Abstract
High tibial osteotomy for correction of varus overload or malalignment should be considered in ACL deficiency, particularly when associated with medial compartment degeneration. This procedure, either in isolation or in concert with ACL reconstruction, can provide the patient with stability and improved joint mechanics, which can ameliorate the symptoms of unicompartmental gonarthrosis. This chapter discusses the role of high tibial osteotomy in the surgical management of ACL deficiency, and provides evidence-based support for its role in the management of these complex patients. The surgical technique, with pearls and pitfalls, is also described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anterior Cruciate Ligament
- Anterior Cruciate Ligament Reconstruction
- High Tibial Osteotomy
- Medial Compartment
- Tibial Slope
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Anterior cruciate ligament (ACL) deficiency in the setting of underlying lower extremity malalignment poses a special clinical challenge for surgeons because of the myriad considerations required to reconstruct a stable, durable, and functional knee. Many clinical and biomechanical studies have examined soft-tissue reconstructions for ACL deficiency, often without consideration for global coronal and/or sagittal plane deformities. Although their relative contributions continue to be debated, malalignment and ACL deficiency, both independently and in combination, can contribute to abnormal knee kinematics, which may hasten the development of osteoarthritis [7, 22, 29, 40]. Therefore, when considering a soft-tissue reconstruction, concomitant assessment of overall alignment is paramount to restoring a functional limb. Several authors have noted that soft-tissue procedures alone have a propensity for failure if concomitant malalignment, particularly varus, is not addressed [32, 34].
In patients with lower extremity varus malalignment and medial compartment gonarthrosis, high tibial osteotomy (HTO) for deformity correction has been associated with delayed progression of arthritis and improved clinical outcomes, especially in patients under 50 years of age [8, 16, 18, 31]. In the younger patient with ACL deficiency and malalignment, HTO in concert with ACL reconstruction (either concomitantly or staged) has been shown to improve both knee pain and instability [5, 10, 24, 33]. These procedures, performed in concert, can offset the repetitive abnormal stresses associated with soft-tissue reconstructions in isolation.
2 ACL Deficiency and Coronal Plane Malalignment
There is a direct relationship between varus malalignment and ACL tension [26, 27, 44]. In an examination of cadaveric knees loaded in increasing degrees of varus, van de Pol et al. [44] noted tensile forces in the ACL increased from 37.9 to 53.9N. With subsequent resection of the ACL, these same knees demonstrated increasing lateral opening and developed a visible varus thrust with increasing stresses.
Noyes et al. have previously described primary-, double-, and triple-varus knee syndromes [33]. Primary varus is defined by a shift of the weight-bearing axis stemming from medial compartment narrowing due to meniscal loss or chondral damage. With progressive medial compartment narrowing, a double varus condition develops as the posterolateral restraints become lax, leading to separation of the lateral tibiofemoral articulation. As the varus malalignment becomes more chronic, a hyperextension varus-recurvatum deformity develops. This constellation is referred to as triple varus. Although reconstruction of the ACL in a triple-varus knee will alleviate the anterior tibial translation, the underlying varus is not addressed, and consequently, stresses on the reconstructed ACL will be high. High tibial osteotomy in concert with ACL reconstruction can address the triple-varus deformity constellation and minimize stresses on the reconstructed ligament. Additionally, this hyperextension varus-recurvatum deformity can also be accentuated by concomitant posterior cruciate ligament (PCL) and posterolateral corner injuries, requiring special attention and consideration of high tibial osteotomy in the care of multiligamentous instability [23, 25].
3 ACL Deficiency and Sagittal Plane Malalignment
Sagittal plane malalignment, such as variations in posterior tibial slope, also has implications for instability in cruciate deficiency. After ACL reconstruction and simultaneous high tibial osteotomy, DeJour et al. [10] noted that postoperative tibial translation was associated with tibial slope. They found a significant positive correlation between anterior tibial translation and increasing posterior tibial slope. Conversely, decreased anterior tibial translation was found with lesser degrees of posterior tibial slope. Giffin et al. [15] further noted increased tibial translation with increasing posterior tibial slope but did not demonstrate altered cruciate kinematics. They concluded that inadvertent alterations of tibial slope during HTO would not alter knee stability or cruciate forces in situ. These findings have been supported by a recent cadaveric study suggesting that large variations of tibial slope can influence the resting position of the tibiofemoral articulation but do not appear to adversely influence the strain environment of the ACL [12].
