Abstract
The association between renal diseases and dyslipidemia has been recognized for a long time. Dyslipidemia increases the risk of cardiovascular events, contributes to the progression of renal insufficiency, and has been associated with allograft injury in renal transplant recipients. Although it is well known that the process of atherosclerosis begins in childhood, there were a limited number of studies in pediatric patients with chronic kidney diseases. The pattern of dyslipidemia differs among the major categories of renal diseases: nephrotic syndrome, chronic renal insufficiency/end-stage renal disease, and renal transplantation. Some patients with certain diseases encountered each of these stages progressively; thus, exposure to dyslipidemia can be more extended. In this chapter, epidemiology, causes, clinical implications, and treatment of lipid abnormalities in major renal disease categories of pediatric patients are discussed in light of the limited number of studies in this population. Concerning the differences between the disease profile of adults and children, adult data could not be directly translated in children. Thus, prospective investigations regarding the clinical implications and treatment of dyslipidemia in pediatric patients with kidney diseases are needed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic Kidney Disease
- Chronic Renal Insufficiency
- Kidney Transplant Recipient
- Cholesterol Ester Transfer Protein
- Chronic Allograft Nephropathy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Dyslipidemias in Patients with Nephrotic Syndrome
Introduction
Nephrotic syndrome (NS) is among the most common types of kidney diseases seen in children, and its incidence varies with age, race, and geography. The annual incidence in children in the United States and in Europe has been estimated to be 1–3 per 100,000 with a cumulative prevalence of 16 per 100,000 children [1, 2]. It is characterized by massive proteinuria, hypoalbuminemia, hyperlipidemia, and edema. Although NS most often occurs as a primary disorder in children, it can also be associated with systemic illnesses. Structural and functional abnormalities in the glomerular filtration barrier resulting in severe proteinuria are responsible for the clinical manifestations of NS. Minimal change NS is the most common form of idiopathic NS, accounting for more than 90 % of cases; other types, such as focal segmental glomerulosclerosis (FSGS) and membranoproliferative glomerulonephritis, are seen rarely [3]. It is more appropriate to categorize childhood NS according to response to steroid therapy, because renal biopsy is usually not performed in patients who respond to steroid therapy. Response to steroid therapy carries a greater prognostic weight than the histological findings on initial biopsy. Thus, two types of NS can be defined in the childhood period: steroid-responsive NS, in which the proteinuria rapidly resolves with therapy, and steroid-resistant NS, in which steroids do not induce remission [4]. It is estimated that about 80 % of children with idiopathic NS will respond to corticosteroid treatment with complete resolution of proteinuria and edema. Among this steroid-responsive group, the clinical course is variable, with up to 60 % having frequent relapses or becoming dependent on steroid therapy to maintain them in remission. Both of these groups are at increased risk of developing complications of NS and complications from frequent use of steroid and other immunosuppressive agents. On the other hand, the steroid-resistant group had significantly higher risk for development of complications of the disease, as well as progression of the disease to chronic kidney disease (CKD) and end-stage renal failure [5].
Hyperlipidemia is an almost universal finding in children with NS. In plasma, lipids are bound to lipoproteins, and the disturbances in lipid metabolism in NS result in increased levels of lipoproteins (hyperlipoproteinemia) and remodeling of the composition of lipoproteins (dyslipoproteinemia). The lipid profile is characterized by elevations in total plasma cholesterol, very low-density lipoprotein (VLDL), and low-density lipoprotein (LDL) cholesterol, and often triglyceride levels, as well as variable alterations (more often decreased) in high-density lipoprotein (HDL) cholesterol [6]. In addition, significant increases in plasma levels of lipoprotein(a), which is known to be both atherogenic and thrombogenic, are also often seen in children with proteinuria [7].
The definition of dyslipidemia differs in children and adults. The National Cholesterol Education Program pediatric report recommended that in order to identify children and adolescents with abnormal lipid and lipoprotein concentrations, total cholesterol concentrations of >200 mg/dL and LDL concentrations of >130 mg/dL be considered elevated [8]. The American Heart Association has recommended that triglyceride concentrations of >150 mg/dL and HDL concentrations of <35 mg/dL be considered abnormal for children and adolescents [9]. Owing to the concerns for using the same cut points for all children, percentile values for total cholesterol, triglycerides, LDL, and HDL cholesterol concentrations according to age and gender were developed in the 1981 prevalence study of the Lipid Research Clinics Program from the National Institute of Health [10]. Hyperlipidemia in children is defined as lipid levels greater than the 95th percentile for age and gender. For example, LDL concentrations greater than the 95th percentile (or HDL concentration less than the 5th percentile) would be considered abnormal, particularly if the abnormality was insistent. LDL concentrations between the 90th and 95th percentiles (5th–10th for HDL concentration) would be considered borderline. Clinical effects of natural changes in lipid and lipoprotein concentrations with age will be reduced with the use of these tables and percentiles [11].
Epidemiology
Almost all patients with NS or nephrotic range proteinuria have elevated total cholesterol levels, although some exceptions do occur (e.g., in glomerulonephritis). The plasma cholesterol concentration shows an inverse hyperbolic correlation with plasma albumin, accompanied by a steep rise in triglycerides in patients with severe hypoalbuminemia [12]. In patients with steroid-sensitive NS, hyperlipidemia resolves gradually upon developing a remission, whereas children with steroid-resistant NS who are refractory to therapy are often exposed to prolonged hyperlipidemia and its associated risks [13]. Moreover, it was shown that children with frequently relapsing NS have prolonged periods of hypercholesterolemia, even during clinical remission [14]. Merouani et al. [15] compared plasma lipid profiles of 25 children with NS at remission, with or without active prednisone treatment, with those of an age-matched population. Plasma total and LDL cholesterol were above normal in 12 of the 25 patients (48 %), with 7 of them having apolipoprotein B and triglyceride concentrations above normal. Hyperlipidemic profiles correlated significantly with number of relapse episodes.
Causes and Pathogenesis
Pathophysiology of nephrotic dyslipoproteinemia is multifactorial, including both an increased hepatic synthesis and a diminished plasma catabolism of lipoproteins [6]. Since its details have been mentioned in the “Dyslipidemia in Nephrotic Syndrome” chapter, herein, we do not further discuss the pertinent pathophysiology.
Clinical Implications
As early as 1969, Berlyne and Mallick reported an 85 times greater incidence of ischemic heart disease in adult patients with NS [16]. The question whether nephrotic hyperlipidemia is a cardiovascular (CV) risk factor for the patients is studied further exclusively in adults. In nephrotic children, there is only anecdotal evidence of myocardial infarction or documented atherosclerosis [17–19]. Antikainen et al. [20] investigated the arterial pathologies in renal arteries collected at nephrectomy in congenital NS of Finnish-type patients. They concluded that the vascular pathology, together with altered lipoprotein metabolism, indicates that children with congenital NS might have early atherosclerotic arterial disease risk. In an autopsy study of 40 children with NS due to mixed renal disease, a significantly increased incidence of mild to severe atherosclerotic changes were found when compared with 29 matched controls who died of non-renal causes [21]. These patients frequently have additional risk factors for ischemic events besides hyperlipidemia, such as hypertension, steroid-induced obesity, and insulin resistance, which may act together to produce atherosclerotic vascular lesions. Lechner et al. [22] evaluated if relapsing childhood NS would predispose patients to develop cardiovascular (CV) disease as young adults, in 62 patients between 25 and 53 years of age who had steroid responsive-dependent NS during childhood. They found that the occurrence of cardiovascular mortality is similar to that of the general population; and suggest that steroid-responsive NS during childhood is not a risk factor for cardiovascular events in early adulthood in the absence of traditional risk factors.
Therapy-resistant NS almost invariably leads to progressive renal insufficiency, which is histologically characterized by progressive glomerulosclerosis and tubulointersititial fibrosis. This development is driven by pathological mechanisms analogous to atherosclerosis, regarded by many investigators as an active process [23–25]. There is also evidence that hyperlipidemia contributes to the progression of renal insufficiency in nephrotic patients. This was first shown in animal experiments with cholesterol-rich diets that induced focal sclerosis in strains of guinea pigs, rats, and rabbits [26]. Lipid-lowering drugs reduced proteinuria and the development of focal sclerosis, and retarded the progression of established glomerular disease in rats [27]. Muntner et al. [28] studied the relationship between plasma lipids and decreasing renal function in 12,728 patients in their Atherosclerosis Risk in Communities Study and found that HDL, HDL-2 cholesterol, and triglycerides appeared to be predictors of creatinine increase. Thus, experimental and clinical evidence demonstrates that hyperlipidemia could cause renal injury.
Treatment
Healthy-eating dietary advice is advocated in steroid-responsive NS, where the hyperlipidemia usually resolves as proteinuria abates. Dietary fat restriction is usually recommended in hyperlipidemic states of steroid-resistant NS. Dietary supplementation with fish oil has some lipid-lowering effects, mainly decreasing triglycerides [29].
There are some major classes of lipid-lowering drugs: bile acid sequestrants (cholestyramine, colestipol), fibric acid derivatives (gemfibrozil, bezafibrate), nicotinic acid derivatives (niacin), probucol, hydroxymethylglutaryl CoA (HMG-CoA) reductase inhibitors (lovastatin, fluvastatin, pravastatin, simvastatin), and cholesterol absorption inhibitors such as ezetimibe [6, 30]. In general, these drugs are widely used in adult patients, but experience in patients with childhood NS is limited.
