Abstract
For most clinicians managing a patient with encephalitis will be an infrequent event. The range of differential diagnoses in a child presenting with a clinical syndrome that could be encephalitis is broad. In addition, there are many pathogens that can cause encephalitis. In view of these facts, a systematic approach to clinical assessment, investigation and treatment, based on epidemiology and an understanding the limits of investigations, is crucial to effective management of this condition. This review focuses on encephalitis aetiology and investigation; HSV encephalitis; mycoplasma encephalitis; and flavivirus encephalitis as a globally important cause of disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- West Nile Virus
- Central Nervous System Infection
- Japanese Encephalitis
- Viral Encephalitis
- Intravenous Acyclovir
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
10.1 Introduction
Encephalitis presents several challenges to the clinician. Firstly. the presenting signs and symptoms of central nervous system (CNS) disease (e.g. altered consciousness/behaviour, seizures, focal neurology) and infection (e.g. fever, rash) are common to a wide variety of non-infectious and infectious conditions which are hard to distinguish on clinical grounds alone. Secondly, the pathogens able to cause encephalitis are numerous. Finally, at presentation children are usually becoming progressively more unwell and may have significant neurological and respiratory compromise for which timely intervention and support will prevent secondary damage.
In view of these facts a systematic approach to clinical assessment, investigation and treatment, based on epidemiology and an understanding the limits of investigations, is crucial to the effective management of this condition. This short review will focus on encephalitis aetiology and investigation, HSV encephalitis (due to its prevalence and the existence of treatment), mycoplasma encephalitis (frequently implicated in encephalitis but for which there are significant uncertainties around pathogenesis and treatment), flavivirus encephalitis (as a globally important cause of disease) and ‘Louping ill’ (out of local interest) .
Several comprehensive reviews of childhood encephalitis have been published recently [1, 2] and recommendations on investigation and management produced in the US and UK [3, 4].
10.2 Regional Epidemiology Together with a History of Travel, Immunisation Status, Immune Compromise and Animal Exposure Guides Initial Investigation
Although viral causes are most common, encephalitis or encephalitis-like syndromes can also be caused by bacteria, mycobacteria, fungi and parasites .
UK and North American studies demonstrate the importance of the following pathogens in childhood encephalitis (treatable causes are underlined) [5−7]: | |
1. | Herpes viruses (HSV , VZV, EBV) |
2. | Respiratory viruses (e.g. influenza, para-influenza, adenovirus) |
3. | Enteroviruses |
4. | Mycoplasma pneumoniae |
A history of travel, lack of immunisation, immune compromise and animal exposure extends this list to include: | |
5. | Lack of immunisation—Measles, mumps |
6. | Travel—Arboviruses (e.g. Japanese encephalitis, West Nile virus, tick borne encephalitis; St Louis encephalitis) |
7. | Immunocompromise —HIV, Listeria, Toxoplasma, CMV, HHV6, JC, Cryptococcus |
8. | Animal exposure—Borrelia burgdorferi, Rabies, Bartonella henselae (Cat-scratch disease) |
Other pathogens may cause clinical syndromes very similar to encephalitis and these, although usually considered separately, are an important consideration in the differential diagnosis of treatable causes. Such pathogens include; bacteria causing meningitis (or a meningo-encephalitis) such as Streptococcus pneumoniae, Neisseria meningitidis and Haemophilus influenzae; Plasmodium falciparum causing malaria; Mycobacterium tuberculosis causing TB meningitis.
The relative importance of these pathogens varies by region of the world and season [8]. In central, northern and eastern Europe, tick borne encephalitis is the a prevalent pathogen associated with encephalitis. In areas of South-East Asia, such as Vietnam, Japanese encephalitis predominates. Such is the importance of tick borne encephalitis and Japanese encephalitis in these regions that in some countries, vaccines against these pathogens are part of the routine immunisation schedule.
Whilst not exhaustive, the above list, combined with a full history, allows investigation for the pathogen causing encephalitis to be focused on the most likely organisms. However it is important to note that even with extensive investigation no definite pathogen is identified in a significant proportion of cases [5, 9, 10].
