Abstract
Ovarian cancer is associated with a high morbidity and mortality, and is the leading cause of gynecologic cancer-related death in the US. In recent years, the molecular pathophysiology of ovarian tumors has been better elucidated, allowing for the distinction of two tumor types: the more indolent type I tumors (encompassing endometrioid, clear cell, low-grade serous, and mucinous carcinomas) and the highly aggressive type II tumors (encompassing high-grade serous carcinomas and malignant mixed müllerian tumors). Type I tumors are related to abnormalities in the MAPK signaling pathway (KRAS and BRAF mutations), the PI3K/Akt2/PTEN pathway, and the Wnt/beta-catenin pathway, as well as mutations in other genes such as ARID1a, PPP2R1A, and HNF1-beta. Type II tumors, in contrast, are characterized by mutations in p53, as well as inactivation of BRCA1/2 and mutations in genes such as Notch3, Rsf-1, and NAC1. In this chapter, we discuss the characteristics and frequency of these molecular abnormalities, with an emphasis on their implications for diagnosis and treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
-
Ovarian cancer is the fifth most common cause of cancer-related death in women in the US, and the leading cause of death among gynecologic neoplasms
-
The 5-year survival for ovarian cancer is only 37%
-
Understanding the pathophysiology of ovarian neoplasms, particularly the molecular basis of disease, is crucial in improving diagnostic and treatment modalities
Classification of Ovarian Epithelial Neoplasms
-
The traditional idea of a progression from well- to poorly differentiated carcinoma for all ovarian cancer subtypes has recently been replaced by a comprehensive, dualistic model of ovarian epithelial neoplasia based on new morphologic and molecular data (Shih and Kurman 2004) (Table 7.1)
Table 7.1 Characteristics of Type I vs. Type II ovarian tumors -
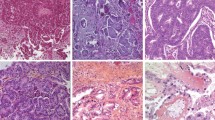
This classification is described below, with a more detailed description of the molecular abnormalities included in subsequent sections (Fig. 7.1).
Fig. 7.1 Prevalence of epithelial ovarian cancer histotypes and their associated molecular abnormalties. (Reprinted from Human Pathology, Kurman and Shih 2011, with permission from Elsevier)
Type I Tumors
-
Type I tumors are composed of several diverse histotypes including low-grade serous carcinoma (LGSC), mucinous carcinoma, endometrioid carcinoma, malignant Brenner tumor, and clear cell carcinoma
-
Precursors/origin
-
These tumors are thought to develop in a stepwise fashion from benign to borderline to malignant tumors Borderline tumors
-
Borderline tumors
-
The term “borderline tumor” refers to an entity intermediate in behavior between cystadenomas and carcinomas
-
Findings in recent years have led to refinement of this category and the histologic and behavioral spectrum it encompasses
-
For serous tumors, two categories have been defined based on behavior: atypical proliferative serous tumors (APST), which is a typical borderline tumor with or without noninvasive implants; and micropapillary serous carcinoma (MPSC), a term synonymous with noninvasive LGSC
-
Mucinous borderline tumors of intestinal type are relatively indolent even if they contain areas of intraepithelial carcinoma or foci of microinvasion (<5 mm), and therefore are best categorized as atypical mucinous proliferative tumors (APMT), with qualification as necessary (“with intraepithelial carcinoma” or “with microinvasion”)
-
Atypical proliferative seromucinous tumor, also known as mucinous borderline tumor of endocervical type, has been found to be associated with endometriosis and endometrioid tumors
-
-
Low-grade serous tumors are believed to progress from adenomas to borderline tumors to noninvasive micropapillary carcinoma (noninvasive LGSC), and finally to invasive LGSC
-
Mucinous tumors may arise from the tubal–peritoneal junction, based on their association with Walthard nests and Brenner tumors, and the presence of transitional metaplasia at the tubal–peritoneal junction in some salpingectomy specimens (Seidman et al. 2011)
-
Many endometrioid and clear cell carcinomas have also been found to be associated with benign or borderline-like lesions, as well as with endometriosis, which is thought to be the benign precursor of these tumors
-
-
Clinical behavior
-
These are indolent tumors which grow to a large size while remaining confined to the ovary at diagnosis
-
Although LGSC demonstrates a pattern of spread similar to its high-grade counterpart, it behaves in a more indolent fashion and is associated with a better prognosis
-
-
Summary of molecular findings
-
Endometrioid and clear cell carcinomas commonly have abnormalities in ARID1A, CCND1/β(beta)-catenin, and the PI3K/Akt2/PTEN pathway
-
LGSC commonly has abnormalities in the MAPK signaling pathway (KRAS and BRAF) and the PI3K/Akt2/PTEN pathway
-
Mucinous carcinoma commonly has mutations in KRAS
-
Type I tumors generally lack mutations in TP53, unlike type II tumors, and therefore this helps in differentiating the two categories
-
Type II Tumors
-
This category includes high-grade serous carcinoma (HGSC), malignant mixed müllerian tumor (MMMT, carcinosarcoma), and undifferentiated carcinoma
-
Histopathology
-
Tumors in this category are high grade in appearance, with complex architecture and significant nuclear atypia
-
Necrosis and high mitotic activity are common
-
HGSC is exclusively epithelial in differentiation, while MMMT displays both epithelial and stromal differentiation
-
-
Precursors/origin
-
The majority of type II tumors appear to arise from tubal epithelium, either from intraepithelial carcinomas which shed cells that implant on the ovary, or from normal tubal epithelium that implants on the ovary to form inclusion cysts from which serous carcinoma can develop (Kurman and Shih 2010)
-
Evidence that supports an origin from the distal fallopian tube includes:
-
Gene expression profiling has found a significant correlation between serous carcinomas and the normal fallopian tube
-
Higher rates of tubal hyperplasia, dysplasia, and occult carcinoma (particularly in the distal tube or fimbriae), as well as TP53 mutations within dysplastic foci, have been found in prophylactic salpingo-oophorectomy specimens compared to resections for other causes
-
In patients with concurrent serous tubal intraepithelial carcinoma (STIC) and ovarian serous carcinoma, identical TP53 mutations have been found in both components
-
-
-
Clinical behavior
-
These tumors behave aggressively, with rapid progression and early metastasis
-
-
Summary of molecular findings
-
Type II tumors commonly have mutations in TP53, chromosomal instability, and inactivation of BRCA1 and BRCA2
-
Molecular Pathways and Alterations by Tumor Type
Type I Ovarian Tumors
Low-Grade Serous Tumors
-
Introduction
-
This category of tumors includes APST and LGSC
-
Low-grade serous tumors of all types commonly demonstrate a papillary architecture and psammoma bodies
-
APST demonstrates papillary epithelial proliferation with hierarchical branching
-
Foci of invasion less than 5 mm are permitted (APST with microinvasion)
-
Extraovarian implants may be noninvasive, noninvasive desmoplastic, or invasive
-
-
MPSC, or noninvasive LGSC, demonstrates an appearance similar to that of APST but with a micropapillary or cribriform epithelial proliferation
-
LGSC also demonstrates cells with a higher nuclear–cytoplasmic ratio and slightly more cytologic atypia than APST
-
The following discussion focuses largely on the molecular pathology of LGSC, but also addresses findings in APST and benign serous tumors where relevant
-
-
Genetic pathways: functions, role in pathogenesis, and frequency of abnormalities
-
MAPK signaling pathway
-
MAPK (mitogen-activated protein kinase), also known as ERK (extracellular signal-regulated protein kinase), is a downstream target of RAS, RAF, and MAPK/ERK kinase
-
MAPK responds to growth factors and other signals by promoting cell proliferation and opposing cell death, and is important in mediating drug-induced apoptosis in tumor cells
-
KRAS and BRAF are both oncogenes involved in the activation of the MAPK pathway
-
Frequency of mutations
-
KRAS mutations have been found in 22–36% of serous borderline tumors and up to 33% of LGSC (Mok et al. 1993)
-
BRAF mutations have been found in up to 31% of serous borderline tumors and up to 36% of LGSC (Mayr et al. 2006)
-
Overall, 60–88% of APST express mutations in either KRAS or BRAF (Ho et al. 2004)
-
With rare exceptions, these mutations are mutually exclusive
-
-
Mutations in KRAS and BRAF help distinguish low-grade serous tumors from HGSC, as these mutations are found in only up to 12% of HGSC (Sieben et al. 2004)
