Abstract
With increasing life expectancy, a major concern is whether the years gained are spent in good or in poor health. Disability has become the main indicator of health at older ages. Important questions are how it increases with age, what factors increase the chance of disability and what consequences disability has. In this chapter, evidence is provided based on results from the Longitudinal Aging Study Amsterdam (LASA), a study on determinants and consequences of changes in daily functioning in a representative sample of ages 55 and over in the Netherlands. In this chapter, the focus is on changes in physical functioning. From longitudinal data, it is observed that many elders experience function loss, especially at higher ages. A host of factors are associated with function loss, such as chronic diseases, cognitive decline, depressive complaints, socio-economic status and lifestyle. A few of these factors are causal, others are characteristics of groups with raised chances of function loss. From trend analyses, it is apparent that the prevalence of functional limitations is not fixed, but varies over time. The LASA study shows that this prevalence is increasing. In light of the absolute and relative rise of the number of older people in the population, it is of great importance to realise a lower prevalence of function loss and a delay of function loss to older ages. Based on the findings presented, some suggestions for this are given. Also, some directions for future research are described.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The steady increase in life expectancy in most European countries implies that a growing number of citizens reaches higher ages increasingly. For decades now, this development has been a cause for concern to policy makers and the general public because of the expected increase in costs of health and social care. This concern has given rise to the need for population-based data to monitor health and daily functioning of older persons, and to obtain insight into trajectories leading to the utilisation of care services . For projections of health and social care costs, it is furthermore of interest to monitor trends in the prevalence of ill-health and disability at the population level to see how this changes over time.
The concept of disability , in this chapter, is defined as a consequence of ill-health or illness, generally chronic diseases. Disability is established as a powerful indicator of health status at older age (Guralnik et al. 1996). Some theoretical models have been developed with the aim of conceptually linking ill-health to disability, including the model adopted by the World Health Organisation (WHO 2002), which defines functional ability as encompassing all body functions, tasks, or actions, and disability as including impairment, limited capacity or restricted performance of activities. Measurement of disability usually entails self-reports of difficulty or need of help in performing everyday tasks needed for independent living. The term disability is often used to include mobility impairment, which is considered to precede disability in activities of daily living (Verbrugge and Jette 1994). In a growing number of studies, performance-based tests are used to capture early stages of disability (Guralnik et al. 1994).
If prevalences of ill-health and disability rise or fall, factors responsible for these changes need to be traced. Thus, determinants of the onset and course of disability, as well as consequences of disability , need to be studied using longitudinal data. This chapter reviews empirical data on trends in the prevalence of disability , on changes in functional ability and on determinants and consequences of such changes.
Availability of Data
Comparison of morbidity and disability across European countries is difficult, because each country shapes its health policy using its own concepts and measurement of health indicators . The first international studies started in the 1960s and 1970s in a few European countries, but were limited in scope or included only a selection of the older population (Appels et al. 1996; Jylhä et al. 1998; Knoops et al. 2004).
Since the 1980s, epidemiological studies of health and functioning in older age have boomed. Although the initial focus of epidemiological studies was mainly on ageing-related chronic diseases, their focus shifted to independence in daily functioning as this was increasingly considered to be an essential aspect of healthy ageing. Several of these studies, moreover, were interdisciplinary in scope, because there was an understanding that with ageing, physical, mental and social aspects of functioning are closely related. Most were confined to smaller geographic areas such as one city or county.
Only in the 1990s, a number of cross-national surveys became available that used common instruments and sampling methods. The best known is the European Community Household Panel survey, conducted in the non-institutionalised population in 13 countries. For the assessment of health in older age, however, this survey is less suitable, because in many countries a sizeable proportion of older persons live in institutions.
In the early 1990s, in various countries across Europe , longitudinal studies on ageing were started that were in part or fully funded by national governments. A decade later, the European Union started to fund consortia that performed cross-national longitudinal studies, either making use of existing cohort studies, or setting up identical data collection in a number of countries (e.g. Minicuci et al. 2003; Börsch-Supan et al. 2005). In the Netherlands, the Ministry of Welfare, Health and Culture in 1991 initiated a nation-wide, interdisciplinary, longitudinal study to monitor changes in daily functioning in the older Dutch population, the Longitudinal Aging Study Amsterdam (LASA), with data collection cycles every 3 years. It includes more than 4,000 participants aged 55–102 years (Huisman et al. 2011). This study now spans almost 20 years and is one of the longest running nationally representative studies in Europe . This chapter will draw predominantly on findings from this study.
Daily Functioning: Morbidity and Disability
Daily functioning in ageing in the first place is dependent on the presence of chronic diseases, also termed morbidity . Although their prevalences vary across European countries, there is a fair agreement in the top five of chronic conditions. First in rank are musculoskeletal diseases, including arthritis and osteo-porosis , with a prevalence ranging from 40 % to 70 %, depending on the country. Heart diseases, including myocardial infarction, angina pectoris, heart failure and peripheral artery disease, rank second. Respiratory diseases, including chronic bronchitis, emphysema and asthma , rank next. Diabetes ranks fourth, and stroke and cancer share the fifth rank with prevalences from 5 % to 11 % (Minicuci et al. 2003).
