Abstract
Soft tissue calcifications are a relatively common finding on radiographs. Knowledge of the different patterns and locations can lead to accurate diagnosis of various disease processes. This chapter will focus on soft tissue calcification commonly encountered in rheumatology.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Heterotopic Ossification
- Synovial Sarcoma
- Giant Cell Tumor
- Venous Insufficiency
- Idiopathic Inflammatory Myopathy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Overview
Soft tissue calcifications are a relatively common finding on radiographs. Knowledge of the different patterns and locations can lead to accurate diagnosis of various disease processes. This chapter will focus on soft-tissue calcification commonly encountered in rheumatology.
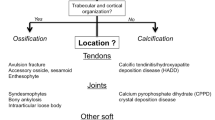
Soft tissue calcification permeates many diseases, and their pathophysiology and clinical implications can vary just like their appearance in radiological evaluation. There is no universally accepted classification; however, the etiology of soft tissue calcification is commonly divided into dystrophic, metastatic, and idiopathic. Dystrophic calcification is by far the most common cause of soft tissue calcification and is present in damaged tissue such as in areas of trauma, inflammation, and devitalized tissue and in neoplasms. Connective tissue disease, hydroxyapatite, and calcium pyrophosphate deposition are included in this subdivision. The VINDICATE acronym provides a more extensive differential for dystrophic calcification (Vascular, Infectious, Neoplastic, Drug, Autoimmune, Trauma, and Extravascular findings).
Metastatic calcifications occurs in the setting of raised calcium and/or phosphorus, with subsequent deposition of calcium salts within normal soft tissue and includes: hyperparathyroidism, hypoparathyroidism, renal osteodystrophy with secondary hyperparathyroidism, milk alkali syndrome, sarcoidosis, hypervitaminosis D, and conditions with extensive bone destruction as can occur in leukemia and myeloma. Idiopathic calcinosis occurs in tumoral calcinosis. Soft tissue ossification should be differentiated from calcification. New bone formation within soft tissues is commonly posttraumatic, physical or thermal injuries (heterotopic ossification), secondary to neurologic disease, or related to benign or malignant tumors. Soft tissue ossification demonstrates an internal trabecular pattern and when fully formed has a corticated rim, both of which are absent in calcification, and thus allows for easy differentiation. The following is an overview of the most commonly encountered soft tissue calcification in clinical practice.
Connective Tissue Disease
Scleroderma and CREST syndrome (calcinosis, Raynaud’s, esophageal dysmotility, sclerodactyly, and telangiectasia) can present with soft tissue calcification (Fig. 16.1). On radiographic evaluation, the lesions are present in the hands and feet as well as areas of the extremities such as the elbow that frequently rub or experience other forms of mild trauma. Hydroxyapatite crystals are frequently present. The soft-tissue calcifications of scleroderma may be either focal or diffuse. A cobblestone appearance is often noted, similar to ESRD or tumoral calcinosis. Calcifications are homogenously dense without associated septa or calcium-fluid level. Another key diagnostic feature of scleroderma-related soft-tissue calcifications are their unique predilection for the hands, being seen in over 50 % of afflicted individuals.
Systemic lupus erythematosus patients may develop periarticular or soft tissue calcification (Fig. 16.2). Calcification can occasionally ulcerate and become secondarily infected.
Other connective tissue diseases which contribute to soft tissue calcification include dermatomyositis and polymyositis. Fascial calcifications are almost invariably secondary to the closely related diseases of dermatomyositis and polymyositis. Each of these entities is an uncommon idiopathic inflammatory myopathy. During healing from episodes of myositis, calcifications develop in areas of necrosis (granulomatous changes incorporating calcium) involving the fascial planes and sometimes the subcutaneous tissues. Calcification develops with recurrent myositis. Radiographically, this manifests as numerous small densities in the appendicular skeleton that go on to coalesce and become sheetlike in appearance along ligaments, tendons, and fascial planes and is termed calcinosis universalis (Fig. 16.3).
Crystal Depositional Diseases
Calcium pyrophosphate depositional disease (CPPD), hydroxyapatite depositional disease (HADD), and gout are reviewed in detail in Chap. 8. Calcific tendinosis is most commonly related to the deposition of hydroxyapatite calcific deposits in dystrophic tendons (Fig. 16.4). This is commonly seen around the shoulder, hip, elbow, and wrist. CPPD crystal deposition can occur in hyaline and fibrocartilage. Classically involved areas include the wrist (triangular fibrocartilage), pubic symphysis, knee (hyaline cartilage and meniscus), hip, and shoulder (Fig. 16.5). Calcification can also occur in the rotator cuff muscle secondary to pyrophosphate crystals. Calcified tophi in gout appear as periarticular soft tissue calcification of variable density (Fig. 16.6).
Tumoral Calcinosis
Tumoral calcinosis is an uncommon familial entity characterized by the presence of large lobulated masses of calcifications located in the subcutaneous juxta-articular soft tissues and extensor aspect of the extremities (Fig. 16.7). While the majority of individuals are asymptomatic, diminished range of motion is a known complication from large juxta-articular masses as well as neuropathic symptoms due to compression of nearby nerves. Lesions develop in the first two decades, commonly in the locations of known bursae around the hip, elbow, and shoulder. Deposits are often cystic and are composed primarily of calcium hydroxyapatite crystals. Calcium levels are normal, and there is often a mild hyperphosphatemia. Patients may develop associated periosteal reaction, a CPPD-like arthropathy and dental abnormalities. Tumoral calcinosis mimics include the many etiologies of metastatic calcifications, most commonly chronic renal failure.
