Abstract
Significant advances, especially in microbiologic diagnostics and brain imaging, have broadened our understanding of the etiology, pathogenesis, and natural history of acute encephalitis. In some instances this had led to specific therapies and preventive measures. The clinical hallmark of acute encephalitis is the triad of fever, headache, and altered mental status. Common neurologic features include disorientation or depressed level of consciousness; disturbances of behavior, speech, or executive function; and diffuse or focal neurologic signs such as cranial nerve dysfunction, hemiparesis, or seizures. These features distinguish the unusual patient with encephalitis from the more commonly encountered patient with uncomplicated meningitis who has fever, headache, and nuchal rigidity but lacks abnormal global or focal neurologic signs. Etiologies of acute encephalitis are myriad. Most are viral infections. Table 1 shows a robust but not exhaustive list of viral etiologies. Beyond this there is another robust but not exhaustive list (Table 2) of important considerations in the differential diagnosis. These include infectious agents (bacterial, fungal, parasitic, and amebic) as well as non-infectious etiologies (parainfectious, post-infectious, autoimmune, neoplastic, cerebrovascular, systemic, and other conditions). The challenge for the clinician is to rapidly hone the list and make critical management decisions by considering the specific features of the setting of the patient’s illness, host susceptibility, clinical and neurologic findings, and results of laboratory and imaging studies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Herpes Simplex Virus
- West Nile Virus
- Herpes Simplex Virus Encephalitis
- Acute Flaccid Paralysis
- Viral Encephalitis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Approach to Focusing Possible Etiologies
1.1 Pathogenesis
Most cases of acute encephalitis are due to viruses (Table 1). Tropism of different viruses for different cell types as well as the balance of the pathogen damage-response framework determines clinical findings [1, 2]. Bunyaviridae, Togaviridae, Flaviviridae, and Reoviridae are neurotropic, i.e., although the infection is unusual, infection is likely to lead to central nervous system infection. Others, such as herpesviruses, West Nile virus, human immunodeficiency virus (HIV), parvovirus B19, measles, and mumps virus, cause frequent enough infections that their modest neurotropism leads to the infrequent consequence of CNS dissemination and gives them importance on the list. Additionally, some neurotropic viruses, such as enteroviruses, lymphocytic choriomeningitis virus, and poliovirus usually lead to aseptic meningitis but occasionally can cause encephalitis. Finally, rabies virus is a unique example in which human infection inevitably results in central nervous system infection in the absence of systemic infection. Cellular mechanisms of damage that lead to clinical encephalitis are as diverse as associated agents and are not addressed in this chapter [1].
The same principles of tropism apply to non-viral infectious causes of acute encephalitis listed in Table 2. Some bacteria that are not uncommon causes of systemic infection also are neurotropic, such as Neisseria meningitidis, Haemophilus influenzae, and Rickettsia species. Although CNS site of infection usually leads to clinical meningitis, encephalitis can occur occasionally. Other less neurotropic agents are so prevalent that the occasional manifestation as encephalitis makes them important considerations. Borrelia burgdorferi, parasites, and ameba are such examples. Bartonella henselae is unique on this list, both as an under-recognized cause of acute onset of status epilepticus and stupor or coma and because the clinical syndrome is encephalopathy rather than true encephalitis (absent cellular necrosis and cerebrospinal fluid [CSF] pleocytosis) [3].
1.2 Prioritizing Treatable Etiologies
Focussing on the primary clinical question of which causes of acute encephalitis have possible treatments, the major virus entries in Table 1 disappear, leaving a skeletal few as treatable causes of viral encephalitis shown in Table 3. The herpesviruses, and especially herpes simplex virus (HSV), tops the list with randomized, placebo-controlled trials of antiviral therapy providing evidence of life-saving, morbidity-reducing efficacy [4]. The possibility of HSV in all cases of acute encephalitis drives empiric therapy with acyclovir. There are only single or series of case reports or open label trials for other possibly treatable causes, such as intravenous ribavirin for La Crosse virus [5] and Nipah virus [6], interferon-alpha for West Nile virus [7], interferon alpha-2B for St. Louis encephalitis virus, and drug-induced coma, ribavirin, and neurotransmitter modulation (Milwaukee protocol) for rabies [8–10]. Efficacy of intravenous immunoglobulin containing high anti-West Nile virus antibody titers has been studied in a randomized, placebo-controlled trial in patients with West Nile neuroinvasive disease; results are pending.
In contrast to viral etiologies of acute encephalitis, there are specific anti-infective therapies and other potentially life-saving management for most infectious and non-infectious causes on the list of non-viral encephalitis-like syndromes in Table 2 that translate to treatable non-viral encephalitis considerations as shown in Table 4. Empiric therapy for encephalitis almost always includes anti-bacterial therapy. Anti-infective therapy has no proven efficacy in B. henselae or Mycoplasma pneumoniae encephalopathy/encephalitis. This table of differential diagnoses must be considered early and repeatedly in the course of management of patients with acute encephalitis. Brain imaging and examination of CSF and clinical course are most useful in guiding clinical management for the non-infectious cause of encephalitis most frequently encountered by a pediatric infectious diseases subspecialist – acute disseminated encephalomyelitis (ADEM) (discussed below).
