ECT and a benzodiazepine may be administered concurrently. Discontinuation or rapid taper of the benzodiazepine may not be advisable at the start of the ECT course, because of a risk of altering the seizure threshold. Concurrent use of lorazepam (or another benzodiazepine) and ECT is then a useful treatment variant. Intravenous administration of flumazenil, a benzodiazepine antagonist, can be used if lorazepam interferes with eliciting seizures during ECT and may be beneficial even if seizures outwardly appear adequate; indeed, use of flumazenil has also been proposed in benzodiazepine-naïve patients for augmentation of ECT effect (75).
3.9 Maintenance ECT in Catatonia
Maintenance-ECT (M-ECT) may be useful for sustained symptom-remission (76, 77). There are no studies which suggest evidence for structural or histopathological changes during M-ECT (78, 79). Studies of various cognitive functions also demonstrate a stability of various longitudinal cognitive measures (80–82).
Less information is available regarding M-ECT in patients with catatonia and autism. One case series (83) presents the M-ECT courses of three autistic catatonic patients who received up to 286 maintenance treatments with sustained remission of catatonia and without subjective evidence of decline in cognitive or adaptive skills. One patient was unable to access M-ECT for legal reasons and promptly relapsed into catatonia. While the number of M-ECT delivered to these patients appears high, this finding is considered within the context of a special patient population who are known to have a relatively poor response to psychotropic agents, and possibly a higher overall propensity for treatment resistance.
4 Malignant Catatonia and Related Conditions
Malignant catatonia is a severe form of catatonia, coined as “lethal catatonia” by Stauder (50) in 1934, that includes the constellation of catatonic signs, motoric excitement, stuporous exhaustion, autonomic instability, respiratory failure, collapse, coma and ultimately death. This malignant form of catatonia is of acute onset and systemically devastating requiring intensive medical care. Patients appear to have an acute infectious process leading to exhaustive but negative evaluations. Patients with malignant catatonia may present in both agitated and stuporous states (3). Untreated malignant catatonia is fatal in 10–20% of cases, with death ensuing within mere days of onset. Malignant catatonia also occurs in children and adolescents (84–87). Malignant catatonia should feature prominently in the differential diagnosis of the acute encephalopathies as a treatable syndrome with acute onset of unresponsiveness, muteness, echolalia, echopraxia, and other psychomotor abnormalities, along with fever and signs of autonomic instability.
Neuroleptic Malignant Syndrome (NMS) is a similar syndrome caused by typical as well as atypical antipsychotics and other psychotropic medications, and characterized by motor rigidity, lowered consciousness, autonomic instability, and fever. NMS is best considered malignant catatonia caused by administration of antipsychotic and other psychotropic agents; indeed, the physical and physiological symptoms as well as the laboratory indices, such as leukocytosis, elevated creatine phosphokinase, and decreased serum iron, show prominent correlation (2, 3). NMS responds to classic anti-catatonic treatments, i.e., benzodiazepines and ECT (2, 3, 69).
Toxic serotonin syndrome, malignant hyperthermia, and delirium constitute another group of disorders that are characterized by varying levels of hypokinesis and muscle stiffness, in combination with altered levels of consciousness and autonomic dysfunction. For example, there is discussion in the literature if toxic serotonin syndrome truly differs in key aspects with catatonia, or alternatively, if toxic serotonin syndrome should be regarded as another medication-induced form of catatonia (69, 88). Response of toxic serotonin syndrome to the same treatments as catatonia would strengthen the argument of relatedness. Malignant catatonia is similar to malignant hyperthermia in that both share muscular rigidity, hypermetabolic and hyperthermic states, yet the latter is uniquely associated with either succinylcholine usage or a genetic response to inhaled anesthetics (2, 3). A genetic model of hyperthermia is the Porcine Stress Syndrome, a congenital, autosomal recessive disorder which affects pigs, dogs, cats, and horses and is caused by a fundamental intolerance of stress due to a defective ryanodine receptor which affects closure of calcium channels in the sarcoplasmic reticulum and causing a sudden, sustained rise in intracellular calcium and consequent muscle contracture and up-regulation of metabolism (89).
Some patients diagnosed with delirium meet criteria for malignant catatonia (90, 91). Classifying these patients is difficult because DSM diagnostic rules state that catatonia should not be diagnosed if occurring exclusively during the course of a delirium while acknowledging that similar medical conditions of infectious, metabolic, endocrine and neurological etiologies are associated with both catatonia and delirium (44). The validity of this DSM provision is uncertain given the lack of studies in the literature that have assessed the importance of catatonia during delirium. The issue is important because treatments for catatonia and delirium are different, albeit with overlap. While delirium is typically treated with (typical or atypical) antipsychotics, the emergence of catatonia in delirium may caution against the use of antipsychotic medications due to the aforementioned risk of worsening catatonia with antipsychotic medications (69, 70). There are no new guidelines regarding this issue in DSM-5, probably due to the lack of studies.
Another unresolved classification issue is whether catatonia should be included in the differential diagnosis in patients with coma (complete unresponsiveness) (92), and, in a similar vein, if stupor or profound unresponsiveness can be the sole presenting symptom of catatonia (92–94). Recent case-reports have shown that patients with levels of unresponsiveness similar as in coma, and without other catatonic symptoms (except resistance to eye-opening) responded to electroconvulsive therapy (95) and intravenous benzodiazepines (94).
5 Pediatric Catatonia
A previous literature review from 1966–1996 (20, 22) found 30 cases of catatonia in patients younger than 18 years of age. Several children and adolescents had underlying mental retardation or autism spectrum disorder. Benzodiazepines and ECT were the most reliable treatments, similar as reported in adult catatonia. Table 27.7 shows the frequencies of the most common catatonic symptoms in children and adolescents reported by Dhossche & Bouman (20, 22).
Since then, other cases have been published confirming that catatonia occurs in children and adolescents with associated psychotic, affective, drug-induced, or medical disorders, but also in patients with autistic, developmental, and tic disorders, and occasionally in children with no clearly identifiable medical or psychiatric conditions (4, 19).
Table 27.8 lists pediatric studies showing a wide variability of prevalence rates of catatonia in selected patient groups and settings, suggesting that catatonia may not be rare. Adolescents with catatonia comorbid with schizophrenia and affective disorders have a 60-fold increased risk of premature death, including suicide, when compared to the general population of same sex and age (96).
