Abstract
Extramedullary devices are being extensively employed to treat fractures in normal and diseased bone. Studies conducted in hospitals have shown that there is a wide variability in the manner different surgeons employ these devices for similar fracture types. Clinically, fixation devices are required to be able to: sustain loads; minimise patient discomfort and possible implant loosening; and promote healing. Computer simulation of the mechanical behaviour of these devices can help clinicians in selecting a device and optimising its configuration. Numerical modelling of the mechanical behaviour of bone-fixator constructs has been used in the past to evaluate the performance of these devices with respect to some of the clinical requirements. This Chapter considers the mechanics of some of the most commonly used extramedullary devices, their peculiarities and modelling implications while appraising existing numerical modelling literature that has attempted to address the above clinical demands. It finds that while many of the clinical questions have been answered satisfactorily using simple models, answers to some others require complex and sophisticated modelling approaches.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Fixation devices that use screws, pins, or wires are widely used for fracture management. Any implant will alter the natural load distribution within the host bone. Indeed, in fracture fixation, the intention is to redirect load and shield the bone from undesirable motion while supporting motion beneficial for callus formation until healing has occurred [1, 2]. This redirection of load also results in other unwanted effects: stress-shielding and stress concentration at the bone-implant interface. Stress-shielding, where the implant unloads a region of bone, has received much attention [3]. If shielding occurs, the load that has been removed from one area must be transferred somewhere else; hence, overloading of the device can also occur. On the other hand, stress concentrations in the bone arise because loads are transferred via the screws, pins, or wires that traverse the bone inducing large stresses/strains at the bone-implant interface. Extramedullary devices represent a considerable engineering challenge as they are eccentric to the dominant loading axis which induces additional bending and shear [4]. This chapter will focus exclusively on fixators which transmit the full weight-bearing loads until fracture healing is initiated (i.e. load-bearing as opposed to load-sharing devices).
For any fixation device there are three key clinical requirements and mechanical demands arising from them:
-
(a)
The device must promote healing. The correct level of relative motion between the bone ends at the fracture site, inter-fragmentary motion (IFM), is crucial for healing; too much or too little can inhibit fracture healing [2]. The most commonly investigated aspect of a device is its axial stiffness—usually derived from the IFM produced by a given load. The term “stability” is often used, clinically, as a synonym.
-
(b)
The device must sustain the applied loads for the duration of healing. This concerns the strength and potential failure of the device itself. Stresses within implants are of interest as breakage can occur; this is more likely if healing has been delayed [5]. Failure of devices is generally due to fatigue and not a single traumatic event, meaning small differences in stress can have a significant effect on the lifespan [6].
-
(c)
To minimise the detrimental impact of the device on the limb and any patient discomfort resulting from it. Excessive stress at the screw-bone (or wire-bone) interface is known to cause loosening around screw holes and carries a risk of infection [7, 8]. In addition, compromising the integrity of the bone due to screw holes or bone atrophy can lead to periprosthetic fracture during fixation or re-fracture after device removal [9].
The above requirements can be interdependent, for example, faster healing may reduce the fatigue strength demanded of a device; minimising damage to host bone around the screws will prevent discomfort and loosening and will, therefore, lead to faster healing. Therefore, the key variables of interest in numerical simulations, most commonly conducted using finite element (FE) models, are: IFM, device strength, and screw-bone interface damage.
With an ageing population fracture incidence will continue to rise leading to an increased use of these devices, particularly in bone of poorer quality. This will require robust biomechanically grounded guidance to help clinicians in selecting a device and optimising its configuration. This chapter outlines the mechanics of some of the most commonly used extramedullary devices. Each device has peculiarities which must be considered in the development of a computational model capable of addressing the above clinical requirements. The aim of this Chapter is to appraise the existing FE modelling research with respect to its ability in providing clinical guidance to surgeons who employ these devices.
2 Commonly Used Extramedullary Devices
2.1 Mono-Lateral Fixation
External fixation devices using screws can have a wide range of configurations [7]. One of the most widely used is the mono-lateral configuration which uses pins rigidly connected to an external frame on a single side of a limb (Fig. 1aa) making it useful in bones with subcutaneous boundaries such as the tibia [10]. Mono-lateral devices are fairly unobtrusive and are often better accepted than devices which encircle the whole limb, particularly by children [11]. Unfortunately, in all external fixation devices, pin loosening and infection are common complications, although these, and the risk of neurovascular and musculotendinous injury, are minimised when using “safe corridors” [7, 8, 12].