-
The V599E mutation in BRAF occurs exclusively in LGSC (36%)
-
-
Of note, serous cystadenomas adjacent to KRAS- or BRAF-mutated serous borderline tumors were found to have identical mutations in 86% of cases, suggesting that mutation of these two genes precedes progression to serous borderline tumors
-
Others have found these mutations in early APST, supporting their early role in tumorigenesis
-
-
-
Immunohistochemical findings
-
By immunohistochemical staining, activated (phosphorylated) MAPK was found to be expressed in 71% of APST, 80–81% of LGSC, and 41% of HGSC (Hsu et al. 2004)
-
In low-grade serous tumors, MAPK immunoexpression correlates with mutations in KRAS and BRAF. This is in contrast to findings in HGSC
-
-
-
CDKN2/p16
-
p16, encoded by CDKN2 (p16ink4) on 9p21, is a tumor suppressor gene involved in the Rb pathway, and is discussed in more detail below (see section “HGSC and MMMT”)
-
Although found more frequently overexpressed in HGSC, p16 has been found by some authors to be expressed in a significant percentage of low-grade serous tumors
-
Immunohistochemistry
-
-
-
Clinical implications
-
MAPK signaling pathway
-
The constitutive activation of the MAPK signaling pathway in type I tumors suggests a role for MAPK kinase inhibitors in treatment
-
In fact, treatment of KRAS- or BRAF-mutated ovarian cancer cell lines with a MAPK kinase inhibitor was found to cause significant apoptosis and growth inhibition (Pohl et al. 2005)
-
-
Treatment with cisplatin may induce activation of MAPK, with subsequent development of cisplatin resistance
-
Furthermore, treatment with a proteasome inhibitor sensitizes cisplatin-resistant ovarian cancer cells to cisplatin-induced cell death, indicating a potential role for proteasome inhibitors along with cisplatin in MAPK-activated tumors (Wang et al. 2011)
-
-
Patients with both MAPK expression and paclitaxel sensitivity have significantly better 5-year survival than those without these two characteristics (74.9 vs. 31%) (Hsu et al. 2004)
-
-
-
Summary
-
The most common molecular abnormalities in low-grade serous tumors are in the MAPK signaling pathway
-
MAPK expression is common in APST and LGSC, and correlates with mutations in KRAS and BRAF
-
-
Mutations in KRAS and BRAF are useful in distinguishing LGSC from HGSC, in which they occur much less frequently
-
A possible role exists for MAPK kinase inhibitors and proteasome inhibitors in the treatment of MAPK-activated cancers
-
Aberrant expression of p16 is more common in HGSC, but has also been found in a subset of LGSC, with some authors finding a correlation with lower stage and lower grade tumors
-
Endometrioid and Clear Cell Carcinomas
-
Introduction
-
Endometrioid carcinomas of the ovary, most commonly found in woman in their 50s, demonstrate a histologic appearance similar to that of their uterine counterparts
-
Well-differentiated endometrioid carcinomas are composed of branching and confluent glands lined by tall columnar stratified cells
-
Grading is based primarily on the extent of nonsquamous solid architecture, with grade 1 having <5% solid areas, grade 2 with 5–50%, and grade 3 with >50%
-
Nuclear atypia is variable and can be significant, and may also be used as a criterion to assign a tumor one grade higher than that indicated by architecture
-
Various types of metaplasia may be seen, including squamous, secretory, and mucinous
-
Endometrioid carcinomas tend to demonstrate expansile invasion, but also may be infiltrative
-
-
Clear cell carcinomas, which affect a similar age group, display diverse but distinct histologic appearances
-
Common patterns include papillary, tubulocystic, and solid, and these often coexist in a single tumor
-
Papillary areas commonly have hyalinized stroma
-
Tubulocystic carcinomas demonstrate tubules and cysts of varying sizes lined by tumor cells
-
Solid areas demonstrate sheets of polygonal cells with clear cytoplasm
-
-
A variable number of cells may demonstrate eosinophilic cytoplasm rather than the classic clear cytoplasm
-
PAS-positive hyaline globules in the cytoplasm may also be seen
-
-
A spectrum of nuclear atypia is observed, often within the same tumor
-
However, clear cell carcinomas are classified as high grade by definition
-
-
Endometrioid and clear cell carcinomas are discussed together in this section due to the significant overlap of molecular pathways involved in their respective pathogeneses
-
-
Genetic pathways: functions, role in pathogenesis, and frequency of abnormalities
-
Wnt/β(beta)-catenin pathway
-
The gene CTNNB1 on 3p22.1 encodes β(beta)-catenin, a protein involved in the Wnt signaling pathway, which plays a role in the regulation of cell proliferation and differentiation
-
Missense mutations of CTNNB1 frequently result in constitutive activation of the Wnt signaling pathway in endometrioid carcinomas
-
Frequency of mutations
-
Mutations in CTNNB1 have been found in 31–38% of ovarian endometrioid tumors, primarily in exon 3 of the gene (Catasús et al. 2004)
-
Although CTNNB1 mutations have been linked to microsatellite instability in colon cancers, only rare cases of ovarian endometrioid carcinoma have been found to have both CTNNB1 mutations and microsatellite instability
-
While CTNNB1 mutations are always associated with nuclear staining for β(beta)-catenin, microsatellite instability is associated with a membranous β(beta)-catenin staining pattern
-
These abnormalities therefore likely represent two independent mechanisms of pathogenesis
-
-
-
Immunohistochemistry
-
Nuclear β(beta)-catenin immunohistochemical staining has been found in 38–85% of endometrioid carcinomas and up to 5.5% of clear cell carcinomas (Moreno-Bueno et al. 2001)
-
In endometrioid carcinomas, immunopositivity has been strongly correlated with the presence of CTNNB1 mutations
-
-
Nuclear expression of β(beta)-catenin in endometrioid carcinomas has been associated with squamous differentiation in these tumors
-
-
-
Cyclin D1
-
The protein Cyclin D1, encoded by the oncogene CCND1 on 11q13, is a target of the β(beta)-catenin pathway, with activation of the pathway resulting in increased expression of cyclin D1
-
Cyclins are involved in the regulation of cyclin-dependent protein kinases (cdks), with cyclin D1 functioning specifically in allowing the cell to progress from G1 to S phase
-
Immunohistochemistry
-
Although some studies have found no association between cyclin D1 overexpression and histotype, others have found a more frequent association with endometrioid carcinomas, with immunohistochemical positivity being found in 32% of ovarian endometrioid carcinomas and 6% of clear cell carcinomas (Catasús et al. 2004)
-
-
-
PI3K/Akt2/PTEN pathway
-
The PI3K/Akt2/PTEN pathway is involved in the regulation of apoptosis, angiogenesis, cell proliferation and growth, and cell metabolism
-
Activation of the pathway can be the result of amplification of PIK3CA or Akt2, activating mutations in PIK3CA, or inactivating mutations of PTEN
-
PIK3CA is an oncogene located on chromosome 3q26.32, and encodes the PI3K catalytic subunit
-
Akt2 is an oncogene located on chromosome 19q13.1–13.2, and encodes a protein–serine/threonine kinase
-
PTEN (phosphatase and tensin homolog deleted on chromosome 10) is a tumor suppressor gene located on chromosome 10q23.3
-
-
Frequency of mutations/amplifications
-
Mutation or amplification of PIK3CA has been found in 30.5% of ovarian cancers overall, and up to 45% of endometrioid and clear cell carcinomas (Campbell et al. 2004)
-
PTEN is mutated in 14–31% of endometrioid carcinomas (mostly of low grade and low stage), up to 8.3% of clear cell carcinomas, and 20.6% of endometrial cysts (Sato et al. 2000; Willner et al. 2007)
-
Most of the identified mutations have been frameshift mutations
-
LOH at the 10q23.3 locus has been found in 42% of endometrioid carcinomas, 27.3% of clear cell carcinomas, 56.5% of endometrial cysts, and 0% of normal endometrium
-
-
Mutations in Akt2 are more often seen in HGSC (see below)
-
-
-
ARID1A
-
The gene ARID1A encodes the protein BAF250a, which binds to AT-rich DNA sequences and functions as a component of a complex (SWI/SNF) involved in regulating the expression of cell proliferation genes
-
Because many cases of ARID1A mutations show both alleles to be affected, it is hypothesized that ARID1A is a tumor suppressor gene
-
Frequency of mutations
-
Mutations in ARID1A have been found in 46–57% of ovarian clear cell carcinomas, as well as 71% of ovarian clear cell carcinoma cell lines (Jones et al. 2010)
-
Endometrioid carcinomas have also been found to harbor ARID1A mutations at a frequency of up 30% (Wiegand et al. 2010)
