Abstract
Pharmaceutical excipients play a significant role in stabilization of amorphous solid dispersions, as these systems are thermodynamically unstable. This chapter illustrates the challenges associated with amorphous solid dispersion stability and the role that excipients play in stabilization of amorphous solid dispersions by influencing the physicochemical properties of the drug molecule of interest. The classification of various excipients is categorized in detail, covering polymers, solubilizers, plasticizers, antioxidants, and other suitable fillers. The impact of excipients on various amorphous solid dispersion technologies is also discussed in detail. Discovery of newer polymers and greater understanding of excipients’ role in the stabilization of amorphous solid dispersion are the primary reasons for successful launch of several marketed drug products. In addition, safety and regulatory aspects of these excipients also need to be considered for the development of successful products. In summary, excipients play a significant role in stabilizing amorphous solid dispersions, maximizing bioavailability, and overcoming absorption issues associated with poorly soluble drugs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Excipients
- Ionic polymers
- Nonionic polymers
- Solid dispersion
- Plasticizers
- Non-polymeric excipients
- Hot-melt extrusion
- Spray drying
- Microprecipitated bulk powder
- Glass transition temperature
- Hygroscopicity
- Polymeric excipients
1 Introduction
Amorphous solid dispersions (ASD) have been a topic of interest in recent years for the pharmaceutical community due to their potential in improving the oral bioavailability of poorly water-soluble drugs (Craig 2002; Leuner and Dressman 2000). Amorphous forms, which have high free energy and greater chemical and thermodynamic activity as compared to crystalline polymorphs, provide faster dissolution rates and higher apparent solubility. However, the most common concerns of ASD are the lack of thermodynamic stability. One of the approaches typically used to overcome the stability problems with amorphous active pharmaceutical ingredients (APIs) is to formulate them with pharmaceutically acceptable polymers to form ASD. The ability to form intermolecular interactions (hydrogen bonding, ionic interaction, or dipole–dipole interactions) is one of the most important criteria in the formation of amorphous molecular dispersions. In case of miscible ASD, improved physical stability can be attributed to the reduction of molecular mobility of the API molecules and/or by inhibition of nucleation and crystal growth through preferential API–polymer interactions (Ivanisevic 2010).
The polymer serves as a carrier in which API is dispersed in an ASD. Polymer selection is very important as it influences manufacturing, bioavailability, and stability of the ASD. Initial assessment of potentially “useful” excipients should be based on basic physicochemical properties of the polymers such as glass transition temperature (T g), hygroscopicity , solid solution capacity and solubilization capacity to name a few.
2 Challenges of Amorphous Solid Dispersions
ASD are certainly a valuable formulation strategy to enhance bioavailability of poorly soluble drugs by improving their solubility and dissolution rate. However, inherent thermodynamic instability leading to relaxation, nucleation, and crystallization during storage is one of the biggest challenges associated with the development of ASD. Critical parameters, namely temperature, moisture, and pressure, which are generally encountered during manufacturing, could adversely affect physical stability of amorphous solids. Some amorphous solids easily get plasticized with water resulting in low T g. Typically, plasticization enhances the molecular mobility, leading to gelling or crystallization of the amorphous solid. Temperature naturally enhances molecular mobility and crystallization rate of an amorphous drug. As a rule of thumb, the storage temperature for an amorphous solid should be at least 50 °C below its T g, irrespective of other factors such as the impact of water and pressure. Similarly, pressure may initiate nucleation of the drug, which could act as seeds and adversely impact long-term physical stability of the amorphous formulation. Crystallization of amorphous solids could also occur during the transit through gastrointestinal (GI) tract.
Pure amorphous drugs are not commonly developed as commercial dosage forms but are manufactured in combination with excipients to stabilize the amorphous state during storage as well as to prevent crystallization of API during in vivo dissolution in the GI tract. The high kinetic solubility of the amorphous form can drop to the equilibrium solubility of the crystalline form if devitrification is induced by the dissolution medium. Therefore, appropriate carriers that can serve as stabilizers of the amorphous state of the API are needed in the formulation. The dissolved carrier can also influence the supersaturated drug solution that is formed following dissolution. Some carriers solubilize the released drug, whereas others stabilize the supersaturated drug solution. Ideally, it is preferred to have an ASD with improved extent and rate of dissolution and one which maintains supersaturation of the drug in the GI fluids to maximize drug absorption. It should be noted that in the case of amorphous systems, kinetic solubility carries a thermodynamic representation of a high-energy form, and quantifies the degree of metastability of the amorphous phase relative to the crystalline form. Therefore, a supersaturation kinetic study is typically performed for initial screening of ASD.
3 Role of Excipients in Amorphous Solid Dispersions
In many instances, amorphous drug by itself cannot withstand the processing conditions involved in manufacturing. Polymers impact shelf-life stability of amorphous solid dosage forms by immobilizing and isolating amorphous drug in a rigid glass, preventing drug crystallization. ASD stabilized by polymers can be categorized into solid solutions and solid suspension. However, in general, ASD refers to solid solution.
A. Solid Solution
If an amorphous drug is miscible with the polymer, the system is known as an amorphous solid solution or molecular dispersion distinguished by one T g value. The physical stability of these systems is expected to be API concentration dependent. The major determining factors for designing solid solutions include solubility parameters, drug loading , and other properties of drug and polymer. Van Krevelen and Fedor group contribution methods are useful for solubility parameter calculation as a first screening tool in selecting appropriate polymers. The differences in solubility parameters of less than 7.0 MPa1/2 between materials predict miscibility or a one-phase system (Greenhalgh et al. 1999). For an amorphous solid solution, T g of the drug/polymer can be predicted by using the Gordon–Taylor (GT) equation:
where T g is the glass transition temperature, w 1 and w 2 are the weight fractions of components, and K is calculated from the densities ρ and T g of amorphous components. One-phase system is preferred only when the system has sufficiently high T g.
B. Solid Suspension
If the amorphous drug is dispersed in the polymer matrix at the particle level, it is referred to as an amorphous solid suspension, distinguished by two separate T g values of the drug and the polymer. The physical stability relies on immobilization and isolation of the amorphous particles in a rigid polymer matrix.
To maximize the stabilization effect, it is critical to ensure that the amorphous drug is molecularly embedded in the polymer matrix as solid solution (Fig. 4.1).
Polymers play a pivotal role in (a) attaining and maintaining supersaturation, (b) preventing API from nucleation and crystallization, and (c) modulating the hygroscopicity of the amorphous API. In addition, drug polymer interactions can also impart stability to ASD by providing mechanical rigidity due to increase in the glass transition temperature of a given matrix.
It is essential to understand the molecular and thermodynamic properties that contribute to the solubility and stability of an ASD. The properties include glass transition temperature, fragility, molecular mobility , devitrification kinetics, and chemical interactions. A thorough understanding of all of these aspects is imperative for a rational formulation strategy.
3.1 Glass Transition Temperature (Tg)
Glass transition temperature is defined as a temperature at which the material is converted from a “rubbery” to a “glassy” state. Generally speaking, polymers with a “hard” monomer and high molecular weight have high glass transition temperature (e.g., cellulose ethers: hydroxypropyl methylcellulose, HPMC, and hypromellose acetate succinate, HPMCAS) . The glass transition temperature of the polymer can be lowered by using a plasticizer that should be perfectly mixed with the polymer at the molecular level. When choosing a polymer for ASD, one has to be careful to select one that has a high enough glass transition temperature to reduce molecular mobility and hence decrease crystallization tendency of the API while still having acceptable attributes from the processing point of view.
3.2 Molecular Mobility
Molecular mobility in amorphous materials is related to the macromolecular properties like viscosity; it is generally quantified in terms of mean relaxation time and it determines physical stability and reactivity. The relaxation time is defined as the time necessary for a molecule or chain segment to diffuse across the distance of one molecule or chain segment. The relaxation time varies with temperature and the typical relaxation times at T g are estimated to be 100–200 s (Ediger et al. 1996). Molecular relaxation times can be characterized by the change of several bulk properties like enthalpy or volume or spectroscopic properties. The extent of relaxation is described empirically by the Kohlrausch–Williams–Watts equation (Hodge 1994):
where ϕ(t) is the extent of relaxation at time t, τ is mean relaxation time constant, and β is relaxation time distribution parameter. Molecular mobility is also viewed as antiplasticizing of the drug by the polymer. Miscible ASD will typically have a higher glass transition temperature (T g) compared to the amorphous API due to the antiplasticizing effect of a high T g polymer in the formulation. In addition, certain specific chemical interactions between the drug and polymer can also limit the molecular motion of the drug in the amorphous state resulting in stabilization of the system. Polymer content and its molecular weight have been found to be a major contributory factor in restricting the molecular mobility of amorphous drugs (Kaushal et al. 2004; Albano et al. 2002) .
