Abstract
Acute stroke is common, has high morbidity and mortality, and is grossly undertreated in the United States. The goals for ischemic stroke therapy should be rapid and safe reperfusion of the culprit artery, either through the use of thrombolytic drugs or mechanical therapies in appropriate patients. Many options currently exist for mechanical embolectomy of stroke and each has unique advantages and disadvantages. The field of stroke intervention is constantly evolving as new devices and new insights are employed. Nevertheless, the “optimal” therapy for acute stroke remains elusive, as the field searches for large-scale multicenter randomized trials which can help build consensus and shape guideline recommendations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Stroke currently affects 750,000 patients yearly in the United States and is projected to increase in frequency to one million per year by 2025 [1]. As such, stroke represents the third leading cause of death in the United States and is the most common cause of adult disability, with healthcare expenditures of approximately 73 billion dollars in hospitalization and lost productivity in 2010 [2]. The vast majority of all strokes (>80 %) are ischemic in nature [3]. Treatment for stroke has undergone rapid advances in the past two decades, beginning with the first FDA-approved therapy for acute ischemic stroke, intravenous thrombolysis, in 1995 [4]. New understanding of the pathophysiology of stroke in conjunction with advances in endovascular equipment have created the field of stroke intervention, which has fostered a host of new devices and technologies to treat acute stroke in patients not eligible for thrombolysis [5–11]. Many of these new techniques and devices have shown promise for offering improved outcomes following ischemic stroke in small case series, yet the field remains very much in its infancy with little in the way of large randomized trials to guide policy-level decision making or guideline generation.
Moreover, acute stroke cannot be treated in isolation or by a single specialty provider. Instead, it requires complex coordination between multiple providers from different specialties, organized towards a single goal [12]. Whereas the patient with an acute ST-elevation myocardial infarction can be treated by a single interventional cardiologist throughout his or her hospital stay, stroke patients are unique in their requirements for coordinated, multidisciplinary care. The fields of emergency medicine, neurology, neurosurgery, radiology, interventional neuroradiology, vascular surgery, and interventional cardiology all have important contributions to the care of the individual patient and advancement of the field. As a result, it is difficult to develop a stroke program without cooperation between colleagues across disciplines. In fact, the American Stroke Association’s Task Force on the Development of Stroke Systems identifies fragmentation of care as a major contributor to suboptimal treatment of stroke and inefficient use of healthcare resources [13]. As such, coordinated systems of care which integrate prevention and treatment and provide patient and community education should be a primary focus in the development of stroke programs. This chapter will focus on the current treatment modalities that exist for acute ischemic stroke management, with a primary focus on new devices targeted for the endovascular specialist.
Intravenous Thrombolysis
For the appropriately selected patients, intravenous (IV) thrombolysis represents the current standard of care for treating acute stroke [14]. Whereas the initial window for administration of IV thrombolytics extended to 3 h from symptom onset in early trials [4], more recent European data has suggested that with the proper patient selection, the window can be extended to four and a half hours from symptom onset [15]. The concern with later administration of thrombolytics involves higher rates of hemorrhagic transformation of the infracted brain tissue, particularly in large territory strokes which are more susceptible to hemorrhagic conversion. Because of this, there has been much interest in finding novel mechanisms for identifying patients at high risk for hemorrhage. Evidence suggests that advanced MRI-based perfusion techniques may be able to select late-presenting patients least likely to have hemorrhagic transformation following administration of IV thrombolytics [16, 17]. Nevertheless, the benefit of intravenous thrombolysis is clearly time related, with a decreasing benefit the later the administration of drug occurs from the onset of symptoms [18].
The National Institute of Neurological Disorders and Stroke (NINDS) published the landmark trial of intravenous recombinant tissue plasminogen activator (t-PA) in 1995 [4]. In the trial, 624 patients who presented with an acute ischemic stroke within 3 h of symptom onset and had no evidence of brain hemorrhage by CT scanning were randomized to t-PA or placebo infusions. All patients received baseline National Institutes of Health Stroke Score (NIHSS), a 42-point scale which quantifies the degree of neurologic deficit in 11 categories [19]. Outcomes including neurologic recovery and overall survival were assessed at 24 h and 90 days. In this trial, patients who received t-PA were 30 % more likely than those who received placebo to have minimal or no neurologic deficits at 90 days and had no increase in mortality [4]. Moreover, this benefit was maintained out to 1 year, with continued neurologic benefit for treatment with t-PA and no adverse effect on overall mortality [20]. Nevertheless, t-PA treatment was not risk-free and was associated with higher rates of intracranial hemorrhage within the first 36 h, and some have suggested that the stroke severity was lower in the t-PA group, which may have skewed the results [21]. In spite of the controversy, the FDA-approved intravenous thrombolytic therapy for appropriate patients and it remains the standard of care.
More recently, the strict 3-h time window cutoff was tested in a European setting of acute ischemic stroke [15] in which the time window was extended to 4.5 h after symptom onset in appropriate patients. In this trial, 821 patients who were between 3 and 4.5 h from stroke symptoms onset were randomly assigned to intravenous t-PA or placebo, and neurologic outcomes were assessed at 90 days using the modified Rankin score, which scores functional capacity on a 6-point scale (lower numbers are higher functional capacity, with 0 indicating no deficit and 6 indicating death) [22]. In patients who received thrombolytic therapy, 52 % had a favorable outcome versus only 45 % in the placebo group. Of note, intracranial hemorrhage was higher in those treated with t-PA (27 % vs. 18 %), but there was no difference in overall survival [15].
