Abstract
Stroke remains a leading cause of human death and disability. There is a growing consensus that an effective stroke therapy needs to exert protective and/or regenerative actions on both gray and white matters. However, white matter injury after ischemic stroke has been less investigated and is inadequately understood. This review summarizes the current understanding of the pathophysiology and potential treatments for white matter injury, focusing on animal data and its potential application to human patients. It is expected that more investigations on white matter injury and more comprehensive therapeutic approaches will increase the chances of developing an effective clinical treatment for ischemic stroke.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
According to the latest census, stroke has now fallen to the fourth leading cause of human death in the USA, yet remains a leading cause of long-term disability (Towfighi and Saver 2011). Multiple factors have contributed to successfully saving lives affected by stroke; meanwhile, there is real and urgent need for effective stroke therapy to minimize and treat the damaging repercussions of brain injury.
Ischemic stroke, occurring when blood supply to a region of the brain is occluded by blood clot, constitutes more than 80 % of stroke cases. The recombinant tissue plasminogen activator (tPA) is effective in treating acute ischemic stroke through dissolving the clot formed in blood vessels. Because of the narrow administration window (3–4.5 h) for tPA and its side effects (Lansberg et al. 2009; Del Zoppo et al. 2009), most patients with ischemic stroke cannot receive tPA treatment. Aside from tPA, a variety of neuroprotectants have been found effective in protecting gray matter and preventing neuronal death in rodent stroke models. However, all these drugs have failed to demonstrate beneficial outcomes in human stroke treatment (Cheng et al. 2004; Jeyaseelan et al. 2008). Although many factors may affect drug efficacy, underestimation of white matter injury is likely one important reason for the translational failures.
In the rodent brain used for stroke models, white matter constitutes a small part (~14 %) of the brain. Human brain differs from rodent brain in the proportion of white and gray matters. A human brain has almost equal proportional volumes of white matter and gray matter (Goldberg and Ransom 2003), and it has become a common view that human brain white matter is highly vulnerable to ischemia (Sozmen et al. 2012). The white matter is composed of astrocytes, oligodendrocytes, and myelinated axons responsible for transmitting input (afferent) and output (efferent) signals between neurons and neural networks. Oligodendrocyte processes produce the myelin sheath, which wraps around axons. The main function of the myelin sheath is to support axons and increase signal transduction speed along axonal fibers. Oligodendrocytes and axons, which compose the functional unit of the myelinated fiber, are vulnerable to many pathological conditions such as periventricular leukomalacia, brain trauma, vascular dementia, and cerebral ischemia (Volpe 2001; Kim et al. 2005; Matute et al. 2001; Dewar et al. 2003; Zaidi et al. 2004; Brown et al. 2002). Damaged axonal fibers and disrupted neuronal circuits contribute to functional deficits in these cerebrovascular diseases. In the current stroke research field, the pathological changes of ischemic white matter have become increasingly emphasized and investigated in mouse, rat, nonhuman primates, and human patients. Here, we summarize the current consensus and add some recent knowledge obtained from experimental stroke models for assessing white matter damage.
2 Morphological Assessment of Ischemic White Matter Damage
In histological sections of brain tissues, axonal fiber and oligodendrocytes can be identified under light and electron microscopes based upon their characteristic morphology, distribution, and ultrastructure. The corpus callosum, for example, is the largest white matter structure in the brain and relatively easy to identify. In a common stroke model, induced by occluding the middle cerebral artery (MCA) supplying the cerebral cortex, the corpus callosum, subcortical area, and striatum are the most suitable regions for assessing initial or secondary white matter injury. In a cerebral ischemia model, swollen oligodendrocytes and astrocytes in subcortical areas can be identified in the ischemic core by electron microscope 30 min after MCA occlusion (Pantoni et al. 1996). Three hours after ischemia, axonal swelling appears, and oligodendrocytes undergo pyknosis; 12–24 h later, pyknotic oligodendrocytes begin to necrose. Demyelination of myelin sheaths around axonal fiber occurs 30 min after ischemia and becomes a feature of white matter injury 12–24 h later (Pantoni et al. 1996). Evidence from a sciatic nerve ischemic model also suggests that swelling is the earliest morphological change in white matter injury (Nukada and Dyck 1987).
To obtain more detailed assessments of ischemic white matter damage, researchers employ more specific indicators and methodologies to detect cellular elements of interest in axons and oligodendrocytes. Neuronal markers, neurofilament (NF) and class III β-Tubulin (Tuj1), are frequently used to show the changes of axonal fiber in stroke and other neurological diseases. Reduction or loss in NF and Tuj1 positive processes can be detected by immunohistochemical staining 12–24 h after ischemia (Akpan et al. 2011). There are three major subunits of NF, termed: NF 68 (68 kDa), NF 150 (NF 150 kDa), and NF 200 (200 kDa). NF 68 is the most abundant of the three components, and has shown a more pronounced decrease in density by immunohistochemistry 1–4 days after hippocampal ischemia in male Mongolian gerbils (Nakamura et al. 1992). Much earlier axonal damage can be detected by immunoblot analysis of brain sections to assess protein breakdown of neurofilament. It was reported that the proteolysis of NF 68 and NF 200 occurred 3 h after cerebral cortex ischemia in adult male rats (Aronowski et al. 1999). Earlier degradation of NF 150 and NF 200 at 15 min after cerebral ischemia was found in rats (Ogata et al. 1989). The three neurofilament components are all substrates of the calcium/calmodulin-dependent protease, calpain (Nixon and Lewis 1986; Zimmerman and Schlaepfer 1988). Thus, neurofilament protein degradation may be regarded as the consequence of calcium imbalance occurring soon after ischemic injury.