3.3 Polymer Molecular Weight
Selection of an ideal polymer with the desired structural features is very important to the performance of ASD. Molecular weight of the polymer is directly related to its T g; hence, a polymer with high molecular weight has a high T g, thereby favoring its use as a stabilizing carrier. In addition, the molecular weight of the polymer is also directly related to its intrinsic viscosity which in turn affects drug dissolution. A high molecular weight polymer will form a high viscosity diffusion boundary layer around the ASD particles, resulting in diffusion-controlled release of drug, whereas a low molecular weight polymer will dissolve rapidly, resulting in release of drug as a single entity (Kaushal et al. 2004; Omelczuk and McGinity 1992).
3.4 Drug–Polymer Ratio
The drug–polymer ratio in ASD is based on the influence of the polymer on the drug’s physical form. Moreover, the maximum amount of the polymer that can be employed is governed by its ability to formulate the ASD into a dosage form of administrable size. High drug loading may lead to crystallization within the dispersion. On the other hand, a high polymer amount in the formulation may ensure absence of drug crystallinity, but at a cost. The low drug loading would potentially result in a higher pill burden. The polymer also prevents fusion/nucleation of amorphous API particles under compaction. Hence, drug–polymer ratio needs to be optimized to formulate an ASD into a stable dosage form (Kaushal et al. 2004).
3.5 Solubility Parameters
Solubility parameters are used to predict drug–polymer miscibility. Systems with similar solubility parameter values are likely to be miscible because the energetics of interactions within one component are similar to those in other component. As a result, the overall energy needed to facilitate the mixing of components will be small because the energy required to break the interactions within like molecules will be equally compensated for the energy released by interactions between unlike molecules. Hilderbrand solubility parameters have been used to predict drug–polymer miscibility and were found useful in selecting suitable polymers. However, the limitation of Hilderbrand solubility parameters is that it does not consider the various types of forces such as hydrogen bonding/polar/dispersion operating in the system. Hence, Hansen solubility parameters were developed to take into account all of these forces, in addition to molar volumes and molar attraction constants. As it has been reported that drug’s crystallinity affects the solubility parameter values, due care must be taken while calculating these parameters (Kaushal et al. 2004).
3.6 Solid Solution Capacity
Solid solution capacity is the maximum concentration of an active ingredient which can be completely dissolved in a polymer. Typically, solid solution capacity is influenced by drug lipophilicity, solubility parameters, presence of hydrogen bonds, as well as presence of amide structures that can act as hydrogen bond acceptors. For example, polymers with amide structure such as polyvinyllactam polymers (e.g., Kollidon® VA 64) have better solid solution capacity than the polymers with other structures.
3.7 Solubilization Capacity
Solubilization capacity is defined as solubilization effect of polymers on active ingredients in an aqueous solution. Needless to say, if the polymer can retain the drug in supersaturation state in the GI tract, it will significantly enhance bioavailability . Of all polymers used in ASD, amphiphilic polymers such as Soluplus® have better solubilization capacity due to their ability to create micellar structures . On the other hand, most of ionic polymers such as methacrylate copolymers can create complexes with the drug and thus increase its solubility.
3.8 Hygroscopicity
Moisture is known to have a profound effect on the T g of amorphous solids, acting as a plasticizer by increasing the free volume of the material, enhancing structural mobility, and thereby decreasing T g. At any particular temperature, the amorphous system may change from the glassy to the rubbery state if water uptake takes place. Apart from plasticization, moisture can accelerate chemical degradation and crystallization. Therefore, water vapor sorption analysis is very useful for the early evaluation of amorphous solids. Also, storage at high relative humidity is also an important factor influencing solid-state properties of the amorphous system. As shown previously by other researchers, the enteric polymers, e.g., HPMCAS, and acrylate polymers such as Eudragits® are somewhat less hygroscopic than the water-soluble polymers like povidone or copovidone, thereby imparting better stability to the amorphous form (Rumondor and Taylor 2010). In addition, due to the hydrophobicity and somewhat low hygroscopicity, the ionic polymers also offer distinct advantage with respect to water immiscibility (pH-dependent solubility). As these polymers are water insoluble, they can absorb water without dissolving and hence the polymer: API interactions may be preserved to ensure stability of the amorphous form. As discussed previously, the amorphous state has greater free volume, molecular mobility, and enthalpy relative to the crystalline state, resulting in higher dissolution rates .
3.9 Chemical Reactivity
Amorphous forms tend to degrade at a higher rate than the crystalline forms. This may be due to increased specific surface area and enhanced level of molecular mobility which reduces the activation energy for solid-state chemical reactions. Moreover, higher hygroscopicity of amorphous forms may enhance the rate of degradation by plasticization. Increasing molecular mobility consequently mediates degradation reactions. It has been reported that in presence of moisture, thermal degradation rates of β-lactam antibiotics were a magnitude higher in amorphous form than in the crystalline form (Pikal et al. 1977). The chemical reactivity in case of amorphous systems could be reduced by formulation interventions such as the addition of high molecular weight polymers to the amorphous formulation; this results in a high level of positional specificity between reacting components. In addition, the enhanced chemical reactivity in case of amorphous systems can be overcome through the use of appropriate packaging and storage conditions (Kaushal et al. 2004).
4 Classification of Excipients
The excipients used in solid dispersions can be broadly classified as (a) polymeric and (b) non-polymeric excipients . Polymeric excipients are the primary excipients, whereas the non-polymeric ones are the auxiliary excipients. Polymeric excipients are further classified based on their charge into the following categories: (a) nonionic or non-pH-dependent and (b) ionic or pH-dependent polymers. Further, nonionic polymers are classified as polyvinyllactam polymers and cellulose ethers. The ionic polymers are further classified as cationic and anionic polymers (Fig. 4.2).
A summary in Table 4.1 lists important properties of commonly used polymers in solid dispersions, including glass transition temperature (T g), hygroscopicity , solubility parameters, and degradation temperature, based on which initial assessment of potentially “useful” excipients can be made. In general, polymeric materials having higher glass transition temperatures will result in solid dispersions with higher glass transition temperatures and lower molecular mobility . However, stability will also be influenced by intermolecular drug polymer interactions and moisture absorption during storage . Therefore, when selecting excipient, one should consider polymer chemistry together with the properties of the API and manufacturing aspects.
4.1 Nonionic/Non-pH-Dependent Polymers
4.1.1 Polyvinyllactam Polymers
This family of excipients is typically synthesized using vinylpyrrolidone as a monomer. This monomer is polymerized to the homopolymer polyvinylpyrrolidone (povidone; PVP) or copolymerized with vinyl acetate to copovidone. In recent years, a new addition to this family of excipient is vinylcaprolactam (Soluplus®).
4.1.1.1 Polyvinylpyrrolidone (Povidone)
The different grades of povidone are predominantly based on their molecular weight (Reintjes 2011). They have good solubility in water and organic solvents with medium lipophilicity (Table 4.1) and most importantly have the ability to interact with both hydrophilic and lipophilic active ingredients. Due to their hydrophilic nature, they have been the most commonly used as precipitation inhibitors. PVP-based hydrophilic matrices prevent drug crystallization by arresting reorientation and forming stronger drug–polymer interactions . Furthermore, once the matrix is in the GI tract, it maintains the supersaturation state by inhibiting drug crystallization by preventing aggregation of nuclei formed due to increased mobility of the matrix. The crystal inhibition is very drug specific and may be dependent on the type of the polymeric excipient. In one of the classic examples, Lindfors et al. used PVP as a crystal inhibitor for the bicalutamide; in this case, PVP gets adsorbed on the fresh nuclei of the drug. However, PVP did not control the formation of nuclei; it rather inhibited the addition of solute onto the nuclei, preventing crystal growth. Hydrogen bonding between the drug and the polymer excipients in the aqueous solution also led to the crystal inhibition (Lindfors et al. 2008).