The posterior tibial slope can be changed by distracting the osteotomy more posteriorly or anteriorly, which changes the resting position of the tibia with respect to the femur. The more posterior slope, the more anterior the resting position. Cruciate-intact knees, however, may be less susceptible to these alterations [12, 15]. It is unclear how alterations of posterior tibial slope affect the integrity of ACL reconstructions in cruciate deficiency, and further studies are necessary to delineate the true effect of sagittal plane adjustment on cruciate kinematics in high tibial osteotomy and ligament reconstruction.
4 Indications for Osteotomy
For more than half a century, high tibial osteotomy has been used for correction of lower extremity malalignment and alleviation of unilateral compartment gonarthrosis [19–21]. Coventry [8] initially defined indications for high tibial osteotomy and suggested that the optimal candidate was relatively active, with a stable knee, good range of motion, localized medial compartment osteoarthritis, and age less than 65 years. Due to concomitant surgical procedures, contemporary indications for HTO have expanded to encompass coronal and sagittal malalignment, anteroposterior and varus/valgus instability, and ligamentous deficiency [9, 10, 33, 36]. In patients with ACL insufficiency, symptomatic instability, and coronal and/or sagittal malalignment, the surgeon should consider correction of the underlying malalignment in addition to soft-tissue reconstruction [5, 9, 10, 14, 15, 24, 33]. Table 24.1 summarizes the author’s indications for osteotomy in the setting of instability.
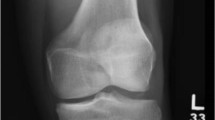
When a patient with ACL deficiency also presents with varus overload and medial compartment osteoarthritis, conservative care should be optimized, including activity modification, physical therapy, and unloader bracing. When arthritic symptoms include sequelae of prior meniscectomy, mechanical axis deviation into the medial compartment, and degenerative changes, high tibial osteotomy may be indicated (Fig. 24.1).
Younger, active patients with ACL insufficiency and symptomatic instability in the setting of underlying or secondary malalignment may be candidates for combined ACL/HTO procedures. Patients who have undergone previous ACL reconstruction, yet maintain an underlying malalignment, may continue to have symptoms of pain, instability, and/or laxity. Furthermore, in the setting of an unsuccessful soft-tissue reconstruction, the surgeon must consider failure to address an underlying malalignment at the index procedure as a contributing factor in graft failure [32, 34]. There is no specific threshold age limit for consideration of these procedures, and the correct approach must be tailored to the patient’s specific activity level and expectations.
5 Preoperative Evaluation
The preoperative evaluation should include a detailed medical history, physical examination, and appropriate imaging studies. The symptoms and age of the patient demand special attention. In general, the younger the patient, the more active they are likely to be and, therefore, the more likely to have true instability from the ACL deficiency. In the older patient with chronic ACL deficiency, symptoms may be more likely to originate from degenerative changes. Such patients may benefit from HTO in isolation, without the ligamentous reconstruction. Latterman and Jakob [24] suggested a threshold age of 40 years for this treatment, as many of their older patients did very well with HTO alone, but individual treatment should be tailored to individual patient needs. The younger patient with malalignment, ACL deficiency, and instability would likely benefit from both procedures. The ACL reconstruction and HTO can be done as either a single-stage or two-stage procedure. Several authors have described either one- or two-stage procedures with excellent results [2, 4, 5, 10, 24]. The decision to proceed with single-stage or two-stage surgery is therefore dependent on surgeon preference. However, it should be emphasized that correction of malalignment should be the minimum surgical treatment or as the initial procedure in a staged approach. The ACL reconstruction should be performed secondarily, either as the latter half of a combined procedure or as the second stage of a two-stage procedure. In the setting of malalignment, ACL reconstruction in isolation may lead to inferior results, failures, and progression of osteoarthritic change [32].
Bone quality must also be considered, as it may be challenging to obtain robust fixation in patients with osteoporosis and other diseases that affect bone density and quality. Consideration must also be given to other risk factors for failure, including smoking, corticosteroid dependency, chronic illness, immunosuppressants, etc.
Physical examination findings that may support an osteotomy include abnormal gait patterns, lateral thrust, limb alignment in stance, joint line tenderness, etc. Instability tests including Lachman maneuver, pivot shift, anterior drawer, and so forth should be documented. Presence of the double- or triple-varus constellations should be noted, if present.