Despite the results of the above trials, time restrictions continue to exclude a significant number of patients from candidacy for IV thrombolysis. In addition to patients presenting more than 4.5 h beyond symptom onset, many patients present with “wake-up” strokes where the time on onset cannot be calculated and therefore are excluded from receiving thrombolytic therapy. As a result of the time limitations in conjunction with fear of litigation and lack of appropriate treatment algorithms, less than five percent of all stroke patients who present for medical care receive intravenous thrombolysis [23]. Additionally, intravenous thrombolysis is less effective for large vessel occlusive disease (particularly distal carotid), and in these cases, which typically have high stroke scores and larger clot burden, catheter-based devices may hold an advantage in terms of more effective reperfusion and lower risk for hemorrhagic transformation [24].
Endovascular Therapies for Stroke: An Overview
Because of the limitations of intravenous thrombolysis, multiple catheter-based thrombectomy approaches have been developed to allow for reperfusion of ischemic brain tissue. Advantages to this approach include a longer time window (6–8 h after symptom onset) [25] for treatment than intravenous thrombolysis, where guidelines dictate administration within 3 h of symptom onset [14]. Recent data suggests that there may be benefit to intravenous thrombolysis up to 4.5 h from symptom onset in select patients, although the benefits are small and there is increased risk of intracranial hemorrhage [15]. Moreover, only a small fraction (~2 %) of patients with ischemic stroke receive intravenous thrombolysis, largely due to the narrow time window in which it can be administered [26]. Efforts to predict which patients outside the 3-h window for thrombolysis will benefit from catheter-based intervention have relied on several imaging modalities to identify jeopardized brain tissue, or ischemic penumbra, including CT perfusion and MRI perfusion/diffusion mismatch [27, 28]. The penumbra represents the brain tissue which is at risk for permanent injury, but has not yet been irreversibly damaged. A large penumbra signifies more brain tissue at jeopardy and therefore higher potential benefit for reperfusion therapy. Current data suggests that more than three-fourths of ischemic strokes will have a penumbra size which would favor reperfusion within the first 6–8 h following symptom onset [29]. Mechanical reperfusion strategies which facilitate recanalization of the culprit vessel may therefore be helpful during this time to salvage brain tissue.
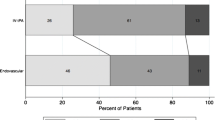
There is no one “ideal” endovascular treatment for stroke. The goal of all technologies currently available is to reperfuse the culprit artery while avoiding the most feared complication of intracranial intervention: brain hemorrhage. Symptomatic intracranial hemorrhage is associated with high morbidity and mortality [20] and occurs in roughly 5–12 % of patients undergoing endovascular stroke therapy [9, 25, 30]. Initial efforts at reperfusion outside the intravenous thrombolytic time window focused on intra-arterial (IA) delivery of thrombolytics adjacent to the obstructing thrombus in selected patients with middle cerebral artery occlusions [25, 31]. In this population of patients, IA thrombolysis compared with placebo improved both recanalization rates (66 % with IA thrombolysis and 18 % with placebo) and 90-day neurologic outcomes as measured by the modified Rankin score [25]. Nevertheless, IA thrombolysis remains non-FDA approved for stroke treatment [14]. Mechanical reperfusion with the Merci Retrieval System (Concentric Medical, Mountain View, CA) in selected patients ineligible for intravenous thrombolysis up to 8 h after symptom onset resulted in recanalization rates approaching 70 %, and those patients who were successfully revascularized had improved functional status at 90 days [9, 10] (Fig. 36.1). Another extraction device (Fig. 36.2), the Penumbra System (Penumbra, San Leandro, CA), has demonstrated excellent results at restoring artery patency up to 8 h after symptom onset in a cohort of patients with severe stroke (mean NIHSS of 21) [7].
MERCI device. The MERCI device: (a) Left middle cerebral artery thrombus in a patient with acute right-sided weakness (arrow shows thrombus). (b) MERCI device engaged in the thrombus. (c) Angiogram of the left middle cerebral artery post embolectomy with the MERCI device (arrow shows resolution of thrombus)
Mechanical strategies can broadly be divided into several groupings: clot retrievers, aspiration- or suction-type devices, balloons and stents, and ultrasonography-based devices [32]. Ultimately, each of these techniques requires detailed understanding of not only the operational characteristics of the device but also the methods for delivering these potentially bulky tools to the intracranial circulation. As such, injury to the neurovasculature, distal embolization of clot, and conversion of ischemic injury to hemorrhagic injury are all possible complications. Specialized training is required not only to learn the individualized techniques for operation of these devices but also for approaches to selecting the optimal patient population who may benefit from their use.
Intra-arterial Thrombolysis
The concept of intra-arterial (IA) thrombolysis for acute stroke was a logical progression from IV thrombolysis in that it allowed local delivery of the thrombolytic drug directly to the thrombus rather than systemic administration (Fig. 36.3). In theory, this technique offers fewer systemic side effects and more effective thrombolysis. As a result, the therapeutic window for delivery was broader in time scope, as well as patient inclusion [33]. Downsides of this approach include the need for highly skilled interventionalists who can identify the culprit thrombus and successfully navigate the tortuous brain arteries to deliver drug locally as well as appropriate facilities and support staff to allow for successful patient treatment during and after the procedure.