4.1.1.2 Copovidone (Kollidon® VA64/ Plasdone™ S-630)
Kollidon® VA64 is a vinylpyrrolidone–vinyl acetate copolymer, soluble in water and alcohols. This polymer is amorphous in nature, with a T g value of 101 °C, with a degradation temperature around 230 °C (Table 4.1). It has good processability and is commonly used for manufacturing of solid dispersions using either hot-melt extrusion (HME) or spray drying (SD). Kaletra® is the most successful example of copovidone-based solid dispersions on the market. Kaletra®, a combination of lopinavir and ritonavir, is used for the treatment of HIV-1 infected individuals. This tablet formulation is practically a solid solution, which serves two purposes: (a) increases the dissolution rate of the APIs and (b) stabilizes the amorphous drug as a solid solution in the solid glassy hydrophilic polymer. In case of Kaletra®, Meltrex® technology using melt extrusion with copovidone was employed to manufacture the extrudates; these were further subjected to downstream processing to produce a stable product with an acceptable shelf life.
4.1.1.3 Polyvinylcaprolactam–Polyvinyl Acetate–Polyethyelne Glycol Graft Copolymer (Soluplus®)
This polymer was designed to be amphiphilic in nature, soluble in organic solvents, having a high molecular weight, low glass transition temperature, and a high degradation temperature (Table 4.1). All of these characteristics indicate that this polymer is an excellent candidate for the manufacture of solid dispersions using either HME or SD. Also, due to its amphiphilic nature, Soluplus® provides high solid solution and solubilization capacity.
Soluplus®-based solid dispersions showed promising results when used with model drugs like itranconazole, fenofibrate, and carbamazepine, to name a few. For example, solid solution of itranconazole in Soluplus® showed significantly enhanced absorption by ~ 26-fold, while the absorption of fine crystals of API was enhanced approximately twofold for the marketed product Sempera®. Overall, due to its amphiphilic properties, Soluplus® can serve as an excellent solubilizer and matrix former in solid dispersions.
4.1.2 Cellulose Ethers
Several research groups have successfully used cellulose ethers in solid dispersions. These polymers are hydrophilic in nature and have high molecular weight and good thermal and mechanical properties , which makes them good candidates for HME (Table 4.1). The most commonly used polymers in this family of excipients are HPMC and hydroxypropyl cellulose (HPC).
4.1.2.1 Hydroxypropyl Methyl Cellulose
HPMC, a cellulosic derivative with a melting point of approximately 190 °C is a water-soluble polymer used extensively in the pharmaceutical solid dispersions. HPMC has been shown to be a good stabilizer for amorphous tacrolimus by maintaining a kinetic supersaturation over a much more prolonged period of time as compared to PVP and PEG (Yamashita et al. 2003; Fig. 4.3). The PVP and PEG polymers are well known for solubility enhancement, but they lack stabilization effect for ASD.
To date, there are numerous commercial products in the market such as Certican®, Nivadil®, Crestor®, Prograf®, and Sporanox® in which HPMC is used as a carrier for the solid dispersions. Sporanox® utilized spray-dried layering of the HPMC and the drug onto non-pareil beads. The amorphous API was shown to be stabilized by the hydrophilic matrix.
4.1.2.2 Hydroxypropyl Cellulose
HPC has excellent thermoplastic properties, low-melt viscosity, fast melt-flow properties, and low glass transition temperature ( − 4 °C) which makes it a good candidate for HME (Table 4.2). Low molecular weight grades such as Klucel EF or ELF are typically processed at lower temperatures (120 °C) and are commonly used in immediate release applications to enhance solubility of low solubility drugs. In general, Klucel acts as a matrix in which APIs are immobilized and dispersed in either nanocrystalline or amorphous state. On the other hand, high molecular weight grade (HF) is processed at high temperature (200 °C) and is used for controlled release applications.
Due to the unique mechanical properties of HPC, it is widely used in many applications such as extruded films, solid dispersions, and hot-melt extruded tablet formulations to name a few.
4.2 Ionic/pH-Dependent Polymers
Ionic/pH-dependent polymers are further categorized into two categories: (1) cationic polymers and (2) anionic polymers.
4.2.1 Cationic Polymers
4.2.1.1 Eudragit® EPO
Eudragit® EPO is a cationic copolymer composed of dimethylaminoethyl methacrylate, butyl methacrylate, and methyl methacrylate. The polymer gets ionized and solubilized at pH below 5.5. It is swellable and permeable at higher alkaline pH conditions. The molecular weight of the polymer is approximately 47,000 g/mol with a glass transition temperature of ~ 48 °C (Table 4.1). Although glass transition temperature is low, due to its cationic nature, Eudragit® EPO has the capability to form a complex with anionic drugs, thus stabilizing the amorphous drug in the matrix due to strong intermolecular drug polymer interactions. Due to these unique properties, Eudragit® EPO is commonly used as an excipient in solid dispersions as well as in taste-masking applications using the melt extrusion and SD process. For example, Eudragit® EPO with cationic tertiary amine groups was shown to form a complex with anionic drugs like ibuprofen and masking the taste of the bitter API. High loading of drug > 35 % with 10 % talc using an extrusion process gave good results in terms of taste masking (Gryczke et al. 2011). In another study, bioavailability of fenofibrate solid dispersions manufactured using HME with Eudragit® EPO was significantly enhanced compared to conventional formulations (He et al. 2010).
4.2.2 Anionic Polymers
4.2.2.1 Eudragit® L 100-55
Eudragit® L100-55 is an anionic polymer based on methacrylic acid and ethyl acrylate, which starts dissolving at pH 5.5. It is a high molecular weight polymer, with a T g value of 110 °C, and capable of strong molecular interactions which results in improved supersaturation of amorphous drugs. Since it is an anionic polymer, it has a strong intermolecular interaction with the cationic drugs. For example, Maniruzzaman et al. have demonstrated that Eudragit® L100-55 interacted strongly with propranolol and diphenhydramine hydrochloride salts. The drugs were shown to be stable and maintained the amorphous state in the Eudragit® L100-55 polymer matrices (Maniruzzaman et al. 2013). Further, this polymer has ideal attributes for the formation of solid solution using the microprecipitated bulk precipitation (MBP) technique. The great potential of this polymer for application to MBP technology due to its anionic nature can be tapped to great advantage. Shah et al. successfully demonstrated the utility of the polymer in the preparation of solid dispersions using the MBP technique (Shah et al. 2012). Eudragit® L100-55 shows onset of significant degradation at 160 °C.
4.2.2.2 Eudragit® L100
Eudragit® L100, a pH-dependent anionic polymer that is fully ionized at pH 6.80, is extensively used as an excipient for controlled MBP, HME, and fluid bed layering to stabilize the amorphous dispersions. This polymer is commonly used for enteric functional coating as well as for controlled release delivery applications. Fan et al. 2009 have studied the effect of anionic (Eudragit® L100) and nonionic (Kollidon® K30) polymers on the dissolution profile of an amorphous gellable drug with low glass transition temperature (60 °C). The API was coated on cellet beads in a fluid bed with the help of either Eudragit® L100 or Kollidon® K30. The authors have successfully demonstrated that the anionic polymer (Eudragit® L100) protected API by preventing its gelling and clumping in situ, while the nonionic polymer (Kollidon® K30) promoted gelling. The observed phenomena can be explained by the fact that API molecules were dissolved in Eudragit® L100 matrix; in this manner, intermolecular interaction of drug molecules with water was minimized during the dissolution process and the surface area of interaction of the water molecules with that of the drug was increased before the drug molecules could be clumped into small particles. Eudragit® L100, being an ionic polymer, dissolves by exchanging ions with the alkaline phosphate buffer ions; hence, surface erosion is mainly the mechanism of dissolution. Ion-exchange ability results in fast erosion of the film. Additionally, the steady and fast hydration of the polymer is accelerated by the ion water-absorbing capacity of the API (Fig. 4.4; Fan et al. 2009).
4.2.2.3 Eudragit® S100
Eudragit® S100, an anionic methacrylate copolymer which ionizes at pH 7.0, is primarily used as an excipient for colonic drug delivery. However, this polymer has recently gained importance in the amorphous formulation development. Chauhan et al. showed that Eudragit® S100 inhibited the precipitation kinetics of the dipyridamole primarily due to drug–polymer interaction and increase in glass transition temperature . Also, Eudragit® S100 was shown to be superior compared to polymers with similar glass transition temperature such as Eudragit® E100, HPMC, PVP K90, and Eudragit® L100 (Chauhan et al. 2013). In another case, solid dispersions of piroxicam with Eudragit® S100 were prepared using spherical crystallization technique. The dissolution rate of piroxicam increased in vitro, and the amorphous state of the drug was stabilized over its shelf life (Maghsoodi and Sadeghpoor 2010).
