Abstract
Tumour oxygenation is an important determinant of radiotherapy outcome as it could modulate cellular radiation sensitivity. Advanced PET imaging able to characterise this microenvironmental aspect in vivo might be used to devise counteracting therapies as it could provide information on the severity and the spatial distribution of the hypoxic regions. This study reviews the advantages and limitations of PET for imaging and quantifying tumour hypoxia and proposes a novel approach to obtain absolute levels of hypoxia from PET images through the use of EPR oximetry. This would offer a significant advantage over proposals based on empirical conversions of the intensities in the PET images to relative radiosensitivities. Thus, tumour hypoxia must be taken into account at the stage of treatment planning for photons and particle therapy by accounting for its extent and severity through the use of PET imaging combined with absolute EPR measurements.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
One of the problems in the management of cancer resides in the characteristics of the tumour microenvironment in comparison to the normal tissues [1]. For radiation therapy in particular, tumour hypoxia has an important role to play since the radiosensitivity of the cells is related to their oxygenation, as proposed more than 60 years ago by Gray and colleagues [2]. Thus, as hypoxic cells are less sensitive to radiation, they have increased probabilities of surviving at the end of curative radiotherapy. This has been supported by several clinical studies that have shown that impaired tumour oxygenation correlates with the failure of radiation treatment [3–5]. Consequently, several approaches have been proposed to overcome the resistance to treatment of the hypoxic tumours, including the use of radiation sensitisers, increasing the oxygen content of the tumours or targeting the hypoxic foci in tumours. The latter approach has seen increasing momentum in recent years due to technological developments of imaging methods capable of rendering the localisation and the extent of adverse metabolic processes.
This article presents a short review of available dose painting techniques based on PET hypoxia imaging and their limitations from the point of view of the ability to accurately map the target in terms of radiation resistance related to the tumour oxygenation. A solution for overcoming the most severe limitations has been identified and the conceptual approach will be presented here.
2 Treatment Planning Based on Tumour Oxygenation
Current practice in radiation therapy is based on physical optimisation of the dose distribution according to the anatomical information regarding the localisation and the extent of the tumour and the normal tissues. Routine planning in clinical radiation treatment does not generally take into account the particular radiation sensitivity of the tumour of an individual patient or the spatial and temporal heterogeneity of cellular radioresistance. However, it is well known that these aspects may be the cause of treatment failure for a considerable proportion of the non-responding patients, as the standard dose prescription does not ensure the dose levels needed to counteract the radiation resistance of the tumour cells.
The progress in imaging methods during the last decade has significantly improved cancer diagnosis and prognosis by increasing the accuracy of delineating target structures on a background of normal tissue anatomy and has formed the basis for 3D and 4D-based radiation treatment methods. Among the imaging techniques, positron emission tomography (PET) has the advantage of being almost non-invasive, using tracers that are usually metabolic substitutes and relatively sensitive, since quite low concentrations of tracers could be imaged.
Several tracers are now available for imaging tumour hypoxia with PET. Fluoromisonidazole (FMISO) was the first nitroimidazole derivative radiolabeled with 18F proposed for hypoxia imaging with PET and currently is the most used hypoxia tracer [6, 7]. The relatively low uptake of FMISO in hypoxic lesions coupled with its slow clearance from the well oxygenated healthy tissue, has led to the development of other 18F-labelled nitroimidazoles like Fluoroetanidazole (FETA) and Fluoroazomycinarabinofuranoside (FAZA) [8, 9] and non-imidazole tracers like Cu(II)-diacetyl-bis-N-(4)-methylthiosemicarbazone (Cu-ATSM) [10].
Several modelling studies have presented various approaches with different degrees of complexity to include the imaging information into treatment planning. A common approach is to delineate a hypoxic subtarget in the tumour and prescribe a more or less empirical escalation of the dose according to available radiation therapy techniques considering the tolerance of the normal tissues around the tumour [7, 11]. The risk, however, is that the prescribed dose is not large enough to counteract the hypoxic radioresistance and therefore the method might fail to achieve the expected results in clinical settings. Other approaches have recommended highly heterogeneous dose distributions based on a linear increase of the prescribed dose according to the signal intensity in the PET image [12] or as a result of redistributing the dose to the target, by increasing the dose to the hypoxic voxels while decreasing the prescribed dose to the remaining voxels in the tumour [13]. More complex approaches for heterogeneous dose prescription make use of dynamic PET information [14]. However, heterogeneous dose distributions are at risk of failing to provide the expected results for cases of dynamic hypoxia, as have indeed been seen in the clinic [15, 16].
