Abstract
In the last years, we have faced a blooming of mechanical thrombectomy (MT). Numerous randomized controlled trials have shown the benefit of MT, combined with the best medical treatment, in the setting of acute ischemic stroke with large vessel occlusion. Thus, the management and triage of patients with acute ischemic stroke have become crucial in order to offer a swift recanalization to these patients. In this chapter, we will summarize the recent data of the literature on MT, review the indications and guidelines for MT, and discuss the different strategies for triage. We will also present the different techniques available for MT, and their respective safety and effectiveness.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Recent Data on Mechanical Thrombectomy
Until 2015, all randomized controlled trials (RCTs) that have evaluated the effectiveness of mechanical thrombectomy (MT) in the setting of acute ischemic stroke (AIS) with large vessel occlusion (LVO) failed to demonstrate a benefit in terms of 3 months’ neurological outcome compared with the best medical treatment (BMT) (Ciccone et al. 2013; Broderick et al. 2013; Kidwell et al. 2013). In 2015, five RCTs (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015), with a close design, showed a strong benefit of MT in patients with LVO, associated with the BMT. Indeed, in these studies, the gap of good neurological outcome (i.e., modified Rankin Scale [mRS] score ≤2 at 3 months’ follow-up) in favor of MT + BMT varied from 13.5 to 31%, and the number of patients needed to treat (NNT) to gain a patient with independency at 3-month follow-up ranged from 3 to 8. In most of the studies, the time window to start the MT procedure was 6 h, but some studies, selecting the patients with a small core infarct, extended the time window to 8 or even 12 h (REVASCAT (Jovin et al. 2015) and ESCAPE(Goyal et al. 2015) studies, respectively).
One could wonder what happened between the negative studies published in 2013 and the positive ones published in 2015. First, the patients’ selection was more rigorous in the recent studies, which involved only patients with imaging-proven LVO. Second, all positive RCTs used the most recent MT devices, especially stent retrievers, while first-generation devices were used in previous RCTs. These methodological issues may explain the discrepancies between older and recent RCTs.
Since then, two additional RCTs have been published (Bracard et al. 2016; Mocco et al. 2016), confirming the results of the first five RCTs published in 2015.
2 Indications of Mechanical Thrombectomy
In 2015, the American Heart Association (AHA)/American Stroke Association (ASA) published its recommendations concerning the indications of MT in the setting of AIS with LVO, based on the five above-mentioned RCTs published in 2015 in the New England Journal of Medicine (Powers et al. 2015). These recommendations specified that patients for whom MT was considered should receive IV thrombolysis if no contraindication is found. MT should be performed in patients ≥18 years, with an imaging proven LVO (M1 or ICA), with pre-MT mRS score ≤1, with a NIHSS (National Institutes of Health Stroke Scale) ≥6 and an ASPECTS (Alberta Stroke Program Early CT score) ≥6. MT should be initiated (groin puncture) within 6 h of symptom onset and performed with a stent retriever.
Recently, two RCTs have expanded the time window for mechanical thrombectomy in patients with an AIS due to LVO: the DWAN trial (Nogueira et al. 2018) and the DEFUSE 3 study (Albers et al. 2018).
The DAWN (Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo) trial (Nogueira et al. 2018) is a RCT that involved 206 patients and aimed at comparing MT associated with BMT vs BMT alone between 6 and 24 h from symptoms’ onset (known symptoms’ onset or last known well) in patients with AIS and LVO. Selection criteria, based on the core infarct volume, were as follows: infarct volume <31 ml in patients less than 80 years with a NIHSS ≥10 or infarct volume <51 ml in patients less than 80 years with a NIHSS ≥20 or infarct volume <21 ml in patients ≥80 years with a NIHSS ≥10. At 3 months’ follow-up, good clinical outcome (i.e., mRS ≤ 2) was observed in 48.6% in the group MT + BMT vs 13.1% in the BMT group. Additionally, the NNT was close to 3 (2.8). For comparison purpose, the NNT for the exclusion treatment of ruptured intracranial aneurysms is 13 (Lanzino et al. 2013). It is noteworthy that about two-third of the patients included in the DWAN trial were wake-up strokes and that one-fourth were AIS with undetermined stroke onset.
Another recent study has expended the time window for MT: the DEFUSE3 trial (Albers et al. 2018). This study involved 182 patients from 38 centers from the United States. Patients with an AIS with LVO (proximal MCA or ICA occlusions), between 6 and 16 h after the symptom onset (or last known to be well) an initial infarct size of less than 70 ml, and a ratio of the volume of ischemic tissue on perfusion imaging to infarct volume of 1.8 or more, were randomized either for MT + BMT vs BMT alone. Results in terms of independency (mRS ≤2 at 3 months’ follow-up) were better for the MT + BMT arm (45% vs 17%, P < 0.001). Additionally, the 90-day mortality rate was 14% in the endovascular therapy group and 26% in the medical therapy group (P = 0.05).