Microcatheter for primary reperfusion. The patient presented with an acute stroke but was lytic ineligible and received catheter-based therapy with local delivery of t-PA via a microcatheter. (a) Occlusion of the right middle cerebral artery (arrow). (b) Reestablished patency of the right middle cerebral artery post-local delivery of t-PA via microcatheter
The PROACT-II trial [25] was a randomized and placebo-controlled trial of patients with middle cerebral artery occlusions and moderately high NIH Stroke Scores (mean 17) who presented within 6 h of symptom onset. The 180 patients enrolled were randomly assigned to treatment with intra-arterial catheter-delivered recombinant prourokinase or low-dose heparin, and standard neurologic outcomes were examined at 90 days, including the modified Rankin Scale score (mRS) which measures functional status. The protocol allowed for placement of a microcatheter up to the thrombotic occlusion, but no mechanical disruption of the clot with wires or catheters. Patients enrolled were highly selected, with over 12,000 patients screened to identify the 180 patients who were enrolled. In this trial, patients who received the thrombolytic therapy had higher rates of artery reperfusion (66 % vs. 18 %) and had better neurologic outcomes as measured by the mRS (40 % had mRS 2 or less in lytic arm versus only 25 % in the control arm). The overall mortality was about 25 % and not different between the two groups, despite a higher rate of intracranial hemorrhage in the patients who received thrombolysis during the first 24 h (35 % vs. 13 %) [25].
Despite the improvements in neurologic outcomes seen in PROACT-II, intra-arterial thrombolytic therapy has not been approved in the United States. Nevertheless, enthusiasm remains for off-label use of commercially available thrombolytics including urokinase and recombinant t-PA, both as stand-alone therapy and when used in combination with intravenous thrombolytics [6]. The concept of a dual thrombolytic approach is appealing in that it allows for rapid treatment of patients in the emergency room setting with IV thrombolytics, followed by local, intra-arterial delivery of additional thrombolytic directly at the site of occlusion (Fig. 36.4). Intra-arterial thrombolysis allows for a higher recanalization rate than systemic intravenous administration, which is less effective in large clots. The Emergency Management of Stroke Bridging Trial (EMS) [34] examined the feasibility and safety of combining intravenous with intra-arterial thrombolytics in patients with acute stroke. In this small study, which enrolled 35 patients with stroke, patients randomized to intravenous and intra-arterial thrombolytics had improved rates of recanalization of infarct arteries compared with those randomized to placebo followed by intra-arterial thrombolysis. Despite no difference in intracerebral bleeding rates, there was no improvement which was noted in overall neurologic outcomes [34]. Since then, other trials have examined the safety endpoints of combined therapy in a nonrandomized fashion, but there has not been overwhelming adoption of this approach [35].
Microcatheter for assisted reperfusion after failed systemic thrombolytics. The patient presented with an acute stroke to an outside hospital and received full-dose systemic thrombolysis. Her symptoms did not improve and she was transferred for rescue intervention. Local delivery of t-PA via a microcatheter allowed for successful reperfusion. (a) Thrombotic occlusion of the left MCA with visible thrombus despite intravenous thrombolytic administration. (b) A microcatheter is delivered distal to the obstruction in the left middle cerebral artery and contrast injection is performed to confirm intraluminal placement. Thrombolytics (t-PA) are then delivered locally to the thrombus via the microcatheter. (c) Final cerebral angiogram demonstrating patency of the left middle cerebral artery after local delivery of thrombolytics. Clinically, this patient had a nearly complete neurologic recovery
The Interventional Management of Stroke II Study (IMS II) [6] used a combined approach of intravenous thrombolysis followed by immediate cerebral angiography with additional intra-arterial delivery of thrombolytics for patients with persistent cerebral artery occlusion. IMS II also employed the EKOS ultrasound catheter for enhanced thrombolysis in a portion of the patients. Overall, this trial found that, when compared with IV thrombolysis alone as in the NINDS trial, the combined approach had no higher rates of intracranial hemorrhage and numerically improved survival when compared to the treatment or placebo arms of the NINDS trial [6]. This encouraging result leads to the organization of the IMS III trial, which is currently enrolling and is randomizing acute stroke patients to intravenous thrombolytic versus combination therapy [36].
Mechanical Thrombectomy
In addition to thrombolytic therapies, there has been an explosion of devices in the past few years which are designed to mechanically remove thrombus from the infarct-related artery. The Mechanical Embolus Removal in Cerebral Ischemia (MERCI) device is FDA approved for the treatment of intracranial clot removal in acute stroke [10]. It has a corkscrew shape and is designed to engage a clot and allow for physical removal of the clot from the cerebral circulation (see Fig. 36.1). It is deployed via a specialized delivery system which is equipped with an occlusion balloon. In theory, this allows for cessation of forward blood flow while the thrombus is being removed and also allows for aspiration of the affected artery so as to prevent further embolization of clot fragments to distal vessels. The pivotal MERCI trial enrolled patients with acute stroke within the first 8 h of symptom onset who were ineligible for intravenous thrombolytic therapy. Successful recanalization was achieved in 48 % of the patients in whom the device was used, with a symptomatic intracranial hemorrhage rate of about 8 % [10]. In patients in whom successful recanalization was achieved, univariate analysis of neurologic outcomes at 90 days showed improvement in mRS, which leads to much excitement about the device and its possible role in thrombolytic-ineligible patients. Interestingly, with multivariate analysis, successful recanalization was no longer a predictor of a good neurologic outcome [37], and there remains much debate about the benefits of the MERCI device and the role that this device should have in the treatment of acute stroke. Newer versions of the MERCI device which incorporate Prolene microfilaments were used in the nonrandomized phase I Multi-MERCI trial, where high rates of successful recanalization were seen when the device was used alone (54 %) or in conjunction with intra-arterial thrombolytics (69 %) [30].
