Abstract
Singh M, Nagrath AR, Maini PS.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Author
Singh M, Nagrath AR, Maini PS.
2 Reference
J Bone Joint Surg Am. 1970;53:1063–7.
3 Institution
Department of Orthopaedic Surgery, Medical College Hospital, Rohtak, Haryana, India
4 Abstract
Radiographs of the hip region, in a series of 35 patients older than 50 years, were studied with reference to the trabecular pattern of the upper end of the femur. The findings were linked with the clinical data and the Beck and Nordin iliac crest biopsy rating of the same patients.
It was found that definite progressive changes occurred in the trabeculae of the upper end of the femur as normal bone deteriorates to severe osteoporosis. With increasing degrees of bone loss, six different trabecular patterns are found in the upper femur. It is proposed that these patterns can be used as a radiographic scale for the diagnosis and grading of osteoporosis.
5 Summary
Singh and associates report the progressive structural changes that occur in the trabecular pattern of the proximal femur as normal bone deteriorates to severe osteoporosis with age. They describe six trabecular patterns. They reported a good correlation between the histological findings of the iliac crest biopsy and this grading system. The pattern of trabeculae loss thus provided a semi-quantitative estimate of osteoporosis.
6 Citation Count
576
7 Related References
-
1.
Pramudito J, Soegijoko S, et al. Trabecular pattern analysis of proximal femur radiographs for osteoporosis detection. J Biomed Pharm Eng. 2007;1(1):45–51.
-
2.
Koot V, Kesselaer S, et al. Evaluation of the Singh index for measuring osteoporosis. J Bone Joint Surg Br.1996;78(5):831.
-
3.
Legrand E, Chappard D, Pascaretti C, Duquenne M, Krebs S, Rohmer V, et al. Trabecular bone microarchitecture, bone mineral density, and vertebral fractures in male osteoporosis. J Bone Miner Res. 2000;15(1):13–9.
8 Key Message
The Singh index (SI) historically has been used in the diagnosis and classification of osteoporosis. It is based on the radiological appearance of trabecular bone structure of the proximal femur on a plain anteroposterior (AP) radiograph.
Today it has little practical value in modern orthopaedics practice as this method has been superceeded by Dual-energy X-ray absorptiometry (DEXA) scan. DEXA scan provides a more precise estimate of bone mineral density and is considered the gold standard for diagnosis and quantification of osteoporosis [1].
9 Why It’s Important
Osteoporotic fractures are a major public health problem in developed countries in terms of morbidity, mortality and cost, with bone mineral density (BMD) being a major determinant of future fracture risk.
The Singh index is a simple radiographic method for estimating bone mass in bones suspected of osteoporosis. A typical Singh index describes the pattern of trabeculae in the proximal femur.
Before the introduction of DEXA scans it was probably the most widely used method of estimating the degree of osteoporosis in clinical and research articles.
10 Strengths
The Singh index is a simple, cheap method for giving a rough measurement of bone mass that may still be used to classify osteoporosis grade in countries where access to DEXA scanning is limited.
Although Singh’s index has a low sensitivity, it is specific in diagnosing low bone mass, suggesting its suitability for use in classifying large populations, but not individuals with osteoporosis [2].
11 Weaknesses
Several studies have found that the Singh index is an inaccurate technique of measuring bone mineral density when compared to DEXA scanning [1, 3]. They caution against its use suggesting the Singh index has no value in assessing the grade of osteoporosis.
The Singh index has also been criticised for its poor interobserver and intraobserver levels of agreement and poor diagnostic value in the screening of femoral neck osteoporosis.
Koot et al. [4] reported significant interobserver disagreement when radiographs of hip fracture patients were assessed by 6 different observers. Only 3 of 72 radiographs were given the same grading by all six observers with Kappa values ranging from 0.15 to 0.54. Intraobserver rates were much better with a kappa value from 0.63 to 0.88.
Intraobserver agreement is generally less important than interobserver agreement, since different observers apply the Singh index in a different way.
Older criticisms, probably not now relevant are the suggestion that the index needed to be simplified in order to increase its reliability. It relies on observation and thus has an inherent drawback. The limitations of plain radiographs include inability to see the trabeculae clearly due to soft tissue shadow in a fatty patient with bulky thighs and buttocks and the possibility of poor quality radiographs due to a technical lag.