2.2 Ilizarov Fixation
In the Ilizarov fixator each bone fragment is supported by two or more tensioned Kirschner wires (typically 1.5–1.8 mm diameter) which are clamped to circular frames that surround the limb (Fig. 1bb) [13]. Paradoxically, Ilizarov devices are associated with lower rates of loosening than mono-lateral devices despite their smaller wire diameter, which would be expected to result in larger stress concentrations [14]. All external fixation devices allow for modifications during the course of healing; Ilizarov devices, in particular, are remarkable in their potential for bone regeneration with limb-lengthening gains of up to 1 mm per day [15]. They are, however, unwieldy and like all external fixators, they require significant wire entry-site care to prevent infection [8]. Compared with mono-lateral devices, Ilizarov fixation requires wires at many more entry sites around the bone which can tether musculotendinous units [7, 12, 16]. Hybrid devices comprising mono-lateral elements and Ilizarov rings have also been used to overcome the respective limitations of each.
2.3 Locked Plating
A specialised type of screw with a threaded head is able to “lock” into a plate producing a fixed-angle device—thereby functioning as an internal fixator rather than a plate (Fig. 1cc) [9, 17]. Locked plating is not associated with the many preloads induced by compression screws and is being widely promoted as having superior fixation in osteoporotic bone [18]. One of the benefits of internal fixation is fast rehabilitation and precise anatomical alignment. Percutaneous surgical techniques have also been developed to retain the soft tissue envelope reducing the detrimental impact of the operation [19]. Due to their close proximity to the bone locking plates can produce a very stiff mechanical environment [20]. While this has advantages, it can reduce inter-fragmentary movement inhibiting fracture healing [21]. Recently, some studies have advocated far-cortical locking where the locking screw only engages with the far cortex and thus produces a more flexible system [22].
3 Modelling Challenges
3.1 Modelling Boundary and Loading Conditions
Human gait imposes a number of different loading sources and directions. Bone experiences forces emanating from the joints and from muscles and ligaments. Ideally, all muscle forces and joint reactions should be included an a computational model; however, inclusion of all muscle forces in finite element models for a range of physiological activities is complex and is rarely undertaken [23, 24]. It can be argued that simplifications that incorporate key muscle forces and joint reactions are adequate for reasonable predictions of the behaviour of bone-fixator constructs. It is important, however, to ensure that the boundary conditions represent the in vivo loading scenario as closely as possible. Sometimes simplifications are made in order to validate in vitro experiments which have limitations in the type of loading that can be applied to the bone. Fully restrained boundary conditions (also called clamped or potted) are often used in experimental and numerical work to provide stability to the bone [24]. In some cases, fully restrained boundary conditions have been shown to offer an acceptable representation—provided they are far enough away from the region of interest [25]; in other cases, a clamped region will influence the global mechanical behaviour [23, 24].
The authors have been particularly interested in the manner in which the load is applied to the bone (in a lab experiment or for numerical simulation); this can result in significant differences to the mechanical response of the bone-fixator construct. For example, a common method of load application is through a universal joint which restrains translation but allows rotation [26, 27]. This produces an entirely different mechanical behaviour to an unrestrained load (which is only possible numerically). Clearly, the amount of restraint applied to the bone will influence the global stiffness of the bone-fixator system. This is reflected in the wide range of stiffness values predicted in the literature [26–28]. Typical conditions employed are shown in Fig. 2 along with the corresponding stiffness estimates for locked plating. It can be seen that, in the configuration shown, the predicted stiffness can vary by over seven times; however, with larger bridging spans or more flexible plates the differences observed could be even greater. The location of peak stress around screws or pins is also altered by the restraint applied to the system. It has been shown that critical screw location also changes with the manner of load application; the screw farthest from the fracture is critical for conditions 5a and 5b [28], whereas the screw closest to the fracture is critical for the condition shown in 5c [29, 30].
Examples of typical loading conditions employed by previous studies and the axial stiffness produced by the construct: (a) fully restrained proximally and distally [31, 32]; (b) fully restrained proximally pinned distally [28]; (c) pinned proximally and distally [26, 27]; and (d) hinged proximally and pinned distally which could be used as an alternative to the other conditions
In external fixation devices where the bending rigidity of the traversing screws or pins is much lower than the device itself, the majority of the IFM is produced by the deformation of the traversing elements. This is particularly true for full-pin or Ilizarov devices with bi-lateral or circular support. Due to the cantilever support, mono-lateral devices are more liable to bend resulting in IFM contributions from both screw bending and the device itself [4, 30]. The IFM generated by locking plates is largely produced by plate bending; as such, the length of plate free to bend between the two innermost screws (known as working length) has the most significant influence on construct stiffness [26, 27].
