Abstract
Tumor invasion is the hallmark of malignancy. The concept of invasion consists on translocation of tumoral cells from the primary focus into neighboring host tissues, further penetration of vessel endothelium and access to the circulation to form distant metastasis (Guarino et al., Pathology 39:305–318, 2007). Therefore, invasion and metastases are connected comprising the major causes of morbidity and mortality related to cancer. They consist of multiple steps and complex processes, including cellular detachment and motility within the local microenvironment, degradation of the surrounding extracellular matrix , and cellular movement, all of which must be successfully completed to permit the growth of metastatic tumors in a new location (Ruan et al., J Cell Biochem 107:1053–1062, 2009; Liotta et al., Cell 64:327–336, 1991).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Tumor invasion is the hallmark of malignancy. The concept of invasion consists on translocation of tumoral cells from the primary focus into neighboring host tissues, further penetration of vessel endothelium and access to the circulation to form distant metastasis (Guarino et al. 2007). Therefore, invasion and metastases are connected comprising the major causes of morbidity and mortality related to cancer. They consist of multiple steps and complex processes, including cellular detachment and motility within the local microenvironment, degradation of the surrounding extracellular matrix , and cellular movement, all of which must be successfully completed to permit the growth of metastatic tumors in a new location (Ruan et al. 2009; Liotta et al. 1991).
Within a tumor, it is known that multiple signal-transduction pathways changes the adhesive and migratory capabilities of tumor cells, and tumor microenvironment have critical roles in forming an invasive front that is responsible for malignant tumor progression. At this stage of tumor development, tumor cells migrate into and invade the surrounding tissue either as single cells or in collective clusters (Christofori 2006).
The importance of changes in cell phenotype between epithelial and mesenchymal states, defined as epithelial–mesenchymal (EMT) and mesenchymal–epithelial (MET) transitions, has been increasingly recognized in the pathogenesis of cancer (Polyak and Weinberg 2009). The main characteristic of EMT is the disruption of intercellular contacts and the enhancement of cell motility. The resulting mesenchymal-like phenotype is suitable for migration . Although the molecular bases of EMT have not been completely elucidated, several interconnected transduction pathways and a number of potentially involved signaling molecules have been identified (Guarino et al. 2007).
Also, in the hypoxic environment, tumor cells undertake a series of changes not only to survive and grow in hypoxic microenvironments but also to subsequently expand and promote invasion and metastasis (Ruan et al. 2009).
2 Epithelial–Mesenchymal Transition (EMT) and Invasion
It is well known that epithelial cells are tight and closely related to each other, compounding an unmovable structure. On the other hand, mesenchymal cells are loosely-associated cells with a high capability of movement. The concept of epithelial-mesenchymal transition is related to the change of the phenotype of a malignant cell (in carcinomas) and acquisition of an ability of movement. For example, at the histological level, the invasive front of a solid carcinoma differs from the more central parts by showing a less differentiated and less cohesive architecture, where invading elements appear as individual cells or groups of very few cells in intimate connection with the peritumoural stroma (Gatenby et al. 2007) (Fig. 11.1).
Histopathology of tumours from a transgenic mouse model of pancreatic β-cell carcinogenesis (Rip1Tag)25. Note the differences between the epithelial organization of a benign adenoma (a) and the cell invasion and nuclear atypia of a malignant carcinoma (b) this transition coincides with partial epithelial–mesenchymal transition (EMT)—that is, loss of E-cadherin but not cytokeratin expression, and gain of N-cadherin but not vimentin expression (not shown) (c, d) cultured normal murine mammary gland (NMuMG) epithelial cells express E-cadherin and grow in epithelial-like sheets. On stimulation with TGF-β, the cells undergo full EMT—that is, they change to a mesenchymal, migratory phenotype through the loss of epithelial and the gain of mesenchymal gene expression, including the cadherin switch. (Christofori, G. New signals from the invasive front. Nature 441, 444–450, doi:nature04872 [pii]10.1038/nature04872 (2006))
EMT is a process, among other things, related to the invasiveness potential of the cell, which includes: disruption of intercellular adhesion mediated by cadherins at adherens junction, the loss of apicobasal polarity, cytoskeletal architecture reorganization, and the degradation of the basement membrane. At the end, the well-polarized, adhesive epithelial cells are converted to non-polarized mesenchymal cells (Ruan et al. 2009).
In fact, EMT is a physiological process seen in tissue morphogenesis during embryonic development and in some tissue fibrosis in response to injury (Guarino et al. 1999, 2007). Interestingly, many tumors have embryonic characteristics and it is hypothesized that EMT can be considered an embryonic feature acquired by tumor cells that enables them to metastasize. Carcinoma cells become more motile and able to invade by acquiring characteristics similar to embryonic mesenchymal cells, thereby allowing penetration of the stroma adjacent to the initial neoplastic focus (Gatenby et al. 2007).