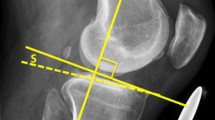
Radiographic evaluation begins with standard knee radiographs, including weight-bearing A/P, lateral, posteroanterior tunnel views in 30° of flexion, and merchant patellar views. The surgeon should assess the extent of knee arthrosis, fractures, retained hardware, etc. Lower extremity alignment should be assessed with weight-bearing long-leg (pelvis to ankle) anteroposterior views, which have been shown to be a simple, reliable, and accurate method for determining the degree of malalignment [17, 35, 38]. The HTO correction can also be calculated from these radiographs according to published techniques [11]. The mechanical and weight-bearing axes are estimated, and the correction to be made is then calculated by shifting this axis just lateral to the lateral tibial spine, at a point representing approximately 62 % of the joint surface as referenced from the medial joint line (Fig. 24.2). Care must be taken in the patient with a large, severe, or complex deformity. In such cases, the accurate correction may be difficult to determine. Mathematical modeling, although complex, can aid in the planning of such osteotomies [39].
A case of double varus left knee with a failure of previous ACL reconstruction. The patient has both preexisting varus alignment and lateral opening of the knee on a weight-bearing radiograph. (a) The right knee was used as a template for the correction of preexisting bony alignment. (b) The mechanical axis, shown as a short line, falls into the center of the medial compartment. The new weight-bearing lines are aligned at the point 62.5 % across the width of the tibial plateau, extending proximally to the center of the hip joint and distally to the center of the tibiotalar joint. The size of the opening wedge corresponds to the angle between the weight-bearing lines. (c) The medial opening wedge of the proximal tibia is simulated with restoration of the center of the knee joint (d) (Figure reproduced with permission from Phisitkul et al. [36])
Magnetic resonance imaging (MRI) is a useful adjunct in the evaluation of the patient with ACL deficiency and malalignment. MRI can provide the surgeon with useful information regarding subtle osseous abnormalities, soft-tissue injury, and meniscal and chondral pathology that may be less evident on plain radiographs.
6 Author’s Preferred Surgical Technique
The patient is met in the preoperative area and the operative site is marked. Preoperative prophylactic intravenous antibiotics are administered. After surrendering to anesthesia, the patient is positioned supine and a tourniquet is placed high on the thigh. The limb is then prepared and draped in standard fashion (Fig. 24.3).
We begin with low-pressure arthroscopy of the knee to assess the condition of the cartilage surfaces and integrity of the menisci. We do not perform any meniscal transplantation or cartilage resurfacing procedures at the time of this surgery. These procedures, if indicated, are performed in a staged manner at a later date, with the osteotomy being performed first. At the conclusion of arthroscopy, the extremity is exsanguinated, and the tourniquet is inflated for the balance of the osteotomy procedure.
A soft bump is positioned under the leg in order to hyperextend the knee and assist with closing the osteotomy anteriorly. This serves to decrease the tibial slope and therefore anterior tibial translation in the ACL-deficient knee.
A vertical incision is made halfway between the patellar ligament and the posterior border of the tibia, directly over the pes anserinus insertion. Dissection is carried down through skin and subcutaneous tissue to the sartorial fascia (Fig. 24.4). If a hamstring autograft is to be used for the ultimate ACL reconstruction, the gracilis and semitendinosus tendons are harvested at this time. Graft preparation is performed on the back table (Figs. 24.5 and 24.6).
Incision. A vertical incision is made halfway between the patellar ligament and the posterior border of the tibia, directly over the pes anserinus insertion. If a hamstring autograft is to be used for the ultimate ACL reconstruction, the gracilis and semitendinosus tendons are also harvested at this time
Subperiosteal elevation of the medial collateral ligament (MCL) is performed, and blunt retractors are placed anteriorly behind the patellar ligament and posteriorly in front of the hamstring tendons and superficial MCL.
We prefer the medial opening wedge osteotomy for several reasons. The medial opening wedge procedure avoids a secondary osteotomy of the proximal fibula with its concomitant risk of peroneal nerve and posterolateral corner injury [6, 23, 43]. This technique also allows correction in both the coronal and sagittal planes, as hinging through the intact proximal tibiofibular joint decreases the posterior tibial slope [1]. Furthermore, the medial opening wedge incision provides access to the hamstring tendons for autograft ACL reconstruction, as well as convenient positioning of the tibial tunnel.