When the majority of IFM is produced by flexure of the traversing elements, the external frame or plate can be assumed to be rigid simplifying the numerical model [13, 30].
3.2 Modelling Implant-Bone Interface
Extramedullary devices rely on a secure bone-implant connection to transfer loads from bone to device. One of the difficulties when using extramedullary fixation is the progressive mechanical deterioration of the screw-bone interface [8, 20]. Stress/strain localisation at the implant-bone interface is the cause of the most common complications—loosening and infection, which are often severe enough to require implant removal [8].
Interface modelling is generally conducted using one of the following two approaches: (a) the implant and bone are assumed to be tied or (b) the interface is assumed to be separable with appropriate frictional contact conditions. The latter condition makes the model non-linear. The primary reason for inclusion of contact non-linearity between the screw and the bone is that a tied interface does not allow separation and so tensile strains can develop where in reality separation would occur [4, 33, 34]. A tied interface can, therefore, significantly underestimate strains at the screw-bone interface as they are transmitted in both tension and compression [4, 34]. Frictional contacts generally use linear Coulomb friction, with coefficients of friction ranging from 0 to 0.9 with the larger values used to represent screw threads [35, 36]. Non-linear friction has been used to replicate load-deformation pullout behaviour in the absence of screw threads [37]; however, idealised cylindrical representations of screws neglect the significant influence that screw threads can have on the local strain environment and the pullout force of screws [38]. It is known that, under pullout loading, the amount of load transmitted by each thread reduces with its distance from the screw head and the majority of the load is transferred at the first few threads [39, 40]. It should be noted that, despite the profound local influence, both the screw-bone interface representation and the inclusion of screw threads have minimal impact on the global load-deformation in most situations [34].
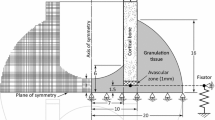
Studies have shown that each device produces a specific pattern of strain through the cortex at the screw-bone interface as shown in Fig. 3 [13, 29, 34]. Mono-lateral devices and locking screws (Figs. 3bb, c) induce large strains that penetrate the full cortical thickness particularly in bone of poor quality [29]. In Ilizarov and far-cortical locking fixation, however, strain localisation is at the periosteum and endosteum and does not penetrate the entire cortical thickness (Fig. 3aa, d) [13]. Device asymmetry and offset from the bone affect the stiffness of the construct. Although Fig. 3aa shows a bone centrally positioned between the supports at the mid-span of the wire, this is rarely possible as a prohibitively large ring would be required [16]. Asymmetric positioning of Ilizarov devices is known to increase their stiffness, due to a decrease in wire length to the support [7]; however, it also causes greater stress on the cortex closer to the ring. Similarly, when using mono-lateral devices, increasing offset from the bone has an approximately linear increase on screw-bone interface stress [4].
Clinically, in extramedullary fixation, the pilot hole initially drilled prior to screw insertion has a smaller diameter than the screw; this induces preloading at the screw-bone interface which has been shown to reduce loosening rates [41]; however, this feature is still rarely incorporated in modelling [37, 41–43]. A recent study by the authors employed anisotropic thermal expansion to mimic this preload and found that even small mismatches in size (1 %) can produce strains larger than those due to weight-bearing, causing yielding of surrounding bone [34, 44]. Bone, however, exhibits viscoelasticity causing a reduction in radial and circumferential preload over time [42, 43]. These effects can considerably influence predictions of interface stress and pullout strength and must be considered if the longer-term response is of interest.
The principal reason for screw-bone interface modelling is to examine the impact of the device on the host bone; therefore, the constitutive model of bone is also fundamental to the prediction [33].
