Abstract
Peripheral vascular disease is better recognized as an epidemic that’s impacting millions of patients and their families. Health-care providers currently consider PVD as a significant comorbidity and have been actively screening, treating, and spreading public awareness. In addition to medical therapy, surgery has been considered the mainstay of therapy for years. The recent advancement in endovascular technology and the increasing level of expertise by endovascular specialist allow revascularization in patients deemed inoperable in the past. This chapter highlights through our case presentation the current evidence behind endovascular therapy in patients with superficial femoral artery disease. We also discuss some of the current devices available and used by endovascular operators.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Peripheral Vascular Disease
- Limb Salvage
- Superficial Femoral Artery
- Critical Limb Ischemia
- Chronic Total Occlusion
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Background
Over the past decade, considerable progress has been made in endovascular therapy treatment of patients with peripheral vascular disease (PVD). Surgical bypass, while effective and safe, is losing ground to less invasive endovascular techniques [1]. PVD is on the rise in the United States. It is estimated that 20 % of patients >75 years will be living with the disease by the year 2030 [2]. The prevalence of PVD is particularly more common in high-risk groups such as patients with diabetes mellitus (DM), hypertension (HTN), hyperlipidemia, and smoking [3]. A significant proportion of earlier trials comparing surgery to endovascular therapy have been limited in size and have primarily compared balloon angioplasty results [4]. The recent trial of bypass versus angioplasty in severe ischemia of the leg (BASIL trial) provided evidence that endovascular therapy can be as effective as surgery in patients with critical limb ischemia [5]. The trial, while recent by time standards, lags significantly due to rapidly evolving technology. In an effort to categorize the anatomical properties of the femoral popliteal lesions, the Transatlantic Inter-Society Consensus (TASC) divided these lesions in four categories. This classification has been recently updated to TASC II (Fig. 52.1) [6].
Case Presentation
Here, we describe a patient referred to our institution from his primary care physician’s office. The patient is a 56-year-old Caucasian male with a past medical history significant for hypertension and hyperlipidemia and a remote history of smoking. The patient presented mainly with pain on exertion involving his left leg. Initially, the patient thought it might be related to arthritis in his left knee. Despite a trial of nonsteroidal anti-inflammatory drugs, his pain continued to worsen. His symptoms appear mainly with ambulation. Peripheral vascular disease was suspected as possibly the culprit. In our office, the exam revealed a well-nourished male. His vascular exam revealed equal blood pressure in both arms. Radial and femoral pulses were both equal. There was evidence of a soft left femoral bruit. The popliteal, posterior tibial, and dorsalis pedis pulses were all absent on the left side. The popliteal, posterior tibial, and dorsalis pedis on the right were graded at +1. Handheld Doppler showed evidence of biphasic flow in the left posterior tibial and dorsalis pedis artery. An ankle-brachial index measured at 0.8 on the right and 0.6 on the left. The patient complained of left lower extremity pain with walking less than 200 ft, clearly indicative of significant claudication. The patient was placed at Rutherford class III. The Rutherford classification is a clinical tool that grades the degree of PVD based on the patient’s symptoms (Table 52.1) [7]. There was no evidence of any wounds or ulcers involving the left lower extremity. Our physical exam and the clinical scenario identified the arterial level of disease at the superficial femoral artery (SFA) or the popliteal vessels. The patient was scheduled for an elective angiogram of the left lower extremity with a plan to revascularize the SFA.
The practical steps involving the revascularization process are numbered below:
-
1.
The right common femoral artery was chosen for access in this patient. The operator chose a retrograde approach.
-
2.
The operator used a combination of fluoroscopy- and ultrasound-guided techniques to evaluate the access site. Vascular access is an important aspect of any endovascular procedure.
-
3.
With fluoroscopy, the operator identified the femoral head as the area of interest. A handheld ultrasound was used to identify the common femoral artery. The operator identified the bifurcation of the profunda and the SFA (Fig. 52.2).