Bile acid-binding resins act by binding the cholesterol in bile acids in the intestinal lumen, which prevents their reuptake as part of the enterohepatic circulation. Average lowering of cholesterol is 10–20 % below baseline. Although these drugs do not have systemic effects, the side effect of gastrointestinal discomfort and difficulties in the administration of the medicines limit their use for young patients [11].
Fibrates are used for elevated triglyceride concentration; however, these drugs have not been extensively studied in children. Fibric acid derivatives lead to a decrease in VLDL production by inhibiting the synthesis and increasing the clearance of the VLDL apoprotein B. These medications also impede peripheral lipolysis and decrease hepatic extraction of free fatty acids, which reduces hepatic triglyceride production. The risk of myopathy and rhabdomyolysis is markedly increased when fibrates are used together with statins or in patients with renal insufficiency [11]. Büyükçelik et al. [31] evaluated the effects of gemfibrozil on hyperlipidemia in 12 children with persistent NS and found that at the end of the fourth month, gemfibrozil reduced total cholesterol by 34 %, LDL by 30 %, apolipoprotein B by 21 %, and triglycerides by 53 % without any side effects. HDL cholesterol and apolipoprotein A levels were not significantly altered.
Niacin or nicotinic acid lowers LDL and triglyceride concentrations while increasing HDL concentration. The mechanism of action is by decreasing hepatic production of VLDL. Niacin may also lower lipoprotein(a) levels. Niacin is a potentially attractive medication for management of dyslipidemia. However, adverse effects, including flushing, hepatic failure, myopathy, glucose intolerance, and hyperuricemia, were impediments to recommending niacin for routine use in the treatment of pediatric dyslipidemia [11].
Probucol is a diphenolic compound with anti-oxidant and anti-inflammatory properties that reduces atherosclerosis and lipid-lowering effects [32]. Querfeld et al. [33], in a prospective uncontrolled multicenter study, found that probucol treatment decreased serum concentrations of triglycerides (15 %), total cholesterol (25 %), VLDL cholesterol (27 %), LDL cholesterol (23 %), and HDL cholesterol (24 %), as well as apolipoprotein A-I, apolipoprotein B, and malondialdehyde levels after 12 weeks of treatment in persistent childhood NS. The positive effects of probucol on the lipoprotein profile persisted over 24 weeks; however, there was no significant effect on either proteinuria or glomerular filtration rate (GFR). The drug was well tolerated but had to be discontinued because of prolonged QT interval in some patients.
Statins inhibit the rate-limiting enzyme 3-hydroxy-3-methyl-glutaryl coenzyme A (HMG-CoA) reductase for endogenous synthesis of cholesterol, which lowers the intracellular cholesterol level and upregulates the LDL receptors, resulting in increased clearance of LDL from the circulation. The adverse effects of statins are increased hepatic transaminase and also creatine kinase levels, which may be associated with rare but clinically important episodes of rhabdomyolysis. Patients should be instructed to report symptoms of muscle aches or cramping, and they should be monitored with periodic measurement of liver transaminase and creatine kinase levels [11]. The US Food and Drug Administration has approved the use of pravastatin for children with familial hypercholesterolemia who are 8 years and older, and lovastatin, simvastatin, fluvastatin, atorvastatin, and rosuvastatin for children ≥10 years, regardless of pubertal status. Coleman et al. [34] have assessed the efficacy and tolerability of diet prior to and in combination with HMG-CoA reductase inhibitor, simvastatin, in seven children with steroid-resistant NS with a mean age of 8 years. They found that dietary advice alone had little impact on lipid levels of children with persistent NS, whereas simvastatin produced a significant and sustained reduction in lipid levels. On a median simvastatin dose of 10 mg/day, there was a 41 % reduction in cholesterol level and 44 % reduction in triglyceride level at 6 months that was sustained at 12 months in five patients. The drug was well tolerated with no clinical side effects noted. Similarly, Sanjad et al. [35] evaluated the efficacy and safety of statins (lovastatin and simvastatin) in 12 children with steroid-resistant NS followed prospectively for 1–5 years. A marked reduction in their total cholesterol (40 %), LDL cholesterol (44 %), and triglyceride levels (33 %) was observed, but there was no appreciable change in HDL cholesterol. Statin therapy was well tolerated without clinical and laboratory adverse effects. No changes were observed in the degree of proteinuria, hypoalbuminemia, or in the rate of progression to chronic renal failure.
The dietary cholesterol-absorption inhibitors represent the newest class of cholesterol-lowering agents. However, these medications have not been extensively studied in children. They are assumed to act mainly on intestinal absorption; but these drugs are absorbed, enter the enterohepatic circulation, and may have systemic effects [11]. Additional studies will be needed to evaluate their long-term effectiveness in young patients and patients with kidney diseases.
Another approach to the management of hyperlipidemia in refractory NS is the use of LDL apheresis. A prospective uncontrolled trial of LDL apheresis and steroid treatment in 17 patients with FSGS revealed rapid improvement in hyperlipidemia and partial or complete remission of NS in 71 % of the patients [36]. In another study, 11 children with steroid- and cyclosporine-resistant NS due to FSGS were treated with LDL apheresis, and 63 % entered into either complete or partial remission [37]. These findings suggest that in addition to its ability to ameliorate the hyperlipidemia seen in NS, LDL apheresis may be useful in maintaining remission in pediatric FSGS patients.
In view of the available evidence, it seems logical to treat hyperlipidemia in patients with unremitting NS in order to prevent progression of atherosclerosis and chronic renal failure. However, slowing the progression of renal failure by lowering cholesterol has not yet been demonstrated in patients with NS, and the degree of the preventive effect of lowering cholesterol level in atherosclerosis prevention is presently not measurable exactly. Concerns about possible side effects of the medications and the absence of clearly defined therapeutic endpoints are clear limitations. Therefore, it is not possible to make evidence-based recommendations for treatment of hyperlipidemia in pediatric patients. Pharmacological therapy with statins in children with NS should be done cautiously until controlled studies are conducted in this population.
Dyslipidemias in Patients with Chronic Renal Insufficiency and End-Stage Renal Disease
Introduction
The association between CKD and dyslipidemia has long been recognized; however, compared to the adult population, data about dyslipidemia in children with CKD remain scarce. Findings in children largely parallel those in adults. Dyslipidemia in chronic renal insufficiency (CRI) manifests principally as increased triglyceride and decreased HDL with nearly normal total cholesterol. The degree of dyslipidemia is usually found to be parallel to the degree of renal impairment. The addition of hemodialysis (HD) does not seem to significantly alter the pattern of dyslipidemia found in CRI, while peritoneal dialysis (PD) usually results in elevation of the total cholesterol level with further increases in hypertriglyceridemia [38].
Epidemiology
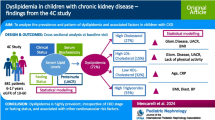
In 1981, Papadopoulou et al. [39] showed for the first time that alterations in serum triglycerides and alpha lipoproteins (HDL) occur early in CRI and before the onset of uremia when the GFR falls below 40 mL/min/1.73 m2 in pediatric patients. In these patients, the serum triglyceride levels become significantly elevated and alpha lipoproteins (HDL) markedly decreased as renal function deteriorates. These lipid abnormalities become further aggravated with the onset of hemodialysis. These findings were further supported by Zacchello et al. [40]. Recently, dyslipidemia profile of the largest number of patients (n = 391) with CKD was reported by Chronic Kidney Disease in Children (CKiD) investigators. One-third (32 %) of children had elevated triglyceride, 21 % had low HDL cholesterol, and 16 % had high non-HDL cholesterol. Overall, 45 % of the cohort had dyslipidemia, defined as one or more abnormal lipid measure; 45 % of those had combined dyslipidemia. Lower GFR was associated with higher triglyceride, lower HDL cholesterol, and higher non-HDL cholesterol. Compared to children with GFR >50 mL/min/1.73 m2, children with GFR <30 mL/min/1.73 m2 had an OR of 2.9 for any dyslipidemia (prevalence 65 %) and an OR of 8.58 for combined dyslipidemia (39 % prevalence). Compared to normal proteinuria, nephrotic proteinuria was strongly associated with dyslipidemia in these patients [41].
Dyslipidemia in pediatric HD patients were recognized earlier than CRI patients. Pennisi et al. [42] in 1976 reported that 93 % of the hemodialysis patients had elevated triglyceride levels and 13 % had elevated cholesterol. Then, further studies also showed elevated triglyceride levels and decreased HDL cholesterol in pediatric HD patients [7, 39, 40, 42, 43]. Papadopoulou et al. [39] showed the aggravation of these lipid abnormalities after onset of hemodialysis in CRI patients. Total cholesterol levels were found to be normal in majority of the hemodialysis patients. Elevated triglyceride and total cholesterol levels have been reported in 63–100 % and 30–100 % of pediatric PD patients, respectively [44–47]; some studies also revealed decreased HDL cholesterol levels [7, 47]. Muller et al. [48] compared the lipid profiles of patients with HD and PD and found that cholesterol and triglyceride levels were significantly higher in PD patients.