Compared with the above histopathologic staining, amyloid precursor protein (APP) is a more sensitive marker for assessment of ischemia-damaged axons. In healthy brain, APP is transported by fast axonal transport throughout axons and maintained at a low concentration that is hard to detect by immunohistochemistry. Once axons are damaged by ischemia, APP transportation slows, and accumulated APP becomes a useful injury reporter. Thus, APP staining has been used for quantitative assessment of axonal damage after cerebral ischemia and has shown advantages such as high sensitivity to ischemic insult and easy detection in assays (Imai et al. 2002).
For more specific identification of damage to oligodendrocytes, many markers have been developed, such as: myelin basic protein (MBP) for mature cells, lipid sulfatide (O4) for immature cells, and NG2 proteoglycan for precursor cells. Antiadenomatous polyposis coli (APC) and 2′, 3′-Cyclic-nucleotide 3′-phosphodiesterase (CNPase) are also used to label mature oligodendrocytes and detect damage. MBP protein is a major constituent of the myelin sheath, and myelin damage can be identified with antibody that recognizes degraded MBP (dMBP). In a rat focal cerebral ischemia model induced by endothelin-1 injection, the density of MBP progressively decreased in the ischemic core and penumbra region at 1, 3, and 7 days after stroke, while the density of dMBP progressively increased (Moxon-Emre and Schlichter 2010). Ischemia-damaged oligodendrocytes in the brain are also immunoreactive to the cytoskeletal protein, tau. The number of tau positive oligodendrocytes increased 6–8-folds at 40 min after the onset of cerebral ischemia (Irving et al. 1997).
Ischemia not only causes damage to oligodendrocytes but also induces oligodendrogenesis. This regenerative response from oligodendrocyte progenitor cells is usually assessed by BrdU incorporation with NG2 or O4 immuno-positive cell populations. The proliferation of NG2 oligodendrocyte progenitor cells takes place in a delayed fashion, showing increased maximal activity at 5–7 days after stroke induction, and then significant decline 14–28 days later (Iwai et al. 2010; Sozmen et al. 2009).
These morphological methods enable researchers to assess and quantify temporal and spatial changes in white matter after brain ischemia. Since white matter is vulnerable to ischemic damage, it is more and more recognized that the characteristic changes of white matter are of great importance when assessing extent of ischemic brain damage and evaluating therapeutic effect of treatment in animal and human stroke.
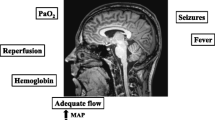
3 Ionic Mechanism of Ischemic Axonal Damage
A few minutes after occlusion of cerebral blood flow, ischemic brain tissue becomes deprived of oxygen and glucose, resulting in mitochondrial damage and failure of ATP synthesis. This energy depletion causes Na+/K+-ATPase dysfunction and cellular Na+ and K+ homeostasis disruption, leading to depolarization of the soma and axonal membrane. Membrane depolarization is one of the major early mechanisms contributing to excessive release of glutamate from neurons and glial cells, which over-activates glutamate receptors. This glutamate-mediated excitotoxicity causes rapid gray matter and white matter damage in acute ischemic stroke. Other mechanisms such as increased production of free radicals, inflammatory activity, apoptotic cascade activation and loss of trophic support have been implicated in ischemic injury. We here focus on the discussion of ionic mechanisms underlying ischemic white matter damage.
Myelinated axon fibers are sensitive to hypoxia and ischemia. The concentration gradient of Na+ and K+ and a resting membrane potential across the axonal membrane depend on a normal activity of Na+/K+-ATPase. Axoplasmic accumulation of Na+ is mediated by failure of Na+/K+-ATPase. A persistent Na+ influx and axonal swelling is a result of excessive Na+ and Cl- influx. Accumulation of cellular Na+ may lead to activation of the reverse model of the Na+/Ca2+ exchanger and axoplasmic Ca2+ increases (Philipson and Nicoll 2000). Membrane potential collapse will impair axonal conduction and suppress action potential propagation along the axonal fiber.
In a study of isolated rat optic nerve fibers (a white matter tract), energy deprivation depolarized neuronal resting membrane potential in a Na+ influx dependent manner (Leppanen and Stys 1997). The evoked compound action potential (CAP) in adult optic nerves can be abolished by deprivation of either oxygen or glucose for 60 min (Fern et al. 1998). In an ischemic brain slice model, the corpus callosum injury was induced by deprivation of oxygen and glucose (OGD), and the function of corpus callosum was monitored by recording CAP. Blockade of Na+ influx was found to partially protect corpus callosum function from OGD injury (Tekkok and Goldberg 2001). On the other hand, axoplasmic Ca2+ is also involved in damaged axonal function based on the observation that anoxia-induced suppression of CAP in rat optic nerve was restored close to control level by Ca2+-free solution (Stys et al. 1990). Ca2+-free solution preserved CAP in OGD-damaged corpus callosum and protected the axonal cytoskeleton against anoxia in optic nerve axons (Tekkok and Goldberg 2001; Waxman et al. 1993). These studies demonstrate that Na+ and Ca2+ influx plays important roles in ischemia-induced axonal damage.