-
Mutations have not been found in HGSC
-
-
Immunohistochemical findings
-
Mutations in ARID1A in both endometrioid carcinomas and clear cell carcinomas have been correlated with a loss of immunopositivity for BAF250a, with 73% of ARID1A-mutated clear cell carcinomas and 50% of ARID1A-mutated endometrioid carcinomas showing this loss
-
Loss of expression is specific for these tumors vs. HGSC
-
-
ARID1A may be mutated earlier than HNF1-β(beta) in tumorigenesis
-
-
-
HNF-1-β(beta)
-
HNF-1-β(beta) (hepatocyte nuclear factor-1-β(beta), also known as vHNF-1 or LFB3), along with the related protein HNF-1-α(alpha), has been shown to play a role in transcriptional activation during embryogenesis
-
HNF-1-β(beta) mRNA expression levels have been found to be several times higher in clear cell carcinomas vs. other ovarian tumors
-
The mechanism of upregulation may be related to CpG island hypomethylation
-
-
Immunohistochemical findings
-
Almost all clear cell carcinomas have been found to be immunopositive for HNF-1-β(beta), with most other tumors showing either no staining or only focal faint positivity
-
Nuclear staining is also absent in endometriosis and in normal ovarian surface epithelium (Tsuchiya et al. 2003)
-
-
-
-
Microsatellite instability
-
Microsatellite instability refers to the inactivation of DNA mismatch repair genes, with a resulting increase in mutation frequency of oncogenes and tumor suppressor genes, and a consequently increased risk of neoplastic transformation in various tissue types
-
This is the mechanism responsible for Lynch syndrome (hereditary nonpolyposis colorectal cancer, or HNPCC), a hereditary cancer syndrome in which loss of function of the mismatch repair genes MLH1, MSH2, and MSH6 is frequently found
-
In addition to colorectal cancers, patients with Lynch syndrome are at increased risk of developing cancers at numerous other sites, including the upper gastrointestinal tract, urinary system, and female genital tract, particularly the endometrium and ovary
-
Mechanisms of microsatellite instability in ovarian cancers include frameshift mutations in the coding tracts of BAX, IGFIIR, and MSH3, as well as MLH-1 promoter hypermethylation
-
Loss of hMSH2 expression has also been demonstrated
-
-
Frequency
-
The overall frequency of microsatellite instability in sporadic ovarian cancers was found to be 17%
-
Endometrioid tumors show a frequency of 17–50%, and clear cell carcinomas show a frequency of 6% (Fujita et al. 1995)
-
Microsatellite instability is uncommon in other ovarian tumor types
-
-
Immunohistochemical findings
-
Loss of hMLH-1 nuclear staining has been reported to occur in 14% of endometrioid carcinomas and 6% of clear cell carcinomas, with most tumors being of high grade but low stage (Catasús et al. 2004)
-
-
-
MAPK signaling pathway
-
Mutations in KRAS and BRAF, both oncogenes involved in the activation of the MAPK pathway, are more commonly associated with mucinous tumors and LGSC, but may also be mutated in endometrioid and clear cell carcinomas. (See sections “Mucinous Tumors” and “Low-Grade Serous Tumors” for more details on these two genes and the MAPK pathway.)
-
Frequency of mutations
-
-
TP53
-
Although found with the greatest frequency in serous tumors, TP53 mutations have also been reported to occur in a subset of endometrioid and clear cell carcinomas, particularly those of advanced stage and high grade
-
Frequency of mutations
-
TP53 mutations have been reported to occur in as many as 42% of endometrioid carcinomas and 8% of clear cell carcinomas, with the highest frequency (75%) in grade 3 endometrioid carcinomas (Willner et al. 2007)
-
In a mouse model, TP53 mutations were found with lower frequency in tumors which had defects in the Wnt/β(beta)-catenin or PI3K/Akt2/PTEN signaling pathways, suggesting two separate pathways in the development of low vs. high-grade endometrioid carcinomas (Wu et al. 2007)
-
-
-
PPP2R1A
-
The serine–threonine protein phosphatase PP2A is a family of holoenzymes containing a heterodimer core with a catalytic subunit and a regulatory subunit (PPP2R1A or PPP2R1B)
-
PPP2R1A acts as a scaffold in this complex, which is involved in regulating cell growth and proliferation
-
-
The heterozygous and clustered nature of mutations in this gene suggest that PPP2R1A is an oncogene in tumorigenesis
-
Frequency of mutations
-
Mutations in the PPP2R1A gene have been found in 7.1% of clear cell carcinomas, as well as in 3/7 ovarian clear cell carcinoma cell lines (Jones et al. 2010)
-
-
-
-
Clinical implications
-
Wnt/Β(beta)-catenin pathway
-
The presence of CTNNB1 mutations or β(beta)-catenin nuclear immunopositivity in endometrioid carcinomas has been associated with better differentiation, low grade, early stage, and a favorable prognosis
-
One group found cyclin D1 expression to be inversely correlated with tumor grade, suggesting a better prognosis for tumors with high cyclin D1 expression (Sui et al. 1999)
-
-
HNF-1-β(beta)
-
Silencing of HNF-1-β(beta) in ovarian cancer cell lines results in significantly more apoptosis compared to controls. It is therefore an important potential target for novel ovarian cancer therapies
-
Given its relative specificity for clear cell carcinomas compared to other ovarian cancer histotypes, HNF-1-β(beta) is also a useful immunohistochemical marker in diagnosis
-
-
Microsatellite instability
-
PCR analysis of tumor tissue using microsatellite markers as well as detecting loss of expression of mismatch repair genes by immunohistochemistry are useful methods of assessing for microsatellite instability in patients deemed to be at risk
-
Data concerning the effect of microsatellite instability on clinical behavior are somewhat inconsistent, with evidence of association with longer survival at odds with the association of microsatellite instability with undifferentiated components and aggressive behavior
-
-
-
Summary
-
Endometrioid and clear cell carcinomas show significant similarities and overlap in their molecular pathology
-
The Wnt/β(beta)-catenin pathway, including cyclin D1, is most commonly aberrant in endometrioid carcinomas
-
Mutations in CTNNB1, which correlate with immunohistochemical positivity for β(beta)-catenin, are commonly seen, and have been linked to squamous differentiation of the tumor
-
Cyclin D1 immunopositivity may also be seen
-
-
The PI3K/Akt2/PTEN pathway is also affected in these two tumor types, with PIK3CA abnormalities common in both, and PTEN mutations more common in endometrioid carcinomas
-
Of note, endometrioid carcinomas with PTEN mutations have been associated with a lower grade and a better prognosis
-
-
ARID1A is a putative tumor suppressor gene, aberrations in which can be seen in both tumor types, although they are more frequently associated with clear cell carcinomas
-
In ARID1A-mutated carcinomas, loss of the BAF250a protein is seen by immuno-histochemistry
-
-
Expression of HNF-1-β(beta) is relatively specific for clear cell carcinomas, and immunohistochemical staining for the protein therefore serves as a useful diagnostic tool
-
Microsatellite instability is particularly associated with endometrioid carcinomas, which are seen with increased frequency in patients with Lynch syndrome
-
A small percentage of clear cell carcinomas also demonstrate microsatellite instability
-
-
MAPK signaling pathway defects, namely mutations in KRAS and BRAF, may also be present in endometrioid and clear cell carcinomas
-
Although TP53 mutations are more frequently associated with type II tumors, they also occur in a significant number of high-grade endometrioid carcinomas
-
Clear cell carcinomas also demonstrate abnormalities in the gene PPP2R1A
-
Mucinous Tumors
-
Introduction
-
The category of ovarian mucinous tumors includes APMT and mucinous carcinoma, both of which are often unilateral and may grow to a large size prior to resection
-
Two types of APMT have been described: the gastrointestinal type and the endocervical-like or seromucinous type
-
The more common subtype is the gastrointestinal type, a generally multicystic tumor with an intestinal-type mucinous lining
-
Endocervical-like or seromucinous APMT demonstrates both mucinous and serous-type lining cells, and may also demonstrate endometrioid or eosinophilic epithelium
-
These tumors are more often bilateral and small, with an architecture resembling that of APST, and are more frequently associated with endometrioid and clear cell carcinomas
-
-
APMT may display architectural complexity
-
The presence of marked nuclear atypia without invasion warrants a diagnosis of mucinous intraepithelial carcinoma
-
The prognosis of these tumors is still favorable
-
-