6 Catatonia in Autism Spectrum Disorders
Catatonia has been increasingly recognized as a comorbid syndrome of autism spectrum disorders, identified at a rate of 12–17% in adolescents and young adults with autism spectrum disorders (99, 101) and with other intellectual disabilities (22, 105). Catatonic symptoms, such as mutism, stereotypic speech, echolalia, stereotypic or repetitive behaviors, posturing, grimacing, rigidity, mannerisms and purposeless agitation feature prominently in autism. Therefore, only a sharp and marked increase in these symptoms, often in adolescence, qualifies for a diagnosis of catatonia (99, 106, 107).
In some cases, catatonia may be a feature of another major psychiatric syndrome such as depression (108), bipolar illness (109) or schizophrenia (110), yet many patients do not qualify for a clear diagnosis of mood or a psychotic disorder, often due to the fact that patients are nonverbal and have severe cognitive impairments. Case-reports also describe catatonia in pediatric patients with genetic disorders which are characterized by varying degrees of developmental impairment but the autistic features often do not amount to a full diagnosis of autism; catatonia has been reported in patients with Prader-Willi Syndrome (22) and Down Syndrome (111).
Most cases of catatonia in children and adolescents with autism spectrum disorders are not associated with underlying medical or psychiatric conditions. For example, in a sample of 58 children and adolescents with catatonia, 18 (31%) had a history of developmental disorder, i.e., autism spectrum disorder, intellectual disability or neurodevelopmental malformation (112). Only two of those had an identifiable underlying medical or psychiatric condition.
Two systematic studies show catatonia to occur in 12% to 17% of adolescents and young adults with autism spectrum disorders (99, 101). Wing & Shah report that 17% of a large referred sample of adolescents and young adults with autism spectrum disorders satisfied modern criteria for catatonia (99). Thirty individuals with autism spectrum disorders aged 15 years or older met criteria for catatonia, with classic Autistic Disorder diagnosed in 11 (37%), atypical autism in 5 (17%), and Asperger Disorder in 14 (47%). Under age 15, no child demonstrated the full syndrome although isolated catatonic symptoms were often observed. In the majority of cases, catatonic symptoms started between 10 and 19 years of age. Five individuals had brief episodes of slowness and freezing during childhood before age 10. Obsessive-compulsive and aggressive behaviors preceded catatonia in some. Visual hallucinations or paranoid ideas were occasionally reported, but no diagnosis of schizophrenia could be made. This study also emphasized additional symptoms of catatonia that may be particularly characteristic of catatonia in autism spectrum disorders, including amotivation, global slowness, and prolonged time to complete previously mastered tasks. It is important to recognize these additional symptoms along the catatonic spectrum, because they may otherwise be erroneously attributed to as oppositional or “stubborn” behavior.
In the second study, 13 (12%) of 120 autistic individuals, between ages 17–40 years, had clinically diagnosed catatonia with severe motor initiation problems (101). Another four individuals had several catatonic symptoms, but did not meet criteria for the full syndrome. Eight of the 13 individuals with catatonia suffered from classic Autistic Disorder; the remaining five were diagnosed with atypical autism. The proportion of those with Autistic Disorder that were diagnosed with catatonia was 11% (8/73). Fourteen percent (5/35) of those with atypical autism had catatonia.
A recent hospital-based study (104) of 101 child and adolescent psychiatric inpatients with "at risk" diagnoses including any autism spectrum disorder, psychotic disorder not otherwise specified, intermittent explosive disorder, mental retardation, neuroleptic malignant syndrome or previously diagnosed catatonia found that 18% of patients met criteria for catatonia, based upon three or more symptoms, including unexplained agitation or excitement, disturbed or unusual movements, reduction in movement, reduction or loss of speech and repetitive/stereotyped movements. The authors emphasized poor recognition of catatonia in these pediatric conditions, including, but not limited to, pervasive development disorders.
Functional regression in daily self-care, social and educational activities may also be a prominent feature of the catatonic presentation in autism. In many cases, the ability to self-feed, dress and bathe, or participate in previously mastered leisure and educational activities may be sharply compromised. Additionally, continence may be lost (22).
7 Post-traumatic Catatonia: The Ultimate Motor Response to Fear
Catatonia has been called “the ultimate response to fear” (113), representing a common final pathway in the response to impending doom, analogous to the animal defense strategy of tonic immobility or freezing (114). Tonic immobility is a last-ditch animal defense strategy against entrapment by a predator within a sequence of freezing-flight-fight-tonic immobility.
This notion is supported by observations that catatonia can develop after severe traumatic events in children and adolescents (115–117). For example, a recent case was reported of a 14-year-old-girl with severe catatonia precipitated by emotional turmoil due to cyber-bullying who was successfully treated with ECT and amantadine (118). In an epidemiologic study of 1098 adolescents, those who experienced bullying three or more times a month were 3.43 times as likely to report increasing psychotic experiences (119). The case-report extends findings that adolescent bullying increases the risk for psychotic experiences by linking cyber-bullying, an intrusive form of bullying, to onset of catatonia.
Shah & Wing (120) found that ongoing stressful experiences often precede the development of catatonia in autistic young adults. Life events, the loss of routine and structure, experiences of loss, conflicts with parents, caregivers, or peers, and discrepancies between the higher functioning autistic individual’s capabilities and the expectations of parents, can precipitate catatonia.
Observations that catatonia follows overwhelming anxiety due to trauma or perceived danger, the positive response of catatonia to anxiolytics such as benzodiazepines or barbiturates, and psychogenic theories of catatonia (121) are particularly applicable to people with psychosis or autism spectrum disorders due to their increased social, cognitive, and sensory vulnerabilities (115, 122). It is recommended that patients with catatonia are assessed for traumatic and abusive events in family and broader environments in addition to medical causes for catatonia.
8 Mechanism of Catatonia
Although the etiology and pathophysiology of catatonia are unknown, findings about the occurrence of catatonia in a wide variety of conditions, including autism, suggests that the available models (66, 123) to study catatonia should be broadened to include models of developmental impairment.