3.3 Constitutive Modelling of Bone
Bone is known to be well represented by orthotropy or transverse isotropy [45]; despite this, isotropic representations are almost always used in simulation. In osteoporotic bone the cortex is thinner and the strength lower which increases susceptibility to damage at the screw-bone interface [13]. Due to the offset from the bone, mono-lateral devices can cause substantial pullout forces [29]. Osteoporotic bone is known to deteriorate more transversely and radially than axially, meaning its resistance to transverse forces is compromised [46]. This highlights the importance of material anisotropy when predicting bone damage in patients with osteoporosis [29, 47]. As well as a reduction in Young’s modulus, the cortical thickness of osteoporotic bone is known to decrease [48], which will influence predictions of screw-bone interface stress [4]. A wide range of constitutive models have been employed to represent the post-elastic behaviour of bone; these have been well summarised in some previous reviews [25, 49]. It is now generally agreed that strain-based constitutive models are more suitable than their stress-based counterparts [50, 51]. If damage or loosening at the screw-bone interface is to be predicted, material non-linearity must be included. Its inclusion, however, does not significantly influence IFM predictions [25, 29].
3.4 Modelling Geometrical Non-linearities
The inclusion of non-linear geometrical effects updates the deformation of the system as the loading increases. The geometric non-linearity of Ilizarov systems has been previously noted [52]. The wires behave more like cables than beams and axial forces transmitted through them change rapidly as the wires sag. As a result, geometrically non-linear analysis becomes essential. Also in these devices the inclusion of wire pretension increases the wire stiffness and hence reduces the screw-bone interface stress [13]. The deformation response of the system also becomes more linear with an increasing wire pretension [52].
In plating, the effect of plate bending must be captured to accurately predict IFM and stress in the plate. As load is applied to the plate, the plate bends which increases the eccentricity of the load. Figure 4 shows the relative importance of plate working length with and without the incorporation of non-linear geometrical effects.
The inclusion of non-linear geometrical effects is, therefore, essential for predictions of stress within the implants and motion at the fracture site [53]. This will be particularly relevant for fracture healing simulations in which interfragmentary strain is used at the stimulus [54].
4 Conclusions
Computer simulation of extramedullary devices can provide valuable information with respect to the clinical requirements which include: sustaining loads; minimising patient discomfort and possible implant loosening; and promoting healing. IFM or bone-fixator stiffness is a key determinant in indirect bone healing. Loading and boundary conditions can dramatically influence the stiffness and IFM of the bone-fixator system and must therefore be carefully considered in all fixator analyses. Similarly, inclusion of geometric non-linearity can radically alter IFM predictions and needs to be included. If only IFM prediction is required, then simplified material properties and implant-bone interactions are adequate.
If prediction of damage at the screw-bone interface or device loosening is required, the models need to be more complex as the local mechanical environment around the screws is significantly influenced by the bone properties and the model employed for screw-bone interaction. Consequently, these predictions require non-linear interface modelling and improved constitutive modelling of bone incorporating both anisotropy and material non-linearity. Due to this additional complexity, fewer studies have addressed these issues satisfactorily and research into non-linear modelling of bone and implant-bone interaction is on-going though it is still in its infancy.
References
McKibbin B (1978) The biology of fracture healing in long bones. J Bone Joint Surg Br 60-B(2):150–162
Gaston MS, Simpson AHRW (2007) Inhibition of fracture healing. J Bone Joint Surg Br 89-B(12):1553–1560
Uhthoff HK, Poitras P, Backman DS (2006) Internal plate fixation of fractures: short history and recent developments. J Orthop Sci 11(2):118–126