Mucinous carcinomas, the majority of which are of the gastrointestinal type, are uncommon compared to other types of ovarian tumors
-
A well-differentiated architecture is typical, and grading is best determined based on nuclear features
-
Invasion in these tumors may be destructive and infiltrative or expansile
-
Mucinous carcinomas often coexist with adjacent APMT
-
-
-
Genetic pathways: functions, role in pathogenesis, and frequency of abnormalities
-
MAPK signaling pathway
-
KRAS (vi-Ki-ras2 Kirsten rat sarcoma 2 viral oncogene homolog) and BRAF (v-raf murine sarcoma viral oncogene homolog B1) are both members of the RAS–RAF–MEK–ERK–MAP kinase pathway (see section “Low-Grade Serous Tumors” above), and are also downstream activators of the EGFR pathway
-
Both KRAS and BRAF function as oncogenes
-
Frequency of mutations
-
KRAS mutations have been found in 13–33% of mucinous adenomas, 33–79% of mucinous borderline tumors, and 10–75% of mucinous carcinomas (Mok et al. 1993; Sieben et al. 2004)
-
Codon 12 is the most common site of mutation in the KRAS gene
-
BRAF mutations are relatively uncommon in mucinous tumors, found in up to 9% of mucinous carcinomas and not at all in mucinous borderline tumors (Mayr et al. 2006)
-
All BRAF mutations were found in exon 15, with most involving codon 600
-
As in other tumor types, KRAS and BRAF mutations have been found to be mutually exclusive in most cases
-
-
-
-
Clinical implications
-
KRAS mutations have been demonstrated to be more common in lower stage tumors, but no association with prognosis has been found
-
-
Summary
-
The most commonly mutated gene in mucinous tumors of the ovary is KRAS, with mutations found in adenomas, APMT, and carcinomas
-
BRAF mutations are much less common, but when present have been found to be mutually exclusive with KRAS mutations
-
Type II Ovarian Tumors
HGSC and MMMT
-
Introduction
-
HGSC is the most common type of ovarian cancer, and usually occurs in the sixth and seventh decades
-
Patients often present at an advanced stage, with abdominal and pelvic dissemination of tumor
-
Architecturally, these carcinomas are complex, with papillary, glandular, cribriform, and solid patterns; necrosis is common
-
High-grade cytology is seen, with marked nuclear atypia and high mitotic activity
-
Overall survival is generally poor
-
-
MMMT, or carcinosarcoma, is characterized by both epithelial and stromal malignant components
-
The epithelial component may be comprised of any ovarian carcinoma type, most often HGSC or endometrioid carcinoma
-
The stromal component demonstrates a sarcomatous appearance and may contain heterologous elements
-
The frequent expression of epithelial markers in the sarcomatous component, as well as the demonstration of monoclonality in these tumors, supports the idea that these are carcinomas with sarcomatoid differentiation
-
Some have referred to them as “metaplastic carcinomas”
-
-
HGSC and MMMT are discussed together in this section because of similar molecular aberrations, particularly in TP53, as well as their putative similar origin from STIC
-
-
-
Genetic pathways: functions, role in pathogenesis, and frequency of abnormalities
-
TP53
-
TP53 is a tumor suppressor gene located on chromosome 17p, encoding the transcription factor p53, which is involved in apoptosis
-
TP53 has frequently been found to be inactivated in diverse tumor types
-
-
Mutations in TP53 are the most common and significant molecular abnormality found in type II ovarian carcinomas
-
Frequency of mutations
-
Mutations in TP53 are found in 40–60% of all advanced ovarian cancer cases, and as many as 79% of all malignant ovarian or similar peritoneal epithelial tumors
-
Among pelvic (ovarian, tubal, and peritoneal) HGSC, more than 96% were found to have TP53 mutations, including tumors of low stage
-
Most were missense mutations in exons 4–8 (Cancer Genome Atlas Research Network 2011)
-
-
MMMT has also been found to have TP53 mutations, with identical mutations and LOH patterns in the carcinoma and sarcoma components
-
In two cases of MMMT arising in serous carcinoma, the MMMT was found to have the same TP53 mutation as the serous carcinoma, supporting the idea of the sarcomatous component arising from the carcinoma (Gallardo et al. 2002)
-
-
Immunohistochemical findings
-
The majority of malignant ovarian cancers are p53-immunopositive, with a significant correlation between immunopositivity and TP53 gene mutations
-
-
-
CDKN2/p16
-
The gene CDKN2 (also known as p16ink4 or MTS1), located on 9p21, encodes the cyclin-dependent kinase inhibitor p16
-
p16 is a tumor suppressor which binds cdk4 and cdk6, inhibiting the activity of the cdk4-6/cyclin D enzyme complex, which is required for the phosphorylation of Rb and resulting progression of the cell cycle
-
Immunohistochemical findings
-
Overexpression of p16 by immunohistochemical analysis has been found in the majority of HGSC, with 83.3% of these showing diffuse positivity, compared to less than 30% of LGSC (O’Neill et al. 2007)
-
Some groups have found differing results (see section on LGSC above); however, the diffuse expression of p16 by immunohistochemistry is still generally most consistent with HGSC
-
-
-
Telomere length
-
Telomeres are the noncoding ends of eukaryotic chromosomes, consisting of guanine-rich simple tandem repeats
-
Telomeres function to protect the chromosome from end to end fusions, exonuclease activity, and other damage
-
In normal cells, telomeres shorten with each replication cycle, eventually contributing to the onset of replicative senescence
-
In immortal cell lines, such as tumor cells, the enzyme telomerase is activated, functioning to maintain telomere length and allowing the cell to continue dividing indefinitely
-
Frequency of abnormalities
-
STIC has been found to have telomeres shorter than those of normal tubal epithelium in 82% of cases
-
This shortening of telomeres may be due to ovulation-induced oxidative stress, resulting in chromosomal instability and contributing to the development of STIC
-
Those STICs which acquire the ability to maintain telomere length may then progress to HGSC (Kuhn et al. 2010)
-
-
Most HGSC demonstrate shorter telomeres than the associated normal tubal epithelium
-
This is also true of metastatic malignant cells in ascites specimens compared to the accompanying benign cells (Counter et al. 1994)
-
-
Telomerase activity is seen more frequently and to a greater degree in invasive carcinomas compared to normal ovaries and benign and borderline serous tumors
-
Telomerase activity also helps distinguish malignant from benign cells in ascites specimens
-
-
-
Familial ovarian cancer: BRCA1 and BRCA2
-
Both BRCA1 and BRCA2 are tumor suppressor genes involved in DNA double-strand break repair
-
BRCA1, located on 17q21, and BRCA2, located on 13q12, have both been linked to a hereditary predisposition for breast cancer
-
Mutations in BRCA1 and BRCA2 have also been linked to ovarian cancers
-
It has been found that the majority of breast-ovarian cancer families carry BRCA1 mutations, and most of the remainder carry BRCA2 mutations
-
-
Frequency of abnormalities
-
Approximately 10–17% of ovarian cancer occurs in patients with a known predisposing genetic mutation, primarily BRCA1 and BRCA2, as well as Lynch syndrome (see above)
-
BRCA1 mutations particularly predispose to serous carcinoma, which comprises 90% of ovarian cancers in BRCA1 mutation carriers
-
These two genes and their related pathways may also play a role in sporadic cancers, which can be categorized into “BRCA1-like” and “BRCA2-like” based on gene expression profiles
-
Epigenetic effects or changes in downstream effectors of BRCA1 and BRCA2 may be responsible (Jazaeri et al. 2002)
-
-
Recent results from The Cancer Genome Atlas project have demonstrated somatic mutations in BRCA1 or BRCA2 in 3% of HGSC
-
11–31% of lost BRCA1 expression has been found to be due to DNA hypermethylation rather than mutation (Wang et al. 2004)
-
-
Alterations have also been found in other homologous recombination genes, with approximately half of all HGSC found to have homologous recombination defects
-
-
PI3K/Akt2/PTEN pathway
-
Abnormalities in this pathway are more commonly found in endometrioid and clear cell carcinomas (discussed previously)
-
However, the oncogenes Akt2 and PIK3CA are more frequently amplified in HGSC than in other tumor types
-
Frequency of abnormalities
-
HGSC is Akt2-amplified in 18.2–29% of cases (Park et al. 2006)
-
Normal ovarian tissue, benign tumors, borderline tumors, and LGSC show no amplification of the gene
-
-
Although PIK3CA mutations are infrequently seen in HGSC, PIK3CA amplifications are seen in approximately 13% of these tumors (Nakayama et al. 2006b)