Since the publication of the DAWN and DEFUSE3 trials, AHA and ASA have updated their recommendations in 2018 (Powers et al. 2018), which now take into account a wider time window for MT, in selected patients, according to the above-described imaging criteria.
What DAWN and DEFUSE3 trials have in common is the patients’ selection based on some form of mismatch. The mismatch is defined as the difference between hypoperfused and infarcted tissue and has many imaging and clinical surrogates. Identifying patients with symptomatic ischemic penumbra, at risk of evolution toward infarction, and amenable to tissue salvage by emergent LVO revascularization, is bound to be the cornerstone of patient selection for MT in the future.
3 Triage for Mechanical Thrombectomy
With the blooming of mechanical thrombectomy, due to the critical influence of the time to recanalization, triage of patients eligible for MT has become a crucial point. Indeed, the benefit of MT in terms of functional outcome decreases with time. For instance, it has been shown in the meta-analysis of Saver et al. that for every 4-min delay in emergency department door-to-reperfusion time, 1 of every 100 treated patients had a worse disability outcome, leading to no significant benefit of MT when initiated more than 7.3 h after the symptoms’ onset (Saver et al. 2016). Thus, numerous strategies have been proposed and studied to improve the patient workflow and reduce, as much as possible, these critical times.
3.1 “Mothership” Vs “Drip and Ship”
Discrepancies in terms of equipment and facilities exist between the different hospitals in which patients with AIS associated with LVO may be managed. Indeed, some of them have both a neurovascular unit and an interventional neuroradiology department, in which MT can be performed. In these hospitals (called “comprehensive stroke centers”), the patients are directly sent to the angiography suite. This workflow is called the “Mothership” paradigm. In other hospitals (called “primary stroke centers”), no department of interventional neuroradiology is present. Thus, after neurological examination and imaging confirming the diagnosis of AIS with LVO, the patient will be transferred to another hospital in which MT will be performed. If the patient is admitted in the primary stroke center within the time window for IV thrombolysis, the tPA injection will be performed before the transfer to the comprehensive center. This workflow is called the “Drip and Ship” paradigm (Detraz et al. 2018).
In terms of safety, numerous non-randomized studies (Park et al. 2016a, b; Hiyama et al. 2016; Gerschenfeld et al. 2017) have shown no difference between the 2 paradigms on mortality rate, symptomatic hemorrhages, or intraoperative adverse events. Additionally, effectiveness of both paradigms, in terms of 3 months’ neurological outcome, appears equivalent according to these non-randomized series (Park et al. 2016a, b; Hiyama et al. 2016; Gerschenfeld et al. 2017).
Interestingly, no RCT has compared the safety and the effectiveness of these two paradigms.
3.2 Clinical Scores
To improve the prehospital triage of patients who may benefit from MT, clinical scores may be used (Perez de la Ossa et al. 2014; Hastrup et al. 2016; Lima et al. 2016; Katz et al. 2015). This strategy may help to depict indirectly patients who may have LVO in order to refer them directly to a comprehensive stroke center. However, according to a recent publication, using published cut-offs of these scores for triage would result in a loss of opportunity for ≥20% of patients with LVO, who would be inappropriately sent to a center without neurointerventional angiography suite. On the contrary, using these cut-offs would result in sending patients inappropriately (false positive for LVO eligible to MT) to a comprehensive stroke center in 10% of the cases (Turc et al. 2016). To date, none of these scores can avoid performing cerebral imaging for triage.
3.3 Triage in Angiography Suite
Recently, some teams have proposed performing triage directly in the angiography suite (Ribo et al. 2018). Indeed, the recent advances in the cone-beam flat panel technology allow performing CT scan, CT angiography, and CT perfusion directly in the angio suite (van der Bom et al. 2012). This option may help avoiding loosing time during the different transfers of the patients. This “all-inclusive” option with C-arm CT acquisitions seems at a first glance very seducing since it reduces the delay between imaging acquisition and groin puncture and thus revascularization time (Ribo et al. 2017). However, this strategy for patients triage may have some limitations (Clarencon et al. 2018). Indeed, a consistent number of patients with no AIS (intraparenchymal hemorrhage, stroke mimic) or with AIS but no LVO may be screened in the angiography suite with this triage method, which may be a considerable source of disorganization for interventional neuroradiology departments, and may also be not cost-effective.
3.4 Perspectives
A perspective to improve the patient workflow is the use of an ambulance carrying a CT scan on which regular CT acquisition, as well as CTA and CT perfusion, could be performed (John et al. 2016). Preliminary experiences with such “mobile stroke units” have been described in different towns like Berlin (Ebinger et al. 2015) or Cleveland (Taqui et al. 2017). This strategy may help improving the patient transfer to the comprehensive stroke center (El-Ghanem et al. 2017). Telestroke management, mobile neuro-endovascular teams, or smart device applications may be other potential solutions to improve the patient workflow (El-Ghanem et al. 2017).
