Abstract
This chapter describes the physical principles and instrumentation of computed tomography (CT) and outlines several recent advances in CT technology. First, the history of CT is presented. Secondly, the essential physical principles are described. Thirdly, the technology of CT including image post-processing such as windowing is explained in detail. The elements of spiral/helical CT principles and technology are also outlined. Finally, multislice CT applications are reviewed followed by a radiation protection overview.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Compute Tomography Scanner
- Radiation Protection
- Dose Length Product
- Automatic Exposure Control
- Compute Tomography Dose Index
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Radiation dose in CT has received increased attention over the past few years, since CT delivers one of the highest doses to patients compared to other imaging modalities [1–3]. For this reason, it will be reviewed here. Only major factors will be considered.
An important first consideration is the beam geometry. As described in Chap. 5, CT uses a fan-shaped X-ray beam directed to an array of detectors that rotate 360° around the patient to collect attenuation data. The patient imaging table moves during the scanning process, and the X-ray tube traces a spiral or helical beam path around the patient. Ideally the radiation intensity measured along the z-axis would have equal intensity everywhere inside the beam and would have no intensity on either side, and it is clear that the dose distribution is almost always wider than the nominal slice width (SW). An important consideration in discussing CT dose is the dose distribution. Seeram [4] points out that the dose distribution is given by the function D(z), which describes an arbitrarily shaped dose intensity along the patient axis. In general, the shape varies between CT scanners. D(z) is very important to dose in CT, since it is this dose distribution that is measured.
1 CT Dose Descriptors
To describe the dose in CT, several dose descriptors are used; however, only two will be described here since it is beyond the scope of this chapter to address all aspects of CT radiation dose. These include the volume CTDI (CTDIvol) and the dose length product (DLP).
1.1 Computed Tomography Dose Index (CTDI)
The first definition of the CTDI was the one developed by the US Food and Drug Administration (FDA) and was therefore labeled CTDIFDA and is defined as
where n is the number of distinct planes of data collected during one revolution, SW is the nominal slice width (in mm), D(z) is the dose distribution, and z is the dimension along the patient’s axis. For axial (non-spiral/helical) CT scanners and spiral/helical CT scanners with a single row of detectors, n = 1. For multislice CT scanners, n is the number of active detector rows (e.g., n = 64) during the scan.
This definition, which was accepted by the International Electrotechnical Commission (IEC) [5], is good for all shapes of dose distribution curves D(z) that are emitted by CT scanners. With the CTDIFDA, only 14 sections of 7 mm thickness could be measured, and so another dose index, the CTDI100, extended the length of the scan measurement to 100 mm. The index is given by the equation
where nT is the nominal collimated slice thickness.
The next major change in the CT dose descriptor was the introduction of the weighted CTDI (CTDIW) to account for the average dose in the x-y axis of the patient instead of the z-axis, and it is expressed as follows:
In order to consider the dose in the z-axis, yet another dose descriptor was developed. This is the CTDIvol, and it can be calculated using the following relationship for spiral//helical CT imaging:
For a pitch of 1, the CTDIvol is equal to the CTDIW.
1.2 The Dose Length Product
The dose length product (DLP) is yet another dose descriptor used in CT dose studies, and reported in the literature and on CT scanners. While the CTDIvol provides a measurement of the exposure per slice of tissue, the DLP provides a measurement of the total amount of exposure for a series of scans. The DLP can be calculated knowing the length of the irradiated volume (scan length) and the CTDIvol using the following relationship:
It is important to note that while the CTDIvol is not dependent on the scan length, the DLP is directional proportional to the scan length. It is not within the scope of this book to describe the details of how to measure the CTDI.
2 Factors Affecting Dose in CT
There are several factors that affect the dose in CT including the exposure technique factors, X-ray beam collimation, pitch, patient centering, number of detectors, and over-ranging (also referred to as z-overscanning); particularly important for the operator are pitch, patient centering, and automatic tube current modulation.
First, note that the relationship between the absorbed dose and pitch is as follows:
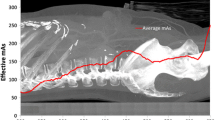
Therefore, if the pitch increases, the dose decreases proportionally. Another important factor under the control of the operator is that of patient centering. The patient must be centered in the gantry isocenter for accurate imaging of the anatomy. Inaccurate patient centering (miscentering) degrades the image quality and increases the dose to the patient, especially with the use of automatic exposure control (AEC) in CT. Finally, automatic exposure control (AEC) is now commonplace on CT scanners. AEC uses a technique referred to as automatic tube current modulation (ATCM) to optimize the dose to the patient while maintaining constant image quality regardless of the size of the patient in the z-axis, and the attenuation changes in the x-y axis.
