Abstract
Chronic immune activation has been shown to be an important driver of HIV-1 disease progression. It has been demonstrated that the humanized mouse model can be infected with HIV-1 and can lead to subsequent CD4+ T cell decline and immune activation similarly to what is observed in human chronic HIV-1 infection. Toll-like receptors (TLRs) and innate immune cells have been shown to play a pivotal role in both HIV-1 control and pathogenesis but attempts to exploit these pathways have been limited. Studies to date suggest that many of the TLR pathways are intact in the humanized mouse model, suggesting that this model can provide a useful tool to examine and manipulate the interplay between immune system and virus in efforts to control viral replication and disease. This review discusses the role of TLRs in HIV-1 infection and their expression and manipulation in the humanized mouse model.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Immune Activation in HIV-1 Infection—Pathogenesis and Priming
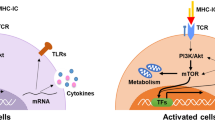
Human immunodeficiency virus (HIV)-1 infection induces activation of the innate and adaptive immune responses, which can mediate both beneficial viral control and detrimental immune pathology . At first encounter with the virus, innate immunity can contribute to the initial restriction of viral replication and plays an important role in the activation of the adaptive immune response. Despite these initial benefits of activating the immune response, the level of ongoing CD8+ T cell activation during chronic HIV-1 infection has been revealed to be a better predictor of HIV-1 disease progression than HIV-1 viral load alone [1]. Furthermore, T cell activation has also been associated with slower CD4+ T cell recovery and enhanced CD4+ T cell apoptosis even when HIV-1 viral load is suppressed by antiretroviral therapy [2, 3] . This elevated immune activation in chronic HIV-1 infection can be driven directly by HIV-1 replication and indirectly through changes in the microbiome, microbial translocation , coinfections , immune deregulation, and lymphoid tissue fibrosis [4–7]. The mechanisms that drive chronic immune activation in HIV-1, therefore, need to be examined and targeted to improve disease management in HIV-1-infected individuals. Examination of HIV-1 has largely been limited to in vitro work with human samples or to studies in nonhuman primate models. The development of a small animal model will allow for easier dissection of the individual mechanisms contributing to HIV-1-associated immune activation, in part through the possibility to perform interventional studies blocking and enhancing individual pathways .
2 Innate Immune System in Humanized Mouse Model
The use of humanized mouse model in examining human immune responses has been carried out in cancer, autoimmunity, viral infections, and vaccinations [8, 9] . The advantage of this model is that it allows for the in vivo manipulation of human immune response through the depletion of specific cell populations [10], administration of inhibiting and activating compounds [10–14] and inoculation with infectious agents [11, 12, 15]. Over 20+ years, the humanized mouse model itself has been modified and adapted, and several different models are now available. The dominant mouse strains recently used for the humanized mouse model can include NOD/SCID[16, 18], NOD/SCID/β2m−/− [18], and NOD/SCID/IL-2rγ−/− (NSG) mice [19, 20], as well as other mouse strains deficient in both Rag2 and IL-2rγ [21, 22]. Furthermore, the method of “humanizing” the mice with a human immune system can also vary and include adoptive transfer of human PBMC (Hu-PBL mice) [23], human CD34+ hematopoietic cells (huCD34+) isolated from cord blood [21] or fetal liver tissue (Hu-HSC mice) [22], co-engraftment with human fetal thymus and liver (SCID-Hu mice) [24], and a combination of human fetal thymus and liver engraftment with injection of huCD34+ cells (BLT mice) [11, 25]. The reconstituted human immune system can also be further enhanced by the administration of cytokines or cytokine-expressing plasmids [26] .
These variations of the mouse models result in differing human immune system developments. Those mice with the NOD/SCID-based backgrounds and Rag2−/−/IL-2rγ−/–-based backgrounds have different reconstitution of immune cells at different tissue sights [27, 28]. However, further enhancements can be used to assist the development of the human immune system and thereby overcome some of the defects in each model. In both the NOD/SCID/β2m−/− and NSG models, human T cells, B cells, and antibodies can successfully develop [29]. Human fetal thymus and liver engraftment allowed for development of the major human T cell subsets and can be improved by the administration of huCD34+ cells (BLT mouse model) , which also have better development of B cells and monocytes [30, 31]. The presence of dendritic cells (DC)s in different humanized mouse models has been demonstrated in bone marrow, blood, and spleen [10]. HuCD34+-transplanted NSG and NOD/SCID/β2m−/− mice develop myeloid dendritic cells (mDCs) [10, 13], plasmacytoid dendritic cells (pDCs) [10, 32], and natural killer (NK) cells [13]. DCs and monocyte development in NSG mice reconstituted with huCD34+ cells can further be enhanced by the administration of GM-CSF and IL-4 [33]. Presence of GM-CSF and IL-4 can also help the development of human T cells, B cells, as well as IgG antibody production [33]. Using mice with the NOD/SCID/β2m−/− or NSG backgrounds also helps to reduce murine NK cell development as compared to NOD/SCID models but unfortunately also result in poor human NK cell reconstitution [34–36]. Administration of human IL-15 and Flt-3 via DNA vectors or recombinant proteins assists in the development of human NK cells in both NOD/SCID, NSG and Balb/c/Rag2−/−/IL-2rγ−/− mouse models reconstituted with huCD34+ cells [26, 34, 37]. Furthermore, the manipulation of the genetic background of the mouse can also be used to enhance development of specific human cell subsets. Knock-ins of human IL-3 and GM-CSF in Rag2−/−/IL-2rγ−/− mice and CSF1 in Balb/c/Rag2−/−/IL-2rγ−/− mice allowed for better macrophage reconstitution following administration with huCD34+ cells [38, 39]. Overall, the genetic background of mice, tissue used for human reconstitution, and any subsequent cytokine treatment can all vary between different humanized mouse models described, each with its strength and weaknesses. The specific humanized mouse model to be used should, therefore, be carefully chosen and depends on the experimental question and the specific immune cell population of interest .