Historically, the study of experimental catatonia in animals induced by bulbocapnine injections was introduced in 1928 by de Jong and Baruk (124). Bulbocapnine is an alkaloid resembling apomorphine, a dopamine agonist. Later mescaline was found to produce similar effects in animals, along with reserpine, adrenocorticotropic hormone (ACTH), and chlorpromazine. Baruk also described hypopituitary, hepatic, and asphyxia models of catatonia. Table 27.9 shows an overview of tentative clinical (66) and corresponding experimental models.
An appropriate focus is the area of stereotypic or repetitive movement abnormalities which are considered cardinal symptoms of several disorders including catatonia, autism, stereotypic movement disorder, and tic disorders (when tics are viewed as sudden and non-rhythmic variants of stereotypy) (4, 130). Motor stereotypy constitutes a separate domain with increasing evidence of a neurobiological mechanism involving neuroadaptations in cortico-basal ganglia pathways arising from the interplay of genetic and experiential factors (125, 131).
Catatonia has been associated with Prader-Willi Syndrome (PWS), a genetic disorder arising from the lack of expression of genes on the paternally derived chromosome 15q11-q13 (22, 105). The behavioral phenotype of PWS consists of catatonic symptoms, stereotypies, compulsive self-injury, excessive sleepiness or unresponsiveness, and psychosis. The abnormal pattern of expression of sex-specific imprinted genes on 15q11-13 (containing a cluster of GABAA receptor subunit genes) may increase risk for catatonia in PWS.
Several lines of evidence suggest the importance of neuroendocrine abnormalities in catatonia. A clinical endocrine model is provided by the Kleine-Levin Syndrome (KLS), a poorly understood syndrome, occurring mostly in male adolescents, that is characterized by recurrent episodes of excessive sleep, and behavioral abnormalities such as hyperphagia or hypersexuality, in which altered diencephalic function is considered a central feature. KLS has been proposed as a type of episodic adolescent-onset catatonia based on the symptom overlap between KLS and catatonia and on the profound response of all symptoms, including “hypersomnia”, to lorazepam (19).
The overlap between catatonia and pediatric autoimmune (limbic) encephalitis (32, 36) suggests involvement of autoimmunity and cerebral antibodies. There are now a few reports that show the efficacy of treatment with high-dose benzodiazepine and ECT in the recently coined and purportedly autoimmune anti-NMDA receptor encephalitis (36, 48, 49).
The finding that severe trauma may precipitate catatonia raises questions about mechanisms by which trauma leads to catatonia or other disorders. The biological pathways of early trauma leading to psychiatric and medical disorders are thought to encompass endocrine, immune, electrophysiological, and neuropsychological factors as well structural changes in the developing brain (132–136). The likely involvement in catatonia of central GABA function and its major role in central integration of hypothalamic-pituitary-adrenal stress responses in the basal forebrain and hypothalamus (137) is an important lead for future clinical and experimental studies assessing early trauma as contributing to the development of catatonia.
A speculative model concerns developmental catatonia, i.e., the occurrence of catatonia in young children causing over time irreversible psychopathology similar to autistic impairment (138, 139). Prenatal exposure to valproic acid (VPA) is a promising animal model of early-onset catatonia that has also been studied as a model for autism (129). Offspring of female rats injected with VPA on day 12.5 of gestation show brain abnormalities including smaller cerebella with fewer Purkinje cells. The rats exhibit catatonic-like behaviors appearing before puberty that include lower sensitivity to pain, diminished acoustic prepulse inhibition, repetitive hyperactivity, unresponsiveness and withdrawal.
9 Novel Vagal Theory of Catatonia
Although catatonia is considered primarily a motor syndrome, forty percent of catatonic patients show autonomic symptoms including abnormalities of temperature, blood pressure, pulse rate, respiratory rate, and perspiration (3, 22). Forty-five percent of pediatric cases show urinary-fecal incontinence (22), another feature of autonomous dysfunction. Some cases show bradycardia (94, 140) and bronchorrhea (141), indicative of strong vagal activity. Autonomic dysfunction is the hallmark of malignant catatonia (2, 3), its drug-induced variant Neuroleptic Malignant Syndrome (142), and aseptic encephalitis with catatonic symptoms, including the recently coined anti-NMDAR encephalitis (19, 32, 47). Early studies also support that there is autonomic dysfunction in catatonia (143, 144).
Autonomic abnormalities in catatonia support the image that catatonia represents a common end state response to feelings of impending doom across a wide range of medical and psychiatric disorders, finding its evolutionary counterpart in tonic immobility (114). Volchan et al. (145) found signs of tonic immobility, such as reduced body sway, increased heart rate, and diminished heart rate variability, in trauma-exposed patients with PTSD while listening to their autobiographical trauma, implying that tonic immobility is preserved in humans as an involuntary defensive strategy.
Autonomic dysfunction in catatonia implies involvement of the autonomic nervous system that consists of the parasympathetic subsystem, mediated by the vagus nerve, and the sympathetic subsystem, mediated by sympathetio-adrenal circuits in the spinal cord. A useful framework is the Polyvagal Theory that was first formulated by Porges in 1995 (146, 147).
The Polyvagal Theory poses that two different vagal branches control different behavioral responses to threat, and that a human immobility response with behavioral (stupor) and metabolic shutdown (increased sweating, hypoventilation, decreased peristalsis, urinary and fecal incontinence, and vasovagal responses) represents the most primitive response to perceived imminent danger when fight-flight reactions fail or are not available.
A separate set of unmyelinated vagal fibers projecting to the nucleus dorsalis of the vagal nerve is thought to mediate this response through efferent fibers to the diaphragm, heart, gastrointestinal tract, lungs, pancreas, and other visceral organs. This reflex is adaptive in reptiles but potentially lethal in humans. Catatonia resonates clearly in the description of the immobility response and yet is not recognized or acknowledged in the Polyvagal Theory as its clinical manifestation.