The molecular mechanisms by which the cells acquire a mesenchymal phenotype are complex and involve multiple steps related to degradation and formation of some crucial proteins. The main type of adhesion system in epithelia is E-cadherin mediated cell-cell interaction. In turn, the mesenchymal cells are surrounded by an extracellular matrix and the adhesion system comprises an integrin-mediated cell-matrix interaction that allows the motility of single elements (Gatenby et al. 2007).
The pathways related to EMT-inducing includes TGF-b, Wnt, Notch, Hh, and other tumor microenvironmental signals via the activation of multiple EMT transcription factors such as Twist 1, Twist 2, Snai1, Slug, ZEB1 and ZEB2 (Ouyang et al. 2010).
The most important molecular mechanisms involved in the tumoral invasion are summarized above (Fig. 11.2).
Overview of molecular markers and cellular changes during the epithelial-mesenchymal transition (EMT). EMT is a well-coordinated event during embryonic development and a pathological feature in tumorigenesis. During the EMT process, epithelial cells undergo dramatic phenotypic changes, lose expression of E-cadherin and other components of epithelial cell junctions, adopt a mesenchymal cell phenotype, and acquire motility and invasive properties that allow them to migrate through the extracellular matrix. (Ouyang, G., Wang, Z., Fang, X., Liu, J. & Yang, C. J. Molecular signaling of the epithelial to mesenchymal transition in generating and maintaining cancer stem cells. Cell Mol Life Sci, doi:10.1007/s00018-010-0338-2 (2010)
3 Invasion and Signaling Pathways
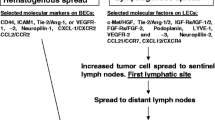
Several cellular proteins implicated in invasion and metastastic activities belong to larger families, members of which serve different activities and which may switch from one isotype to another during tumor progression (Mareel et al. 2009). On this section we will summarize only the most significant ones for invasion (Fig. 11.3).
Selected signalling pathways and some of their downstream effects and interactions are depicted. Receptor tyrosine kinases (RTKs), transforming growth factor-β (TGFβ), Notch, endothelin A receptor (ETAR), integrins, Wnt, hypoxia and matrix metalloproteinases (MMPs) can induce EMTs through multiple different signalling pathways, and the relative importance of each of these may depend on the particular cellular context. EMTs and mesenchymal–epithelial transitions (METs) are associated with dramatic changes in the cytoskeleton and extracellular matrix (ECM) composition and attachment that act together to alter cell morphology. EMT-inducing signals can lead to the disruption of tight junctions and desmosomes through protein phosphorylation (for example PAR6A phosphorylation by TGFβ signalling (Ketolainen et al. 2010)) or by repressing protein levels (for example ZEB1 represses plakophilin 3 (Ref. 83)). EMT also results in the dramatic reorganization of the ECM as many EMT-inducing factors upregulate the expression of ECM proteins (such as fibronectin and collagens), proteases (such as MMPs) and other remodelling enzymes (such as lysyl oxidase). Hypoxia, RAC1B activation and activation of certain kinase pathways (such as Akt) may lead to increased mitochondrial production of reactive oxygen species (ROS) that elicit pleiotropic effects, including activation of hypoxia-inducible factor 1α (HIF1α) and nuclear factor-κB (NF-κB) (orange circles), signalling and inactivation of glycogen synthase kinase-3β (GSK3β). Besides the interaction among the various signalling pathways, there is also extensive crosstalk among the EMT-inducing transcription factors (purple circles) and the microRNAs (miRNAs) regulating them. E-cadherin, epithelial cadherin; H/E(Spl), hairy and enhancer of split; WNTR, Wnt receptor. (Polyak, K. & Weinberg, R. A. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9, 265–273, doi:nrc2620 [pii]10.1038/nrc2620 (2009)
3.1 TGF-β
Transforming growth factor β (TGF-β ) is a multifunctional polypeptide signaling, which regulates multiple cellular processes including proliferation, apoptosis , and differentiation. It plays an important but incompletely understood role in normal and cancerous tissues (Chung et al. 2009). Actually, it has a dual role during tumour progression: as a suppressor of tumour growth during the early phases of tumorigenesis by inducing cell-cycle arrest and apoptosis; But during the late phases of carcinogenesis, it promotes EMT, tumour invasion and metastatic dissemination of tumour cells (Christofori 2006).