Pathogenesis
In CRI and end-stage renal disease (ESRD), lipoprotein synthesis does not appear to be significantly exaggerated, but studies consistently demonstrate impaired catabolism of triglyceride [38]. The diminished clearance of triglycerides, which can lead to hypertriglyceridemia, stems both from an alteration in the composition of triglycerides and from reductions in the activity of lipoprotein lipase and hepatic triglyceride lipase, which are involved in triglyceride removal. This results in accumulation of VLDL with impaired conversion to LDL, accompanied by low levels of circulating HDL. Therefore, uremic dyslipidemia is characterized by high triglyceride and low HDL cholesterol levels [49]. An important association is the consistent finding of increased concentrations of apoC-III, which has been implicated as a mediator of increased plasma triglyceride in several studies, in patients with CRI [50, 51].
Insulin resistance is a consistent finding of renal insufficiency [52]. The pattern of dyslipidemia associated with insulin resistance is similar to that found in patients with uremia [53]. Insulin regulates lipoprotein lipase in a tissue-specific manner, increasing its activity in adipose and decreasing it in muscle [54, 55]. Many individuals with uremia demonstrate a decreased insulin secretory response in addition to a post-receptor defect [56, 57]. Abnormalities of both insulin secretion and sensitivity may have significant roles in the development of disordered lipid metabolism in uremia.
The concentration of triglyceride-rich lipoproteins (TRL) (chylomicrons, VLDLs, and their remnants) is increased among individuals with CRI [58]. This relative hypertriglyceridemia also manifests within individual lipoprotein classes: the ratio of triglyceride to cholesteryl ester (CE) is higher in LDL and HDL and lower in VLDL and IDL [49, 59, 60]. A pathological increase in TRL is followed by the cholesterol ester transfer protein (CETP)-mediated transfer of the triglyceride from this expanded pool of substrate into HDL and LDL in exchange for CE [61]. Chylomicron and VLDL remnants have prolonged circulation and are found in increased levels in patients with CRI. HDL and its principal apolipoprotein, apoA-I, are found to be significantly decreased, probably as a consequence of elevated TRL, which induces transfer of excess triglyceride into HDL particles, increasing their susceptibility to serve as substrate for hepatic lipase [59, 62].
Patients with CRI usually demonstrate total cholesterol and LDL cholesterol that are similar to or slightly less than that of the general population, except for those on chronic PD, in whom these levels are usually elevated [58, 63]. Despite normal or low concentrations of LDL cholesterol, LDL particles are small and more dense than normal because of increased VLDL precursor and triglyceride/CE exchange followed by triglyceride lipolysis [64]. As small, dense LDL are prone to oxidation, and as oxidative stress is increased in CRI, levels of oxidized LDL are increased [65, 66].
Non-nephrotic proteinuria also affects lipoprotein physiology, and CRI is commonly associated with non-nephrotic proteinuria [49].
Peritoneal dialysis could aggravate dyslipidemia, since a high glucose load and peritoneal protein losses could stimulate hepatic production of VLDL. However, although most studies have observed an increase in lipoprotein lipids after the start of PD, reports have been inconsistent with respect to the influence of glucose load, nutrition, or protein losses on these abnormalities. Peritoneal losses of lipoproteins and apolipoproteins theoretically favor the loss of lower molecular weight lipoproteins, that is, HDL and apoA, which are protective against atherosclerosis [67].
Clinical Implications
Estimates of cardiovascular mortality rates in children and young adults who developed ESRD during childhood are 1,000 times greater than comparably aged healthy individuals [68]. For children on dialysis therapy, the anticipated lifespan is reduced by 40–60 years, and for transplant recipients, by 20–25 years compared with an age- and race-matched population [69, 70]. The most likely cause of this reduction in survival is an excessive burden of CV mortality, with 30–50 % of all deaths in this population attributed to CV causes that are related to both accelerated ischemic heart disease and premature development of dilated cardiomyopathy in young adult survivors of childhood-onset CKD [71]. Clinically evident CV lesions (symptomatic coronary artery disease, myocardial infarction, and cerebrovascular accident) luckily are rare in children and adolescents with CKD. However, there is increasing evidence showing significant subclinical CV abnormalities in this population [72]. In the 2006 American Heart Association guidelines for CV-risk reduction in high-risk pediatric patients, children with CKD were stratified for the first time as “high risk” for the development of CV disease, with associated “pathological and/or clinical evidence for manifest coronary disease before 30 years of age” [73]. As in adults, the risk factors believed to be responsible for accelerated CV disease in children with CKD can be divided into two primary groups: traditional risk factors for atherosclerotic disease (e.g., dyslipidemia, diabetes, hypertension, and smoking) and uremia-related risk factors that are unique to or far more prevalent in patients with CKD [72].
Treatment
Management of dyslipidemia is multifactorial. Therapeutic lifestyle changes (TLC) for children are similar to those recommended for adults. General nutritional guidelines on fat consumption, including lowering total, saturated, and trans fats and limiting cholesterol, should be carried out along with the proposals suitable for patients with CRI. Heart-healthy fats (margarines oils made from canola, corn, sunflower, soy, olives, peanuts) should be used. Obesity should be addressed, if present, and treatment of malnutrition related to CRI is essential, and increasing physical activity to reach and maintain a healthy body weight is recommended. Nutritional requirements to maintain growth should be provided. Studies in the general pediatric population have shown no adverse effects of dietary fat restriction on growth, development, or nutritional status; diet and lifestyle recommendations should be used with caution or not at all in children who are malnourished [74, 75]. Tube feeding can provide an appropriate energy intake with a balanced fat and carbohydrate profile that does not adversely affect serum lipids [76]. Correction of metabolic acidosis, vitamin D therapy, and correction of anemia with erythropoietin are essential because each of them is associated with improvements in lipid abnormalities [77–79]. Treatments known to reduce proteinuria may improve the lipid profile. Dietary fish oil supplementation (3–8 g/dL) was shown to reduce hypertriglyceridemia and improve atherogenic serum lipoprotein profiles in a small group of children with ESRD [80]. Dyslipidemia management should be undertaken in conjunction with all other available measures to reduce the overall risk of atherosclerotic CV disease. Modifiable, conventional risk factors (hypertension, cigarette smoking, obesity, glucose intolerance) should be assessed and managed according to existing guidelines. The phosphate binding agent sevelamer hydrochloride also acts as a bile acid sequestrant, and it has been shown to lower cholesterol levels in patients with CKD. A multicenter study that compared the efficacy and safety of sevelamer with calcium acetate in pediatric patients with CRI and ESRD showed that total cholesterol (−27 %) and LDL cholesterol (−34 %) levels decreased significantly with sevelamer treatment [81]. Similar results were shown by Gulati et al. [82] in pediatric patients with CKD stages 3 and 4.
The treatment of dyslipidemia in pediatric CKD is not well studied; there is limited information in the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines, and it is recommended that prepubertal children be managed according to existing national guidelines for children in the general population and that pubertal and postpubertal children and adolescents in any stage of CKD or with a kidney transplant be managed according to the K/DOQI guidelines for adults [74]. According to K/DOQI guidelines, adolescents with CKD should be considered to be in the highest risk category for dyslipidemias. Evaluation of dyslipidemias should occur after presentation with CKD, after a change in kidney failure treatment modality, and annually. Adolescents with CKD should be evaluated for dyslipidemia with a fasting lipid profile for total cholesterol, LDL, HDL, and triglycerides. If LDL is 130–159 mg/dL, start TLC diet (if nutritional status is adequate), followed in 6 months by a statin if LDL ≥130 mg/dL. If LDL ≥160 mg/dL, start TLC plus a statin.
For prepubertal children, The National Cholesterol Expert Panel on Children (NCEP-C) recommendations exist for the management of dyslipidemia in younger children [83]. However, they are not specific for patients with CKD or kidney transplant recipients. The NCEP-C recommends diet therapy as the primary approach for treating dyslipidemia in children. If LDL levels are more than 130 mg/dL, a step I diet (less than 10 % of total calories from saturated fatty acids, no more than 30 % of calories from total fat, less than 300 mg/day of cholesterol) is prescribed, followed in 3 months by a step II diet (further reduction of the saturated fatty acid intake to less than 7 % of calories, the cholesterol intake to less than 200 mg/day) if the target levels are not achieved. Pharmacological treatment is recommended in children aged ≥10 years, after an adequate trial of diet therapy, if LDL cholesterol remains ≥190 mg/dL or if LDL is ≥160 mg/dL and there is a positive family history of CV disease or if two or more CV disease risk factors are present in the child. However, the American Heart Association expert panel released an updated scientific statement addressing high-risk pediatric patients that considered pediatric CKD patients to be in the highest risk group [73]. In children with CKD and a fasting LDL >100 mg/dL, TLC, such as reduced dietary saturated fat and cholesterol intake and moderate exercise, are first recommended for the initial 6 months. If target levels (<100 mg/dL) are not reached, initiation of statin therapy is indicated. According to American Academy of Pediatrics (AAP) 2008 guideline, for patients 8 years and older with an LDL concentration of ≥190 mg/dL (or ≥160 mg/dL with a family history of early heart disease or ≥2 additional risk factors present or ≥130 mg/dL if diabetes mellitus is present), pharmacological intervention should be considered [11]. The initial goal is to lower LDL concentration to <160 mg/dL. However, targets as low as 130 mg/dL or even 110 mg/dL may be warranted when there is a strong family history of CV disease, especially with other risk factors, including obesity, diabetes mellitus, the metabolic syndrome, and other higher-risk situations [11].
