Abstract
With the first demonstration in the early 1990s that plasmid DNA could be taken up by somatic cells in vivo, resulting in expression of genes encoded by the plasmid and controlled by mammalian promoters, the stage was set for the investigation of the range of compelling applications for endogenous expression of proteins in animals and humans [1]. The finding that simple injection of purified plasmid DNA into a target tissue could induce sustained endogenous production of proteins from the recipient’s own cells precipitated a flurry of research that was hoped would quickly lead to therapies for genetic, metabolic, and infectious diseases, as well as cancer. Unfortunately, while the past two decades have seen substantial progress in understanding the advantages and limitations of nucleic acid-based interventions for human disease as well as licensure of multiple veterinary products, there are currently no DNA-based products approved for human use. With well over 100 human clinical studies of DNA-based product candidates conducted to date, the overarching conclusion from these studies is that, for the vast majority of applications, conventional injection of plasmid DNA into tissues at clinically feasible dose levels is unable to produce consistent, biologically meaningful responses, especially when scaled up from rodent models into larger animal species (including humans) [2]. One key factor contributing to these results is the relatively low efficiency with which DNA crosses the cell membrane to reach its intracellular site of action [3]. To address this issue, many approaches for improving the intracellular uptake of DNA have been evaluated, with electroporation-mediated DNA delivery being one of the most promising. This chapter will discuss the utility of DNA vaccines, and the promise that electroporation delivery systems bring to the use of nucleic acid-based vaccine strategies, as well as the potential impact of electroporation on the field of vaccines in general.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Human Papilloma Virus
- West Nile Virus
- Electrode Array
- Hemorrhagic Fever With Renal Syndrome
- Venezuelan Equine Encephalitis Virus
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
With the first demonstration in the early 1990s that plasmid DNA could be taken up by somatic cells in vivo, resulting in expression of genes encoded by the plasmid and controlled by mammalian promoters, the stage was set for the investigation of the range of compelling applications for endogenous expression of proteins in animals and humans [1]. The finding that simple injection of purified plasmid DNA into a target tissue could induce sustained endogenous production of proteins from the recipient’s own cells precipitated a flurry of research that was hoped would quickly lead to therapies for genetic, metabolic, and infectious diseases, as well as cancer. Unfortunately, while the past two decades have seen substantial progress in understanding the advantages and limitations of nucleic acid-based interventions for human disease as well as licensure of multiple veterinary products, there are currently no DNA-based products approved for human use. With well over 100 human clinical studies of DNA-based product candidates conducted to date, the overarching conclusion from these studies is that, for the vast majority of applications, conventional injection of plasmid DNA into tissues at clinically feasible dose levels is unable to produce consistent, biologically meaningful responses, especially when scaled up from rodent models into larger animal species (including humans) [2]. One key factor contributing to these results is the relatively low efficiency with which DNA crosses the cell membrane to reach its intracellular site of action [3]. To address this issue, many approaches for improving the intracellular uptake of DNA have been evaluated, with electroporation-mediated DNA delivery being one of the most promising. This chapter will discuss the utility of DNA vaccines, and the promise that electroporation delivery systems bring to the use of nucleic acid-based vaccine strategies, as well as the potential impact of electroporation on the field of vaccines in general.
2 DNA Vaccines
2.1 Overview
DNA vaccines are typically composed of plasmid DNA encoding one or more antigens of interest. The antigen sequences incorporated into a DNA vaccine can range from a single peptide epitope all the way to the entire coding sequence for a protein target. There is tremendous flexibility in antigen design, making it possible to encode antigens using strategies such as consensus or mosaic sequences, inclusion of multiple epitope sequences, incorporation of specific mutations, or as fusion protein sequences. Most DNA vaccines now use antigen sequences that have been adapted to optimize codon usage to the codon bias of human genes and modified to optimize production and stability of RNA by removing such elements as cryptic splice donor or acceptor sites [4]. The coding regions are positioned between a strong mammalian promoter (e.g., CMV) and a polyadenylation signal, and may include upstream enhancer and/or intron sequences. If multiple antigenic sequences are expressed by the same plasmid, the coding sequences may be separate and controlled by different promoters, or a single open reading frame may be used with expression of the individual proteins controlled by an IRES (internal ribosome entry site) sequence. Alternatively, processing signals may be interspersed between different antigen sequences that lead to proteolytic cleavage of the various protein components into separate entities. DNA vaccines may also encode immunopotentiators designed to enhance resultant immune responses, such as a cytokine, chemokine, or pathogen-derived adjuvant (e.g., tetanus toxin). These may be included on a separate plasmid or may be encoded on the same plasmid as the antigen of interest. In some cases, the immunopotentiator and antigen may be expressed as a synthetic fusion protein.
2.2 Advantages of DNA Vaccines
DNA-based vaccines offer a number of potential advantages compared to the conventional immunization strategies which are utilized in the majority of vaccines currently licensed for human use (i.e., delivery of a live attenuated pathogen, an inactivated pathogen, or a protein subunit). The foremost of these advantages is the ability to simultaneously induce both cellular and humoral immune responses against the encoded antigens even in the absence of a live pathogen or a potent adjuvant. The ability of DNA vaccines to target both arms of the adaptive immune response while maintaining a favorable safety profile has been demonstrated in numerous studies in both animals and humans (reviewed in [5]).
A second advantage of DNA vaccines is that the manufacture of plasmid DNA is a straightforward, well-defined process that takes advantage of the scalability of Escherichia coli fermentation and the ease of isolating DNA from bacterial cultures. Importantly, the production processes for DNA vaccines do not require access to or production of the pathogen itself and are largely independent of the sequence encoded within a given plasmid. Thus, DNA vaccines constitute a true manufacturing platform in which the production processes developed for one product candidate can be readily and predictably leveraged for subsequent product candidates with the attendant reductions in cost and technical risk as multiple candidates progress in clinical development.
Third, DNA also offers tremendous flexibility in design of the antigen and/or immunopotentiator sequences encoded by DNA vaccines. Antigen sequences can be rapidly and simply synthesized, greatly facilitating vaccine strategies based on rational antigen design/modification. As previously discussed, changes in the DNA sequence of the encoded antigen exhibit minimal impact on the DNA manufacturing process, thus allowing target antigens to be readily and quickly modified in response to new variants or to developments in selection of vaccine targets.
Fourth, the plasmid DNA platform is conducive to inclusion of multiple antigens/components in the vaccine product. As discussed above, the antigens may be encoded on separate plasmids or combined into one or more plasmids encoding multi-antigens. Since all components of the DNA vaccine have the same basic chemical structure and properties, there is virtually no risk of unwanted interactions among vaccine components during the manufacturing process. Fifth, the stability profile of DNA is generally superior to that of protein or attenuated/inactivated vaccines, making it attractive with respect to shelf life and reduced need for maintenance of the cold chain during product transportation and storage. Finally, in contrast to vaccines based on live viral vectors, preexisting or vector-induced host immune responses to DNA plasmids themselves have not been described and therefore do not limit vaccine efficacy. As has been well documented in recent years with viral vector delivery platforms, host immune responses to virus-encoded proteins can raise potential safety concerns [6] and/or prevent effective re-administration of the same viral serotype, thereby diminishing or preventing the desired biological effects [7, 8]. The lack of interference by host immune responses to the vector allows the use of the DNA-based platform for a variety of indications.
Currently, there are three DNA vaccines licensed for use in veterinary indications, including vaccines for prevention of infection by West Nile virus in horses, hematopoietic necrosis virus in farmed salmon, and a therapeutic melanoma vaccine for dogs [9–11]. Despite these successes, the initial high level of enthusiasm for human clinical applications of DNA vaccines waned because of the limited success in extrapolating favorable results from small animals to humans. Even with promising nonclinical proof of concept, clinical trials testing a range of DNA vaccines delivered by conventional needle injection were disappointingly unable to demonstrate consistent, target levels of immune responses [5]. One significant factor contributing to the success of DNA vaccines in small animals is the relatively high DNA doses and volumes of injection used in these species. It is recognized that the injection of comparatively large volumes of fluid in a small rodent muscle can generate hydrostatic forces which can improve the efficiency of intracellular DNA uptake. On a body mass basis, the volume that is typically injected into mouse muscle (50 μl) would scale up to an (infeasible) injection volume of 150 ml in a 60 kg human. Thus, the hydrostatic pressures generated in the mouse muscle under these conditions are unlikely to be recapitulated in larger species. However, as illustrated by the robust immunogenicity of the West Nile virus DNA vaccine in horses, even relatively low efficiency delivery characteristic of conventional low volume injection in a large animal species can be sufficient to confer protective immunity if the target antigen is sufficiently immunogenic.
In spite of the suboptimal immunogenicity observed in a majority of DNA vaccine clinical trials conducted with conventional needle injection, the numerous advantages of the DNA-based vaccine platform spurred investigations into means to enhance the potency in large species, including humans. A number of approaches have been evaluated as a means to resurrect the DNA vaccine field, including improvements in vaccine design; formulations, such as cationic lipids or polymers; adjuvants, such as toll-like receptor agonists; and delivery techniques such as jet injection, ballistic (gene gun) delivery, and electroporation. Among these, electroporation-mediated DNA delivery has proved to be very promising, with substantial evidence of increased potency of DNA vaccines delivered with electroporation in multiple large animal species and, more recently, in several human clinical trials. Note that there are a number of excellent, recent reviews on DNA vaccines that provide depth beyond the scope of this chapter [12, 13].
3 Electroporation-Mediated Delivery of DNA Vaccines
3.1 Clinical Electroporation Devices for DNA Vaccine Delivery
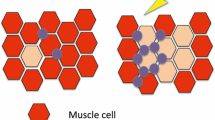
With respect to in vivo DNA delivery, electroporation refers to the propagation of electrical fields within tissues resulting in a transient increase in cell membrane permeability. This enables increased intracellular uptake and expression of DNA molecules present in the local tissue at the time of electroporation application. Most commonly, the electroporation-inducing electrical fields are applied in tissue using arrays of slender rod or needle electrodes contacting the target tissue. Alternatively, larger “plate” style electrodes have also been used for application in surface accessible tissues. The requisite electrical fields are generated using a power source that supplies a series of pulses with a defined waveform, duration, frequency, and field strength. The power source may be configured to generate electrical fields using either constant voltage or constant current. Initial studies in rodents clearly demonstrated that electroporation greatly enhanced expression of proteins encoded by the transferred plasmid DNA [14–16], and this was soon expanded to include applicability of the procedure to larger species [17, 18]. Building on these initial observations, it was rapidly demonstrated that administration of DNA vaccines with electroporation to multiple species, including rodents, rabbits, cattle, and nonhuman primates, resulted in increases in humoral and cellular immune responses of 10–1,000-fold compared to conventional DNA injection alone [19–22]. These enhanced responses were initially and primarily described following intramuscular vaccine delivery, but in recent years, a number of studies have also demonstrated improved responses following electroporation-mediated DNA delivery in skin [23–25].