-
-
-
MAPK
-
MAPK (mitogen-activated protein kinase) is most frequently expressed in low-grade serous tumors (see above) but has also been found in HGSC
-
Immunohistochemical findings
-
By immunohistochemical staining, activated (phosphorylated) MAPK was found to be expressed in 41% of HGSC (Hsu et al. 2004)
-
In contrast to LGSC, HGSC demonstrating MAPK expression all had wild-type KRAS and BRAF
-
-
-
Notch3
-
Notch receptors are membrane receptors which play a role in cell fate regulation, cell proliferation, and cell death during development
-
The Notch3 gene, located at 19p13.2, encodes one such Notch receptor
-
Frequency of abnormalities
-
Overexpression of Notch3 is more common in HGSC (amplification frequency of 19.5%, overexpression in 66%) vs. low-grade serous tumors and nonneoplastic epithelium (Park et al. 2006)
-
-
Immunohistochemical findings
-
-
Immunohistochemical staining for Notch3 (both nuclear and cytoplasmic) has been found in 55% of ovarian carcinomas but not in normal ovarian surface epithelium
-
The intensity of staining is correlated with the DNA copy ratio
-
-
HBXAP (Rsf-1)
-
The gene Rsf-1 (HBXAP, Hepatitis B virus x-associated protein), located at 11q13.5, encodes a protein which partners with hSNF2H to form the RSF complex; this complex is involved in chromatin remodeling
-
Frequency of abnormalities
-
Amplification of the 11q13.5 locus has been found in 13.2–15.7% of HGSC, with Rsf-1 found to have the most significantly amplified mRNA expression among genes at this locus
-
No amplification is seen in low-grade tumors and normal ovaries (Shih et al. 2005)
-
-
Immunohistochemical findings
-
Immunohistochemical staining for Rsf-1 correlates with the presence of gene amplification
-
A correlation has also been found between the intensity of Rsf-1 nuclear immunostaining and that for hSNF2H, with evidence suggesting that Rsf-1 may stabilize the hSNF2H protein (Sheu et al. 2008)
-
-
-
NAC1
-
NAC1 (nucleus accumbens 1), encoded by the gene NAC1 on 19p13, is a member of the BTB/POZ domain family, and contains a domain which may play a role in chromatin organization and transcription
-
The role of NAC1 in ovarian cancer pathogenesis may also be partly mediated by its negative regulation of the growth inhibitor Gadd45GIP1 (DNA-damage-inducible 45-gamma interacting protein)
-
Immunohistochemical findings
-
Immunopositivity for NAC1 is stronger in serous carcinomas than in benign tumors or normal ovaries, with high immunointensity seen more frequently in HGSC compared to LGSC
-
Higher staining intensity and mRNA levels were also found in recurrent tumors compared to primary tumors (Nakayama et al. 2006a )
-
-
-
HLA-G
-
HLA-G (human leukocyte antigen G) is a major histocompatibility (MHC) protein, the expression of which has been shown to facilitate evasion of immunosurveillance by tumor cells and has been linked to multiple nonovarian cancers
-
Immunohistochemical findings
-
By immunohistochemical analysis, 61% of HGSC have been found to express HLA-G, with a discrete membranous staining pattern
-
Expression has not been found in low-grade serous tumors or normal ovarian surface epithelium
-
-
By PCR analysis, the HLA-G isoforms 1 and 5 were found to predominate in HGSC (Singer et al. 2003a, 2003b)
-
-
Cyclin E1 (CCNE1)
-
Cyclin E, encoded by the gene CCNE1 at 19q13, is involved in promoting the progression of the cell cycle from S1 to G phase
-
Frequency of abnormalities
-
Amplification of the CCNE1 locus has been found to be specific for HGSC vs. LGSC or normal ovarian tissue, with a frequency of 32.2–36.1% (Nakayama et al. 2007a )
-
-
Immunohistochemical findings
-
High cyclin E1 expression by immunohistochemical analysis has been correlated with amplification of the CCNE1 gene (Farley et al. 2003)
-
-
-
-
Clinical implications
-
TP53
-
TP53 gene mutations and overexpression have been linked to cisplatin resistance, resulting from the inability of the mutated protein to activate apoptosis (Perego et al. 1996)
-
The evidence for the prognostic significance of TP53 mutations is still somewhat contradictory, with some evidence pointing to these mutations as a negative prognostic factor, others finding no correlation, and one study even finding a short-term survival benefit
-
Additional data is needed to more definitively define the role of p53 in prognosis
-
-
Immunohistochemical staining for p53 is useful in differentiating type I and type II tumors
-
Telomere length and telomerase activity
-
The increased telomerase activity seen in HGSC suggests a potential utility for telomerase inhibitors in treatment; several studies have explored this potential
-
The cytokine interferon-β(beta) (IFN-β(beta)), which inhibits tumor cell growth, was found to suppress telomerase activity in ovarian cancer cells (Lee et al. 2010)
-
Inhibition of hTERT (human telomerase reverse transcriptase), the major site of transcriptional regulation of the enzyme, has demonstrated rapid inhibition of growth in ovarian cancer cell lines (Luo et al. 2009)
-
-
-
-
BRCA1 and BRCA2
-
In comparison to women with sporadic ovarian cancer, those with BRCA1- and BRCA2-mutated cancers have better outcomes.
-
Patients with epigenetically silenced BRCA1 have survival similar to those with wild-type BRCA1
-
-
PARP1 (poly-ADP-ribose-polymerase) is a nuclear enzyme required for base excision repair of single-strand breaks
-
PARP inhibitors may have potential in treating patients with defects in DNA repair, including those with BRCA1 and BRCA2 mutations
-
-
-
PI3K/Akt2/PTEN pathway
-
Amplification of Akt2 has been associated with undifferentiated histology and with age over 50 years; a trend towards higher mortality is also observed
-
-
MAPK
-
Greater expression of MAPK is seen in high-grade tumors from younger patients (Hsu et al. 2004)
-
-
Notch3
-
Tumors with Notch3 overexpression may be amenable to targeted therapy, either by γ(gamma)-secretase inhibitors or by disruption of Notch3 and ligand binding
-
γ(gamma)-secretase inhibitors prevent activation of Notch3, and are found to inhibit proliferation and promote apoptosis in Notch3-expressing cancer cell lines
-
-
HBXAP (Rsf-1)
-
Rsf-1 may have prognostic significance, as patients with HGSC and Rsf-1 amplification demonstrate shorter overall survival compared to those with nonamplified tumors (Shih et al. 2005)
-
Implications for treatment also exist, with silencing of Rsf-1 in overexpressing cell lines resulting in a significant inhibition of growth, and expression of Rsf-1 in cell lines being associated with paclitaxel resistance (Choi et al. 2009)
-
-
NAC1
-
The intensity of NAC1 immunostaining was found to be predictive of recurrence within 1 year in patients with advanced stage HGSC status post optimal debulking and standard chemotherapy (Nakayama et al. 2006a )
-
NAC1 expression may also be associated with resistance to paclitaxel and resulting shorter survival in paclitaxel-treated patients
-
This resistance may be mediated by Gadd45GIP1, which is also a potential target for treatment (Jinawath et al. 2009)
-
-
-
HLA-G
-
An HLA-G-specific ELISA test has been developed to measure sHLA-G, a product of the HLA-G5 isoform
-
Using this test, sHLA-G was found in almost all malignant ascites samples and at significantly higher levels than in benign samples (Singer et al. 2003b), indicating potential use as a diagnostic tumor marker
-
-
HLA-G may also have prognostic implications, with an association between the presence of HLA-G-expressing tumor cells in effusions and better survival (Davidson et al. 2005)
-
-
Cyclin E1
-
High cyclin E1 expression has been associated with shorter median survival and an increased relative risk of death in women with advanced stage ovarian cancer status post suboptimal debulking (Farley et al. 2003)
-
-
-
Summary
-
Mutations in TP53 are the most common genetic abnormality in HGSC and in ovarian cancer overall
-
The presence of these mutations is helpful for diagnosis, and is thought to confer a worse prognosis, although data on the latter are somewhat contradictory
-
-
In MMMT, identical TP53 mutations have been found in both the epithelial and stromal components
-
p16 is commonly overexpressed in HGSC
-
The enzyme telomerase, expressed in a wide variety of tumors, is also found in ovarian carcinomas, and has demonstrated potential as a target for therapy
-
Expression of MAPK, although more common in type I tumors, may also be seen in HGSC
-
MAPK-expressing HGSC are wild type for KRAS and BRAF
-
-
Within the PI3K/Akt2/PTEN pathway, amplification of Akt2 is most associated with HGSC, and has been associated with undifferentiated histology and a worse prognosis.