It is difficult to develop an evidence-based approach for the specific age at which pharmacological treatment should be implemented. Statin use was limited in children. Long-term data on efficacy in pediatric patients are not available, and safety information on use of statins in children is not conclusive. The main indication was familial hyperlipidemia, and it was shown that they were efficacious and safe in this population [84]. In contrast to adults with CKD, there have been nearly no systematic studies on drug-induced lowering of serum lipids in children with CKD. A randomized, double-blind, placebo-controlled, cross-over clinical trial in children with hyperlipidemia secondary to kidney disorders showed that total cholesterol levels were significantly reduced by 23 %, LDL cholesterol levels by 34 %, and triglyceride levels by 21 % during the 3-month simvastatin treatment period. No differences were found across groups with respect to adverse events [85]. In another study, atorvastatin led to a decrease in total cholesterol and LDL levels in a small number of children with CKD stage 3–4 [86]. Thus, data on benefits of statin therapy in children with CKD are limited. Concerning the differences between the etiology of CKD in adults and children, adult data could not be directly interpreted in children [87]. Studies are needed to evaluate the benefits and adverse effects of statin and other treatment modalities in children with CKD.
Dyslipidemias in Patients with Renal Transplantation
Introduction
Together with improvements in the surgical techniques and immunosuppressive therapy, the success of pediatric renal transplantation increases and patient and organ survival get better. However, with the increase of long-term survivors, chronic complications are becoming more frequent. The expected lifespan is shortened compared with the age-matched population, mostly as a result of accelerated cardiovascular disease. The cardiovascular morbidity and mortality in renal transplant recipients are much lower than in dialysis patients, but still remain high. Heart disease is the second most common cause of death in children after infection, and is the leading cause of death in young adults who have undergone renal transplantation [68, 88, 89]. Post-transplant hyperlipidemia affects the majority of solid organ transplant recipients. Changes in serum lipid profiles reported after transplantation include an increase in total cholesterol, triglyceride, LDL cholesterol, and VLDL cholesterol and a variable effect on HDL cholesterol [90]. As a consequence, interest in monitoring and attempting to prevent and treat hyperlipidemia in the post-transplant period has increased dramatically.
Epidemiology
In the early reports, the incidence of hyperlipidemia in pediatric renal transplant recipients is reported to be 50 % on average, and as high as 66 %; increasing levels of cholesterol and triglyceride are also associated with higher corticosteroid dosages [91–95]. Alterations in lipid metabolism already exist prior to transplantation in patients with chronic renal failure. The pattern of hyperlipidemia is known to be different in uremic children according to the mode of renal replacement therapy before transplantation, and after transplantation the pattern of hyperlipidemia rapidly changes during the first few months. Muller et al. [48] showed that after transplantation, serum cholesterol tended to increase in HD and CRI patients, but to decrease in the PD group; similarly, triglyceride levels decrease in the PD and CRI patients and increase in the HD patients. Therefore, at 9 months post-transplant, the serum lipid levels in all children, with different pretransplant treatment modalities, were indiscernible and no longer influenced by prior renal replacement therapy. Thus, serum lipids converge to a common pattern of “post-transplant hyperlipidemia” in pediatric renal graft recipients.
The prevalence of dyslipidemia in the post-transplant period is thought to decrease over time and may reflect changes in immunosuppression. Sgambat et al. [96] evaluated the dyslipidemia profile of 38 pediatric patients who were at least 6 months post-transplant and receiving a lower dose of corticosteroids (0.1 mg/kg/day), tacrolimus, and mycophenolate mofetil. They found that 26 % had high total cholesterol, 24 % had high LDL cholesterol, 29 % had low HDL cholesterol, and 10 % had elevated triglyceride, although lower than the previous reports indicating the high prevalence of dyslipidemia even after immunosuppressive regimen change.
Oberholzer et al. [97] reported significantly less hyperlipidemia among children treated with an early steroid withdrawal protocol compared with those who continued on steroids after transplantation. Sarwal et al. [98] also reported no hyperlipidemia in ten pediatric recipients at 6 months post-transplant that were treated with complete steroid avoidance protocol. All children were treated with tacrolimus in both studies. On the other hand, steroid-minimization protocols were also associated with lower levels of HDL cholesterol.
Causes and Pathogenesis
There are many causes for the development of post-transplant dyslipidemia. Risk factors for the development of hyperlipidemia include degree of renal impairment, pretransplant hyperlipidemia, nephrotic syndrome that can occur after transplantation, use of antihypertensive agents such as thiazide diuretics and B-adrenergic blockers, genetic predisposition, lifestyle factors such as obesity, high-fat diet, and immunosuppressive agents [99, 100]. However, Siirtola et al. [101] recently showed that high serum cholesterol and triglyceride concentrations observed in renal transplant recipients were not explained by their diets, since comparable dietary intakes of total, saturated, and polyunsaturated fats and cholesterol were seen in their patients and controls.
The type of post-transplant treatment immunosuppressive regimen is one of the most important contributors to dyslipidemia prevalence. Of the immunosuppressive drugs, especially prednisone, cylosporin A (CSA) and sirolimus are more likely to be associated with dyslipidemia; however, tacrolimus and mycophenolate mofetil appear to have minimal to no dyslipidemic effects [102–104].
Corticosteroids, until recently, were used almost universally in the post-transplant period. A variety of mechanisms have been postulated for steroid-induced dyslipidemia. These include the induction of a hyperinsulinemic state that would increase the hepatic synthesis of TRL, inhibit the LDL receptor activity, reduce the activity of lipoprotein lipase and hepatic lipase, and an increase in the rate-limiting enzymes involved in lipogenesis (acetyl-CoA carboxylase and free fatty acid synthetase) [100]. On the other hand, corticosteroid therapy may raise the HDL level by increasing the apolipoprotein A-1 synthase and by decreasing the activity of CETP [105].
Possible mechanisms for CSA-induced hypercholesterolemia include impaired LDL clearance associated with interference at the LDL receptor, CSA-mediated impairment of steroid clearance and CSA-induced hepatic dysfunction. CSA also reduces bile acid synthesis by inhibiting hepatic 27-hydroxylation of cholesterol which is a potent suppresser of HMG-CoA reductase [106–109]. CSA is known to increase the rate of atherogenesis [110, 111]. The reasons for decreased incidence of hyperlipidemia observed on tacrolimus therapy when compared with CSA are not well understood. With the modern immunosuppression therapies, the incidence of acute rejection episodes decreases, together with the need for aggressive steroid therapy for the treatment of rejection.
Sirolimus increases serum triglycerides, LDL cholesterol, and HDL cholesterol levels in a dose-dependent manner. This defect in lipid metabolism is characterized by either a decrease in the catabolism of apoB100-containing lipoproteins or an increase in circulating free fatty acids leading to increased hepatic synthesis of triglycerides [112–114]. In pediatric renal transplant recipients, hyperlipidemia has been reported in a range of 10–61 % [104, 115–117]. Antiatherogenic effects of sirolimus via inhibiting vascular smooth muscle cell proliferation may balance the risk of hyperlipidemia [112].
Clinical Implications
Cardiovascular disease is one of the leading causes of death in pediatric kidney transplant recipients and accounts for over 15 % of all deaths [118]. Post-transplant CV disease has a multifactorial origin and is related to a combination of adverse factors that are prevalent in the post-transplant period to varying degrees. Silverstein et al. [119] assessed 45 children who received kidney transplants, all with stages 2–4 CKD at the time of study; two-thirds of patients had at least two risk factors for CVD, and one-third had at least three risk factors. A multicenter study of more than 200 kidney transplant recipients (aged 1–21 years) showed that 37 % met at least three (of a possible five) of the diagnostic criteria for metabolic syndrome at 1 year post-transplantation [120].
Dyslipidemia has been identified as a major contributor to CV mortality within this population. Very little direct data exist on the long-term clinical significance of lipid levels in children. Autopsy studies, such as the Pathobiological Determinants of Atherosclerosis in Youth (PDAY) study [121] and the Bogalusa Heart Study [122, 123], have demonstrated that the atherosclerotic process begins in childhood. PDAY study found that the development of fatty streaks (which are precursors of atherosclerotic plaques) in the coronary arteries and aorta was positively correlated with the elevated LDL cholesterol and low HDL cholesterol levels in young adults. In children, the extent of atherosclerotic lesions correlated significantly with serum total cholesterol, LDL cholesterol, and triglyceride concentrations. The Bogalusa Heart Study investigators followed a cohort of children who had their risk-factor status measured during assessments at school. As this population became older, some people died of accidental causes. The investigators obtained autopsies on these people in order to evaluate the presence and extent of atherosclerotic lesions. They reported that the extent of the arterial intimal surface covered with fatty streaks and fibrous plaques increased with age and the prevalence was almost 70 % in young adulthood. They also found that the extent to which the intimal surface was covered with atherosclerotic lesions was significantly associated with elevation of total cholesterol, LDL, and triglycerides concentrations, as well as a lower concentration of HDL. Another important discovery was that increased coverage of atherosclerotic lesions was positively correlated with the number of risk factors for CV disease present, such as dyslipidemia, obesity, and hypertension.