TGF-β signals through serine/threonine kinase receptor complexes. When activated, it regulates the transcriptional activation of various TGF-β responsive genes. In addition, TGF-β activates cellular mitogen-activated protein kinase signaling pathways, which regulate growth, survival and motility of cells. During tumorigenesis, malignantly transformed cells often lose the response to the tumor suppressive effects of TGF-β, which, in turn, starts to act as an autocrine tumor promoting factor by enhancing cancer invasion and metastasis (Nagaraj and Datta 2010). Moreover, it induces angiogenesis by upregulating the expression of angiogenic factors, such as vascular endothelial growth factor-A (VEGF-A) and angiopoietin-1 (Christofori 2006).
In breast cancer cells, a protein that belongs to the TGF-β family called bone morphogenetic protein seems to be implicated in cell growth, cell migration and invasion , and possesses both tumor suppressive and oncogenic properties in breast cancer cells (Ketolainen et al. 2010). Another in vitro studied showed that TGF-β signaling is transiently and locally activated in motile single cells. TGF-β1 switches cells from cohesive to single cell motility through a transcriptional program involving Smad4, EGFR, Nedd9, M-RIP, FARP and RhoC. Blockade of TGF-β signaling prevented cells moving singly in vivo but did not inhibit cells moving collectively. Cells restricted to collective invasion were capable of lymphatic invasion but not blood-borne metastasis (Giampieri et al. 2009).
In lung carcinoma, dysregulation of TGF-β signaling was identified as an important mediator of tumor invasion seen by microarray gene expression profiling of human tumors (Toonkel et al. 2010). Also, in prostate cancer, increased production of TGF-β causes immunosuppression , extracellular matrix degradation, EMT and angiogenesis that promotes tumor cell invasion and metastasis (Jones et al. 2009).
3.2 E-cadherin
E-cadherin , a single-span transmembrane glycoprotein of five repeats and cytoplasmic domain, is expressed primarily in epithelial cells. Its extracellular region has a Ca2+-dependent homophilic adhesion function and the cytoplasmic domain interacts with catenins. It is a tumor suppressor protein of many tumors, including breast cancer (Baranwal and Alahari 2009).
As said, epithelial cells are attached to each other by e-cadherin mediated cell-cell interaction, sustaining an immovable structure (Gatenby et al. 2007). It has been proposed that in malignant tumors, hypermethylation can down-regulate e-cadherin allowing dissociation of cells from the primary tumor enhancing the invasive capability of cells. Subsequently, a decrease in methylation with re-expression of e-cadherin in the metastatic site would restore cell-cell adhesion allowing establishment of secondary colonization (Graff et al. 2000). Moreover, experimental studies have shown that expression of e-cadherin reduces the progressiveness and invasion of tumoral cells, as well as formation of metastasis (Kowalski et al. 2003).
In several cancers, loss of e-cadherin is accompanied by a gain in the expression of n-cadherin, in a process known as ‘cadherin switch’. N-cadherin, a cadherin typically expressed in mesenchymal cells, enhances tumour cell motility and migration and exerts a dominant effect over E-cadherin function (Guarino et al. 2007). It is not a surprise that this mechanism seems to be related to the EMT of tumoral cells, in breast (Baranwal and Alahari 2009; Lester et al. 2007), prostate (Gravdal et al. 2007) and other cancers. By various mechanisms, expression of n-cadherin promotes the aggressive behavior of tumor cells, ranging from interacting with receptor tyrosine kinases at the cell surface to influencing the activation levels of Rho-GTPases in the cytosol (Baranwal and Alahari 2009).
In sporadic breast cancer, inactivation of e-cadherins is important for the cancer progression and it is completely lost in infiltrative lobular breast cancer, which suggests its function as a tumor suppressor (Baranwal and Alahari 2009). Morphologically, breast lobular carcinoma cells are more loosely infiltrative compared to others breast carcinomas. Also, abnormal expression of e-cadherins has been correlated to poor prognostic survival in patients with non-small cell lung carcinoma (Miao et al. 2009; Tseng et al. 2010; Liu et al. 2009).
In prostate cancer, loss of e-cadherin has been shown to be correlated to worse prognosis and bone metastasis (Pontes et al. 2010; Oort et al. 2007), the most common site of prostate metastatic growth. Moreover, it was demonstrated an association of the concurrent expression of unmethylated E-cadherin gene and E-cadherin protein with metastatic prostate cancer cells in bone, showing that its expression may have a role in the intercellular adhesion in the formation of metastatic lesions in bone (Saha et al. 2008).
3.3 Tyrosine-kinase receptors
Activation of tyrosine-kinase receptors is a molecular feature that leads to the migratory phenotype implicated in EMT/invasion. These receptors, located on the cell surface, are activated by growth factors (Eg.: EGF, FGF, HGF and IGF) that are related to cell proliferation differentiation and invasion (Guarino et al. 2007).