1.3 Etiologically Focussed Prevention of Acute Encephalitis
Prevention is not in the scope of this chapter. However, before leaving the lists of etiologies and treatable causes of acute viral encephalitis, one recognizes that the highly successful approach of vaccine prevention of bacterial meningitis is not possible currently for most viral encephalitides. Table 5 shows in italics the vaccine preventable viral encephalitides – varicella zoster virus, Japanese encephalitis virus (IXIARO, licensed by the US Food and Drug Administration March 30, 2009 as the only available JE vaccine in the United States), tick-borne encephalitis virus (two vaccines licensed in Europe) [11], poliovirus, influenza, measles, mumps, and rabies. It is noteworthy that prior to universal immunization in childhood in the United States, measles and mumps viruses were the most common causes of encephalitis and post-infectious encephalitis, and measles virus was the cause of subacute sclerosing panencephalitis. These viruses still cause substantial CNS disease where immunization is not universal.
Table 5 also shows (in standard font) avoidable causes of acute encephalitis. This list is lengthy. Methods of control for the arboviruses predominantly are reduction or avoidance of the virus’ vector or the amplifying host. It is important then to attempt to identify outbreaks of arboviral infections and emerging infections specifically to implement optimal control measures, to use appropriate therapies if available, and to understand burden of disease as the first step in vaccine development. The lesson from the Nipah virus outbreak in Malaysia is an example of identification of the causative agent informing control [12]. From September 1998 to May 1999, 265 cases of encephalitis with 105 deaths occurred. Because the outbreak initially was attributed to Japanese encephalitis virus, mosquito control measures were implemented but were ineffective and the epidemic spread. Only when the Nipah virus was identified from a case, did it become clear that close contact with infected pigs was the mechanism of acquisition; pig culling halted the epidemic. In the extended story, typical of such epidemics, fruiting failure due to drought and fires in Indonesia drove the fruit bats (the natural reservoir host for Nipah virus) from forest habitat to farming areas, where bat excretions contaminated pig swill.
1.4 Season, Geography, and Epidemiology of Viral Encephalitis
Taken together, clues provided by intersections of certain characteristics of the host, the season of illness, geography, and epidemiologic setting as well as specific neurologic abnormalities help hone a long list of possibilities, eliminating many and elevating certain pathogens for specific consideration in each patient (Fig. 1).
Table 6 provides an example of virus considerations in which geography and season are not highly relevant, as viruses are common or ubiquitous and not seasonal. A healthy immunologically competent host can develop encephalitis from most pathogens shown, although immunocompromised individuals are unduly susceptible to CNS disease due to cytomegalovirus, JC virus, and varicella zoster virus. Certain etiologic possibilities become almost certainties with careful delineation of the epidemiologic setting and clinical extra-CNS manifestations (e.g., history of animal bite or exposure to bat for rabies, findings of clinical manifestations compatible with mononucleosis-like seroconversion syndrome for HIV). Nonspecific neurologic findings of decreased sensorium can be the only signs for most etiologies, but the presence of certain neurologic laboratory or imaging findings, if present, heighten certain possibilities (e.g., focal neurologic abnormalities, focal seizures and temporal lobe predilection for HSV, or autonomic and mood abnormalities due to limbic predilection for rabies virus).
Example pathogens shown in Table 7 share particular predilection for season, almost always summer and fall, with human infection being dependent on circulation of a vector, a neutral host or an amplifying host, and opportunity for human exposure. Exposure, travel history, and knowledge of incubation period are important considerations. Enteroviruses are the obvious exception to vector-positive history. Enteroviral disease burden is seasonal, but infection follows human-to-human transmission; there is no extra-human natural or amplifying host or vector.
Clinical neurologic clues sometimes stand out to suggest an etiologic agent, such as fulminant course to coma for Eastern equine encephalitis, focal seizures but mild encephalitis for La Crosse virus, acute flaccid paralysis for tick-borne encephalitis virus and West Nile virus, and findings typical of hippocampal predilection for Powassan virus. Epidemiologic shifts of a few pathogens in Table 8 highlight infinite ecological and evolutionary complexities as well as our meager understanding of events that shape emergence and spread of arthropod-borne viruses. Toscana virus, a member of the family Bunyaviridae, was first registered in the international catalogue of arboviruses only in 1980, first isolated from CSF in 1983, and transmission subsequently was shown to be by the Phlebotomine sandfly. Currently endemic in the Siena province of Central Italy, the virus is responsible for at least 80% of local acute viral CNS infections in children throughout the summer and for global sporadic cases following travel to the area [13].
West Nile virus (WNV) historically has been considered to be among the least virulent of the Japanese serogroup of the family Flaviviridae. However, a virus subtype with greater epidemic potential and virulence emerged in the early 1990s, facilitating geographic expansion in Asia, the Middle East, and Mediterranean, with westward spread. WNV first appeared in the western hemisphere in 1999. Birds serve as the natural vertebrate host and Culex mosquitoes are the enzootic and epizootic vector. With a broad host and vector range, WNV moved sequentially westward in the United States with human cases reported from the northeast in 1999 to California by 2002. In recent epidemics of WNV, approximately 80% of cases are asymptomatic, 20% have dengue-like syndromes, and <1% have neuroinvasive disease (WNND) including encephalitis, meningitis, and polio-like flaccid paralysis [14]. Children are less likely than adults with WNV to have WNND, accounting for only 4% of such cases from 1999 to 2007 reported in the United States; unlike older adults with WNND, children and young adults are more likely to have meningitis than encephalitis [15].
