Abstract
A prostatic utricle is a congenital outpouching of the prostatic urethra. Signs, symptoms, and indications for surgical intervention include hematuria, pseudo-incontinence from urine trapping within the utricle, lower urinary tract symptoms, recurrent urinary tract infections, and stone formation within the pouch. A combined cystoscopic and laparoscopic approach may be employed to safely perform an utriculectomy using standard instrumentation and techniques. Etiologies, indications for surgical intervention, preoperative studies, instrumentation and operative technique, as well as postoperative management are described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
A prostatic utricle, or Müllerian duct cyst, is an outpouching of the prostatic urethra derived from both Müllerian and Wolffian duct origins [1]. It is an embryologic remnant likely resulting from a transient decline in fetal testicular function during the period of urethral formation [2, 3]. Not surprisingly, the incidence has been reported to be higher in association with hypospadias, particularly proximal hypospadias [4]. Indeed, an enlarged utricle is most commonly discovered when difficulty is encountered catheterizing the urethra during a hypospadias repair. In addition, an enlarged prostatic utricle may be associated with persistent Müllerian duct structures such as fallopian tubes and uterus [2]. A prostatic utricle may become symptomatic, requiring surgical excision. Adequate exposure of the utricle is challenging because of its position deep within the pelvis. Consequently, a wide variety of surgical approaches have been described, including retropubic, transvesical, transurethral, perineal, and posterior sagittal. The advantages of a laparoscopic approach include excellent visualization, improved cosmesis, and a higher rate of complete excision in a single setting while minimizing perioperative morbidity.
Indications/Contraindications
A prostatic utricle is most often asymptomatic but may cause a variety of signs or symptoms, including hematuria, pseudo-incontinence from urine trapping within the utricle, lower urinary tract symptoms, recurrent urinary tract infections, epididymo-orchitis, and calculus formation within the pouch. Obstruction of the ejaculatory ducts by the enlarged utricle has also been reported as a cause of infertility [5]. Furthermore, there is concern for neoplastic degeneration that has been reported to be as high as 3 % [6, 7].
Preoperative Investigations
Retrograde urethrography, voiding cystourethrography, or direct visualization by cystourethroscopy can be used to characterize a prostatic utricle. Contrast can be seen filling a tubular structure posterior to the prostate and bladder. A classification system has been proposed to characterize utricles [8]. Others have defined a clinically significant utricle as one large enough to accommodate a cystoscope to a depth of at least 2 cm [2]. Ultrasonography or MRI is an appropriate adjuvant investigation to better characterize the utricle and screen for persistent Müllerian duct structures.
Instrumentation
An appropriately sized rigid cystoscope is used for cystourethroscopy. An occlusion balloon catheter (Fogarty catheter) may be employed to inflate a balloon within the utricle.
Three laparoscopic ports and a 0° or 30° laparoscope may be used. A fourth port may be required to aid with retraction. A grasper, such as a Maryland, may be used for retraction, and a monopolar hook or scissors may be used for electrocautery and dissection. A needle driver and suction device should be available.
Patient Positioning
The patient is placed in dorsal lithotomy position for cystoscopy. The patient is then placed in the supine position for laparoscopy. Gentle Trendelenburg positioning may be employed as needed to displace the bowel cephalad by gravity.
Operative Technique
Cystoscopy may be performed to access the utricle. An occlusion balloon catheter (Fogarty catheter) may be employed to inflate a balloon within the utricle. Gentle traction may be used to occlude the neck of the diverticulum. Placement of an intrautricular balloon may be technically challenging but significantly aids in identifying the utricle and distinguishing it from the prostate. A Foley catheter may be placed into the bladder to aid in identification of the urethra and provide postoperative drainage of the bladder.
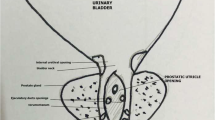
The patient is then placed in the supine position. A transumbilical incision is utilized to gain access to the peritoneal cavity. The abdomen is insufflated to an age-appropriate pressure. A working port is placed in each lower quadrant of the abdomen (Fig. 15.1).
The ureters and vas deferens are identified. The peritoneal reflection is incised transversely posterior to the bladder. A hitch stitch can be used to retract the bladder anteriorly. Alternatively, an additional working port may be placed in the suprapubic midline to aid with retraction. The presence of a balloon within the utricle significantly aids in identifying a smaller utricle and distinguishing it from the prostate, particularly when manipulated by an assistant.