The various improvements to the humanized mouse model allow for the examination of the interplay between the innate and adaptive immune system during viral infections or vaccinations, and provide avenues of intervention. BLT, Hu-HSC, and Hu-PBL mice can be successfully infected with Epstein Barr virus (EBV), which activates and matures human DCs, and in turn, induces both a virus-specific T cell response as well as NK cell response [11, 15, 28, 40]. Utilizing the ability to deplete specific cell populations, depletion of pDCs demonstrated their importance in delaying EBV-induced mortality [15] . Rag2−/−IL-2rγ−/− and NSG mice reconstituted with huCD34+ cells can be infected with influenza A virus and produce inflammatory cytokines and neutralizing antibodies in response to the virus. This demonstrates the ability of the humanized mouse model to imitate the natural multifaceted immune responses that is observed in vivo as compared to in vitro models [33, 38]. HuCD34+-transplanted Balb/c/Rag2−/−/IL-2rγ−/− mouse model can be infected with Hepatitis C virus (HCV) , which not only induced HCV-specific T cell responses but infiltration of the mouse liver with human innate and adaptive immune cells [41]. The same mouse model can also be infected with HSV-2, and when the virus is used in a vaginal challenge model, T cells and NK cells were detected at the mucosa [27]. Both of these viral infection models demonstrated the ability to use these mice to examine local immune responses at specific sites of infection. In addition, the use of attenuated HSV-2 in humanized mice demonstrated protection against subsequent challenge infections [27]. These examples of viral infections in different humanized mouse models demonstrate the possibilities of using these models to examine interactions between human immune cell subsets with each other and the virus, tissue and mucosa specific immunity, and the effects of vaccination. Similar to other viruses, HIV-1 can also successfully infect human immune cells in the humanized mice, thus providing a small animal model alternative to nonhuman primates . Like several other viruses, HIV-1 can infect a range of humanized mouse models including huCD34+-transplanted Rag2−/−/IL-2rγ−/− [42], NSG BLT mice [30, 31], and NOD/SCID BLT mice [31]. Following HIV-1 infection, a decline of CD4+ T cell is observed [30, 31, 42], CD4+ and CD8+ T cell activation develops [30, 31], and antigen-specific T cell and B cell responses are induced [31, 43]. Furthermore, the viral reservoir can be assessed, and initial studies have tested approaches to eliminate the HIV-1 reservoir using the humanized mouse model [44]. This highlighted the possibility of using the BLT humanized mouse model to examine not only the role of innate immunity in HIV-1 infections but also its consequences on the development of the adaptive immunity and subsequent disease outcome .
3 Direct Activation of TLR7/8 by HIV-1 and IFNα-Mediated Immune Activation
HIV-1 ssRNA encodes for multiple TLR7/8 ligands which have been shown to activate pDCs, mDCs, and other immune cells in the in vitro system [45–47] . In pDCs, activation of the TLR7 pathway by HIV-1 leads to the production of IFNα [45–48] and induction of the adaptive T cell response [46, 49]. This has potentially beneficial outcomes as the stimulation of TLRs have demonstrated importance not only in the priming of CD4+ and CD8+ T cells but also in directly modulating the type of adaptive immune response induced [50, 51]. However, the persistent production of IFNα might be detrimental in the setting of a chronic persistent infection [52, 53]. In SIV infection of nonhuman primates , pDCs in rhesus macaques, the pathogenic host of SIV, produce large quantities of IFNα [54], while in sooty mangabeys, the natural host with reduced pathogenesis [55], lower IFNα levels are observed in chronic infection [54, 56, 57] . This is also observed in the expression of interferon-stimulated genes (ISGs), which are elevated in SIV-infected rhesus macaques [58]. Likewise, in human HIV-1 infections, pDCs also express high levels of IFNα , resulting in the upregulation of ISGs, which may contribute to the overall systemic immune activation [48, 59, 60]. Consistent expression of IFNα can also contribute to the apoptosis of CD4+ T cells and hence, exacerbate the immune deficiency observed in HIV-1-infected individuals [61]. In addition, pDC activation by HIV-1 has also been shown to induce an increase in indoleamine 2,3-dioxygenase expression which, through modulating regulatory T cells, can suppress T cell responses and proliferation [49, 62–64]. Therapeutic manipulation to suppress the pDC/TLR7/IFNα responses have thus far led to conflicting results . Treatments with chloroquine, which can inhibit endosomal acidification and therefore inhibit signaling through TLR3, 7, 8 and 9, have shown to help reduce HIV-1 replication [65, 66] and immune activation [67–69]. However, other studies have also demonstrated that chloroquine can increase HIV-1 infectivity [70, 71]. Further studies in adequate in vivo models are therefore needed to assess the repercussions of suppressing specific arms of the innate immune response for HIV-1 pathogenesis and immune activation, and also to examine other venues that may more specifically target isolated pathways of innate immunity. These studies will also provide important insights into the contribution of individual pathways to the overall immune activation associated with HIV-1 infection .