Chikungunya virus (CHIKV) is a mosquito-borne alphavirus indigenous in the sylvatic cycle in tropical Africa and Asia where it causes endemic and epidemic high fever, disabling joint and muscle pain (chikungunya in Swahili meaning “that which bends up”), and often a maculopapular rash and gastrointestinal complaints. CNS infection can lead to meningoencephalitis or polyneuropathy. In 2005–2006, an explosive epidemic of CHIK fever occurred on islands in the Indian Ocean, affecting almost one-half of the population and resulting in an estimated millions of cases in the islands and in India. Previously transmitted by Aedes aegypti (an exclusive human feeder), a point mutation in the virus more recently has been shown to make the Asian tiger mosquito, Aedes albopictus (a multi-species feeder) an enhanced transmitter [16]. Epidemic CHIK fever in Italy in 2007, Ae. albopictus transmitted, and global spread of the mosquito during the past two decades is worrisome for broader endemic disease as well as infection following travel.
1.5 Studies of Causes of Acute Encephalitis
The California Encephalitis Project (CEP) was initiated in 1998 by the California Department of Health in collaboration with the Emerging Infections Program of the Centers for Disease Control and Prevention to study causative agents, disease trends, risk factors, and clinical features of encephalitis in California. Comprehensive results have been published following intensive evaluations (which evolved somewhat over the first decade of study) of more than 1,500 patients enrolled. Although the majority of study subjects have been adults, studies have enlightened understanding of relative importance of pathogens, clinical patterns of disease, and usefulness of diagnostic tests [17–22]. Enrollment consisted of subjects with encephalopathy (altered level of consciousness for at least 24 h, lethargy, or change in personality) or ataxia, plus ≥ 1 of the following: temperature ≥ 38°C, seizure, focal neurologic finding, CSF pleocytosis, abnormal EEG, or neuroimaging study. Patients were excluded who were <6 months of age, immunosuppressed, or had underlying neurologic conditions (http://ceip.us/encephalitis.htm). A summary list of diagnostic tests performed is shown in Table 9. Additional tests for 24 pathogens were performed on a case-by-case basis if history, examination, laboratory, or imaging findings suggested certain pathogens. Etiologies of infections were assigned as confirmed, probable, or possible by pre-fixed definitions; confirmed non-infectious causes also were defined; the remainder of cases was designated as of unknown cause. Infection was designated as confirmed when an agent well established as a cause of encephalitis was detected in CSF or brain by PCR or by an antibody test when PCR is not the diagnostic test of choice. Infection was designated as probable when an agent well established as a cause of encephalitis was not identified in CSF or brain but when there was strong evidence by culture or serologic evidence of infection. Infection was designated as possible when an agent well established as a cause of encephalitis was identified by suggestive but not conclusive testing of a specimen other than the CSF (e.g., enteroviruses, HSV-1, and influenza) or when an agent not well established as a cause of encephalitis was identified by strong serologic or culture-based evidence at a site other than CNS (e.g., adenovirus and Mycoplasma) [18].
Despite extensive investigation in >1,500 subjects, no etiology was found in >60% of encephalitis cases. Infection accounted for 28% of cases (confirmed/probable, 15% and possible, 13%). Table 10 shows infectious causes identified. Viruses accounted for approximately 70% of confirmed and probable causes, with enteroviruses and HSV-1 heading the list. One extremely important finding that impacts decisions for empiric therapy was that approximately 20% of subjects with infectious encephalitis-like clinical presentation had CNS bacterial infections. Enteroviruses, influenza, and adenoviruses headed the list of possible viral etiologies. In a prospective registry in Toronto, influenza infection was identified in 7% of children with acute encephalitis [23]. It is noteworthy that although the association of influenza with neurologic disease is well established, the virus is almost never identified in the CSF or brain; pathophysiology appears in some cases to be acute necrotizing encephalopathy (ANE) (discussed below) due to CNS cytokine dysregulation, and in others, infection-triggered ADEM.
Mycoplasma accounted for 47% of possible non-viral cases (and no probable or confirmed cases in the CEP). In fact, Mycoplasma was the most frequently identified pathogen associated with encephalitis in the CEP. Christie et al. [19] reported on the 84 patients ≤ 18 years of age with evidence of acute Mycoplasma infection among 1988 encephalitis subjects accrued in the CEP by 2007. Median age was 11 years; 70% had fever, 45% had respiratory tract symptoms, and 44% had gastrointestinal symptoms. CSF showed mild pleocytosis (median 33 cells, predominantly mononuclear in 67%), with median protein of 45 mg/dL and normal glucose concentration. Clinical findings were different from adults and were most similar in presentation and outcome to proven enterovirus encephalitis. Diagnosis was made solely by positive serum IgM test in 92%; only 2 of 39 who had acute and convalescent serum IgG tests performed had confirmation of acute Mycoplasma infection. PCR test on respiratory specimen was positive in 30%. Sixty-two of the 84 patients had CSF Mycoplasma tested by PCR; none was positive. One patient had CSF IgM antibody detected [19]. In another study, Christie et al. [24] investigated auto-antibodies to galactocerebroside (anti-GalC) in CEP patients with evidence of acute Mycoplasma infection, since anti-GalC previously had been associated with Mycoplasma CNS disease; 8 of 21 had CSF anti-GalC antibody found, indicating that this is not a specific marker for Mycoplasma CNS disease (or that Mycoplasma was not the cause of CNS disease). At present it is not clear whether and how Mycoplasma is associated with CNS disease in children. Limitations of nonspecificity of the serum IgM Mycoplasma antibody test and common occurrence of subclinical Mycoplasma infection in children raise doubt about this association. There is no evidence that treatment for Mycoplasma infection alters the course of CNS-associated symptoms.