A variety of device technologies have been developed to support the in vivo application of electroporation for DNA vaccine delivery, and they have been described in detail in other publications [26, 27]. Briefly, the primary objective of these device development efforts is the provision of devices and associated administration procedures capable of achieving safe, effective, and reproducible DNA vaccine delivery within the target tissue. Since the enhanced DNA delivery characteristic of electroporation occurs only in tissues where the DNA is present contemporaneously with the electrical fields, this is best achieved through the provision of devices which can facilitate co-localization of the DNA injection and subsequent electrical field application in the target tissue. Additionally, early clinical experience indicates that the degree of discomfort perceived by the recipients of electroporation is highly correlated with the volume of tissue exposed to the electrical fields [28]. Thus, propagation of electroporation should ideally be confined to tissue in which the DNA has been distributed, making devices which have sufficient precision to reliably achieve this likely to be favored from a tolerability perspective.
As the technology is further refined for human clinical applications, additional considerations that are likely to play a role in the commercial feasibility of the approach include further emphasis on the tolerability profile of the device, the implementation of appropriate safety features, the simplicity of its use, and finally, the upfront and recurring cost of use. A summary of the electroporation devices in development for DNA vaccine delivery in the clinical setting is provided below.
3.1.1 Devices for DNA Vaccine Delivery in Skeletal Muscle
One of the first devices to enter clinical testing for DNA vaccine delivery was the “MedPulser” device developed by Inovio Biomedical [29]. Adapted from devices designed for intratumoral delivery of DNA and chemotherapeutics, the MedPulser utilizes a three-step, manually controlled administration procedure. The procedure is initiated with the intramuscular injection of the DNA into the target tissue using a conventional hypodermic needle and syringe. The withdrawal of the injection syringe is followed by the intramuscular insertion of four needle electrodes arranged in a rectangular array at the site and depth at which the operator judges the DNA to be distributed. The procedure concludes with the user activating the pulse generator connected to the electrodes and then withdrawing the electrode array from the tissue. Although the MedPulser device has generated encouraging results in at least one study to date, it is recognized that the success of this device is largely dependent on the ability of the operator to ensure that the electroporation is reliably applied at the tissue site in which the DNA has been distributed. While perhaps suitable for use in small-scale clinical trials with well-trained operators, it is unclear whether a manually controlled approach can sustain the degree of reproducibility across operators and recipient populations that will be required for product commercialization.
Prompted by these concerns, the field has made significant strides in the development of devices which facilitate co-localization of the DNA administration with the application of the electrical fields. Of foremost importance has been the development of devices in which the means for DNA vaccine administration and electroporation application are integrated into a single device. By integrating the procedural steps required for electroporation-mediated DNA vaccine administration, these devices have the potential to provide more consistent administration while reducing the need for operator training. Moreover, the simpler and more rapid procedure application achievable with these integrated devices is likely to improve acceptance among both recipients and operators. Several integrated device technologies have progressed into clinical testing for DNA vaccine delivery.
The first integrated device to be utilized in clinical testing was the “Twinjector” device (Inovio Biomedical Corporation) [30] followed recently by a more refined version called the “Elgen” (Inovio Biomedical Corporation). Each of these device configurations comprise a multi-use handheld applicator device that is connected to a constant voltage electrical signal generator. In the Twinjector/Elgen device configurations, the DNA dose to be delivered is drawn up into two conventional injection syringes which are affixed with an appropriate injection needle and then inserted into the applicator. The device is placed against the skin of the recipient above the target muscle site. Operator actuation of a gearing mechanism driven either manually (Twinjector) or by motor (Elgen) causes the device to slowly insert the injection needles while simultaneously depressing the syringe plungers to distribute the agent. The resulting DNA distribution comprises a roughly circular column of DNA centered each injection needle. Once the injections have been completed, the electrical signal generator is activated with the two injection needles serving as a bipolar electrode array for propagating the electrical fields. Following completion of the electrical field application, the two injection needles/electrodes are withdrawn from the tissues.
Another integrated device currently in clinical testing for electroporation-mediated DNA vaccination is the TriGrid™ Delivery System for intramuscular administration (TDS-IM) developed by Ichor Medical Systems (San Diego, CA) [26, 31]. The TDS-IM comprises three components: an Application Cartridge, a handheld Integrated Applicator, and a Pulse Stimulator. The Application Cartridge is a sterile, single use component that contains an array of four electrodes and a syringe/injection needle with the DNA dose to be administered. The electrodes are arranged in two equilateral triangles with a common base, forming a diamond shape around the central injection needle. Prior to administration, the Application Cartridge is inserted into the reusable Integrated Applicator which is then connected to the Pulse Stimulator which controls the administration procedure sequence and generates the required signals for induction of electroporation. Prior to administration, a depth gauge on the Application Cartridge is adjusted based on the skin thickness of the recipient to ensure intramuscular administration. The device is then placed against the skin of the recipient above the target muscle site. It is aligned so that the major axis of the diamond-shaped electrode array parallels the orientation of the underlying muscle fibers so that the propagation of the electrical fields will correspond to the ellipsoid fluid distribution characteristic of an intramuscular injection. Upon device activation, mechanisms housed in the Integrated Applicator deploy the recessed electrodes and injection needle into the target muscle. Brief signals from the Pulse Stimulator are used to verify proper deployment of the injection needle and electrodes, followed immediately by administration of the DNA at a controlled rate of injection. Once the injection is completed, constant voltage electrical signals from the Pulse Stimulator are relayed to the deployed electrodes, inducing the electroporation effect. Importantly, the application of electroporation is confined to the site of DNA administration through the aforementioned diamond-shaped configuration of the electrodes combined with the use of electrical insulation limiting electroporation application only to the depth of DNA injection. At the conclusion of the procedure, the device is withdrawn and an automatic sharps protection shield deploys in order to minimize post procedure visualization and exposure to the electrodes and injection needle. Overall, the automated, user-independent TDS-IM device has been designed to perform the administration procedure in a rapid and reproducible fashion while ensuring that the application of electroporation is confined to the site of DNA distribution.
The final device in clinical testing for intramuscular DNA vaccine delivery is the CELLECTRA device originally developed by Advisys, Inc. and now owned by Inovio Biomedical [32]. Developed originally for use in veterinary applications, including the porcine growth hormone releasing hormone (GHRH) product currently licensed for use in Australia (see Sect. 9.3.2 for discussion), the CELLECTRA utilizes a five electrode circular array connected to a constant current pulse generator through a reusable handle device. Prior to the administration procedure, the electrode array is inserted into the handle device. The handle is then manually depressed over the skin at the target site of administration, inserting the electrodes into the underlying muscle tissue. A syringe and injection needle containing the DNA to be delivered is inserted through a central injection port in the handle and into the tissue. Once full insertion is reached, a depth control stop prevents further needle insertion. The user then initiates the injection of the agent into the tissue followed by activation of the pulse generator. The procedure concludes with the withdrawal of the device following completion of the electroporation sequence.
3.1.2 Devices for DNA Vaccine Delivery in Skin
The encouraging findings with electroporation-mediated intramuscular delivery of DNA vaccines combined with the potential advantages of skin delivery for certain DNA vaccine applications have prompted substantial efforts to develop device technology to support the application of electroporation for DNA delivery in skin. This includes adaptation of device platforms developed originally for intramuscular delivery (e.g., CELLECTRA, TDS) as well as development of dedicated platforms for skin delivery (Cyto Pulse DermaVax™, Inovio Minimally Invasive Device). While the basic principles and requirements for electroporation delivery in skin are the same as those for intramuscular delivery, the ability to directly visualize the site of DNA distribution following skin injection has reduced the impetus to develop integrated devices to facilitate co-localization of the DNA and electrical fields. As a result, most of the current device configurations use a manually controlled multistep procedure comprising user-performed injection followed subsequently by electrode array insertion and activation at the site of DNA injection (the lone exception being the TDS-ID device).
The first device to enter clinical testing for electroporation-based delivery in skin was the DermaVax [33] device originally developed by Cyto Pulse Sciences, Inc. and now owned by Cellectis, Inc. The DermaVax device utilizes a single use electrode array comprising two parallel rows of 2 mm length needle electrodes that are connected to a constant voltage pulse generator through a reusable connector cord. Of note, the DermaVax pulse generator device is capable of varying the amplitude and duration of the pulses within a given sequence, potentially allowing for the identification of more complex stimulation conditions that may be beneficial for certain applications. Electrode arrays with four or six electrodes per row are available to accommodate varying tissue volumes. The DermaVax administration procedure is initiated with a user-controlled injection of DNA into the skin of the recipient. Clinical studies have been performed using both needle injection using the Mantoux technique as well as using needle-free injection with the Biojector device. Following completion of the injection, the electrode array is manually inserted into the site the user judges to be the site of DNA distribution (typically demarcated by a skin weal) such that the two rows of electrodes span the injection site and the pulse generator is activated to generate the electrical fields across the administration site.
Another device in early phase clinical testing is the CELLECTRA skin device derived from the intramuscular CELLECTRA device described in Sect. 9.3.1.1. The CELLECTRA skin device utilizes an array of three penetrating electrodes arranged in a triangular configuration which interfaces with a reusable handle connected to the CELLECTRA constant current pulse generator. Consistent with the DermaVax device, the procedure is initiated with a manual DNA injection in the skin followed by insertion and activation of the electrode array at the putative DNA distribution site.
The TriGrid Delivery System for skin administration (TDS-ID) [28] is scheduled to enter clinical testing in 2012. Designed to function analogously to the TDS-IM device, the TDS-ID device is based on an integrated, automated three-component design. At the initiation of the procedure, the user inserts a single use Application Cartridge into the handheld Integrated Applicator. The Application Cartridge houses an array of four electrodes configured to form two isosceles triangles with an adjoining base around a central needle-free injection port. This configuration is designed to accommodate the circular injection distribution characteristic of a skin injection. Placement and activation of the TDS-ID device at the target skin site result in the automated deployment of the electrode array and verification of insertion followed by the injection of the DNA by needle-free jet injection into the skin. Immediately after injection, the electroporation-inducing electrical fields are propagated at the site of DNA administration by the constant voltage TDS Pulse Stimulator device. At the conclusion of the procedure the device is withdrawn and a sharps protection shield deployed over the electrodes. Consistent with the rationale described for the TDS-IM device, the TDS-ID device is designed to support a consistent, user-independent administration procedure in which the electrical fields are co-localized with the site of DNA distribution.
In addition to the devices either in clinical testing or on the cusp of initiation, there are several novel minimally invasive skin delivery device concepts for which initial proof of concept for epidermal DNA delivery has been established. These include two similar systems which utilize a closely spaced grid of non-penetrating “point” electrodes configured in a 4 × 4 arrangement; one was developed at Inovio utilizing a 1.5 mm intraelectrode spacing [34] and the other in the laboratory of Richard Heller utilizing a 2 mm intraelectrode [35]. In both cases, the administration procedure is initiated with a user-controlled injection into the skin followed by the placement and activation of the electrode arrays at the site of DNA administration. Inovio has also assessed the initial feasibility of a non-contact electrode system which utilizes repeated activation of a piezoelectric spark generator placed above (i.e., not in contact with) the site of DNA administration resulting in localized electric field propagation [36].