The humanized mouse model is one such model that could be utilized to examine responses by specific innate immune pathways and to manipulate these pathways to alter the resulting immune response. NSG BLT mice and Hu-HSC mice all have demonstrated reconstitution of human pDCs, which can respond to TLR7 stimulation (Table 23.1) [10, 42]. Even sex-based differences observed in human studies of TLR7-associated IFNα production [46] have been duplicated in huCD34+-transplanted NOD/SCID/β2m−/− mouse models [32] . Furthermore, TLR7 stimulation of pDCs and its contribution to immune activation and deregulation can be mimicked in mice, where chronic stimulation of TLR7 and TLR9 by synthetic ligands has been shown to result in immune activation and lymphoid follicle destruction similar to that observed in chronic HIV-1 infection in humans [30, 72, 73]. Humanized mice can be infected with HIV-1 and following such infection in huCD34+-transplanted Rag2−/−IL2rγc −/− and NSG BLT mice, pDC activation and production of IFNα can be observed, demonstrating that the humanized mouse model can be used to examine the roles of pDCs, TLR7, and IFNα in HIV-1 infection [30, 42]. Using the NSG BLT mouse model , the administration of recombinant IFNα2b not only induced immune activation levels comparable to that induced by HIV-1 infection, but also induced infiltration of activated T cells in secondary lymphoid organs, adding to the growing evidence that IFNα contributes to immune activation in HIV-1 infection [30] . Although IFNα has potentially detrimental properties in inducing chronic immune activation, it also stimulates the expression of ISGs which possess antiviral activities [74–76]. Cholesterol-25-hydrolase (CH25H), an ISG which can inhibit HIV-1 entry in in vitro cell cultures, can also lead to reduced HIV-1 viral replication in vivo when used to treat HIV-1-infected NOD/Rag2−/−IL2rγc −/− humanized mice [77]. Overall, these early studies using different humanized mouse models of HIV-1 infection suggest that they allow for a reasonable assessment of TLR pathways, the type I IFN axis, and DC function. Future studies will determine the validity of this model to study pathways leading to HIV-1-associated immune activation, and to assess interventions aimed at reducing HIV-1-associated immune activation .
4 Activation of TLRs by Microbe and Microbial Products
Although HIV-1 directly encodes for TLR7/8 ligands, it can also stimulate directly and indirectly through the other TLR pathways . It has been well established that HIV-1 infection leads to depletion of gut-associated CD4+ T cells and therefore compromises the gut mucosal barrier allowing for microbial translocation [4]. One microbial product, lipopolysaccharide (LPS), which can stimulate through the TLR4 pathway has been associated with HIV-1 associated T cell activation [4, 7, 78], monocyte activation [79], lower CD4+ T cell count [80], and CD4+ T cell recovery [7]. In addition to stimulation of TLR4, stimulation of other TLR pathways including TLR3, 5, and 9 also activates T cells and leads to CD4+ T cell apoptosis [78]. Furthermore, gram-positive bacterial stimulation via the TLR2 pathway has been described to result in increased HIV-1 susceptibility of skin-resident DCs [81] as well as transmission of HIV-1 from DCs to CD4+ T cells [82] . Presence of microbial products resulting from microbial translocation or coinfection can not only cause deregulation of the immune system by themselves, but the activating signal might be further amplified by the presence of HIV-1 [83]. Preexposure of monocytes with HIV-1 and HIV-1-encoded TLR8 ligands enhanced subsequent TLR4 stimulation, exacerbating the microbial-induced immune activation [83], and the stimulation of TLR2, 4, and 9 can increase HIV-1 replication in chronically infected cells [84]. In addition, HIV-1 can also lead to increase in TLR2, 3, 4, 6, 7, and 8 expression, all of which can amplify the activation of these immune cells [85–87] . All these factors can contribute to and amplify HIV-1-associated immune activation, which suggest that suppression of HIV-1 or microbial stimulation of TLRs might therefore be beneficial in reducing HIV-1 pathogenesis . These studies have demonstrated the complexities of the various immune cell populations and TLR pathways that play a role in HIV-1 infection and pathogenesis. The question of how each pathway contributes to progressive HIV-1 disease and methods of therapeutically modulating these pathways still needs to be examined .