Other large-scale investigations of causes of acute central nervous system infection have been reported, none as intensely investigated as in the CEP. Two recent studies were reported in 2004 [25] and 2007 [26] from upstate New York and Helsinki, respectively. Huang et al. [25] report a 6-year study of CSF or brain tissue samples submitted to the Clinical Virology Laboratory at the New York State Department of Health from 3,465 patients with encephalitis or meningitis of unknown etiology. PCR and RT-PCR were performed for 12 viruses. For the 1,584 patients who met CEP-like criteria for acute encephalitis, 7.8% had a virus identified. Ranking of agents was identical to CEP ranking: enteroviruses, followed by HSV, VZV, and WNV [25]. Huttunen et al. [26] report a prospective 3-year study of 213 children admitted to the Hospital for Children and Adolescents, Helsinki University Hospital with suspicion of CNS infection. Extensive culture, PCR, and serologic testing were performed. Sixteen patients had encephalitis; most frequently confirmed etiologies were enteroviruses, human herpesvirus 6, and VZV. Additionally, nine patients had neuroborreliosis.
Although nonspecific neurologic symptom can be associated with any etiologic agent, specific neurologic findings are more commonly associated with certain pathogens. Examples include acute flaccid paralysis with enterovirus, tick-borne encephalitis virus, and WNV; seizures with HSV, La Crosse virus, Eastern equine encephalitis virus, and B. henselae; focal temporal abnormalities with HSV, VZV, and Mycobacterium tuberculosis; cerebellar abnormalities with Epstein–Barr virus, Listeria monocytogenes, and non-infectious etiologies; and hydrocephalus with bacteria, parasites, and thromboses. In the CEP, etiology was identified in approximately 75% of patients who had hydrocephalus, 63% who had focal temporal signs, 31% who had cerebellar signs, 64% who had seizure(s) with rapid recovery, and only 27% who had intractable seizures (a neurologic course with poor outcome more common in the pediatric age group than in adults in this study [21]).
1.6 Additional Noteworthy Diagnoses
1.6.1 Acute Disseminated Encephalomyelitis (ADEM)
Post-infectious encephalomyelitis was a term used when neurologic signs and symptoms followed a known infection (e.g., measles and varicella) or immunization (e.g., rabies vaccine made in neural tissue) [27]. There is no direct infection of neural cells, but there is widespread perivenular inflammation and demyelination localized in the white matter of the brain. PIEM is now rare. ADEM is PIEM, with similar neurologic signs and symptoms, with demyelination evident on MRI, usually following a nonspecific illness. A variety of viruses and vaccines have been temporally associated in case reports of ADEM. ADEM by definition has all of the following components: acute onset over days of a monophasic, multifocal, inflammatory, and demyelinating autoimmune CNS disorder [28]. It is not rare. In the CEP, 120 (9%) patients had multifocal white matter lesions; 23 (19%) of these patients had associated viral illnesses (enteroviruses, adenovirus, and influenza >2 cases each and 9 other viruses 1–2 cases each) and 14 (12%) had associated non-viral infections (M. pneumoniae in 6 cases). The remaining 7 patients (6%) had non-infectious etiologies (including malignancies and multiple sclerosis) and 63% had no inciting infection or associated condition found.
Davis and Booss reviewed 360 pediatric cases of ADEM [29]. Median age was 6.7 years (rare < 1 year), 60% were boys, >50% had history of preceding illness or immunization. Clinical, imaging, and CSF findings are shown in Table 11. Patients can come to medical attention acutely ill with fever, nausea, and vomiting or because of neurologic changes without systemic illness. In our experience, motor signs (weakness with spasticity or diminished reflexes) are present frequently with impaired attention and “executive” function and/or with limbic signs (autonomic dysregulation, hallucinations, and behavioral changes), which frequently are out of proportion to global depression of sensorium. MRI shows specific abnormalities with bilateral, usually asymmetric white matter lesions (lesions present in the thalamus and basal ganglion can be symmetric). ADEM is a clinical diagnosis with compatible MRI findings.
The pathogenesis of ADEM is thought to be molecular mimicry of microbes with myelin proteins. Theoretically, T lymphocytes respond to the microbe and by mimicry to myelin protein. Antigen-specific T or B lymphocytes or both gain access to the central nervous system, or antigen-presenting microglial cells encounter homologue myelin protein. Perivenulitis and demyelination ensue. Host-specific immune dysregulation rather than certain infectious agents has been speculated as possibly causative. No pathogen, RNA, or DNA is expected to be found in the CNS. ADEM must be differentiated from multiple sclerosis (MS). Diagnosing MS requires “dissemination in time and space,” meaning affecting multiple areas of demyelination in a polyphasic course. Concerning factors for MS in patients with first episode, presumed ADEM are age > 12 years, optic neuritis, or involvement of the spinal cord [29]. New symptoms or signs within 3 months of diagnosis of ADEM (and especially if associated with weaning of corticosteroid) are considered as part of the same ADEM event and not as fulfilling criteria for MS [28]. A recent review of ADEM, especially as differentiated from MS is a valuable resource [28].