Of the many organisms causing encephalitis only a limited number have specific treatment (these are highlighted in the list above). Despite the prevalence of arboviruses in many regions of the world there is currently little to support specific treatment for any of these organisms. There is a single case report of an individual surviving rabies associate with a specific intensive care unit based treatment protocol but this is the exception and has not been replicated [11].
10.3 Initial Investigation and Empirical Treatment should be Focussed on Non-infectious Differential Diagnoses Together with Common or Treatable Infectious Causes
The extent of investigation will depend on resources available and region. Confirmation of encephalitis is based on the combination of findings from cerebrospinal fluid (CSF) microscopy, CNS imaging, identification of a specific pathogen (e.g. HSV from CSF PCR) and in some cases EEG. The importance of investigation for non-infectious causes lies in the lack of specificity of the initial presenting clinical syndrome and the wide variety of other treatable causes (Table 10.1). Various guidelines have been published and the list of first-line investigations used in one UK centre, for the child presenting with encephalopathy which may be encephalitis, is given here (Table 10.2).
Empirical anti-microbial treatment should include cover for likely bacterial pathogens causing CNS infection . In the UK, penicillin would cover N. meningitidis and most S. pneumoniae, however the possibility of H. influenzae, Staphylococcus aureus, penicillin resistant S. pneumoniae and Gram negative pathogens means that a third generation cephalosporin (eg ceftriaxone) is indicated. For the severely unwell child it is reasonable to cover Listeria with amoxicillin until the clinical picture is clearer as, although rare, it is described in immunocompetent children. High dose intravenous acyclovir treatment is mandatory for any child with suspected encephalitis. Other treatments depend on the specific history and risk factors for the individual case.
10.4 HSV Encephalitis is Treatable but Still Problematic
HSV is the commonest non-seasonal cause of encephalitis (HSVE) and is treatable. Despite this HSV often provides the clinician with diagnostic and therapeutic dilemmas. The outcome of HSVE in the pre-acyclovir era was devastating, with a mortality of 70 % and neuro-disability almost the rule amongst survivors. In 1986 a comparison of 10 days of acyclovir demonstrated a significantly improved outcome in comparison to vidarabine [12]. Of 69 individuals recruited to the trial the mortality in the 32 randomised to acyclovir treatment was 28 % versus 54 % in the vidarabine group. Of the survivors, 38 % in the acyclovir group versus 14 % in the vidarabine group were ‘functioning normally’. In these trials the duration of treatment was 10 days and there were no relapses. However one of the authors of this study noted that ‘many patients were still febrile at the conclusion of treatment suggesting that a longer duration of therapy …may be advisable’ [13]. Relapses of patients treated with acyclovir have been reported and in addition neonatal trials indicated the improved outcomes of 21 days of treatment versus 10 days (although the latter group also had a lower dose of acyclovir) [14]. These factors have led to the current recommendations for treatment duration of 14–21 days. The major modifiable factor associated with poor outcome in HSVE is now delay in starting acyclovir and clinicians should have a low threshold for starting acyclovir in any child with a compatible syndrome.
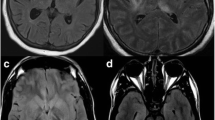
Detection of HSV DNA on PCR testing of CSF is the current ‘gold standard’ of diagnosis. However a negative CSF PCR is found in a number of children in the early stages of disease (see Table 10.3). Diagnostic work-up should therefore include an LP at least 72 h after the onset of symptoms even if this means a repeat LP for children who presented at < 72 h. An important issue is that a number of children with subsequently proven HSV will have a normal CSF white cell count [15]. Whilst scanning is usually abnormal in HSVE, this may not be the case early in the course of the illness particularly with CT [16]. A wide variety of imaging findings have been described from the classic fronto-temporal lesions through to more diffuse lesions. The decision to discontinue acyclovir treatment in a child with an encephalitis-like illness needs to be considered in the light of these diagnostic uncertainties and should be based on clinical recovery together with (i) normal MRI, (ii) negative CSF PCR at > 72 h post-onset of symptoms and negative EEG [1]. In practice if all of these investigations are normal and there is complete recovery then discontinuing acyclovir around 10 days may be considered in that the risk of HSVE is relatively low and a course of treatment has been given that was shown to be efficacious in the original trials. If there are significant clinical, CSF, MRI or EEG abnormalities consistent with HSVE, and no alternative diagnosis, then a full 21-day course of treatment is warranted despite a negative CSF PCR [1, 17]. An algorithm to facilitate the decision to discontinue acyclovir treatment has been described previously [17] and this issue is discussed in detail in a recent review of childhood encephalitis [1].