The Penumbra System is another mechanical thrombectomy device which is designed to allow removal of thrombus in the setting of acute stroke. The system consists of an aspiration catheter and a stator which fits through the lumen of the catheter and helps facilitate thrombus maceration and removal (see Fig. 36.2). It was utilized in a single-arm, multicenter registry in 125 patients who presented within 8 h of acute stroke and allowed for successful recanalization in 81 % on the arteries in which it was attempted [38]. Intracranial hemorrhage occurred in 28 % of patients in whom the device was used, with just less than half of hemorrhages classified as symptomatic. Yet despite the high rate of successful recanalization, the rate of favorable clinical outcomes as determined by the mRS was only 25 %, and mortality at 90 days remained high at 33 % [38]. Results such as this have called into question the continued focus on recanalization as a surrogate for success in treating acute stroke, but trials continue to try to define the role for mechanical thrombectomy devices in acute stroke.
Intracranial Stenting
Taking a lesson from the world of coronary intervention, the use of intracranial stents has emerged in the past few years as a means of providing immediate restoration of flow in an acute stroke. Whereas thrombolytics may fail because of the fibrous nature of a more mature embolus, and other mechanical approaches may fail because of embolic adherence to the vessel wall, intracranial stenting is very effective at reestablishing artery patency [39]. Initial attempts at intracranial stenting utilized balloon-expandable stents, which resulted in reasonably high recanalization rates (79 %) but continued high mortality of over 30 % [40]. Part of the difficulty with balloon-expandable stents is the bulky nature of the devices, which have to be delivered to the intracranial circulation via highly tortuous vessels. Moreover, cerebral vessels lack a robust external elastic membrane and have little mobility to stretch and move as a stiff stent travels through because of extensive fixation from branching and perforating arteries [41]. As a result, the chances of vessel damage via dissection or perforation are higher than would be expected when working in the coronary realm. In addition, the consequences of plaque shifting with subsequent compromise of a small perforator artery can be disastrous in the cerebral circulation, making intracranial stenting with balloon-expandable stents a potentially risky proposition.
Because of these unique challenges discussed above, self-expanding stents have gained popularity in the intracranial circulation. They have more flexible delivery systems and are able to track more easily to the target vessel with less risk of vessel injury [42]. There are currently five commercially available stents for use in the intracranial circulation: Wingspan (Stryker, former Boston Scientific, Fremont, CA), Solitaire (ev3, Plymouth, MN), Enterprise (Cordis, Miami Lakes, FL), Leo (Balt, Montmorency, France), and Neuroform (Boston Scientific, Natick, MA). These devices can all be used for the treatment of acute stroke, although they are actually indicated for use in coiling wide-neck aneurysms in the cerebral circulation. Several small single-center experiences with these devices have been reported, including one which included nine patients who were treated just over 5 h after symptom onset and found an 89 % recanalization rate with one intracranial hemorrhage and one acute stent thrombosis [43].
The Stent-Assisted Recanalization in Acute Ischemic Stroke (SARIS) trial is a prospective trial examining the role for stenting in acute stroke [44]. In the trial, 20 patients who either failed intravenous thrombolysis or were not eligible to receive thrombolysis underwent stent-assisted recanalization of the infarct-related artery. Successful recanalization (TIMI 3 or TIMI 2 flow) was achieved in 100 % of the patients, and at 1 month, roughly 60 % of patients had mRS of 3 or less. Many other smaller studies and case series have validated these findings, suggesting that a stent-based approach has real merit in the management of patients with acute stroke [45–47]. An interesting approach which has been utilized in the intracranial circulation is the use of “temporary” stent placement to allow for rapid reestablishment of flow at which point the stent is then retrieved, essentially leaving nothing behind in the intracranial circulation. This approach has several advantages. First, there is no need for dual antiplatelet therapy which can increase the risk of bleeding, particularly intracranial bleeding. Second, stents in the intracranial circulation have been noted to have very high rates of restenosis in small angiographic follow-up studies, although the Wingspan stent used in the SARIS trial had low rates of restenosis at follow-up angiography 6 months after placement [48]. The first case report of temporary endovascular bypass was published in 2008 and detailed a case involving a patient with an unsuccessful mechanical thrombectomy of a large M1 clot where an Enterprise stent was used to successfully reestablish flow to the occluded segment [49]. The stent was left in place for only 20 min and then retrieved from the circulation once flow was restored. The patient did well clinically with a significant fall in NIH Stroke Scale following the procedure. Since then, there have been additional reports which detail similar successes in using stents in a retrievable manner [50]. Based on the high success rates with recanalization and good clinical outcomes, it seems that stent-based therapies for acute stroke hold much promise in the future of stroke therapy.
Neuroprotection
The concept of neuroprotection for acute stroke involves the administration of a drug or other therapy to help minimize ischemic brain injury. While enticing to imagine a drug treatment which blocks the effects of ischemia or protects from cellular damage, the field of neuroprotection has been littered with many “wonder drugs” which held great promise in early animal models yet demonstrated no benefit when studied in man [51]. Many of these drugs are targeted at modulating mediators of neuronal damage, including free radicals, excitatory neurotransmitters, inflammatory markers, and even temperature. There has also been enthusiasm for therapeutic hypothermia in the setting of acute stroke, as it seems to provide benefit following cardiac arrest [52]. However, concerns exist about complications from the required intubation and paralysis which accompanies hypothermia, and the beneficial cerebral effects seen during cooling may be lessened by the requisite rewarming phase [53]. Because of the lack of evidence, there are no current recommendations for administration of neuroprotective agents in the setting of acute stroke, although research continues in this area.