Dyslipidemia after transplantation has been associated with allograft injury, and therefore may contribute to the progression of chronic allograft nephropathy and subsequent graft loss [124, 125]. The prominence of the vascular lesions and certain similarities with the pathological features of atherosclerosis suggest that lipids may be involved in the pathogenesis of chronic rejection. In the series of Massy et al. [125], 706 consecutive renal transplants with long-term follow-up were included, increased post-transplant serum triglycerides, but not total cholesterol, were strong predictors of graft loss due to chronic rejection. This effect was independent of other risk factors for chronic rejection such as age, acute rejections, proteinuria, and hypoalbuminemia. Data in the pediatric population are also limited in this topic. Valavi et al. [126] performed a cross-sectional study in 62 renal transplant recipients, aged 5–18 years, with the mean follow-up time of 48 months and found that hypercholesterolemia and high LDL cholesterol levels have significant association with chronic allograft nephropathy.
Treatment
Adherence to standard practices of post-transplant care to ensure preservation of good renal function and education of patients regarding the benefits of maintaining a healthy lifestyle are extremely important. The first therapeutic step to be taken in all pediatric patients with post-transplant hyperlipidemia is dietary modification. Despite the perception that dietary modification is not achievable for the majority of pediatric patients, it should be tried. In a study of Obarzanek et al. [127], 663 children, 8–10 years of age, with elevated LDL cholesterol without renal disease were randomized to a dietary intervention or usual care group, with a mean of 7.4 years follow-up, and it was shown that the intervention compared with the usual care group had lower LDL cholesterol. On the other hand, Delucchi et al. [128] offered the Step II American Heart Association diet (containing low fat and low saturated cholesterol content) to 22 children with hyperlipidemia after renal transplantation; only about half of the eligible children agreed to participate in the study. Moreover, none of the patients demonstrated 100 % compliance with the diet. No patient lost weight, nor was the mean body mass index affected, and while the total cholesterol and LDL cholesterol did decrease, the magnitude of the decline was small (11 % and 14 %, respectively, at 12 weeks). Recently, Filler et al. [129] showed that supplementation of omega-3 fatty acids may be effective in reducing total cholesterol in pediatric renal transplant recipients. Children with adequate graft function who have no other disabilities should be able to assume a normal exercise regimen.
Avoidance of medications implicated in causing lipid abnormalities, including substitution of tacrolimus for cyclosporine in the medication regimen, can be an alternative treatment option. Filler et al. [130] performed a multicenter, 6-month, randomized, prospective, open, parallel group study with an open extension phase in 18 centers from nine European countries. In total, 196 pediatric patients were randomly assigned to receive either tacrolimus or CSA administered concomitantly with azathioprine and corticosteroids. Tacrolimus was significantly more effective than CSA in preventing acute rejection in pediatric renal recipients. Renal function and graft survival were also superior with tacrolimus. Cholesterol remained significantly higher in the CSA group throughout follow-up. Another approach may be the use of calcineurin inhibitor (CNI) avoidance or withdrawal protocols. Most, if not all, of these CNI-free regimens are steroid-based and many have also employed the use of sirolimus as a substitute to the CNIs, which makes them more risky for the development of hyperlipidemia. However, by improving long-term graft function, a CNI-free regimen could reduce dyslipidemia.
Steroid withdrawal and minimization protocols seemed to be associated with a reduction in lipid abnormalities. Lau et al. [131] compared 16 children that were receiving maintenance steroids with 13 children on a steroid-minimization regimen, who were also receiving preemptive pravastatin treatment. At 1 month, children receiving maintenance steroids had higher cholesterol compared with the steroid minimization group. Statistically significant differences in total cholesterol were not seen at other time points. Similar findings were noted for the LDL cholesterol, LDL/HDL, and cholesterol/HDL ratios. At 1 month, the serum HDL cholesterol was substantially lower in the steroid-minimization group.
The National Kidney Foundation K/DOQI Working Group created guidelines for the management of dyslipidemia in kidney transplant recipients in 2004 [132]. The working group considered that adolescents be included in the guidelines and that children before the onset of puberty be managed according to existing national guidelines for children in the general population. The K/DOQI guidelines recommend that a fasting lipid profile (total cholesterol, LDL, HDL, triglycerides) be measured during the first 6 months post-transplant, at 1 year after transplant, and annually thereafter. A lipid profile should also be measured 2–3 months after stopping or starting an immunosuppressive medication known to affect lipid levels. Kidney transplant recipients with dyslipidemias should be evaluated for remediable, secondary causes. For adolescent kidney transplant recipients with fasting triglycerides ≥500 mg/dL that cannot be corrected by removing an underlying cause, treatment with TLC should be considered. For adolescent kidney transplant recipients with LDL ≥130 mg/dL, treatment should be considered to reduce LDL to <130 mg/dL. Secondary causes of dyslipidemias should be treated first. Thereafter, for LDL 130–159 mg/dL, TLC should be used first. If, after 6 months of TLC, LDL is ≥130 mg/dL, then consider pharmacological management. If LDL is ≥160 mg/dL, then consider starting atrovastatin at the same time as TLC. For adolescent kidney transplant recipients with LDL < 130 mg/dL, fasting triglycerides ≥200 mg/dL, and non-HDL cholesterol (total cholesterol minus HDL) ≥160 mg/dL, treatment should be considered to reduce non-HDL cholesterol to <160 mg/dL. Therefore, statins should be considered for therapy in adolescent kidney transplant recipients and elevated LDL, or in hypertriglyceridemic adolescent kidney transplant recipients and increased non-HDL cholesterol. For adolescents who do not achieve the desired target with a statin, addition of a bile acid sequestrant can be considered. For prepubertal children, the existing guidelines are already described in the CKD section [11, 83].
Statins is an option in patients who remain persistently dyslipidemic in spite of TLC and modification of their immunosuppressive regimen. There are only a limited number of studies describing the use of lipid-lowering agents in pediatric renal transplant patients. Penson et al. [133] showed for the first time that pravastatin therapy is effective and safe when used in 21 pediatric and adolescent cardiac transplant recipients. Patients receiving pravastatin experienced a mean 32 mg/dL decrease in total cholesterol and a mean 31 mg/dL decrease in LDL cholesterol, regardless of their immunosuppressive regimen. Krmar et al. [134] used low-dose atorvastatin in eight children and young adult renal transplant recipients who had inadequately controlled hypercholesterolemia; at the end of the study, the total serum cholesterol was lowered by 32 % and the LDL cholesterol by about 42 %. Argent et al. [135], in a prospective study, showed that atorvastatin safely reduced total cholesterol, LDL cholesterol, and serum triglyceride by approximately 40 %, 60 %, and 45 %, respectively, in nine children with renal transplants who had persistent hyperlipidemia. Butani et al. [136] demonstrated that the preemptive use of pravastatin in seven pediatric renal transplant recipients appears to be effective in significantly reducing serum cholesterol. At 1 month only 43 % of the pravastatin group had hypercholesterolemia compared with 67 % of the controls; by 12 months this difference was even more significant (0 % in the pravastatin group vs. 45 % in the control group). The same group further evaluated the efficacy of the preemptive use of pravastatin in the post-transplant period in 17 children who were receiving maintenance steroids, and demonstrated it to effectively reduce total cholesterol, triglyceride, and LDL cholesterol after transplantation. The general linear model analysis showed that with time, there was a significant decline in the total cholesterol, serum triglyceride, LDL, and also HDL cholesterol. Compared with the controls, the mean serum cholesterol was lower at all time points post-transplant in the treated patients. However, despite treatment, the prevalence of hypercholesterolemia increased from 31 % pretransplant to 53 % at 1 month, but declined thereafter to 6 % at 3 and 6 months and 0 % at 1 year. Multivariable regression analyses showed the prednisone dose, pre-transplant cholesterol, and age to be the most important risk factors for the development of dyslipidemia. This group remarkably has been using a fixed dose of pravastatin preemptively in pediatric renal allograft recipients since 1999 [137]. Sgambat et al. [96] also showed a significant reduction in total cholesterol, LDL, VLDL, and triglyceride levels after 3–6 months of atrovastatin treatment compared with pretreatment value in five children. No difference in HDL was observed. There are various potential side effects associated with statins such as myopathy, rhabdomyolysis, and elevation of liver enzymes. In addition, there appears to be interaction between statins and cyclosporine, based upon their similar metabolism via the P450 cytochrome pathway [100]. Thus, drug levels should be monitored carefully.
It is not possible to make evidence-based recommendations for treatment of hyperlipidemia in pediatric renal transplant patients. The prevalence of dyslipidemia in the post-transplant period seems to decrease over time, together with the improvements in the immunosuppression regimen. Pharmacological therapy with statins in children with renal transplantation must be done carefully until controlled studies are conducted in this population.
References
Nephrotic syndrome in children: prediction of histopathology from clinical and laboratory characteristics at time of diagnosis. A report of the International Study of Kidney Disease in Children. Kidney Int. 1978;13:159–65.
McKinney PA, Feltbower RG, Brocklebank JT, Fitzpatrick MM. Time trends and ethnic patterns of childhood nephrotic syndrome in Yorkshire, UK. Pediatr Nephrol. 2001;16:1040–4.
White RH, Glasgow EF, Mills RJ. Clinicopathological study of nephrotic syndrome in childhood. Lancet. 1970;1:1353–9.
Niaudet P. Steroid resistant idiopathic nephrotic syndrome in children. In: Avner ED, Harmon WE, Niaudet P, editors. Pediatric nephrology. Philadelphia, PA: Lippincott Williams & Wilkins; 2004. p. 557–73.
Gbadegesin R, Smoyer WE. Nephrotic syndrome. In: Geary DF, Schaefer F, editors. Comprehensive pediatric nephrology. 1st ed. Philadelphia, PA: Mosby, Elsevier; 2008. p. 204–18.