Glutamate-mediated excitotoxicity not only affects gray matter but is also involved in ischemic axonal injury. In axonal damage, activation of AMPA/kainate receptors but not NMDA receptors mediates the excitotoxic effect (Matute 1998; Li and Stys 2000; Domercq et al. 2005). The AMPA receptor blocker, NBQX, is able to preserve axonal structure and functional activity in brain slices treated with OGD conditions, and this effect has been explained as a secondary effect resulting from protection of oligodendrocytes by NBQX (Tekkok and Goldberg 2001). Most recent studies have shown that rat dorsal column axons express glutamate receptor subunit 4 (GluR4) AMPA receptors, GluR5 and GluR6 containing kainate receptors. Application of AMPA/kainate receptor agonists induces progressive elevation of intra-axonal Ca2+ and impairs functional CAP in dorsal axons (Ouardouz et al. 2009a; Ouardouz et al. 2009b). These observations are consistent with the idea that glutamate excitotoxicity in axons is directly mediated by AMPA/kainate receptors. On the other hand, it has been suggested that the NMDA receptor is irrelevant in excitotoxic axonal death because these cells contains negligible levels of NMDA receptors (Jones and Baughman 1991). Although NMDA receptor blockers are effective in protection of gray matter, none of them were proven to be protective against axonal damage in focal cerebral ischemia and spinal cord injury (Yam et al. 2000; Agrawal and Fehlings 1997; Ouardouz et al. 2006). This might partially explain the failure of NMDA receptor antagonists in clinical stroke treatments.
4 Ionic Mechanism of Ischemic Oligodendrocyte Damage
The ionic mechanisms identified in ischemic axonal fibers are not completely applicable to oligodendrocytes. Blockade of Na+ channels by TTX, while preventing axonal loss, does not prevent oligodendrocyte loss, so it can be deduced that Na+ influx mediated by Na+ channels is not involved in excitotoxic oligodendrocyte death (Tekkok and Goldberg 2001). Neurotoxic Ca2+ entry plays an important role in oligodendrocyte death, and the route of Ca2+ entry may include activation of AMPA/kainate receptors, NMDA receptors, voltage-gated Ca2+ channels, and possible reversal operation of Na+/Ca2+ exchangers. Primarily cultured oligodendrocytes are vulnerable to AMPA/kainate receptor-mediated excitotoxicity and hypoxic–ischemic injury. It has been shown that direct activation of AMPA/kainate receptors by AMPA, kainate, glutamate, or by OGD shows dose-dependent toxicity to cultured oligodendrocytes. On the other hand, application of AMPA/kainate receptor antagonists or removal of Ca2+ from culture medium protects cultured oligodendrocytes from excitotoxic injury. Blockade of AMPA/Kainate receptors also suppresses OGD-induced Ca2+ entry (Yoshioka et al. 1995; Sanchez-Gomez and Matute 1999; McDonald et al. 1998).
Cultured oligodendrocytes can be divided into precursor and mature type cells based on their morphological and antigenic classification (Raff 1989). Oligodendrocyte precursor cells are much more vulnerable than mature cells to hypoxic–ischemic insults; this is associated with an enhanced activation of Ca2+ permeable AMPA/kainate receptors in these precursor cells (Deng et al. 2003). In mature oligodendrocytes, AMPA receptors rather than kainate receptors are suggested as the major mediator of excitotoxic cell death (Leuchtmann et al. 2003). Aside from this in vitro evidence, in situ and in vivo experiments also show that blockade of AMPA/kainate receptors reduces Ca2+-dependent oligodendrocyte death in hypoxic–ischemic acute brain slices and hypoxic–ischemic injury in developing white matter (Tekkok and Goldberg 2001; Follett et al. 2000). Although enhanced Ca2+ influx through Ca2+ permeable AMPA/kainate receptors alone is sufficient to initiate excitotoxicity in cultured oligodendrocytes, selective blockade of voltage-gated Ca2+ channels and the Na+/Ca2+ exchangers still partially attenuates Ca2+ influx and reduces cell death induced by AMPA receptor activation (Alberdi et al. 2002; Chen et al. 2007). Therefore, activation of voltage-gated Ca2+ channels and the reversal Na+/Ca2+ exchangers may contribute to neurotoxic Ca2+ entry following activation of AMPA/kainate receptors.
NMDA receptors are Ca2+ permeable receptors; it has long been thought that the NMDA receptor was not involved in oligodendrocyte death because these cells lack functional expression of NMDA receptors (Berger et al. 1992; Patneau et al. 1994; Liu and Almazan 1995). This concept, however, has been challenged by several reports showing the existence of NMDA receptor subunits and their functional expression in mature and immature oligodendrocytes of the cerebellum and corpus callosum. It was shown that activation of NMDA receptors contributes to ischemia-induced intracellular Ca2+ increase and oligodendrocyte damage (Karadottir et al. 2005; Salter and Fern 2005; Micu et al. 2006). Hence, it is likely that NMDA receptors also participate in hypoxic–ischemic injury of oligodendrocytes. The importance of this contribution in ischemic stroke remains to be further elucidated in animal experiments and human research.
In terms of glutamate-mediated excitotoxicity in ischemic white matter injury and oligodendrocyte loss, it must be acknowledged that this cell death mechanism was established on the simplistic and abstract models of in vitro and in vivo experiments that simulate acute ischemia and excitotoxic injury. In stroke patients, complex ischemic cascades are activated after the onset of stroke. Specifically, glutamate excitotoxicity is a dominant player in the acute phase of ischemic injury, but may not be responsible for all of the dynamic changes and pathological progression in the subacute and chronic stages. Cellular necrosis, apoptosis, and inflammation occur in succession and/or parallel from hours to days after stroke.