Manpower Issues
Widespread adoption of reperfusion strategies outside intravenous thrombolysis will require a sizable pool of appropriately trained “stroke interventionalists” who are capable of delivering therapy to the brain 24 h a day and 365 days a year. Recent surveys have indicated that fewer than 400 interventional neuroradiologists are currently working in the United States, an inadequate supply to treat even a fraction of the 700,000 strokes which occur in this country every year [54]. Proposals for increasing neuroendovascular manpower have focused on utilizing the pool of carotid-stent-trained interventionalists, a diverse group of providers including neurologists, surgeons, and cardiologists [12]. Specific universal guidelines and training qualifications for acute stroke intervention do not currently exist, but the Society for Coronary Angiography and Interventions (SCAI) is now offering small, multidisciplinary meetings specifically designed to build competence in stroke intervention, including the use of simulators to teach intracranial intervention [55]. More widespread effort to grow the cadre of stroke interventionalists at the community level is the best strategy for impacting stroke outcomes at the national and health policy level.
Despite the multitude of options for the endovascular treatment of stroke, it is clear that not all patients will benefit from this therapy. The role of the “team approach” is to help select the patients who are best suited to catheter-based therapies, determined through assessing the degree of neurologic deficit, duration of symptoms, and size of penumbra as well as incorporating anatomic variables such as degree of collateral circulation. A stroke neurologist is a crucial component of the stroke team and can help guide decision making for the endovascular specialist.
Stroke Centers
Stroke centers are a key component of building a successful stroke program. The concept of stroke centers is relatively new, outlined by the Brain Attack Coalition (BAC) in the year 2000 [56] in response to earlier publications detailing the potential benefits of such centers [57, 58]. The model which has evolved through these efforts is similar to the model for trauma centers or for ST-elevation myocardial infarction (MI). Both trauma care and acute myocardial infarction care share similarities to acute stroke treatment in that they require rapid identification and triage of patients in order to provide timely access to care. This systems-based approach requires community-wide coordination and planning in order to execute in an efficient manner, beginning with empowering ambulances to bypass hospitals in order to bring stroke patients to facilities with appropriate treatment capabilities. To improve stroke care, the BAC has delineated specific components for both Primary Stroke Centers (PSC) [56] and Comprehensive Stroke Centers (CSC) [59]. PSCs are organized to provide a basic infrastructure for acute stroke care, including thrombolytic therapy administration by stroke teams, stroke units, and 24-h access to computed tomography scanning, while CSCs build upon this framework to allow for more comprehensive care.
The components of CSC have been outlined in the BAC consensus document [59] and broadly include (1) adequately trained personnel, (2) specific neuroimaging capability, (3) surgical and endovascular interventional capabilities, and (4) the infrastructure to support the above activities. Each of these components plays a key role in the rapid and effective diagnosis and treatment of stroke. Adequately trained personnel form the backbone of comprehensive stroke centers. Providers are needed to rapidly assess a stroke patient, determine time of symptom onset, and perform a neurologic exam which includes a National Institutes of Health Stroke Score (NIHSS) [19]. Timely assessment is important because of the narrow window (3 h from symptom onset) in which to administer intravenous thrombolytic therapy in eligible patients [14]. Imaging capability includes a CT scanner which is available around the clock, preferably with CT perfusion imaging capability, along with magnetic resonance imaging and angiography (MRI/MRA), angiography suites with digital subtraction angiography (DSA) to allow for percutaneous catheter-based therapy when appropriate, carotid duplex and transcranial Doppler scanning, and transesophageal echo. An endovascular specialist and a neurosurgeon need to be available for consultation and immediate procedural support, including aneurysm clipping, ventriculostomy placement, intracranial pressure transducer placement, and percutaneous, catheter-based therapy. Dedicated stroke units or neuroscience ICUs with appropriate staffing allow for close monitoring of stroke patients by providers accustomed to treating stroke patients and familiar with their unique needs. Part of the infrastructure of CSCs includes rigorous data collection and outcomes assessment for stroke patients, with the goal of national presentations and peer-reviewed publication in order to advance the field of stroke care. Additionally, community education about recognition of stroke risk factors in conjunction with ambulance bypass systems are crucial components to building successful stroke systems.
Beyond the manpower necessary, organizational components include written protocols that detail the treatment for stroke in a concise and easy-to-follow algorithm. Ideally, these algorithms should be posted in conspicuous locations in the emergency rooms, where any provider who may have contact with stroke patients can have easy access to them. Additionally, the algorithms should spell out the steps to activate the stroke alert teams and what testing (imaging, lab panels, etc.) needs to be performed immediately in stroke patients. Stroke team activation should involve a single call to a standard number, to minimize confusion and response time. Members of the stroke alert teams, including an endovascular specialist, need to be ready to respond to stroke alerts rapidly, including the technicians and nurses which are necessary to operate the angiography suite. Thrombolytic eligibility criteria and contraindications should be included in the algorithms, along with dosing guidelines for intravenous thrombolysis. Pharmacies should have thrombolytics prepackaged and ready to administer within emergency rooms. Again, there is a heavy emphasis on rapid assessment and triage because of the narrow time window in which therapy can be effective in stroke patients. Many of these practices have already been successfully utilized in reducing door-to-balloon times in acute myocardial infarction [60] and are logical to apply to reducing door-to-treatment times for acute stroke. The “time is muscle” paradigm used for treating heart attacks is an excellent model from which to construct a “time is brain” paradigm for treating acute stroke.