4.2.2.4 Hypromellose Acetate Succinate
HPMCAS is a commonly used excipient in solid dispersions due to its desirable melt viscosity , high glass transition temperature , good thermal stability, and low hygroscopicity. It is soluble in organic solvents and insoluble in water and acidic media (pH < 5.5), but it dissolves at pH higher than 5.5. It is important to note that selection of the appropriate grade of HPMCAS polymer plays a significant role in terms of solubilization and crystallization inhibition. There are three available chemical grades (MF, AF, and LF) based on the succinyl to acetate ratios, each of which has two physical grades with different particle size (Table 4.1). The LF and LG grades are soluble at pH ≥ 5.5, MF and MG at pH ≥ 6.0, and HF and HG at pH ≥ 6.80. Higher succinyl to acetate ratio leads to higher hydrophilicity compared to lower ratios, which are more hydrophobic in nature. In case of drugs having higher melting temperature, lower succinyl to acetate ratio HPMCAS produce greater crystallization inhibition. In contrast, higher succinyl to acetate ratio HPMCAS produce better solubilization of the lipophilic drugs .
HPMCAS was extensively researched in the field of amorphous spray-dried dispersions, HME, and controlled precipitation and was proven to significantly enhance the solubilization of APIs, as well as physical stability and manufacturing reproducibility (Morgen et al. 2013; Friesen et al. 2008). Miller et al. reported that HPMCAS ASD enhanced the solubility and permeability of progesterone over other solubility enhancement techniques such as use of surfactant (SLS)/cyclodextrin (HPβCD) cosolvent (PEG-400). HPMCAS is indeed the excellent candidate for solid dispersions technology due to its high T g in the un-ionized state, high solubility in organic solvents, and low hygroscopicity. In addition to its amphiphilic nature, it has the capability to interact with the hydrophobic and hydrophilic pockets of the drug molecules. Moreover, its low adsorption of water molecules enhances the physical stability of the ASD (Miller et al. 2012) .
4.2.2.5 Hydroxypropyl Methylcellulose Phthalate
Hydroxypropyl methylcellulose phthalate (HPMCP) is a phthalic half ester of HPMC. Two types of HPMCP with different solubility (HP-55 and HP-50) are available. In addition, there is HP-55S, a special type of HP-55 which has higher molecular weight, higher film strength, and higher resistance to simulated gastric fluid compared to the regular grades. It has been reported that the ASD of griseofulvin prepared by coevaporation and of a new triazol antifungal drug candidate by SD using an enteric cellulosic ester HPMCP showed drastic increase in the dissolution rate compared to the pure drugs (Hasegawa et al. 1985; Kai et al.1996). Engers et al. reported that the amorphous SDD of itraconazole with HPMCP displayed the best homogeneity (the narrowest T g width) and the highest physical stability among the different stabilizers tested (Engers et al. 2010).
4.2.2.6 Cellulose Acetate Phthalate
Cellulose acetate phthalate (CAP) is a partial acetate ester of cellulose. One carboxyl group of the phthalic acid is esterified with the cellulose acetate. The finished product contains about 20 % acetyl groups and about 35 % phthalyl groups. In the acid form, it is soluble in organic solvents and insoluble in water. The salt formed is readily soluble in water. DiNunzio et al. investigated the effect of CAP on the bioavailability of itraconozole (ITZ) solid dispersions prepared by ultra-rapid freezing. The results indicated that ITZ to CAP ratio formulations provided the greatest degree and extent of supersaturation in neutral media. Although not fully investigated, it has been reported that the stabilization mechanism was due to interactions between the drug and polymer, primarily attributed to steric hindrance resulting from the molecular weight of the polymer chain and chemical composition of the polymer backbone relative to position of hydrogen-bonding sites. In addition, in vivo testing conducted in Sprague-Dawley rats (n = 6) demonstrated a significant improvement in oral bioavailability from the 1:2 ITZ:CAP (AUC = 4516 ± 1949 ng*h/mL) compared to the Sporanox pellets (AUC = 2132 ± 1273 ng*h/mL; p ≤ 0.05). From the results, it was concluded that amorphous compositions of ITZ and CAP provided improved bioavailability due to enhanced intestinal targeting and increased durations of supersaturation (DiNunzio et al. 2008).
4.2.2.7 Polyvinyl Acetate Phthalate
Polyvinyl acetate phthalate (PVAP) is a vinyl acetate polymer that is partially hydrolyzed and then esterified with phthalic acid. It has been reported to have a promising ability as a solid dispersion polymer for low solubility APIs due to a high T g and its propensity for hydrogen bond donating and accepting ability. Minikis et al. reported that PVAP spray-dried dispersions of fenofibrate, carbamazepine, and dipyridamole are found to be amorphous by powder X-ray diffraction (PXRD) and exhibited high T g values relative to the crystalline drug. Non-sink dissolution performance of the solid dispersions formulated with PVAP also showed increased solubility in vitro compared to the respective native crystalline drug. In addition, it has also been reported that the stability studies with PVAP as a dispersion polymer indicated no change in performance under accelerated storage conditions (Minikis et al. 2013).
4.3 Non-Polymeric Excipients
4.3.1 Amino Acid Derivatives
The high T g of the polymer does not always lead to protection of the amorphous drug from crystallization . Hence, very few drugs are commercially available on the market due to the physical instability of the drug in solid solutions. The smart concept of “co-amorphous drugs” utilizes low molecular weight polymers together with the amorphous drug. They protect the amorphous drugs by strong specific molecular interactions , which are better than the higher T g effect of the solid solutions. Löbmann et al. used the concept with the low molecular weight amino acids (e.g., phenylalanine, arginine, tyrosine, and tryptophan) as the polymer excipients for the co-amorphous drug formulations . The low molecular weight of the amino acids results in lower fraction of the excipient in the formulation. These materials are generally regarded as safe (GRAS) materials (Löbmann 2013).
4.3.2 Mesoporous Silica
Mesoporous silica was recently investigated as an excipient for formulations of molecules with low water solubility. These materials have very high specific surface area and small pore size. The customized template synthesis produces highly porous silica materials which can enhance the drug dissolution of hydrophobic molecules. Due to the porous nature and the controlled pore size volume of these materials, surface adsorption of the molecules to the mesoporous silica not only enhances the dissolution but also prevents the recrystallization of the amorphous materials . Due to the relatively finite space available to the amorphous molecules, the probability to align with their crystalline counterparts is low to negligible, resulting in amorphous stabilization of the drug. Van Speybroeck et al. used fenofibrate as the model drug for evaluating the SBA-15 (mesoporous silica) solid dispersion formulations. The DSC study showed the glassy nature of fenofibrate at a 40 % drug load, compared to 20 % load in their previous formulations. The amorphous nature could be attributed to the decrease in the availability of pore space, decreased surface adsorption of the fenofibrate molecule, as well as no molecular interaction with silanoyl groups. The formulations are stable over 6 months, thus the mesoporous silica could be a viable option for those drugs which are less miscible with the established polymers (Van Speybroeck et al. 2010) .
4.3.3 Solubilizers and Wetting Agents
Surfactants are most commonly used as solubilizers or emulsifying agents in ASD . Their primary objective is to increase the apparent aqueous solubility and bioavailability of the drug. As with polymers, solubility in organic solvents is an important consideration when preparing ASD from solutions in solvents. In the case of HME, surfactants can have a plasticizing effect, which allows processing at lower temperatures. Some of the commonly used surfactants include Polysorbate 20, Polysorbate 80, Vitamin E polyethylene glycol succinate, Polyoxyl 40 hydrogenated castor oil, etc. (Padden et al. 2011).
4.3.4 Plasticizers
The use of polymeric carriers in the case of HME processes generally requires the incorporation of a plasticizer into the formulation in order to improve the processing conditions of certain high molecular weight polymers or to improve the physical and mechanical properties of the final product. According to the free volume theory, with the inclusion of plasticizers (usually small molecules) in the polymers, the free volume between the polymer chains is increased, resulting in increased molecular motion, which is referred to as the plasticization effect. The choice of the suitable plasticizers depends on factors such as plasticizer–polymer compatibility and plasticizer stability (McGinity et al. 2000). Plasticizers help in lowering the processing temperatures necessary for production and improving the stability profile of the active compound and/or of the polymeric carrier (Repka and McGinity 2000). Plasticizers also lower the shear forces needed to extrude a polymer, thereby improving the processing of certain high molecular weight polymers (Zhang and McGinity 1999; Follonier et al. 1994).