-
4.
Under direct visualization, the common femoral artery was accessed.
-
5.
A 5 French 11 cm sheath was introduced into the right common femoral artery.
-
6.
A rim catheter was introduced into the lower abdominal aorta. Under fluoroscopic guidance, the contralateral left iliac system was engaged.
-
7.
A road map was created. A 0.035″ glide wire was advanced into the left common femoral artery (Fig. 52.3).
-
8.
The Rim catheter was advanced over the glide wire to the left common femoral artery.
-
9.
The glide wire was withdrawn and angiographic images of the SFA and popliteal arteries were obtained.
-
10.
Images identified multiple tandem lesions in the distal SFA (Fig. 52.4).
-
11.
It is the opinion of these authors that atherectomy should be employed in treating atherosclerotic lesions. Plaque modification is an important step in treating the vessel.
-
12.
We proceeded with the placement of a 0.035″ “Magic Torque wire” (Boston Scientific, Miami, FL) into a relatively healthy segment of the proximal SFA.
-
13.
A 7 French Destination Pinnacle sheath (Terumo Interventional Systems, Somerset, NJ) was advanced under fluoroscopic guidance into the proximal SFA.
-
14.
Antithrombotic therapy with heparin was initiated on a weight-adjusted bases. Typically, we bolus the patient with 60 units/kg. Our ACT target is in the 250 range.
-
15.
A soft-angled glide wire was manipulated across the lesion into the infrapopliteal segment.
-
16.
Utilizing a 0.035″ exchange catheter, we exchanged the glide wire for a 0.009 Viper Wire (Cardiovascular Systems, Inc.).
-
17.
We decided to perform orbital atherectomy using a 1.5 mm Diamondback Classic Crown (Cardiovascular Systems, Inc.). The CSI system utilizes a differential sanding system that modifies the atherosclerotic plaque, changing the compliance of the vessel wall and allowing for a more sustained and controlled angioplasty result.
-
18.
We then proceeded with performing balloon angioplasty of the distal portion of the SFA and the proximal popliteal. The operator utilized a 5.0 × 120 mm Mustang balloon (Boston Scientific, Natick, MA) that was inflated at 4 atmospheric pressure for 2 min. Repeated angiogram showed type C dissection in a focal area with contrast stagnation.
-
19.
Repeat balloon angioplasty did not resolve or tack up the type C dissection (Fig. 52.5). Decision was made to proceed with stent placement. 5 × 160 mm Supera stent (IDEV, Houston, TX) was deployed with excellent TIMI III flow and resolution of the type C dissection (Fig. 52.6).
The patient was discharged home the following day. At 3-month follow-up, he was asymptomatic, Rutherford 0 category.
Discussion
With the increasing prevalence of PVD in an aging population and the limitation of vascular surgery in patients with significant comorbidities, operators are gravitating more toward less invasive endovascular therapy. Both approaches have been proven equivalent in patients with critical limb ischemia (CLI) [5]. The use of balloon angioplasty (POBA) has been shown to be effective. However, the benefit is limited to short, noncomplex lesions [8]. In contrast, trials have shown superior long-term patency with moderate length lesions when stents were used as compared to POBA only [9–11]. Earlier trials have failed to document or compare the difference between subintimal and intraluminal interventions. Nonetheless, most operators prefer to remain intraluminal whenever the conditions allow. Whatever the modality of crossing the lesion, stenting appears to yield better results compared to angioplasty alone. In essence, selective stenting depending on the lesion length and characteristics will offer the most sustainable results. We believe that POBA should be the first option of therapy in patients with the less complex, short TASC II A and B lesions. Stenting appears to provide a more favorable outcome in patients with complex, long TASC II C and D lesions. In a study by Nguyen et al., stenting had a better primary patency rate at long-term follow-up (up to 98 months) [12]. In the above-mentioned trial, the primary patency rate in patients treated with POBA was 27 % compared to 36 % in the stenting arm. More than 70 % of patients were categorized at TASC II A and B. However, the limb salvage rates were at 80–90 %. These rates are certainly comparable to autogenous vein grafts and certainly better than prosthetic conduits [13, 14]. As endovascular techniques continue to evolve, the durability and sustainability of treatment options will improve. Data regarding TASC II C and D are scarce. The results of balloon angioplasty in long and complex lesions have been disappointing. In patients with chronic total occlusion (CTO) and TASC II C and D lesions, the use of subintimal angioplasty has been adopted by many operators. The technique relies on deliberately dissecting the vessel proximal to the lesion. This method has a good technical success rate; however, the 12-month patency rates ranged anywhere from 22 to 79 % [15–19]. In a recent paper by Boisers et al., the 12-month primary patency rate related to the use of long stents (>200 mm) in 100 patients with TASC II C and D lesions was 64.5 %. Each patient received on average 1.5 stents [20]. The authors of this chapter tend to use, as many other operators, selective stenting in patients with long and complex lesions. We tend to reserve POBA to short and less complex lesions.