Finally, Inovio has published results from the initial testing of a device capable of simultaneous electroporation application at multiple depths (e.g., muscle and skin) [37]. The device utilizes the 4 × 4 minimally invasive skin device described above, where the four corner electrodes of the grid are extended to a 1.5 cm length. Following independent but overlying DNA injections in both the skin and the muscle, the electrode array is then inserted into the skin, with the four corner electrodes penetrating into the muscle tissue. The electrodes are then activated in a staged fashion using a pulse generator device capable of applying the required stimulation conditions for application in skin and muscle, respectively.
3.2 Animal Studies and Vaccination Strategies
Electroporation-mediated delivery of DNA vaccines has been evaluated for a number of indications, including prophylactic and therapeutic applications for infectious diseases, cancer, and allergy. This delivery technology has been used for DNA vaccines in numerous mammalian and avian species, including mice, rats, hamsters, guinea pigs, ferrets, rabbits, woodchucks, dogs, pigs, goats, sheep, cattle, rhesus macaques, cynomolgus macaques, chimpanzees, baboons, chickens, and ducks [19, 22, 38–47]. Electrode arrays are readily adaptable to different species, with the intraelectrode spacing and depth of penetrating electrodes typically adjusted to suit the target muscle or skin.
In addition to its use for DNA vaccine delivery, electroporation has also been used to deliver DNA encoding therapeutic proteins that have systemic and/or local tissue effects, such as interferon-beta [48] or VEGF [49]. In fact, the only DNA product that is currently licensed for delivery by electroporation is a veterinary product in Australia consisting of a DNA plasmid encoding porcine GHRH that is delivered intramuscularly to sows to improve the viability of offspring [50]. Electroporation-mediated plasmid delivery has also been used to provide long-term expression of DNA-encoded monoclonal antibodies [51–53], indicating that DNA-based monoclonal antibody products could potentially replace the need for frequent injections of recombinant monoclonal antibody therapies. Electroporation has also been widely used to deliver DNA vaccines as a means of generating antibodies against antigens, such as self-proteins, for which high affinity antibodies were difficult to generate with traditional vaccination methods [54, 55]. In addition, intratumoral delivery of plasmid DNA encoding immunotherapies such as IL-12 and AMEP (anti-angiogenic metargidin peptide) for melanoma have shown intriguing antitumor effects in animal models [56, 57] and is now being evaluated in human clinical studies. In a Phase I clinical trial, intratumoral delivery of plasmid encoding IL-12 resulted in complete regression of metastases in 10% of subjects and disease stabilization or partial response in 42% of subjects [58]. This approach is undergoing further evaluation in several clinical trials. A Phase I trial of intratumoral AMEP is in progress (ClinicalTrials.gov Identifier NCT01045915), and another Phase I evaluated AMEP antitumor activity using intramuscular delivery with electroporation has recently been initiated (NCT01664273).
One key issue related to vaccine product development is whether the immune response generated following vaccination is capable of protecting the host from the pathogen (infectious disease vaccines) or tumor (cancer vaccines). The ability of DNA vaccines delivered with electroporation to provide protective immunity has been demonstrated in several animal models. Electroporation-mediated vaccination with various influenza DNA constructs followed by challenge with homologous and/or heterologous virus strains has clearly shown that protective levels of antibodies can be generated by this vaccination approach in mice, ferrets, and/or nonhuman primates [20, 39, 59–61]. Multiple studies of electroporation-mediated delivery of SIV or SHIV DNA vaccines in macaques have also shown some degree of viral control following viral challenge [62–64]. Protection of macaques from anthrax spore challenge or Venezuelan equine encephalitis virus has also been demonstrated following electroporation-mediated delivery of DNA vaccines encoding proteins specific to each pathogen [45, 65]. Interestingly, electroporation-mediated administration of the anthrax DNA vaccine generated neutralizing antibodies and protection from challenge at levels comparable to those provided from the currently licensed recombinant anthrax vaccine, supporting the robustness of the DNA vaccine/electroporation delivery platform [65]. Other indications for which electroporation-mediated delivery of DNA vaccines have provided protective immunity include infection with Clostridium difficile (mice) [66], chikungunya (mice, macaques) [67], lymphocytic choriomeningitis virus (mice) [68], monkeypox (macaques) [24], bovine viral diarrhea virus (cattle) [69], Schistosoma (mice) [70], Mycobacterium tuberculosis (mice) [71], foot-and-mouth disease virus (mice) [72], Pseudomonas aeruginosa (mice) [73], Japanese encephalitis virus (mice) [74], or challenge with tumor cells (mice, rat, hamster) [75–79]. In addition to protective efficacy, the ability to elicit therapeutic responses has also been described in several animal models, including chronic viral infection [80] and cancer [81, 82].
Mucosal immune responses are likely to play an important role in protection against initial infection from many pathogens. With electroporation-mediated delivery, strong mucosal responses, particularly T cell responses, have been detected in macaques following intramuscular administration of plasmids encoding SIV antigens [83], especially when a plasmid encoding the CCL27/CTACK chemokine was co-administrated with the SIV DNA vaccine [84]. In addition, mucosal IgA responses have been detected in mice following electroporation-mediated delivery of plasmid-encoded influenza antigens [20]. The inclusion of biological response modifiers, such as CCL27/CTACK, that enhance T cell migration to mucosal surfaces may be an effective strategy to elicit antigen-specific immunological responses at the primary site of pathogen entry.
3.3 Nonclinical Safety of Electroporation-Mediated DNA Vaccine Delivery
A number of issues are involved in assessing the safety of DNA vaccines delivered with electroporation. First, the clinical electroporation device and procedure should have safeguards that avoid accidental discharge, prevent administration of the incorrect electrical field, and protect the operator from the electrodes or the syringe used to administer DNA. For the most part, these issues have been addressed in the clinical electroporation devices currently being evaluated in the clinic [26]. A second important safety issue is that the antigen produced by the vaccine should not produce unwanted or harmful biological effects in the subject. For example, when selecting a bacterial toxin as the antigen in a vaccine, the gene encoding the toxin must be modified to reduce the potential for toxicity to the host (e.g., inactivation of C. difficile toxin A [66]). If a vaccine includes a gene encoding a protein with potential toxic systemic effects, the risk of potential adverse side effects may be mitigated by performing a dose escalation in initial human testing, starting with delivery of low quantities that are unlikely to produce high amounts of the protein, and increasing levels if no severe adverse events are observed. Toxicity due to the DNA vaccine and/or the administration method typically has been evaluated by repeat dose toxicity studies in a species predicted to have biological responses (including immune responses) similar to those of humans. With electroporation-mediated delivery of DNA vaccines, no significant systemic effects have been reported in animals. In the first few days following the procedure, low to moderate levels of inflammation have been observed at the injection site tissues (muscle and/or skin) due to recruitment of macrophages, T cells, B cells, and dendritic cells, probably in response to antigen expression and tissue damage [85–87], as evidenced by the presence of muscle fibers with centrally located nuclei, suggestive of regeneration. The inflammation and associated tissue damage are typically rapidly resolved, with tissue appearing normal within several weeks following delivery of the DNA vaccine [32, 88–90], indicating that electroporation-mediated DNA vaccine delivery does not lead to long-term deleterious effects to the tissue.
The biodistribution and persistence of DNA vaccines following administration have been of particular interest to regulatory agencies, since integration of the DNA into host genomic DNA is a potential safety concern, especially in the gonads. Biodistribution studies examining the fate of the DNA vaccines delivered with electroporation have demonstrated that, similar to conventional injection, the DNA is found primarily at the injection site, with only low levels detectable in other tissues [89–91]. Although electroporation delivery results in higher initial levels of DNA vaccines in transfected tissue compared to conventional needle injection, the levels drop dramatically over time [89–92]. The decrease in plasmid DNA with time is probably the result of immune-mediated clearance of cells expressing the vaccine antigen [85, 86, 93], and the exact kinetics of clearance depends on host immune responses to the antigen. According to FDA Guidance for plasmid DNA vaccines for infectious disease indications, evaluation of whether the plasmid DNA has integrated into the host DNA is currently recommended when there are >30,000 copies of plasmid DNA detected per μg host genomic DNA [94]. Integration studies typically involve separation of high molecular weight genomic DNA from low molecular weight plasmid DNA using various gel electrophoresis methods. The level of plasmid DNA remaining associated with genomic DNA is then measured by qPCR using primers specific for the plasmid DNA. In published studies examining persistence of plasmid DNA vaccines delivered with electroporation in rats or macaques, levels of plasmid DNA that co-purified with genomic DNA were extremely low and similar to those described following conventional DNA injection [90, 91, 95]. Currently, there are no published studies demonstrating that plasmid DNA vaccines delivered with electroporation into animals have actually integrated into host chromosomal DNA. The only study that has found direct evidence of plasmid DNA integration into host DNA following delivery with electroporation was with a plasmid encoding a self-protein, erythropoietin [96]. In this study, the very sensitive RAIC–PCR method used for detection of integration events identified only a few examples of plasmid DNA/host genomic DNA junctions, and was a non-quantitative assay, making it difficult to reach conclusions about the propensity of the plasmid DNA to integrate, other than that it was a rare event. Thus, concerns about integration of plasmid DNA vaccines delivered with electroporation have largely been assuaged by the lack of data indicating that significant levels of plasmid DNA actually integrate into host genomic DNA. Overall, studies of DNA vaccines delivered to multiple animal species with electroporation have not identified any general safety issues that would preclude testing of this approach in humans.
3.4 Human Clinical Trials of DNA Vaccines Delivered with Electroporation
The dramatic enhancement in potency of DNA vaccines delivered with electroporation in animal models has sparked great interest in testing this approach in humans (reviewed in [97]). Currently, there are more than 25 Phase I and II clinical trials ongoing or completed worldwide using electroporation to deliver DNA vaccines for multiple indications (see Table 9.1) (www.clinicaltrials.gov and www.abedia.com/wiley). In addition to evaluating the safety, tolerability, and feasibility of electroporation-mediated DNA delivery, these trials are testing a variety of strategies for inducing potent immune responses. These include the use of vaccines encoding multiple antigens, codon and RNA transcript optimization, inclusion of DNA-encoded adjuvants, use of xenogeneic or consensus antigen sequences, targeting of the antigen to antigen presenting cells, inclusion of T helper cell epitopes, use of epitope or poly-epitope-based antigen designs, or DNA priming followed by boosting with viral-encoded antigens. In addition to the primary characterization of safety, many of the trials are focused primarily on generation of antigen-specific T cell responses (e.g., for therapeutic vaccines), although several also include assessment of antibody responses (e.g., for influenza vaccines) or initial evaluation of efficacy endpoints (e.g., for control of viremia or disease progression).
The first clinical trial using electroporation for delivery of a DNA vaccine was a Phase I/II trial initiated in 2005 in HLA-A2+ subjects with prostate cancer [98]. The vaccine encodes an HLA-A2 restricted tumor-derived epitope from prostate-specific membrane antigen (PSMA) fused to a portion of the tetanus toxin fragment C that provides CD4+ T cell epitopes to enhance responses to PSMA. The vaccine was delivered intramuscularly by conventional injection or with the Inovio Twinjector, with crossover between study groups allowed after safety and immunological data were generated from the initial series of vaccine administrations given at increasing doses. Study results published thus far have indicated that electroporation delivery significantly enhanced antibody responses to the tetanus toxin portion of the vaccine compared to those generated following conventional needle injection [98]. Since the subjects receiving the PSMA vaccine had all previously been immunized with a tetanus vaccine, it is possible that the observed antibody responses were due to activation of tetanus memory responses. Analysis of CD4+ responses to the tetanus toxin fragment and CD8+ responses to the PSMA epitope showed increased responses in vaccinated subjects [99], but there was no clear distinction between subjects that received conventional delivery versus electroporation delivery, although interpretation of the results was complicated by the crossover design of the trial. Importantly, this trial provided safety and tolerability data that indicated that the electroporation procedure was tolerable, with no reports of serious device or vaccine-related adverse events.