To perform the medial wedge opening osteotomy, a guide wire is inserted into the proximal tibia from medial to lateral under fluoroscopic guidance. This wire is oriented obliquely from the superior aspect of the tibial tubercle to a point 1 cm below the lateral joint line at the far lateral tibial cortex (Figs. 24.7 and 24.8). This positioning allows the osteotomy to be proximal to the patellar ligament insertion on the tibia, yet remote enough from the joint to decrease the risk of intra-articular fracture. Furthermore, this allows the osteotomy to be in the metaphyseal region, which is favorable for healing.
The osteotomy is performed with an oscillating saw, oriented just distal to the guide wire to avoid intra-articular extension (Fig. 24.9). Shallow cuts are made with the saw, and the osteotomy is subsequently deepened with flexible and rigid osteotomes, again under fluoroscopic guidance (Figs. 24.10 and 24.11).
The osteotomy is then opened with a medial wedge to a depth predetermined from preoperative radiographic templating (Figs. 24.12 and 24.13). Femorotibial alignment is then estimated by intraoperative fluoroscopy using an extramedullary alignment guide. Caution must be exercised with these measurements, however, as supine non-weight-bearing estimation of the axis in obese patients or patients with sizable malalignment may not accurately reflect the true mechanical axis [37].
The posterior tibial slope is also assessed fluoroscopically and can be modified by distracting the osteotomy more anteriorly or posteriorly. If there is excessive anterior opening, a tibial tubercle osteotomy may be required to advance the tubercle to the same height as the osteotomy.
With the orientation of the osteotomy complete, an open wedge plating system (Arthrex, Naples, FL) is contoured to the bone and fixed proximally with 6.5-mm cancellous screws and distally with 4.5-mm cortical screws. Screw placement is confirmed with fluoroscopy (Figs. 24.14, 24.15, and 24.16). Corticocancellous allograft wedges (harvested from femoral head allograft) or synthetic allograft wedges are employed to fill the osteotomy site and achieve the desired position (Fig. 24.17).
Having completed the osteotomy, ACL reconstruction then ensues. The osteotomy is performed first to avoid the creation of stress risers in the ACL tunnels and to also avoid inadvertent disruption of the tunnel with the osteotomy. Arthroscopic ACL reconstruction is performed using standard techniques. We prefer to drill the tibial tunnel so that it exits just above the osteotomy site, anteromedially. The femoral tunnel is then drilled, and the ACL graft is passed (Figs. 24.18 and 24.19). We prefer extracortical button fixation for femoral fixation. The tibial side is secured with interference screw fixation above the osteotomy site, with secondary fixation below the osteotomy if desired/warranted (Figs. 24.20 and 24.21). The wounds are then closed in layers over a drain.
Tunnel preparation and graft fixation. The femoral and tibial tunnels are prepared for ACL reconstruction. The ACL graft is passed and secured with extracortical button fixation on the femoral side and with an interference screw on the tibial side, above the osteotomy site. The free end of the graft can be seen exiting below the osteotomy site
7 Postoperative Care
The majority of patients stay overnight for pain control, serial examinations for evaluation of compartment syndrome, and administration of prophylactic antibiotics. The knee is immobilized in a hinged knee brace. With the brace locked in extension, the patient is allowed toe-touch weight bearing using crutches or a walker for ambulatory assistance. While recumbent, knee range of motion is allowed through a 0–90° arc to decrease the incidence of postoperative stiffness. Sutures are removed within 2 weeks, and radiographs are obtained beginning at the 6-week postoperative appointment (Figs. 24.22 and 24.23). Once there is radiographic evidence of bony consolidation, the brace is discontinued. Full weight bearing, in concert with a formal physical therapy program for strengthening, is then initiated. Radiographs are repeated at the 10-week postoperative visit, and if osseous consolidation has been achieved, then sport-specific rehabilitation is initiated.
8 Complications
Surgical and postoperative complications affiliated with HTO include nonunion, hardware failure, fracture, infection, prominent/symptomatic hardware, peroneal nerve palsy, compartment syndrome, vascular injury, thromboembolic disease, and others. Intraoperative fracture of the proximal tibia is reported to be as high as 18 % in high tibial osteotomy [41]. Staying distal to the guide pin placed as described in our operative technique can minimize this complication. Instances of intra-articular fracture require anatomic reduction and rigid fixation. Nonunion is reported to range from 0.7 to 4.4 % [3, 41, 42]. Bone grafts, bone substitutes, and growth factors have been used as adjuncts to encourage consolidation at the osteotomy site. We routinely use corticocancellous femoral heal allograft.