A vagal theory of catatonia (148) supports abnormalities in a wide range of functions, regulated by the efferent vagal nerve and associated with catatonia, encompassing brain electrical and motor circuitry function, neurotransmitters, neuroendocrine and immune function. Toxic and medical factors may also trigger catatonia through afferent vagal activation. It is an intriguing thought that the vagal nerve, whose fibers are eighty percent afferent, may also be involved in signaling, through its afferent pathways, information to the brain about “internal” (toxic, immune, infectious, metabolic) precipitants of catatonia. Studies support effects on vagal tone by benzodiazepines (149–151), zolpidem (152) (a non-benzodiazepine sedative that has been effectively used in catatonia) and ECT (153), as predicted and required by a vagal theory.
Studies are warranted into various aspect of autonomic dysfunction of catatonia. There is evidence that increased anxiety and arousal accompany the development of catatonia (115). These observations beg for more scrutiny, using modern techniques, along the lines of earlier studies (143, 144). A vagal theory intimates use of vagal nerve stimulatory techniques as novel treatments for catatonia. The Food and Drug Administration (FDA) approved intermittent stimulation of the left vagal nerve (Vagal Nerve Stimulation; VNS) as adjunctive therapy for partial-onset epilepsy in July 1997 and for treatment-resistant depression in 2005. Improvement in the control of seizures has been well documented with VNS. The effects in treatment-resistant depression remain controversial. Non-epileptic benefits in the quality of life and changes in behavior have not been as well documented, except for the enhancement of short-term memory (154). Further studies need to assess if vagal nerve stimulation has any role in the treatment and relapse prevention of catatonia. Several patients require maintenance ECT for months and even years to avoid relapses into catatonia. Although maintenance ECT is safe and without neuropsychological sequelae in such patients, finding adjuvant or alternative preventive treatments would be very valuable.
10 Conclusions
There have been advances in demarcating catatonia in a wide variety of patients as a treatable condition that requires prompt identification. Benzodiazepines and electroconvulsive therapy remain first-line interventions. The new DSM-5 Catatonia NEC purports to improve proper diagnosis and early treatment and to intensify research of this condition.
References
Wernicke C. Grundriss der Psychiatrie in klinischen Vorlesungen (Parts I-III). Leipzig: Thieme; 1900.
Caroff S, Mann S, Francis A, Fricchione G. Catatonia. From Psychopathology to Neurobiology. Arlington, VA: American Psychiatric Association Publishing; 2004.
Fink M, Taylor M. Catatonia. A clinician's guide to diagnosis and treatment. Cambridge: University Press; 2003.
Dhossche DM, Reti IM, Shettar SM, Wachtel LE. Tics as signs of catatonia: electroconvulsive therapy response in 2 men. J ECT 2010;26:266–269.
Wachtel LE, Dhossche DM. Self-injury in autism as an alternate sign of catatonia: implications for electroconvulsive therapy. Med Hypotheses 2010;75:111–114.
Dhossche D, Cohen D, Ghaziuddin N, Wilson C, Wachtel LE. The study of pediatric catatonia supports a home of its own for catatonia in DSM-5. Med Hypotheses 2010;75:558–560.
Dhossche D, Wilson C, Wachtel L. Catatonia in childhood and adolescence: implications for the DSM-5. Primary Psychiatry 2010;17:35–39.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, (5th Edition) (DSM-5). Arlington, VA: American Psychiatric Association Publishing 2013.
Kahlbaum K. Die Katatonie oder das Spannungsirresein. Berlin: Verlag August Hirshwald; 1874.
Morrison J. Catatonia: retarded and excited types. Arch Gen Psychiatry 1973;28:39–41.
Abrams R, Taylor M. Catatonia: a prospective clinical study. Arch Gen Psychiatry 1976;33:579–581.
Gelenberg A. The catatonic syndrome. Lancet 1976;1:1339–1341.
Braunig P, Kruger S, Shugar G. Prevalence and clinical significance of catatonic symptoms in mania. Compr Psychiatry 1998;39:35–46.
Wing L, Attwood A. Syndromes of autism and atypical development. In: Cohen D, Donnellan A, eds. Handbook of autism and pervasive developmental disorders. New York: Wiley-Interscience; 1987:3–19.
Realmuto G, August G. Catatonia in autistic disorder: a sign of comorbidity or variable expression. J Autism Dev Disorder 1991;21:517–528.
Dhossche D, Wing L, Ohta M, Neumarker K-J, eds. Catatonia in Autism Spectrum Disorders. San Diego, California and London, UK: Elsevier Academic Pres; 2006.
Wachtel L, Kahng S, Dhossche D, Cascella N, Reti I. Electroconvulsive Therapy for catatonia in an autistic girl. Am J Psychiatry 2008;165:329–333.
Creten C, van der Zwaan S, Blankespoor RJ, Maatkamp A, Nicolai J, van Os J, Schieveld JN. Late onset autism and anti-NMDA-receptor encephalitis. Lancet 2011;378:98.
Dhossche DM, Wachtel LE. Catatonia is hidden in plain sight among different pediatric disorders: a review article. Pediatr Neurol 2010;43:307–315.
Dhossche D, Bouman N. Catatonia in children and adolescents (letter). J Am Acad Child Adolesc Psychiatry 1997;36:870–871.
Jap SN, Ghaziuddin N. Catatonia Among Adolescents With Down Syndrome: A Review and 2 Case Reports. J ECT 2011;27:334–337.
Dhossche D, Bouman N. Catatonia in an adolescent with Prader-Willi Syndrome. Ann Clin Psychiatry 1997;4:247–253.
Sullivan B, Dickerman J. Steroid-associated catatonia: report of a case. Pediatrics 1979;63:677–679.
Elia J, Dell M, Friedman D, Zimmerman RA, Balamuth N, Ahmed AA, Pati S. PANDAS with catatonia: a case-report. Therapeutic response to lorazepam and plasmapheresis. J Am Acad Child Adolesc Psychiatry 2005;44:1145–1150.
Davis E, Borde M. Wilson's disease and catatonia. Br J Psychiatry 1993;162:256–259.
Perisse D, Amoura Z, Cohen D, Saintigny P, Mekhloufi F, Mazet P, Piette JC. Case study: effictiveness of plasma exchange in an adolescent with systemic lupus erythematosus and catatonia. J Am Acad Child Adolesc Psychiatry 2003;42:497–499.
Wang H-Y, Huang T-L. Benzodiazepines in catatonia associated with systemic lupus erythematosus. Psychiatry Clin Neurosci 2006;60:768–770.