Although morbidity itself may not profoundly affect daily functioning, it may have consequences in terms of functional ability and ultimately, disability (WHO 2002). Severity levels of disability are distinguished , depending on the tasks of daily living in which difficulty is present. More complex activities such as shopping, preparing a meal and doing housework are termed instrumental activities of daily living (IADLs), and disability in IADLs is considered mild disability. More basic, and at the same time more obligatory activities, such as bathing, dressing and toileting, are termed activities of daily living (ADLs), and disability in ADLs is considered severe disability. The latter are less likely to be affected by socio-cultural factors than the former. Nevertheless, a surprising variety is observed in prevalence of ADL disability across European countries, ranging from 6 to 35 %. ADL disability turns out to have highest prevalence in Italy and Spain, and lowest in Finland, suggesting a north-south gradient (Pluijm et al. 2005; Van den Brink et al. 2003).
Trends in the Prevalence of Morbidity and Disability
In all western countries, there is ample evidence of an increase in the age-specific prevalence of chronic diseases in the past 20 years (Freedman and Martin 2000; Fleming et al. 2005). This increase may partly be explained by earlier diagnosis and improved medical treatment. As a result, persons with a chronic disease may live longer with their disease, thus raising the prevalence of chronic diseases.
For the Netherlands, based on data from LASA, Fig. 8.1 shows changes in the prevalence of several common chronic diseases among 65–85-year olds during the period 1992–2009. In general, a rise in the prevalence of diseases is observed. Detailed calculations show that these increases are greater than 10 % for heart diseases, diabetes , cancer and joint disorders. Thus, also for the Dutch older population, a substantial increase in the prevalence of chronic diseases is seen.
The prevalence of disability may also change over time as it is linked to chronic diseases, but the trend in disability prevalence may not correspond to the trend in chronic disease prevalence. Indeed, according to the dynamic equilibrium theory (Manton 1982), morbidity or mild disability may show a trend that is different from severe disability. Following the course of a chronic disease, we will first encounter mild disability, and later on, severe disability. This would mean that the prevalence of disability rises parallel to the development of the disease. Of course, improvements in the treatment of chronic diseases can delay the onset of disability, but so far no cure exists for the major chronic conditions. Thus, unless improvement in the treatment of diseases can delay the onset of disability enough to compensate for the increase in disease prevalence, it is likely that the prevalence of disability increases along with the growing prevalence of chronic diseases. However, persons with a chronic disease may have fewer disabilities because their disease is diagnosed at an earlier stage or because improved medical care and increased use of assistive devices have reduced its deleterious effects (Wolf et al. 2005). Several studies, including European ones, showed that specific chronic diseases have become less disabling during the last decades of the twentieth century (Deeg et al. 1994; Puts et al. 2008; Robine et al. 1998). However, in the most recent decade, the association between chronic diseases and disability did not show significant changes (Hoeymans et al. 2012).
There is a host of recent evidence on population trends in disability showing different results across countries and periods (Robine and Michel 2004). Most studies show a decline in the prevalence of disability since the 1980s (Freedman et al. 2004), the majority of which have been conducted in the United States. In European countries, reported trends include both decreases and increases in disability (Parker et al. 2005; Sagardui-Villamor et al. 2005). In a recent report or the Organisation for Economic Cooperation and Development (OECD) , in many western countries an increase in the prevalence of severe disability was observed, but equally in many western countries a decline in this prevalence was seen (Lafortune et al. 2007).
Notably, disability trends may differ across gender and socio-economic status . Although women have been found to have more disability than men in several countries, the trend in disability in women was not different from that in men (Fors et al. 2008). In contrast, disability in population groups with higher education is higher than in groups with lower education, but prevalence of disability in the higher educated tends to be declining, whereas this is not always the case in population groups with lower education (Crimmins and Saito 2001).
Several reports based on LASA data show that the prevalence of self-reported disability in the Netherlands has increased since 1992. This increase is seen in older ages (65 and over; Portrait et al. 2010; Sonnenberg et al. 2008) as well as in late midlife (ages 55–64; Hoogendijk et al. 2008). The increase in the prevalence of disability is observed only in mild, but not in severe disability (Fig. 8.2a, b). Whereas in the age group of 65–84 years the prevalence of mild disability rose from 21 % in 1992 to 32 % in 2009, the prevalence of severe disability showed a slight decline of 3 % points (Deeg and Broese van Groenou 2007; Galenkamp et al. in press). Also, in the Netherlands, trends differ across sub-groups of the older population. A more unfavourable trend is seen in women as compared with men, and in those with a low education level as compared with the higher educated.
The increase in the prevalence of mild disability may be partly attributed to the increase in the prevalence of chronic diseases, as described, but also to a worsening of lifestyle factors such as physical activity, nutrition and alcohol use (Visser et al. 2005), and to psychosocial factors such as a lower sense of mastery (Deeg and Huisman 2010). These are individual characteristics, which are essentially amenable for intervention. These are discussed in detail in the paragraph on longitudinal change. Other factors responsible for changes in the prevalence of disability are less easily influenced. These may be demographic factors related to changes in the composition of the population, such as the relatively fast increase in the proportion of the oldest-old (Robine and Michel 2004).