The role of microbial translocation and the stimulation of the other TLR pathways have also been examined in humanized mice (Table 23.1). Although limited, the expression and function of TLRs in different humanized mouse models have now been started to be studied. TLR2 and TLR4 expressions have been observed on monocytes in huCD34+-transplanted NSG mice [13], and TLR3 expression on mDCs in huCD34+-transplanted NOD/SCID and both huCD34+ and human PBMC-transplanted NSG mice [10, 36, 88] . Stimulation through TLRs can lead to DC activation and maturation [10, 33, 36, 88, 89], production of cytokines [10, 38, 39], and recruitment and priming of T cells [10, 36, 88, 89]. HIV-1 infection of huCD34+-transplanted Rag2−/−IL2γc −/− mice also results in depletion of gut CD4+ T cells and subsequent microbial translocation [90]. The use of humanized mice also allowed for the administration of dextran sodium sulfate which can cause gut barrier dysfunction in the absence of HIV-1 infection. Treatment in huCD34+-transplanted Rag2−/−IL2γc −/− mice demonstrate that dextran sodium sulfate disruption only induces microbial translocation while HIV-1 additionally inhibits microbial clearance potentially reflecting the in vivo consequences of HIV-1 disruption of TLR responses highlighted above [90]. Although the presence of murine immune cells has been reduced in these different humanized mouse models, it is still possible that they may play a role in responding to microbial products. Examination of sepsis in the BLT mouse model , however, suggests that any remnant mouse innate or adaptive immunity that may respond to bacterial products are not enough to induce an inflammatory response on their own and that the reconstituted human immune cells are essential [12]. The humanized mouse models therefore can be utilized to examine not only TLR pathways directly stimulated by HIV-1 but also those induced by microbial translocation or coinfections . However, the expression and function of the various TLR pathways still needs to be more comprehensively studied, particularly the TLR expression patterns and function on the reconstituted human immune cells at various tissue sites .
5 Future Direction and Development of the Model
Significant progress has been made in the development of humanized mouse models to more accurately replicate the in vivo human immune system. The establishment of stable human T cell populations has allowed it to be used as a small animal model for HIV-1 infection. Although there have only been a very limited number of studies to date, initial studies assessing immune responses in different humanized mouse models have demonstrated that the TLRs respond to HIV-1 and other microbial pathogens in humanized mice similar to that observed in humans. Furthermore, studies employing in vivo stimulation and blocking of TLRs in humanized mice have already started to dissect how various TLR pathways can contribute to HIV-1-associated immune activation. The expression and functionality of TLRs in the various humanized mouse models still needs to be fully examined in addition to the role of residual mouse TLR responses, which might represent a confounding factor in these models. Although these early studies are limited, they provide a potential avenue to evaluate activators and inhibitors of individual innate pathways for both dissecting the contribution of these pathways to HIV-1-induced immune activation as well as their therapeutic effect in reducing HIV-1 pathogenesis.
Abbreviations
- DC:
-
Dendritic cells
- EBV:
-
Epstein Barr virus
- HCV:
-
Hepatitis C virus
- HIV:
-
Human immunodeficiency virus
- huCD34+ :
-
Human CD34+ hematopoietic cells
- mDC:
-
Myeloid dendritic cells
- NK:
-
Natural killer
- NSG:
-
NOD/SCID/IL-2rγ−/−
- pDC:
-
Plasmacytoid dendritic cells
- TLR:
-
Toll-like receptor
References
Giorgi JV, Hultin LE, McKeating JA, Johnson TD, Owens B, Jacobson LP, et al. Shorter survival in advanced human immunodeficiency virus type 1 infection is more closely associated with T lymphocyte activation than with plasma virus burden or virus chemokine coreceptor usage. J Infect Dis. 1999;179(4):859–70.
Hunt PW, Martin JN, Sinclair E, Bredt B, Hagos E, Lampiris H, et al. T cell activation is associated with lower CD4+ T cell gains in human immunodeficiency virus-infected patients with sustained viral suppression during antiretroviral therapy. J Infect Dis. 2003;187(10):1534–43.
Groux H, Torpier G, Monte D, Mouton Y, Capron A, Ameisen JC. Activation-induced death by apoptosis in CD4+ T cells from human immunodeficiency virus-infected asymptomatic individuals. J Exp Med. 1992;175(2):331–40.
Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S, et al. Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med. 2006;12(12):1365–71.
Biancotto A, Grivel JC, Iglehart SJ, Vanpouille C, Lisco A, Sieg SF, et al. Abnormal activation and cytokine spectra in lymph nodes of people chronically infected with HIV-1. Blood. 2007;109(10):4272–9.
Gonzalez VD, Falconer K, Blom KG, Reichard O, Morn B, Laursen AL, et al. High levels of chronic immune activation in the T-cell compartments of patients coinfected with hepatitis C virus and human immunodeficiency virus type 1 and on highly active antiretroviral therapy are reverted by alpha interferon and ribavirin treatment. J Virol. 2009;83(21):11407–11.
Jiang W, Lederman MM, Hunt P, Sieg SF, Haley K, Rodriguez B, et al. Plasma levels of bacterial DNA correlate with immune activation and the magnitude of immune restoration in persons with antiretroviral-treated HIV infection. J Infect Dis. 2009;199(8):1177–85 (Clinical trial Research Support, N.I.H., Extramural).
Shultz LD, Brehm MA, Garcia-Martinez JV, Greiner DL. Humanized mice for immune system investigation: progress, promise and challenges. Nat Rev Immunol. 2012;12(11):786–98.
Ito R, Takahashi T, Katano I, Ito M. Current advances in humanized mouse models. Cell Mol Immunol. 2012;9(3):208–14.
Meixlsperger S, Leung CS, Ramer PC, Pack M, Vanoaica LD, Breton G, et al. CD141+ dendritic cells produce prominent amounts of IFN-alpha after dsRNA recognition and can be targeted via DEC-205 in humanized mice. Blood. 2013;121(25):5034–44.
Melkus MW, Estes JD, Padgett-Thomas A, Gatlin J, Denton PW, Othieno FA, et al. Humanized mice mount specific adaptive and innate immune responses to EBV and TSST-1. Nat Med. 2006;12(11):1316–22 (Research Support, N.I.H., Extramural).
