Abstract
This chapter discusses the auscultation findings and fundamental clinical aspects of aortic stenosis including causes, diagnostic indicators, pathophysiology and treatment options. Aortic stenosis is a crescendo-decrescendo systolic ejection murmur with ejection click heard best at the base of the heart. The pathophysiology of aortic stenosis includes progressive stenosis over time due to calcification. This stenosis leads to an increased pressure gradient across the valve over time with a subsequently decreased ejection fraction. The decreased ejection fraction causes compensatory hypertrophic changes in the heart and leads to clinical symptoms including angina, syncope and heart failure. Treatment options for patients with aortic stenosis differ depending on a variety of factors including age, underlying cause, presence or absence of symptoms and symptom severity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Key Teaching Points
-
A crescendo-decrescendo systolic ejection murmur which may affect the quality of the carotid pulses is characteristic of aortic stenosis.
-
Auscultation findings that aid in the diagnosis of aortic stenosis include an increase in the murmur after a pause, such as an extrasystole, and diminished aortic component of the second heart sound (S2).
-
Increased intensity of the murmur, and higher murmur pitch, in addition to reduced and delayed carotid artery upstrokes, suggest a more severe stenosis.
-
There are no medical therapies for aortic stenosis. Surgery for aortic valve replacement is typically reserved for individuals with symptoms related to AS.
2 Case Description
2.1 History
A 59 year old man presents with a history of a heart murmur since childhood and was diagnosed with aortic valve disease in the late 1980s. The patient runs every other day but has noticed a recent reduction in stamina, occasional chest pain, and intermittent dizziness. He has no significant past medical history or family history of heart disease.
2.2 Physical Exam
-
BP: 131/76 mmHg.
-
Pulse: 65 bpm, regular.
-
Cardiac: No abnormal impulses.
-
Carotids: Somewhat difficult to palpate, therefore moderately diminished; delayed upstrokes noted.
-
Auscultation (Fig. 5.1).
2.3 Text Results
3 Clinical Basics
3.1 Normal Anatomy
-
The normal aortic valve has three leaflets, the right, left and noncoronary leaflet. The right coronary artery arises from the right cusp, and the left coronary artery arises from the left cusp.
-
The normal aortic valve has an area of 3–4 cm2.
3.2 Definition
-
Aortic stenosis is a pathologic narrowing of the aortic valve.
3.3 Causes
-
Causes of AS include congenital aortic stenosis, bicuspid calcific aortic stenosis, tricuspid aortic valve sclerosis and calcific stenosis.
3.4 Prevalence
The prevalence of AS increases with age:
-
0.02 % at age 18–44 years.
-
0.1 % at age 45–54 years.
-
0.2 % at age 55–64 years.
-
1.3 % at age 65–74 years.
-
2.8 % at age 75 years and older.
3.5 Pathophysiology
-
Stenosis of valve usually occurs gradually over time due to calcification.
-
The narrowing of the valve causes an increased pressure gradient across the valve leading to high velocity, turbulent ejection of blood.
-
The increased pressure gradient leads to decreased ejection fraction which subsequently causes hypertrophic changes of the heart, specifically, left ventricular hypertrophy which maintain ejection fraction.
-
The increased muscle mass of the heart puts it at an increased risk for left ventricular failure, reduced coronary blood flow per gram of muscle, and limited coronary vasodilator reserve.
3.6 Symptoms
Hallmark symptoms of aortic stenosis include:
-
Angina.
-
Syncope.
-
Heart failure.
4 Key Auscultation Features
-
Crescendo-decrescendo systolic ejection murmur with ejection click that is heard best at the base of the heart and may radiate to the carotids. The underlying physiologic cause is turbulent flow through a narrowed aortic valve.
-
Murmur intensity increases following a post-extrasystolic pause (post-extrasystolicaccentuation) and during the release phase of the Valsalva maneuver.
-
Loss of splitting of S2 (loss of A2) due to inflexible aortic leaflets closing inaudibly.
-
Presence of S4 due to vigorous atrial contraction in the face of a partially closed mitral valve during presystole.
-
Auscultation examples of aortic stenosis.
-
Click here to listen to an example of moderate aortic stenosis and see an image of the phonocardiogram (Video 5.1). The peak to peak gradient was 60 mmHg.
-
Click here to listen to an example of severe aortic stenosis as described by Dr. W. Proctor Harvey (Video 5.2).
-
5 Differential Diagnosis of Key Auscultation Features
-
A systolic murmur with ejection may arise from:
-
pulmonary valve stenosis.
-
atrial septal defect.
-
mitral regurgitation.
-
tricuspid regurgitation.
-
high cardiac output state.
-
hypertrophic obstructive cardiomyopathy.
-
-
High-pitched decrescendo diastolic murmur due to regurgitation through a compromised aortic valve.
-
Differential diagnosis for a diastolic murmur.
-
aortic regurgitation.
-
pulmonary regurgitation.
-
mitral valve stenosis.