Although researchers have investigated triacetin, citrate ester, and lower molecular weight polyethylene glycols as plasticizers in hot-melt extruded systems, most of them are in liquid state (Zhang and McGinity 1999; Follonier et al. 1994, 1995). It is difficult to get a homogeneous blend of ingredients prior to extrusion in case of liquid plasticizers. An incomplete mixing of a polymer powder with a liquid additive has been shown to result in unstable mass flow when feeding the mixture into the extruder (Tate et al. 1996). Studies have shown that the evaporation and loss of plasticizer, during a high-temperature process, may lead to stability problems in the finished dosage forms (Frohoff-Hulsmann et al. 1999; Gutierrez-Rocca and McGinity 1993). To overcome the shortcomings of liquid plasticizers , it may be useful to evaluate solid-state pharmaceutical excipients with plasticizing properties.
Desai investigated the effect of three plasticizers, stearic acid (284.48 g/mol), glyceryl behenate (414.66 g/mol), and PEG 8000 (8000 g/mol), on Eudragit® EPO during HME processing with respect to T g and percentage motor load. From the thermal analysis results, it was reported that with increasing concentration of the plasticizer, the T g of the polymer was found to decrease in case of stearic acid and had no effect on glyceryl behenate and PEG 8000, indicating that stearic acid is miscible with the polymer, whereas glyceryl behenate and PEG 8000 are immiscible (Desai 2007; Fig. 4.5).
In case of the HME process, the motor load is generally considered as a dependent parameter and mainly depends on feed rate, screw speed, as well as molecular and rheological properties of polymers and overall formulation. In another study, feed rate and screw speed were kept constant and the motor load was used as a response variable to determine the effect of solid-state plasticizers on the HME process. The results indicated that all the three plasticizers were successful in lowering percentage motor load with increase in concentration of plasticizers. This is attributed to increase in the free volume of the polymer which permits greater freedom of movement, thereby reducing the viscosity resulting in lowering the motor load (Desai 2007; Fig. 4.6). However, the impact of plasticizer on long-term stability of ASD and maintenance of supersaturation kinetics of the amorphous drug needs to be carefully assessed.
Repka et al. prepared films with HPC and polyethylene oxide by HME with and without Vitamin E TPGS. It was shown that Vitamin E TPGS reduces glass transition temperature by almost 11 °C compared to the films without Vitamin E TPGS (Fig. 4.7). In addition, films containing 3 % Vitamin E TPGS had similar mechanical properties to the films plasticized with PEG 400 and showed improved processing conditions by decreasing barrel pressure and torque during extrusion (Fig. 4.8; Repka et al. 2007).
4.3.5 Antioxidants
Antioxidants are most effective in stabilizing oxidation-prone drug formulations. They have the ability to inhibit or slow down chain reaction oxidative processes at relatively low concentrations. This property of the antioxidant substances is of considerable importance with respect to formulations because of the large number of chemically diverse medicinal agents known to undergo oxidative decomposition. Antioxidants are classified as preventive antioxidants or chain-breaking antioxidants based upon their mechanism. Preventive antioxidants include materials that act to prevent initiation of free radical chain reactions. Reducing agents, such as ascorbic acid, are able to interfere with autoxidation in a preventive manner since they preferentially undergo oxidation. The preferential oxidation of reducing agents protects drugs, polymers, and other excipients from attack by oxygen molecules. Chelating agents such as edetate disodium (EDTA) and citric acid are another type of preventive antioxidant that decrease the rate of free radical formation by forming a stable complex with metal ions that catalyze these reduction reactions.
Hindered phenols and aromatic amines are the two major groups of chain-breaking antioxidants that inhibit free radical chain reactions. Commonly used antioxidants such as butylated hydroxyanisole (BHA), butylated hydroxytoluene (BHT), and vitamin E are hindered phenols. Because the O–H bonds of phenols and the N–H bonds of aromatic amines are very weak, the rate of oxidation is generally higher with the antioxidant than with the polymer (Crowley et al. 2007).
4.4 Selection and Optimization of Excipients
As discussed in previous sections, there are various types of polymers, solubilizers, plasticizers, antioxidants, and other suitable fillers that can be used in the formulation of ASD. However, based on the physicochemical properties of the API, the type and level of excipients need to be carefully selected, as these would significantly impact the overall stability of ASD and eventually the bioavailability . Hence, it is strongly recommended to perform a proper study design based on quality by design (QbD) by varying ratios within the specifications of the excipients to better understand their effect on the selected API.
For example, there are three commercial grades of HPMCAS with fixed succinyl and acetyl content (wt %). In order to better understand the effect of the succinyl and acetyl content on solubility enhancement , Dow Pharma & Food Solutions in collaboration with Bend Research carried out the QbD studies within the United States Pharmacopoeia (USP) specifications of succinyl and acetyl content. The results of the studies of ASD of various drugs with varying physicochemical properties prepared by SD indicated that there is a big difference in solubility enhancement with respect to substitution of succinyl and acetyl content. However, some compounds are insensitive to changes in substitution level of succinyl and acetyl content. Hence, selection of right grade of HPMCAS is very crucial to maximize the solubility enhancement or find an area within the substitution space that will give an overall robust formulation and be less sensitive to change. In addition, the effect of molecular weight (succinate/acetate, wt %/wt %) on solubility enhancement has been studied and was found that in case of spray-dried dispersions, the solubility enhancement would depend on the type of API. In order to overcome the effect of molecular weight (high/low) during the SD process, Dow Pharma & Food Solutions developed Affinisol™ High Productivity HPMCAS (HP-HPMCAS) which falls within the USP monograph. It is a low molecular weight, low viscosity grade which allows increased solid loading as compared to commercial HPMCAS.
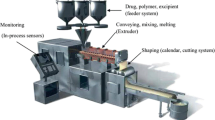
5 Impact of Excipients on Amorphous Solid Dispersion Processes
ASD are generally prepared by melting (fusion) or solvent methods (Chiou and Riegelman 1971). Polymers are the critical components in the manufacturing of ASD as they act as carriers for the drug and inhibit crystallization in both the dosage form and in vivo. The most important properties of the polymers such as the glass transition temperature (T g), solubility in organic solvents, and hygroscopicity need to be considered to make ASD that are stable and manufacturable so as to achieve target pharmacokinetic profiles for bioavailability enhancement.
5.1 Melting (Fusion) Methods
The critical polymer attributes that need to be considered for the manufacture of ASD by melt extrusion includes the melt viscosity, melting point/T g, and miscibility/solubility.
Melt Viscosity of the Polymer
Melt viscosity determines the extent of miscibility of the drug and polymer as well as the efficiency of the process. Polymers with low-melt viscosities and high thermal conductivity exhibit a more efficient melting process (Crowley et al. 2007). In contrast, if the melt viscosity of the polymer is too high, it may limit miscibility of the API and polymer (Forster et al. 2001). The melt viscosity of Kollidon® VA-64 is shown to be much lower than that of HPMCAS as shown in Fig. 4.9. Melt viscosity regulates motor load and diffusivity during processing. With respect to melt viscosity and solid solution capacity, Kollidon® VA-64 is a good candidate for HME, as it enables lower processing temperature with lower motor load and faster melt-dissolution rates compared to HPMCAS.
Melting point/Tg
To facilitate easy material transfer during the melt extrusion, the processing is performed at temperatures at least 20 °C above the melting point of a semi-crystalline polymer (or drug) or the T g of an amorphous polymer (Chokshi et al. 2005). Other material variables such as molecular weight and molecular weight distribution of the polymer, hygroscopicity, and presence of monomeric impurities can affect the melting point/T g and should be taken into consideration. As a rule of thumb, the processing temperature should be lower than T M of the crystalline drug substance but greater than T M or T g of the polymer.
Miscibility/Solubility
In order to form a one-phase system, the two molten components (drug and polymer) have to be miscible. It has been reported that the changes in melting point/T g as a function of polymer concentration provide a phase diagram to establish the boundary of solid-state miscibility and helps in selecting the processing temperature (Chokshi et al. 2005).