Chronic Renal Disease
Soft tissue calcification in end-stage renal disease is a manifestation of secondary and tertiary hyperparathyroidism. Primary hyperparathyroidism may frequently manifest as soft-tissue calcification independent of renal disease. Such manifestations of primary hyperparathyroidism occur quite frequently. With continued advances in hemodialysis and transplantation, leading to improved survival, the radiographic findings of this disease are encountered with increasing frequency. It is an inappropriately high level of calcium and phosphorus that result in the soft-tissue calcifications commonly seen in these individuals (Fig. 16.8). Another cutaneous manifestation of soft-tissue calcification is calciphylaxis which occurs in end-stage renal disease and renal transplant patients (Fig. 16.9). Calciphylaxis occurs due to calcium deposition in arterioles, which leads to ischemic ulceration of overlying skin. Calciphylaxis is most common in hyperparathyroidism secondary to chronic renal impairment and rarely occurs in the setting of normal renal function.
Benign and Malignant Tumors
Malignancy can also manifest as soft-tissue calcification or ossification within a mass (Fig. 16.10). Malignancies include hemangioma, synovial sarcoma, leiomyosarcoma, giant cell tumor, chondrosarcoma, and osteosarcoma. Calcification of muscle tissue can have manifestations that originate in sarcomatous origins. Radiographs of hemangiomas demonstrate a soft-tissue mass containing phleboliths (as described with arterial/venous calcification), which are seen as round densities ranging from 2 to 8 mm in size with a characteristic central lucency.
Leiomyoma and leiomyosarcoma are benign and malignant neoplasms of mesodermal etiology with smooth muscle differentiation. Recurrent rapid growth can lead to deposition of calcific tissue. Histologically, mineralization in leiomyosarcoma appears to be caused by either nonneoplastic ossification or dystrophic mineralization in the tumor. This feature can cause leiomyosarcomas to be confused with other neoplasms. Extraskeletal chondrosarcoma may present as either a noncalcified or a calcified soft-tissue mass. Calcified masses are common findings in extraskeletal chondrosarcoma, often showing stippled and ring- or arc-like calcifications.
Vascular Calcification
Atherosclerotic vascular disease is a disease of the arterial intima that arises from the abnormal deposition of fatty substances, cholesterol, and calcium. It typically involves the large- and medium-sized arteries. A primary manifestation of vascular disease is arterial calcification. They present as patchy, irregular, plaquelike or even tubular densities of variable shape and size distributed along the path of large- and medium-sized arteries (Fig. 16.11).
Venous insufficiency in the extremities is generally seen in the superficial venous system and therefore mostly limited to the subcutaneous compartment. Their development occurs in the presence of long-standing varicosities and/or thrombus formation. Any partial occlusions can result in vascular turbulence and calcific deposition. These factors result in venous stasis, which in turn leads to calcium deposition along the venous intimal layer. On radiographs of the extremities, venous insufficiency calcification most frequently appears as phleboliths in the subcutaneous tissue. Phleboliths have a ring or oval shape with a central lucency that represents a focus of calcified thrombus. Associated evidence of chronic venous stasis may be present such as soft-tissue edema or in chronic cases adjacent periosteal reaction.
Heterotopic Ossification
Heterotopic ossification is the pathological development of ossification within soft tissue (Fig. 16.12). It is usually related to direct trauma to the affected musculoskeletal tissue or may be neurogenic in origin, e.g., spinal cord injury. Occasionally no precipitating factor is identified. Mechanical traumas include high-voltage electric injury, burns, post joint arthroplasties, and soft-tissue hematomas. The involved area may become swollen, tender, and erythematosus with associated fever with loss of adjacent joint function and diminished mobility although in the majority of cases there are limited symptoms. Radiographically there is a peripheral rim of calcification that proceeds to ossify with initially a lucent center and gradual centripetal advancement of ossification. In addition there is a non-ossified cleft between the ossification and adjacent cortical bone. These two findings are important to help differentiate heterotopic ossification from a more aggressive lesion such as an osteosarcoma.
Further Reading
Abedin M, Tintut Y, Demer LL. Vascular calcification: mechanisms and clinical ramifications. Arterioscler Thromb Vasc Biol. 2004;24(7):1161–70.
Banks KP, Bui-Mansfield LT, Chew FS, Collinson F. A compartmental approach to the radiographic evaluation of soft-tissue calcifications. Semin Roentgenol. 2005;40(4):391–407.
Boulman N, Slobodin G, Rozenbaum M, Rosner I. Calcinosis in rheumatic diseases. Semin Arthritis Rheum. 2005;34(6):805–12.
Olsen KM, Chew FS. Tumoral calcinosis: pearls, polemics, and alternative possibilities. Radiographics. 2006;26(3):871–85.
Vanden Bossche L, Vanderstraeten G. Heterotopic ossification: a review. J Rehabil Med. 2005;37(3):129–36.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this chapter
Cite this chapter
Bobba, R.S., O’Neill, J. (2015). Soft Tissue Calcifications. In: O'Neill, J. (eds) Essential Imaging in Rheumatology. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1673-3_16
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1673-3_16
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1672-6
Online ISBN: 978-1-4939-1673-3
eBook Packages: MedicineMedicine (R0)