With sensitive CSF PCR testing, cases of possible HSVE may be identified in clinical settings where the illness appears very mild compared to typical HSVE or there are possible alternative diagnoses [18]. Whilst it has been speculated that some of these may be reactivation, of what is a persistent neurotropic virus, identification of HSV in CSF remains a clear indication for a full course of acyclovir treatment.
The availability of valaciclovir, a highly bioavailable alternative to intravenous acyclovir, has prompted some discussion about its role in treating invasive HSV disease . This is particularly relevant where a prolonged course of intravenous treatment requires secure venous access which in some cases can become more challenging as treatment progresses. There is a case report of oral valaciclovir use in one child with confirmed HSVE during the last week [19] and an uncontrolled series of cases from Vietnam treated with oral valaciclovir [20]. In the latter six individuals with confirmed HSVE were treated with oral valaciclovir and two died (days 2 and 3) whilst the other four completed treatment. These four had negative CSF PCRs by day 10 and CSF aciclovir concentrations were considered to be therapeutic, although levels fell with increasing duration of treatment. At present this agent cannot be recommended at any stage of treatment of HSVE.
Even with acyclovir there are still significant sequelae to HSVE and adjunctive treatments have been considered. Steroids have been associated with clinical recovery in some case reports [21] and improved outcomes in some case series [22]. A randomised trial is currently in progress in Europe [23] . At the present time corticosteroids remain of unproven benefit in HSVE.
10.5 Mycoplasma pneumoniae is Frequently Identified in the Setting of Encephalitis
M. pneumoniae is a common respiratory tract infection in childhood and is associated with a wide variety of neurological complications including encephalitis. In some studies of encephalitis M. pneumoniae has accounted for 5–13 % of cases [24, 25]. It’s relative rarity in other studies may relate to limitations of current diagnostic methods [26] and also the occurrence of disease in cycles (3–4 years in the UK) longer than most epidemiological studies [27]. The detection of organisms via culture or PCR in CSF suggests that direct invasion of the central nervous system plays an important role in pathogenesis in at least some individuals [24, 26]. However immunological mechanisms are likely to be important in many children including cases of ADEM [28]. In most centres testing is limited to serology whose limited specificity and sensitivity reduces the ability to determine the role of this agent in encephalitis. In one of the most detailed case series, PCR identified M. pneumoniae DNA in CSF, or in throat swabs in conjunction with positive serological evidence of infection, in almost 7 % of cases of childhood encephalitis (11 out of 159 children) [24]. Around two-thirds of these children had significant neurological sequelae at follow-up. In a further 25 % of cases of encephalitis there was evidence for a possible role of M. pneumoniae although many of these children also had other pathogens detected as well. Not all children had a respiratory prodrome and the lack of such a prodrome was associated with the detection of M. pneumoniae by PCR in the CSF (rather than confirmation by serology with a negative CSF PCR) . Given the evidence regarding neurological sequelae it is reasonable to consider empirical treatment for M. pneumoniae in settings and seasons where infection is common. A CNS penetrating agent should be used and options include azithromycin [29], fluoroquinolones [30] and doxycycline although there is no definitive evidence for efficacy [3].