3.4 Src
Src is the prototypic member of a family of non-receptor membrane-associated tyrosine kinases including Fyn, Yes, Blk, Yrk, Fgr, Hck, Lck, and Lyn (Guarino 2010), present in several normal tissues including neurons, platelets and osteoclasts (Yeatman 2004). It translate signals from the extracellular environment into intracellular biochemical pathways that either activate nuclear factors ensuing in transcriptional responses, or target cytoplasmic components resulting in a reorganization of the cytoskeleton. Important physiological functions related to Src include cell proliferation and survival, regulation of the cytoskeleton, cell shape control, maintenance of normal intercellular contacts, cell–matrix adhesion dynamics, motility, and migration (Guarino 2010; Thomas and Brugge 1997). Src can affect cell adhesion and migration via interaction with integrins, actins, GTPase-activating proteins, scaffold proteins, such as p130(CAS) and paxillin, and kinases such as focal adhesion kinases (Kim et al. 2009). Also, Src is known to promote the expression of matrix-degrading proteases, such as metalloproteinases (MMPs), by diverse mechanisms (Guarino 2010).
It was demonstrated that in several tumors, the Src family kinases are over expressed or highly activated, and they are central mediators in multiple signaling pathways that are important in oncogenesis. Moreover, Src have a critical role in cell adhesion, invasion , proliferation, survival, and angiogenesis during tumor development. Moreover, it is involved in tumor cell proliferation and angiogenesis (Kim et al. 2009).
In prostate cancer cells, in vitro studies have shown that the chemopreventive bioflavonoid apigenin inhibits cell motility through decreasing the activation of Focal Adhesion Kinase/Src signaling (Franzen et al. 2009). Src has been shown to have a role in breast cancer, as a key co-regulator of Estrogen receptor-α, but further studies are necessary to define the potential diagnostic and prognostic value of this protein and as a possible therapeutic target (Gojis et al. 2010). It was also demonstrated that activation of Src in breast carcinoma is related to bone metastasis (Zhang et al. 2009).
Innumerous other signaling pathways exist regarding invasion and many of them are interlinked. For example, Tumor necrosis factor-α (TNF-α) also induces tumor cell invasion through NF-κB- and JNK-mediated upregulation of migration-inhibitor factor (MIF) in macrophages, through enhanced matrix metaloproteinases (see below) production or α2β1 integrin in tumour cells. Furthermore, TNF-α enhances the invasive property of cancer cells by inducing EMT through Snail- or ZEB1/ZEB2-dependent mechanisms (Wu and Zhou 2010).
4 The Relation of Hypoxia in Metastatic Signalling Pathways
As one of the most pervasive microenvironmental stresses and common features of solid tumors, hypoxia plays an important but complex role in mediating or regulating some hallmarks in the progression of human tumors from microinvasive to metastatic cancers in vivo (Ruan et al. 2009). Hypoxia induces cancer cells to adopt mechanisms that promote proliferation, induce or evade apoptosis, obtain unlimited replication potential and genomic instability, evade immune attack, induce angiogenesis, and invade and metastasize (Ruan et al. 2009).
Clinical studies have shown that tumor hypoxia is one of the important microenvironmental determinants for tumor cell dissemination (Ruan et al. 2009). In breast cancer, Gatenby et al. showed that adaptation to hypoxia may represent one of the key events during the transition from in situ to invasive breast cancer (Gatenby et al. 2007).
Hypoxia is known to activate a protein called HIF (Hypoxia Inducible Factor Protein) by regulating two major switches that converge on α subunits (Kaluz et al. 2008). In human colon carcinoma cells, hypoxia or HIF-1α over expression promotes matrigel invasion, whereas this process is inhibited by HIF-1α siRNA (Krishnamachary et al. 2003). In human pancreatic cancer cells, HIF-1α inhibition can enhance apoptosis, and restrain the invasion and metastasis (Chang et al. 2006).
It was shown that hypoxia and over expression of HIF-1 can promote EMT (see above) and metastatic phenotypes (Ruan et al. 2009; Krishnamachary et al. 2006) by upregulation of several proteins including Snail 1, Twist 1, Zeb 1 and 2 (Yang et al. 2008; Pouyssegur et al. 2006). It has been hypothesized that hypoxia within tumors, resulting in tumor necrosis, causes down regulation of E-cadherin , and ultimately sets the metastatic cascade in motion. This dysfunction of the E-cadherin–catenin complex would carry out an accumulation of β-catenin in the nucleus which is accompanied by a more invasive phenotype of tumor cells at the tumour front (Demir et al. 2009). Hypoxia may attenuate the expression of E-cadherin via activation of the lysyl oxidase (LOX)-Snail pathway, indicating that hypoxia-induced LOX and HIFs may be important factors that regulate tumor microenvironments to favor metastasis (Ruan et al. 2009).