4 Technique(S)
4.1 Stent Retriever or Aspiration Catheter?
In most of the recent RCTs, the benefit of MT in AIS with LVO has been proven with stent retrievers (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015). Fewer evidences are available concerning the effectiveness of aspiration with large bore catheters (Mocco et al. 2016). Stent retrievers are non-detachable stents, which will be opened in the clot in order to grab the clot within the stent retriever’s mesh. Then, the stent retriever will be removed opened in the guiding catheter (Kang and Park 2017). In this technique, the clot is anchored in the stent retriever’s mesh and withdrawn through the guiding catheter. To avoid fragmentation of the clot during removal, and thus the risk of clot migration in the same and/or another territory, flow arrest with balloon guiding catheters or combination of stent retriever with aspiration catheter close to the thrombus may be used (cf infra).
Based on mTICI (modified thrombolysis in cerebral infarction) score (Zaidat et al. 2013) grading (Table 1), a 77% recanalization rate (mTICI 2b or 3) has been reported with stent retrievers (Campbell et al. 2016).
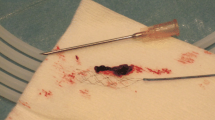
An alternative strategy is the contact aspiration. This technique consists in navigating a large bore catheter in contact with the clot and to aspirate the clot, either by manual aspiration or by means of an aspiration pump (Fig. 1). ADAPT (a direct aspiration first-pass technique) is a variant of the aspiration technique, which consists in using aspiration thrombectomy as the first-line treatment with the possibility of adjuvant treatment if recanalization is not initially achieved. Fewer evidences are available for the effectiveness of aspiration/ADAPT for the management of AIS with LVO. Effectiveness of the aspiration technique in terms of recanalization (TICI 2b-3) has been reported ranging from 65 to 89% (Wei et al. 2017); the one of ADAPT technique from 76% to 97% (Wei et al. 2017). Good 3 months’ clinical outcome with the aspiration technique has been reported ranging from 38 to 78% (Wei et al. 2017) and from 39 to 84% with the ADAPT technique (Wei et al. 2017) .Interestingly a benchtop study has shown that the ADAPT technique was responsible for fewer distal emboli, compared with stent retriever thrombectomy technique (Chueh et al. 2016).
A 63-year-old female with sudden onset of left hemiplegia. NIHHSS = 12. (a) MRI diffusion-weighted image, axial slice, showing a faint hyperintense signal located on the right aspect of the pons (arrow). (b) 3D time-of-flight MR angiography demonstrating an occlusion of the mid- and distal aspects of the basilar artery (arrow). (c) Left vertebral artery digital subtraction angiography (DSA) in anteroposterior (AP) projection confirming the occlusion of the basilar artery, distally to the origin of the antero-inferior cerebellar arteries (arrow). (d) Road map from the left vertebral artery in AP projection. Navigation of a large bore catheter (0.068″) close to the occlusion site. After a 90s aspiration, the catheter is removed under aspiration with a pump. (e) Left vertebral artery DSA in AP projection at the end of the procedure. Complete recanalization of the basilar artery is seen, after one aspiration pass. The procedure, from the groin puncture to the final DSA run, lasted 15 min
The THERAPY trial (Mocco et al. 2016) was the sole RCT that compared MT performed with the ADAPT technique + BMT vs BMT alone. This study did not show significant difference between the two treatment strategies (38% vs 30%, P = 0.52) but the study was prematurely stopped (108 patients enrolled; 692 patients planed for inclusion) after the publication of the results of the MR CLEAN trial (Berkhemer et al. 2015).
Only one RCT has compared the ADAPT technique vs the stent retriever technique: the ASTER trial (Lapergue et al. 2017). The results of this study showed no statistically significant difference in terms of recanalization rate or good clinical outcome between the two techniques. A non-significant trend toward a lower complication rate (emboli in a new territory, symptomatic hemorrhage) was observed in the group treated by the ADAPT technique.
4.2 Balloon Guiding Catheters
Balloon guiding catheters (BGCs) are guiding catheters with a balloon mounted at their tip. The balloon is inflated during the retrieval of the stent retriever in order to obtain flow arrest and to reduce the risk of emboli migration either in the same territory or in another one. A number of benchtop studies have shown the benefit of using BGCs to reduce distal emboli during MT and to obtain more effective revascularization (Chueh et al. 2013; Mokin et al. 2016). Numerous clinical studies have also shown a benefit in terms of angiographic and clinical outcomes with the use of BGCs in MT (Nguyen et al. 2014; Velasco et al. 2016). In a recent meta-analysis, it has been shown that patients treated with BGCs had higher odds of first-pass recanalization and higher rates of TICI 3 or TICI 2b/3 recanalizations (Brinjikji et al. 2018). Additionally, patients treated with BGCs had a higher rate of 3 months’ good neurological outcome (59.7% vs 43.8%) and a lower mortality rate (13.7% vs 24.8%). Mean procedure time was also significantly shorter for patients treated with BGCs (weighted mean difference: −7.7 min, 95% CI − 9.0 to −6.4) (Brinjikji et al. 2018). It is however noteworthy that no RCT has proven the superiority of BGCs in MT over the other techniques.