Recent evidence has shown that extracellular ATP may also act as an excitatory neurotransmitter, inducing Ca2+-dependent ischemic damage to oligodendrocytes via activating P2X and P2Y receptors (Domercq et al. 2010; Arbeloa et al. 2012). It was shown that in addition to glutamate, enhanced ATP signaling during ischemia is also deleterious to oligodendrocytes and myelin, and impairs white matter function. Oligodendrocytes in culture under OGD condition display an inward current and cytosolic Ca2+ overload, which is partially mediated by P2X7 receptors. Oligodendrocytes release ATP after OGD through the opening of pannexin hemichannels. Consistently, oligodendrocyte death and optic nerve damage are partially reversed by P2X7 receptor antagonists, by the ATP degrading enzyme apyrase, and by blockers of pannexin hemichannels (Domercq et al. 2010). In primary cortical neuron cultures and in brain slices, OGD caused neuronal death that was reduced by Brilliant Blue G (BBG) at concentrations which specifically inhibit P2X7 receptors. In ischemic stroke rats, BBG produced a 60 % reduction in the extent of brain damage compared to treatment with vehicle alone (Arbeloa et al. 2012). These data indicate that ATP released during ischemia and the subsequent activation of P2X7 receptor may contribute to white matter demise during stroke and point to this receptor type as a therapeutic target to limit tissue damage in cerebrovascular diseases.
4.1 Neuroprotection Targeting AMPA and NMDA Receptors
To date, there is no successful translation of glutamate receptor antagonism into efficient drugs for human stroke treatment. The underlying reasons may include, but are not limited to, severity and complexity of ischemic damage, narrowness of therapeutic window, unknown cell death mechanisms in humans, pathophysiological differences between animal and human stroke, lack of focus on ischemic white matter damage, and undesirable side effects of the experimental treatments in humans. Among these potential factors, white matter injury or axonal demyelination after stroke has remained less investigated compared to gray matter injury.
Despite failure in clinical trials, excessive activation of AMPA/NMDA receptors and consequent excitotoxicity are still a predominant theory for stroke pathology and a guide for the development of neuroprotective agents against acute ischemic damage. A novel AMPA receptor antagonist, SPD 502, is reported to reduce ischemic oligodendrocyte damage in a rat stroke model induced by MCA occlusion (McCracken et al. 2002). The well-known NMDA receptor antagonist memantine is clinically licensed by the FDA to treat moderate-to-severe Alzheimer’s disease. Memantine is also found to protect corpus callosum oligodendrocytes and optic nerve fibers from ischemic damage at clinically relevant concentrations (Bakiri et al. 2008). Whether this approach will be effective or not in human patients, the idea that an effective stroke therapy will likely require a combinational approach that targets multiple receptors/channels and multiple signaling pathways is gaining in popularity.
For example, glutamate, released upon an ischemic insult, activates AMPA/kainate receptors, resulting in cell membrane depolarization and consequent activation of NMDA receptors. Thus, it is possible that combination therapy targeting AMPA and NMDA receptors will likely show more efficacy in preventing white matter injury. Glutamate also actives metabotropic receptors that indirectly affect cellular Ca2+, cAMP, protein phosphorylation, and other signaling pathways (Mao and Wang 2002). However, the role of metabotropic glutamate receptors in oligodendrocyte toxicity is obscure and remains to be elucidated.
4.2 Neuroprotection Targeting Axonal Demyelination
An additional neuroprotective strategy is to target axonal demyelination (loss of myelin proteins). As discussed above, several pathways mediate intracellular Ca2+ accumulation in the acute phase of ischemic white matter damage. Neurotoxic Ca2+ seems to be the common signal for axonal skeleton degeneration and oligodendrocyte myelin protein degradation. It is well known that excessive increases of cellular Ca2+ causes mitochondrial dysfunction and enhances generation of reactive oxygen species (ROS) and nitric oxide (NO) (LoPachin and Lehning 1997; Stys 1998; Coleman 2005), which all play important roles in axonal demyelination (Campbell and Mahad 2011; Linares et al. 2006; Smith et al. 1999). ROS inhibition and reduction of NO have been shown to be neuroprotective in experimental models of brain ischemia (O’Mahony and Kendall 1999; Tuttolomondo et al. 2009). Intracellular Ca2+ elevation activates Ca2+-dependent protein kinases and neutral protease (calpain). Calpain activation has been identified as the trigger for axonal demyelination in stroke and multiple sclerosis (Lankiewicz et al. 2000; Shields et al. 1999). Calpain inhibition is effective to reduce neurofilament breakdown and attenuate axonal demyelination in ischemic axons and other injury models (Stys and Jiang 2002; Das et al. 2012). Thus, strategies targeting the downstream signaling behind neurotoxic Ca2+ are alternative neuroprotective approaches to prevent axonal demyelination.
Although axonal degradation and demyelination occur quickly in the ischemic core, a gradual restoration of oligodendrocytes and remyelination have been observed in the peri-infarct area (Gregersen et al. 2001; Tanaka et al. 2003). In the CNS of humans and animals, the capability of remyelination as well as regeneration is preserved for neurogenesis and repair activity following brain injury (Dubois-Dalcq et al. 2008; Duncan et al. 2009; Franklin and Ffrench-Constant 2008). Remyelinating activity has been shown effective in preventing axons from demyelination-associated degeneration (Irvine and Blakemore 2008). Revealing the mechanisms underlying remyelination will afford critical clues to develop novel regeneration strategies. In a mouse brain demyelination model, transplanted neural progenitor cells were found to enhance remyelination via secreting trophic factors: platelet-derived growth factor-AA, and fibroblast growth factor-2 (Einstein et al. 2009).