Another modality of peripheral vascular revascularization resorts to plaque modification with excision and atherectomy. Endovascular plaque excision is a catheter-based approach where plaque removal improves blood flow in the area supplied. Plaque excision has several theoretical advantages compared to balloon angioplasty or stent placement. There is lack of barotrauma or dottering effect when the vessel is treated with atherectomy. One of the commonly used atherectomy devices is the SilverHawk device (Fig. 52.7) (Covidien/EV3, Mansfield, MA). It consists of a metal chamber containing a cylindrical knife. The excised plaque is caught in a metal housing distal to the cutting mechanism. When the metal housing is full, it needs to be emptied to reuse the device. The device has been evaluated in multiple small trials, [21–25]. One of the largest series was the data reported from treating peripherals with SilverHawk: Outcomes Collection (TALON Registry). In a midterm analysis, 1,258 patients with Rutherford scale >4 underwent atherectomy with the SilverHawk device. Freedom from target lesion revascularization was reported at 80 % in 1 year [26]. Nearly 73 % of lesions did not require any additional therapy. Only 6 % of patients required additional stent placement. Perforation was reported in 0.8 % of patients. The Diamondback 360 orbital atherectomy (Cardiovascular Systems Inc, St. Paul, MN) is a device that was initially advocated for the treatment of tibial vessels (Fig. 52.8). The device employs a diamond-coated crown that rotates at high speeds to sand away plaque as it slowly advances through atherosclerotic lesions [27]. Atherectomy results of this device have been favorable in the tibial vessels [28]. The device has been traditionally used for SFA disease because of ease of use and low profile. Another new device is the Jetstream atherectomy system (Pathway Medical Technologies, Kirkland, WA) that employs a cutting tip (Fig. 52.9). The tip remains at a certain diameter (2.1 mm) as it rotates clockwise. The cutting tip expands to 3 mm when it is rotating counterclockwise. The excised material is aspirated through ports within the tip into an aspiration bag. This device has the theoretical advantage of modifying the vessel compliance with decreased risk of aspiration. Another atherectomy device is the excimer laser (Spectranetics, Colorado Springs, CO) (Fig. 52.10). The laser acts by creating a vapor bubble that ablates the plaque up to 50 μm in depth. It is essential to ablate at a steady rate of 1 mm/s to achieve the best results. The benefits of laser therapy have been highlighted in limb salvage following laser-assisted angioplasty for critical limb ischemia (LACI trial) [29]. The LACI was a multicenter trial (15 sites in the United States and 1 German site) that enrolled 145 CLI patients with 155 ischemic limbs classified as Rutherford Class IV–VI. The patients were considered poor or nonsurgical candidates. This was a limb salvage trial with 41 % of the lesions treated in the SFA. At 6-month follow-up, the rate of limb salvage was reported at 92 %.