Ye C, Choi JG, Abraham S, Wu H, Diaz D, Terreros D, et al. Human macrophage and dendritic cell-specific silencing of high-mobility group protein B1 ameliorates sepsis in a humanized mouse model. Proc Natl Acad Sci U S A. 2012;109(51):21052–7.
Tanaka S, Saito Y, Kunisawa J, Kurashima Y, Wake T, Suzuki N, et al. Development of mature and functional human myeloid subsets in hematopoietic stem cell-engrafted NOD/SCID/IL2rgammaKO mice. J Immunol. 2012;188(12):6145–55.
Seung E, Dudek TE, Allen TM, Freeman GJ, Luster AD, Tager AM. PD-1 blockade in chronically HIV-1-infected humanized mice suppresses viral loads. PLoS ONE. 2013;8(10):e77780.
Lim WH, Kireta S, Russ GR, Coates PT. Human plasmacytoid dendritic cells regulate immune responses to Epstein–Barr virus (EBV) infection and delay EBV-related mortality in humanized NOD-SCID mice. Blood. 2007;109(3):1043–50.
Hesselton RM, Greiner DL, Mordes JP, Rajan TV, Sullivan JL, Shultz LD. High levels of human peripheral blood mononuclear cell engraftment and enhanced susceptibility to human immunodeficiency virus type 1 infection in NOD/LtSz-scid/scid mice. J Infect Dis. 1995;172(4):974–82.
Lowry PA, Shultz LD, Greiner DL, Hesselton RM, Kittler EL, Tiarks CY, et al. Improved engraftment of human cord blood stem cells in NOD/LtSz-scid/scid mice after irradiation or multiple-day injections into unirradiated recipients. Biol Blood Marrow Transplant. 1996;2(1):15–23.
Christianson SW, Greiner DL, Hesselton RA, Leif JH, Wagar EJ, Schweitzer IB, et al. Enhanced human CD4+ T cell engraftment in beta2-microglobulin-deficient NOD-scid mice. J Immunol. 1997;158(8):3578–86.
Shultz LD, Lyons BL, Burzenski LM, Gott B, Chen X, Chaleff S, et al. Human lymphoid and myeloid cell development in NOD/LtSz-scid IL2R gamma null mice engrafted with mobilized human hemopoietic stem cells. J Immunol. 2005;174(10):6477–89.
Ito M, Hiramatsu H, Kobayashi K, Suzue K, Kawahata M, Hioki K, et al. NOD/SCID/gamma(c)(null) mouse: an excellent recipient mouse model for engraftment of human cells. Blood. 2002;100(9):3175–82.
Traggiai E, Chicha L, Mazzucchelli L, Bronz L, Piffaretti JC, Lanzavecchia A, et al. Development of a human adaptive immune system in cord blood cell-transplanted mice. Science. 2004;304(5667):104–7.
Gimeno R, Weijer K, Voordouw A, Uittenbogaart CH, Legrand N, Alves NL, et al. Monitoring the effect of gene silencing by RNA interference in human CD34+ cells injected into newborn RAG2−/− gammac−/− mice: functional inactivation of p53 in developing T cells. Blood. 2004;104(13):3886–93.
Mosier DE, Gulizia RJ, Baird SM, Wilson DB. Transfer of a functional human immune system to mice with severe combined immunodeficiency. Nature. 1988;335(6187):256–9.
McCune JM, Namikawa R, Kaneshima H, Shultz LD, Lieberman M, Weissman IL. The SCID-hu mouse: murine model for the analysis of human hematolymphoid differentiation and function. Science. 1988;241(4873):1632–9.
Lan P, Tonomura N, Shimizu A, Wang S, Yang YG. Reconstitution of a functional human immune system in immunodeficient mice through combined human fetal thymus/liver and CD34+ cell transplantation. Blood. 2006;108(2):487–92.
Chen Q, Khoury M, Chen J. Expression of human cytokines dramatically improves reconstitution of specific human-blood lineage cells in humanized mice. Proc Natl Acad Sci U S A. 2009;106(51):21783–8.
Kwant-Mitchell A, Ashkar AA, Rosenthal KL. Mucosal innate and adaptive immune responses against herpes simplex virus type 2 in a humanized mouse model. J Virol. 2009;83(20):10664–76.
Strowig T, Gurer C, Ploss A, Liu YF, Arrey F, Sashihara J, et al. Priming of protective T cell responses against virus-induced tumors in mice with human immune system components. J Exp Med. 2009;206(6):1423–34.
Ishikawa F, Yasukawa M, Lyons B, Yoshida S, Miyamoto T, Yoshimoto G, et al. Development of functional human blood and immune systems in NOD/SCID/IL2 receptor {gamma} chain(null) mice. Blood. 2005;106(5):1565–73.
Long BR, Stoddart CA. Alpha interferon and HIV infection cause activation of human T cells in NSG-BLT mice. J Virol. 2012;86(6):3327–36.
Brainard DM, Seung E, Frahm N, Cariappa A, Bailey CC, Hart WK, et al. Induction of robust cellular and humoral virus-specific adaptive immune responses in human immunodeficiency virus-infected humanized BLT mice. J Virol. 2009;83(14):7305–21.
Seillet C, Laffont S, Tremollieres F, Rouquie N, Ribot C, Arnal JF, et al. The TLR-mediated response of plasmacytoid dendritic cells is positively regulated by estradiol in vivo through cell-intrinsic estrogen receptor alpha signaling. Blood. 2012;119(2):454–64.