4.3 Combined Technique
Numerous series have studied a technique combining aspiration catheter and stent retriever for clot removal (Delgado Almandoz et al. 2016) (Fig. 2). Various names have been given to this technique with faint variations: Solumbra (Delgado Almandoz et al. 2016), ARTS (aspiration-retriever technique for stroke) (Massari et al. 2016), SAVE (Stent retriever Assisted Vacuum-locked Extraction) (Maus et al. 2018).
A 47-year-old female presenting a sudden onset of right hemiplegia and aphasia (NIHSS = 24). (a) MRI diffusion-weighted image, axial slice, showing a slight hyperintense signal on the right insula (white arrow) and of the left caudate nucleus (black arrow). (b) 3D time-of-flight MR angiography demonstrating an occlusion of the left MCA (M1 segment). Left internal carotid artery (ICA) DSA in AP (c) and lateral (d) projections showing an occlusion of the M1 segment (c, arrow) with hypoperfusion of the whole left MCA territory (d). (e) Road map from the left ICA with the aspiration catheter positioned in M1 (black arrow) and the stent retriever opened in the thrombus (white arrowhead). (f) Retrieval of the stent retriever inside the aspiration catheter under aspiration (black arrow, aspiration catheter’s tip; white arrowhead, stent retriever). On control DSA in AP (g) and lateral (h) projection, complete recanalization of the left MCA territory is seen (mTICI3)
Recently, a technique combining stent retriever + aspiration catheter + balloon guiding catheter (the so-called “PROTECT” [PRoximal balloon Occlusion TogEther with direCt Thrombus aspiration] technique) has been described, with promising results (Maegerlein et al. 2018). Finally, a RCT comparing BGC associated with intermediate catheter and stent retriever vs BGC with stent retriever alone has recently been performed (the “ASTER2” trial, ClinicalTrial NCT03290885); the results of this study will soon be published.
5 Safety of Mechanical Thrombectomy
The safety of MT has been proven, and regarding adverse events, many RCTs have proven that patients who underwent MT with BMT vs BMT alone did not have significantly higher mortality or symptomatic intracranial hemorrhage rates (Barral et al. 2018).
Mortality rate in patients treated by MT has been reported ranging from 9% to 21% (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015), which is not significantly higher than in patients with LVO who received the BMT (Marmagkiolis et al. 2015).
A meta-analysis has found a symptomatic intracranial hemorrhage rate of 5.6% in patients treated by MT (range: 0–7.7%), which is quite similar to the one of medical treatment (5.2%) (Hao et al. 2017). However, the rate of asymptomatic intracranial hemorrhage is higher in patients treated by MT compared with BMT (28% vs 13.9%) (Hao et al. 2017). The perforation rate (with either the microguide wire, the microcatheter, or the stent retriever) in MT has been reported ranging from 0% to 4.9% in the first RCTs (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015).
Migration of emboli in another territory (for instance migration in an embolus in the anterior cerebral artery during an MCA thrombectomy) may also occur during MT and may worsen the patient’s clinical condition. They have been reported occurring as frequently as in about 10% of the cases (Chalumeau et al. 2018).
Another complication that may occur after MT is a groin hematoma. Groin hematomas may be observed in about 5% of the cases (Chivot et al. 2018). Most of these hematomas are ≤5 cm and do not require surgical treatment and/or blood transfusion. They are not more frequently observed in patients who received IV tPA, or those previously treated with antiplatelet therapy. Interestingly, groin hematomas are not more frequent when the puncture is ipsilateral to the inferior limb’s neurological deficit (Chivot et al. 2018).
6 Effectiveness of Mechanical Thrombectomy
Effectiveness of MT in terms of recanalization (mTICI 2b-3) has been reported ranging from 58.7% to 100% in the recent RCTs (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015). The pooled estimate of patients with mTICI 2b–3 after MT was 71% (95% CI: 62–79%). These RCTs also demonstrated a significant improvement in terms of neurological outcome (mRS scores 0–2 at 3 months) in patients treated with MT: OR = 2.14, 95% CI: 1.72–2.67 (P < 0.00001) (Barral et al. 2018).
Only three studies (REVASCAT (Jovin et al. 2015), ESCAPE (Goyal et al. 2015), and THRACE (Bracard et al. 2016)) reported the results of Barthel index scores and showed the superiority of MT + BMT over BMT alone (scores of 95–100 at 3 months, OR: 2.43, 95% CI) (Barral et al. 2018).
However, it is noteworthy that MT has no significant impact on survival rate (OR: 0.82, 95% CI: 0.62–1.07) (Barral et al. 2018).
7 Questions Yet to be Answered
7.1 Is Intravenous Thrombolysis Still Necessary in Combination with Mechanical Thrombectomy?
In all the RCTs demonstrating the effectiveness of MT, endovascular treatment was associated with the BMT, being most of times the IV thrombolysis. One could wonder if IV thrombolysis is really required in combination with MT. Indeed, IV tPA could potentially be responsible for higher intracranial hemorrhage rates and may worsen puncture site complications. Additionally, IV thrombolysis may lead to a clot fragmentation, which could be responsible for more challenging MT procedures with numerous distal emboli to remove instead of one proximal thrombus.