In addition, the selection of optimal melt-extrusion conditions depends on the chemical stability of the drug and polymer and the physical properties of the polymer. The processing parameters for melt extrusion and the impact of solid-state intermolecular drug–polymer interactions on supersaturation have been investigated by several research groups. HME performed on physical mixtures of poorly water-soluble drugs (Indomethacin, Itraconazole, and Griseofulvin) and hydrophilic polymers (Eudragit® EPO, Eudragit® L100-55, Eudragit® L100, HPMCAS-LF, HPMCAS-MF, Pharmacoat® 603, Kollidon® VA-64) at different drug to polymer ratios (30:70, 50:50, 70:30) indicated that higher supersaturation could be achieved for indomethacin, itraconazole, and griseofulvin using Eudragit® EPO, HPMCAS-LF, and Eudragit® L100-55, respectively. Transparent glassy extrudates were produced from most of the physical mixtures of indomethacin, itraconazole, and griseofulvin at the temperatures within ± 20 °C of their softening temperatures and speeds of 100, 150, and 200 rpm, respectively. It was reported that when the temperatures for HME were reduced significantly below their softening temperatures in order to compensate for low zero-rate viscosity of physical mixtures, nontransparent extrudates were produced as a dispersion of crystalline drug into the polymer matrix, whereas when the temperatures for HME were significantly increased above the softening temperatures, charring was reported due to degradation of the polymers (Sarode et al. 2013). Based on rheological properties of the materials, the HME conditions such as the lowest processing temperature and speed can be determined to prevent degradation of the drug and the polymer. An overview of various polymers with respect to their T g and degradation temperature (T deg) is summarized in Fig. 4.10. The polymer utility for melt extrusion is strongly related to the T g toT deg ratio. The processing conditions must be below the degradation temperature of the polymer, as thermal stability of the polymer can become an operating constraint in HME.
HPMCAS exhibits trend of increasing polymer degradation with temperature and rate of shear; the LF grade appears to be the most stable as shown in Fig. 4.11 (Sarode et al. 2014).
The stability of HPMCAS at higher temperatures for shorter periods of time has been examined to understand its behavior while considering processes such as HME (Shin-Etsu Chemicals Co., Ltd). In this study, the stability was tested at 150–180 °C, for 15–30 min. A powder sample was stored in an oven, and the tests were carried out according to Japanese Pharmaceutical Excipients (JPE), with the exception of the yellowness index , which was measured using a color computer. The observed changes were a decrease in viscosity (due to a decrease in the molecular weight of the polymer), an increase in free acid, and discoloration. From the results, it is suggested that the polymer itself will be fairly stable up to about 150 °C when subjected to this temperature for a short period of 15 min. The results are shown in Table 4.3 .
Drug dissolution in molten polymer can be accelerated to achieve a solid solution in the same way dissolution in aqueous media is improved:
-
Increase A (drug surface area): pre-micronization \(\frac{\boldsymbol{dM}}{\boldsymbol{dt}}{\bf =}\frac{\boldsymbol{DA}(\boldsymbol{C}_{\boldsymbol{S}}-\boldsymbol{C})}{\boldsymbol{h}}\)
-
Increase C s: Increase T, choice of polymer, cosolvents
-
Increase D: reduce viscosity, addition of plasticizers
-
Decrease h: screw design, screw speed, reduce viscosity
-
Increase Δt: HME residence time
In addition to the processing conditions, the miscibility of drug and polymer relies on their solubility parameter and interactions, hydrophobicity, and interfacial tension. An overview of the key points to consider for the commonly used polymers during HME process is summarized in Table 4.4. To reduce the processing temperature for high T g polymers, such as HPMC and PVP, it is a prerequisite that API is plasticized in the polymer.
5.2 Solvent-Based Methods
An important prerequisite for the manufacture of amorphous formulation using this process is that both the drug and the carrier polymer are sufficiently soluble in a low boiling point solvent (practically less than 75 °C). The solvent can be removed commonly by SD. SD is a common method to produce amorphous pharmaceuticals. In case of ASD prepared by solvent method like SD, the drug is dissolved in a solution of the hydrophilic polymer in an organic solvent. The critical material attributes that need to be considered include the solubility of the polymer in the solvent or solvent mixture and the viscosity of the feed solution. In general, 10 % or higher solubility of the polymer and the drug is desired to achieve a sufficient SD efficiency. The affinity of the solvent to the polymer and the drug as well as the drying conditions will determine the amount of residual solvent, which would impact the stability of the ASD. The viscosity of the feed solution should be kept below 250 cps for the pressure nozzles and centrifugal atomizers to assure adequate atomization (Gibson 2001).
Some amorphous drugs may be easily plasticized by water, resulting in gelling and incomplete dissolution recovery. Solid dosage form development of such amorphous drugs is considered quite challenging. Fan et al. (2009) have successfully shown that by understanding the drug and polymer properties together with appropriate selection of a manufacturing process, it is possible to develop an ASD with a low glass transition temperature of 60 °C and aqueous solubility of 0.8 mg/mL by overcoming gelling issues of the amorphous drug during dissolution. The drug and polymer (e.g., Eudragit® L100 versus PVP K30) are first dissolved in a solvent. This solution mixture is sprayed through a nozzle onto the surface of microcrystalline cellulose spheres in a fluid-bed coater. No drug–polymer interactions were reported when examined using FTIR, implying that this factor did not play a role in the differences observed in the release profiles. The anionic polymer protected the drug by preventing its gelling and clumping in situ, while the nonionic polymer promoted gelling (Fig. 4.12). On the other hand, gelling, clumping, and agglomeration were observed on the surface of the particles coated with PVP K30 which resulted in slow and incomplete release of the drug. From the anionic polymer coating, greater than 90 % drug was dissolved in 50 min, whereas the nonionic polymer coating released 60 % drug in 5 h (Fig. 4.13). As the drug gels at a critical moisture level and at a critical time interval, any delivery system that can protect the drug from reaching the critical moisture level can control the drug release. The drug is released via surface erosion from the Eudragit® L100 coating, whereas PVP K30, the nonionic polymer, releases the drug via a diffusion process. The results indicate that polymer properties can play a critical role in the release mechanism and kinetics of gellable drugs. An understanding of mechanisms involved in drug–polymer interactions will be useful to screen the polymers that are useful in engineering suitable delivery systems for such drugs.
5.3 Solvent-Controlled Precipitation/Microprecipitated Bulk Powder
This method is useful for the manufacture of ASD of poorly soluble compounds that do not have adequate solubility in low boiling point solvents and those that have very high melting points, rendering them less attractive for SD or melting (fusion) methods. Due to the nature of precipitation process employed in this technology, it is applicable only to ionic polymers that have pH-dependent solubility. Shah et al. (2012) investigated the efficiency of this technology in the manufacturing of ASD of two oncology compounds with different physicochemical properties using the solvent-controlled precipitation method. The polymers which were evaluated in this study included anionic polymers like Eudragit® L100, Eudragit® L100-55, and HPMCAS . The MBP formulation showed approximately 20-fold higher bioavailability compared to the micronized crystalline drug, suggesting that the amorphous form of API produced using MBP process was able to maintain the desired stability that resulted in complete dissolution and absorption. Based on the dog PK results, it was observed that the MBP process provided consistent pharmacokinetic profiles at different batch scales. The stabilization of amorphous dispersion was attributed to the high T g, ionic nature of the polymer that helped to stabilize the amorphous form by possible ionic interactions, and/or due to insolubility of polymer in water. As these polymers are water insoluble, they can absorb water without dissolving and hence the polymer: API interactions may be preserved to ensure stability of the amorphous form. Commonly used solid dispersions where water-soluble polymers such as povidone or copovidone are used as hydrophilic carrier can produce amorphous form due to high drug concentration: polymer miscibility, hydrogen bonding, and/or high T g. These, however, fail to maintain amorphous solid state because the carrier has high affinity for water, resulting in a drop in T g followed by disruption of the stabilizing hydrogen bonds. The enteric-polymers provide added advantage of ionic interactions that can better withstand the heat and moisture stress. This has been observed with other processes as well as HPMCAS in SD or melt extrusion (Rumondor and Taylor 2010; Dong et al. 2008). In addition to being an alternate technology to SD or HME, MBP technology provides advantages with respect to stability, density, and downstream processing.
An intrinsic primary particle size of the drug in the two-phase ASD system is one of the key factors that are critically important for bioavailability enhancement and amorphous stabilization. Shah et al. have shown that in an investigational oncology drug present in a two-phase ASD system, the particle size can be determined by stripping the polymer in an appropriate medium (i.e., Eudragit® L100 in phosphate buffer, pH 10, in which the drug is practically insoluble). The intrinsic primary particle size of the drug present in the ASD called MBP is much finer with narrower distribution than that produced by SD process. MBP is produced by a solvent-controlled precipitation (CP) method. Microscopic examination with high magnification, such as a Hirox digital camera, revealed that phase separation between drug and polymer was observed in the ASD produced by SD process due to differences in precipitation rate between drug and polymer (Fig. 4.14).