Chen Q, He F, Kwang J, Chan JK, Chen J. GM-CSF and IL-4 stimulate antibody responses in humanized mice by promoting T, B, and dendritic cell maturation. J Immunol. 2012;189(11):5223–9.
Kalberer CP, Siegler U, Wodnar-Filipowicz A. Human NK cell development in NOD/SCID mice receiving grafts of cord blood CD34+ cells. Blood. 2003;102(1):127–35.
Rajesh D, Zhou Y, Jankowska-Gan E, Roenneburg DA, Dart ML, Torrealba J, et al. Th1 and Th17 immunocompetence in humanized NOD/SCID/IL2rgammanull mice. Hum Immunol. 2010;71(6):551–9.
Vuckovic S, Abdul Wahid FS, Rice A, Kato M, Khalil D, Rodwell R, et al. Compartmentalization of allogeneic T-cell responses in the bone marrow and spleen of humanized NOD/SCID mice containing activated human resident myeloid dendritic cells. Exp Hematol. 2008;36(11):1496–506.
Huntington ND, Legrand N, Alves NL, Jaron B, Weijer K, Plet A, et al. IL-15 trans-presentation promotes human NK cell development and differentiation in vivo. J Exp Med. 2009;206(1):25–34.
Willinger T, Rongvaux A, Takizawa H, Yancopoulos GD, Valenzuela DM, Murphy AJ, et al. Human IL-3/GM-CSF knock-in mice support human alveolar macrophage development and human immune responses in the lung. Proc Natl Acad Sci U S A. 2011;108(6):2390–5.
Rathinam C, Poueymirou WT, Rojas J, Murphy AJ, Valenzuela DM, Yancopoulos GD, et al. Efficient differentiation and function of human macrophages in humanized CSF-1 mice. Blood. 2011;118(11):3119–28.
Sato K, Misawa N, Nie C, Satou Y, Iwakiri D, Matsuoka M, et al. A novel animal model of Epstein–Barr virus-associated hemophagocytic lymphohistiocytosis in humanized mice. Blood. 2011;117(21):5663–73.
Washburn ML, Bility MT, Zhang L, Kovalev GI, Buntzman A, Frelinger JA, et al. A humanized mouse model to study hepatitis C virus infection, immune response, and liver disease. Gastroenterology. 2011;140(4):1334–44.
Zhang L, Jiang Q, Li G, Jeffrey J, Kovalev GI, Su L. Efficient infection, activation, and impairment of pDCs in the BM and peripheral lymphoid organs during early HIV-1 infection in humanized rag2(-)/(-)gamma C(-)/(-) mice in vivo. Blood. 2011;117(23):6184–92.
Dudek TE, No DC, Seung E, Vrbanac VD, Fadda L, Bhoumik P, et al. Rapid evolution of HIV-1 to functional CD8+ T-cell responses in humanized BLT mice. Sci Transl Med. 2012;4(143):143ra98.
Hauber I, Hofmann-Sieber H, Chemnitz J, Dubrau D, Chusainow J, Stucka R, et al. Highly significant antiviral activity of HIV-1 LTR-specific tre-recombinase in humanized mice. PLoS Pathog. 2013;9(9):e1003587.
Meier A, Alter G, Frahm N, Sidhu H, Li B, Bagchi A, et al. MyD88-dependent immune activation mediated by human immunodeficiency virus type 1-encoded Toll-like receptor ligands. J Virol. 2007;81(15):8180–91.
Meier A, Chang JJ, Chan ES, Pollard RB, Sidhu HK, Kulkarni S, et al. Sex differences in the Toll-like receptor-mediated response of plasmacytoid dendritic cells to HIV-1. Nat Med. 2009;15(8):955–9.
Beignon AS, McKenna K, Skoberne M, Manches O, DaSilva I, Kavanagh DG, et al. Endocytosis of HIV-1 activates plasmacytoid dendritic cells via Toll-like receptor-viral RNA interactions. J Clin Invest. 2005;115(11):3265–75.
Lehmann C, Harper JM, Taubert D, Hartmann P, Fatkenheuer G, Jung N, et al. Increased interferon alpha expression in circulating plasmacytoid dendritic cells of HIV-1-infected patients. J Acquir Immune Defic Syndr. 2008;48(5):522–30.
Boasso A, Shearer GM. Chronic innate immune activation as a cause of HIV-1 immunopathogenesis. Clin Immunol. 2008;126(3):235–42 (Review).
Lombardi V, Van Overtvelt L, Horiot S, Moingeon P. Human dendritic cells stimulated via TLR7 and/or TLR8 induce the sequential production of Il-10, IFN-gamma, and IL-17A by naive CD4+ T cells. J Immunol. 2009;182(6):3372–9.
Agrawal S, Agrawal A, Doughty B, Gerwitz A, Blenis J, Van Dyke T, et al. Cutting edge: different Toll-like receptor agonists instruct dendritic cells to induce distinct Th responses via differential modulation of extracellular signal-regulated kinase-mitogen-activated protein kinase and c-Fos. J Immunol. 2003;171(10):4984–9.
Odorizzi PM, Wherry EJ. Immunology. An interferon paradox. Science. 2013;340(6129):155–6.