Diagnosis is important as empiric corticosteroid therapy is first-line therapy and decreases time to recovery [30, 31]. Bilateral asymmetric white matter lesions are the sine qua non of ADEM. There can be a lag of days to weeks in MRI findings in some patients as well as a “mismatch” in other patients who have remarkable MRI findings and relatively few neurologic abnormalities. CSF usually is abnormal, but nonspecifically and frequently mildly (Table 9).
Therapy for ADEM has evolved from case reports and series rather than randomized, blinded placebo-controlled trials, but evidence of effect of immunosuppressive therapy is compelling – sudden remarkable improvement in some patients, decreased signs of CNS inflammation, decreased time to recovery, and relapses on weaning [28, 29]. Intravenous corticosteroid in doses of 20–30 mg/kg/day (maximum 1 g) for 3–5 days often results in dramatic clinical improvement. Oral prednisone at a dose of 1 mg/kg/day is then tapered over 14–21 days. Duration of initial and tapering doses has been lengthened after experience of frequent relapses after 5-day treatment/10-day taper regimen [28]. Immunoglobulin intravenously (IGIV) usually is given if corticosteroid response is not clinically remarkable; dose is 2 g/kg divided over 2–5 days. Plasma exchange usually is third-line therapy; it has been subject only of case reports, in which benefits appear to approximate that of IGIV.
1.6.2 Acute Necrotizing Encephalopathy (ANE)
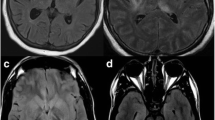
Acute necrotizing encephalopathy is less frequent than ADEM. ANE is a distinct form of acute encephalopathy triggered by respiratory tract infections, especially viral infections such as influenza A and B [32]. First described as a novel disease by Mizuyuchi in 1995, the condition has been reported mainly from Japan, although increasingly ANE is recognized in multiple countries [33]. It is not a rare encounter among pediatric infectious diseases subspecialists in the United States. Affected children usually are 5 months to 10 years of age, previously healthy, who in the peak of a febrile respiratory tract illness have acute onset of seizures or changes in mental status or both; global suppression ranges from obtundation to coma. Specific neurologic abnormalities are not universal, but speech abnormalities and akinetic mutism as well as delirious behavior [34] may occur more commonly in ANE than in acute infectious encephalitis or ADEM. CSF is acellular, glucose concentration is normal, and protein concentration typically is normal or mildly elevated. Serum hepatic enzymes may be elevated, severity of which has been associated with poor prognosis in Japanese children. The hallmark of ANE is the MRI findings on T2-weighted images of high intensity signal diffusely and symmetrically in the periventricular white matter – characteristically affecting the thalamus, internal capsule, cerebellum, and brainstem in some cases. Changes are seen within 12 h after onset of coma.
Pathogenesis is thought to be cytokine dysregulation localized to the CNS. Autopsy of fatal cases shows apoptosis of neurons, with edema but no inflammatory infiltrate or vasculitis. No evidence of pathogen entry into the CNS is evident by culture, PCR, antibody test, or in situ hybridization tests on tissue. Possible role of non-steroidal anti-inflammatory medication in precipitation of ANE has been suggested. The same clinical syndrome following infection with different viruses also is compatible with predisposition due to host factors. Recent data suggest that some cases of ANE represent a familiar disorder or may be the result of an inherited predisposition due to a mutation in the RANBP2 gene [33].
ANE can be fatal, and outcome of survivors generally is poor. Efficacy of therapies has been anecdotal or evaluated only retrospectively in case series [35]. In such a series of 34 children with ANE, corticosteroid therapy within 24 h of onset was correlated with improved outcome (good outcome in 7 of 12 treated patients compared with none of 5 untreated patients). Children with brainstem involvement had poor outcome regardless of corticosteroid therapy. Intravenous administration of immunoglobulin (IGIV) had no apparent effect on the clinical course in this series.
1.7 Additional Noteworthy Pathogens
1.7.1 B. burgdorferi
B. burgdorferi is the most common tick-borne infection in the northeastern United States. Spirochetes can invade the central nervous system and cause subacute aseptic meningitis, acute facial nerve palsy, or other cranial nerve palsies. A prospective study of 177 children evaluated for neuroborreliosis in Sweden showed frequent fatigue, headache, fever, neck pain, and facial nerve palsy in confirmed cases [36]. Encephalopathy was not described in this series, 118 of whom had confirmed or probable Lyme disease. B. burgdorferi was not found in the CEP [18], not tested for in the New York state encephalitis study [25], and was identified in the Helsinki study in children with meningitis (not encephalitis) and facial nerve palsy [26]. Lyme encephalitis with altered consciousness, therefore, must be a rare disease. A useful clinical prediction model for Lyme meningitis, however, was proposed recently from clinical study of 50 children from a Lyme endemic area in Rhode Island [37]. The so-called rule of 7 s would predict a < 10% probability of CNS Lyme disease if headache was present for < 7 days, cranial nerve 7 palsy was absent, and CSF had < 70 mononuclear cells/mm3.