Thakur A, Jagadheesan K, Dutta S, Sinha V. Incidence of catatonia in children and adolescents in a pediatric psychiatric clinic. Aust NZ J Psychiatry 2003;37:200–203.
Woodbury M, Woodbury M. Neuroleptic-induced catatonia as a stage in the progression toward neuroleptic malignant syndrome. J Am Acad Child Adolesc Psychiatry 1992;31:1161–1164.
Revuelta E, Bordet R, Piquet T, Ghawche F, Destee A, Goudemand M. Acute catatonia and neuroleptic malignant syndrome. A case of infantile psychosis. Encephale 1999;20:351–354.
Cavanna A, Robertson M, Critchley H. Catatonic signs in Gilles de la Tourette syndrome. Cogn Behav Neurol 2008;21:34–37.
Dhossche D, Fink M, Shorter E, Wachtel LE. Anti-NMDA receptor encephalitis versus pediatric catatonia (letter to the editor). Am J Psychiatry 2011;168:749–750.
Consoli A, Ronen K, An-Gourfinkel I, Barbeau M, Marra D, Costedoat-Chalumeau N, Montefiore D, Maksud P, Bonnot O, Didelot A, Amoura Z, Vidailhet M, Cohen D. Malignant catatonia due to anti-NMDA-receptor encephalitis in a 17-year-old girl: case report. Child Adolesc Psychiatry Ment Health 2011;5:15.
Lee A, Glick D, Dinwiddie S. Electroconvulsive therapy in a pediatric patient with malignant catatonia and paraneoplastic limbic encephalitis. J ECT 2006;22:267–270.
Schimmel M, Bien C, Vincent A, Schenk W, Penzien J. Successful treatment of anti-N-methyl-D-aspartate receptor encephalitis presenting with catatonia. Arch Dis Child 2009;94:314–316.
Agarwala P. Catatonia in an adolescent with anti-N-Methyl-D-Aspartate receptor encephalitis: successful treatment with high-dose lorazepam. Resident J 2011:10–11.
Ono Y, Manabe Y, Hamakawa Y, Omori N, Abe K. Steroid-responsive encephalitis lethargica syndrome with malignant catatonia. Intern Med 2007;46:307–310.
Ali S, Welch C, Park L, Pliakas AM, Wilson A, Nicolson S, Huffman J, Fricchione GL. Encephalitis and catatonia treated with ECT. Cogn Behav Neurol 2008;21:46–51.
Kanner L. The occurrence of cataleptic phenomena in children. J Pediatrics 1934;5:330–340.
Spitz RA. Hospitalism. An inquiry into the genesis of psychiatric conditions in early childhood. Psychoanalytical Study Child 1945;1:53–74.
Spitz RA. Hospitalism. A follow-up report on investigation described in volume 1 1945. Psychoanalytical Study Child 1946;2:113–117.
Bodegard G. Pervasive loss of function in asylum-seeking children in Sweden. Acta Paediatr 2005;94:1706–1707.
Bodegard G. Depression-withdrawal reaction in refugee children. An epidemic of a cultural-bound syndrome or an endemic of re-traumatized refugees? Acta Paediatr 2010;99:959.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed.). Arlington, VA: American Psychiatric Association Publishing; 1994.
McCall W, Mann S, Shelp F, Caroff S. Fatal pulmonary embolism in the catatonic syndrome: Two case reports and a literature review. J Clin Psychiatry 1995;56:21–25.
Lachner C, Sandson N. A case of catatonia-induced deep venous thrombosis. Psychosomatics 2003;44:512–514.
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098.
Braakman HM, Moers-Hornikx VM, Arts BM, Hupperts RM, Nicolai J. Pearls & Oy-sters: electroconvulsive therapy in anti-NMDA receptor encephalitis. Neurol 2010;75:e44–6.
Matsumoto T, Matsumoto K, Kobayashi T, Kato S. Electroconvulsive therapy can improve psychotic symptoms in anti-NMDA-receptor encephalitis. Psychiatry Clin Neurosci 2012;66:242–243.
Stauder K. Die todliche Katatonie. Arch Psychiatr Nervenkrank 1934;102:614–634.
Starkstein S, Petracca G, Teson A, Chemerinski E, Merello M, Migliorelli R, Leiguarda R. Catatonia in depression: prevalence, clinical correlates, and validation of a scale. J Neurol Neurosurg Psychiatry 1996;60:326–332.
Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia: I: Rating scale and standardized examination. Acta Psychiatr Scand 1996;93:129–136.
Northoff G, Koch A, Wenke J, Eckert J, Böker H, Pflug B, Bogerts B. Catatonia as a psychomotor syndrome: a rating scale and extrapyramidal motor symptoms. Mov Disord 1999;14:404–416.
Braunig P, Kruger S, Shugar G, Hoffler J, Borner I. The catatonia rating scale I — development, reliability, and use. Compr Psychiatry 2000;41:147–158.
Wong E, Ungvari G, Leung S, Tang W. Rating catatonia in patients with chronic schizophrenia: Rasch analysis of the Bush–Francis Catatonia Rating Scale. Int J Methods Psychiatr Res 2007;16:161–170.
Carroll BT, Kirkhart R, Ahuja N, Soovere I, Lauterbach EC, Dhossche D, Talbert R. Katatonia: a new conceptual understanding of catatonia and a new rating scale. Psychiatry 2008;5:42–50.
Sienaert P, Rooseleer J, De Fruyt J. Measuring catatonia: a systematic review of rating scales. J Affect Disord 2011;135:1–9.
Kirkhart R, Ahuja N, Lee JW, Ramirez J, Talbert R, Faiz K, Ungvari GS, Thomas C, Carroll BT. The detection and measurement of catatonia. Psychiatry 2007;4:52–56.
McCall WV, Shelp FE, McDonald WM. Controlled investigation of the amobarbital interview for catatonic mutism. Am J Psychiatry 1992;149:202–206.
Naples M, Hackett T. The amytal interview: history and current uses. Psychosomatics 1978;19:98–105.
Perry JC, Jacobs D. Overview: clinical applications of the Amytal interview in psychiatric emergency settings. Am J Psychiatry 1982;139:552–559.
Panzer M, Grunhaus L. The diazepam interview: an underutilized diagnostic procedure? Ann Clin Psychiatry 1991;3:73–78.