Chang JJ, Lacas A, Lindsay RJ, Doyle EH, Axten KL, Pereyra F, et al. Differential regulation of toll-like receptor pathways in acute and chronic HIV-1 infection. AIDS. 2012;26(5):533-41 (Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t).
Mandl JN, Barry AP, Vanderford TH, Kozyr N, Chavan R, Klucking S, et al. Divergent TLR7 and TLR9 signaling and type I interferon production distinguish pathogenic and nonpathogenic AIDS virus infections. Nat Med. 2008;14(10):1077–87.
Silvestri G, Sodora DL, Koup RA, Paiardini M, O’Neil SP, McClure HM, et al. Nonpathogenic SIV infection of sooty mangabeys is characterized by limited bystander immunopathology despite chronic high-level viremia. Immunity. 2003;18(3):441–52.
Sodora DL, Allan JS, Apetrei C, Brenchley JM, Douek DC, Else JG, et al. Toward an AIDS vaccine: lessons from natural simian immunodeficiency virus infections of African nonhuman primate hosts. Nat Med. 2009;15(8):861–5.
Harris LD, Tabb B, Sodora DL, Paiardini M, Klatt NR, Douek DC, et al. Downregulation of robust acute type I interferon responses distinguishes nonpathogenic simian immunodeficiency virus (SIV) infection of natural hosts from pathogenic SIV infection of rhesus macaques. J Virol. 2010;84(15):7886–91.
Bosinger SE, Li Q, Gordon SN, Klatt NR, Duan L, Xu L, et al. Global genomic analysis reveals rapid control of a robust innate response in SIV-infected sooty mangabeys. J Clin Invest. 2009;119(12):3556–72.
Bosinger SE, Hosiawa KA, Cameron MJ, Persad D, Ran L, Xu L, et al. Gene expression profiling of host response in models of acute HIV infection. J Immunol. 2004;173(11):6858–63.
Chang JJ, Woods M, Lindsay RJ, Doyle EH, Griesbeck M, Chan ES, et al. Higher expression of several interferon-stimulated genes in HIV-1-infected females after adjusting for the level of viral replication. J Infect Dis. 2013;208(5):830–8.
Herbeuval JP, Nilsson J, Boasso A, Hardy AW, Kruhlak MJ, Anderson SA, et al. Differential expression of IFN-alpha and TRAIL/DR5 in lymphoid tissue of progressor versus nonprogressor HIV-1-infected patients. Proc Natl Acad Sci U S A. 2006;103(18):7000–5.
Boasso A, Herbeuval JP, Hardy AW, Anderson SA, Dolan MJ, Fuchs D, et al. HIV inhibits CD4+ T-cell proliferation by inducing indoleamine 2,3-dioxygenase in plasmacytoid dendritic cells. Blood. 2007;109(8):3351–9 (Clinical Trial, Comparative Study Multicenter Study Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov’t).
Malleret B, Maneglier B, Karlsson I, Lebon P, Nascimbeni M, Perie L, et al. Primary infection with simian immunodeficiency virus: plasmacytoid dendritic cell homing to lymph nodes, type I interferon, and immune suppression. Blood. 2008;112(12):4598–608.
Manches O, Munn D, Fallahi A, Lifson J, Chaperot L, Plumas J, et al. HIV-activated human plasmacytoid DCs induce Tregs through an indoleamine 2,3-dioxygenase-dependent mechanism. J Clin Invest. 2008;118(10):3431–9.
Chiang G, Sassaroli M, Louie M, Chen H, Stecher VJ, Sperber K. Inhibition of HIV-1 replication by hydroxychloroquine: mechanism of action and comparison with zidovudine. Clin Ther. 1996;18(6):1080-92 (Comparative Study Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.).
Naarding MA, Baan E, Pollakis G, Paxton WA. Effect of chloroquine on reducing HIV-1 replication in vitro and the DC-SIGN mediated transfer of virus to CD4+ T-lymphocytes. Retrovirology. 2007;4:6 (Research Support, Non-U.S. Gov’t).
Murray SM, Down CM, Boulware DR, Stauffer WM, Cavert WP, Schacker TW, et al. Reduction of immune activation with chloroquine therapy during chronic HIV infection. J Virol. 2010;84(22):12082–6 (Randomized Controlled Trial Research Support, N.I.H., Research Support, Non-U.S. Gov’t).
Martinson JA, Montoya CJ, Usuga X, Ronquillo R, Landay AL, Desai SN. Chloroquine modulates HIV-1-induced plasmacytoid dendritic cell alpha interferon: implication for T-cell activation. Antimicrob Agents Chemother. 2010;54(2):871–81.
Piconi S, Parisotto S, Rizzardini G, Passerini S, Terzi R, Argenteri B, et al. Hydroxychloroquine drastically reduces immune activation in HIV-infected, antiretroviral therapy-treated immunologic nonresponders. Blood. 2011;118(12):3263–72 (Research Support, Non-U.S. Gov’t).
Fredericksen BL, Wei BL, Yao J, Luo T, Garcia JV. Inhibition of endosomal/lysosomal degradation increases the infectivity of human immunodeficiency virus. J Virol. 2002;76(22):11440–6 (Research Support, U.S. Gov’t, P.H.S.).
Vijaykumar TS, Nath A, Chauhan A. Chloroquine mediated molecular tuning of astrocytes for enhanced permissiveness to HIV infection. Virology. 2008;381(1):1–5 (Research Support, N.I.H., Extramural).