10.6 Arboviruses Including Japanese Encephalitis are Rarely Seen in the UK but are Globally Important Causes of Viral Encephalitis
Arbovirus (Arthropod Borne virus) is a colloquial term referring to viruses that are sustained in cycles of transmission between host vertebrate species and vector arthropods such as mosquitoes or ticks. A number of these viruses can cause encephalitis in humans, who are usually not the primary host but an evolutionary ‘dead-end’ for the virus. The major families of ‘arboviruses’ are Bunyaviridae (La Crosse virus), Togaviridae (e.g. Eastern and Western Equine encephalitis and Chikungunya) and Flaviviridae (e.g. Japanese encephalitis, West Nile virus, St Louis encephalitis, tick borne encephalitis). Globally it is viruses from the genus flavivirus , within the family Flaviviridae, which are responsible for the greatest burden of disease. The combination of vector ecology, host ecology and virus biology result in very specific geographic and seasonal patterns for these infections and the most significant flaviviruses vary by region. The mosquito-transmitted flaviviruses that typically cause encephalitis are Japanese encephalitis, West Nile virus and St Louis encephalitis. Although only a minority of infections result in significant disease, encephalitis is one of the characteristic disease syndromes of these viruses [31].
Japanese encephalitis is estimated to cause up to 67,900 cases of encephalitis annually [32] despite the fact that there is an effective vaccine which has been incorporated into routine immunisation programmes in many areas of the world. This virus is endemic in many areas of Asia and causes sporadic disease in the western Pacific and north Australia. Cases are predominantly in children, with significant neurological morbidity and a case fatality rate of 20–30 %. Between 30–50 % of survivors suffer neuropsychological sequelae. Disease in returning travellers is rare. Whether this is due to exposure or immunisation of travellers is unclear but the short incubation period (5–15 days) reduces the probability of Japanese encephalitis being a significant consideration except in the first 1–2 weeks after return. The prevalence of this disease in certain regions has driven attempts to find an effective treatment including trials of steroids and interferon-2 alpha but to date none have been shown to have efficacy [33, 34]. Effective immunisation programmes of individuals exposed to infection is the mainstay of prevention for this disease. For many years Japanese encephalitis was known as Japanese B encephalitis although the use of this term has now mostly lapsed. The origin of this term was as a distinction from type A epidemic encephalitis (encephalitis lethargica).
Since the introduction of its mosquito vector into the US in 1999 West Nile virus has become an important diagnostic consideration in the North America [35]. The arrival of this pathogen to the USA demonstrates the dynamic epidemiology of this virus family related to the interdependence of host, vector and virus. Despite suggestive experiments in animal models with immunoglobulin treatment and some human data there remains no proven treatment for infection with this virus [36].
Some other flaviviruses rely on tick vectors . In many areas of central and eastern Europe and across Russia into China one of several strains of tick borne encephalitis make up one of the most common aetiologies of encephalitis [37]. The incidence of disease has been increasing over recent years perhaps in response to climatic variables. Several countries in this region include vaccines against this virus in routine immunisation schedules.
10.7 ‘Louping ill’: the UK Flavivirus
Many regions of the world have syndromes of viral encephalitis related to arboviruses sustained in life-cycles adapted to very specific local ecologies and the UK is no exception. The ‘Louping ill’ virus is the only flavivirus endemic in the UK [38] . It is closely related to tick borne encephalitis virus. The life-cycle involves tick vector (Ixodes ricinus) which is found mainly in areas of rough upland grazing or moorland. ‘Louping ill’ is an infection of the nervous system and occurs mostly in sheep and grouse. Human cases are rare and usually related to occupational exposure (abattoir workers, shepherds, vets). A range of syndromes have been described one of which is an encephalitis. There is no specific treatment and the name relates to the leaping behaviour of the sheep which develop symptomatic disease manifest by ‘spring(ing) into the air.’
10.8 Conclusion
For the clinician, managing a child with an encephalitis-like syndrome a detailed history (including travel, immunisation status, animal exposure and evidence of immune-compromise) will facilitate prompt and effective investigation and treatment of important causative pathogens. Despite this, in a significant number of cases no aetiology will be identified. Key issues in management are prompt empiric treatment with antibiotics and acyclovir, consideration of other likely treatable causes (infectious and non-infectious) and good supportive care.