-
PIK3CA amplification is also seen in HGSC
-
-
BRCA1 and BRCA2 are the genes responsible for most familial cases of breast and ovarian cancer
-
Patients with ovarian carcinomas in this setting have better outcomes than those with sporadic cancers
-
These genes and their related pathways may also be involved in sporadic cancers
-
-
Several other genetic abnormalities have also been described in HGSC, including overexpression of Notch3, HBXAP, NAC1, HLA-G, and Cyclin E
-
Many of these abnormalities have diagnostic and therapeutic relevance, as discussed above
-
-
Molecular Abnormalities not Associated with Specific Histology
-
EGFR family
-
The EGFR (epidermal growth factor receptor) family, also known as the ERBB or HER family, is a group of transmembrane receptors which include both EGFR and HER2 (ERBB2)
-
Activation of EGFR family receptors by ligand binding leads to the activation of multiple different signaling pathways, including MAPK and PI3K/Akt2/PTEN, with resulting effects on cell survival, proliferation, and differentiation (Fig. 7.2)
Fig. 7.2 Interaction of pathways involved in the pathogenesis of LGSC and other type I tumors. (Reprinted from Human Pathology, Kurman and Shih (2011), with permission from Elsevier)
-
Frequency of abnormalities
-
Amplification of EGFR has been found in up to 22% of ovarian cancers overall (Stadlmann et al. 2006)
-
Activating mutations may also be seen
-
-
Amplifications of HER2 have been found in 23% of borderline tumors and 8–66% of ovarian carcinomas, both of various subtypes (Ross et al. 1999)
-
No correlation has generally been found between gene amplification and tumor type, stage, or grade
-
-
-
Immunohistochemical findings
-
EGFR expression by immunohistochemistry has been found in as many as 64.5% of invasive ovarian carcinomas overall, including mucinous, serous, and endometrioid carcinomas (Vermeij et al. 2008)
-
-
Clinical implications
-
There may be a role for EGFR inhibitors in patients with EGFR mutations, although the evidence remains unclear
-
The response rate has been relatively low (Gordon et al. 2005), possibly due to the fact that the mutations most often found in ovarian cancers are not the same as those found in non-small cell lung cancers
-
-
EGFR expression has been associated with poor outcome in multiple studies, as well as with higher tumor grade, abnormal TP53 expression, larger residual tumor size, and a higher proliferation index
-
The finding of a greater frequency of HER2 amplification in higher stage tumors in one study suggests that this may be a marker of poor prognosis (Afify et al. 1999)
-
Trastuzumab and pertuzumab are monoclonal anti-HER2 antibodies commonly used in the treatment of HER2-amplified breast cancer
-
In ovarian cancer, overall response rates for these two drugs individually have been relatively low, but recent evidence suggests a potentially greater response rate using both in combination (Faratian et al. 2011)
-
-
-
-
DNA methylation
-
DNA methylation is an epigenetic alteration which has been shown to occur aberrantly in a wide variety of human neoplasms
-
Global hypomethylation results in the activation of oncogenes, while tumor suppressor genes can be silenced via hypermethylation of CpG islands within their promoter regions
-
Hypermethylation of various genes has been described in ovarian cancers
-
For example, promoter hypermethylation of specific genes (CDKN2, E-cadherin, RAR-β(beta), H-cadherin, APC, GSTP1, MGMT, and RASSF1A) increases in frequency from benign cystadenomas to invasive carcinomas
-
-
Hypomethylation has also been shown to progressively increase from nonneoplastic ovarian tissue to carcinoma
-
Other examples of aberrant methylation status have been discussed earlier in relation to specific genetic loci
-
Clinical implications
-
The detection of DNA methylation status has promising potential as a screening tool, particularly with the development of sensitive assays to detect the methylation status of multiple genes, and the potential to detect biomarkers in fluids draining the tumor site
-
Strong hypomethylation in ovarian cancer tissue has been associated with advanced stage and high grade
-
-
Conclusions
-
Studies of the molecular characteristics of ovarian cancer have led to numerous new insights into the pathophysiology of this disease
-
Differences in the involved molecular pathways have supported the division of epithelial ovarian cancers into type I tumors, which are slow-growing tumors thought to develop in a stepwise manner from benign and borderline precursors, and type II tumors, which are more aggressive and arise in a de novo fashion
-
Although there is much overlap in the molecular pathways involved in the various ovarian tumor types, each histologic type is associated with certain characteristic abnormalities
-
These insights into the specific aberrations present in each ovarian cancer histotype have translated into insights on new diagnostic, therapeutic, and prognostic modalities
-
Continued efforts to better understand the molecular characteristics of ovarian cancer promise to offer further insights into its pathophysiology and best clinical management, with the hopes of ultimately reducing the burden of this high-mortality disease
References
Abeln EC, Smit VT, Wessels JW, et al. Molecular genetic evidence for the conversion hypothesis of the origin of malignant mixed müllerian tumours. J Pathol. 1997;183:424–31.
Afify AM, Werness BA, Mark HF. HER2/neu oncogene amplification in stage I and stage III ovarian papillary serous carcinoma. Exp Mol Pathol. 1999;66:163–9.
Ahmed AA, Etemadmoghadam D, Temple J, et al. Driver mutations in TP53 are ubiquitous in high grade serous carcinoma of the ovary. J Pathol. 2010;221:49–56.
Auner V, Kriegshäuser G, Tong D, et al. KRAS mutation analysis in ovarian samples using a high sensitivity biochip assay. BMC Cancer. 2009;9:111.
Barton CA, Hacker NF, Clark SJ, et al. DNA methylation changes in ovarian cancer: implications for early diagnosis, prognosis and treatment. Gynecol Oncol. 2008; 109:129–39.
Bellacosa A, de Feo D, Godwin AK, et al. Molecular alterations of the AKT2 oncogene in ovarian and breast carcinomas. Int J Cancer. 1995;64(4):280–5.
Berchuck A, Kohler MF, Marks JR, et al. The p53 tumor suppressor gene frequently is altered in gynecologic cancers. Obstet Gynecol. 1994;170:246–52.
Bookman MA, Darcy KM, Clarke-Pearson D, et al. Evaluation of monoclonal humanized anti-HER2 antibody, trastuzumab, in patients with recurrent or refractory ovarian or primary peritoneal carcinoma with overexpression of HER2: a phase II trial of the gynecologic oncology group. J Clin Oncol. 2003;21: 283–90.
Campbell IG, Russell SE, Choong DY, et al. Mutation of the PIK3CA gene in ovarian and breast cancer. Cancer Res. 2004;64:7678–81.
Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011; 474:609–15.
Catasús L, Bussaglia E, Rodrguez I, et al. Molecular genetic alterations in endometrioid carcinomas of the ovary: similar frequency of beta-catenin abnormalities but lower rate of microsatellite instability and PTEN alterations than in uterine endometrioid carcinomas. Hum Pathol. 2004;35:1360–8.
Chetrit A, Hirsh-Yechezkel G, Ben-David Y, et al. Effect of BRCA1/2 mutations on long-term survival of patients with invasive ovarian cancer: the National Israeli Study of Ovarian Cancer. J Clin Oncol. 2008;26:20–5.
Cho KR. Ovarian cancer update: lessons from morphology, molecules, and mice. Arch Pathol Lab Med. 2009;133:1775–81.
Choi JH, Sheu JJ, Guan B, et al. Functional analysis of 11q13.5 amplicon identifies rsf-1 (HBXAP) as a gene involved in paclitaxel resistance in ovarian cancer. Cancer Res. 2009;69:1407–15.
Counter CM, Hirte HW, Bacchetti S, et al. Telomerase activity in human ovarian carcinoma. Proc Natl Acad Sci U S A. 1994;91:2900–4.