All these data indicate that tumor hypoxia and/or HIF signaling are strongly associated with malignant progression. However, the mechanisms that result in the increased metastatic potential of tumor cells exposed to hypoxia and the exact role of HIF-1α in the metastasis still have not been well defined (Ruan et al. 2009).
Tumor hypoxia also induces tumor angiogenesis, and modulates the expression of several genes that have been implicated in tumor metastasis. For example is the hypoxic induction of c-met gene expression, which amplifies HGF signaling by sensitizing cells to HGF signaling. Thus, hypoxia seems to affect tumor cells in two ways: it induces angiogenesis (for instance, through hypoxia-inducible factor (HIF)-1α- and HIF-2α-driven expression of the angiogenic factor VEGF-A) and locally adapts the tumor environment for optimal tumor growth (Demir et al. 2009).
Tumor hypoxia can be now widely recognized as a cause of treatment failure and poor outcome for a wide variety of adult malignancies and, thus, needs to be taken into account when evaluating prognostic and therapeutic options for cancer patients. HIF-1 inhibition may represent a global strategy for targeting the hypoxic tumor microenvironment and there is an extensive effort involved in identifying more potent and specific HIF-1 inhibitors (Ruan et al. 2009).
5 Matrix Metalloproteinase (MMP) and Tumor Invasion
Degradation of the basement membrane and invasion of the underlying connective tissue by neoplastic cells are recognized as fundamental steps in the development of many epithelial cancers. Degradation of extracellular matrix (ECM) components is primarily controlled by a balance among the proteolytic enzymes called matrix metalloproteinases (MMPs) and the corresponding tissue inhibitors of MMPs (TIMPs) (Chuang et al. 2008), which are also commonly expressed in tumor sites.
Several studies suggest that MMP, a family of zinc-dependent endopeptidases, play a significant role in extracellular matrix invasion. The 23 MMPs expressed in humans are categorized by their architectural features (Kessenbrock et al. 2010). Two members of the MMP family, MMP-2 (gelatinase A, 72-kDa type IV collagenase) and MMP-9 (gelatinase B, 92-kDa type IV collagenase), are primarily responsible for invasion of the ECM and basement membrane. The expression of these gelatinases is relatively low in normal tissues and is induced when ECM remodeling is required. While gelatinase expression is primarily controlled at the transcriptional level, its activity is also regulated by post-translational factors, including proenzyme activation by membrane-type MMPs and inhibition of enzyme activity by naturally occurring TIMP (O-charoenrat et al. 2008). Because MMPs including MMP-2 are secreted as an inactive zymogen, activation is another key regulatory step for MMP function in vivo. The molecular environment in tumors appears conducive to MMP activation. Activated MMP-2 was specifically observed in a variety of tumor tissues, suggesting the presence of pro-MMP-2 activator(s) in tumor tissues (Sato and Takino 2010). Indeed, aberrant expression or activation of MMP-2 and MMP-9 has been reported in many different human tumors and has been linked to enhanced tumor invasion or metastasis in in vitro and in vivo model systems (O-charoenrat et al. 2008). Also, there are macrophage-derived MMP-2 and -9 that could act as tumor-associated macrophages that might contribute to intravasation of cancer cells into the blood stream (Kessenbrock et al. 2010).
Studies using high-resolution multimodal microscopy have showed the importance of ECM remodeling by another MMP member, the MMP-14-driven pericellular proteolysis, which potently modeled the tissue to facilitate single-cell and collective-cell migration and invasion (Kessenbrock et al. 2010; Wolf et al. 2007). A number of ECM degrading proteolytic enzymes, such as MMP-1, -2, -13, and -14 and cathepsins B, K, and L have been also implicated in this process; however MMP-14 may be critical and rate limiting in collagen turnover (Kessenbrock et al. 2010; Friedl and Wolf 2008).
In summary, MMPs have been implicated in cancer for more than 40 years, and the notion that MMP-mediated ECM degradation leads to cancer cell invasion and metastasis has been a guiding principle in MMP research (Kessenbrock et al. 2010). MMP has been asssociated to tumor invasion in breast (Hancox et al. 2009; Sun et al. 2009; Mizuma et al. 2008), lung (Lin et al. 2009), colorrectal (Kitamura et al. 2009), pancreatic (Han and Zhu 2010) and endometrial carcinoma (Wang et al. 2010), astroglial tumors (Lettau et al. 2010) and several other types of cancer, and diverse anti-MMP compounds are experimentally being tested as therapeutic drugs . Besides tissue invasion and intravasation , MMPs also affects growth signals, regulate apoptosis, tumor vasculature, and initiation of the neoplastic progression (Kessenbrock et al. 2010).