In CT, ATCM refers to the automatic control of the mA in two directions of the patient (the x-y axis and the z-axis) during data acquisition using specific procedures that take into consideration not only the patient size but also the attenuation differences of the various tissues. The overall goal of ATCM is to provide consistent image quality, despite the size of the patient and the tissue attenuation differences, and to control the dose to the patient compared with manual mA selection techniques. The interested reader should refer to Seeram [4] for a further description of this technique.
While the automatic control of the tube current (mA) in the x-y axis (in-plane) is referred to as angular modulation, changing the tube current automatically in the z-axis (through-plane) is referred to as z-axis modulation or longitudinal modulation. When used together, that is, angular-longitudinal tube current modulation, AEC is the result. The use of angular-longitudinal modulation can reduce the dose by as much as 52 % compared to using only the angular modulation technique [6].
The operator must always pay careful attention to the image quality and dose during a CT examination. Image quality includes spatial resolution, contrast resolution, and noise. While spatial resolution depends on geometric factors (such as focal spot size, slice thickness, and pixel size), contrast resolution and noise depend on both the quality (beam energy) and quantity (number of X-ray photons) of the radiation beam. Several mathematical equations have been derived to express the relationship between dose and image quality. For CT operators, the following mathematical expression is important:
As noted by Seeram [4], this expression implies the following about dose and image quality:
-
(a)
To reduce the noise in an image by a factor of 2 requires an increase in the dose by a factor of 4.
-
(b)
To improve the spatial resolution (pixel size) by a factor of 2 (keeping the noise constant) requires an increase in the dose by a factor of 8.
-
(c)
To decrease the slice thickness by a factor of 2 requires an increase in the dose by a factor of 2 (keeping the noise constant).
-
(d)
To decrease both the slice thickness and the pixel size by a factor of 2 requires an increase in the dose by a factor of 16 (23 × 2 = 2 × 2 × 2 × 2).
-
(e)
Increasing mA and kVp increases the dose proportionally. For example, while a twofold increase in mA increases the dose by a factor of 2, additionally, doubling the dose will require an increase by the square of the kVp.
3 Radiation Protection Considerations
The effects of radiation can be described as being either stochastic or deterministic. Stochastic effects are usually due to a low dose of radiation which could be received over a long period of time. These effects are random, and the likely outcome is cancer or genetic effects. There is no threshold value below which it is certain that cancer or genetic effects will not occur but doubling the radiation doubles the risk, that is, the relationship is a linear one. Deterministic effects are usually the result of a higher radiation dose usually over a shorter time period. There is a threshold value above which a deterministic effect will happen, and the severity of this effect increases with the amount of radiation received. An example of this would be induction of cataracts following radiation dose. The minimum single dose necessary to produce a progressive cataract would be 2 Gy. Above this threshold, the biological response will increase. Lower doses of radiation will cause the same effect, but the threshold value will be higher. Cataracts develop approximately 8 years postexposure [7]. The purpose of radiation protection is to limit the radiation dose received by patients (and staff) from medical exposures. Radiation dose received can be increased considerably if X-ray equipment is used inappropriately or radiation protection is inadequate.
3.1 Need for Radiation Protection in CT
There has been an increase in the use of CT in recent years which has led to a potential increase in radiation burden to the general population [8]. As well as the increase in use within diagnostic CT departments, there has also been a rise in the number of nuclear medicine departments which now utilize CT.
There are two types of CT scanners that are used in conjunction with SPECT—diagnostic quality with a full range of parameters available and low dose/low resolution where the parameters are less flexible or fixed. Low-dose scanners tend to use a much lower tube current (mA) than diagnostic scanners. As radiation dose is directly proportional to mA when peak tube voltage (kVp), scan time, and slice width remain constant, use of a reduced mA can significantly lower the dose received by the patient [9]. It will, however, have an effect on the quality of the resultant image (see Sect. 10.4).
Diagnostic CT scanners used as an adjunct to SPECT can also be used in a low-dose way by selecting parameters similar to those used by scanners designed to operate at a lower tube current. However, even when used for attenuation correction purposes, it is probable that the slice width and other parameters might vary which in turn could increase the radiation burden of the patient.
3.2 Legislation
Each country will have its own arrangements for the regulation of radiation in relation to humans. It is beyond the scope of this chapter to consider all regulatory arrangements, and instead we shall focus into one country (UK). Readers from other countries may find the following information helpful as there are many commonalities between regulatory arrangements of different countries. However, for specific details of any particular country, the reader is encouraged to review the regulation and guidance documents that apply locally.