4.3 Pharmacological Hypothermia Therapy for Ischemic Stroke
Hypothermia, or cooling, is an established method to decrease metabolic activity and protect animal brain or isolated organs/tissues against a variety of injuries in the laboratory or operating room. The neuroprotective effect of therapeutic hypothermia has been consistently demonstrated in ischemic and traumatic brain injury (Tokutomi et al. 2007; Sahuquillo and Vilalta 2007; Kwon et al. 2008; Hemmen and Lyden 2009; Yenari and Hemmen 2010). Animal and human studies suggest that mild to moderate hypothermia (2–5 °C reduction) is generally safe and beneficial for functional recovery after cerebral ischemia. Early administration of physical cooling after cerebral ischemia reduces loss of immature oligodendrocytes in near-term fetal sheep (Roelfsema et al. 2004). Most recently, we have developed a novel neurotensin receptor 1 (NTR1) agonist, ABS201, to effectively induce regulated hypothermia in a focal ischemic stroke model (Choi et al. 2012). We showed that pharmacologically induced hypothermia (PIH) reduces ischemic infarct volume, decreases cell death and improves recovery of sensorimotor function (Choi et al. 2012). We propose that PIH provides not only neuronal protection, but also protects against ischemia-induced axonal and neurovascular damage. The comprehensive effects of PIH are thus regarded as a brain protective therapy as compared to the conventional approach that targets only one individual cell type (e.g., neuron) or a single receptor/signaling pathway. Further investigations are necessary to explore brain protection strategies using hypothermia-inducing drugs or other approaches in protecting structure in the ischemic brain, including the white matter.
4.4 Stem Cell Therapy for Ischemic Stroke
A rapidly developing strategy for stroke therapy is the application of stem cells to repair ischemia-damaged brain tissue through either cell replacement or tropic action after transplantation. In a neonatal hypoxia–ischemia model, transplanted bone marrow stem cells reduced MBP loss and increased oligodendrogenesis in the damaged brain through adapting into the damaged tissue and stimulating several endogenous repair pathways (van Velthoven et al. 2010). Our recent study has shown that transplantation of bone marrow mesenchymal stem cells (BMSCs) into the peri-infarct region of adult stroke mice partially restored thalamocortical circuitry and enhanced functional recovery (Song et al. 2012). BMSCs were implanted 1 and 7 days after barrel cortex stroke. This treatment reduced infarct formation. The behavioral corner test showed better long-term recovery of sensorimotor activities in BMSC-treated mice. Six weeks post-stroke, extracellular recordings of field potentials in the BMSC-transplanted brain slices showed noticeable recovery of ischemia-disrupted intracortical activity from layer 4 to layers 2/3, and the thalamocortical circuit activity was also partially restored. Immunofluorescence showed that the density of neurons, axons and blood vessels in the peri-infarct area was significantly higher in BMSC-treated mice, accompanied with enhanced local blood flow. BMSC treatment increased the levels of SDF-1, VEGF, and BDNF in peri-infarct region. The expression of axonal growth associated protein-43 (GAP-43) was markedly increased, and the axonal growth inhibiting proteins, ROCK II and NG2, were suppressed in the BMSC-treated brain, suggesting a potential signaling pathway that mediates the BMSC effect on axon growth and regeneration. This study provides electrophysiological, morphological, and molecular evidence that BMSC transplantation has a clear potential to repair the ischemia-damaged neural networks involving gray and white matters. More efforts are needed to optimize the strategy by exploring the mechanisms underlying stem cell therapy and discerning the appropriate time window for stem cells to adapt to the environment of the ischemic brain.
5 Conclusion
Stroke therapy has come a long way in terms of improving survival and chronic treatment such as physical therapies, but current effective treatments for acute ischemic stroke patients are very limited. Recent studies have suggested that the key to improving recovery, restoring function, and reducing long-term disability lies in reducing white matter as well as gray matter injury. Multiple markers of axonal and oligodendrocyte injury have been identified and are being utilized. Therapy targeting AMPA and NMDA receptors, the ionic balance across membranes and a variety of second messengers may be promising. In addition, recent progresses in developing pharmacological hypothermia therapy and stem cell therapy have brought promising hopes for clinical applications of brain protective and regenerative medicine for stroke patients. Regardless, a more comprehensive approach to research involving multimodal treatments will likely result in a more effective overall stroke therapy in humans.
References
Agrawal SK, Fehlings MG (1997) Role of NMDA and non-NMDA ionotropic glutamate receptors in traumatic spinal cord axonal injury. J Neurosci 17:1055–1063