Querfeld U. Should hyperlipidemia in children with the nephrotic syndrome be treated? Pediatr Nephrol. 1999;13:77–84.
Querfeld U, Lang M, Friedrich JB, Kohl B, Fiehn W, Schörer K. Lipoprotein(a) serum levels and apolipoprotein(a) phenotypes in children with chronic renal disease. Pediatr Res. 1993;34:772–6.
American Academy of Pediatrics. National Cholesterol Education Program: report of the expert panel on blood cholesterol levels in children and adolescents. Pediatrics. 1992;89: 525–84.
Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107(11):1562–6; copublished in J Pediatr. 2003;142:368–72.
Tamir I, Heiss G, Glueck CJ, Christensen B, Kwiterovich P, Rifkind B. Lipid and lipoprotein distributions in white children ages 6–19 yrs: the lipid research clinics program prevalence study. J Chronic Dis. 1981;34:27–39.
Daniels SR, Greer FR. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208.
Baxter JH, Goodman HC, Havel RJ. Serum lipid and lipoprotein alterations in nephrosis. J Clin Invest. 1960;39:455–65.
Valentini RP, Smoyer WE. Nephrotic syndrome. In: Kher KK, Schnaper HW, Makker SP, editors. Clinical pediatric nephrology. 2nd ed. London: Informa; 2007. p. 155–94.
Tsukahara H, Haruki S, Hiraoka M, Hori C, Sudo M. Persistent hypercholesterolaemia in frequently relapsing steroid-responsive nephrotic syndrome. J Paediatr Child Health. 1997;33:253–5.
Merouani A, Levy E, Mongeau JG, Robitaille P, Lambert M, Delvin EE. Hyperlipidemic profiles during remission in childhood idiopathic nephrotic syndrome. Clin Biochem. 2003;36:571–4.
Berlyne G, Mallick N. Ischemic heart disease as a complication of nephrotic syndrome. Lancet. 1969;II:339–40.
Hopp L, Gilboa N, Kurland G, Weichler N, Orchard TJ. Acute myocardial infarction in a young boy with nephrotic syndrome: a case report and review of the literature. Pediatr Nephrol. 1994;8:290–4.
Kallen RJ, Brynes RK, Aronson AJ, Lichtig C, Spargo BH. Premature coronary atherosclerosis in a 5-year-old with corticosteroid-refractory nephrotic syndrome. Am J Dis Child. 1977;131:976–80.
Silva JM, Oliveira EA, Marino VSP, Oliveira JS, Torres RM, Ribeiro AL, et al. Premature acute myocardial infarction in a child with nephrotic syndrome. Pediatr Nephrol. 2002;17:169–72.
Antikainen M, Sariola H, Rapola J, Taskinen MR, Holthöfer H, Holmberg C. Pathology of renal arteries of dyslipidemic children with congenital nephrosis. APMIS. 1994;102:129–34.
Portman R, Hawkins E, Verani R. Premature atherosclerosis in pediatric renal patients: report of the Southwest Pediatric Nephrology Study Group. Pediatr Res. 1991;29:2075A (Abstract).
Lechner BL, Bockenhauer D, Iragorri S, Kennedy TL, Siegel NJ. The risk of cardiovascular disease in adults who have had childhood nephrotic syndrome. Pediatr Nephrol. 2004;19:744–8.
Moorhead JF, El-Nahas M, Chan MK, Varghese Z. Lipid nephrotoxicity in chronic progressive glomerular and tubulointerstitial disease. Lancet. 1982;II:1309–12.
Diamond J. Hyperlipidemia of nephrosis: pathophysiologic role in progressive glomerular disease. Am J Med. 1989;87:25–9.
Keane WF, Mulcahy WS, Kasiske BL, Kim Y, O’Donnell MP. Hyperlipidemia and progressive renal disease. Kidney Int. 1991;39:41–8.
Keane WF, Kasiske BL, O’Donnell P, Kim Y. The role of altered lipid metabolism in the progression of renal disease: experimental evidence. Am J Kidney Dis. 1991;17:38–42.
O’Donnell MP, Kasiske BL, Kim Y, Schmitz PG, Keane WF. Lovastatin retards the progression of established glomerular disease in obese Zucker rats. Am J Kidney Dis. 1993;22:83–9.
Muntner P, Coresh J, Smith JC, Eckfeldt J, Klag MJ. Plasma lipids and risk of developing renal dysfunction: the atherosclerosis risk in communities study. Kidney Int. 2000;58:293–301.
Cerkauskiene R, Kaminskas A, Kaltenis P, Vitkus D. Influence of omega-3 fatty acids on lipid metabolism in children with steroid sensitive nephrotic syndrome. Medicina (Kaunas). 2003;39:82–7.
Kwiterovich PO. Clinical and laboratory assessment of cardiovascular risk in children: guidelines for screening, evaluation, and treatment. J Clin Lipidol. 2008;2:248–66.
Büyükçelik M, Anarat A, Bayazıt AK, Noyan A, Ozel A, Anarat R, et al. The effect of gemfibrozil on hyperlipidemia in children with persistent nephrotic syndrome. Turk J Pediatr. 2002;44:40–4.
Yamashita S, Matsuzawa Y. Where are we with probucol: a new life for an old drug? Atherosclerosis. 2009;207:16–23.
Querfeld U, Kohl B, Fiehn W, Minor T, Michalk D, Schörer K, et al. Probucol for treatment of hyperlipidemia in persistent childhood nephrotic syndrome. Pediatr Nephrol. 1999;13:7–12.
Coleman JE, Watson AR. Hyperlipidemia, diet and simvastatin therapy in steroid resistant nephrotic syndrome of childhood. Pediatr Nephrol. 1996;10:171–4.
Sanjad SA, Al-Abbad A, Al-Shorafa S. Management of hyperlipidemia in children with refractory nephrotic syndrome: the effect of statin therapy. J Pediatr. 1997;130:470–4.
Muso E, Mune M, Fujii Y, Imai E, Ueda N, Hatta K, et al. Low density lipoprotein apheresis therapy for steroid-resistant nephrotic syndrome. Kansai-FGS-Apheresis Treatment (K-FLAT) Study Group. Kidney Int. 1999;71(Suppl):122–5.
Hattori M, Chikamoto H, Akioka Y, Nakakura H, Ogino D, Matsunaga A, et al. A combined low-density lipoprotein apheresis and prednisone therapy for steroid-resistant primary focal segmental glomerulosclerosis in children. Am J Kidney Dis. 2003;42:1121–30.
Saland JM, Ginsberg H, Fisher EA. Dyslipidemia in pediatric renal disease: epidemiology, pathophysiology, and management. Curr Opin Pediatr. 2002;14:197–204.
Papadopoulou ZL, Sandler P, Tina LU, Jose PA, Calcagno PL. Hyperlipidemia in children with chronic renal insufficiency. Pediatr Res. 1981;15:887–91.
Zacchello G, Pagnan A, Sidran MP, Ziron L, Braggion M, Pavanello L, et al. Further definition of lipid-lipoprotein abnormalities in children with various degrees of chronic renal insufficiency. Pediatr Res. 1987;21:462–5.
Saland JM, Pierce CB, Mitsnefes MM, Flynn JT, Goebel J, Kupferman JC, et al. Dyslipidemia in children with chronic kidney disease: a report of the chronic kidney disease in children (CKiD) study. Kidney Int. 2010;78:1154–63.
Pennisi AJ, Heuser ET, Mickey MR, Lipsey A, Malekzadeh M, Fine RN. Hyperlipidemia in pediatric haemodialysis and renal transplant patients. Am J Dis Child. 1976;130:957–61.
El Bishti M, Counahan R, Jarrett RJ, Stimmler L, Wass V, Chantler C. Hyperlipidaemia in children on regular haemodialysis. Arch Dis Child. 1977;52:932–6.
Querfeld U, Salusky IB, Nelson P, Foley J, Fine RN. Hyperlipidemia in pediatric patients undergoing peritoneal dialysis. Pediatr Nephrol. 1988;2:447–52.
Querfeld U, LeBoeuf RC, Salusky IB, Nelson P, Laidlaw S, Fine RN. Lipoproteins in children treated with continuous peritoneal dialysis. Pediatr Res. 1991;29:155–9.
Scolnik D, Balfe JW. Initial hypoalbuminemia and hyperlipidemia persist during chronic peritoneal dialysis in children. Perit Dial Int. 1993;13:136–9.
Kosan C, Sever L, Arisoy N, Caliskan S, Kasapcopur O. Carnitine supplementation improves apolipoprotein B levels in pediatric peritoneal dialysis patients. Pediatr Nephrol. 2003;18: 1184–8.
Muller T, Koeppe S, Arbeiter K, Luckner D, Salzer U, Balzar E, et al. Serum lipid pattern unifies following renal transplantation in children. Pediatr Nephrol. 2003;18:939–42.
Saland JM, Ginsberg HN. Lipoprotein metabolism in chronic renal insufficiency. Pediatr Nephrol. 2007;22:1095–112.
Moberly JB, Attman PO, Samuelsson O, Johansson AC, Knight-Gibson C, Alaupovic P. Apolipoprotein C-III, hypertriglyceridemia and triglyceride-rich lipoproteins in uremia. Miner Electrolyte Metab. 1999;25:258–62.