The Ionising Radiation (Medical Exposure) Regulations 2000 (IR(ME)R 2000) relates to patient safety with regard to radiation dose. IR(ME)R 2000 specifies personnel who are involved in patient safety during medical exposures as the referrer (the person who requests the medical image to be created), practitioner (the person who justifies that the imaging procedure can go ahead), and operator (the person who physically makes the radiation exposure). Different professional groups may take on these roles, and there can be some overlap between duties. For example, a practitioner can also act as an operator, but an operator cannot necessarily act as a practitioner. It is necessary to have the appropriate skill mix so that justification and optimization of the procedure can be performed. This is a fundamental component of radiation protection.
The Ionising Radiations Regulations 1999 (IRR 99) [10] aims to ensure a structured approach to radiation safety by employers. It defines that all radiation doses should be kept as low as reasonably practicable (ALARP principle). IRR 99 specifies that there should be safe working practices covered by local rules and that there should be specific dose limits for both staff and patients.
3.3 General Principles of Radiation Protection
The essential factor in radiation protection is keeping the dose to patient, staff, and members of the public as low as reasonably practicable (ALARP). In general, this can be addressed by justification of referrals and optimization of parameters used and good explanation to the patient to ensure compliance and reduced need for repeat examinations. This corresponds with the basic principles identified by the International Commission on Radiological Protection (ICRP) [11]. The principles are as follows:
-
1.
Justification
The principle of justification is that a patient will only be exposed to ionizing radiation if that exposure is beneficial to them and that the benefit they receive outweighs the risk from the radiation dose. It is the first step in radiation protection and is reliant on candid clinical information [11].
-
2.
Optimization
Optimization can be achieved by selection of the appropriate parameters to ensure that the radiation dose administered is ALARP so as to achieve the required image(s). For SPECT-CT, the CT images are often for attenuation correction (AC) so a diagnostic quality image is not required. This lower image quality commands a lower mA, and so radiation burden to the patient is naturally reduced. This explains why on low-dose CT scanners, which are used purely for AC, the selection of CT acquisition parameters is limited or even set to achieve a very low dose.
-
3.
Dose Limitation
As stated previously, limitation of radiation dose is applicable to staff and members of the public as well as the patient. While it is essential that the radiation dose to the patient is limited as much as possible, staff also have a duty to ensure good radiation protection measures are in place for themselves and other patients, visitors, or members of the public escorting patients for X-ray procedures.
The Ionising Radiation Regulations 1999 have imposed dose regulations which must not be exceeded in order to ensure that the risk of cancer induced by exposure to radiation is not at an unacceptable level [6, 12]. Table 9.1 provides a summary of radiation dose limits.
3.4 Designated Areas
Within a department utilizing ionizing radiation, there will be designated areas. These areas are classified as either controlled area or supervised area depending on the amount of radiation dose an employee is likely to receive while working in this area. Monitoring of radiation levels should be done regularly to ensure correct designation of the area is maintained.
In a controlled area, the staff member is likely to receive an effective annual radiation dose of greater than 6 mSv. It is necessary that all controlled areas are clearly demarcated and that warning signs are clearly visible. An example of a controlled area would be a CT scan room. Warning signs should indicate that the area is controlled and that access is restricted. A light indicating that X-rays are being transmitted should be visible on all access points to the room, and all external doors should remain locked during the examination.
A supervised area is one where a member of staff is likely to receive an effective annual radiation dose of greater than 1 mSv. An example of a supervised area would be the control room within a SPECT-CT unit. Again, suitable warning signs should be visible, and although restriction to a supervised area is less stringent than a controlled area, it is often restricted to ensure patient privacy.
3.5 Local Rules
Local rules are a set of written instructions provided for use in designated areas. They should provide a clear reference for radiation safety within the associated area and provide information of contingency plans in the event of an accident. Where local rules are applicable, it is always necessary that at least one radiation protection supervisor is employed to ensure adherence to the rules. IRR 99 specifies that an employee should not knowingly expose themselves or others to ionizing radiation greater than that necessary and that they should make proper use of any personal protective devices and shielding available to them.
4 Monitoring and Dose Recording for Staff
It is important to monitor staff radiation dose to ensure that exposure is controlled and within dose limits. If doses appear to be higher than expected, then the information can help prompt investigation into underlying reasons. This could lead to further training or review of working conditions and practices. It should also provide evidence in cases of underlying overexposure or accident. Two of the most common ways to measure radiation dose to staff from ionizing radiation are the use of film badges or thermoluminescent dosimeters (TLDs). These are normally issued on a monthly basis, but this might be reduced to three monthly if doses are found to be low [13].