Starting a Stroke Program
The development of a new stroke program should incorporate the various components discussed above in an integrated package to provide complete care for stroke patients. A systematic approach to building a stroke program can help the process proceed in manageable steps. The first step is to analyze the available resources in the community, assess what care systems are currently in place for acute stroke, and determine who is providing this care. Next, stroke providers need to come together to form a multidisciplinary consortium to discuss the resources which exist in the community and the benefits of multidisciplinary cooperation, as well as establish a written plan outlining how the available resources can be utilized in unified and systematic way to treat stroke. Part of this process includes setting goals and expectations for how stroke care can be improved in the community, preferably with an understanding of the local stroke outcomes at baseline. A method for tracking outcomes must be established, ideally in the form of a database which can collect key patient and procedural variables and measure both functional outcomes and survival at prespecified time intervals (ideally at discharge, 1 month, and 3 months). Finally, the multidisciplinary consortium must arrange to meet on a regular basis to assess progress, discuss outcomes, and review new developments in the field.
The first step in building a stroke program is to assess what resources are currently available in the community. This includes both physical resources (CT scanners, MRI, etc.) and manpower resources. Remember that these providers can be from multiple disciplines, including neurology, cardiology, vascular surgery, and neurosurgery. Importantly, rehabilitation services following an acute hospital stay are a crucial component of comprehensive stroke care and should not be overlooked. Additionally, emergency services including ambulance crews and emergency physicians should be included in the survey of community resources, as they play an important role in controlling the flow of stroke patients and are the first responders for the majority of stroke patients. Once assessed, the resources should be recorded in a systematic way so that any deficiencies can be recognized. Unique solutions to a lack of community resources may exist in the form of telemedicine, a technology which has been used successfully to help improve outcomes in the treatment of stroke [61].
Following a thorough assessment of resources, the next step in beginning a stroke program is to bring together the key community providers in a forum to discuss the benefits and goals of a stroke program. Ideally, this discussion will be led by the person wishing to form the stroke program, acting as a “cheerleader” to raise awareness of the potential benefits of a stroke program. This meeting is a time to outline the information collected about community resources which are available, discuss acute stroke treatment (including thrombolytic and catheter-based therapy), and identify the barriers which may exist to implementation of these resources. Discussion points include rational for program development, assessment of availability for round-the-clock care, and a plan for how to arrange subsequent meetings. Part of the process is setting expectations for what can be achieved in stroke care. It should be emphasized that the mortality for acute stroke patients is high (approximately 20 % at 3 months for both arms of the NINDS thrombolytic trial [4]) no matter what treatment is rendered and that the benefits of thrombolytic therapy and catheter-based therapy are realized not immediately but at 30–90-day timepoints [4, 5]. Because much of the benefit comes late, it is important to establish a system to follow patients after they receive stroke care. A database which collects pertinent baseline and follow-up clinical variables allows for tracking outcomes and providing feedback to providers. At a minimum, this database should include demographic data, time from symptom onset to presentation, treatments delivered, baseline and follow-up NIHSS and modified Rankin scores [22], and mortality. The rational for cost saving with increased utilization of intravenous thrombolysis for acute stroke should also be discussed [62].
Finally, regularly scheduled meetings need to occur to discuss progress and outcomes. This will allow a forum for the various providers to discuss successes as well as difficulties which they may face in implementing stroke care. A review of the written protocols should be conducted regularly, along with a periodic comprehensive review of new publications and guidelines in the field. As the program takes form, marketing to the community can help educate the public and local providers, which can then fuel further program growth.
Conclusions
Acute stroke is common, has high morbidity and mortality, and is grossly undertreated in the United States. The goals for ischemic stroke therapy should be rapid and safe reperfusion of the culprit artery, either through the use of thrombolytic drugs or mechanical therapies in appropriate patients. Many options currently exist for mechanical embolectomy of stroke and each has unique advantages and disadvantages. The field of stroke intervention is constantly evolving as new devices and new insights are employed. Nevertheless, the “optimal” therapy for acute stroke remains elusive, as the field searches for large-scale multicenter randomized trials which can help build consensus and shape guideline recommendations.
The stroke center concept, which has been outlined by the BAC, provides guidance as to the important components which should be present in order to safely and effectively treat stroke. Current treatment options for ischemic stroke include intravenous thrombolysis as well as catheter-based therapy. Because of the narrow time window and broad exclusion criteria for intravenous thrombolytic therapy, a very small number of patients receive this therapy. Catheter-based therapy offers hope to patients who are ineligible for intravenous thrombolysis by extending the time window for treatment, but is limited by both the small number of providers who are currently performing this therapy and the lack of guidelines for which devices are “best” to use for an individual patient. Efforts are being undertaken by the SCAI and other organizations to increase the number of “stroke interventionalists” who are capable of providing round-the-clock catheter-based therapy. Carotid-stent operators, a broad group of providers from multiple disciplines, are the natural fit to expand the pool of stroke interventionalists, as they are familiar with cannulation of arch vessels and intracerebral anatomy. To realize the full benefits of stroke therapy, organization needs to exist at the community level to treat stroke with the same urgency and systemized approach that has been used for acute MI. This can be accomplished by conducting a thorough assessment of community resources, cooperating across disciplines, and developing written protocols for the standardization of stroke care. Importantly, we need more data in the form of randomized trials as we move forward into the twenty-first century in order to determine the safest and most efficacious ways to treat acute ischemic stroke.
References
Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics–2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117(4):e25–146.
Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010;121(7):e46–215.
Bozzao L, Fantozzi LM, Bastianello S, et al. Ischaemic supratentorial stroke: angiographic findings in patients examined in the very early phase. J Neurol. 1989;236(6):340–2.
Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581–87.
Combined intravenous and intra-arterial recanalization for acute ischemic stroke: the Interventional Management of Stroke Study. Stroke. 2004;35(4):904–11.
The Interventional Management of Stroke (IMS) II Study. IMS II Trial Investigators. Stroke; a journal of cerebral circulation. 2007;38(7):2127–35.
Bose A, Henkes H, Alfke K, et al. The penumbra system: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol. 2008;29(7):1409–13.
Ramee SR, Subramanian R, Felberg RA, et al. Catheter-based treatment for patients with acute ischemic stroke ineligible for intravenous thrombolysis. Stroke. May 2004;35(5):e109–11.
Smith WS, Sung G, Saver J, et al. Mechanical thrombectomy for acute ischemic stroke. Final results of the multi MERCI trial. Stroke. 2008;39:1205–12.
Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke. Jul 2005;36(7):1432–8.
DeVries JT, White CJ, Collins TJ, et al. Acute stroke intervention by interventional cardiologists. Catheter Cardiovasc Interv. 2009;73(5):692–8.
White CJ, Cates CU, Cowley MJ, et al. Interventional stroke therapy: current state of the art and needs assessment. Catheter Cardiovasc Interv. 2007;70(3):471–6.
Schwamm LH, Pancioli A, Acker III JE, et al. Recommendations for the establishment of stroke systems of care: recommendations from the American Stroke Association’s Task Force on the Development of Stroke Systems. Circulation. 2005;111(8):1078–91.
Adams Jr HP, del Zoppo G, Alberts MJ, et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115(20):e478–534.
Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317–29.
Albers GW, Thijs VN, Wechsler L, et al. Magnetic resonance imaging profiles predict clinical response to early reperfusion: the diffusion and perfusion imaging evaluation for understanding stroke evolution (DEFUSE) study. Ann Neurol. Nov 2006;60(5):508–17.
Schaefer PW, Barak ER, Kamalian S, et al. Quantitative assessment of core/penumbra mismatch in acute stroke. CT and MR perfusion imaging are strongly correlated when sufficient brain volume is imaged. Stroke. 2008 Nov;39(11):2986–92.
Hacke W, Donnan G, Fieschi C, et al. Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet. 2004;363(9411):768–74.
NIHSS Web Page. www.strokecenter.org/trials/scales/nihss.html. Accessed 28 Feb 2008.
Kwiatkowski TG, Libman RB, Frankel M, et al. Effects of tissue plasminogen activator for acute ischemic stroke at one year. National Institute of Neurological Disorders and Stroke Recombinant Tissue Plasminogen Activator Stroke Study Group. N Engl J Med. 1999;340(23):1781–7.
Magid D, Naviaux N, Wears RL. Stroking the data: re-analysis of the NINDS trial. Ann Emerg Med. Apr 2005;45(4):385–7.
Modified Rankin Scores. www.strokecenter.org/trials/scales/rankin.html. Accessed 28 Feb 2008.
Demaerschalk BM, Yip TR. Economic benefit of increasing utilization of intravenous tissue plasminogen activator for acute ischemic stroke in the United States. Stroke. Nov 2005;36(11):2500–3.
Thomassen L, Bakke SJ. Endovascular reperfusion therapy in acute ischaemic stroke. Acta Neurol Scand Suppl. 2007;187:22–9.
Furlan A, Higashida R, Wechsler L, et al. Intra-arterial prourokinase for acute ischemic stroke. The PROACT II study: a randomized controlled trial. Prolyse in Acute Cerebral Thromboembolism. JAMA. 1999;282(21):2003–11.
Kleindorfer DO, Khatri P, Katzan I. Reasons for exclusion from thrombolytic therapy following acute ischemic stroke. Neurology. 2005;65(11):1844; author reply 1844.
Davalos A, Blanco M, Pedraza S, et al. The clinical-DWI mismatch: a new diagnostic approach to the brain tissue at risk of infarction. Neurology. 2004;62(12):2187–92.
Kidwell CS, Warach S. Mismatch and defuse: harvesting the riches of multicenter neuroimaging-based stroke studies. Stroke. Jun 2007;38(6):1718–19.
2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1-203.
Smith WS. Safety of mechanical thrombectomy and intravenous tissue plasminogen activator in acute ischemic stroke. Results of the multi Mechanical Embolus Removal in Cerebral Ischemia (MERCI) trial, part I. AJNR Am J Neuroradiol. 2006;27(6):1177–82.
del Zoppo GJ, Higashida RT, Furlan AJ, Pessin MS, Rowley HA, Gent M. PROACT: a phase II randomized trial of recombinant pro-urokinase by direct arterial delivery in acute middle cerebral artery stroke. PROACT Investigators. Prolyse in Acute Cerebral Thromboembolism. Stroke. 1998;29(1):4–11.
Baker WL, Colby JA, Tongbram V, et al. Neurothrombectomy devices for the treatment of acute ischemic stroke: state of the evidence. Ann Intern Med. 2011;154(4):243–52.
Meyers PM, Schumacher HC, Higashida RT, et al. Indications for the performance of intracranial endovascular neurointerventional procedures: a scientific statement from the American Heart Association Council on Cardiovascular Radiology and Intervention, Stroke Council, Council on Cardiovascular Surgery and Anesthesia, Interdisciplinary Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research. Circulation. 2009;119(16):2235–49.
Lewandowski CA, Frankel M, Tomsick TA, et al. Combined intravenous and intra-arterial r-TPA versus intra-arterial therapy of acute ischemic stroke: Emergency Management of Stroke (EMS) Bridging Trial. Stroke. Dec 1999;30(12):2598–605.