Additional trials evaluating electroporation-mediated intramuscular DNA vaccine delivery were initiated in 2007 for cancer, hepatitis C virus (HCV), and HIV vaccines. The cancer studies included Phase I evaluation of a DNA vaccine encoding the tumor-associated antigens carcinoembryonic antigen (CEA) and HER-2 delivered with the Inovio MedPulser to patients with cancers known to express the CEA and/or HER-2 antigens (NCT00647114), and Phase Ia/Ib evaluation of a DNA vaccine encoding a xenogeneic melanosomal antigen (murine tyrosinase) delivered to Stage IIB–IV melanoma patients by Ichor’s TDS-IM (NCT00471133). Although results have not yet been published for these cancer studies, the data from the HCV and HIV studies have been encouraging. The HCV vaccine is designed for therapeutic use in patients with chronic HCV infection, and encodes the viral NS3/4A protein complex that is critical for viral replication. Designed as a Phase I/II dose escalation study in 12 treatment-naïve patients with genotype I chronic HCV infection, subjects received 0.167, 0.5 or 1.5 mg of plasmid (NCT00563173). Transient reductions in viral load were detected in a subset of subjects in the two higher dose cohorts, and persisting T cell responses to the vaccine HCV proteins were observed in four of nine patients in the two highest dose groups [100]. In addition, the MedPulser electroporation procedure was well tolerated by the subjects. Interestingly, following completion of the vaccination schedule and placement onto an HCV standard-of-care regimen of interferon-alpha plus ribavirin, the majority of patients had rapid responses to the antiviral treatment, with loss of viral RNA occurring much earlier than expected when compared to historical outcomes in these populations [100]. The intriguing finding that therapeutic vaccination followed by standard-of-care therapy may speed control of chronic viral infection is being further investigated in a recently initiated Phase II trial of the HCV vaccine (NCT01335711). In this randomized trial, patients will receive an interferon-alpha plus ribavirin standard-of-care course of therapy alone, or the HCV DNA vaccine delivered with electroporation followed by the same standard-of-care regimen.
The HIV study initiated in 2007 was the first trial of electroporation-mediated DNA delivery in healthy volunteers (NCT00545987 [101]). Initiation of this trial was significant to the field in that it indicated that the safety risks associated with electroporation-mediated delivery of DNA vaccines were considered acceptable in a healthy adult population by regulatory authorities. The HIV vaccine was composed of two plasmids encoding multiple HIV-1 subtype C antigens and was delivered intramuscularly by conventional injection or with the TDS-IM electroporation system. The randomized, placebo-controlled trial included three vaccine doses delivered with electroporation (0.2, 1.0 or 4.0 mg) plus a conventional delivery group at the highest dose. Although the study was initially designed to include only two administrations of vaccine or placebo, following favorable safety and tolerability results after the two administrations, the protocol was amended to include a third immunization in the subjects that received the highest vaccine dose with electroporation (4 mg) or placebo. HIV-specific T cells were detected in 75% (4 mg), 63% (1 mg), and 13% (0.2 mg) of volunteers receiving two vaccine administrations with electroporation, in contrast to 0% in the conventional delivery group. The response level with electroporation was increased to 88% following the third vaccine administration. Notably, the antigen-specific T cell responses were sustained throughout the course of the study and were directed toward multiple antigens encoded by the vaccine [101, 102]. The electroporation procedure was well tolerated, and no participants discontinued the study as a result of adverse events. These results provided strong evidence that the enhancement of immune responses observed in animals with electroporation-mediated plasmid DNA delivery could also be generated in human subjects.
In 2008, a Phase I trial of a human papilloma virus (HPV) DNA vaccine was initiated in subjects diagnosed with CIN (cervical intraepithelial neoplasia) 2 or 3 that had undergone surgical or ablative treatment (NCT00685412). This vaccine targets the E6 and E7 oncogenic proteins of HPV subtypes 16 and 18, and is composed of two plasmids encoding E6/E7 fusion proteins that were generated using consensus sequences. It was delivered intramuscularly with the Inovio CELLECTRA device three times at 0.6, 2.0 and 6.0 mg. The trial is completed, and although results have not been published yet, several meeting abstracts and presentations have indicated that the vaccine was generally well tolerated, and no serious adverse events were reported [103, 104]. Cytotoxic T lymphocyte (CTL) responses were observed in 13 out of 18 subjects, and responses were detected to all four target antigens. Humoral responses to the HPV antigens were also detected, with 15 out of 18 subjects developing antibody responses to at least one antigen. Encouraged by these results, a fourth administration of the vaccine with electroporation was added to the trial design using the highest dose (6 mg) to evaluate whether responses could be boosted and whether broader responses could be generated. Although results from this trial have not been published, a randomized, placebo-controlled Phase II study of the vaccine in 148 CIN 2/3 or 3 patients that have not received surgical or ablative interventions was initiated in the USA and will include study sites in at least four other countries (NCT01304524). The primary endpoint for this trial is efficacy, as measured by the number of subjects with confirmed HPV 16 or 18 that show regression of cervical lesions to CIN 1 or less by 36 weeks after study initiation. A secondary endpoint is whether subjects responding to the vaccine also exhibit clearance of the HPV 16 or 18 infection. This Phase II study will provide valuable information about the ability of a DNA vaccine delivered with electroporation to promote immune responses capable of therapeutic activity, and if viral clearance is observed, will provide a strong impetus for further studies not only of this vaccine but also of other therapeutic DNA vaccines. Other recently initiated trials evaluating HPV DNA vaccines for cancer indications include a trial in the US evaluating calreticulin fused to HPV-16 E7 for head and neck cancer associated with HPV-16 infection (NCT01493154), and a trial in the Republic of Korea for HPV-16 or -18 associated CIN (NCT01634503). Ichor’s TDS-IM is being used in both trials for vaccine delivery.
The first trial using electroporation to deliver a DNA vaccine to skin was initiated in 2008. The vaccine uses a xenogeneic approach for prostate cancer and encodes the rhesus macaque prostate-specific antigen (PSA). It is being delivered with the Cyto Pulse (now Cellectis) DermaVax electroporation system at one of four dose levels (0.05, 0.1, 0.4 or 1 mg) to patients with relapsing, non-metastatic prostate cancer (NCT00859729). Besides safety, the trial is monitoring whether the vaccine induces PSA-specific immune responses, as well as whether antitumor effects are observed.
A number of other cancer DNA vaccine trials have been initiated. A DNA vaccine encoding a portion of the human telomerase reverse transcriptase was evaluated in multiple solid tumors including various stages of non-small cell lung carcinoma, breast cancer, melanoma, upper gastrointestinal tract carcinoma, colon carcinoma, renal cell carcinoma, bladder carcinoma, and prostate carcinoma (NCT00753415). The study has been completed, but results of the primary (safety) and secondary (immune responses to the vaccine) endpoint measures have not yet been published. Another cancer trial using the DermaVax delivery system is a Phase I/II trial evaluating a plasmid DNA-encoded fusion of human CEA and a T helper epitope from tetanus toxin in stage I or II colorectal cancer (NCT01064375). This trial includes intravenous cyclophosphamide administration 3 days prior to each vaccine administration. One treatment group receives two doses of vaccine delivered with electroporation at weeks 0 and 12. A second group that had already received the CEA/tetanus toxin DNA vaccine delivered by conventional needle injection receives the vaccine at weeks 0 and 12 with electroporation to test the ability of electroporation delivery to boost responses. The third group receives the vaccine with electroporation at weeks 0 and 12 and in addition, recombinant GM-CSF is administered intradermally/subcutaneously for 4 days starting the day before vaccination. The primary endpoints are safety and immunogenicity of the vaccine, with secondary endpoints including evaluation of the ability of electroporation to boost responses or GM-CSF to enhance immunogenicity. Another ongoing cancer DNA vaccine trial is for acute or chronic myelogenous leukemia. The vaccine consists of HLA-A2 restricted epitopes from the zinc finger transcription factor, Wilm’s tumor protein (WT1), which has been associated with the development of various leukemias, fused to a portion of the tetanus toxin to provide CD4 help. In the Phase I/II trial, the DNA vaccine is delivered intramuscularly with the Inovio MedPulser (NCT01334060). The objectives of the trial are to evaluate whether the vaccine alters mRNA levels of the oncogenes BCL-ABL or WT1, immune responses to these proteins, time to disease progression and survival, as well as whether there is a correlation of changes in oncogene transcript levels with immune responses. One additional cancer vaccine trial that is currently in progress is a Phase I/II trial that was initiated in the spring of 2011 in HLA-A2+ patients with malignant melanoma (NCT01138410). The vaccine contains an HLA-A2-restricted CTL epitope from the melanosomal antigen, TRP-2, and helper T cell epitope sequences encoded within a human antibody molecule. This approach takes advantage of the ability of the Fc region of the antibody to bind to Fc-gamma receptors expressed on antigen presenting cells, thus targeting the vaccine to cells responsible for promoting vaccine responses [105]. It is being delivered by the Ichor TDS-IM device to resected Stage IIIb or Stage IV malignant melanoma in doses of up to 4 mg of plasmid DNA.