Radiation monitoring badges are usually worn on the front of the torso at waist height. They should be worn at all times during the working day, and in the event of protective clothing being worn, for example, a lead-rubber apron, the badge should be worn underneath the protective garment. TLD badges are approximately ten times more sensitive than film badges. This renders them more susceptible to changes in background radiation. For this reason, control badges tend to be used to allow subtraction of background doses from personal doses.
5 Maintenance of Equipment
It is important that equipment is maintained to ensure that it is performing at a level that is fit for intended clinical purposes. Quality control (QC) tests (Chap. 5) should be carried out on a regular basis to monitor performance of the CT system against an accepted standard to ensure consistency. Any faults which are noted from QC tests should be reported to the employer immediately as should any damage or faults observed during normal working practice.
6 Acquisition Parameter Differences: Diagnostic CT and Low-Dose CT in SPECT
CT is a transmission technique as opposed to the emission technique used in the SPECT part of the study. Therefore, unlike the use of radionuclides, the radiation dose is dependent upon the parameters selected. We have already determined that the way in which low-dose CT equipment varies from diagnostic quality CT equipment (by the parameters that are available for selection). Adding further clarity to this, Table 9.2 demonstrates differences between a low-resolution CT scanner and a diagnostic quality CT scanner.
7 Room Design: Shielding
Radiation protection considerations for SPECT-CT need to include radiation from the patient (emission) and radiation from the CT scanner (transmission). The amount of shielding necessary will depend upon the CT scanner capability and the parameters used [14]. For instance, when used in conjunction with a low mA scanner, then 3 mm of lead room shielding is considered sufficient. The estimated workload and existing structural shielding (which could also include floor and ceiling if rooms above and below are occupied) will also be taken into consideration when calculating the required thickness of lead shielding. In most cases, CT scanners used in conjunction with SPECT will have a much lower workload than those used for diagnostic CT purposes.
References
Tsapaki V, et al. Radiation safety in abdominal CT. Semin Ultrasound CT MR. 2010;31:29–38.
Huppmann MV, et al. Radiation risks from exposure to chest CT. Semin Ultrasound CT MR. 2010;31:14–28.
Colang JE, et al. Patient dose from CT: a literature review. Radiol Technol. 2007;79(1):17–25.
Seeram E. Computed tomography-physical principles, clinical applications, and quality control. St. Louis: Saunders/Elsevier; 2009.
IEC (International Electrotechnical Commission). Medical electrical equipment-60601 Part 2–44: particular requirements for the safety of X-ray equipment for CT. Geneva. 1999.
Goodman TR, Brink JA. Adult CT: Controlling dose and image quality. In: RSNA Categorical Course in Diagnostic Radiology Physics: from invisible to visible-The science and practice of X-ray imaging and radiation dose optimization. 2006;157–165.
Hall EJ, Giaccia AJ. Radiobiology for the radiologist, Chap. 13. 6th ed. Philadelphia: Lippincott Williams and Wilkins; 2006. p. 185.
Mettler FA, Wiest PW, Locken JA, Kelsey CA. CT scanning patterns of use and dose. J Radiol Prot. 2000;20:353–9.
McNitt-Gray MF. AAPM/RSNA physics tutorial for residents: topics in CT – radiation dose in CT. Radiographics. 2002;22:1541–53.
Her Majesty’s Stationary Office. The ionising radiations regulations 1999. Statutory Instruments No. 1059. London: HMSO; 1999.
International Commission on Radiological Protection. Recommendations of the International Commission on Radiological Protection 1990. ICRP Publication 60. Ann ICRP. 1990;21:1–3.
Ball J, Moore AD, Turner S. Ball and Moore’s essential physics for radiographers, Chap. 21. 4th ed. Oxford: Blackwell Science; 2008. p. 346–58.
Health and Safety Executive. Radiation doses – assessment and recording. Suffolk: Health and Safety Executive. Available from http://www.hse.gov.uk/pubns/irp2.pdf. Accessed 3 May 2011.
O’Connor MK, Kemp BJ. Single-photon emission computed tomography/computed tomography: basic instrumentations and innovations. Available from http://medlib.yu.ac.kr/eurjoph/senu/snu/364258.pdf. Accessed 17 June 2011.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag London
About this chapter
Cite this chapter
Sil, J., Seeram, E. (2013). Practical Radiation Dose and Practical Radiation Protection Considerations. In: Jones, D., Hogg, P., Seeram, E. (eds) Practical SPECT/CT in Nuclear Medicine. Springer, London. https://doi.org/10.1007/978-1-4471-4703-9_9
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4703-9_9
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4702-2
Online ISBN: 978-1-4471-4703-9
eBook Packages: MedicineMedicine (R0)