1.7.2 Parvovirus B19
A retrospective report of 81 cases of neurologic disease, including encephalitis, meningitis, stroke, and peripheral neuropathy, was published recently from an English and French literature review [38]. One-third of patients had altered immune status. Two-thirds of patients were < 18 years of age. Encephalitis, stroke, and seizures were more common heralding manifestations in children than in adults; peripheral neuropathy (brachial plexus palsy and carpal tunnel syndrome) occurred in adults. Overall, rash was reported in 36% of patients. CSF was normal or showed modest mononuclear cell pleocytosis and elevated protein concentration. Diagnosis was confirmed by PCR testing on CSF sample (81%), serum (85%), or by specific antibody testing on CSF (33%). The methods of PCR and antibody testing were not reviewed. This review raises parvovirus B19 into considerations among causes of encephalitis, especially in children. It is noteworthy that in the CEP testing for parvovirus was performed only when rash or anemia was present (15 instances); no case of confirmed parvovirus etiology was reported [18]. Parvovirus B19 serology was performed in patients in the Helsinki study.
1.7.3 Balamuthia mandrillaris
In the >3,500 cases referred to the CEP, 10 patients (5 cases < 18 years of age) were found to have amebic encephalitis due to the free-living ameba B. mandrillaris. Presentations were nonspecific – headache, seizures, cranial nerve palsies, and lethargy – and would have been described as “encephalitis of unknown etiology” except for the CEP protocol. Nine cases were fatal. Neuroimaging was abnormal in all, with ringed enhancing focal lesions or hydrocephalitis or both [22].
1.8 Specific Clinical Neurologic Syndromes
Certain cardinal neurologic findings in patients with encephalitis make specific etiologic agents more likely to be confirmed. Table 8 shows some examples – from author’s experience, case reports, and the CEP results. In the CEP, likelihood of confirming a cause varied substantially by neurologic finding: 75% confirmation for cases with hydrocephalus, 63% for focal temporal lobe signs, 31% for cerebellar signs, and only 28% for status epilepticus [18]. Acute flaccid paralysis cases were not tallied as such. The most important clinical conclusions from these data are that hydrocephalus should not be thought to be due to viral encephalitis or post-infectious ADEM without exclusion of treatable, more likely causes, e.g., bacterial, fungal, or parasitic infections or thromboses.
2 Approach to Empiric Management
Predicting precise etiologic agent of encephalitis in an individual case is extremely difficult. Empiric therapy is urgently necessary for the minority of infections that are treatable as outcome is dependent on severity of neurologic findings at commencement of effective therapy. Approach to choosing agents for empiric therapy can be based on consideration of categories of treatable infectious agents: common bacteria – Streptococcus pneumoniae, H. influenzae, N. meningitidis, and in the case of focal brain or parameningeal lesions, viridans Streptococcus and anaerobic bacteria, or Staphylococcus aureus; uncommon bacteria – L. monocytogenes (which has propensity among bacteria to cause an encephalitis syndrome), B. burgdorferi; treatable virus – herpes simplex virus; mycobacteria – M. tuberculosis; fungi – Cryptococcus neoformans, other fungi in immunocompromised hosts; rickettsia – Rickettsia rickettsiae, Ehrlichia, and Anaplasma species; parasites and ameba – Baylisascaris procyonis, agents of neurocysticercosis, Balamuthia species, Acanthamoeba, and Naegleria fowleri.
Simple laboratory tests – complete blood count, sedimentation rate, C-reactive protein, serum chemistry panel – which frequently are helpful in categorizing systemic infectious diseases, are not discriminating for encephalitis. Cerebrospinal fluid analysis and MRI are the cornerstones for choosing empiric therapy and for pursuing confirmation of etiology to plan definitive therapy. It is noteworthy with regard to HSV encephalitis that first sampling of CSF may show negative PCR test results. When the unfolding clinical course is compatible with HSV encephalitis, it is our practice to continue acyclovir until plasma and a second CSF PCR test are negative. Clinical practice guidelines for management of patients with encephalitis have been published recently by the Infectious Diseases Society of America [39].
Figure 2 delineates the author’s strategy for empiric therapy based on analysis of cerebrospinal fluid (CSF). Opening pressure is measured; increased intracranial pressure suggests that bacteria, mycobacteria, rickettsia, fungi, or parasites are more likely etiologies than are viruses. Presence of eosinophils would cue pursuit of parasites such as B. procyonis [40] and Angiostrongylus and Gnathostoma species [41]. Pleocytosis predominantly comprised of neutrophils leads to empiric treatment for common meningitis pathogens – S. pneumoniae, H. influenzae, N. meningitidis, L. monocytogenes, and herpes simplex virus. Although HSV is not equally likely as causative, therapy should include high-dose acyclovir (60 mg/kg/day for neonates to 2- to 3-year-old children; 30 mg/kg/day for older children) for a patient with encephalitis regardless of age and CSF findings. Vancomycin plus a third-generation cephalosporin (usually cefotaxime or ceftriaxone) are given for usual pathogens of meningitis, which occasionally cause meningoencephalitis. Because L. monocytogenes is considered as having propensity among bacteria to cause encephalitis, ampicillin usually is given. Antibiotic therapy generally is discontinued when cultures of CSF and blood are negative, and imaging does not suggest an abscess.
Hypoglycorrhachia should lead to increased suspicion of bacteria, including Listeria and can occur with HSV encephalitis (especially when necrotizing). Empiric therapy should include therapy for these pathogens. Because hypoglycorachia (especially in the presence of modest mononuclear pleocytosis) is typical of mycobacterial and fungal CNS infection, these diagnoses should be considered specifically and pursued depending on the setting and likelihood of another diagnosis.