Several trials have been initiated in the last few years to evaluate DNA vaccines for infectious diseases. These include four Phase I HIV trials assessing whether addition of a plasmid encoding IL-12 enhances immune responses to the HIV proteins encoded by the vaccines. A randomized, double-blind trial evaluating 3 mg of a multi-plasmid HIV vaccine coding for consensus sequence gag, pol, and env proteins with or without 1 mg of a plasmid coding for human IL-12 delivered intramuscularly with Inovio’s CELLECTRA to healthy volunteers has been completed (NCT00991354). Interim results presented in a press release [106] showed that a higher number of subjects developed T cell responses to the vaccine when IL-12 was included (91%) versus the vaccine encoding only HIV antigens (67%), indicating that IL-12 may improve vaccine responses when included as a gene-based component of the DNA vaccine. This HIV vaccine, without the IL-12 plasmid, is now being evaluated in a trial in HIV-infected subjects on stable HAART (Highly Active Antiretroviral therapy) with the vaccine delivered intramuscularly with the CELLECTRA system (NCT01082692). Another trial evaluating the ability of IL-12 to enhance responses has been initiated in HIV-infected subjects on HAART (NCT01266616). In contrast to the previous trial, one of the trial objectives is to determine the most favorable dose of IL-12 plasmid delivered in combination with plasmids encoding HIV antigens. The HIV portion of the DNA vaccine (called HIV-MAG) consists of two plasmids encoding an HIV-1 clade B gag/pol fusion, a nef/tat/vif fusion, and the env protein. A third plasmid codes for human IL-12. The two HIV plasmids are being delivered at a total dose of 3 mg, with an escalation of the IL-12 plasmid including 0.0, 0.05, 0.25, or 1 mg. All administrations are intramuscular at weeks 0, 4, and 12 by either conventional needle injection or with the Ichor TDS-IM, and include saline placebo controls. Delivery of this vaccine with the Ichor TDS-IM is also being evaluated in two trials in healthy subjects. The first study (NCT01496989) is a randomized, double-blind placebo-controlled trial taking place in three countries in Africa. The HIV-MAG vaccine regimen includes groups that will receive a replication-defective adenovirus (Ad35) encoding HIV-1 antigens (gag, reverse transcriptase, integrase, nef and env) following or preceding administration of the DNA vaccine. The second prophylactic trial utilizing the HIV-MAG construct also includes a dose escalation of the IL-12 plasmid, and in addition, will evaluate the effect of a boost with a recombinant vesicular stomatitis virus (VSV) encoding HIV gag (NCT01578889). Another trial evaluating a DNA plus electroporation prime with viral boost for HIV prophylaxis is underway in healthy adults (NCT01260727). In this trial, the DNA vaccine encodes env and gag and is delivered intramuscularly with the CELLECTRA device or the Biojector 2000 jet injector followed by administration of a modified vaccinia Ankara (MVA) vaccine encoding env, gag, and pol. Altogether, these HIV trials of DNA vaccines will provide a solid basis for determining whether DNA vaccine-based strategies for HIV are worth pursuing, and whether enhancing technologies such as electroporation and immune modulators such as IL-12 are of benefit.
Another trial for an infectious disease indication was initiated in the fall of 2010 for malaria caused by the parasite, Plasmodium falciparum. This prophylactic vaccine is being evaluated in healthy subjects not previously exposed to malaria, and is a polyepitope DNA vaccine consisting of multiple CTL and helper T lymphocyte (HTL) epitopes from antigens expressed during the pre-erythrocytic stage of the parasite life cycle (NCT01169077). The vaccine is being delivered on days 0, 28, and 56 by Ichor’s TDS-IM device, at doses of 0.25, 1.0, and 4.0 mg. The primary outcome is safety, with additional objectives including immunogenicity of the polyepitope vaccine and tolerability of the electroporation administration procedure.
A paper was published in early 2012 describing the results of a Phase I/II trial in China that evaluated electroporation-mediated delivery of a therapeutic vaccine for chronic hepatitis B virus (HBV) infection [107]. This study used a two-needle electroporation device that was designed specifically for the trial. The ED-DNA vaccine consists of two plasmids; one plasmid codes for the HBV envelope middle protein and the second plasmid codes for a human IL-2/interferon-γ (IFN-γ) fusion protein. In the first part of the trial, six subjects with chronic hepatitis B infection and serum alanine aminotransferase (ALT) values of one to two times the upper limit of normal (and therefore not indicated for antiviral treatment according to current guidelines) received the ED-DNA vaccine with electroporation at weeks 0, 4, 12, and 24. Increases over baseline of HBV-specific IFN-γ T cell responses were detected in five of six subjects, and the two subjects that demonstrated the highest HBV-specific T cell responses also exhibited reductions in viral load. The second part of the trial was double-blinded, randomized, and placebo-controlled in subjects chronically infected with HBV with ALT values of two to ten times the upper limit of normal. The subjects received the ED-DNA vaccine with electroporation as well as concurrent lamivudine antiviral treatment (20 completed the study) versus lamivudine only (9 completed the study). The lamivudine was administered to both groups for 72 weeks beginning at week 0, with vaccine delivered at weeks 12, 16, 24, and 36. A significantly higher proportion of subjects on the combined therapy exhibited reduced viral loads at week 60 compared to lamivudine monotherapy, fewer mutations associated with lamivudine resistance were found in the combined therapy group, and T cell response rates were significantly higher with the combined therapy. The vaccination regimen, which included administration at four different sites in the deltoid muscles per time point, was well tolerated. A larger, second Phase II trial using the same vaccination approach (lamivudine monotherapy versus ED-DNA vaccination with electroporation plus concurrent lamivudine therapy) is currently underway in China to further investigate the antiviral effects of ED-DNA vaccination added to standard of care nucleoside therapy (NCT01487876). A similar approach is currently being tested in the Republic of Korea using a vaccine consisting of three plasmids that encode the HBV core, polymerase, and S and L envelope proteins as well as human IL-12 (NCT01641536). The chronically infected HBV subjects are also receiving nucleoside antiviral therapy. The trial includes a plasmid DNA dose escalation, with delivery provided by Ichor’s TDS-IM.
Multiple trials for influenza DNA vaccines delivered with electroporation have been initiated and/or completed. Previously, encouraging results were obtained with influenza DNA vaccines delivered with other enhancing technologies (gene gun or cationic-lipid-based Vaxfectin) in Phase I clinical trials [108, 109]. Although target hemagglutination-inhibition (HI) responses were detected in subjects in both trials, overall, the responses to these vaccines were not as robust as would be needed for a commercial product. These results indicated the continued need for enhancement of responses to DNA vaccines, possibly by electroporation. The first trials of an influenza DNA vaccine delivered with electroporation were located in the USA (NCT01142362) and Korea (NCT01184976), with administration using the CELLECTRA intramuscular device. The vaccine consists of three plasmids encoding consensus sequences for the hemagglutinin (HA), neuraminidase (NA), and M2e-nucleoprotein (M2e-NP) antigens of the H5N1 avian influenza virus. Healthy subjects received 0.2, 0.67, or 2.0 mg of each plasmid at two time points separated by 1 month. According to a press release (http://ir.inovio.com/index.php?s=43&item=443), the results from the US trial indicated that ELISA analyses detected high levels of antibody responses in 96% of the subjects, with antibody responses generated to all vaccine antigens. However, HI titers greater than the indicator of protection titer for influenza virus of 1:40 were detected in only 3 out of 27 of subjects against the Vietnam (A/H5N1/1203/04) strain. Two of these subjects also exhibited HI titers greater than 1:40 against the Indonesia (A/H5N1/5/2005) strain, indicating cross-protection in these subjects. To evaluate effects of a boost with a DNA vaccine encoding a single influenza antigen, as well as to test electroporation-mediated skin delivery in the prophylactic setting, an additional trial was initiated in the subjects from the first influenza trial in which a single administration of 0.9 mg of a plasmid encoding H5 was delivered using the CELLECTRA skin device, with the goal of increasing HI titers (NCT01403155). It is not known why the vaccine evaluated in the initial trial generated strong binding antibody responses yet low HI titers. The use of consensus sequences in the vaccine design, antigen competition between multiple vaccine components, and/or preexisting T cell responses to vaccine components may be factors contributing to this finding; elucidation of the mechanism will lead to improved vaccine and clinical trial designs that should be applicable to other indications as well.
In July 2011, a Phase I trial was initiated using the Inovio CELLECTRA skin device for an influenza vaccine targeting H5N1 and H1N1. Three plasmids encoding two different H1 HA sequences and one H5 HA sequence, designed using consensus sequences, are being administered individually and in combination to healthy volunteers (NCT01405885). This trial will allow an analysis of whether administration of multiple antigens inhibits responses to individual components, and will provide valuable information regarding the safety and tolerability of the new skin electroporation device. Recently, a clinical trial was initiated in Canada (NCT01587131) investigating whether administration of a plasmid DNA-based influenza vaccine expressing two different H1 HA proteins and delivered intramuscularly with Inovio’s CELLECTRA enhances responses to a trivalent inactivated seasonal vaccine in the elderly (>65 years of age). If enhanced responses to the seasonal influenza vaccine are observed with the DNA prime, this could be an important strategy for improving immune responses to vaccines in the elderly.
Finally, DNA vaccines encoding hantavirus antigens from Hantaan and Puumala viruses, pathogens that can cause the sometimes fatal hemorrhagic fever with renal syndrome (HFRS), are being evaluated in healthy subjects in a Phase I clinical trial (NCT01502345). The Haantan and Puumala antigens are encoded on separate plasmids. Studies in hamsters using either gene gun or electroporation delivery of the DNA vaccines showed that immune interference (i.e., reduced immune responses to Hantaan antigens) was detected when the DNA for both viruses was delivered to the same cells [110]. In the current clinical trial, the vaccines are being delivered with Ichor’s TDS-IM either separately or together, and the results should indicate whether immune interference by the Puumala antigens is also observed in human subjects.
4 Challenges and Future of Electroporation-Based DNA Vaccine Delivery
Although initial clinical trial results indicate that DNA vaccines delivered with electroporation generate more robust immune responses than DNA delivered by conventional needle injection, strategies for further enhancing immune responses to DNA vaccines delivered with electroporation in humans would increase the likelihood of successful development of product candidates. Based on studies showing marked enhancement of antigen-specific responses in animals, multiple approaches for improving responses to DNA vaccines are currently being evaluated in clinical trials, as described in Sect. 9.3.4. In addition, a better understanding of the role that regulatory T cells may play in vaccine responses will be important, since there is evidence that these cells can affect the magnitude of primary CD8+ T cell responses as well as the quality of memory T cell responses following DNA vaccination [111]. Other cells that can reduce immune responses are myeloid-derived suppressor cells, which can be potent suppressors of T cell functions and are present in greatly increased numbers in cancer patients (reviewed in [112]). For therapeutic vaccines, it is also becoming more apparent that combining disease-modifying drugs (e.g., chemotherapeutics or antivirals) with vaccination may be an important strategy for controlling disease [100, 107, 113].
The results of tolerability assessments of the electroporation approach conducted in clinical trials to date have been encouraging, with generally favorable responses to the procedure by the subjects even in the prophylactic setting [101]. Although anesthetics are typically used prior to electroporation application in animals to enable precise location of the injection and to avoid the startle reflex, local anesthetics are not typically used in human subjects, supporting general feasibility of the approach for vaccine applications. However, to support the broadest range of applications for electroporation-mediated DNA vaccine delivery, including prophylactic mass immunization and pediatric use, further modifications in device designs and administration procedures may be necessary. Initial clinical experience indicates that electroporation-mediated DNA vaccine delivery in skin exhibits a more favorable tolerability profile than intramuscular delivery, likely due to the smaller volume of tissue in which the electroporation-inducing electrical fields are propagated. Additionally, administration in skin is conducive to a simple application of a topical anesthetic which could further improve the tolerability profile of the procedure.
The design of a DNA vaccine can make a huge impact on the overall ability of the vaccine to promote immune responses. Vaccine features that must be carefully selected so as to maximize expression in target tissues include choice of target antigens, DNA sequence of the antigen (e.g., codon optimization), regulatory regions such as promoter/enhancer and polyadenylation signal, secretion signal, and total number of plasmids. The ongoing accumulation of clinical data for electroporation-based delivery of a broad range of DNA vaccine designs is expected to support identification of specific vaccine strategies and components that promote strong immune responses, enabling subsequent incorporation into other candidate vaccines in development.