Monzani G, Bergesio F, Ciuti R, Rosati A, Frizzi V, Serruto A, et al. Lipoprotein abnormalities in chronic renal failure and dialysis patients. Blood Purif. 1996;14:262–72.
Hager SR. Insulin resistance of uremia. Am J Kidney Dis. 1989;14:272–6.
Howard BV. Insulin resistance and lipid metabolism. Am J Cardiol. 1999;84:28–32.
Lithell H, Boberg J, Hellsing K, Lundqvist G, Vessby B. Lipoprotein-lipase activity in human skeletal muscle and adipose tissue in the fasting and the fed states. Atherosclerosis. 1978;30:89–94.
Farese Jr RV, Yost TJ, Eckel RH. Tissue-specific regulation of lipoprotein lipase activity by insulin/glucose in normal-weight humans. Metabolism. 1991;40:214–6.
Mak RH. Insulin secretion and growth failure in uremia. Pediatr Res. 1995;38:379–83.
Alvestrand A, Mujagic M, Wajngot A, Efendic S. Glucose intolerance in uremic patients: the relative contributions of impaired beta-cell function and insulin resistance. Clin Nephrol. 1989;31:175–83.
Kimak E, Ksiazek A, Solski J. Disturbed lipoprotein composition in non-dialyzed, hemodialysis, continuous ambulatory peritoneal dialysis and post-transplant patients with chronic renal failure. Clin Chem Lab Med. 2006;44:64–9.
Grutzmacher P, Marz W, Peschke B, Gross W, Schoeppe W. Lipoproteins and apolipoproteins during the progression of chronic renal disease. Nephron. 1988;50:103–11.
Horkko S, Huttunen K, Laara E, Kervinen K, Kesaniemi YA. Effects of three treatment modes on plasma lipids and lipoproteins in uraemic patients. Ann Med. 1994;26:271–82.
Horowitz BS, Goldberg IJ, Merab J, Vanni TM, Ramakrishnan R, Ginsberg HN. Increased plasma and renal clearance of an exchangeable pool of apolipoprotein A-I in subjects with low levels of high density lipoprotein cholesterol. J Clin Invest. 1993;91:1743–52.
Bergesio F, Monzani G, Ciuti R, Serruto A, Benucci A, Frizzi V, Salvadori M. Lipids and apolipoproteins change during the progression of chronic renal failure. Clin Nephrol. 1992;38:264–70.
Kasiske BL. Hyperlipidemia in patients with chronic renal disease. Am J Kidney Dis. 1998;32:142–56.
Berneis KK, Krauss RM. Metabolic origins and clinical significance of LDL heterogeneity. J Lipid Res. 2002;43:1363–79.
Massy ZA, Nguyen-Khoa T. Oxidative stress and chronic renal failure: markers and management. J Nephrol. 2002;15:336–41.
Oberg BP, McMenamin E, Lucas FL, McMonagle E, Morrow J, Ikizler TA, et al. Increased prevalence of oxidant stress and inflammation in patients with moderate to severe chronic kidney disease. Kidney Int. 2004;65:1009–16.
Querfeld U. Cardiovascular considerations of pediatric ESRD. In: Warady BA, Schaefer FS, Fine RN, Alexander SR, editors. Pediatric dialysis. Dordrecht: Kluwer Academic; 2004. p. 353–67.
Parekh RS, Carrol CE, Wolfe RA, Port FK. Cardiovascular mortality in children and young adults with end-stage kidney disease. J Pediatr. 2002;141:191–7.
National Kidney Foundation Task Force on Cardiovascular Disease. Controlling the epidemic of cardiovascular disease in chronic renal disease: what do we know? What do we need to know? Special report from the National Kidney Foundation task force on cardiovascular disease. Am J Kidney Dis. 1998;32:1–121.
U.S. Renal Data System: USRDS Annual Report. Bethesda: The National Institute of Diabetes and Digestive and Kidney Diseases. 2003. http://www.usrds.org
Mitsnefes MM. Cardiovascular complications of pediatric chronic kidney disease. Pediatr Nephrol. 2008;23:27–39.
Wilson AC, Mitsnefes MM. Cardiovascular disease in CKD in children: update on risk factors, risk assessment, and management. Am J Kidney Dis. 2009;54:345–60.
Kavey RE, Allada V, Daniels SR, Hayman LL, McCrindle BW, Newburger JW, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association expert panel on population and prevention science: the councils on cardiovascular disease in the young, epidemiology and prevention, nutrition, physical activity and metabolism, high blood pressure research, cardiovascular nursing, and the kidney in heart disease; and the Interdisciplinary Working Group on quality of care and outcomes research: endorsed by the American Academy of Pediatrics. Circulation. 2006;114: 2710–38.
National Kidney Foundation: K/DOQI. Clinical practice guidelines for managing dyslipidemias in chronic kidney disease. Am J Kidney Dis. 2003;41 Suppl 3:61–70.
Secker D, Mak R. Nutritional challenges in pediatric chronic kidney disease. In: Geary DF, Schaefer F, editors. Comprehensive pediatric nephrology. 1st ed. Philadelphia, PA: Mosby, Elsevier; 2008. p. 743–59.
Kari JA, Shaw V, Vallance DT, Rees L. Effect of enteral feeding on lipid subfractions in children with chronic kidney failure. Pediatr Nephrol. 1998;12:401–4.
Mak RH. Metabolic effects of erythropoietin in patients on peritoneal dialysis. Pediatr Nephrol. 1998;12:660–5.
Mak RH. 1,25-Dihydroxyvitamin D3 corrects insulin and lipid abnormalities in uremia. Kidney Int. 1998;53:1353–7.
Mak RH. Effect of metabolic acidosis on hyperlipidemia in uremia. Pediatr Nephrol. 1999;13:891–3.
Goren A, Stankiewicz H, Goldstein R, Drukker A. Fish oil treatment of hyperlipidemia in children and adolescents receiving renal replacement therapy. Pediatrics. 1991;88:265–8.
Pieper AK, Haffner D, Hoppe B, Dittrich K, Offner G, Bonzel KE, et al. A randomized crossover trial comparing sevelamer with calcium acetate in children with CKD. Am J Kidney Dis. 2006;47:625–35.
Gulati A, Sridhar V, Bose T, Hari P, Bagga A. Short-term efficacy of sevelamer versus calcium acetate in patients with chronic kidney disease stage 3–4. Int Urol Nephrol. 2010;42:1055–62.
National Cholesterol Education Program. Report of the expert panel on blood cholesterol levels in children and adolescants. Pediatrics. 1992;89:495–584.
Avis HJ, Vissers MN, Stein EA, Wijburg FA, Trip MD, Kastelein JJ, et al. A systematic review and meta-analysis of statin therapy in children with familial hypercholesterolemia. Arterioscler Thromb Vasc Biol. 2007;27:1803–10.
Garcia-de-la-Puenta S, Arredondo-Garcia JL, Gutierrez-Castrellon P, Bojorquez-Ochoa A, Maya ER, Perez-Martinez MDP. Efficacy of simvastatin in children with hyperlipidemia secondary to kidney disorders. Pediatr Nephrol. 2009;24:1205–10.
Mackie FE, Rosenberg AR, Harmer JA, Kainer G, Celermajer DS. HMG CoA reductase inhibition and endothelial function in children with chronic kidney disease (CKD)—a pilot study. Acta Paediatr. 2010;99:457–9.
Tullus K. Dyslipidemia in children with CKD: should we treat with statins. Pediatr Nephrol. 2012;27:357–62.
McDonald SP, Craig JC. Long-term survival of children with end-stage renal disease. N Engl J Med. 2004;350:2654–62.
United States Renal Data System. Experts from the USRDS 2001 annual report. Am J Kidney Dis. 2001;38 Suppl 3:147–58.
Kobashigawa JA, Kasiske BL. Hyperlipidemia in solid organ transplantation. Transplantation. 1997;63:331–8.
Pennisi AJ, Fiedler J, Lipsey A, Mickey R, Malekzadeh MH, Fine NR. Hyperlipidemia in pediatric renal allograft recipients. J Pediatr. 1975;87:249–51.
Saldanha LF, Hurst KS, Amend Jr WJ, Lazarus JM, Lowrie EG, Ingelfinger J, et al. Hyperlipidemia after renal transplantation in children. Am J Dis Child. 1976;130:951–3.
Goldstein S, Duhamel G, Laudat MH, Berthelier M, Hervy C, Tete MJ, et al. Plasma lipids, lipoproteins and apolipoproteins AI, AII, and B in renal transplanted children: what risk for accelerated atherosclerosis? Nephron. 1984;38:87–92.
Sharma AK, Myers TA, Hunninghake DB, Matas AJ, Kashtan CE. Hyperlipidemia in long-term survivors of pediatric renal transplantation. Clin Transplant. 1994;8:252–7.
Silverstein DM, Palmer J, Polinsky MS, Braas C, Conley SB, Baluarte HJ. Risk factors for hyperlipidemia in long-term pediatric renal transplant recipients. Pediatr Nephrol. 2000;14:105–10.
Sgambat K, He J, McCarter R, Moudgil A. Lipoprotein profile changes in children after renal transplantation in the modern immunosuppression era. Pediatr Transplant. 2008;12: 796–803.
Oberholzer J, John E, Lumpaopong A, Testa G, Sankary HN, Briars L, et al. Early discontinuation of steroids is safe and effective in pediatric kidney transplant recipients. Pediatr Transplant. 2005;9:456–63.