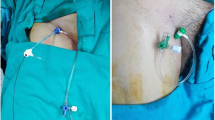
Recently, the Crosser recanalization system (Bard Peripheral Vascular, Tempe, AZ) has been approved as an atherectomy device (Fig. 52.11a, b). The Crosser system employs ultrasonic vibration that is created by conversion of electrical energy through piezoelectric crystals within the system. Ultimately, the vibration will help guide the catheter through the vessel. The technique is very helpful in patients with chronic total occlusions.
The treatment of SFA disease is changing rapidly. All the techniques described above have both multiple benefits and drawbacks. The operator needs to choose the appropriate technique depending on the patient presentation and lesion characteristics. Table 52.2 describes the authors’ own experience in applying these modalities. Until we have more clear evidence that supports one modality over the other, clinical judgment and experience will guide the treatment plan. The near future may hold the answers with the introduction of drug-eluting balloons and bio-absorbable stents. The success of these techniques will depend initially on operator skill and experience. It is the responsibility of the operator to document the outcomes of these procedures to adequately capture the impact of these new technologies on patient care.
References
Bates MC, Aburahma AF. An update on endovascular therapy of the lower extremities. J Endovasc Ther. 2004;11 Suppl 2:II107–27.
Shammas NW. Epidemiology, classification, and modifiable risk factors of peripheral arterial disease. Vasc Health Risk Manag. 2007;3(2):229–34.
McDermott MM. The magnitude of the problem of peripheral arterial disease: epidemiology and clinical significance. Cleve Clin J Med. 2006;73 Suppl 4:S2–7.
Cheng SW, Ting AC, Ho P. Angioplasty and primary stenting of high-grade, long-segment superficial femoral artery disease: is it worthwhile? Ann Vasc Surg. 2003;17(4):430–7.
Forbes JF, Adam DJ, Bell J, Fowkes FG, Gillespie I, Raab GM, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: health-related quality of life outcomes, resource utilization, and cost-effectiveness analysis. J Vasc Surg. 2010;51(5 Suppl):43S–5151.
Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007;45(Suppl S):S5–67.
Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, et al. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997;26(3):517–38.
Krankenberg H, Schluter M, Steinkamp HJ, Burgelin K, Scheinert D, Schulte KL, et al. Nitinol stent implantation versus percutaneous transluminal angioplasty in superficial femoral artery lesions up to 10 cm in length: the femoral artery stenting trial (FAST). Circulation. 2007;116(3):285–92.
Laird JR, Katzen BT, Scheinert D, Lammer J, Carpenter J, Buchbinder M, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv. 2010;3(3):267–76.
Schillinger M, Sabeti S, Dick P, Amighi J, Mlekusch W, Schlager O, et al. Sustained benefit at 2 years of primary femoropopliteal stenting compared with balloon angioplasty with optional stenting. Circulation. 2007;115(21):2745–9.
Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006;354(18):1879–88.
Nguyen BN, Conrad MF, Guest JM, Hackney L, Patel VI, Kwolek CJ, et al. Late outcomes of balloon angioplasty and angioplasty with selective stenting for superficial femoral-popliteal disease are equivalent. J Vasc Surg. 2011;54(4):1051–7.e1.
Faries PL, Logerfo FW, Arora S, Hook S, Pulling MC, Akbari CM, et al. A comparative study of alternative conduits for lower extremity revascularization: all-autogenous conduit versus prosthetic grafts. J Vasc Surg. 2000;32(6):1080–90.
Nasr MK, McCarthy RJ, Budd JS, Horrocks M. Infrainguinal bypass graft patency and limb salvage rates in critical limb ischemia: influence of the mode of presentation. Ann Vasc Surg. 2003;17(2):192–7.
Desgranges P, Boufi M, Lapeyre M, Tarquini G, van Laere O, Losy F, et al. Subintimal angioplasty: feasible and durable. Eur J Vasc Endovasc Surg. 2004;28(2):138–41.