12 Relevance
The cancellous bone of the upper end of the femur is composed of two distinct systems of trabeculae. In the frontal section, these trabeculae are seen to form two arches, one arising from the medial (or inner) cortex of the shaft of femur and the other from the lateral (or outer) cortex. The trabeculae forming these arches are called compressive and tensile trabeculae because they are disposed along the lines of maximum compression and tension stresses produced in the bone during weight bearing. These trabeculae are divided into five groups:
-
1.
The principle compressive group, which extends from the medial cortex of the femoral neck to the upper portion of the femoral head in slightly curved radial lines
-
2.
The secondary compressive group, which curves upwards and slightly laterally towards the greater trochanter and the upper portion of the femoral neck
-
3.
The greater trochanter group, which arises laterally below the greater trochanter and extends upwards to terminate near its superior surface
-
4.
The principle tensile group, which extends in a curvillnear fashion and medially across the femoral neck, ending in the inferior portion of the femoral head
-
5.
The secondary tensile group, which extends superiorly and medially to terminate after crossing the middle of the femoral
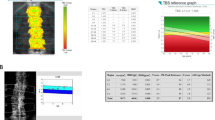
The trabeculae in the upper end of the femur of normal individuals are arranged along the lines of compression and tension stresses produced in the bone during weight bearing [3]. The Singh index assesses patterns of trabecular loss with 6 different patterns recognised representing increased degrees of bone loss (See Table 31.1 and Fig. 31.1)
With early trabecular resorption, the principal compressive and principal tensile trabecular groups become accentuated. With increasing resorption, the tensile trabeculae become reduced in number. Progressive loss of trabeculae leads to disappearance of the outer portion of the principal tensile trabeculae opposite the greater trochanter. Resorption of all trabecular groups except the bony trabeculae in the principal compressive group follows, although in severe osteoporosis, even these latter trabeculae may be obliterated partially or complete.
Singh et al. devised their index of osteopenia grading after showing a good correlation between histological osteopenia grading of iliac crest biopsies and trabecular pattern grading of the contralateral hip radiographs in 35 patients aged over 50 years. Later studies assessing the Singh Index histopathologically and correlating it with fractures, bone mineral content and density have shown conflicting results [5, 6].
Although conventional radiography is widely available and inexpensive compared to DEXA scans it has a low sensitivity in diagnosing osteopenia and traditionally it is thought that at least 30 % of bone calcium content must be lost before it can be detected by plain radiography.
In summary the Singh index has been shown to be an inaccurate method of estimating the degree of osteoporosis and the technique is not relevant with the current use of DEXA scans. As such this article is more of historic interest and will gradually assume less importance as its citation rank decreases in time.
References
Gulati D, Kumar S, Arora A, Aggarwal AN, Bhargava SK. Bone mineral density in young Indian adults with traumatic proximal femoral fractures. A case control study. Acta Orthop Belg. 2010;76(3):335–40.
Masud T, Jawed S, Doyle DV, Spector TD. A population study of the screening potential of assessment of trabecular pattern of the femoral neck (Singh index): the Chingford Study. Br J Radiol. 1995;68(808):389–93.
Wachter NJ, Augat P, Hoellen IP, Krischak GD. Predictive value of Singh index and bone mineral density measured by quantitative computed tomography in determining the local cancellous bone quality of the proximal femur. Clin Biomech. 2001;16:257–62.
Koot V, Kesselaer S, Clevers GJ, De Hooge P, Weits T, van der Werken C. Evaluation of the Singh index for measuring osteoporosis. J Bone Joint Surg Br. 1996;78(5):831.
Wilkinson JM, Cotton DW, Harris SC, Patterson EA. Assessment of osteoporosis at autopsy: mechanical methods compared to radiological and histological techniques. Med Sci Law. 1991;31(1):19–24.
Robertson A. Singh and metacarpal cortical indices. Australas Radiol. 1978;22(3):257–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Banaszkiewicz, P.A. (2014). Changes in Trabecular Pattern of the Upper End of the Femur as an Index of Osteoporosis. In: Banaszkiewicz, P., Kader, D. (eds) Classic Papers in Orthopaedics. Springer, London. https://doi.org/10.1007/978-1-4471-5451-8_31
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5451-8_31
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5450-1
Online ISBN: 978-1-4471-5451-8
eBook Packages: MedicineMedicine (R0)