6 Contribution of the Tumor Stroma Microenvironment
In addition to the genetic, epigenetic, or somatic changes that occur in cancer, the tumor microenvironment is now considered to be a critical factor in malignant progression and metastasis , and it influences the response to conventional anti-tumor therapies (Ruan et al. 2009).
The background of the tumor microenvironment is similar to the inflammatory response in a healing wound, which promotes angiogenesis, turnover of the ECM, and tumor cell motility. Understanding the molecular mechanisms of this complex interplay between malignant cancer cells and the surrounding nonmalignant stroma represents one of the major challenges in cancer research (Kessenbrock et al. 2010).
Maintenance of epithelial tissues needs the stroma and when there is an epithelial change, the stroma also changes (Wever and Mareel 2003). The main stromal cells on this process are fibroblasts, also termed myofibroblasts or cancer-associated fibroblasts (CAFs) (Micke and Ostman 2004). In fact, the term fibroblast encompasses a number of stromal cells with a broadly similar phenotype. These cells have received increased attention because of their participation in tumor development, including invasion and metastasis (Franco et al. 2010). CAFs directly stimulate cell proliferation as they produce growth factors, hormones and cytokines such as hepatocyte growth factor, members of the epidermal growth factor, fibroblast growth factor, stromal-derived factor-1α and IL-6 (Pietras and Ostman 2010a; Kalluri and Zeisberg 2006). Moreover, CAFs are known to produce insulin-like growth factor-1 and 2, which appear to impart tumor growth by transmitting survival signals. Additionally, CAFs produces high quantities of pro-angiogenic factors, apart from VEGF-A (Pietras and Ostman 2010b).
Interestingly, in colon cancer myofibroblasts were preferentially located at the tumour–stroma border, and in invasive breast cancer, myofibroblasts were found in a much higher proportion than in in situ carcinomas, and predominantly at the invasive front (Micke and Ostman 2004). Moreover, it has been proposed that CAFs could be a new target of the cancer therapy, as shown in the Fig. 11.4.
Strategies for targeting tumour–stroma interaction. a Signals from CAFs that initiate or promote tumour growth, invasion and metastases can be inhibited. b Signals from the cancer cells that are responsible for the recruitment of CAFs can be blocked and inhibit myofibroblastic differentiation or angiogenesis. c CAF eradication leads to elimination of signals in both directions and additionally abolishes CAF effects on other stromal cells. (Micke and Ostman 2004)
7 Summary
Cancer invasion into adjacent tissue as well as vessels is a complex process mediated by diverse signaling pathways, which are usually interlinked. EMT of the cancer cells as well as degradation of the stromal proteins by MMPs are important features related to cancer invasion . The microenvironment characteristics such as hypoxia and presence of CAFs also contribute to the more invasive phenotype of cancer cells. Innumerous compounds to block these pathways are currently being studied as promising future therapies.
References
Baranwal S, Alahari SK (2009) Molecular mechanisms controlling E-cadherin expression in breast cancer. Biochem Biophys Res Commun 384:6–11
Chang Q, Qin R, Huang T, Gao J, Feng Y (2006) Effect of antisense hypoxia-inducible factor 1alpha on progression, metastasis, and chemosensitivity of pancreatic cancer. Pancreas 32:297–305
Christofori G (2006) New signals from the invasive front. Nature 441:444–450
Chuang HC et al (2008) Active matrix metalloproteinase-7 is associated with invasion in buccal squamous cell carcinoma. Mod Pathol 21:1444–1450
Chung SW et al (2009) Quantitative modeling and analysis of the transforming growth factor beta signaling pathway. Biophys J 96:1733–1750
De Wever O, Mareel M (2003) Role of tissue stroma in cancer cell invasion. J Pathol 200:429–447
Demir R et al (2009) Malignant progression of invasive tumour cells seen in hypoxia present an accumulation of beta-catenin in the nucleus at the tumour front. Exp Mol Pathol 87:109–116
Franco OE, Shaw AK, Strand DW, Hayward SW (2010) Cancer associated fibroblasts in cancer pathogenesis. Semin Cell Dev Biol 21:33–39