One issue confounding interpretation of clinical trial results that is not unique to DNA vaccines but is certainly a factor affecting trials for DNA vaccines delivered with electroporation is that often a true correlate of protection (i.e., an immune response responsible for protection [114]) is not known for a specific indication, particularly for vaccines designed primarily for induction of T cell immunity. In addition, nonclinical findings in animal models may not be predictive of human responses, further complicating the vaccine development pathway. Nevertheless, often a surrogate correlate of protection can be identified that can be used to monitor human responses; whether this surrogate is also an appropriate measure of vaccine efficacy in animal models has to be tested empirically.
The plethora of data generated in animal models and the initial results generated in human clinical trial results have produced continued enthusiasm for further investigation of DNA vaccines delivered with electroporation. Improvements in vaccine design, electroporation delivery devices, and clinical trial designs will continue to bring this field closer to licensure of a DNA vaccine/electroporation-based product for human use. The results of clinical trials currently in progress, as well as results generated by several more trials of DNA vaccines delivered with electroporation that are expected to be initiated in the next year, will be critical for maintaining strong interest in this approach to vaccine development.
References
Wolff JA, Malone RW, Williams P, Chong W, Acsadi G, Jani A, Felgner PL (1990) Direct gene transfer into mouse muscle in vivo. Science 247:1465–1468
Ulmer JB, Wahren B, Liu MA (2006) DNA vaccines: recent technological and clinical advances. Discov Med 6:109–112
Donnelly J, Berry K, Ulmer JB (2003) Technical and regulatory hurdles for DNA vaccines. Int J Parasitol 33:457–467
Ingolotti M, Kawalekar O, Shedlock DJ, Muthumani K, Weiner DB (2010) DNA vaccines for targeting bacterial infections. Expert Rev Vaccines 9:747–763
Kutzler MA, Weiner DB (2008) DNA vaccines: ready for prime time? Nat Rev Genet 9:776–788
Buchbinder SP, Mehrotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, Gilbert PB, Lama JR, Marmor M, Del Rio C, McElrath MJ, Casimiro DR, Gottesdiener KM, Chodakewitz JA, Corey L, Robertson MN (2008) Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 372:1881–1893
Nayak S, Herzog RW (2010) Progress and prospects: immune responses to viral vectors. Gene Ther 17:295–304
Mingozzi F, High KA (2011) Immune responses to AAV in clinical trials. Curr Gene Ther 11:321–330
Davis BS, Chang GJ, Cropp B, Roehrig JT, Martin DA, Mitchell CJ, Bowen R, Bunning ML (2001) West Nile virus recombinant DNA vaccine protects mouse and horse from virus challenge and expresses in vitro a noninfectious recombinant antigen that can be used in enzyme-linked immunosorbent assays. J Virol 75:4040–4047
Corbeil S, Kurath G, La Patra SE (2000) Fish DNA vaccine against infectious hematopoietic necrosis virus: efficacy of various routes of immunisation. Fish Shellfish Immunol 10:711–723
Bergman PJ, Camps-Palau MA, McKnight JA, Leibman NF, Craft DM, Leung C, Liao J, Riviere I, Sadelain M, Hohenhaus AE, Gregor P, Houghton AN, Perales MA, Wolchok JD (2006) Development of a xenogeneic DNA vaccine program for canine malignant melanoma at the Animal Medical Center. Vaccine 24:4582–4585
Liu MA (2011) DNA vaccines: an historical perspective and view to the future. Immunol Rev 239:62–84
Ferraro B, Morrow MP, Hutnick NA, Shin TH, Lucke CE, Weiner DB (2011) Clinical applications of DNA vaccines: current progress. Clin Infect Dis 53:296–302
Aihara H, Miyazaki J (1998) Gene transfer into muscle by electroporation in vivo. Nat Biotechnol 16:867–870
Mir LM, Bureau MF, Rangara R, Schwartz B, Scherman D (1998) Long-term, high level in vivo gene expression after electric pulse-mediated gene transfer into skeletal muscle. C R Acad Sci III 321:893–899
Mathiesen I (1999) Electropermeabilization of skeletal muscle enhances gene transfer in vivo. Gene Ther 6:508–514
Draghia-Akli R, Fiorotto ML, Hill LA, Malone PB, Deaver DR, Schwartz RJ (1999) Myogenic expression of an injectable protease-resistant growth hormone-releasing hormone augments long-term growth in pigs. Nat Biotechnol 17:1179–1183
Mir LM, Bureau MF, Gehl J, Rangara R, Rouy D, Caillaud JM, Delaere P, Branellec D, Schwartz B, Scherman D (1999) High-efficiency gene transfer into skeletal muscle mediated by electric pulses. Proc Natl Acad Sci USA 96:4262–4267
Widera G, Austin M, Rabussay D, Goldbeck C, Barnett SW, Chen M, Leung L, Otten GR, Thudium K, Selby MJ, Ulmer JB (2000) Increased DNA vaccine delivery and immunogenicity by electroporation in vivo. J Immunol 164:4635–4640
Kadowaki S, Chen Z, Asanuma H, Aizawa C, Kurata T, Tamura S (2000) Protection against influenza virus infection in mice immunized by administration of hemagglutinin-expressing DNAs with electroporation. Vaccine 18:2779–2788
Selby M, Goldbeck C, Pertile T, Walsh R, Ulmer J (2000) Enhancement of DNA vaccine potency by electroporation in vivo. J Biotechnol 83:147–152
Zucchelli S, Capone S, Fattori E, Folgori A, Di Marco A, Casimiro D, Simon AJ, Laufer R, La Monica N, Cortese R, Nicosia A (2000) Enhancing B- and T-cell immune response to a hepatitis C virus E2 DNA vaccine by intramuscular electrical gene transfer. J Virol 74:11598–11607
Roos AK, Moreno S, Leder C, Pavlenko M, King A, Pisa P (2006) Enhancement of cellular immune response to a prostate cancer DNA vaccine by intradermal electroporation. Mol Ther 13:320–327
Hirao LA, Draghia-Akli R, Prigge JT, Yang M, Satishchandran A, Wu L, Hammarlund E, Khan AS, Babas T, Rhodes L, Silvera P, Slifka M, Sardesai NY, Weiner DB (2011) Multivalent smallpox DNA vaccine delivered by intradermal electroporation drives protective immunity in nonhuman primates against lethal monkeypox challenge. J Infect Dis 203:95–102
Martinon F, Kaldma K, Sikut R, Culina S, Romain G, Tuomela M, Adojaan M, Mannik A, Toots U, Kivisild T, Morin J, Brochard P, Delache B, Tripiciano A, Ensoli F, Stanescu I, Le Grand R, Ustav M (2009) Persistent immune responses induced by a human immunodeficiency virus DNA vaccine delivered in association with electroporation in the skin of nonhuman primates. Hum Gene Ther 20:1291–1307
Luxembourg A, Evans CF, Hannaman D (2007) Electroporation-based DNA immunisation: translation to the clinic. Expert Opin Biol Ther 7:1647–1664
Rabussay D (2008) Applicator and electrode design for in vivo DNA delivery by electroporation. Methods Mol Biol 423:35–59
Hannaman D (2011) Electroporation-based Trigrid™ delivery system (TDS) for DNA vaccine administration. In: Thalhamer J, Weiss R, Scheiblhofer S (eds) Gene vaccines. Springer, New York (Chapter 8)
Wallace M, Evans B, Woods S, Mogg R, Zhang L, Finnefrock AC, Rabussay D, Fons M, Mallee J, Mehrotra D, Schodel F, Musey L (2009) Tolerability of two sequential electroporation treatments using MedPulser DNA delivery system (DDS) in healthy adults. Mol Ther 17:922–928
Tjelle TE, Salte R, Mathiesen I, Kjeken R (2006) A novel electroporation device for gene delivery in large animals and humans. Vaccine 24:4667–4670
Luxembourg A, Hannaman D, Ellefsen B, Nakamura G, Bernard R (2006) Enhancement of immune responses to an HBV DNA vaccine by electroporation. Vaccine 24:4490–4493
Draghia-Akli R, Khan AS, Brown PA, Pope MA, Wu L, Hirao L, Weiner DB (2008) Parameters for DNA vaccination using adaptive constant-current electroporation in mouse and pig models. Vaccine 26:5230–5237
Roos AK, Eriksson F, Walters DC, Pisa P, King AD (2009) Optimization of skin electroporation in mice to increase tolerability of DNA vaccine delivery to patients. Mol Ther 17:1637–1642
Broderick KE, Shen X, Soderholm J, Lin F, McCoy J, Khan AS, Yan J, Morrow MP, Patel A, Kobinger GP, Kemmerrer S, Weiner DB, Sardesai NY (2011) Prototype development and preclinical immunogenicity analysis of a novel minimally invasive electroporation device. Gene Ther 18:258–265
Donate A, Coppola D, Cruz Y, Heller R (2011) Evaluation of a novel non-penetrating electrode for use in DNA vaccination. PLoS One 6:e19181
Broderick KE, Kardos T, McCoy JR, Fons MP, Kemmerrer S, Sardesai NY (2011) Piezoelectric permeabilization of mammalian dermal tissue for in vivo DNA delivery leads to enhanced protein expression and increased immunogenicity. Hum Vaccin 7:22–28
Lin F, Shen X, McCoy JR, Mendoza JM, Yan J, Kemmerrer SV, Khan AS, Weiner DB, Broderick KE, Sardesai NY (2011) A novel prototype device for electroporation-enhanced DNA vaccine delivery simultaneously to both skin and muscle. Vaccine 29:6771–6780
Hooper JW, Ferro AM, Wahl-Jensen V (2008) Immune serum produced by DNA vaccination protects hamsters against lethal respiratory challenge with Andes virus. J Virol 82:1332–1338
Laddy DJ, Yan J, Kutzler M, Kobasa D, Kobinger GP, Khan AS, Greenhouse J, Sardesai NY, Draghia-Akli R, Weiner DB (2008) Heterosubtypic protection against pathogenic human and avian influenza viruses via in vivo electroporation of synthetic consensus DNA antigens. PLoS One 3:e2517
Liu KH, Ascenzi MA, Bellezza CA, Bezuidenhout AJ, Cote PJ, Gonzalez-Aseguinolaza G, Hannaman D, Luxembourg A, Evans CF, Tennant BC, Menne S (2011) Electroporation enhances immunogenicity of a DNA vaccine expressing woodchuck hepatitis virus surface antigen in woodchucks. J Virol 85:4853–4862
Peruzzi D, Mesiti G, Ciliberto G, La Monica N, Aurisicchio L (2010) Telomerase and HER-2/neu as targets of genetic cancer vaccines in dogs. Vaccine 28:1201–1208