Bleckwenn W. The production of sleep and rest in psychotic cases. Arch Neurol Psychiatry 1930;24:365–372.
Bolton PF, Carcani-Rathwell I, Hutton J, Goode S, Howlin P, Rutter M. Epilepsy in autism: features and correlates. Br J Psychiatry 2011;198:289–294.
Tuchman R, Cuccaro M. Epilepsy and autism: neurodevelopmental perspective. Current Neurol Neurosci Rep 2011;11:428–434.
Dhossche DM, Stoppelbein L, Rout UK. Etiopathogenesis of catatonia: generalizations and working hypotheses. J ECT 2010;26:253–258.
Fink M. The intimate relationship between catatonia and convulsive therapy. J ECT 2010;26:243–245.
Lahutte B, Cornic F, Bonnot O, Consoli A, An-Gourfinkel I, Amoura Z, Sedel F, Cohen D. Multidisciplinary approach of organic catatonia in children and adolescents may improve treatment decision making. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1393–1398.
Fink M, Taylor M. Neuroleptic malignant syndrome is malignant catatonia, warranting treatments efficacious for catatonia. Prog Neuropsychopharmacol Biol Psychiatry 2006;30:1182–1183.
Seitz DP, Gill SS. Neuroleptic malignant syndrome complicating antipsychotic treatment of delirium or agitation in medical and surgical patients: case reports and a review of the literature. Psychosomatics 2009;50:8–15.
Carroll B, Lee JW, Appiani F, Thomas C. Pharmacotherapy of Catatonia. Primary Psychiatry 2010;17:41–47.
Wachtel LE, Dhossche DM. Challenges of electroconvulsive therapy for catatonia in youth with intellectual disabilities: another tomato effect? J ECT 2012;28:151–153.
Bush G, Fink M, Petrides G, Dowling F, Francis A. Catatonia. II. Treatment with lorazepam and electroconvulsive therapy. Acta Psychiatri Scand 1996;93:137–143.
Thomas P, Rascle C, Mastain B, Maron M, Vaiva G. Test for catatonia with zolpidem. Lancet 1997;349:702.
Yi J, Torres J, Azner Y, Vaidya P, Schiavi A, Reti IM. Flumazenil Pretreatment in Benzodiazepine-Free Patients: A Novel Method for Managing Declining ECT Seizure Quality. J ECT 2012;28:185–189.
Kellner CH, Knapp GR, Petrides G, Rummans TA, Husain MM, Rasmussen K, Mueller M, Bernstein HJ, O'Connor K, Smith G, Biggs M, Bailine SH, Malur C, Yim E, McClintock S, Sampson S, Fink M. Continuation electroconvulsive therapy vs pharmacotherapy for relapse prevention in major depression: a multisite study from the Consortium for Research in Electroconvulsive Therapy (CORE). Arch Gen Psychiatry 2006;63:1337–1344.
Petrides G, Dhossche D, Fink M, Francis A. Continuation ECT: relapse prevention in affective disorders. Convul Ther 1994;10:189–194.
Lippman S, Manshadi M, Wehry M, Byrd R, Past W, Keller W, Schuster J, Elam S, Meyer D, O'Daniel R. 1,250 electroconvulsive treatments without evidence of brain injury. Br J Psychiatry 1985;147:203–204.
Scalia J, Lisanby SH, Dwork AJ, Johnson JE, Bernhardt ER, Arango V, McCall WV. Neuropathologic examination after 91 ECT treatments in a 92-year-old woman with late-onset depression. J ECT 2007;23:96–98.
Devanand DP, Verma AK, Tirumalasetti F, Sackeim HA. Absence of cognitive impairment after more than 100 lifetime ECT treatments. Am J Psychiatry 1991;148:929–932.
Wijkstra J, Nolen WA. Successful maintenance electroconvulsive therapy for more than seven years. J ECT 2005;21:171–173.
Zisselman M, Rosenquist P, Curlik S. Long-term weekly continuation electroconvulsive therapy: a case-series. J ECT 2007;23:274–277.
Wachtel LE, Hermida A, Dhossche DM. Maintenance electroconvulsive therapy in autistic catatonia: a case series review. Prog Neuropsychopharmacol Biol Psychiatry 2010;34:581–587.
Dhossche D, Shettar S, Kumar T, Burt L. Electroconvulsive therapy for malignant catatonia in adolescence. Southern Med J 2009;102:1170–1172.
Wachtel LE, Griffin MM, Dhossche DM, Reti IM. Brief report: Electroconvulsive therapy for malignant catatonia in an autistic adolescent. Autism 2010;14:349–358.
Consoli A, Benmiloud M, Wachtel L, Dhossche D, Cohen D, Bonnot O. Electroconvulsive therapy in adolescents with the catatonia syndrome: efficacy and ethics. J ECT 2010;26:259–265.
Slooter A, Braun K, Balk F, van Nieuwenhuizen O, van der Hoeven J. Electroconvulsive therapy of malignant catatonia in childhood. Pediatr Neurol 2005;32:190–192.
Fink M. Recognizing NMS as a type of catatonia. Neuropsychiatr Neuropsychol Behav Neurol 1995;8:75–76.
Rempel WE, Lu M, el Kandelgy S, Kennedy CF, Irvin LR, Mickelson JR, Louis CF. Relative accuracy of the halothane challenge test and a molecular genetic test in detecting the gene for porcine stress syndrome. J Animal Sci 1993;71:1395–1399.
Francis A, Lopez-Canino A. Delirium with catatonic features. Psychiatric Times 2009;26:32–36.
Rizos DV, Peritogiannis V, Gkogkos C. Catatonia in the intensive care unit. Gen Hosp Psychiatry 2011;33:e1–e2.
Hem E, Andreassen O, Robasse J-M, Vatnaland T, Opjodsoen S. Should catatonia be part of the differential diagnosis of coma? Nord J Psychiatry 2005;59:528–530.
Benegal V, Hingorani S, Khanna S. Idiopathic catatonia: validity of the concept. Psychopathology 1993;26:41–46.
Freudenreich O, McEvoy J, Goff D, Fricchione G. Catatonic coma with profound bradycardia. Psychosomatics 2007;48:74–78.