Results from non-randomized studies are contradictory. Indeed, some series have clearly shown the benefit of additional IV thrombolysis in combination with MT (Goyal et al. 2018). Others found no clinical benefit in combining MT with IV thrombolysis (Coutinho et al. 2017; Kass-Hout et al. 2014).
Additionally, symptomatic hemorrhages and groin puncture complication rates are not statically higher in patients treated by MT and IV thrombolysis.
The only RCT that compared BMT alone vs MT, the Synthesis-Expansion trial (Ciccone et al. 2013), was in disfavor of MT. However, in this study, numerous endovascular procedures were not performed with the most recent MT devices, such as stent retrievers.
More evidences on the benefit of pre-MT IV thrombolysis are yet to be provided, through RCTs using the most recent MT devices.
7.2 Distal Occlusions
In the RCTs, most of the occlusion sites were proximal (i.e., ICA terminus or proximal M1). Only limited data on the effectiveness of MT in distal occlusions are thus available. In the above-mentioned RCTs that proved the benefit of MT in LVO (Berkhemer et al. 2015; Jovin et al. 2015; Goyal et al. 2015; Campbell et al. 2015; Saver et al. 2015; Bracard et al. 2016; Mocco et al. 2016), the rate of patients included with a M2 occlusion ranged from 1% to 14.3%.
No RCT has evaluated the benefit of MT in M2 occlusions. According to a recent meta-analysis (Saber et al. 2018), recanalization after MT in M2 occlusions is obtained in 81% of the cases, with no significant difference with the recanalization rate in M1 occlusions. Good clinical outcome is obtained in 56.2% of the cases for MT in M2 occlusions, which is significantly higher than in M1 occlusions (Saber et al. 2018). However, it is noteworthy that patients with a M1 occlusion usually have a poorer initial condition than those with a M2 occlusion (Bhogal et al. 2017). Additionally, MT in M2 occlusions may be associated with a higher risk of vessel perforation due to vessel fragility (Mokin et al. 2017) and an increased risk of symptomatic intracranial hemorrhage (Saber et al. 2018).
Finally, it should be mentioned that only short retrospective case series (Uno et al. 2018) are available on the effectiveness of MT in anterior cerebral arteries occlusions, and no series has been published on PCA occlusions treated by MT. No RCTs studying the effectiveness of MT + BMT vs BMT alone are available for these specific occlusion sites.
7.3 Basilar Artery Occlusions
To date, no RCT has demonstrated the superiority of MT combined with the BMT over the BMT alone in patients with basilar artery occlusion (BAO). A systematic review of the literature showed a recanalization rate ranging from 44 to 100% (average 80%) and a good 3 months’ clinical outcome from 20 to 58% (average 43%) in patients with BAO treated by MT. A recent meta-analysis (Gory et al. 2016) showed a 3 months’ favorable outcome in 42% of the patients and a mortality rate of 30%. Symptomatic intracranial hemorrhage rate in this meta-analysis was 4%. Predictors of mortality in patients treated by MT for BAO were mainly age ≥60 years, a high initial NIHSS at admission, and absence of successful recanalization (Gory et al. 2018). Two prospective RCTs (BASICS [NCT01717755] and Best [NCT02441556] trials) are currently ongoing, comparing MT + BMT vs BMT alone in order to prove definitively the effectiveness of MT in BAO.
7.4 Anesthesia for Mechanical Thrombectomy
The best strategy for anesthesia (i.e., general anesthesia, conscious sedation, or local anesthesia) in MT is still debated. A first meta-analysis from the recent RCTs (Ouyang et al. 2016) showed evidences of a better outcome in patients treated under conscious sedation vs general anesthesia. However, these results were biased since no randomization was performed on this criterion. Additionally, one could wonder that patients in worse condition at admission, who will usually have the worse clinical outcome at follow-up, were more frequently treated under general anesthesia due to an agitation or a comatose state. Three RCTs (Schonenberger et al. 2016; Lowhagen Henden et al. 2017; Simonsen et al. 2018) have been published, comparing general anesthesia vs non-general anesthesia MT. In all these 3 RCTs, no significant difference was observed in terms of clinical outcome between the two techniques. Interestingly, these studies were all mono-centric.
8 Conclusion
In recent years, MT has radically changed the management of patients with AIS secondary to LVO. Numerous evidences have been gathered on its safety and effectiveness and have shown its superiority compared with the BMT alone. Time window for MT has been recently expanded for patients with a small core infarct.
Numerous questions have yet to be answered, especially for distal occlusions or basilar artery occlusions.
