Abstract
This case reviews the various options for treating arterial rupture post-angioplasty including a discussion of principles to be adhered to in order to avoid such a situation in the first place.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Case History
A 68-year-old gentleman attended for right SFA angioplasty for recent onset short distance claudication. Past medical history included a prosthetic aortic valve, CABG, and TIA 10 years previously. The patient was on regular aspirin 75 mg OD and warfarin; the pre-procedural INR was 1.4 and hemoglobin and platelet count were normal.
Procedure
Arterial access was via a right CFA antegrade puncture and placement of a 6 Fr sheath, although insertion of the 6 Fr sheath was difficult due to soft tissue resistance. Angiograms demonstrated a 6 cm occlusion of the mid to distal SFA (Fig. 8.1a, b). Recanalization was successful via a subintimal passage because of the heavily calcified plaque.
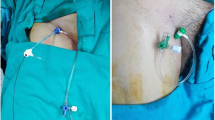
Following angioplasty, there was extravasation of contrast from the angioplasty site (Fig. 8.2a). Balloon occlusion across the leak was successfully performed resulting in only minimal subsequent extravasation. Due to residual stenosis of the proximal portion of the plaque, an uncovered stent was inserted (Bard Luminexx −6 × 80 mm). At the end of the procedure, following stent placement, there remained minor extravasation extending approximately 1–2 cm around the site of rupture (Fig. 8.2b).
Placement of a covered stent/stent-graft was considered but would have required insertion of an 8 Fr antegrade sheath. Due to the difficulties with initial antegrade access, it was decided to avoid this and review the patient following overnight observation and an ultrasound duplex the following day. The duplex study demonstrated patent artery and no residual bleeding. No further intervention was required and the patient was discharged the following day.
Discussion
Vessel rupture is the most serious complication encountered following angioplasty. In the peripheral circulation this is usually self-limiting due to tamponade by the surrounding soft tissues; however, if in the thorax or abdomen, vessel rupture is usually life-threatening. Aside from angiographic evidence of contrast extravasation, clinical indicators of vessel rupture include severe pain experienced by the patient and hemodynamic deterioration.
If the vessel rupture is in the peripheral circulation and is minor, then conservative management may be all that is necessary. Immediate management of vessel rupture in the thorax or abdomen involves maintenance of guidewire access of the ruptured artery followed by immediate balloon reinflation across the extravasation site to control bleeding with subsequent placement of a stent-graft. Alternatively, embolization of the artery can be performed followed by bypass surgery, or the patient may be transferred to theatre for surgical repair.
Rupture occurs more commonly due to eccentric calcified plaque at the angioplasty site, following use of a cutting balloon or high-pressure balloon angioplasty. Avoidance of vessel rupture is potentially aided by adhering to good principles of angioplasty. Most interventional radiologists choose angioplasty balloon diameters based on visual estimation. If in doubt, use of a balloon of smaller diameter with an accurate roadmap is recommended, and if the balloon is too small, then repeat angioplasty with a larger one can be performed subsequently.
Attention to the angioplasty balloon manufacturer’s recommendations is important. The nominal pressure is the pressure at which the balloon reaches its rated diameter. The burst pressure is the average pressure that is required to rupture the balloon. The rated burst pressure is the highest pressure to which the balloon can be inflated with minimal chance of bursting. Use of a pressure inflation device allows more accurate inflation to the recommended pressures. The case described above also illustrates that vessel rupture or extravasation in the peripheral arteries does not necessarily require stent-graft insertion.
The use of covered stents traditionally requires a large sheath, usually greater than 8 Fr. Newer developments in stent-graft technology mean that 6 or 7 Fr sheaths can be used for the SFA or other vessels of the order of 6–7 mm diameter. Examples are the Gore® Viabahn® and Atrium™ Advanta V12 covered stents. With familiarity and knowledge of different techniques and available stent-grafts operators can usually deal with most vessel ruptures by endovascular means.
Commentary
As illustrated by the case above, arterial rupture does not always require placement of a stent-graft in the peripheral circulation and often responds to conservative measures. Rupture as a result of extraluminal recanalization during angioplasty is often self-limiting. When performing subintimal angioplasty, it is crucial to confirm that you are back in the true lumen of the parent vessel and not in a branch vessel before performing balloon dilatation. Rupture of a branch vessel is less likely to be self-limiting. In such a situation, prolonged balloon dilatation (5–10 min) across the origin of the branch vessel should be performed. If the bleeding does not stop and the vessel can be occluded, coil embolization of the vessel can be performed which will stop the bleeding.
When performing angioplasty, in particular within the thorax and abdomen, it is good practice to ensure that an appropriate size stent-graft and sheath are available in the interventional room at the beginning of the procedure. Should there be a vessel rupture, this minimizes time taken to proceed to appropriate endovascular treatment. Many units have a “rupture box” containing the appropriate equipment, primarily for dealing with iliac ruptures.
Further Reading
Tsetis D. Endovascular treatment of complications of femoral arterial access. Cardiovasc Intervent Radiol. 2010;33(3):457–68.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Allison, R.P. et al. (2014). Superficial Femoral Artery Rupture Following Angioplasty. In: Ratnam, L., Patel, U., Belli, A. (eds) Managing Common Interventional Radiology Complications. Springer, London. https://doi.org/10.1007/978-1-4471-5502-7_8
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5502-7_8
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5501-0
Online ISBN: 978-1-4471-5502-7
eBook Packages: MedicineMedicine (R0)