Recently a paradigm shift in the biological prescription and adaptation of the treatment based on the quantitative analysis of the biological and functional information obtained by PET-CT imaging of tumour hypoxia was proposed [17, 18] and included in a research planning system for advanced studies. In order to devise a plan according to the proposed algorithm for treatment planning based on tumour hypoxia in Toma-Dasu et al. [17], the hypoxic compartments within the gross tumour volume (GTV) based on the uptake levels calculated relative to a well-oxygenated region in the patient are delineated. The hypoxic regions are defined according to a preset oxygenation threshold. The PET image is, therefore, first converted into oxygenation maps. The distribution of dose-modifying factors, calculated from the oxygenation map, is subsequently used for defining physical dose objectives for the subregions of the clinical target volume. These objectives are then delivered to the treatment planning module, together with additional objectives and constraints for the organs at risk. The feasibility of the proposed method for dose prescription and treatment planning based on FMISO-PET hypoxia was tested on several head-and-neck patients and the results were recently published [17].
3 Role of EPR Oximetry in PET Hypoxia Calibration for Treatment Planning Based on Tumour Oxygenation
The bioreductive markers used for imaging hypoxia with PET have selective retention in the hypoxic cells according to the inhibition of the chemical reaction of metabolizing the tracer in the presence of oxygen. Thus, the intensity in the PET image results from the differential uptake rate of the tracer according to the local tissue oxygenation. Therefore, the function used for converting the intensities in the PET image to oxygen partial pressures could be obtained by fitting experimental data of the tracer uptake under various hypoxic conditions with equations describing the inhibition of chemical reactions. It is important to note that experimental data on tracer uptake in vitro showed that various tracers would provide different levels of uptake and discrimination between hypoxic levels [6, 10] and hence they will lead to different images according to their uptake characteristics. Consequently, they might impact differently on the treatment planning based on hypoxia tracer uptake [18, 19]. However, it is not known to what extent the uptake of cells in vitro can mimic the uptake in the complex environment in vivo. Therefore, the need for acquiring the calibration of the tracer uptake as function of pO2 in vivo is warranted.
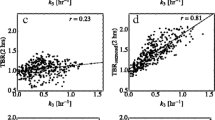
Electron Paramagnetic Resonance (EPR) oximetry is an interesting technique that allows the absolute determination of the oxygen partial pressure in vivo. It was recently shown that it could be used to qualify or disqualify other oxygen imaging methods and that good correlation was found between EPR oxygen measurements and PET hypoxia imaging with the 18F-labelled nitroimidazole derivative FAZA [20]. The full potential of the technique could be further pursued for overcoming the most critical limitation of the current approach for treatment planning based on tumour hypoxia. The method for EPR oximetry—PET hypoxia calibration proposed in this paper is illustrated in Fig. 19.1. Thus, pre-clinical EPR oxygen measurements on human HNSCC tumour xenographs in mice as well as in well oxygenated normal tissues together with subsequent hypoxia imaging with a microPET could provide the in vivo relationship between tracer uptake and pO2 that is needed for accurate quantification of tumour hypoxia. This calibration could be performed for several tracers that are available for PET hypoxia imaging.
The way these calibration curves are integrated in the dose planning chain going from the PET image to the dose distribution is illustrated in Fig. 19.2 for a head-and-neck cancer patient. However, the method has the potential to be used for other cancer types as long as suitable tumour xenografts are available for performing the pre-clinical EPR-based PET calibration.
Dose escalation factors for each voxel in the target relative to the homogeneous dose routinely prescribed could be determined if the relationship between the uptake of the tracer and the actual pO2 is determined based on EPR calibration and subsequently the relationship between pO2 and radiation sensitivity is employed
4 Conclusions
The proposed method for PET calibration with EPR would offer a significant advantage over proposals based on empirical conversions of the intensities in the PET images to relative radiosensitivities. Accurate quantification of PET hypoxia images would then be available and could provide an early identification of the clinical cases that might be suitable for dose escalation as well as the cases that could benefit from other counter-hypoxic measures.