Abbreviations
- ADAPT:
-
A direct aspiration first-pass technique
- AHA:
-
American Heart Association
- AIS:
-
Acute ischemic stroke
- ASA:
-
American Stroke Association
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- BMT:
-
Best medical treatment
- CSS:
-
Comprehensive stroke center
- ICA:
-
Internal carotid artery
- IV:
-
Intravenous
- LVO:
-
Large vessel occlusion
- MCA:
-
Middle cerebral artery
- MT:
-
Mechanical thrombectomy
- mRS:
-
Modified Rankin Scale
- mTICI score:
-
Modified thrombolysis in cerebral infarction score
- NIHSS:
-
National Institutes of Health Stroke Scale
- NNT:
-
Number of patients needed to treat
- RCT:
-
Randomized controlled trial
- tPA:
-
Tissue plasminogen activator
References
Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S et al (2018) Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med 378:708–718
Barral M, Boudour S, Viprey M, Giroudon C, Aulagner G, Schott AM et al (2018) Stent retriever thrombectomy for acute ischemic stroke: a systematic review and meta-analysis of randomized controlled trials, including thrace. Rev Neurol (Paris) 174:319–326
Berkhemer OA, van Zwam WH, Dippel DW, Investigators MC (2015) Stent-retriever thrombectomy for stroke. N Engl J Med 373:1076
Bhogal P, Bucke P, AlMatter M, Ganslandt O, Bazner H, Henkes H et al (2017) A comparison of mechanical thrombectomy in the m1 and m2 segments of the middle cerebral artery: a review of 585 consecutive patients. Interv Neurol 6:191–198
Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T et al (2016) Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol 15:1138–1147
Brinjikji W, Starke RM, Murad MH, Fiorella D, Pereira VM, Goyal M et al (2018) Impact of balloon guide catheter on technical and clinical outcomes: a systematic review and meta-analysis. J Neurointerv Surg. 10:335–339
Broderick JP, Tomsick TA, Palesch YY (2013) Endovascular treatment for acute ischemic stroke. N Engl J Med 368:2432–2433
Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N et al (2015) Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 372:1009–1018
Campbell BC, Hill MD, Rubiera M, Menon BK, Demchuk A, Donnan GA et al (2016) Safety and efficacy of solitaire stent thrombectomy: individual patient data meta-analysis of randomized trials. Stroke 47:798–806
Chalumeau V, Blanc R, Redjem H, Ciccio G, Smajda S, Desilles JP et al (2018) Anterior cerebral artery embolism during thrombectomy increases disability and mortality. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2018-013793
Chivot C, Deramond H, Bouzerar R, Yzet T (2018) Safety and efficacy of femoral artery closure with the femoseal device after cerebral thrombectomy using an 8 french sheath. Eur J Vasc Endovasc Surg 55:730–734
Chueh JY, Kuhn AL, Puri AS, Wilson SD, Wakhloo AK, Gounis MJ (2013) Reduction in distal emboli with proximal flow control during mechanical thrombectomy: a quantitative in vitro study. Stroke 44:1396–1401
Chueh JY, Puri AS, Wakhloo AK, Gounis MJ (2016) Risk of distal embolization with stent retriever thrombectomy and adapt. J Neurointerv Surg. 8:197–202
Ciccone A, Valvassori L, Investigators SE (2013) Endovascular treatment for acute ischemic stroke. N Engl J Med 368:2433–2434
Clarencon F, Rosso C, Degos V, Shotar E, Rolla-Bigliani C, Samson Y et al (2018) Triage in the angiography suite for mechanical thrombectomy in acute ischemic stroke: not such a good idea. AJNR Am J Neuroradiol 39:E59–E60
Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Clark W, Davalos A et al (2017) Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the swift and star studies. JAMA Neurol 74:268–274
Delgado Almandoz JE, Kayan Y, Young ML, Fease JL, Scholz JM, Milner AM et al (2016) Comparison of clinical outcomes in patients with acute ischemic strokes treated with mechanical thrombectomy using either solumbra or adapt techniques. J Neurointerv Surg. 8:1123–1128
Detraz L, Ernst M, Bourcier R (2018) Stroke transfer and its organizational paradigm : review of organizational paradigms and the impact on outcome. Clin Neuroradiol. https://doi.org/10.1007/s00062-018-0715-z
Ebinger M, Kunz A, Wendt M, Rozanski M, Winter B, Waldschmidt C et al (2015) Effects of golden hour thrombolysis: a prehospital acute neurological treatment and optimization of medical care in stroke (phantom-s) substudy. JAMA Neurol 72:25–30
El-Ghanem M, Al-Mufti F, Thulasi V, Singh IP, Gandhi C (2017) Expanding the treatment window for ischemic stroke through the application of novel system-based technology. Neurosurg Focus 42:E7
Gerschenfeld G, Muresan IP, Blanc R, Obadia M, Abrivard M, Piotin M et al (2017) Two paradigms for endovascular thrombectomy after intravenous thrombolysis for acute ischemic stroke. JAMA Neurol 74:549–556
Gory B, Eldesouky I, Sivan-Hoffmann R, Rabilloud M, Ong E, Riva R et al (2016) Outcomes of stent retriever thrombectomy in basilar artery occlusion: an observational study and systematic review. J Neurol Neurosurg Psychiatry 87:520–525