Patients with encephalitis-like syndromes with normal CSF or nonspecifically abnormal CSF, e.g., with mononuclear pleocytosis or elevated protein concentration, also should be treated for HSV infection. Treatments for bacterial causes, rickettsia, and neuroborreliosis are considered based on other findings, such as season and exposures for rickettsia and Borrelia; or rash, hyponatremia, thrombocytopenia for rickettsia.
Tests performed on CSF always will include Gram stain and culture, PCR test for HSV and enterovirus. Decisions to perform CSF PCR or IgM antibody test for Borrelia, WNV, and other herpesviruses; CSF antigen test for Cryptococcus; or serum antibody tests for other viruses, rickettsia, etc. depend on poor clinical “fit” for expected pathogens or specific clues in exposure history, clinical, or laboratory findings that raise suspicion for unusual pathogens. Table 12 may help focus testing.
Neuroimaging, especially MRI, has added immeasurably to management and to diagnostic approach in patients with encephalitis syndromes. Specificity of MRI for diagnosis is beyond the scope of this paper. Basic categorization of findings is useful: normal, predominant gray vs. white matter lesion(s), edema/hydrocephalus, focal vs. multifocal site, symmetric vs. asymmetric distribution, or specific abnormality, such as mass, abscess, calcification, ring lesion, hemorrhage, or meningeal enhancement. Empiric therapy is not limited because of MRI findings but certain findings trigger additional investigations or therapies. A few examples are edema/hydrocephalus for bacteria and fungi; asymmetric white matter abnormalities for ADEM; bilateral, symmetrical increased T2-weighted signal in perivascular deep white matter for ANE; and ring lesions for parasitosis. In patients with normal MRI at presentation whose condition deteriorates or whose diagnosis is unclear, repeated MRI can enlighten next steps in diagnosis and management. Electroencephalopathy, likewise, can show specific abnormalities such as sometimes can be seen in HSV encephalitis or subacute sclerosing panencephalitis or can confirm subclinical seizures, but mostly commonly is nonspecifically abnormal in acute encephalitis of multiple etiologies.
References
Whitley RJ, Gnann JW. Viral encephalitis: familiar infections and emerging pathogens. Lancet. 2002;359:507–14.
Casadevall A, Pirofski L-A. The damage response framework of microbial pathogenesis. Nature Rev/Microbiol. 2003;1:17–24.
Armengol CE, Hendley JO. Cat-scratch disease encephalopathy: a cause of status epilepticus in school-aged children. J Pediatr. 1999;134:635–8.
Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Corey L, Gruber WC et al. Safety and efficacy of high-dose intravenous acyclovir in the management of neonatal herpes simplex virus infections. Pediatrics. 2001;108:230–8.
McJunkin JE, de Los Reyes EC, Irazuzta JE, Caceres MJ, Khan RR, Minnich LL et al. La Crosse encephalitis in children. N Engl J Med. 2001;344:801–7.
Chong HT, Kamarutzaman A, Tan CT, Goh KJ, Thayaparan T, Kunjapan SR et al. Treatment of acute Nipah encephalitis with ribavirin. Ann Neurol. 2001;49:810–13.
Diamond MS. Progress on the development of therapeutics against West Nile virus. Antiviral Res. 2009;83:214–27.
Willoughby RE Milwaukee protocol: rabies treatment protocol and interactive advice. http://www.mcw.edu/rabies
Willoughby RE, Opladen T, Maier T, Rhead W, Schmiedel S, Hoyer J et al. Tetrahydrobiopterin deficiency in human rabies. Inherit Metab Dis. 2009;32:65–72.
Rubin J, David D, Willoughby RE Jr, Rupprecht CE, Garcia C, Guarda DC et al. Applying the Milwaukee protocol to treat canine rabies in Equatorial Guinea. Scand J Infect Dis. 2009;41:372–80.
Lindquist L, Vapalahti O. Tick-borne encephalitis. Lancet. 2008;371:1861–71.
Looi LM, Chua KB. Lessons from the Nipah virus outbreak in Malaysia. Malays J Pathol. 2007;29:63–7.
Braito A, Corbisiero R, Corradini S, Fiorentini C, Ciufolini MG. Toscana virus infections of the central nervous system in children: a report of 14 cases. J Pediatr. 1998;132:144–8.
Gubler DJ. The continuing spread of West Nile virus in the western hemisphere. Clin Infect Dis. 2007;45:1039–46.
Lindsey NP, Hayes EB, Staples JE, Fischer M. West Nile virus disease in children, United States, 1999–2007. Pediatrics. 2009;123:e1084–9. URL http://www.pediatrics.org/cgi/doi/10.1542/peds.2008-3278.
de Lamballerie X, Leroy E, Charrel RN, Tsetsarkin K, Higgs S, Gould EA. Chikungunya virus adapts to tiger mosquito via evolutionary convergence: a sign of things to come?. Virol J. 2008;27:33.
Glaser CA, Gilliam S, Schnurr D, Forghani B, Honarmand S, Khetsurian N et al. In search of encephalitis etiologies: diagnostic challenges in the California Encephalitis Project, 1998–2000. Clin Infect Dis. 2003;36:731–42.
Glaser CA, Honarmand S, Anderson LJ, Schnurr DP, Forghani B, Cossen FL et al. Beyond viruses: clinical profiles and etiologies associated with encephalitis. Clin Infect Dis. 2006;43:1565–78.