Datar RH, Naritoku WY, Li P, et al. Analysis of telomerase activity in ovarian cystadenomas, low-malignant-potential tumors, and invasive carcinomas. Gynecol Oncol. 1999;74:338–45.
Davidson B, Elstrand MB, McMaster MT, et al. HLA-G expression in effusions is a possible marker of tumor susceptibility to chemotherapy in ovarian carcinoma. Gynecol Oncol. 2005;96:42–7.
Despierre E, Lambrechts D, Neven P, et al. The molecular genetic basis of ovarian cancer and its roadmap towards a better treatment. Gynecol Oncol. 2010; 117:358–65.
Dimova I, Zaharieva B, Raitcheva S, et al. Tissue microarray analysis of EGFR and erbB2 copy number changes in ovarian tumors. Int J Gynecol Cancer. 2006;16: 145–51.
Drew Y, Calvert H. The potential of PARP inhibitors in genetic breast and ovarian cancers. Annals of the New York Academy of Sciences. 2008;1138:136–45.
Faratian D, Zweemer AJ, Nagumo Y, et al. Trastuzumab and pertuzumab produce changes in morphology and estrogen receptor signaling in ovarian cancer xenografts revealing new treatment strategies. Clin Cancer Res. 2011;17:4451–61.
Farley J, Smith LM, Darcy KM, et al. Cyclin E expression is a significant predictor of survival in advanced, suboptimally debulked ovarian epithelial cancers: a gynecologic oncology group study. Cancer Res. 2003;63: 1235–41.
Fujita M, Enomoto T, Yoshino K, et al. Microsatellite instability and alterations in the hMSH2 gene in human ovarian cancer. Int J Cancer. 1995;64:361–6.
Gallardo A, Matias-Guiu X, Lagarda H, et al. Malignant müllerian mixed tumor arising from ovarian serous carcinoma: a clinicopathologic and molecular study of two cases. Int J Gynecol Pathol. 2002;21:268–72.
Gamallo C, Palacios J, Moreno G, et al. Beta-catenin expression pattern in stage I and II ovarian carcinomas: relationship with beta-catenin gene mutations, clinicopathological features, and clinical outcome. Am J Pathol. 1999;155:527–36.
Gemignani ML, Schlaerth AC, Bogomolniy F, et al. Role of KRAS and BRAF gene mutations in mucinous ovarian carcinoma. Gynecol Oncol. 2003;90(2): 378–81.
Gordon AN, Finkler N, Edwards RP, et al. Efficacy and safety of erlotinib HCl, an epidermal growth factor receptor (HER1/EGFR) tyrosine kinase inhibitor, in patients with advanced ovarian carcinoma: results from a phase II multicenter study. Int J Gynecol Cancer. 2005;15:785–92.
Gordon MS, Matei D, Aghajanian C, et al. Clinical activity of pertuzumab (rhuMAb 2C4), a HER dimerization inhibitor, in advanced ovarian cancer: potential predictive relationship with tumor HER2 activation status. J Clin Oncol. 2006;24:4324–32.
Gras E, Catasús L, Arguelles R, et al. Microsatellite instability, MLH-1 promoter hypermethylation, and frameshift mutations at coding mononucleotide repeat microsatellites in ovarian tumors. Cancer. 2001;92:2829–36.
Hall J, Paul J, Brown R. Critical evaluation of p53 as a prognostic marker in ovarian cancer. Expert Rev Mol Med. 2004;6:1–20.
Havrilesky L, Darcy KM, Hamdan H, et al. Prognostic significance of p53 mutation and p53 overexpression in advanced epithelial ovarian cancer: a gynecologic oncology group study. J Clin Oncol. 2003;21:3814–25.
Ho CL, Kurman RJ, Dehari R, et al. Mutations of BRAF and KRAS precede the development of ovarian serous borderline tumors. Cancer Res. 2004;64:6915–8.
Hsu CY, Bristow R, Cha MS, et al. Characterization of active mitogen-activated protein kinase in ovarian serous carcinomas. Clin Cancer Res. 2004;10:6432–6.
Ishibashi M, Nakayama K, Yeasmin S, et al. A BTB/POZ gene, NAC-1, a tumor recurrence-associated gene, as a potential target for taxol resistance in ovarian cancer. Clin Cancer Res. 2008;14:3149–55.
Jazaeri AA, Yee CJ, Sotiriou C, et al. Gene expression profiles of BRCA1-linked, BRCA2-linked, and sporadic ovarian cancers. J Natl Cancer Inst. 2002;94: 990–1000.
Jinawath N, Vasoontara C, Yap KL, et al. NAC-1, a potential stem cell pluripotency factor, contributes to paclitaxel resistance in ovarian cancer through inactivating Gadd45 pathway. Oncogene. 2009;28:1941–8.
Jones S, Wang TL, Shih I, et al. Frequent mutations of chromatin remodeling gene ARID1A in ovarian clear cell carcinoma. Science. 2010;330:228–31.
Kato N, Tamura G, Motoyama T. Hypomethylation of hepatocyte nuclear factor-1beta (HNF-1beta) CpG island in clear cell carcinoma of the ovary. Virchows Arch. 2008;452:175–80.
Kindelberger DW, Lee Y, Miron A, et al. Intraepithelial carcinoma of the fimbria and pelvic serous carcinoma: evidence for a causal relationship. Am J Surg Pathol. 2007;31:161–9.
Kounelis S, Jones MW, Papadaki H, et al. Carcinosarcomas (malignant mixed müllerian tumors) of the female genital tract: comparative molecular analysis of epithelial and mesenchymal components. Hum Pathol. 1998;29:82–7.
Kuhn E, Meeker A, Wang TL, et al. Shortened telomeres in serous tubal intraepithelial carcinoma: an early event in ovarian high-grade serous carcinogenesis. Am J Surg Pathol. 2010;34:829–36.
Kupryjanczyk J, Thor AD, Beauchamp R, et al. p53 gene mutations and protein accumulation in human ovarian cancer. Proc Natl Acad Sci U S A. 1993;90:4961–5.
Kurman RJ, Shih I. The origin and pathogenesis of epithelial ovarian cancer: a proposed unifying theory. Am J Surg Pathol. 2010;34:433–43.
Kurman RJ, Shih I. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer–shifting the paradigm. Hum Pathol. 2011;42:918–31.
Lassus H, Sihto H, Leminen A, et al. Gene amplification, mutation, and protein expression of EGFR and mutations of ERBB2 in serous ovarian carcinoma. J Mol Med (Berl). 2006;84:671–81.
Lee JH, Lee SY, Lee JH, et al. p21 WAF1 is involved in interferon-beta-induced attenuation of telomerase activity and human telomerase reverse transcriptase (hTERT) expression in ovarian cancer. Mol Cells. 2010;30:327–33.
Luo Y, Yi Y, Yao Z. Growth arrest in ovarian cancer cells by hTERT inhibition short-hairpin RNA targeting human telomerase reverse transcriptase induces immediate growth inhibition but not necessarily induces apoptosis in ovarian cancer cells. Cancer Invest. 2009; 27:960–70.
Makarla PB, Saboorian MH, Ashfaq R, et al. Promoter hypermethylation profile of ovarian epithelial neoplasms. Clin Cancer Res. 2005;11:5365–9.
Marquez RT, Baggerly KA, Patterson AP, et al. Patterns of gene expression in different histotypes of epithelial ovarian cancer correlate with those in normal fallopian tube, endometrium, and colon. Clin Cancer Res. 2005;11:6116–26.
Mayr D, Hirschmann A, Löhrs U, Diebold J. KRAS and BRAF mutations in ovarian tumors: a comprehensive study of invasive carcinomas, borderline tumors and extraovarian implants. Gynecol Oncol. 2006;103: 883–7.
Medeiros F, Muto MG, Lee Y, et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am J Surg Pathol. 2006;30:230–6.
Mok SC, Bell DA, Knapp RC, et al. Mutation of K-ras protooncogene in human ovarian epithelial tumors of borderline malignancy. Cancer Res. 1993;53:1489–92.
Moreno-Bueno G, Gamallo C, Perez-Gallego L, et al. Beta-catenin expression pattern, beta-catenin gene mutations, and microsatellite instability in endometrioid ovarian carcinomas and synchronous endometrial carcinomas. Diagn Mol Pathol. 2001;10:116–22.