Gory B, Mazighi M, Labreuche J, Blanc R, Piotin M, Turjman F et al (2018) Predictors for mortality after mechanical thrombectomy of acute basilar artery occlusion. Cerebrovasc Dis 45:61–67
Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J et al (2015) Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 372:1019–1030
Goyal N, Tsivgoulis G, Frei D, Turk A, Baxter B, Froehler MT et al (2018) Comparative safety and efficacy of combined ivt and mt with direct mt in large vessel occlusion. Neurology 90:e1274–e1282
Hao Y, Zhang Z, Zhang H, Xu L, Ye Z, Dai Q et al (2017) Risk of intracranial hemorrhage after endovascular treatment for acute ischemic stroke: systematic review and meta-analysis. Interv Neurol. 6:57–64
Hastrup S, Damgaard D, Johnsen SP, Andersen G (2016) Prehospital acute stroke severity scale to predict large artery occlusion: design and comparison with other scales. Stroke 47:1772–1776
Hiyama N, Yoshimura S, Shirakawa M, Uchida K, Oki Y, Shindo S et al (2016) Safety and effectiveness of drip, ship, and retrieve paradigm for acute ischemic stroke: a single center experience. Neurol Med Chir (Tokyo) 56:731–736
John S, Stock S, Cerejo R, Uchino K, Winners S, Russman A et al (2016) Brain imaging using mobile ct: current status and future prospects. J Neuroimaging 26:5–15
Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A et al (2015) Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 372:2296–2306
Kang DH, Park J (2017) Endovascular stroke therapy focused on stent retriever thrombectomy and direct clot aspiration: historical review and modern application. J Korean Neurosurg Soc 60:335–347
Kass-Hout T, Kass-Hout O, Mokin M, Thesier DM, Yashar P, Orion D et al (2014) Is bridging with intravenous thrombolysis of any benefit in endovascular therapy for acute ischemic stroke? World Neurosurg 82:e453–e458
Katz BS, McMullan JT, Sucharew H, Adeoye O, Broderick JP (2015) Design and validation of a prehospital scale to predict stroke severity: Cincinnati prehospital stroke severity scale. Stroke 46:1508–1512
Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z et al (2013) A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med 368:914–923
Lanzino G, Murad MH, d'Urso PI, Rabinstein AA (2013) Coil embolization versus clipping for ruptured intracranial aneurysms: a meta-analysis of prospective controlled published studies. AJNR Am J Neuroradiol 34:1764–1768
Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G et al (2017) Effect of endovascular contact aspiration vs stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: the aster randomized clinical trial. JAMA 318:443–452
Lima FO, Silva GS, Furie KL, Frankel MR, Lev MH, Camargo EC et al (2016) Field assessment stroke triage for emergency destination: a simple and accurate prehospital scale to detect large vessel occlusion strokes. Stroke 47:1997–2002
Lowhagen Henden P, Rentzos A, Karlsson JE, Rosengren L, Leiram B, Sundeman H et al (2017) General anesthesia versus conscious sedation for endovascular treatment of acute ischemic stroke: the AnStroke trial (anesthesia during stroke). Stroke 48:1601–1607
Maegerlein C, Monch S, Boeckh-Behrens T, Lehm M, Hedderich DM, Berndt MT et al (2018) Protect: proximal balloon occlusion together with direct thrombus aspiration during stent retriever thrombectomy - evaluation of a double embolic protection approach in endovascular stroke treatment. J Neurointerv Surg. 10:751–755
Marmagkiolis K, Hakeem A, Cilingiroglu M, Gundogdu B, Iliescu C, Tsitlakidou D et al (2015) Safety and efficacy of stent retrievers for the management of acute ischemic stroke: comprehensive review and meta-analysis. JACC Cardiovasc Interv 8:1758–1765
Massari F, Henninger N, Lozano JD, Patel A, Kuhn AL, Howk M et al (2016) Arts (aspiration-retriever technique for stroke): initial clinical experience. Interv Neuroradiol 22:325–332
Maus V, Behme D, Kabbasch C, Borggrefe J, Tsogkas I, Nikoubashman O et al (2018) Maximizing first-pass complete reperfusion with save. Clin Neuroradiol 28:327–338
Mocco J, Zaidat OO, von Kummer R, Yoo AJ, Gupta R, Lopes D et al (2016) Aspiration thrombectomy after intravenous alteplase versus intravenous alteplase alone. Stroke 47:2331–2338
Mokin M, Setlur Nagesh SV, Ionita CN, Mocco J, Siddiqui AH (2016) Stent retriever thrombectomy with the cover accessory device versus proximal protection with a balloon guide catheter: in vitro stroke model comparison. J Neurointerv Surg. 8:413–417
Mokin M, Fargen KM, Primiani CT, Ren Z, Dumont TM, Brasiliense LBC et al (2017) Vessel perforation during stent retriever thrombectomy for acute ischemic stroke: technical details and clinical outcomes. J Neurointerv Surg. 9:922–928