-
tricuspid valve stenosis.
-
atrial septal defect.
-
-
6 Clinical Clues to the Detection of the Lesion
Other clinical findings to aid in the diagnosis of aortic stenosis are below:
-
Carotid pulsus parvus et tardus on palpation caused by reduced stroke volume and a prolonged ejection phase.
-
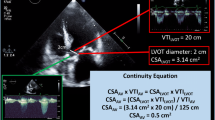
Echocardiography.
-
Reduced aortic valve area (AVA) indicative of a calcified aortic valve unable to open fully.
-
Increased velocity through the aortic valve due to elevated blood flow through a narrowed aortic valve.
-
Increased systolic pressure gradient between the left ventricle and the aorta (AV gradient) caused by left ventricular outflow obstruction in the face of a narrowed aortic valve.
-
-
ECG.
-
Left ventricular hypertrophy caused by the prolonged elevation of left ventricular contractile force required to eject blood through a stenotic aortic valve.
-
T wave inversion and ST segment depression (leads I, AVL, V5, V6) indicative of myocardial ischemia due to left ventricular dysfunction and decreased myocardial O2 supply.
-
Left atrial hypertrophy secondary to the elevated contractile force necessary to eject blood into an over-filled and hypertrophic left ventricle.
7 Classification of the Severity of Aortic Stenosis
See Fig. 5.4.
8 Diagnostic Implications of the Auscultation Features
-
Auscultation findings aid in the diagnosis of the severity of AS.
-
Increased intensity of murmur indicative of a higher pressure gradient.
-
Increased pitch of murmur correlates with a higher pressure gradient (Fig. 5.5) [1].
Fig. 5.5 Relationship between estimated auscultated murmur pressure gradient (AUSC) and the pressure gradient across the aortic valve as measured by Doppler ultrasound (DOPP). AUSC was determined by pitch of the murmur; higher frequency murmurs were assigned higher pressure gradient estimates. A clear positive correlation can be seen between Doppler-measured pressure gradients and the frequency murmurs on clinical exam (r = 0.84, p < 0.0001) (Used with permission from Phoon [1])
-
A murmur with easily heard high frequency sounds correlates to a transvalvular pressure gradient of at least 40 mmHg.
-
Later peak of murmur indicates later peak flow.
-
Single S2 due to the reduction or loss of an A2 sound.
-
-
Carotid upstroke delay and reduction due to the valve impeding ejection. The accuracy of these findings is shown in the Table 5.1.
Table 5.1 Accuracy of physical examination characteristics for prediction of a maximum Doppler echocardiographic velocity of >3.5 m/s -
A murmur grade 3 or greater, and peak in mid or late systole has the highest negative predictive value for predicting a peak velocity >3.5 m/s.
-
Abnormal carotid amplitude or delay has the highest positive predictive value for predicting high valve gradients (Fig. 5.6).
Fig. 5.6 Relationship between peak aortic valve flow velocities measured by Doppler ultrasound and the degree of carotid upstroke amplitude reduction as assessed on physical exam. Moderate and severe reductions in amplitude on clinical exam correlate with elevated peak velocities (Used with permission from Munt et al. [4])
-
9 Prognostic Implications of the Auscultation Features
9.1 Severity [2]
-
AS that is severe on exam may indicate increase risk for mortality. Severe AS is associated with a fourfold increased risk of intermediate term (4-year) all-cause and CVD mortality.
-
Symptoms are a key determinant of prognosis. “Once moderate to severe AS is present, prognosis remains excellent as long as the patient remains asymptomatic.”
9.2 Asymptomatic Patients
-
Aortic valve jet velocity on echocardiography. Graph demonstrates that reduced Vmax indicates a more severe form of stenosis and is associated with a reduced duration of event-free survival (Fig. 5.7) [3].
Fig. 5.7 Natural history of asymptomatic patients with aortic stenosis. Initial aortic jet velocity (Vmax) stratifies patients according to the likelihood that symptoms requiring valve replacement will develop over time. Most events in this series were the onset of symptoms warranting aortic valve replacement (Used with permission from Otto et al. [3])
-
>4 m/s implies 21 % 2-year free of symptoms.
-
<3 m/s implies 84 % 2-year free of symptoms.
-
-
Carotid Amplitude: A moderate to severe decrease indicates reduced event-free survival rates (Fig. 5.8) [4]. This figure indicates the correlation between carotid amplitude and duration of survival without an event. A moderate to severe decrease in carotid amplitude indicates a reduced duration of event-free survival.
Fig. 5.8 Event-free survival of patients with aortic stenosis stratified by severity of carotid upstroke amplitude reduction. Patients with moderate to severe carotid upstroke amplitude reduction on physical exam demonstrated a higher rate of mortality or valve replacement surgery than those patients with normal to mildly reduced carotid upstroke amplitude (Used with permission from Munt et al. [4])
9.3 Symptomatic Patients [5]
-
2-year survival is 50 % without aortic valve replacement.