The incidence of compartment syndrome in high tibial osteotomy is unknown, but cases have been reported in the literature [30, 45]. Marti and Jakob [28] describe elevated compartment pressures requiring fasciotomy following arthroscopic ACL reconstruction and concurrent high tibial osteotomy. When arthroscopy is employed, lower pump pressures and frequent compartment checks should be performed throughout the procedure. Many of the more common neurovascular injuries, particularly those involving the peroneal nerve, are minimized or obviated by the use of opening wedge osteotomies, which are less likely to result in such complications [13, 41, 43].
9 Summary
High tibial osteotomy for correction of varus overload or malalignment should be considered in ACL deficiency, particularly when associated with medial compartment degeneration. This procedure, either in isolation or in concert with ACL reconstruction can provide the patient with stability and improved joint mechanics, which can ameliorate the symptoms of unicompartmental gonarthrosis.
References
Amendola A, Rorabeck CH, et al. Total knee arthroplasty following high tibial osteotomy for osteoarthritis. J Arthroplasty. 1989;4(Suppl):S11–7.
Badhe NP, Forster IW. High tibial osteotomy in knee instability: the rationale of treatment and early results. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):38–43.
Bettin D, Karbowski A, et al. Time-dependent clinical and roentgenographical results of Coventry high tibial valgisation osteotomy. Arch Orthop Trauma Surg. 1998;117(1–2):53–7.
Bonin N, Ait Si Selmi T, et al. Anterior cruciate reconstruction combined with valgus upper tibial osteotomy: 12 years follow-up. Knee. 2004;11(6):431–7.
Boss A, Stutz G, et al. Anterior cruciate ligament reconstruction combined with valgus tibial osteotomy (combined procedure). Knee Surg Sports Traumatol Arthrosc. 1995;3(3):187–91.
Chun Y-M, Kim S-J, et al. Evaluation of the mechanical properties of posterolateral structures and supporting posterolateral instability of the knee. J Orthop Res. 2008;26(10):1371–6.
Clatworthy M, Amendola A. The anterior cruciate ligament and arthritis. Clin Sports Med. 1999;18(1):173–98, vii.
Coventry MB. Upper tibial osteotomy for osteoarthritis. J Bone Joint Surg Am. 1985;67(7):1136–40.
Dejour H, Bonnin M. Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg Br. 1994;76(5):745–9.
Dejour H, Neyret P, et al. Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop. 1994;299:220–8.
Dugdale TW, Noyes FR, et al. Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop. 1992;274:248–64.
Fening SD, Kovacic J, et al. The effects of modified posterior tibial slope on anterior cruciate ligament strain and knee kinematics: a human cadaveric study. J Knee Surg. 2008;21(3):205–11.
Georgoulis AD, Makris CA, et al. Nerve and vessel injuries during high tibial osteotomy combined with distal fibular osteotomy: a clinically relevant anatomic study. Knee Surg Sports Traumatol Arthrosc. 1999;7(1):15–9.
Giffin JR, Stabile KJ, et al. Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med. 2007;35(9):1443–9.
Giffin JR, Vogrin TM, et al. Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med. 2004;32(2):376–82.
Hernigou P, Medevielle D, et al. Proximal tibial osteotomy for osteoarthritis with varus deformity. A ten to thirteen-year follow-up study. J Bone Joint Surg Am. 1987;69(3):332–54.
Hinman RS, May RL, et al. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum. 2006;55(2):306–13.
Holden DL, James SL, et al. Proximal tibial osteotomy in patients who are fifty years old or less. A long-term follow-up study. J Bone Joint Surg Am. 1988;70(7):977–82.
Jackson J. Osteotomy for osteoarthritis of the knee. J Bone Joint Surg Am. 1958;43-B(4):746–51.
Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. Proc R Soc Med. 1960;53(10):888.
Jackson JP, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br. 1961;43-B:746–51.
Kessler MA, Behrend H, et al. Function, osteoarthritis and activity after ACL-rupture: 11 years follow-up results of conservative versus reconstructive treatment. Knee Surg Sports Traumatol Arthrosc. 2008;16(5):442–8.