Babiuk S, Baca-Estrada ME, Foldvari M, Storms M, Rabussay D, Widera G, Babiuk LA (2002) Electroporation improves the efficacy of DNA vaccines in large animals. Vaccine 20:3399–3408
Scheerlinck JP, Karlis J, Tjelle TE, Presidente PJ, Mathiesen I, Newton SE (2004) In vivo electroporation improves immune responses to DNA vaccination in sheep. Vaccine 22:1820–1825
Tollefsen S, Vordermeier M, Olsen I, Storset AK, Reitan LJ, Clifford D, Lowrie DB, Wiker HG, Huygen K, Hewinson G, Mathiesen I, Tjelle TE (2003) DNA injection in combination with electroporation: a novel method for vaccination of farmed ruminants. Scand J Immunol 57:229–238
Dupuy LC, Richards MJ, Ellefsen B, Chau L, Luxembourg A, Hannaman D, Livingston BD, Schmaljohn CS (2011) A DNA vaccine for Venezuelan equine encephalitis virus delivered by intramuscular electroporation elicits high levels of neutralizing antibodies in multiple animal models and provides protective immunity to mice and nonhuman primates. Clin Vaccine Immunol 18:707–716
Capone S, Zampaglione I, Vitelli A, Pezzanera M, Kierstead L, Burns J, Ruggeri L, Arcuri M, Cappelletti M, Meola A, Ercole BB, Tafi R, Santini C, Luzzago A, Fu TM, Colloca S, Ciliberto G, Cortese R, Nicosia A, Fattori E, Folgori A (2006) Modulation of the immune response induced by gene electrotransfer of a hepatitis C virus DNA vaccine in nonhuman primates. J Immunol 177:7462–7471
Shan S, Jiang Y, Bu Z, Ellis T, Zeng X, Edwards J, Tian G, Li Y, Ge J, Chen H, Fenwick S (2011) Strategies for improving the efficacy of a H6 subtype avian influenza DNA vaccine in chickens. J Virol Methods 173:220–226
Jaini R, Hannaman D, Johnson JM, Bernard RM, Altuntas CZ, Delasalas MM, Kesaraju P, Luxembourg A, Evans CF, Tuohy VK (2006) Gene-based intramuscular interferon-beta therapy for experimental autoimmune encephalomyelitis. Mol Ther 14:416–422
Murakami T, Arai M, Sunada Y, Nakamura A (2006) VEGF 164 gene transfer by electroporation improves diabetic sensory neuropathy in mice. J Gene Med 8:773–781
Person R, Bodles-Brakhop AM, Pope MA, Brown PA, Khan AS, Draghia-Akli R (2008) Growth hormone-releasing hormone plasmid treatment by electroporation decreases offspring mortality over three pregnancies. Mol Ther 16:1891–1897
Tjelle TE, Corthay A, Lunde E, Sandlie I, Michaelsen TE, Mathiesen I, Bogen B (2004) Monoclonal antibodies produced by muscle after plasmid injection and electroporation. Mol Ther 9:328–336
Perez N, Bigey P, Scherman D, Danos O, Piechaczyk M, Pelegrin M (2004) Regulatable systemic production of monoclonal antibodies by in vivo muscle electroporation. Genet Vaccines Ther 2:2
Yamazaki T, Nagashima M, Ninomiya D, Arai Y, Teshima Y, Fujimoto A, Ainai A, Hasegawa H, Chiba J (2011) Passive immune-prophylaxis against influenza virus infection by the expression of neutralizing anti-hemagglutinin monoclonal antibodies from plasmids. Jpn J Infect Dis 64:40–49
Allard B, Priam F, Deshayes F, Ducancel F, Boquet D, Wijkhuisen A, Couraud JY (2011) Electroporation-aided DNA immunization generates polyclonal antibodies against the native conformation of human endothelin B receptor. DNA Cell Biol 30:727–737
Alexandrenne C, Wijkhuisen A, Dkhissi F, Hanoux V, Creminon C, Boquet D, Couraud JY (2009) Generating antibodies against the native form of the human prion protein (hPrP) in wild-type animals: a comparison between DNA and protein immunizations. J Immunol Methods 341:41–49
Lucas ML, Heller L, Coppola D, Heller R (2002) IL-12 plasmid delivery by in vivo electroporation for the successful treatment of established subcutaneous B16.F10 melanoma. Mol Ther 5:668–675
Trochon-Joseph V, Martel-Renoir D, Mir LM, Thomaidis A, Opolon P, Connault E, Li H, Grenet C, Fauvel-Lafeve F, Soria J, Legrand C, Soria C, Perricaudet M, Lu H (2004) Evidence of antiangiogenic and antimetastatic activities of the recombinant disintegrin domain of metargidin. Cancer Res 64:2062–2069
Daud AI, DeConti RC, Andrews S, Urbas P, Riker AI, Sondak VK, Munster PN, Sullivan DM, Ugen KE, Messina JL, Heller R (2008) Phase I trial of interleukin-12 plasmid electroporation in patients with metastatic melanoma. J Clin Oncol 26:5896–5903
Chen MW, Cheng TJ, Huang Y, Jan JT, Ma SH, Yu AL, Wong CH, Ho DD (2008) A consensus-hemagglutinin-based DNA vaccine that protects mice against divergent H5N1 influenza viruses. Proc Natl Acad Sci USA 105:13538–13543
Price GE, Soboleski MR, Lo CY, Misplon JA, Pappas C, Houser KV, Tumpey TM, Epstein SL (2009) Vaccination focusing immunity on conserved antigens protects mice and ferrets against virulent H1N1 and H5N1 influenza A viruses. Vaccine 27:6512–6521
Alexander J, Bilsel P, del Guercio MF, Stewart S, Marinkovic-Petrovic A, Southwood S, Crimi C, Vang L, Walker L, Ishioka G, Chitnis V, Sette A, Assarsson E, Hannaman D, Botten J, Newman MJ (2009) Universal influenza DNA vaccine encoding conserved CD4+ T cell epitopes protects against lethal viral challenge in HLA-DR transgenic mice. Vaccine 28:664–672
Rosati M, Bergamaschi C, Valentin A, Kulkarni V, Jalah R, Alicea C, Patel V, von Gegerfelt AS, Montefiori DC, Venzon DJ, Khan AS, Draghia-Akli R, Van Rompay KK, Felber BK, Pavlakis GN (2009) DNA vaccination in rhesus macaques induces potent immune responses and decreases acute and chronic viremia after SIVmac251 challenge. Proc Natl Acad Sci USA 106:15831–15836
Belisle SE, Yin J, Shedlock DJ, Dai A, Yan J, Hirao L, Kutzler MA, Lewis MG, Andersen H, Lank SM, Karl JA, O’Connor DH, Khan A, Sardesai N, Chang J, Aicher L, Palermo RE, Weiner DB, Katze MG, Boyer J (2011) Long-term programming of antigen-specific immunity from gene expression signatures in the PBMC of rhesus macaques immunized with an SIV DNA vaccine. PLoS One 6:e19681
Yin J, Dai A, Lecureux J, Arango T, Kutzler MA, Yan J, Lewis MG, Khan A, Sardesai NY, Montefiore D, Ruprecht R, Weiner DB, Boyer JD (2011) High antibody and cellular responses induced to HIV-1 clade C envelope following DNA vaccines delivered by electroporation. Vaccine 29:6763–6770
Livingston BD, Little SF, Luxembourg A, Ellefsen B, Hannaman D (2010) Comparative performance of a licensed anthrax vaccine versus electroporation based delivery of a PA encoding DNA vaccine in rhesus macaques. Vaccine 28:1056–1061
Gardiner DF, Rosenberg T, Zaharatos J, Franco D, Ho DD (2009) A DNA vaccine targeting the receptor-binding domain of Clostridium difficile toxin A. Vaccine 27:3598–3604
Mallilankaraman K, Shedlock DJ, Bao H, Kawalekar OU, Fagone P, Ramanathan AA, Ferraro B, Stabenow J, Vijayachari P, Sundaram SG, Muruganandam N, Sarangan G, Srikanth P, Khan AS, Lewis MG, Kim JJ, Sardesai NY, Muthumani K, Weiner DB (2011) A DNA vaccine against chikungunya virus is protective in mice and induces neutralizing antibodies in mice and nonhuman primates. PLoS Negl Trop Dis 5:e928
Shedlock DJ, Talbott KT, Cress C, Ferraro B, Tuyishme S, Mallilankaraman K, Cisper NJ, Morrow MP, Wu SJ, Kawalekar OU, Khan AS, Sardesai NY, Muthumani K, Shen H, Weiner DB (2011) A highly optimized DNA vaccine confers complete protective immunity against high-dose lethal lymphocytic choriomeningitis virus challenge. Vaccine 29:6755–6762
van Drunen Littel-van den Hurk S, Lawman Z, Wilson D, Luxembourg A, Ellefsen B, van den Hurk JV, Hannaman D (2010) Electroporation enhances immune responses and protection induced by a bovine viral diarrhea virus DNA vaccine in newborn calves with maternal antibodies. Vaccine 28:6445–6454
Zhu Y, Lu F, Dai Y, Wang X, Tang J, Zhao S, Zhang C, Zhang H, Lu S, Wang S (2010) Synergistic enhancement of immunogenicity and protection in mice against Schistosoma japonicum with codon optimization and electroporation delivery of SjTPI DNA vaccines. Vaccine 28:5347–5355
Zhang X, Divangahi M, Ngai P, Santosuosso M, Millar J, Zganiacz A, Wang J, Bramson J, Xing Z (2007) Intramuscular immunization with a monogenic plasmid DNA tuberculosis vaccine: enhanced immunogenicity by electroporation and co-expression of GM-CSF transgene. Vaccine 25:1342–1352
Kim SA, Liang CM, Cheng IC, Cheng YC, Chiao MT, Tseng CJ, Lee F, Jong MH, Tao MH, Yang NS, Liang SM (2006) DNA vaccination against foot-and-mouth disease via electroporation: study of molecular approaches for enhancing VP1 antigenicity. J Gene Med 8:1182–1191
Saha S, Takeshita F, Sasaki S, Matsuda T, Tanaka T, Tozuka M, Takase K, Matsumoto T, Okuda K, Ishii N, Yamaguchi K, Klinman DM, Xin KQ, Okuda K (2006) Multivalent DNA vaccine protects mice against pulmonary infection caused by Pseudomonas aeruginosa. Vaccine 24:6240–6249
Wu CJ, Lee SC, Huang HW, Tao MH (2004) In vivo electroporation of skeletal muscles increases the efficacy of Japanese encephalitis virus DNA vaccine. Vaccine 22:1457–1464
Lladser A, Ljungberg K, Tufvesson H, Tazzari M, Roos AK, Quest AF, Kiessling R (2010) Intradermal DNA electroporation induces survivin-specific CTLs, suppresses angiogenesis and confers protection against mouse melanoma. Cancer Immunol Immunother 59:81–92
Berta GN, Mognetti B, Spadaro M, Trione E, Amici A, Forni G, Di Carlo F, Cavallo F (2005) Anti-HER-2 DNA vaccine protects Syrian hamsters against squamous cell carcinomas. Br J Cancer 93:1250–1256
Kalat M, Kupcu Z, Schuller S, Zalusky D, Zehetner M, Paster W, Schweighoffer T (2002) In vivo plasmid electroporation induces tumor antigen-specific CD8+ T-cell responses and delays tumor growth in a syngeneic mouse melanoma model. Cancer Res 62:5489–5494
Porzia A, Lanzardo S, Citti A, Cavallo F, Forni G, Santoni A, Galandrini R, Paolini R (2010) Attenuation of PI3K/Akt-mediated tumorigenic signals through PTEN activation by DNA vaccine-induced anti-ErbB2 antibodies. J Immunol 184:4170–4177