References
Thompson C, Kneen R, Riordan A, Kelly D, Pollard AJ (2012) Encephalitis in children. Arch Dis Child 97(2):150–161
Long SS (2011) Encephalitis diagnosis and management in the real world. Adv Exp Med Biol 697:153–173
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL et al (2008) The management of encephalitis: clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis 47(3):303–327
Kneen R, Michael BD, Menson E, Mehta B, Easton A, Hemingway C et al (2012) National guideline for the management of suspected viral encephalitis in children. J Infect 64(5):449–477
Kolski H, Ford-Jones EL, Richardson S, Petric M, Nelson S, Jamieson F et al (1998) Etiology of acute childhood encephalitis at The Hospital for Sick Children, Toronto, 1994–1995. Clin Infect Dis 26(2):398–409
Glaser CA, Gilliam S, Schnurr D, Forghani B, Honarmand S, Khetsuriani N et al (2003) In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998–2000. Clin Infect Dis 36(6):731–742
Granerod J, Ambrose HE, Davies NW, Clewley JP, Walsh AL, Morgan D et al (2010) Causes of encephalitis and differences in their clinical presentations in England: a multicentre, population-based prospective study. Lancet Infect Dis 10(12):835–844
Granerod J, Crowcroft NS (2007) The epidemiology of acute encephalitis. Neuropsychol Rehabil 17(4–5):406–428
Granerod J, Tam CC, Crowcroft NS, Davies NW, Borchert M, Thomas SL (2010) Challenge of the unknown. A systematic review of acute encephalitis in non-outbreak situations. Neurology 75(10):924–932
Fowler A, Stodberg T, Eriksson M, Wickstrom R (2008) Childhood encephalitis in Sweden: etiology, clinical presentation and outcome. Eur J Paediatr Neurol 12(6):484–490
Willoughby RE Jr., Tieves KS, Hoffman GM, Ghanayem NS, Amlie-Lefond CM, Schwabe MJ et al (2005) Survival after treatment of rabies with induction of coma. N Engl J Med 352(24):2508–2514
Whitley RJ, Alford CA, Hirsch MS, Schooley RT, Luby JP, Aoki FY et al (1986) Vidarabine versus acyclovir therapy in herpes simplex encephalitis. N Engl J Med 314(3):144–149
Whitley RJ, Kimberlin DW (2005) Herpes simplex encephalitis: children and adolescents. Semin Pediatr Infect Dis 16(1):17–23
Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Corey L, Gruber WC et al (2001) Safety and efficacy of high-dose intravenous acyclovir in the management of neonatal herpes simplex virus infections. Pediatrics 108(2):230–238
De Tiege X, Heron B, Lebon P, Ponsot G, Rozenberg F (2003) Limits of early diagnosis of herpes simplex encephalitis in children: a retrospective study of 38 cases. Clin Infect Dis 36(10):1335–1339
Baskin HJ, Hedlund G (2007) Neuroimaging of herpesvirus infections in children. Pediatr Radiol 37(10):949–963
Kelly D, Kroll JS (2004) Encephalitis—beyond aciclovir. Adv Exp Med Biol 549:177–183
Elbers JM, Bitnun A, Richardson SE, Ford-Jones EL, Tellier R, Wald RM et al (2007) A 12-year prospective study of childhood herpes simplex encephalitis: is there a broader spectrum of disease? Pediatrics 119(2):399–407
Chan PK, Chow PC, Peiris JS, Mak AW, Huen KF (2000) Use of oral valaciclovir in a 12-year-old boy with herpes simplex encephalitis. Hong Kong Med J 6(1):119–121
Pouplin T, Pouplin JN, Van Toi P, Lindegardh N, Rogier van Doorn H, Hien TT et al (2011) Valacyclovir for herpes simplex encephalitis. Antimicrob Agents Chemother 55(7):3624–3626
Musallam B, Matoth I, Wolf DG, Engelhard D, Averbuch D (2007) Steroids for deteriorating herpes simplex virus encephalitis. Pediatr Neurol 37(3):229–232
Kamei S, Sekizawa T, Shiota H, Mizutani T, Itoyama Y, Takasu T et al (2005) Evaluation of combination therapy using aciclovir and corticosteroid in adult patients with herpes simplex virus encephalitis. J Neurol Neurosurg Psychiatry 76(11):1544–1549