The bioavailability of the drug from ASD produced by SD was substantially reduced after downstream densification processing by roller compaction (Table 4.5). The densification processing of ASD via roller compaction may not be robust for handling the segregated amorphous API in the spray-dried formulation; hence, appropriate processing methods need to be established based on the solid-state properties of the ASD. In contrast, bioavailability of the drug from ASD produced by MBP process was maintained after downstream processing by roller compaction . Micro-embedding amorphous drug in the polymer matrix enhanced wettability of the ASD; therefore, the intrinsic dissolution of the ASD produced by MBP process was superior to the SD process. Wettability and intrinsic primary particle size of the drug present in the ASD are of critical importance to ensure bioavailability of poorly soluble compounds.
In addition, physical stability of the ASD produced by MBP process was maintained after 6-month storage at 40 °C/75 %RH, while crystal formation was observed in the ASD produced by the SD process.
Availability and utilization of various analytical techniques are essential to ensure the quality of the drug product throughout the development of ASD including process selection to effectively micro-embed the amorphous drug into the polymer matrix, downstream processing, and physical stability upon storage.
Intrinsic dissolution rate has been shown by Dong et al. to differentiate the quality attributes of an identical HPMCAS- based ASD composition of a poorly soluble drug, prepared by two different methods: (1) CP and (2) HME. The CP product was more porous and had a larger specific surface area than the HME product, as indicated by the BET results and SEM micrographs. Dissolution study using USP apparatus 2 showed that the CP product had a faster dissolution profile but slower intrinsic dissolution rate than the HME product (Fig. 4.15). The intrinsic dissolution rate of the HME product was shown to be higher than the CP product and it seems to have correlated well with the extent of drug absorption observed in dogs, particularly when given at a higher dose level (Fig. 4.16; Dong et al. 2008).
6 Marketed Products Using Amorphous Solid Dispersions
The selection of the polymer and manufacturing process are key factors in the success of the ASD development. An overview of marketed products using ASD is summarized in Table 4.6. Itraconazole is an interesting example of a drug product that was commercialized using an ASD technology and is among the first marketed solid amorphous dispersion products. The compound is a potent broad-spectrum triazole antifungal drug and is practically insoluble in water (solubility 4 ng/ml). Itraconazole is so insoluble in intestinal fluids that drug therapy with the compound could not be achieved without substantial solubility enhancement by formulation intervention. The original solid oral formulation, Sporanox® Capsule, was produced by a fluid-bed bead layering process that used a cosolvent system of dichloromethane and methanol to dissolve itraconazole and HPMC which was then sprayed on inert sugar spheres (Verreck et al. 2003). The resultant product provided a significant enhancement of itraconazole bioavailability with approximately 55 % of the administered dose absorbed (Lee et al. 2005). Itraconazole has recently been reformulated into a tablet composition that contains an amorphous dispersion in HPMC by HME utilizing MeltRx Technology®. The trade name is Onmel®; it is available in 200 mg strength for once-daily administration and was approved by the Food and Drug Administration (FDA) in April 2010 for the treatment of onychomycosis. The HME formulation not only eliminated the use of organic solvents in manufacturing but also reduced dosing frequency from twice daily to once daily (Six et al. 2004). ZelborafTM is a tablet dosage form containing an amorphous dispersion of vemurafenib in HPMCAS-LF produced by a solvent/anti-solvent precipitation method called MBP technology (Shah et al. 2012). In initial phase I clinical studies with a conventional formulation of vemurafenib, patients did not respond, i.e., no tumor regression, to doses as high as 1600 mg (Harmon 2010b). The issue was identified as low oral bioavailability stemming from poor solubility, which caused halting of the clinical study until it could be reformulated into a more bioavailable form. Due to melting point and organic solubility limitations, traditional ASD processes could not be applied, therefore necessitating the application of the MBP technology. When clinical trials resumed with the new MBP-based formulation, substantial tumor regression was achieved in majority of patients as a result of the enhanced formulation (Harmon 2010a). The application of the MBP technology to vemurafenib is a compelling case study for the application of ASD technology because formulation intervention was directly responsible for enabling the drug therapy and prolonging the lives of patients suffering from metastatic melanoma.
7 Safety and Regulatory Consideration of Excipients
Most of the pharmaceutical polymers used in ASD have already been approved for oral applications by major regulatory agencies (e.g., FDA, EMA) and have been published in the pharmacopeias (USP; European Pharmacopoeia, Ph. Eur.; Japanese Pharmacopoeia, JP). When evaluating safety of excipients used in solid dispersions, several factors have to be considered such as maximum allowable limit (IID) and LD50 (Table 4.7).
8 Summary
A thorough understanding of excipients and processes is crucial for achieving stable amorphous formulations with maximum bioavailability, as excipients and processes play a vital role in stabilization of the amorphous drug throughout its shelf life and in maintaining supersaturation of drug in solution in vivo. While selecting polymers, desirable attributes such as high T g, moisture scavenger capability, high molecular weight, and nucleation inhibition properties need to be evaluated. Micro-embedding amorphous drug in nano or micron sizes in the polymer matrix tremendously improves the wettability and physical stability of amorphous drugs. In addition, downstream processing needs to be selected appropriately based on the physicochemical and particulate properties of the ASD.
References
Albano AA, Phuapradit W, Sandhu HK, Shah N (2002) Stable complexes of poorly soluble compounds in ionic polymers. U.S. Patent 6.350,786 B1
Chauhan H, Hui-Gu C, Atef E (2013) Correlating the behavior of polymers in solution as precipitation inhibitor to its amorphous stabilization ability in solid dispersions. J Pharm Sci 102(6):1924–1935
Chiou WL, Riegelman S (1971) Pharmaceutical applications of solid dispersion systems. J Pharm Sci 60:1281–1302
Chokshi RJ, Sandhu HK, Iyer RM, Shah NH, Malick AW, Zia H (2005) Characterization of physico-mechanical properties of indomethacin and polymers to assess their suitability for hot-melt extrusion process as a means to manufacture solid dispersion/solution. J Pharm Sci 94:2463–2474
Craig DQM (2002) The mechanism of drug release from solid dispersions in water soluble polymers. Int J Pharm 231:131–144
Crowley MM, Zhang F, Repka MA, Thumma S, Upadhye SB, Battu SK, McGinity JW, Martin C (2007) Pharmaceutical applications of hot-melt extrusion: part I. Drug Dev Ind Pharm 33:909–926
Desai D (2007) Solid state plasticizers for melt extrusion. Dissertations and Master’s Theses Paper AAI3276980
DiNunzio JC, Miller DA, Yang W, McGinity JW, Williams RO III (2008) Amorphous compositions using concentration enhancing polymers for improved bioavailability of itraconazole. Mol Pharm 5(6):968–980
Dong Z, Chatterji A, Sandhu H, Choi D, Chokshi H, Shah N (2008) Evaluation of solid state properties of solid dispersions prepared by hot–melt extrusion an solvent co-precipitation. Int J Pharm 355:141–149
Ediger MD, Angell CA, Nagel SR (1996) Super cooled liquids and glasses. J Phys Chem 100:13200–13212
Engers D, Teng J, Jimenez-Novoa J, Gent P, Hossack S, Campbell C, Thomson J, Ivanisevic I, Templeton A, Byrn S, Newman A (2010) A solid-state approach to enable early development compounds: selection and animal bioavailability studies of an itraconazole amorphous solid dispersion. J Pharm Sci 99:3901–3922
Fan C, Pai-Thakur R, Phuapradit W, Zhang L, Tian H, Malick W, Shah N, Kislalioglu MS (2009) Impact of polymers on dissolution performance of an amorphous gelleable drug from surface-coated beads. Eur J Pharm Sci 37(1):1–10
Follonier N, Doelker E, Cole ET (1994) Evaluation of hot-melt extrusion as a new technique for the production of polymer-based pellets for sustained release capsules containing high loadings of freely soluble drugs. Drug Dev Ind Pharm 20:1323–1339
Follonier N, Doelker E, Cole ET (1995) Various ways of modulating the release of diltiazem hydrochloride from hot-melt extruded sustained-release pellets prepared using polymeric material. J Control Release 36:342–250
Forster A, Hempenstall J, Tucker I, Rades T (2001) Selection of excipients for melt extrusion with two poorly water-soluble drugs by solubility parameter calculation and thermal analysis. Int J Pharm 226:147–161
Friesen DT, Shanker R, Crew M, Smithey DT, Curatolo WJ, Nightingale JAS (2008) Hydroxypropyl methylcellulose acetate succinate-based spray-dried dispersions: an overview. Mol Pharm 5(6):1003–1019
Frohoff-Hulsmann MA, Schmitz A, Lippold BC (1999) Aqueous ethyl cellulose dispersions containing plasticizers of different water solubility and hydroxypropyl ethyl cellulose as coating material for diffusion pellets, I. Drug release rates from coated pellets. Int J Pharm 177:69–82.