Christie LJ, Honarmand S, Talkington DF, Gavali SS, Preas C, Pan C-Y et al. Pediatric encephalitis: what is the role of Mycoplasma pneumoniae?. Pediatrics. 2007;120:305–12.
Fowlkes A, Honarmand S, Glaser C, Yagi S, Schnurr D, Oberste MS et al. Enterovirus-associated encephalitis in the California encephalitis project, 1998–2005. J Infect Dis. 2008;198:1685–92.
Glaser CA, Gilliam S, Honarmand S, Tureen JH, Lowenstein DH, Anderson LJ et al. Refractory status epilepticus in suspect encephalitis. Neurocrit Care. 2008;9:74–82.
Schuster FL, Yagi S, Gavali S, Michelson D, Raghavan R, Blomquist I et al. Under the radar: Balamuthia amebic encephalitis. Clin Infect Dis. 2009;48:879–88.
Amin R, Ford-Jones E, Richardson SE, MacGregor D, Tellier R, Heurter H et al. Acute childhood encephalitis and encephalopathy associated with influenza: A prospective 11-year review. Pediatr Infect Dis J. 2008;27:390–4.
Christie LJ, Honarmand S, Yagi S, Ruiz S, Glaser CA. Anti-galactocerebroside testing in Mycoplasma pneumoniae-associated encephalitis. Neuroimmunol. 2007;189:129–31.
Huang C, Morese D, Slater B, Anand M, Tobin E, Smith P et al. Multiple-year experience in the diagnosis of viral central nervous system infections with a panel of polymerase chain reaction assays for detection of 11 viruses. Clin Infect Dis. 2004;39:630–6.
Huttunen P, Lappalainen M, Salo E, Lönnqvist T, Jokela P, Hyypiä T et al. Differential diagnosis of acute central nervous system infections in children using modern microbiological methods. Acta Paediatr. 2009;98(8):1300–6. Electronic ahead of print, April 1.
Johnson RT. Acute encephalitis. Clin Infect Dis. 1996;23:219–26.
Dale RC, Brilot F, Banwell B. Pediatric central nervous system inflammatory demyelination: acute disseminated encephalomyelitis, clinically isolated syndromes, neuromyelitis optica, and multiple sclerosis. Curr Opin Neurol. 2009;22:233–40.
Davis LE, Booss J. Acute disseminated encephalomyelitis in children: a changing picture. Pediatr Infect Dis J. 2003;22:829–31.
Menge T, Hemmer B, Nessler S, Wiendl H, Neuhaus O, Hartung HP et al. Acute disseminated encephalomyelitis: an update. Arch Neurol. 2005;62:1673–80.
Feasby T, Banwell B, Benstead T, Bril V, Brouwers M, Freedman M et al. Guidelines on the use of intravenous immune globulin for neurologic conditions. Transfus Med Rev. 2007;21(2 Suppl 1):S57–S107.
Okumura A, Abe S, Kidokori H, Mizuguchi M. Acute necrotizing encephalopathy: a comparison between influenza and non-influenza cases. Microbiol Immunol. 2009;53:277–80.
Suri M. Genetic basis for acute necrotizing encephalopathy of childhood. Dev Med Child Neurol. (Published online) DOI:101111/j.1469–8749.2009.03405.x.
Okumera A, Mizuguchi M, Alba H, Tanabe T, Tsuji T, Ohno A. Delirious behavior in children with acute necrotizing encephalopathy. Brain Dev. 2009;31:594–9.
Okumura A, Mizuguchi M, Kidokoro H, Tanaka T, Noda E, Imataka G, Kurahashi H. Outcome of acute necrotizing encephalopathy in relation to treatment with corticosteroids and gammaglobulin. Brain Dev. 2009;31:221–7.
Skogman BH, Croner S, Nordwall M, Eknefelt M, Ernerudh J, Forsberg P. Lyme neuroborreliosis in children: a prospective study of clinical features, prognosis, and outcome. Pediatr Infect Dis J. 2008;27:1089–94.
Garro AC, Rutman M, Simonsen K, Jaeger JL, Chapin K, Lockhart G. Prospective validation of a clinical prediction model for Lyme meningitis in children. Pediatrics. 2009;123:1397–1398.
Douvoyiannis M, Litman N, Goldman DL. Neurologic manifestations associated with parvovirus B19 infection. Clin Infect Dis. 2009;48:1713–23.
Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL et al. The management of encephalitis: clinical practice guidelines by the infectious diseases society of America. Clin Infect Dis. 2008;47:303–26.
Gavin PJ, Kazacos KR, Shulman ST. Baylisascariasis. Clin Microbiol Rev. 2005;18:703–18.
Ramirez-Avila L, Slome S, Schuster FL, Gavali S, Schantz PM, Sejvar J, Glaser CA. Eosinophilic meningitis due to Angiostrongylus and Gnathostoma species. Clin Infect Dis. 2009;48:322–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Long, S.S. (2011). Encephalitis Diagnosis and Management in the Real World. In: Curtis, N., Finn, A., Pollard, A. (eds) Hot Topics in Infection and Immunity in Children VII. Advances in Experimental Medicine and Biology, vol 697. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-7185-2_11
Download citation
DOI: https://doi.org/10.1007/978-1-4419-7185-2_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-7184-5
Online ISBN: 978-1-4419-7185-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)