Laprade RF, Engebretsen L, et al. The effect of a proximal tibial medial opening wedge osteotomy on posterolateral knee instability: a biomechanical study. Am J Sports Med. 2008;36(5):956–60.
Lattermann C, Jakob RP. High tibial osteotomy alone or combined with ligament reconstruction in anterior cruciate ligament-deficient knees. Knee Surg Sports Traumatol Arthrosc. 1996;4(1):32–8.
MacDonald P, Miniaci A, et al. A biomechanical analysis of joint contact forces in the posterior cruciate deficient knee. Knee Surg Sports Traumatol Arthrosc. 1996;3(4):252–5.
Markolf KL, Burchfield DM, et al. Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995;13(6):930–5.
Markolf KL, Gorek JF, et al. Direct measurement of resultant forces in the anterior cruciate ligament. An in vitro study performed with a new experimental technique. J Bone Joint Surg Am. 1990;72(4):557–67.
Marti CB, Jakob RP. Accumulation of irrigation fluid in the calf as a complication during high tibial osteotomy combined with simultaneous arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 1999;15(8):864–6.
McDaniel WJ, Dameron TB. The untreated anterior cruciate ligament rupture. Clin Orthop. 1983;172:158–63.
Miller BS, Downie B, et al. Complications after medial opening wedge high tibial osteotomy. Arthroscopy. 2009;25(6):639–46.
Naudie D, Bourne RB, et al. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to −22-year followup study. Clin Orthop. 1999;367:18–27.
Naudie DDR, Amendola A, et al. Opening wedge high tibial osteotomy for symptomatic hyperextension-varus thrust. Am J Sports Med. 2004;32(1):60–70.
Noyes FR, Barber-Westin SD, et al. High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med. 2000;28(3):282–96.
Noyes FR, Schipplein OD, et al. The anterior cruciate ligament-deficient knee with varus alignment. An analysis of gait adaptations and dynamic joint loadings. Am J Sports Med. 1992;20(6):707–16.
Odenbring S, Berggren AM, et al. Roentgenographic assessment of the hip-knee-ankle axis in medial gonarthrosis. A study of reproducibility. Clin Orthop. 1993;289:195–6.
Phisitkul P, Wolf BR, et al. Role of high tibial and distal femoral osteotomies in the treatment of lateral-posterolateral and medial instabilities of the knee. Sports Med Arthrosc. 2006;14(2):96–104.
Sabharwal S, Zhao C. Assessment of lower limb alignment: supine fluoroscopy compared with a standing full-length radiograph. J Bone Joint Surg. 2008;90(1):43–51.
Sabharwal S, Zhao C, et al. Computed radiographic measurement of limb-length discrepancy. Full-length standing anteroposterior radiograph compared with scanogram. J Bone Joint Surg Am. 2006;88(10):2243–51.
Sangeorzan BP, Judd RP, et al. Mathematical analysis of single-cut osteotomy for complex long bone deformity. J Biomech. 1989;22(11–12):1271–8.
Sharma L, Song J, et al. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–95.
Spahn G. Complications in high tibial (medial opening wedge) osteotomy. Arch Orthop Trauma Surg. 2004;124(10):649–53.
Tjörnstrand B, Hagstedt B, et al. Results of surgical treatment for non-union after high tibial osteotomy in osteoarthritis of the knee. J Bone Joint Surg Am. 1978;60(7):973–7.
Tunggal JAW, Higgins GA, et al. Complications of closing wedge high tibial osteotomy. Int Orthop. 2010;34(2):255–61.
van de Pol GJ, Arnold MP, et al. Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med. 2009;37(3):481–7.
Wildner M, Peters A, et al. Complications of high tibial osteotomy and internal fixation with staples. Arch Orthop Trauma Surg. 1992;111(4):210–2.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag London
About this chapter
Cite this chapter
Sybrowsky, C.L., Amendola, A. (2013). The Role of High Tibial Osteotomy in the ACL-Deficient Knee. In: Sanchis-Alfonso, V., Monllau, J. (eds) The ACL-Deficient Knee. Springer, London. https://doi.org/10.1007/978-1-4471-4270-6_24
Download citation
DOI: https://doi.org/10.1007/978-1-4471-4270-6_24
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-4269-0
Online ISBN: 978-1-4471-4270-6
eBook Packages: MedicineMedicine (R0)