Gibson SG (2001) How to optimize your spray dryer’s performance. Powder Bulk Eng 15:31–41
Greenhalgh DJ, Williams AC, Timmins P, York P (1999) Solubility parameters as predictors of miscibility in solid dispersions. J Pharm Sci 88(11):1182–1190
Gryczke A, Schminke S, Maniruzzaman M, Beck J, Douroumis D (2011) Development and evaluation of orally disintegrating tablets (ODTs) containing Ibuprofen granules prepared by hot melt extrusion. Colloids Surf B Biointerfaces 86(2):275–84
Gutierrez-Rocca JC, McGinity JW (1993) Influence of aging on the physical-mechanical properties of acrylic resin films cast from aqueous dispersions and organic solutions. Drug Dev Ind Pharm 19:315–332
Harmon A (2010a) After long fight. Drug gives sudden reprieve. The New York Times, February 23, Page A1
Harmon A (2010b) A roller coaster chase for a cure. The New York Times, New York, February 22, Page A1
Hasegawa A, Kawamura R, Nakagawa H, Sugimoto I (1985) Physical propertiesof solid dispersions of poorly water-soluble drugs with enteric coating agents. Chem Pharm Bull (Tokyo) 33:3429–3435
He H, Yang R, Tang X (2010) In vitro and in vivo evaluation of fenofibrate solid dispersion prepared by hot-melt extrusion. Drug Dev Ind Pharm 36(6):681–687
Hodge IM (1994) Enthalpy relaxation and recovery in amorphous materials. J Non-Cryst Solids 169:211–266
Ivanisevic I (2010) Physical stability studies of miscible amorphous solid dispersions. J Pharm Sci 99(9):4005–4012
Kai T, Akiyama Y, Nomura S, Sato M (1996) Oral absorption improvement of poorly soluble drug using solid dispersion technique. Chem Pharm Bull (Tokyo) 44:568–571
Kaushal AM, Gupta P, Bansal AK (2004) Amorphous drug delivery systems: molecular aspects, design and performance. Crit Rev Ther Drug Carrier Syst 21(3):133–193
Lee SL, Nam K, Kim MS, Jun SW, Park J-S, Woo JS, Hwang S-J (2005) Preparation and characterization of solid dispersions of itraconazole by using aerosol solvent extraction system for improvement in drug solubility and bioavailability. Arch Pharm Res 28:866–874
Leuner C, Dressman J (2000) Improving drug solubility for oral delivery using solid dispersions. Eur J Pharm Biopharm 50:47–60
Lindfors L, Forssén S, Westergren J, Olsson U (2008) Nucleation and crystal growth in supersaturated solutions of a model drug. J Colloid Interface Sci 325(2):404–413
Löbmann K (2013) Co-amorphous drug delivery systems. Pharm Solid State Res Cluster 18:19
Maghsoodi M, Sadeghpoor F (2010) Preparation and evaluation of solid dispersions of piroxicam and Eudragit S100 by spherical crystallization technique. Drug Dev Ind Pharm 36(8):917–925
Maniruzzaman M et al (2013) A review on the taste masking of bitter APIs: hot-melt extrusion (HME) evaluation. Drug Dev Ind Pharm:1–12 [Ahead of Print]
McGinity JW, Koleng JJ, Repka MA, Zhang F (2000) Hot-melt extrusion technology. In: Swarbrick J, Boylan JC (eds) Encyclopedia of pharmaceutical technology, 19th edn. Marcel Dekker, New York, pp 203–225
Miller JM, Beig A, Carr RA, Spence JK, Dahan A (9 Jun 2009–2016; 2012) A win win solution in oral delivery of lipophilic drugs: supersaturation via amorphous solid dispersions increases apparent solubility without sacrifice of intestinal membrane permeability. Mol Pharm 9(7):2009–2016
Minikis R, Konagurthu S, Freauff A, McVey A, Wilmoth J, House B, Kerkmann M, Pickens C (2013) Polyvinyl Acetate Phthalate (PVAP) as a solid dispersion polymer for improving bioavailabilityof poorly soluble compounds. AAPS J. San Antonio, Texas
Morgen M, Lyon D, Schmitt R, Brackhagen M, Petermann O (2013) New excipients for solubilizing APIS: tablets and capsules 2013-BASF
Omelczuk MO, McGinity JW (1992) The influence of polymer glass transition temperature and molecular weight on drug release from tablets containing poly (DL-lactic acid). Pharm Res 9:26–32
Padden BE, Miller JM, Robbins T, Zocharski PD, Prasad L, Spence JK, LaFountaine J (1 January 2011) Amorphous solid dispersions as enabling formulations for discovery and early development. Am Pharm Rev 14(1): pp 66
Pikal MJ, Lukes AL, Lang JE (1977) Thermal decomposition of amorphous beta-lactam antibacterials. J Pharm Sci 66:1312–1316
Reintjes T (2011) Solubility enhancement with BASF polymers: solubility compendium. October 2011
Repka MA, McGinity JW (2000) Influence of vitamin E TPGS on the properties of hydrophilic films produced by hot melt extrusion. Int J Pharm 202:63–70
Repka M, Battu S, Upadhye S, Thumma S, Crowley M, Zhang F, Martin C, McGinity J (2007) Pharmaceutical applications of hot-melt extrusion: part II. Drug Dev Ind Pharm 33:1043–1057
Rumondor AC, Taylor LS (2010) Effect of polymer hygroscopicity on the phase behavior of amorphous solid dispersions in the presence of moisture. Mol Pharm 7:477–490
Sarode AL, Sandhu H, Shah N, Malick W, Zia H (2013) Hot melt extrusion for amorphous solid dispersions: predictive tools for processing and impact of drug-polymer interactions on supersaturation. Eur J Pharm Sci 48:371–384
Sarode AL, Obara S, Tanno FK, Sandhu H, Iyer R, Shah N (2014) Stability assessment of hypromellose acetate succinate (HPMCAS) NF for application in hot melt extrusion (HME). Carbohydr Polym 101:146–53
Shah N, Sandhu H, Phuapradit W, Pinal R, Iyer R, Albano A, Chatterji A, Anand S, Choi DS, Tang K, Tian H, Chokshi H, Singhal D, Malick W (2012) Development of novel microprecipitated bulk powder technology for manufacturing stable amorphous formulations of poorly soluble drugs. Int J Pharm 438:53–60
Six K, Verreck G, Peeters J et al (2004) Increased physical stability and improved dissolution properties of itraconazole, a class II drug, by solid dispersions that combine fast- and slow-dissolving polymers. J Pharm Sci 93:124–131
Tate S, Chiba S, Tani K (1996) Melt viscosity reduction of poly (ethylene terephthalate) by solvent impregnation. Polymer 37 (19):4421–4424
Van Speybroeck M, Mellaerts R, Mols R, Thi TD, Martens JD, Van Humbeeck J, Annaert P, Van den Mooter G, Augustijn P (2010) Enhanced absorption of the poorly soluble drug fenofibrate by tuning its release rate from ordered mesoporous silica. Eur J Pharm Sci 41(20105) 623–630
Verreck G, Six K, Van den Mooter G et al (2003) Characterization of solid dispersions of itraconazole and hydroxypropylmethylcellulose prepared by melt extrusion—part 1. Int J Pharm 251:165–174
Yamashita K, Nakate T, Okimoto K, Ohike A, Tokunaga Y, Ibuki R, Higaki K, Kimura T (2003) Establishment of new preparation method for solid dispersion formulation of tacrolimus. Int J Pharm 267(1–2):79–91
Zhang F, McGinity JW (1999) Properties of sustained-release tablets prepared by hot-melt extrusion. Pharm Dev Tech 4:241–250
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Controlled Release Society
About this chapter
Cite this chapter
Vaka, S., Bommana, M., Desai, D., Djordjevic, J., Phuapradit, W., Shah, N. (2014). Excipients for Amorphous Solid Dispersions. In: Shah, N., Sandhu, H., Choi, D., Chokshi, H., Malick, A. (eds) Amorphous Solid Dispersions. Advances in Delivery Science and Technology. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1598-9_4
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1598-9_4
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1597-2
Online ISBN: 978-1-4939-1598-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)