Bender K, Feutrill J. Comatoid catatonia. Aust NZ J Psychiatry 2000;34:169–170.
Cornic F, Consoli A, Tanguy M, Bonnot O, Périsse D, Tordjman S, Laurent C, Cohen D. Association of adolescent catatonia with increased mortality and morbidity: evidence from a prospective follow-up study. Schizophr Res 2009;113:233–240.
Green W, Campbell M, Hardesty A, Grega DM, Padron-Gayol M, Shell J, Erlenmeyer-Kimling L. A comparison of schizophrenic and autistic children. J Am Acad Child Psychiatry 1984;23:399–409.
Moise FN, Petrides G. Case study: electroconvulsive therapy in adolescents. J Am Acad Child Adolesc Psychiatry 1996;35:312–318.
Wing L, Shah A. Catatonia in autistic spectrum disorders. Br J Psychiatry 2000;176:357–362.
Cohen D, Nicolas J, Flament MF, Périsse D, Dubos PF, Bonnot O, Speranza M, Graindorge C, Tordjman S, Mazet P. Clinical relevance of chronic catatonic schizophrenia in children and adolescents: evidence from a prospective naturalistic study. Schizophr Bull 2005;15:301–308.
Billstedt E, Gillberg IC, Gillberg C. Autism after adolescence: population-based 13- to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. J Autism Dev Disord 2005;35:351–360.
Ohta M, Kano Y, Nagai Y. Catatonia in individuals with autism spectrum disorders in adolescence and early adulthood: a long-term prospective study. Int Rev Neurobiol 2006;72:41–54.
Consoli A, Boulicot V, Cornic F, Fossati P, Barbeau M, Cohen D. Moderate clinical improvement with maintenance ECT in a 17-year-old boy with intractable catatonic schizophrenia. Eur Child Adolesc Psychiatry 2009;18:250–254.
Ghaziuddin N, Dhossche D, Marcotte K. Retrospective chart review of catatonia in child and adolescent psychiatric patients. Acta Psychiatr Scand 2012;125:33–38.
Verhoeven W, Tuinier S. Prader-Willi syndrome: atypical psychoses and motor dysfunctions. Int Rev Neurobiol 2006;72:119–130.
Kakooza-Mwesige A, Wachtel L, Dhossche D. Catatonia in autism: implications across the life span. Eur Child Adolesc Psychiatry 2008;17:327–335.
Dhossche D, Reti I, Wachtel L. Catatonia and Autism: A historical review, with implications for ECT. J ECT 2009;25:19–22.
Wachtel LE, Griffin M, Reti I. Electroconvulsive Therapy in a Man With Autism Experiencing Severe Depression, Catatonia, and Self-Injury. J ECT 2010;96:70–73.
Wachtel LE, Jaffe R, Kellner CH. Electroconvulsive therapy for psychotropic-refractory bipolar affective disorder and severe self-injury and aggression in an 11-year-old autistic boy. Eur Child Adolesc Psychiatry 2011;20:147–152.
Volkmar F, Cohen D. Comorbid association of autism and schizophrenia. Am J Psychiatry 1991;148:1705–1707.
Jap SN, Ghaziuddin N. Catatonia among adolescents with Down syndrome: a review and 2 case reports. J ECT 2011;27:334–337.
Consoli A, Raffin M, Laurent C, Bodeau N, Campion D, Amoura Z, Sedel F, An-Gourfinkel I, Bonnot O, Cohen D. Medical and developmental risk factors of catatonia in children and adolescents: a prospective case-control study. Schizophr Res 2012;137:151–158.
Perkins RJ. Catatonia: the ultimate response to fear? Aust N Z J Psychiatry 1982;16:282–287.
Gallup G, Maser J. Tonic immobility: Evolutionary underpinnings of human catalepsy and catatonia. In: Maser J, Seligman M, eds. Psychopathology: Experimental Models. San Francisco: Freeman; 1977:334–357.
Dhossche DM, Ross CA, Stoppelbein L. The role of deprivation, abuse, and trauma in pediatric catatonia without a clear medical cause. Acta Psychiatr Scand 2012;125:25–32.
Bozkurt H, Mukaddes NM. Catatonia in a child with autistic disorder. Turk J Pediatr 2010;52:435–438.
Saito S, Yamaga K, Kobayashi T, Kato S. A case of Asperger’s disorder with catatonia originally suspected of being catatonic schizophrenia. Seishin Shinkeigaku Zasshi 2011;113:241–247.
Goetz M, Kitzlerova E, Hrdlicka M, Dhossche D. Combined use of ECT and amantadine in adolescent catatonia precipitated by cyber-bullying. J Child Adolesc Psychopharmacol 2013;23:228–231.
Mackie CJ, O'Leary-Barrett M, Al-Khudhairy N, Castellanos-Ryan N, Struve M, Topper L, Conrod P. Adolescent bullying, cannabis use and emerging psychotic experiences: a longitudinal general population study. Psychol Med 2012:1–12.
Shah A, Wing L. Psychological approaches to chronic catatonia-like deterioration in autism spectrum disorders. Int Rev Neurobiol 2006;72:245–264.
Moskowitz AK. "Scared stiff": catatonia as an evolutionary-based fear response. Psychol Rev 2004;111:984–1002.
Dhossche D. Catatonia: the ultimate yet treatable motor reaction to fear in autism. Autism-Open Access 2011;1:e103.
Kanes S. Animal models. In: Caroff S, Mann SC, Francis A, Fricchione GL, eds. Catatonia From Psychopathology to Neurobiology. Arlington, VA: American Psychiatric Association Publishing; 2004:189–200.
De Jong HH, Barruk H. A clinical and experimental study of the catatonic syndrome (Étude comparative expérimentale et clinique des manifestations du syndrome catatonique). H Revue Neurol 1929;21.
Lewis MH, Tanimura Y, Lee LW, Bodfish JW. Animal models of restricted repetitive behavior in autism. Behav Brain Res 2007;176:66–74.
Wong M, Wozniak DF, Yamada KA. An animal model of generalized nonconvulsive status epilepticus: immediate characteristics and long-term effects. Exp Neurol 2003;183:87–99.