Akpan N, Serrano-Saiz E, Zacharia BE, Otten ML, Ducruet AF, Snipas SJ, Liu W, Velloza J, Cohen G, Sosunov SA, Frey WH 2nd, Salvesen GS, Connolly ES Jr, Troy CM (2011) Intranasal delivery of caspase-9 inhibitor reduces caspase-6-dependent axon/neuron loss and improves neurological function after stroke. J Neurosci 31:8894–8904
Alberdi E, Sanchez-Gomez MV, Marino A, Matute C (2002) Ca(2+) influx through AMPA or kainate receptors alone is sufficient to initiate excitotoxicity in cultured oligodendrocytes. Neurobiol Dis 9:234–243
Arbeloa J, Perez-Samartin A, Gottlieb M, Matute C (2012) P2x7 receptor blockade prevents ATP excitotoxicity in neurons and reduces brain damage after ischemia. Neurobiol Dis 45: 954–961
Aronowski J, Cho KH, Strong R, Grotta JC (1999) Neurofilament proteolysis after focal ischemia; when do cells die after experimental stroke? J Cereb Blood Flow Metab 19:652–660
Bakiri Y, Hamilton NB, Karadottir R, Attwell D (2008) Testing NMDA receptor block as a therapeutic strategy for reducing ischaemic damage to CNS white matter. Glia 56:233–240
Berger T, Walz W, Schnitzer J, Kettenmann H (1992) GABA- and glutamate-activated currents in glial cells of the mouse corpus callosum slice. J Neurosci Res 31:21–27
Brown AM, Tekkok SB, Ransom BR (2002) Hypoglycemia and white matter: pathophysiology of axon injury and role of glycogen. Diabetes Nutr Metab 15:290–293, discussion 293–294
Campbell GR, Mahad DJ (2011) Mitochondria as crucial players in demyelinated axons: lessons from neuropathology and experimental demyelination. Autoimmune Dis 2011:262847
Chen H, Kintner DB, Jones M, Matsuda T, Baba A, Kiedrowski L, Sun D (2007) AMPA-mediated excitotoxicity in oligodendrocytes: role for Na(+)-K(+)-CL(-) co-transport and reversal of Na(+)/CA(2+) exchanger. J Neurochem 102:1783–1795
Cheng YD, Al-Khoury L, Zivin JA (2004) Neuroprotection for ischemic stroke: two decades of success and failure. NeuroRx 1:36–45
Choi KE, Hall CL, Sun JM, Wei L, Mohamad O, Dix TA, Yu SP (2012) A novel stroke therapy of pharmacologically induced hypothermia after focal cerebral ischemia in mice. FASEB J 26:2799–2810
Coleman M (2005) Axon degeneration mechanisms: commonality amid diversity. Nat Rev Neurosci 6:889–898
Das A, Kelly Guyton M, Smith A, Iv GW, McDowell ML, Holmes C, Matzelle DD, Ray SK, Banik NL (2012) Calpain inhibitor attenuated optic nerve damage in acute optic neuritis in rats. J Neurochem 124(1):133–146
Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr (2009) Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke 40: 2945–2948
Deng W, Rosenberg PA, Volpe JJ, Jensen FE (2003) Calcium-permeable AMPA/kainate receptors mediate toxicity and preconditioning by oxygen-glucose deprivation in oligodendrocyte precursors. Proc Natl Acad Sci U S A 100:6801–6806
Dewar D, Underhill SM, Goldberg MP (2003) Oligodendrocytes and ischemic brain injury. J Cereb Blood Flow Metab 23:263–274
Domercq M, Etxebarria E, Perez-Samartin A, Matute C (2005) Excitotoxic oligodendrocyte death and axonal damage induced by glutamate transporter inhibition. Glia 52:36–46
Domercq M, Perez-Samartin A, Aparicio D, Alberdi E, Pampliega O, Matute C (2010) P2x7 receptors mediate ischemic damage to oligodendrocytes. Glia 58:730–740
Dubois-Dalcq M, Williams A, Stadelmann C, Stankoff B, Zalc B, Lubetzki C (2008) From fish to man: understanding endogenous remyelination in central nervous system demyelinating diseases. Brain 131:1686–1700
Duncan ID, Brower A, Kondo Y, Curlee JF Jr, Schultz RD (2009) Extensive remyelination of the CNS leads to functional recovery. Proc Natl Acad Sci U S A 106:6832–6836
Einstein O, Friedman-Levi Y, Grigoriadis N, Ben-Hur T (2009) Transplanted neural precursors enhance host brain-derived myelin regeneration. J Neurosci 29:15694–15702
Fern R, Davis P, Waxman SG, Ransom BR (1998) Axon conduction and survival in CNS white matter during energy deprivation: a developmental study. J Neurophysiol 79:95–105
Follett PL, Rosenberg PA, Volpe JJ, Jensen FE (2000) NBQX attenuates excitotoxic injury in developing white matter. J Neurosci 20:9235–9241
Franklin RJ, Ffrench-Constant C (2008) Remyelination in the CNS: from biology to therapy. Nat Rev Neurosci 9:839–855
Goldberg MP, Ransom BR (2003) New light on white matter. Stroke 34:330–332
Gregersen R, Christensen T, Lehrmann E, Diemer NH, Finsen B (2001) Focal cerebral ischemia induces increased myelin basic protein and growth-associated protein-43 gene transcription in peri-infarct areas in the rat brain. Exp Brain Res 138:384–392
Hemmen TM, Lyden PD (2009) Multimodal neuroprotective therapy with induced hypothermia after ischemic stroke. Stroke 40:S126–128
Imai H, McCulloch J, Graham DI, Masayasu H, Macrae IM (2002) New method for the quantitative assessment of axonal damage in focal cerebral ischemia. J Cereb Blood Flow Metab 22: 1080–1089
Irvine KA, Blakemore WF (2008) Remyelination protects axons from demyelination-associated axon degeneration. Brain 131:1464–1477
Irving EA, Yatsushiro K, McCulloch J, Dewar D (1997) Rapid alteration of tau in oligodendrocytes after focal ischemic injury in the rat: Involvement of free radicals. J Cereb Blood Flow Metab 17:612–622
Iwai M, Stetler RA, Xing J, Hu X, Gao Y, Zhang W, Chen J, Cao G (2010) Enhanced oligodendrogenesis and recovery of neurological function by erythropoietin after neonatal hypoxic/ischemic brain injury. Stroke 41:1032–1037