Huiskes R, Chao EYS, Crippen TE (1985) Parametric analyses of pin-bone stresses in external fracture fixation devices. J Orthop Res 3(3):341–349
Vallier HA, Hennessey TA, Sontich JK, Patterson BM (2006) Failure of LCP condylar plate fixation in the distal part of the femur. A report of six cases. J Bone Joint Surg Am 88(4): 846–853
Ellis T, Bourgeault CA, Kyle RF (2001) Screw position affects dynamic compression plate strain in an in vitro fracture model. J Orthop Trauma 15(5):333–337
Fragomen AT, Rozbruch SR (2007) The mechanics of external fixation. HSS J 3(1):13–29
Moroni A, Vannini F, Mosca M, Giannini S (2002) Techniques to avoid pin loosening and infection in external fixation. J Orthop Trauma 16(3):189–195
Perren SM (2002) Evolution of the internal fixation of long bone fractures. J Bone Joint Surg Br 84B(8):1093–1110
Sabharwal S, Kishan S, Behrens F (2005) Principles of external fixation of the femur. Am J Orthop 34(5):218–223
Gordon JE, Schoenecker PL, Oda JE, Ortman MR, Szymanski DA, Dobbs MB, Luhmann SJ (2003) A comparison of monolateral and circular external fixation of unstable diaphyseal tibial fractures in children. J Pediatr Orthop B 12(5):338–345
Behrens F (1989) General theory and principles of external fixation. Clin Orthop Relat Res 241:15–23
Donaldson FE, Pankaj P, Simpson AHRW (2012) Investigation of factors affecting loosening of ilizarov ring-wire external fixator systems at the bone-wire interface. J Orthop Res 30(5): 726–732
Board TN, Yang L, Saleh M (2007) Why fine-wire fixators work: an analysis of pressure distribution at the wire-bone interface. J Biomech 40(1):20–25
Spiegelberg B, Parratt T, Dheerendra SK, Khan WS, Jennings R, Marsh DR (2010) Ilizarov principles of deformity correction. Ann R Coll Surg Engl 92(2):101–105
Bucholz RW, Heckman JD, Court-Brown CM (eds) (2006) Rockwood & green’s fractures in adults, 6th edn. Lippincott Williams & Wilkins, Philadelphia, PA
Kubiak EN, Fulkerson E, Strauss E, Egol KA (2006) The evolution of locked plates. J Bone Joint Surg Am 88:189–200
Kim T, Ayturk UM, Haskell A, Miclau T, Puttlitz CM (2007) Fixation of osteoporotic distal fibula fractures: a biomechanical comparison of locking versus conventional plates. J Foot Ankle Surg 46(1):2–6
Ehlinger M, Adam P, Arlettaz Y, Moor BK, DiMarco A, Brinkert D, Bonnomet F (2011) Minimally-invasive fixation of distal extra-articular femur fractures with locking plates: limitations and failures. Orthop Traumatol Surg Res 97(6):668–674
Chao EYS, Aro HT, Lewallen DG, Kelly PJ (1989) The effect of rigidity on fracture healing in external fixation. Clin Orthop Relat Res 241:24–35
Epari DR, Kassi JP, Schell H, Duda GN (2007) Timely fracture-healing requires optimization of axial fixation stability. J Bone Joint Surg Am 89A(7):1575–1585
Bottlang M, Lesser M, Koerber J, Doornink J, von Rechenberg B, Augat P, Fitzpatrick DC, Madey SM, Marsh JL (2010) Far cortical locking can improve healing of fractures stabilized with locking plates. J Bone Joint Surg Am 92A(7):1652–1660
Phillips ATM, Pankaj P, Howie CR, Usmani AS, Simpson AHRW (2007) Finite element modelling of the pelvis: Inclusion of muscular and ligamentous boundary conditions. Med Eng Phys 29(7):739–748
Speirs AD, Heller MO, Duda GN, Taylor WR (2007) Physiologically based boundary conditions in finite element modelling. J Biomech 40(10):2318–2323
Pankaj P (2013) Patient-specific modelling of bone and bone-implant systems: The challenges. Int J Numer Method Biomed Eng 29(2):233–249
Hoffmeier KL, Hofmann GO, Mückley T (2011) Choosing a proper working length can improve the lifespan of locked plates: a biomechanical study. Clin Biomech (Bristol, Avon) 26(4):405–409
Stoffel K, Dieter U, Stachowiak G, Gächter A, Kuster MS (2003) Biomechanical testing of the LCP—how can stability in locked internal fixators be controlled? Injury 34(Suppl 2):11–19
Bottlang M, Doornink J, Lujan TJ, Fitzpatrick DC, Marsh L, Augat P, von Rechenberg B, Lesser M, Madey SM (2010) Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am 92A:12–22
Donaldson FE, Pankaj P, Simpson AHRW (2012) Bone properties affect loosening of half-pin external fixators at the pin-bone interface. Injury 43(10):1764–1770
Oni OO, Capper M, Soutis C (1993) A finite element analysis of the effect of pin distribution on the rigidity of a unilateral external fixation system. Injury 24(8):525–527