German Trial of Aciclovir and Corticosteroids in Herpes Simplex Encephalitis (GACHE). http://www.klinikum.uni-heidelberg.de/index.php?id = 4223&L = en
Bitnun A, Ford-Jones EL, Petric M, MacGregor D, Heurter H, Nelson S et al (2001) Acute childhood encephalitis and Mycoplasma pneumoniae. Clin Infect Dis 32(12):1674–1684
Koskiniemi M, Vaheri A (1989) Effect of measles, mumps, rubella vaccination on pattern of encephalitis in children. Lancet 1(8628):31–34
Bitnun A, Richardson SE (2010) Mycoplasma pneumoniae: Innocent Bystander or a True Cause of Central Nervous System Disease? Curr Infect Dis Rep 12(4):282–290
Tong CY, Menson E, Lin JP, Lim M (2011) Prevalence of mycoplasma encephalitis. Lancet Infect Dis 11(6):425–426
Narita M (2009) Pathogenesis of neurologic manifestations of Mycoplasma pneumoniae infection. Pediatr Neurol 41(3):159–166
Jaruratanasirikul S, Hortiwakul R, Tantisarasart T, Phuenpathom N, Tussanasunthornwong S (1996) Distribution of azithromycin into brain tissue, cerebrospinal fluid, and aqueous humor of the eye. Antimicrob Agents Chemother 40(3):825–826
Esposito S, Tagliabue C, Bosis S, Principi N (2011) Levofloxacin for the treatment of Mycoplasma pneumoniae-associated meningoencephalitis in childhood. Int J Antimicrob Agents 37(5):472–475
Solomon T (2004) Flavivirus encephalitis. N Engl J Med 351(4):370–378
Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM et al (2011) Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ 89(10):766–774, 74A–74E
Hoke CH Jr., Vaughn DW, Nisalak A, Intralawan P, Poolsuppasit S, Jongsawas V et al (1992) Effect of high-dose dexamethasone on the outcome of acute encephalitis due to Japanese encephalitis virus. J Infect Dis 165(4):631–637
Solomon T, Dung NM, Wills B, Kneen R, Gainsborough M, Diet TV et al (2003) Interferon alfa-2a in Japanese encephalitis: a randomised double-blind placebo-controlled trial. Lancet 361(9360):821–826
Murray KO, Mertens E, Despres P (2010) West Nile virus and its emergence in the United States of America. Vet Res 41(6):67
Jackson AC (2004) Therapy of West Nile virus infection. Can J Neurol Sci 31(2):131–134
Mansfield KL, Johnson N, Phipps LP, Stephenson JR, Fooks AR, Solomon T (2009) Tick-borne encephalitis virus—a review of an emerging zoonosis. J Gen Virol 90(Pt 8):1781–1794
HPA (2011) Louping ill. 2011 (cited 15 Jan 2012). http://www.hpa.org.uk/Topics/InfectiousDiseases/InfectionsAZ/LoupingIll/
Guffond T, Dewilde A, Lobert PE, Lefebvre DC, Hober D, Wattre P (1994) Significance and Clinical Relevance of the Detection of Herpes-Simplex Virus-DNA by the Polymerase Chain-Reaction in Cerebrospinal-Fluid from Patients with Presumed Encephalitis. Clin Infect Dis 18(5):744–749
Studahl M, Bergstrom T, Hagberg L (1998) Acute viral encephalitis in adults—a prospective study. Scand J Infect Dis 30(3):215–220
Weil AA, Glaser CA, Amad Z, Forghani B (2002) Patients with suspected herpes simplex encephalitis: rethinking an initial negative polymerase chain reaction result. Clin Infect Dis 34(8):1154–1157
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Kelly, D. (2013). An Encephalitis Primer. In: Curtis, N., Finn, A., Pollard, A. (eds) Hot Topics in Infection and Immunity in Children IX. Advances in Experimental Medicine and Biology, vol 764. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4726-9_10
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4726-9_10
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4725-2
Online ISBN: 978-1-4614-4726-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)