Jeyaseelan K, Lim KY, Armugam A (2008) Neuroprotectants in stroke therapy. Expert Opin Pharmacother 9:887–900
Jones KA, Baughman RW (1991) Both NMDA and non-NMDA subtypes of glutamate receptors are concentrated at synapses on cerebral cortical neurons in culture. Neuron 7:593–603
Karadottir R, Cavelier P, Bergersen LH, Attwell D (2005) NMDA receptors are expressed in oligodendrocytes and activated in ischaemia. Nature 438:1162–1166
Kim MJ, Lyoo IK, Kim SJ, Sim M, Kim N, Choi N, Jeong DU, Covell J, Renshaw PF (2005) Disrupted white matter tract integrity of anterior cingulate in trauma survivors. Neuroreport 16:1049–1053
Kwon BK, Mann C, Sohn HM, Hilibrand AS, Phillips FM, Wang JC, Fehlings MG (2008) Hypothermia for spinal cord injury. Spine J 8:859–874
Lankiewicz S, Marc Luetjens C, Truc Bui N, Krohn AJ, Poppe M, Cole GM, Saido TC, Prehn JH (2000) Activation of calpain I converts excitotoxic neuron death into a caspase-independent cell death. J Biol Chem 275:17064–17071
Lansberg MG, Bluhmki E, Thijs VN (2009) Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. Stroke 40:2438–2441
Leppanen L, Stys PK (1997) Ion transport and membrane potential in CNS myelinated axons. II. Effects of metabolic inhibition. J Neurophysiol 78:2095–2107
Leuchtmann EA, Ratner AE, Vijitruth R, Qu Y, McDonald JW (2003) AMPA receptors are the major mediators of excitotoxic death in mature oligodendrocytes. Neurobiol Dis 14:336–348
Li S, Stys PK (2000) Mechanisms of ionotropic glutamate receptor-mediated excitotoxicity in isolated spinal cord white matter. J Neurosci 20:1190–1198
Linares D, Taconis M, Mana P, Correcha M, Fordham S, Staykova M, Willenborg DO (2006) Neuronal nitric oxide synthase plays a key role in CNS demyelination. J Neurosci 26: 12672–12681
Liu HN, Almazan G (1995) Glutamate induces c-fos proto-oncogene expression and inhibits proliferation in oligodendrocyte progenitors: receptor characterization. Eur J Neurosci 7: 2355–2363
LoPachin RM, Lehning EJ (1997) Mechanism of calcium entry during axon injury and degeneration. Toxicol Appl Pharmacol 143:233–244
Mao L, Wang JQ (2002) Glutamate cascade to camp response element-binding protein phosphorylation in cultured striatal neurons through calcium-coupled group I metabotropic glutamate receptors. Mol Pharmacol 62:473–484
Matute C (1998) Characteristics of acute and chronic kainate excitotoxic damage to the optic nerve. Proc Natl Acad Sci U S A 95:10229–10234
Matute C, Alberdi E, Domercq M, Perez-Cerda F, Perez-Samartin A, Sanchez-Gomez MV (2001) The link between excitotoxic oligodendroglial death and demyelinating diseases. Trends Neurosci 24:224–230
McCracken E, Fowler JH, Dewar D, Morrison S, McCulloch J (2002) Grey matter and white matter ischemic damage is reduced by the competitive AMPA receptor antagonist, SPD 502. J Cereb Blood Flow Metab 22:1090–1097
McDonald JW, Althomsons SP, Hyrc KL, Choi DW, Goldberg MP (1998) Oligodendrocytes from forebrain are highly vulnerable to AMPA/kainate receptor-mediated excitotoxicity. Nat Med 4:291–297
Micu I, Jiang Q, Coderre E, Ridsdale A, Zhang L, Woulfe J, Yin X, Trapp BD, McRory JE, Rehak R, Zamponi GW, Wang W, Stys PK (2006) NMDA receptors mediate calcium accumulation in myelin during chemical ischaemia. Nature 439:988–992
Moxon-Emre I, Schlichter LC (2010) Evolution of inflammation and white matter injury in a model of transient focal ischemia. J Neuropathol Exp Neurol 69:1–15
Nakamura M, Araki M, Oguro K, Masuzawa T (1992) Differential distribution of 68 kd and 200 kd neurofilament proteins in the gerbil hippocampus and their early distributional changes following transient forebrain ischemia. Exp Brain Res 89:31–39
Nixon RA, Lewis SE (1986) Differential turnover of phosphate groups on neurofilament subunits in mammalian neurons in vivo. J Biol Chem 261:16298–16301
Nukada H, Dyck PJ (1987) Acute ischemia causes axonal stasis, swelling, attenuation, and secondary demyelination. Ann Neurol 22:311–318
O’Mahony D, Kendall MJ (1999) Nitric oxide in acute ischaemic stroke: a target for neuroprotection. J Neurol Neurosurg Psychiatry 67:1–3
Ogata N, Yonekawa Y, Taki W, Kannagi R, Murachi T, Hamakubo T, Kikuchi H (1989) Degradation of neurofilament protein in cerebral ischemia. J Neurosurg 70:103–107
Ouardouz M, Malek S, Coderre E, Stys PK (2006) Complex interplay between glutamate receptors and intracellular ca2+ stores during ischaemia in rat spinal cord white matter. J Physiol 577: 191–204
Ouardouz M, Coderre E, Basak A, Chen A, Zamponi GW, Hameed S, Rehak R, Yin X, Trapp BD, Stys PK (2009a) Glutamate receptors on myelinated spinal cord axons: I. Glur6 kainate receptors. Ann Neurol 65:151–159
Ouardouz M, Coderre E, Zamponi GW, Hameed S, Yin X, Trapp BD, Stys PK (2009b) Glutamate receptors on myelinated spinal cord axons: Ii. AMPA and glur5 receptors. Ann Neurol 65: 160–166
Pantoni L, Garcia JH, Gutierrez JA (1996) Cerebral white matter is highly vulnerable to ischemia. Stroke 27:1641–1646, discussion 1647
Patneau DK, Wright PW, Winters C, Mayer ML, Gallo V (1994) Glial cells of the oligodendrocyte lineage express both kainate- and AMPA-preferring subtypes of glutamate receptor. Neuron 12:357–371