Franzen CA et al (2009) The chemopreventive bioflavonoid apigenin inhibits prostate cancer cell motility through the focal adhesion kinase/Src signaling mechanism. Cancer Prev Res (Phila Pa) 2:830–841
Friedl P, Wolf K (2008) Tube travel: the role of proteases in individual and collective cancer cell invasion. Cancer Res 68:7247–7249
Gatenby RA et al (2007) Cellular adaptations to hypoxia and acidosis during somatic evolution of breast cancer. Br J Cancer 97:646–653
Giampieri S et al (2009) Localized and reversible TGFbeta signalling switches breast cancer cells from cohesive to single cell motility. Nat Cell Biol 11:1287–1296
Gojis O et al (2010) The role of SRC-3 in human breast cancer. Nat Rev Clin Oncol 7:83–89
Graff JR, Gabrielson E, Fujii H, Baylin SB, Herman JG (2000) Methylation patterns of the E-cadherin 5’ CpG island are unstable and reflect the dynamic, heterogeneous loss of E-cadherin expression during metastatic progression. J Biol Chem 275:2727–2732
Gravdal K, Halvorsen OJ, Haukaas SA, Akslen LA (2007) A switch from E-cadherin to N-cadherin expression indicates epithelial to mesenchymal transition and is of strong and independent importance for the progress of prostate cancer. Clin Cancer Res 13:7003–7011
Guarino M (2010) Src signaling in cancer invasion. J Cell Physiol 223:14–26
Guarino M, Micheli P, Pallotti F, Giordano F (1999) Pathological relevance of epithelial and mesenchymal phenotype plasticity. Pathol Res Pract 195:379–389
Guarino M, Rubino B, Ballabio G (2007) The role of epithelial-mesenchymal transition in cancer pathology. Pathology 39:305–318
Han F, Zhu HG (2010) Caveolin-1 regulating the invasion and expression of matrix metalloproteinase (MMPs) in pancreatic carcinoma cells. J Surg Res 159:443–450
Hancox RA et al (2009) Tumour-associated tenascin-C isoforms promote breast cancer cell invasion and growth by matrix metalloproteinase-dependent and independent mechanisms. Breast Cancer Res 11:R24
Jones E, Pu H, Kyprianou N (2009) Targeting TGF-beta in prostate cancer: therapeutic possibilities during tumor progression. Expert Opin Ther Targets 13:227–234
Kalluri R, Zeisberg M (2006) Fibroblasts in cancer. Nat Rev Cancer 6:392–401
Kaluz S, Kaluzova M, Stanbridge EJ (2008) Does inhibition of degradation of hypoxia-inducible factor (HIF) alpha always lead to activation of HIF? Lessons learnt from the effect of proteasomal inhibition on HIF activity. J Cell Biochem 104:536–544
Kessenbrock K, Plaks V, Werb Z (2010) Matrix metalloproteinases: regulators of the tumor microenvironment. Cell 141:52–67
Ketolainen JM, Alarmo EL, Tuominen VJ, Kallioniemi A (2010) Parallel inhibition of cell growth and induction of cell migration and invasion in breast cancer cells by bone morphogenetic protein 4. Breast Cancer Res Treat
Kim LC, Song L, Haura EB (2009) Src kinases as therapeutic targets for cancer. Nat Rev Clin Oncol 6:587–595
Kitamura T, Biyajima K, Aoki M, Oshima M, Taketo MM (2009) Matrix metalloproteinase 7 is required for tumor formation, but dispensable for invasion and fibrosis in SMAD4-deficient intestinal adenocarcinomas. Lab Invest 89:98–105
Kowalski PJ, Rubin MA, Kleer CG (2003) E-cadherin expression in primary carcinomas of the breast and its distant metastases. Breast Cancer Res 5:R217–222
Krishnamachary B et al (2003) Regulation of colon carcinoma cell invasion by hypoxia-inducible factor 1. Cancer Res 63:1138–1143
Krishnamachary B et al (2006) Hypoxia-inducible factor-1-dependent repression of E-cadherin in von Hippel-Lindau tumor suppressor-null renal cell carcinoma mediated by TCF3, ZFHX1A, and ZFHX1B. Cancer Res 66:2725–2731
Lester RD, Jo M, Montel V, Takimoto S, Gonias SL (2007) uPAR induces epithelial-mesenchymal transition in hypoxic breast cancer cells. J Cell Biol 178:425–436
Lettau I et al (2010) Matrix metalloproteinase-19 is highly expressed in astroglial tumors and promotes invasion of glioma cells. J Neuropathol Exp Neurol 69:215–223
Lin SS et al (2009) Curcumin inhibits the migration and invasion of human A549 lung cancer cells through the inhibition of matrix metalloproteinase-2 and −9 and Vascular Endothelial Growth Factor (VEGF). Cancer Lett 285:127–133
Liotta LA, Steeg PS, Stetler-Stevenson WG (1991) Cancer metastasis and angiogenesis: an imbalance of positive and negative regulation. Cell 64:327–336