References
Vaupel P, Kallinowski F, Okunieff P (1989) Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: a review. Cancer Res 49:6449–6465
Gray LH, Conger AD, Ebert M et al (1953) The concentration of oxygen dissolved in tissues at the time of irradiation as a factor in radiotherapy. Br J Radiol 26:638–648
Hockel M, Knoop C, Schlenger K et al (1993) Intratumoral pO2 predicts survival in advanced cancer of the uterine cervix. Radiother Oncol 26:45–50
Hockel M, Schlenger K, Aral B et al (1996) Association between tumor hypoxia and malignant progression in advanced cancer of the uterine cervix. Cancer Res 56:4509–4515
Brizel DM, Sibley GS, Prosnitz LR et al (1997) Tumor hypoxia adversely affects the prognosis of carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 38:285–289
Rasey JS, Grunbaum Z, Magee S et al (1987) Characterization of radiolabeled fluoromisonidazole as a probe for hypoxic cells. Radiat Res 111:292–304
Lee ST, Scott AM (2007) Hypoxia positron emission tomography imaging with 18f-fluoromisonidazole. Semin Nucl Med 37:451–461
Piert M, Machulla HJ, Picchio M et al (2005) Hypoxia-specific tumor imaging with 18F-fluoroazomycin arabinoside. J Nucl Med 46:106–113
Krohn KA, Link JM, Mason RP (2008) Molecular imaging of hypoxia. J Nucl Med 49(Suppl 2):129S–148S
Lewis JS, McCarthy DW, McCarthy TJ et al (1999) Evaluation of 64Cu-ATSM in vitro and in vivo in a hypoxic tumor model. J Nucl Med 40:177–183
Grosu AL, Souvatzoglou M, Roper B et al (2007) Hypoxia imaging with FAZA-PET and theoretical considerations with regard to dose painting for individualization of radiotherapy in patients with head and neck cancer. Int J Radiat Oncol Biol Phys 69:541–551
Alber M, Paulsen F, Eschmann SM et al (2003) On biologically conformal boost dose optimization. Phys Med Biol 48:N31–N35
Flynn RT, Bowen SR, Bentzen SM et al (2008) Intensity-modulated x-ray (IMXT) versus proton (IMPT) therapy for theragnostic hypoxia-based dose painting. Phys Med Biol 53:4153–4167
Thorwarth D, Eschmann SM, Paulsen F et al (2007) Hypoxia dose painting by numbers: a planning study. Int J Radiat Oncol Biol Phys 68:291–300
Roels S, Slagmolen P, Nuyts J et al (2008) Biological image-guided radiotherapy in rectal cancer: is there a role for FMISO or FLT, next to FDG? Acta Oncol 47:1237–1248
Dasu A, Toma-Dasu I (2013) Dose painting by numbers – do the practical limitations of the technique decrease or increase the probability of controlling tumours? IFMBE Proc 39:1731–1734
Toma-Dasu I, Uhrdin J, Antonovic L et al (2012) Dose prescription and treatment planning based on FMISO-PET hypoxia. Acta Oncol 51:222–230
Toma-Dasu I, Dasu A (2013) Biologically-optimised IMRT based on molecular imaging of tumour hypoxia – the impact of the tracer used. IFMBE Proc 39:1742–1745
Toma-Dasu I, Uhrdin J, Dasu A et al (2009) Therapy optimization based on non-linear uptake of PET tracers versus "linear dose painting". IFMBE Proc 25(1):221–224
Tran LB, Bol A, Labar D et al (2012) Hypoxia imaging with the nitroimidazole 18F-FAZA PET tracer: a comparison with OxyLite, EPR oximetry and 19F-MRI relaxometry. Radiother Oncol 105:29–35
Acknowledgments
Financial support from the Cancer Research Funds of Radiumhemmet, Stockholm and the LiU Cancer research network at Linköping University and the County Council of Östergötland (Sweden) is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media, LLC
About this paper
Cite this paper
Toma-Dasu, I., Dasu, A. (2014). Quantitative Hypoxia Imaging for Treatment Planning of Radiotherapy. In: Swartz, H.M., Harrison, D.K., Bruley, D.F. (eds) Oxygen Transport to Tissue XXXVI. Advances in Experimental Medicine and Biology, vol 812. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0620-8_19
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0620-8_19
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0583-6
Online ISBN: 978-1-4939-0620-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)