Philipson KD, Nicoll DA (2000) Sodium-calcium exchange: a molecular perspective. Annu Rev Physiol 62:111–133
Raff MC (1989) Glial cell diversification in the rat optic nerve. Science 243:1450–1455
Roelfsema V, Bennet L, George S, Wu D, Guan J, Veerman M, Gunn AJ (2004) Window of opportunity of cerebral hypothermia for postischemic white matter injury in the near-term fetal sheep. J Cereb Blood Flow Metab 24:877–886
Sahuquillo J, Vilalta A (2007) Cooling the injured brain: How does moderate hypothermia influence the pathophysiology of traumatic brain injury. Curr Pharm Des 13:2310–2322
Salter MG, Fern R (2005) NMDA receptors are expressed in developing oligodendrocyte processes and mediate injury. Nature 438:1167–1171
Sanchez-Gomez MV, Matute C (1999) AMPA and kainate receptors each mediate excitotoxicity in oligodendroglial cultures. Neurobiol Dis 6:475–485
Shields DC, Schaecher KE, Saido TC, Banik NL (1999) A putative mechanism of demyelination in multiple sclerosis by a proteolytic enzyme, calpain. Proc Natl Acad Sci U S A 96: 11486–11491
Smith KJ, Kapoor R, Felts PA (1999) Demyelination: the role of reactive oxygen and nitrogen species. Brain Pathol 9:69–92
Song M, Mohamad O, Gu X, Wei L, Yu SP (2012) Restoration of intracortical and thalamocortical circuits after transplantation of bone marrow mesenchymal stem cells into the ischemic brain of mice. Cell Transplant (in press)
Sozmen EG, Kolekar A, Havton LA, Carmichael ST (2009) A white matter stroke model in the mouse: axonal damage, progenitor responses and MRI correlates. J Neurosci Methods 180: 261–272
Sozmen EG, Hinman JD, Carmichael ST (2012) Models that matter: white matter stroke models. Neurotherapeutics 9:349–358
Stys PK (1998) Anoxic and ischemic injury of myelinated axons in CNS white matter: from mechanistic concepts to therapeutics. J Cereb Blood Flow Metab 18:2–25
Stys PK, Jiang Q (2002) Calpain-dependent neurofilament breakdown in anoxic and ischemic rat central axons. Neurosci Lett 328:150–154
Stys PK, Ransom BR, Waxman SG, Davis PK (1990) Role of extracellular calcium in anoxic injury of mammalian central white matter. Proc Natl Acad Sci U S A 87:4212–4216
Tanaka K, Nogawa S, Suzuki S, Dembo T, Kosakai A (2003) Upregulation of oligodendrocyte progenitor cells associated with restoration of mature oligodendrocytes and myelination in peri-infarct area in the rat brain. Brain Res 989:172–179
Tekkok SB, Goldberg MP (2001) AMPA/kainate receptor activation mediates hypoxic oligodendrocyte death and axonal injury in cerebral white matter. J Neurosci 21:4237–4248
Tokutomi T, Morimoto K, Miyagi T, Yamaguchi S, Ishikawa K, Shigemori M (2007) Optimal temperature for the management of severe traumatic brain injury: effect of hypothermia on intracranial pressure, systemic and intracranial hemodynamics, and metabolism. Neurosurgery 61:256–265, discussion 265-256
Towfighi A, Saver JL (2011) Stroke declines from third to fourth leading cause of death in the United States: historical perspective and challenges ahead. Stroke 42:2351–2355
Tuttolomondo A, Di Sciacca R, Di Raimondo D, Arnao V, Renda C, Pinto A, Licata G (2009) Neuron protection as a therapeutic target in acute ischemic stroke. Curr Top Med Chem 9:1317–1334
van Velthoven CT, Kavelaars A, van Bel F, Heijnen CJ (2010) Repeated mesenchymal stem cell treatment after neonatal hypoxia-ischemia has distinct effects on formation and maturation of new neurons and oligodendrocytes leading to restoration of damage, corticospinal motor tract activity, and sensorimotor function. J Neurosci 30:9603–9611
Volpe JJ (2001) Neurobiology of periventricular leukomalacia in the premature infant. Pediatr Res 50:553–562
Waxman SG, Black JA, Ransom BR, Stys PK (1993) Protection of the axonal cytoskeleton in anoxic optic nerve by decreased extracellular calcium. Brain Res 614:137–145
Yam PS, Dunn LT, Graham DI, Dewar D, McCulloch J (2000) NMDA receptor blockade fails to alter axonal injury in focal cerebral ischemia. J Cereb Blood Flow Metab 20:772–779
Yenari MA, Hemmen TM (2010) Therapeutic hypothermia for brain ischemia: where have we come and where do we go? Stroke 41:S72–574
Yoshioka A, Hardy M, Younkin DP, Grinspan JB, Stern JL, Pleasure D (1995) Alpha-amino-3-hydroxy-5-methyl-4-isoxazolepropionate (ampa) receptors mediate excitotoxicity in the oligodendroglial lineage. J Neurochem 64:2442–2448
Zaidi AU, Bessert DA, Ong JE, Xu H, Barks JD, Silverstein FS, Skoff RP (2004) New oligodendrocytes are generated after neonatal hypoxic-ischemic brain injury in rodents. Glia 46:380–390
Zimmerman UJ, Schlaepfer WW (1988) Calcium-activated neutral proteases (calpains) are carbohydrate binding proteins. J Biol Chem 263:11609–11612
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Song, M., Woodbury, A., Yu, S.P. (2014). White Matter Injury and Potential Treatment in Ischemic Stroke. In: Baltan, S., Carmichael, S., Matute, C., Xi, G., Zhang, J. (eds) White Matter Injury in Stroke and CNS Disease. Springer Series in Translational Stroke Research, vol 4. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-9123-1_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9123-1_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-9122-4
Online ISBN: 978-1-4614-9123-1
eBook Packages: MedicineMedicine (R0)