Flaherty ML, Woo D, Kissela B, et al. Combined IV and intra-arterial thrombolysis for acute ischemic stroke. Neurology. 2005;64(2):386–8.
Mackey J, Khatri P, Broderick JP, Investigators II. Increasing use of CT angiography in interventional study sites: the IMS III experience. AJNR Am J Neuroradiol. 2010;31(3):E34.
Becker KJ, Brott TG. Approval of the MERCI clot retriever: a critical view. Stroke. Feb 2005;36(2):400–3.
Penumbra Pivotal Stroke Trial I, Clark W, Lutsep H, et al. The penumbra pivotal stroke trial: safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke J Cereb Circ. 2009;40(8):2761–8.
Velat GJ, Hoh BL, Levy EI, Mocco J. Primary intracranial stenting in acute ischemic stroke. Curr Cardiol Rep. 2010;12(1):14–9.
Levy EI, Ecker RD, Horowitz MB, et al. Stent-assisted intracranial recanalization for acute stroke: early results. Neurosurgery. 2006;58(3):458–63. discussion 458-463.
Lee VH, Samuels S, Herbst TJ, et al. Histopathologic description of Wingspan stent in acute ischemic stroke. Neurocrit Care. 2009;11(3):377–80.
Levy EI, Sauvageau E, Hanel RA, Parikh R, Hopkins LN. Self-expanding versus balloon-mounted stents for vessel recanalization following embolic occlusion in the canine model: technical feasibility study. AJNR Am J Neuroradiol. 2006;27(10):2069–72.
Zaidat OO, Wolfe T, Hussain SI, et al. Interventional acute ischemic stroke therapy with intracranial self-expanding stent. Stroke J Cereb Circ. 2008;39(8):2392–5.
Levy EI, Siddiqui AH, Crumlish A, et al. First Food and Drug Administration-approved prospective trial of primary intracranial stenting for acute stroke: SARIS (stent-assisted recanalization in acute ischemic stroke). Stroke J Cereb Circ. 2009;40(11):3552–6.
Weber W, Kis B, Siekmann R, Kuehne D. Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. AJNR Am J Neuroradiol. 2007;28(2):371–7.
Castano C, Dorado L, Guerrero C, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation: a pilot study. Stroke J Cereb Circ. 2010;41(8):1836–40.
Roth C, Papanagiotou P, Behnke S, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke J Cereb Circ. 2010;41(11):2559–67.
Levy EI, Rahman M, Khalessi AA, et al. Midterm clinical and angiographic follow-up for the first Food and Drug Administration-approved prospective, Single-Arm Trial of Primary Stenting for Stroke: SARIS (Stent-Assisted Recanalization for Acute Ischemic Stroke). Neurosurgery. 2011;69(4):915–20. discussion 920.
Kelly ME, Furlan AJ, Fiorella D. Recanalization of an acute middle cerebral artery occlusion using a self-expanding, reconstrainable, intracranial microstent as a temporary endovascular bypass. Stroke J Cereb Circ. 2008;39(6):1770–3.
Hauck EF, Mocco J, Snyder KV, Levy EI. Temporary endovascular bypass: a novel treatment for acute stroke. AJNR Am J Neuroradiol. 2009;30(8):1532–3.
O’Collins VE, Macleod MR, Donnan GA, Horky LL, van der Worp BH, Howells DW. 1,026 experimental treatments in acute stroke. Ann Neurol. 2006;59(3):467–77.
Hypothermia after Cardiac Arrest Study G. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549–56.
Ueda Y, Suehiro E, Wei EP, Kontos HA, Povlishock JT. Uncomplicated rapid posthypothermic rewarming alters cerebrovascular responsiveness. Stroke J Cereb Circ. 2004;35(2):601–6.
Suzuki S, Saver JL, Scott P, et al. Access to intra-arterial therapies for acute ischemic stroke: an analysis of the US population. AJNR Am J Neuroradiol. 2004;25(10):1802–6.
SCAI first to offer multidisciplinary course in acute stroke intervention. Cathet Cardiovas Interv. 2008;71:445–6.
Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain Attack Coalition. JAMA. 2000;283(23):3102–9.
Skolnick BE. Guidelines for acute stroke treatment centers. Phys Med Rehabil Clin N Am. 1999;10(4):801–13. viii.
Furlan AJ, Murdock MM, Spilker JA. NSA stroke center network stroke center recommendations. J Stroke Cerebrovas Dis. 1997;6(4):299–302.
Alberts MJ, Latchaw RE, Selman WR, et al. Recommendations for comprehensive stroke centers: a consensus statement from the Brain Attack Coalition. Stroke. Jul 2005;36(7):1597–616.
Antman EM. Time is muscle: translation into practice. J Am Coll Cardiol. 2008;52(15):1216–21.
Meyer BC, Raman R, Hemmen T, et al. Efficacy of site-independent telemedicine in the STRokE DOC trial: a randomised, blinded, prospective study. Lancet Neurol. 2008;7(9):787–95.
Demaerschalk BM, Yip TR. Economic benefit of increasing utilization of intravenous tissue plasminogen activator for acute ischemic stroke in the United States. Stroke. 2005;36(11):2500–3.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
DeVries, J.T. (2014). Acute Stroke Intervention. In: Thompson, C. (eds) Textbook of Cardiovascular Intervention. Springer, London. https://doi.org/10.1007/978-1-4471-4528-8_36
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4528-8_36
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4527-1
Online ISBN: 978-1-4471-4528-8
eBook Packages: MedicineMedicine (R0)