Iurescia S, Fioretti D, Pierimarchi P, Signori E, Zonfrillo M, Tonon G, Fazio VM, Rinaldi M (2010) Genetic immunization with CDR3-based fusion vaccine confers protection and long-term tumor-free survival in a mouse model of lymphoma. J Biomed Biotechnol 2010:316069
Valentin A, von Gegerfelt A, Rosati M, Miteloudis G, Alicea C, Bergamaschi C, Jalah R, Patel V, Khan AS, Draghia-Akli R, Pavlakis GN, Felber BK (2010) Repeated DNA therapeutic vaccination of chronically SIV-infected macaques provides additional virological benefit. Vaccine 28:1962–1974
Peruzzi D, Gavazza A, Mesiti G, Lubas G, Scarselli E, Conforti A, Bendtsen C, Ciliberto G, La Monica N, Aurisicchio L (2010) A vaccine targeting telomerase enhances survival of dogs affected by B-cell lymphoma. Mol Ther 18:1559–1567
Best SR, Peng S, Juang CM, Hung CF, Hannaman D, Saunders JR, Wu TC, Pai SI (2009) Administration of HPV DNA vaccine via electroporation elicits the strongest CD8+ T cell immune responses compared to intramuscular injection and intradermal gene gun delivery. Vaccine 27:5450–5459
Patel V, Valentin A, Kulkarni V, Rosati M, Bergamaschi C, Jalah R, Alicea C, Minang JT, Trivett MT, Ohlen C, Zhao J, Robert-Guroff M, Khan AS, Draghia-Akli R, Felber BK, Pavlakis GN (2010) Long-lasting humoral and cellular immune responses and mucosal dissemination after intramuscular DNA immunization. Vaccine 28:4827–4836
Kraynyak KA, Kutzler MA, Cisper NJ, Khan AS, Draghia-Akli R, Sardesal NY, Lewis MG, Yan J, Weiner DB (2010) Systemic immunization with CCL27/CTACK modulates immune responses at mucosal sites in mice and macaques. Vaccine 28:1942–1951
Wells KE, Maule J, Kingston R, Foster K, McMahon J, Damien E, Poole A, Wells DJ (1997) Immune responses, not promoter inactivation, are responsible for decreased long-term expression following plasmid gene transfer into skeletal muscle. FEBS Lett 407:164–168
Gronevik E, von Steyern FV, Kalhovde JM, Tjelle TE, Mathiesen I (2005) Gene expression and immune response kinetics using electroporation-mediated DNA delivery to muscle. J Gene Med 7:218–227
Liu J, Kjeken R, Mathiesen I, Barouch DH (2008) Recruitment of antigen-presenting cells to the site of inoculation and augmentation of human immunodeficiency virus type 1 DNA vaccine immunogenicity by in vivo electroporation. J Virol 82:5643–5649
Durieux AC, Bonnefoy R, Busso T, Freyssenet D (2004) In vivo gene electrotransfer into skeletal muscle: effects of plasmid DNA on the occurrence and extent of muscle damage. J Gene Med 6:809–816
Ahlen G, Soderholm J, Tjelle T, Kjeken R, Frelin L, Hoglund U, Blomberg P, Fons M, Mathiesen I, Sallberg M (2007) In vivo electroporation enhances the immunogenicity of hepatitis C virus nonstructural 3/4A DNA by increased local DNA uptake, protein expression, inflammation, and infiltration of CD3+ T cells. J Immunol 179:4741–4753
Dolter KE, Evans CF, Ellefsen B, Song J, Boente-Carrera M, Vittorino R, Rosenberg TJ, Hannaman D, Vasan S (2010) Immunogenicity, safety, biodistribution and persistence of ADVAX, a prophylactic DNA vaccine for HIV-1, delivered by in vivo electroporation. Vaccine 29:795–803
Brave A, Gudmundsdotter L, Sandstrom E, Haller BK, Hallengard D, Maltais AK, King AD, Stout RR, Blomberg P, Hoglund U, Hejdeman B, Biberfeld G, Wahren B (2010) Biodistribution, persistence and lack of integration of a multigene HIV vaccine delivered by needle-free intradermal injection and electroporation. Vaccine 28:8203–8209
Roos AK, Eriksson F, Timmons JA, Gerhardt J, Nyman U, Gudmundsdotter L, Brave A, Wahren B, Pisa P (2009) Skin electroporation: effects on transgene expression, DNA persistence and local tissue environment. PLoS One 4:e7226
Davis HL, Millan CL, Watkins SC (1997) Immune-mediated destruction of transfected muscle fibers after direct gene transfer with antigen-expressing plasmid DNA. Gene Ther 4:181–188
Guidance for Industry: Considerations for Plasmid DNA Vaccines for Infectious Disease Indications (November 2007) Food and Drug Administration Center for Biologics Evaluation and Research
Luckay A, Sidhu MK, Kjeken R, Megati S, Chong SY, Roopchand V, Garcia-Hand D, Abdullah R, Braun R, Montefiori DC, Rosati M, Felber BK, Pavlakis GN, Mathiesen I, Israel ZR, Eldridge JH, Egan MA (2007) Effect of plasmid DNA vaccine design and in vivo electroporation on the resulting vaccine-specific immune responses in rhesus macaques. J Virol 81:5257–5269
Wang Z, Troilo PJ, Wang X, Griffiths TG, Pacchione SJ, Barnum AB, Harper LB, Pauley CJ, Niu Z, Denisova L, Follmer TT, Rizzuto G, Ciliberto G, Fattori E, Monica NL, Manam S, Ledwith BJ (2004) Detection of integration of plasmid DNA into host genomic DNA following intramuscular injection and electroporation. Gene Ther 11:711–721
van Drunen Littel-van den Hurk S, Hannaman D (2010) Electroporation for DNA immunization: clinical application. Expert Rev Vaccines 9:503–517
Low L, Mander A, McCann K, Dearnaley D, Tjelle T, Mathiesen I, Stevenson F, Ottensmeier CH (2009) DNA vaccination with electroporation induces increased antibody responses in patients with prostate cancer. Hum Gene Ther 20:1269–1278
Stevenson FK, Mander A, Chudley L, Ottensmeier CH (2011) DNA fusion vaccines enter the clinic. Cancer Immunol Immunother 60:1147–1151
Sallberg M, Frelin L, Diepolder HM, Jung MC, Mathiesen I, Fons M, Ahlen G, Chen M, Weiland O (2010) Therapeutic DNA vaccination followed by standard-of-care therapy in patients with chronic hepatitis C: a rapid clearance of viremia. Mol Ther 18:S110
Vasan S, Hurley A, Schlesinger SJ, Hannaman D, Gardiner DF, Dugin DP, Boente-Carrera M, Vittorino R, Caskey M, Andersen J, Huang Y, Cox JH, Tarragona-Fiol T, Gill DK, Cheeseman H, Clark L, Dally L, Smith C, Schmidt C, Park HH, Kopycinski JT, Gilmour J, Fast P, Bernard R, Ho DD (2011) In vivo electroporation enhances the immunogenicity of an HIV-1 DNA vaccine candidate in healthy volunteers. PLoS One 6:e19252
Kopycinski J, Cheeseman H, Ashraf A, Gill D, Hayes P, Hannaman D, Gilmour J, Cox JH, Vasan S (2012) ADVAX DNA vaccine delivered via in vivo electroporation induced CD4 responses towards the alpha4beta7-binding V2 loop of HIV gp120 in healthy volunteers. Clin Vaccine Immunol 19:1557–1559
Yan J, Pankhong P, Shen X, Giffear M, Lee J, Harris D, Diaz D, Khan A, Bagarazzi M, Boyer J, Weiner DB, Sardesai NY (2010) Phase I safety and immunogenicity of HPV 16 and 18 DNA vaccines delivered via electroporation. Mol Ther 18:S184
Yan J, Shen X, Giffear M, Lee J, Khan A, Harris D, Pankhong P, Shedlock D, Boyer J, Weiner DB, Bagarazzi M, Sardesai NY (2011) Induction of strong cellular and humoral immune responses following immunotherapy of post-LEEP CIN 2/3 with HPV 16 & 18 E6/E7 DNA vaccines. Mol Ther 19:S8
Pudney VA, Metheringham RL, Gunn B, Spendlove I, Ramage JM, Durrant LG (2010) DNA vaccination with T-cell epitopes encoded within Ab molecules induces high-avidity anti-tumor CD8+ T cells. Eur J Immunol 40:899–910
Inovio Pharmaceuticals (2010) Inovio Pharmaceuticals’ HIV DNA vaccine achieves strong T-cell immune responses in Phase I human trial. Press Release: November 17, 2010
Yang FQ, Yu YY, Wang GQ, Chen J, Li JH, Li YQ, Rao GR, Mo GY, Luo XR, Chen GM (2012) A pilot randomized controlled trial of dual-plasmid HBV DNA vaccine mediated by in vivo electroporation in chronic hepatitis B patients under lamivudine chemotherapy. J Viral Hepat 19:581–593
Jones S, Evans K, McElwaine-Johnn H, Sharpe M, Oxford J, Lambkin-Williams R, Mant T, Nolan A, Zambon M, Ellis J, Beadle J, Loudon PT (2009) DNA vaccination protects against an influenza challenge in a double-blind randomised placebo-controlled phase 1b clinical trial. Vaccine 27:2506–2512
Smith LR, Wloch MK, Ye M, Reyes LR, Boutsaboualoy S, Dunne CE, Chaplin JA, Rusalov D, Rolland AP, Fisher CL, Al-Ibrahim MS, Kabongo ML, Steigbigel R, Belshe RB, Kitt ER, Chu AH, Moss RB (2010) Phase 1 clinical trials of the safety and immunogenicity of adjuvanted plasmid DNA vaccines encoding influenza A virus H5 hemagglutinin. Vaccine 28:2565–2572
Spik KW, Badger C, Mathiessen I, Tjelle T, Hooper JW, Schmaljohn C (2008) Mixing of M segment DNA vaccines to Hantaan virus and Puumala virus reduces their immunogenicity in hamsters. Vaccine 26:5177–5181
Furuichi Y, Tokuyama H, Ueha S, Kurachi M, Moriyasu F, Kakimi K (2005) Depletion of CD25+CD4+T cells (Tregs) enhances the HBV-specific CD8+ T cell response primed by DNA immunization. World J Gastroenterol 11:3772–3777
Gabrilovich DI, Nagaraj S (2009) Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol 9:162–174
Menne S, Tennant BC, Gerin JL, Cote PJ (2007) Chemoimmunotherapy of chronic hepatitis B virus infection in the woodchuck model overcomes immunologic tolerance and restores T-cell responses to pre-S and S regions of the viral envelope protein. J Virol 81:10614–10624
Plotkin SA (2010) Correlates of protection induced by vaccination. Clin Vaccine Immunol 17:1055–1065
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Evans, C.F., Hannaman, D. (2013). Current Status of Electroporation Technologies for Vaccine Delivery. In: Singh, M. (eds) Novel Immune Potentiators and Delivery Technologies for Next Generation Vaccines. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-5380-2_9
Download citation
DOI: https://doi.org/10.1007/978-1-4614-5380-2_9
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-5379-6
Online ISBN: 978-1-4614-5380-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)