Nakayama K, Nakayama N, Davidson B, et al. A BTB/POZ protein, NAC-1, is related to tumor recurrence and is essential for tumor growth and survival. Proc Natl Acad Sci U S A. 2006a;103:18739–44.
Nakayama K, Nakayama N, Kurman RJ, et al. Sequence mutations and amplification of PIK3CA and AKT2 genes in purified ovarian serous neoplasms. Cancer Biol Ther. 2006b;5:779–85.
Nakayama K, Nakayama N, Jinawath N, et al. Amplicon profiles in ovarian serous carcinomas. Int J Cancer. 2007a;120:2613–7.
Nakayama K, Nakayama N, Wang TL, et al. NAC-1 controls cell growth and survival by repressing transcription of Gadd45GIP1, a candidate tumor suppressor. Cancer Res. 2007b;67:8058–64.
Nazlioglu HO, Ercan I, Bilgin T, et al. Expression of p16 in serous ovarian neoplasms. Eur J Gynaecol Oncol. 2010;31:312–4.
Obata K, Morland SJ, Watson RH, et al. Frequent PTEN/MMAC mutations in endometrioid but not serous or mucinous epithelial ovarian tumors. Cancer Res. 1998;58:2095–7.
O’Neill CJ, McBride HA, Connolly LE, et al. High-grade ovarian serous carcinoma exhibits significantly higher p16 expression than low-grade serous carcinoma and serous borderline tumour. Histopathology. 2007;50: 773–9.
Park JT, Li M, Nakayama K, et al. Notch3 gene amplification in ovarian cancer. Cancer Res. 2006;66: 6312–8.
Peiro G, Diebold J, Mayr D, et al. Prognostic relevance of hMLH1, hMSH2, and BAX protein expression in endometrial carcinoma. Mod Pathol. 2001;14: 777–83.
Perego P, Giarola M, Righetti SC, et al. Association between cisplatin resistance and mutation of p53 gene and reduced bax expression in ovarian carcinoma cell systems. Cancer Res. 1996;56:556–62.
Piek JM, van Diest PJ, Zweemer RP, et al. Dysplastic changes in prophylactically removed fallopian tubes of women predisposed to developing ovarian cancer. J Pathol. 2001;195:451–6.
Pohl G, Ho CL, Kurman RJ, et al. Inactivation of the mitogen-activated protein kinase pathway as a potential target-based therapy in ovarian serous tumors with KRAS or BRAF mutations. Cancer Res. 2005;65: 1994–2000.
Rahman N, Stratton MR. The genetics of breast cancer susceptibility. Annu Rev Genet. 1998;32:95–121.
Ross JS, Yang F, Kallakury BV, et al. HER2/neu oncogene amplification by fluorescence in situ hybridization in epithelial tumors of the ovary. Am J Clin Pathol. 1999;111:311–6.
Rubin SC, Blackwood MA, Bandera C, et al. BRCA1, BRCA2, and hereditary nonpolyposis colorectal cancer gene mutations in an unselected ovarian cancer population: relationship to family history and implications for genetic testing. Am J Obstet Gynecol. 1998;178:670–7.
Sato N, Tsunoda H, Nishida M, et al. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 2000;60:7052–6.
Schilder RJ, Sill MW, Chen X, et al. Phase II study of gefitinib in patients with relapsed or persistent ovarian or primary peritoneal carcinoma and evaluation of epidermal growth factor receptor mutations and immunohistochemical expression: a gynecologic oncology group study. Clin Cancer Res. 2005;11:5539–48.
Schlosshauer PW, Deligdisch L, Penault-Llorca F, et al. Loss of p16INK4A expression in low-grade ovarian serous carcinomas. Int J Gynecol Pathol. 2011;30:22–9.
Seidman JD, Yemelyanova A, Zaino RJ, et al. The fallopian tube-peritoneal junction: a potential site of carcinogenesis. Int J Gynecol Pathol. 2011;30:4–11.
Sheu JJ, Choi JH, Yildiz I, et al. The roles of human sucrose nonfermenting protein 2 homologue in the tumor-promoting functions of rsf-1. Cancer Res. 2008;68:4050–7.
Shih I, Davidson B. Pathogenesis of ovarian cancer: clues from selected overexpressed genes. Future Oncol. 2009;5:1641–57.
Shih I, Kurman RJ. Ovarian tumorigenesis: a proposed model based on morphological and molecular genetic analysis. Am J Pathol. 2004;164:1511–8.
Shih I, Sheu JJ, Santillan A, et al. Amplification of a chromatin remodeling gene, rsf-1/HBXAP, in ovarian carcinoma. Proc Natl Acad Sci USA. 2005;102:14004–9.
Sieben NL, Macropoulos P, Roemen GM, et al. In ovarian neoplasms, BRAF, but not KRAS, mutations are restricted to low-grade serous tumours. J Pathol. 2004; 202:336–40.
Siegel R, Ward E, Brawley O, et al. Cancer statistics, 2011. CA Cancer J Clin. 2011;61:212–36.
Singer G, Kurman RJ, Chang HW, et al. Diverse tumorigenic pathways in ovarian serous carcinoma. Am J Pathol. 2002;160:1223–8.
Singer G, Oldt III R, Cohen Y, et al. Mutations in BRAF and KRAS characterize the development of low-grade ovarian serous carcinoma. J Natl Cancer Inst. 2003a;95:484–6.
Singer G, Rebmann V, Chen YC, et al. HLA-G is a potential tumor marker in malignant ascites. Clin Cancer Res. 2003b;9:4460–4.
Stadlmann S, Gueth U, Reiser U, et al. Epithelial growth factor receptor status in primary and recurrent ovarian cancer. Mod Pathol. 2006;19:607–10.
Sui L, Tokuda M, Ohno M, et al. The concurrent expression of p27(kip1) and cyclin D1 in epithelial ovarian tumors. Gynecol Oncol. 1999;73:202–9.
Tafe LJ, Garg K, Chew I, et al. Endometrial and ovarian carcinomas with undifferentiated components: clinically aggressive and frequently underrecognized neoplasms. Mod Pathol. 2010;23:781–9.
Tsuchiya A, Sakamoto M, Yasuda J, et al. Expression profiling in ovarian clear cell carcinoma: identification of hepatocyte nuclear factor-1 beta as a molecular marker and a possible molecular target for therapy of ovarian clear cell carcinoma. Am J Pathol. 2003;163:2503–12.
Vermeij J, Teugels E, Bourgain C, et al. Genomic activation of the EGFR and HER2/neu genes in a significant proportion of invasive epithelial ovarian cancers. BMC Cancer. 2008;8:3.
Wang C, Horiuchi A, Imai T, et al. Expression of BRCA1 protein in benign, borderline, and malignant epithelial ovarian neoplasms and its relationship to methylation and allelic loss of the BRCA1 gene. J Pathol. 2004;202: 215–23.
Wang J, Zhou JY, Wu GS. Bim protein degradation contributes to cisplatin resistance. J Biol Chem. 2011;286: 22384–92.
Wen WH, Reles A, Runnebaum IB, et al. p53 mutations and expression in ovarian cancers: correlation with overall survival. Int J Gynecol Pathol. 1999;18:29–41.
Widschwendter M, Jiang G, Woods C, et al. DNA hypomethylation and ovarian cancer biology. Cancer Res. 2004;64:4472–80.
Wiegand KC, Shah SP, Al-Agha OM, et al. ARID1A mutations in endometriosis-associated ovarian carcinomas. N Engl J Med. 2010;363:1532–43.
Willner J, Wurz K, Allison KH, et al. Alternate molecular genetic pathways in ovarian carcinomas of common histological types. Hum Pathol. 2007;38:607–13.
Wu R, Zhai Y, Fearon ER, et al. Diverse mechanisms of beta-catenin deregulation in ovarian endometrioid adenocarcinomas. Cancer Res. 2001;61:8247–55.
Wu R, Hendrix-Lucas N, Kuick R, et al. Mouse model of human ovarian endometrioid adenocarcinoma based on somatic defects in the Wnt/beta-catenin and PI3K/Pten signaling pathways. Cancer Cell. 2007;11:321–33.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Maniar, K.P., Shih, IM., Kurman, R.J. (2013). Molecular Pathology of Ovarian Cancer. In: Cheng, L., Eble, J. (eds) Molecular Surgical Pathology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4900-3_7
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4900-3_7
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4899-0
Online ISBN: 978-1-4614-4900-3
eBook Packages: MedicineMedicine (R0)