Nguyen TN, Malisch T, Castonguay AC, Gupta R, Sun CH, Martin CO et al (2014) Balloon guide catheter improves revascularization and clinical outcomes with the solitaire device: analysis of the north american solitaire acute stroke registry. Stroke 45:141–145
Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P et al (2018) Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 378:11–21
Ouyang F, Chen Y, Zhao Y, Dang G, Liang J, Zeng J (2016) Selection of patients and anesthetic types for endovascular treatment in acute ischemic stroke: a meta-analysis of randomized controlled trials. PLoS One 11:e0151210
Park MS, Yoon W, Kim JT, Choi KH, Kang SH, Kim BC et al (2016a) Drip, ship, and on-demand endovascular therapy for acute ischemic stroke. PLoS One 11:e0150668
Park MS, Lee JS, Park TH, Cho YJ, Hong KS, Park JM et al (2016b) Characteristics of the drip-and-ship paradigm for patients with acute ischemic stroke in South Korea. J Stroke Cerebrovasc Dis 25:2678–2687
Perez de la Ossa N, Carrera D, Gorchs M, Querol M, Millan M, Gomis M et al (2014) Design and validation of a prehospital stroke scale to predict large arterial occlusion: the rapid arterial occlusion evaluation scale. Stroke 45:87–91
Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC et al (2015) 2015 American heart association/American stroke association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 46:3020–3035
Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K et al (2018) 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke 49:e46–e110
Ribo M, Boned S, Rubiera M, Tomasello A, Coscojuela P, Hernandez D et al (2017) Direct transfer to angiosuite to reduce door-to-puncture time in thrombectomy for acute stroke. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2017-013038.
Ribo M, Boned S, Rubiera M, Tomasello A, Coscojuela P, Hernandez D et al (2018) Direct transfer to angiosuite to reduce door-to-puncture time in thrombectomy for acute stroke. J Neurointerv Surg. 10:221–224
Saber H, Narayanan S, Palla M, Saver JL, Nogueira RG, Yoo AJ et al (2018) Mechanical thrombectomy for acute ischemic stroke with occlusion of the m2 segment of the middle cerebral artery: a meta-analysis. J Neurointerv Surg 10:620–624
Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM et al (2015) Stent-retriever thrombectomy after intravenous t-pa vs. T-pa alone in stroke. N Engl J Med 372:2285–2295
Saver JL, Goyal M, van der Lugt A, Menon BK, Majoie CB, Dippel DW et al (2016) Time to treatment with endovascular thrombectomy and outcomes from ischemic stroke: a meta-analysis. JAMA 316:1279–1288
Schonenberger S, Uhlmann L, Hacke W, Schieber S, Mundiyanapurath S, Purrucker JC et al (2016) Effect of conscious sedation vs general anesthesia on early neurological improvement among patients with ischemic stroke undergoing endovascular thrombectomy: a randomized clinical trial. JAMA 316:1986–1996
Simonsen CZ, Yoo AJ, Sorensen LH, Juul N, Johnsen SP, Andersen G et al (2018) Effect of general anesthesia and conscious sedation during endovascular therapy on infarct growth and clinical outcomes in acute ischemic stroke: a randomized clinical trial. JAMA Neurol 75:470–477
Taqui A, Cerejo R, Itrat A, Briggs FB, Reimer AP, Winners S et al (2017) Reduction in time to treatment in prehospital telemedicine evaluation and thrombolysis. Neurology 88:1305–1312
Turc G, Maier B, Naggara O, Seners P, Isabel C, Tisserand M et al (2016) Clinical scales do not reliably identify acute ischemic stroke patients with large-artery occlusion. Stroke 47:1466–1472
Uno J, Kameda K, Otsuji R, Ren N, Nagaoka S, Maeda K et al (2018) Mechanical thrombectomy for acute anterior cerebral artery occlusion. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.08.196
van der Bom IM, Mehra M, Walvick RP, Chueh JY, Gounis MJ (2012) Quantitative evaluation of c-arm ct cerebral blood volume in a canine model of ischemic stroke. AJNR Am J Neuroradiol 33:353–358
Velasco A, Buerke B, Stracke CP, Berkemeyer S, Mosimann PJ, Schwindt W et al (2016) Comparison of a balloon guide catheter and a non-balloon guide catheter for mechanical thrombectomy. Radiology 280:169–176
Wei D, Mascitelli JR, Nistal DA, Kellner CP, Fifi JT, Mocco JD et al (2017) The use and utility of aspiration thrombectomy in acute ischemic stroke: a systematic review and meta-analysis. AJNR Am J Neuroradiol 38:1978–1983
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL et al (2013) Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke 44:2650–2663
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Clarençon, F. et al. (2022). Acute Stroke: Management. In: Scaglione, M., Çalli, C., Muto, M., Wirth, S. (eds) Emergency Radiology of the Head and Spine. Medical Radiology(). Springer, Cham. https://doi.org/10.1007/978-3-030-91047-1_5
Download citation
DOI: https://doi.org/10.1007/978-3-030-91047-1_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-91046-4
Online ISBN: 978-3-030-91047-1
eBook Packages: MedicineMedicine (R0)