-
5-year survival is 20 % without aortic valve replacement.
10 Statement on Management
10.1 Medical Therapies
-
In patients with rheumatic aortic stenosis antibiotic prophylaxis is indicated, to prevent against recurrent rheumatic fever.
-
Currently there is no medical therapy that has been proven to prolong life or delay the disease progression.
-
Since there is no medical therapy currently indicated, if a patient becomes symptomatic surgery is indicated.
10.2 Physical Activity
-
In patients who are asymptomatic and have mild AS there are no restrictions on the level of physical activity.
-
Limitations are recommended for patients with moderate to severe AS. These patients should not partake in competitive sports that are highly physically demanding.
-
Exercise tests can be carefully performed to determine which levels of activity are safe for the patient.
10.3 Aortic Valve Replacement [6]
10.3.1 Recommendations for Symptomatic Patients
-
In these patients aortic valve replacement (AVR) has been shown to decrease symptoms and increase survival.
-
AVR is the only effective treatment in adult patients with severe symptomatic AS.
-
Since sudden death can occur soon after symptoms present rapid progression to AVR is recommended.
-
There are generally no age limits for this surgery, though risks of the operation should be taking into account when recommending the surgery.
-
Surgical AVR is now being complemented by transcutaenous AVR in patients that are poor surgical candidates.
-
-
It is recommended that patients with severe AS who are undergoing heart surgery such as a coronary artery bypass graft procedure or a procedure on another valve should have AVR done. This is also recommended for asymptomatic patients.
10.3.2 Recommendations for Asymptomatic Patients
-
Though there is some debate it appears that most physicians believe that the risks associated with AVR outweigh the benefits when the patient is still asymptomatic.
-
Based on the STS database the mortality associated with AVR in the average hospital ranges from 3 to 4 % (and increases to 5.5–6.8 % with concurrent coronary artery bypass graft).
-
An analysis of Medicare data found that in patients over 65 the mortality rate for AVR is 8.8 %.
-
In younger patients when considering AVR with bioprothesis the breakdown of the valve over time needs to take into consideration.
-
Ultimately the risk for sudden death that can occur without the AVR needs to be weighed against the risk of the procedure. The rate of sudden death is <1 % per year.
-
10.3.3 Recommendations for Aortic Balloon Valvotomy
-
This treatment has some application in younger patients with AS.
-
It is not recommended for older patients.
-
There is a high risk of acute complications (10 %) and the majority of patients experience restenosis of the valve within a year of the procedure.
11 Clinical Summary of the Case
The patient presents with typical symptoms of aortic stenosis (reduced exertional capacity, chest pain and dizziness), in the setting of severe aortic stenosis suggested by a grade 3 murmur with abnormal carotid upstrokes. These findings predict a worse clinical outcome, and, in the setting of symptoms, warrant surgical aortic valve replacement.
References
Phoon CK. Estimation of pressure gradients by auscultation: an innovative and accurate physical examination technique. Am Heart J. 2001;141(3):500–6.
Brown J, Shah P, Stanton T, Marwick TH. Interaction and prognostic effects of left ventricular diastolic dysfunction and patient-prosthesis mismatch as determinants of outcome after isolated aortic valve replacement. Am J Cardiol. 2009;104(5):707–12.
Otto CM, Burwash IG, Legget ME, et al. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation. 1997;95(9):2262–70.
Munt B, Legget ME, Kraft CD, Miyake-Hull CY, Fujioka M, Otto CM. Physical examination in valvular aortic stenosis: correlation with stenosis severity and prediction of clinical outcome. Am Heart J. 1999;137(2):298–306.
Pibarot P, Dumesnil JG. New concepts in valvular hemodynamics: implications for diagnosis and treatment of aortic stenosis. Can J Cardiol. 2007;23:40B–7.
Bonow RO, Carabello BA, Chatterjee K, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008;52(13):e1–142.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Video 5.1
Example of moderate aortic stenosis: 60 mmHg peak gradient (Provided by Robin Winkler Doroshow, MD, Medstar Georgetown University Hospital, Washington, DC) (MP4 1106 kb)
Video 5.2
73-year-old-man with severe AS as described by Dr. W. Proctor Harvey (File 198 from Clinical Cardiology by W. Proctor Harvey, MD, MACC, Jules Bedynek, MD, and David Canfield and published by Laennec Publishing Inc., Fairfield, NJ. Used with permission and copyrighted by Laennec Publishing, Inc. All rights reserved) (MP4 5791 kb)
Rights and permissions
Copyright information
© 2015 Springer-Verlag London
About this chapter
Cite this chapter
Kammel, J.M., Bence, C.M., Money, A.J., Swinford, S.T. (2015). Aortic Stenosis. In: Taylor, A. (eds) Learning Cardiac Auscultation. Springer, London. https://doi.org/10.1007/978-1-4471-6738-9_5
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6738-9_5
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6737-2
Online ISBN: 978-1-4471-6738-9
eBook Packages: MedicineMedicine (R0)