Liu Y et al (2009) Abnormal expression of p120-catenin, E-cadherin, and small GTPases is significantly associated with malignant phenotype of human lung cancer. Lung Cancer 63:375–382
Mareel M, Oliveira MJ, Madani I (2009) Cancer invasion and metastasis: interacting ecosystems. Virchows Arch 454:599–622
Miao Y et al (2009) p120ctn isoform 1 expression significantly correlates with abnormal expression of E-cadherin and poor survival of lung cancer patients. Med Oncol
Micke P, Ostman A (2004) Tumour-stroma interaction: cancer-associated fibroblasts as novel targets in anti-cancer therapy? Lung Cancer 45(Suppl 2):S163–175
Mizuma M et al (2008) Up-regulated p27Kip1 reduces matrix metalloproteinase-9 and inhibits invasion of human breast cancer cells. Anticancer Res 28:2669–2677
Nagaraj NS, Datta PK (2010) Targeting the transforming growth factor-beta signaling pathway in human cancer. Expert Opin Investig Drugs 19:77–91
O-charoenrat P et al (2008) SCCRO (DCUN1D1) induces extracellular matrix invasion by activating matrix metalloproteinase 2. Clin Cancer Res 14:6780–6789
Ouyang G, Wang Z, Fang X, Liu J, Yang CJ (2010) Molecular signaling of the epithelial to mesenchymal transition in generating and maintaining cancer stem cells. Cell Mol Life Sci 67:2605–2618
Pietras K, Ostman A (2010a) Hallmarks of cancer: Interactions with the tumor stroma. Exp Cell Res
Pietras K, Ostman A (2010b) Hallmarks of cancer: Interactions with the tumor stroma. Exp Cell Res 316:1324–1331
Polyak K, Weinberg RA (2009) Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9:265–273
Pontes J Jr et al (2010) E-cadherin and beta-catenin loss of expression related to bone metastasis in prostate cancer. Appl Immunohistochem Mol Morphol 18:179–184
Pouyssegur J, Dayan F, Mazure NM (2006) Hypoxia signalling in cancer and approaches to enforce tumour regression. Nature 441:437–443
Ruan K, Song G, Ouyang G (2009) Role of hypoxia in the hallmarks of human cancer. J Cell Biochem 107:1053–1062
Saha B et al (2008) Unmethylated E-cadherin gene expression is significantly associated with metastatic human prostate cancer cells in bone. Prostate 68:1681–1688
Sato H, Takino T (2010) Coordinate action of membrane-type matrix metalloproteinase —1 (MT1-MMP) and MMP-2 enhances pericellular proteolysis and invasion. Cancer Sci
Sun Y et al (2009) Oroxylin A suppresses invasion through down-regulating the expression of matrix metalloproteinase-2/9 in MDA-MB-435 human breast cancer cells. Eur J Pharmacol 603:22–28
Thomas SM, Brugge JS (1997) Cellular functions regulated by Src family kinases. Annu Rev Cell Dev Biol 13:513–609
Toonkel RL, Borczuk AC, Powell CA (2010) Tgf-beta signaling pathway in lung adenocarcinoma invasion. J Thorac Oncol 5:153–157
Tseng RC et al (2010) SLIT2 attenuation during lung cancer progression deregulates beta-catenin and E-cadherin and associates with poor prognosis. Cancer Res 70:543–551
van Oort IM et al (2007) The prognostic value of E-cadherin and the cadherin-associated molecules alpha-, beta-, gamma-catenin and p120ctn in prostate cancer specific survival: a long-term follow-up study. Prostate 67:1432–1438
Wang FQ et al (2010) Lysophosphatidic acid (LPA) effects on endometrial carcinoma in vitro proliferation, invasion, and matrix metalloproteinase activity. Gynecol Oncol 117:88–95
Wolf K et al (2007) Multi-step pericellular proteolysis controls the transition from individual to collective cancer cell invasion. Nat Cell Biol 9:893–904
Wu Y, Zhou BP (2010) TNF-alpha/NF-kappaB/Snail pathway in cancer cell migration and invasion. Br J Cancer 102:639–644
Yang MH et al (2008) Direct regulation of TWIST by HIF-1alpha promotes metastasis. Nat Cell Biol 10:295–305
Yeatman TJ (2004) A renaissance for SRC. Nat Rev Cancer 4:470–480
Zhang XH et al (2009) Latent bone metastasis in breast cancer tied to Src-dependent survival signals. Cancer Cell 16:67–78
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Pereira, P. (2013). Local Invasion. In: Burnier, J., Burnier, Jr., M. (eds) Experimental and Clinical Metastasis. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-3685-0_11
Download citation
DOI: https://doi.org/10.1007/978-1-4614-3685-0_11
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-3684-3
Online ISBN: 978-1-4614-3685-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)