Sarwal MM, Yorgin PD, Alexander S, Millan MT, Belson A, Belanger N, et al. Promising early outcomes with a novel, complete steroid avoidance immunosuppression protocol in pediatric renal transplantation. Transplantation. 2001;72:13–21.
Massy ZA, Kasiske BL. Post-transplant hyperlipidemia: mechanisms and management. J Am Soc Nephrol. 1996;7:971–7.
Butani L. Dyslipidemia after renal transplantation: a cause for concern? Pediatr Transplant. 2008;12:724–8.
Siirtola A, Virtanen SM, Ala-Houhala M, Koivisto AM, Solakivi T, Lehtimäki T, et al. Diet does not explain the high prevalence of dyslipidaemia in paediatric renal transplant recipients. Pediatr Nephrol. 2008;23:297–305.
Perrea DN, Moulakakis KG, Poulakou MV, Vlachos IS, Nikiteas N, Kostakis A. Correlation between lipid abnormalities and immunosuppressive therapy in renal transplant recipients with stable renal function. Int Urol Nephrol. 2008;40:521–7.
Mathis AS, Dave N, Knipp GT, Friedman GS. Drug-related dyslipidemia after renal transplantation. Am J Health Syst Pharm. 2004;61:565–85.
Kasap B. Sirolimus in pediatric renal transplantation. Pediatr Transplant. 2011;15:673–85.
Moulin P, Appel GB, Ginsberg HN, Tall AR. Increased concentration of plasma cholesteryl ester transfer protein in nephrotic syndrome: role in dyslipidemia. J Lipid Res. 1992;33:1817–22.
Bittar AE, Ratcliffe PJ, Richardson AJ, Raine AE, Jones L, Yudkin PL, et al. The prevalence of hyperlipidemia in renal transplant recipients. Associations with immunosuppressive and antihypertensive therapy. Transplantation. 1990;50:987–92.
Ost L. Impairment of prednisolone metabolism by cyclosporine treatment in renal graft recipients. Transplantation. 1987;44:533–5.
Lopez-Miranda J, Vilella E, Perez-Jimenez F, Espino A, Jiménez-Perepérez JA, Masana L, et al. Low-density lipoprotein metabolism in rats treated with cyclosporine. Metabolism. 1993;42:678–83.
Gueguen Y, Ferrari L, Souidi M, Batt AM, Lutton C, Siest G, et al. Compared effect of immunosuppressive drugs cyclosporine A and rapamycin on cholesterol homeostasis key enzymes CYP27A1 and HMGCoA reductase. Basic Clin Pharmacol Toxicol. 2007;100:392–7.
Apanay DC, Neylan JF, Ragab MS, Sgoutas DS. Cyclosporine increases the oxidizability of low-density lipoproteins in renal transplant recipients. Transplantation. 1994;58:663–9.
Emeson EE, Shen ML. Accelerated atherosclerosis in hyperlipidemic C57BL/6 mice treated with cyclosporin A. Am J Pathol. 1993;142:1906–15.
Augustine JJ, Bodziak KA, Hricik DE. Use of sirolimus in solid organ transplantation. Drugs. 2007;67:369–91.
Hoogeveen RC, Ballantyne CM, Pownall HJ, Opekun AR, Hachey DL, Jaffe JS, et al. Effect of sirolimus on the metabolism of apoBl00-containing lipoproteins in renal transplant patients. Transplantation. 2001;72:1244–50.
Morrisett JD, Abdel-Fattah G, Hoogeveen R, Mitchell E, Ballantyne CM, Pownall HJ, et al. Effects of sirolimus on plasma lipids, lipoprotein levels, and fatty acid metabolism in renal transplant patients. J Lipid Res. 2002;43:1170–80.
Hymes LC, Warshaw BL. Sirolimus in pediatric patients: results in the first 6 months post-renal transplant. Pediatr Transplant. 2005;9:520–2.
Powell HR, Kara T, Jones CL. Early experience with conversion to sirolimus in a pediatric renal transplant population. Pediatr Nephrol. 2007;22:1773–7.
Hymes LC, Warshaw BL, Amaral SG, Greenbaum LA. Tacrolimus withdrawal and conversion to sirolimus at three months post-pediatric renal transplantation. Pediatr Transplant. 2008;12:773–7.
Smith JM, Stablein DM, Munoz R, Hebert D, McDonald RA. Contributions of the transplant registry: the 2006 annual report of the North American Pediatric Renal Trials and Collaborative Studies (NAPRTCS). Pediatr Transplant. 2007;11:366–73.
Silverstein DM, Mitchell M, LeBlanc P, Boudreaux JP. Assessment of risk factors for cardiovascular disease in pediatric renal transplant patients. Pediatr Transplant. 2007;11:721–9.
Wilson AC, Greenbaum LA, Barletta GM, Chand D, Lin JJ, Patel HP, et al. High prevalence of the metabolic syndrome and associated left ventricular hypertrophy in pediatric renal transplant recipients. Pediatr Transplant. 2010;14:52–60.
McGill Jr HC, McMahan CA. Determinants of atherosclerosis in the young. Pathobiological determinants of atherosclerosis in youth (PDAY) research group. Am J Cardiol. 1998;82:30–6.
Newman III WP, Freedman DS, Voors AW, Gard PD, Srinivasan SR, Cresanta JL, et al. Relation of serum lipoprotein levels and systolic blood pressure to early atherosclerosis: the Bogalusa Heart Study. N Engl J Med. 1986;314:138–44.
Berenson GS, Srinivasan SR, Bao W, Newman III WP, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and the early development of atherosclerosis. Bogalusa Heart Study. N Engl J Med. 1998;338:1650–6.
Guijarro C, Massy ZA, Kasiske BL. Clinical correlation between renal allograft failure and hyperlipidemia. Kidney Int Suppl. 1995;52:56–9.
Massy ZA, Guijarro C, Wiederkehr MR, Ma JZ, Kasiske BL. Chronic renal allograft rejection: immunologic and nonimmunologic risk factors. Kidney Int. 1996;49:518–24.
Valavi E, Otukesh H, Fereshtehnejad SM, Sharifian M. Clinical correlation between dyslipidemia and pediatric chronic allograft nephropathy. Pediatr Transplant. 2008;12:748–54.
Obarzanek E, Kimm SY, Barton BA, Van Horn LL, Kwiterovich Jr PO, Simons-Morton DG, et al. Long-term safety and efficacy of a cholesterol-lowering diet in children with elevated low-density lipoprotein cholesterol: seven-year results of the dietary intervention study in children (DISC). Pediatrics. 2001;107:256–64.
Delucchi A, Marin V, Trabucco G, Azocar P, Salas E, Gutierrez E, et al. Dyslipidemia and dietary modification in Chilean renal pediatric transplantation. Transplant Proc. 2001;33: 1297–301.
Filler G, Weiglein G, Gharib MT, Casier S. Ω3 fatty acids may reduce hyperlipidemia in pediatric renal transplant recipients. Pediatr Transplant. 2012;16:835–9.
Filler G, Webb NJ, Milford DV, Watson AR, Gellermann J, Tyden G, et al. Four-year data after pediatric renal transplantation: a randomized trial of tacrolimus vs. cyclosporin microemulsion. Pediatr Transplant. 2005;9:498–503.
Lau KK, Tancredi DJ, Perez RV, Butani L. Unusual pattern of dyslipidemia in children receiving steroid minimization immunosuppression after renal transplantation. Clin J Am Soc Nephrol. 2010;5:1506–12.
Kasiske B, Cosio FG, Beto J, Bolton K, Chavers BM, Grimm Jr R, et al. Clinical practice guidelines for managing dyslipidemias in kidney transplant patients: a report from the managing dyslipidemias in Chronic Kidney Disease Work Group of the National Kidney Foundation kidney disease outcomes quality initiative. Am J Transplant. 2004;4 Suppl 7:13–53.
Penson MG, Fricker FJ, Thompson JR, Harker K, Williams BJ, Kahler DA, et al. Safety and efficacy of pravastatin therapy for the prevention of hyperlipidemia in pediatric and adolescent cardiac transplant recipients. J Heart Lung Transplant. 2001;20:611–8.
Krmar RT, Ferraris JR, Ramirez JA, Sorroche P, Legal S, Cayssials A. Use of atorvastatin in hyperlipidemic hypertensive renal transplant recipients. Pediatr Nephrol. 2002;17:540–3.
Argent E, Kainer G, Aitken M, Rosenberg AR, Mackie FE. Atorvastatin treatment for hyperlipidemia in pediatric renal transplant recipients. Pediatr Transplant. 2003;7:38–42.
Butani L, Pai MV, Makker SP. Pilot study describing the use of pravastatin in pediatric renal transplant recipients. Pediatr Transplant. 2003;7:179–84.
Butani L. Prospective monitoring of lipid profiles in children receiving pravastatin preemptively after renal transplantation. Pediatr Transplant. 2005;9:746–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Özçakar, Z.B., Yalçınkaya, F. (2014). Dyslipidemias in the Pediatric Chronic Kidney Disease Patient. In: Covic, A., Kanbay, M., Lerma, E. (eds) Dyslipidemias in Kidney Disease. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0515-7_13
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0515-7_13
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0514-0
Online ISBN: 978-1-4939-0515-7
eBook Packages: MedicineMedicine (R0)