Laxdal E, Jenssen GL, Pedersen G, Aune S. Subintimal angioplasty as a treatment of femoropopliteal artery occlusions. Eur J Vasc Endovasc Surg. 2003;25(6):578–82.
Markose G, Miller FN, Bolia A. Subintimal angioplasty for femoro-popliteal occlusive disease. J Vasc Surg. 2010;52(5):1410–6.
Nydahl S, Hartshorne T, Bell PR, Bolia A, London NJ. Subintimal angioplasty of infrapopliteal occlusions in critically ischaemic limbs. Eur J Vasc Endovasc Surg. 1997;14(3):212–6.
Vraux H, Hammer F, Verhelst R, Goffette P, Vandeleene B. Subintimal angioplasty of tibial vessel occlusions in the treatment of critical limb ischaemia: mid-term results. Eur J Vasc Endovasc Surg. 2000;20(5):441–6.
Bosiers M, Deloose K, Callaert J, Moreels N, Keirse K, Verbist J, et al. Results of the Protege EverFlex 200-mm-long nitinol stent (ev3) in TASC C and D femoropopliteal lesions. J Vasc Surg. 2011;54(4):1042–50.
Zeller T, Frank U, Burgelin K, Schwarzwalder U, Flugel PC, Neumann FJ. Initial clinical experience with percutaneous atherectomy in the infragenicular arteries. J Endovasc Ther. 2003;10(5):987–93.
Zeller T, Rastan A, Schwarzwalder U, Frank U, Burgelin K, Amantea P, et al. Percutaneous peripheral atherectomy of femoropopliteal stenoses using a new-generation device: six-month results from a single-center experience. J Endovasc Ther. 2004;11(6):676–85.
Zeller T, Rastan A, Schwarzwalder U, Frank U, Burgelin K, Amantea P, et al. Midterm results after atherectomy-assisted angioplasty of below-knee arteries with use of the Silverhawk device. J Vasc Interv Radiol. 2004;15(12):1391–7.
Zeller T, Rastan A, Sixt S, Schwarzwalder U, Schwarz T, Frank U, et al. Long-term results after directional atherectomy of femoro-popliteal lesions. J Am Coll Cardiol. 2006;48(8):1573–8.
Zeller T, Sixt S, Schwarzwalder U, Schwarz T, Frank U, Burgelin K, et al. Two-year results after directional atherectomy of infrapopliteal arteries with the SilverHawk device. J Endovasc Ther. 2007;14(2):232–40.
Ramaiah V, Gammon R, Kiesz S, Cardenas J, Runyon JP, Fail P, et al. Midterm outcomes from the TALON Registry: treating peripherals with SilverHawk: outcomes collection. J Endovasc Ther. 2006;13(5):592–602.
Heuser RR. Treatment of lower extremity vascular disease: the Diamondback 360 degrees Orbital Atherectomy System. Expert Rev Med Devices. 2008;5(3):279–86.
Safian RD, Niazi K, Runyon JP, Dulas D, Weinstock B, Ramaiah V, et al. Orbital atherectomy for infrapopliteal disease: device concept and outcome data for the OASIS trial. Catheter Cardiovasc Interv. 2009;73(3):406–12.
Laird JR, Zeller T, Gray BH, Scheinert D, Vranic M, Reiser C, et al. Limb salvage following laser-assisted angioplasty for critical limb ischemia: results of the LACI multicenter trial. J Endovasc Ther. 2006;13(1):1–11.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Mustapha, J.A., Das, T., Saab, F.A. (2014). Superficial Femoral Artery Endovascular Therapy with Atherectomy. In: Dieter, R., Dieter, Jr., R., Dieter, III, R. (eds) Endovascular Interventions. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7312-1_52
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7312-1_52
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7311-4
Online ISBN: 978-1-4614-7312-1
eBook Packages: MedicineMedicine (R0)