Baenziger S, Heikenwalder M, Johansen P, Schlaepfer E, Hofer U, Miller RC, et al. Triggering TLR7 in mice induces immune activation and lymphoid system disruption, resembling HIV-mediated pathology. Blood. 2009;113(2):377–88.
Heikenwalder M, Polymenidou M, Junt T, Sigurdson C, Wagner H, Akira S, et al. Lymphoid follicle destruction and immunosuppression after repeated CpG oligodeoxynucleotide administration. Nat Med. 2004;10(2):187–92.
Baca-Regen L, Heinzinger N, Stevenson M, Gendelman HE. Alpha interferon-induced antiretroviral activities: restriction of viral nucleic acid synthesis and progeny virion production in human immunodeficiency virus type 1-infected monocytes. J Virol. 1994;68(11):7559–65.
Cullen BR. Role and mechanism of action of the APOBEC3 family of antiretroviral resistance factors. J Virol. 2006;80(3):1067–76.
Okumura A, Lu G, Pitha-Rowe I, Pitha PM. Innate antiviral response targets HIV-1 release by the induction of ubiquitin-like protein ISG15. Proc Natl Acad Sci U S A. 2006;103(5):1440–5 (Research Support, N.I.H., Extramural).
Liu SY, Aliyari R, Chikere K, Li G, Marsden MD, Smith JK, et al. Interferon-inducible cholesterol-25-hydroxylase broadly inhibits viral entry by production of 25-hydroxycholesterol. Immunity. 2013;38(1):92–105.
Funderburg N, Luciano AA, Jiang W, Rodriguez B, Sieg SF, Lederman MM. Toll-like receptor ligands induce human T cell activation and death, a model for HIV pathogenesis. PLoS ONE. 2008;3(4):e1915 (Research Support, N.I.H., Extramural).
Ancuta P, Kamat A, Kunstman KJ, Kim EY, Autissier P, Wurcel A, et al. Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS ONE. 2008;3(6):e2516 [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t).
Balagopal A, Philp FH, Astemborski J, Block TM, Mehta A, Long R, et al. Human immunodeficiency virus-related microbial translocation and progression of hepatitis C. Gastroenterology. 2008;135(1):226–33.
Ogawa Y, Kawamura T, Kimura T, Ito M, Blauvelt A, Shimada S. Gram-positive bacteria enhance HIV-1 susceptibility in Langerhans cells, but not in dendritic cells, via Toll-like receptor activation. Blood. 2009;113(21):5157–66.
Thibault S, Fromentin R, Tardif MR, Tremblay MJ. TLR2 and TLR4 triggering exerts contrasting effects with regard to HIV-1 infection of human dendritic cells and subsequent virus transfer to CD4+ T cells. Retrovirology. 2009;6:42 (Research Support, Non-U.S. Gov’t).
Mureith MW, Chang JJ, Lifson JD, Ndung’u T, Altfeld M. Exposure to HIV-1-encoded Toll-like receptor 8 ligands enhances monocyte response to microbial encoded Toll-like receptor 2/4 ligands. AIDS. 2010;24(12):1841–8 (Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t).
Nordone SK, Ignacio GA, Su L, Sempowski GD, Golenbock DT, Li L, et al. Failure of TLR4-driven NF-kappa B activation to stimulate virus replication in models of HIV type 1 activation. AIDS Res Hum Retroviruses. 2007;23(11):1387–95.
Heggelund L, Muller F, Lien E, Yndestad A, Ueland T, Kristiansen KI, et al. Increased expression of toll-like receptor 2 on monocytes in HIV infection: possible roles in inflammation and viral replication. Clin Infect Dis. 2004;39(2):264–9.
Song Y, Zhuang Y, Zhai S, Huang D, Zhang Y, Kang W, et al. Increased expression of TLR7 in CD8(+) T cells leads to TLR7-mediated activation and accessory cell-dependent IFN-gamma production in HIV type 1 infection. AIDS Res Hum Retroviruses. 2009;25(12):1287–95.
Lester RT, Yao XD, Ball TB, McKinnon LR, Kaul R, Wachihi C, et al. Toll-like receptor expression and responsiveness are increased in viraemic HIV-1 infection. AIDS. 2008;22(6):685–94.
Spranger S, Frankenberger B, Schendel DJ. NOD/scid IL-2Rg(null) mice: a preclinical model system to evaluate human dendritic cell-based vaccine strategies in vivo. J Transl Med. 2012;10:30.
Cravens PD, Melkus MW, Padgett-Thomas A, Islas-Ohlmayer M, Del PMM, Garcia JV. Development and activation of human dendritic cells in vivo in a xenograft model of human hematopoiesis. Stem Cells. 2005;23(2):264–78.
Hofer U, Schlaepfer E, Baenziger S, Nischang M, Regenass S, Schwendener R, et al. Inadequate clearance of translocated bacterial products in HIV-infected humanized mice. PLoS Pathog. 2010;6(4):e1000867.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Chang, J., Altfeld, M. (2014). Role of Toll-Like Receptor (TLR) Signaling in HIV-1-Induced Adaptive Immune Activation. In: Poluektova, L., Garcia, J., Koyanagi, Y., Manz, M., Tager, A. (eds) Humanized Mice for HIV Research. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1655-9_23
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1655-9_23
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1654-2
Online ISBN: 978-1-4939-1655-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)