Nakatani J, Tamada K, Hatanaka F, Ise S, Ohta H, Inoue K, Tomonaga S, Watanabe Y, Chung YJ, Banerjee R, Iwamoto K, Kato T, Okazawa M, Yamauchi K, Tanda K, Takao K, Miyakawa T, Bradley A, Takumi T. Abnormal behavior in a chromosome-engineered mouse model for human 15q11-13 duplication seen in autism. Cell 2009;137:1235–1246.
Jeong HK, Jou I, Joe EH. Systemic LPS administration induces brain inflammation but not dopaminergic neuronal death in the substantia nigra. Exp Mol Med 2010;42:823–832.
Wagner GC, Reuhl KR, Cheh M, McRae P, Halladay AK. A new neurobehavioral model of autism in mice: pre- and postnatal exposure to sodium valproate. J Autism Dev Disord 2006;36:779–793.
Trivedi H, Mendelowitz A, Fink M. Gilles de la Tourette form of catatonia: response to ECT. J ECT 2003;19:115–117.
Singer HS. Motor stereotypies. Semin Pediatr Neurol 2009;16:77–81.
Ali I, Salzberg MR, French C, Jones NC. Electrophysiological insights into the enduring effects of early life stress on the brain. Psychopharmacology (Berl) 2011;214:155–173.
Charmandari E, Kino T, Souvatzoglou E, Chrousos GP. Pediatric stress: hormonal mediators and human development. Horm Res 2003;59:161–179.
De Bellis MD, Baum AS, Birmaher B, Keshavan MS, Eccard CH, Boring AM, Jenkins FJ, Ryan ND. A.E. Bennett Research Award. Developmental traumatology. Part I: Biological stress systems. Biol Psychiatry 1999;45:1259–1270.
De Bellis MD, Keshavan MS, Clark DB, Casey BJ, Giedd JN, Boring AM, Frustaci K, Ryan ND. A.E. Bennett Research Award. Developmental traumatology. Part II: Brain development. Biol Psychiatry 1999;45:1271–1284.
Pechtel P, Pizzagalli DA. Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology (Berl) 2011;214:55–70.
Herman J, Cullinan W. Neurocircuitry of stress: central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci 1997;20:78–84.
Dhossche D. Autism as early expression of catatonia. Med Sci Monit 2004;10:RA31–39.
Dhossche D, Rout U. Are autistic and catatonic regression related? A few working hypotheses involving GABA, Purkinje cell survival, neurogenesis, and ECT. Int Rev Neurobiol 2006;72:55–79.
Wachtel L, Griffin M, Dhossche D, Reti I. Electroconvulsive therapy for malignant catatonia in an autistic adolescent. Autism 2010;14:349–358.
Hayashi H, Aoshima T, Otani K. Malignant catatonia with severe bronchorrhea and its response to electroconvulsive therapy. Prog Neuropsychopharmacol Biol Psychiatry 2006;30:310–311.
Gurrera RJ, Caroff SN, Cohen A, Carroll BT, DeRoos F, Francis A, Frucht S, Gupta S, Levenson JL, Mahmood A, Mann SC, Policastro MA, Rosebush PI, Rosenberg H, Sachdev PS, Trollor JN, Velamoor VR, Watson CB, Wilkinson JR. An international consensus study of neuroleptic malignant syndrome diagnostic criteria using the Delphi method. J Clin Psychiatry 2011;72:1222–1228.
Gjessing LR. A review of periodic catatonia. Biol Psychiatry 1974;8:23–45.
Venables PH, Wing JK. Level of arousal and the subclassification of schizophrenia. Arch Gen Psychiatry 1962;7:114–119.
Volchan E, Souza GG, Franklin CM, Norte CE, Rocha-Rego V, Oliveira JM, David IA, Mendlowicz MV, Coutinho ES, Fiszman A, Berger W, Marques-Portella C, Figueira I. Is there tonic immobility in humans? Biological evidence from victims of traumatic stress. Biol Psychol 2011;88:13–19.
Porges SW. Social engagement and attachment: a phylogenetic perspective. Ann N Y Acad Sci 2003;1008:31–47.
Porges SW. The Polyvagal Theory: phylogenetic contributions to social behavior. Physiol Behav 2003;79:503–513.
Dhossche D. Autonomic dysfunction in catatonia in autism: implications of a vagal theory. Autism-Open Access 2012;2:e114.
Adinoff B, Mefford I, Waxman R, Linnoila M. Vagal tone decreases following intravenous diazepam. Psychiatry Res 1992;41:89–97.
Farmer MR, Ross HF, Chowdhary S, Osman F, Townend JN, Coote JH. GABAergic mechanisms involved in the vagally mediated heart rate response to muscle contraction as revealed by studies with benzodiazepines. Clin Auton Res 2003;13:45–50.
Vogel LR, Muskin PR, Collins ED, Sloan RP. Lorazepam reduces cardiac vagal modulation in normal subjects. J Clin Psychopharmacol 1996;16:449–453.
Chen HY, Kuo TB, Shaw FZ, Lai CJ, Yang CC. Sleep-related vagotonic effect of zolpidem in rats. Psychopharmacology (Berl) 2005;181:270–279.
Bar KJ, Ebert A, Boettger MK, Merz S, Kiehntopf M, Jochum T, Juckel G, Agelink MW. Is successful electroconvulsive therapy related to stimulation of the vagal system? J Affect Disord 2010;125:323–329.
Clark KB, Naritoku DK, Smith DC, Browning RA, Jensen RA. Enhanced recognition memory following vagus nerve stimulation in human subjects. Nat Neurosci 1999;2:94–98.
Bumke O. Lehrbuch der Geisterkrankheiten. Second ed. Munich: Bergmann; 1924.
Acknowledgement
The authors thank Edward Shorter, Professor in the History of Medicine and Professor of Psychiatry, University of Toronto, for lending a copy of Oswald Bumke’s 1924 textbook (155).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Dhossche, D.M., Wachtel, L.E., Goetz, M., Sienaert, P. (2016). Catatonia in Psychiatric Illnesses. In: Fatemi, S., Clayton, P. (eds) The Medical Basis of Psychiatry. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2528-5_27
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2528-5_27
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2527-8
Online ISBN: 978-1-4939-2528-5
eBook Packages: MedicineMedicine (R0)