The utricle is mobilized circumferentially with judicious use of needlepoint electrocautery, and the neck of the utricle is exposed. Great care is taken to avoid injury to the vas deferens and adjacent rectum. Occasionally, it is not possible to excise the whole utricle without damaging the vas deferens. In these patients, it is prudent to leave some of the utricle behind. The occlusion balloon is deflated and catheter is removed. The neck of the utricle is then ligated or transected and closed with an absorbable suture. The Foley catheter can be helpful in identifying the urethral lumen. The resected utricle is then removed through a working port or through a port site incision, which may be enlarged if necessary.
Postoperative Management/Complications
The Foley catheter remains in place for several days. A voiding cystourethrogram may be performed prior to removal of the catheter.
If there is concern for development of a urethral stricture, a retrograde urethrogram may be indicated.
Author Remarks
A wide variety of surgical approaches for excision of prostatic utricles has been reported, including a transvesical approach with marsupialization between the top of the cyst and the bladder [6], transperitoneal transtrigonal approach [12], perineal approach [7, 12], and transrectal approaches [13, 14]. Endoscopic treatments have been limited to unroofing infected cysts or removal of small remnants [15, 16]. The reported success rate and morbidity of these operations appear to be significantly worse compared to recent laparoscopic series, though the number of cases is small.
Robotic-assisted laparoscopy may also be utilized. At this point, it is unclear if the benefits of improved articulation and three-dimensional viewing outweigh the additional procedural costs of this technology.
References
Glenister TW. The development of the utricle and the so called “middle” or “median” lobe of the human prostate. J Anat. 1962;96:443–55.
Devine Jr CJ, Gonzales-Serva L, Stecker JF, et al. Utricular configuration in hypospadias and intersex. J Urol. 1980;123:407–11.
Shima H, Yabumoto H, Okamoto E, et al. Testicular function in patients with hypospadias associated with enlarged prostatic utricle. Br J Urol. 1992;69:192–5.
Meisheri IV, Motiwale SS, Sawant VV. Surgical management of enlarged prostatic utricle. Pediatr Surg Int. 2000;16:199–203.
Hendry WF, Pryor JP. Mullerian duct (prostatic utricle) cyst: diagnosis and treatment in subfertile males. Br J Urol. 1992;69:79–82.
Spence HM, Chenoweth VC. Cysts of the prostatic utricle (mullerian duct cysts): report of two cases in children, each containing calculi, cured by retropubic operation. J Urol. 1958;79:308.
Schuhrke TD, Kaplan GW. Prostatic utricle cysts (Müllerian duct cysts). J Urol. 1978;119:765–7.
Ikoma F, Shima H, Yabumoto H. Classification of enlarged prostatic utricle in patient with hypospadias. Br J Urol. 1985;57:334–7.
Yeung CK, Sihoe JDY, Yam YH, Lee KH. Laparoscopic excision of prostatic utricles in children. BJU Int. 2001;87:505–8.
Luo JH, Zhang D, Tu XA, et al. Laparoscopic excision of a large prostatic utricle revealed by haematuria: 1 year follow-up. Andrologia. 2012;44:214–6.
Willetts IE, Roberts JP, MacKinnon AE. Laparoscopic excision of a prostatic utricle in a child. Pediatr Surg Int. 2003;19:557–8.
Ikoma F, Shima H, Yabumoto H, Mori Y. Surgical treatment for enlarged prostatic utricle and vagina masculine in patients with hypospadias. Br J Urol. 1986;58:432–8.
Domini R, Rossi F, Ceccarelli PL, et al. L’approccio safittale transanorettale anterior nelle malformazion genitor-urinarie complesse del maschio. Eleventh Congresso Nazionale della Scoieta Italiana di Urologia Pediatrica, Tento; May 1993.
Siegel JF, Brock WA, Pena A. Transrectal posterior sagittal approach to prostatic utricle (Mullerian duct cyst). J Urol. 1995;153:785–7.
Hussman DA, Allen TD. Endoscopic management of infected enlarged prostatic utricles and remnants of rectourethral fistula tracts of high imperforate anus. J Urol. 1997;157:1902–6.
Narasimha Y, Winter CC. Cyst of the seminal vesicle: a case report and review of the literature. J Urol. 1972;108:134–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Chalmers, D.J., Campbell, J.B. (2014). Excision of Prostatic Utricle. In: Godbole, P., Koyle, M., Wilcox, D. (eds) Pediatric Endourology Techniques. Springer, London. https://doi.org/10.1007/978-1-4471-5394-8_15
Download citation
DOI: https://doi.org/10.1007/978-1-4471-5394-8_15
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-5393-1
Online ISBN: 978-1-4471-5394-8
eBook Packages: MedicineMedicine (R0)