Yánez A, Cuadrado A, Carta JA, Garcés G (2012) Screw locking elements: a means to modify the flexibility of osteoporotic fracture fixation with DCPs without compromising system strength or stability. Med Eng Phys 34(6):717–724
Ahmad M, Nanda R, Bajwa AS, Candal-Couto J, Green S, Hui AC (2007) Biomechanical testing of the locking compression plate: when does the distance between bone and implant significantly reduce construct stability? Injury 38(3):358–364
Natali AN (1992) Nonlinear interaction phenomena between bone and pin. Clin Mater 9(2):109–114
MacLeod AR, Pankaj P, Simpson AHRW (2012) Does screw–bone interface modelling matter in finite element analyses? J Biomech 45(9):1712–1716
Karunratanakul K, Schrooten J, Van Oosterwyck H (2010) Finite element modelling of a unilateral fixator for bone reconstruction: Importance of contact settings. Med Eng Phys 32(5):461–467
Fouad H (2010) Effects of the bone-plate material and the presence of a gap between the fractured bone and plate on the predicted stresses at the fractured bone. Med Eng Phys 32(7):783–789
Dammak M, ShiraziAdl A, Zukor DJ (1997) Analysis of cementless implants using interface nonlinear friction—experimental and finite element studies. J Biomech 30(2):121–129
Zhang QH, Tan SH, Chou SM (2004) Investigation of fixation screw pull-out strength on human spine. J Biomech 37(4):479–485
Gefen A (2002) Optimizing the biomechanical compatibility of orthopedic screws for bone fracture fixation. Med Eng Phys 24(5):337–347
Grewal AS, Sabbaghian M (1997) Load distribution between threads in threaded connections. J Press Vessel Technol 119(1):91–95
Hyldahl C, Pearson S, Tepic S, Perren SM (1991) Induction and prevention of pin loosening in external fixation: an in vivo study on sheep tibiae. J Orthop Trauma 5(4):485–492
Norman TL, Ackerman ES, Smith TS, Gruen TA, Yates AJ, Blaha JD, Kish VL (2006) Cortical bone viscoelasticity and fixation strength of press-fit femoral stems: an in-vitro model. J Biomech Eng 128(1):13–17
Shultz TR, Blaha JD, Gruen TA, Norman TL (2006) Cortical bone viscoelasticity and fixation strength of press-fit femoral stems: A finite element model. J Biomech Eng 128(1):7–12
Kuhn A, Mc Iff T, Cordey J, Baumgart FW, Rahn BA (1995) Bone deformation by thread-cutting and thread-forming cortex screws. Injury 26(Suppl):12–20
Cowin SC, Mehrabadi MM (1989) Identification of the elastic symmetry of bone and other materials. J Biomech 22(6–7):503–515
Donaldson FE, Pankaj P, Cooper DML, Thomas CDL, Clement JG, Simpson A (2011) Relating age and micro-architecture with apparent-level elastic constants: a micro-finite element study of female cortical bone from the anterior femoral midshaft. Proc Inst Mech Eng H 225(H6):585–596
Giannoudis PV, Schneider E (2006) Principles of fixation of osteoporotic fractures. J Bone Joint Surg Br 88B(10):1272–1278
Russo CR, Lauretani F, Seeman E, Bartali B, Bandinelli S, Di Iorio A, Guralnik J, Ferrucci L (2006) Structural adaptations to bone loss in aging men and women. Bone 38(1):112–118
Carretta R, Lorenzetti S, Muller R (2013) Towards patient-specific material modeling of trabecular bone post-yield behavior. Int J Numer Meth Biomed Eng 29(2):250–272
Pankaj P, Donaldson FE (2012) Algorithms for a strain-based plasticity criterion for bone. Int J Numer Meth Biomed Eng 29(1):40–61
Bayraktar HH, Morgan EF, Niebur GL, Morris GE, Wong EK, Keaveny TM (2004) Comparison of the elastic and yield properties of human femoral trabecular and cortical bone tissue. J Biomech 37(1):27–35
Zamani AR, Oyadiji SO (2009) Analytical modelling of kirschner wires in ilizarov circular external fixator as pretensioned slender beams. J R Soc Interface 6(32):243–256
Prendergast PJ (1997) Finite element models in tissue mechanics and orthopaedic implant design. Clin Biomech 12(6):343–366
Simon U, Augat P, Utz M, Claes L (2011) A numerical model of the fracture healing process that describes tissue development and revascularisation. Comput Methods Biomech Biomed Engin 14(1):79–93
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this paper
Cite this paper
MacLeod, A., Pankaj, P. (2014). Computer Simulation of Fracture Fixation Using Extramedullary Devices: An Appraisal. In: Doyle, B., Miller, K., Wittek, A., Nielsen, P. (eds) Computational Biomechanics for Medicine. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0745-8_7
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0745-8_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0744-1
Online ISBN: 978-1-4939-0745-8
eBook Packages: EngineeringEngineering (R0)