Changes in prevalence may also stem from societal developments that are occurring in the period monitored (period factors), or from characteristics of the particular generations or cohorts that constitute the older population, which can be traced to factors that influenced how they grew up (cohort factors). Portrait et al. (2010) examined a large number of period and cohort factors, such as the business cycle during the childhood of current older generations (an example of a cohort factor) or changes in the availability of care during the study period (an example of a period factor). The authors found no explanatory value for cohort factors, but did find one clear period factor: the decrease in the number of hospital days was associated with the increase in the prevalence of disability . During the study period 1992–1999, the hospital length of stay had fallen steadily for a number of reasons such as greater efficiency. It appears that policy-driven changes in care may affect daily functioning of older people.
Longitudinal Change in Functional Ability
For a better understanding of factors influencing trends in the prevalence of disability, we now turn to factors determining the onset and course of disability in individuals as they age. When following the group of older people who have no difficulty in any of six daily activities at baseline, we can examine which percentage develops disability (i.e. incidence of disability). In the course of 6 years, this incidence amounted to 45 % for a cohort aged 58–88 years (Broese van Groenou et al. 2006). Of course, the incidence rose with age, and amounted to 68 % in the age group of 75–88 years. The incidence showed differences across gender (men: 40 %, women: 52 %) and even more so across levels of education (high: 31 %, low: 56 %).
Recovery from disability was observed as well, but to a much lesser extent. Among older people with disability at baseline, 20 % did not report disability at 6 years follow-up. This percentage decreased with age and was only 10 % in the age group of 75–88 years. Recovery did not show significant differences across gender and level of education.
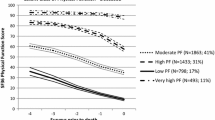
The reported incidence should be regarded with caution, as it may not be very relevant when an older person develops difficulty with only one activity. Hence, it may be more important to examine a change in functional ability that can be defined as relevant, regardless of the level of disability at baseline. This was done by Puts et al. (2005), who reported a relevant function loss in self-reported and performance-based physical functioning of 25 and 23 %, respectively, across 3 years. Again, in women and in the lower educated a greater functional loss was observed than in men and in the higher educated. Moreover, regardless of age or gender, older people living alone showed more functional loss than older people living with their partner: 30 and 20 %, respectively (Puts et al. 2005).
Predictors of Change in Functional Ability
Chronically ill older people were found to have a 3.5 times larger risk of onset of disability than older people without chronic diseases. This risk rate was found to rise to even 4.6 when chronically ill older people were diagnosed with an additional disease (Broese van Groenou et al. 2006). Multi-morbidity, the co-occurrence of two or more chronic diseases, is present in as many as two-thirds in the age group of 65 and over (Schram et al. 2008). In a detailed study of pairs of co-occurring diseases, an additional disease was shown to have an extra effect on function loss only when it affects a body system that is different than the one affected by the first disease (Kriegsman et al. 2004). An example is the onset of osteo-arthritis (affecting the musculoskeletal system) in an individual who already is suffering from heart disease (affecting the cardiovascular system). Cognitive decline is also an important cause of function loss and disability onset in older adults. It was found that older persons declining in cognitive function had a twofold increased risk of function loss (Comijs et al. 2005). Thus, regardless of somatic morbidity, cognitive impairment contributes to complexity of health problems and ensuing need of care.
Frailty is a concept increasingly used by geriatricians and gerontologists, and is defined as the multi-system decline as a consequence of ageing-related changes in the neuromuscular, endocrine and immune systems (Fried et al. 2001). Frailty can be conceived as a measure of taxability and recovery potential. Fried defined it using five indicators: weight loss, weakness, slowness, lack of energy and inactivity. There is, however, a debate whether the concept of frailty should be narrowly defined to include only physiological aspects, or if it should be broader defined to include psychological aspects as well (Morley et al. 2002). In a series of studies based on data from LASA, we adopted the broad concept and included nine indicators: low weight, poor lung function (as a measure of weakness), physical inactivity, cognitive impairment , poor vision, poor hearing, incontinence, depressive symptoms (including lack of energy and slowness) and a poor sense of mastery. Subjects were defined as frail when they scored poorly on three of the nine indicators. Puts et al. (2005) showed that frail subjects ran a more than twofold risk of function loss more than 3 years, as compared with non-frail subjects. This increased risk proved independent of age, sex, education and especially of the presence of chronic diseases. Moreover, it concerned both self-reported and performance-based functional decline.
The predictive ability of frailty for function loss emphasises that maintenance or decline in functional ability depends on multiple factors. Some of these factors may be causal, such as a decreased lung function or the onset of a chronic disease, whereas other factors may accelerate or slow down the rate of function loss. Van Gool et al. (2005) reported that depressive symptoms—one of the frailty indicators commonly used—are an example of the latter: older people with depressive symptoms showed accelerated functional decline. Geerlings et al. (2001) demonstrated that the influence of depression was especially strong for decline in functioning in daily activities, and less strong for decline in mobility, which generally precedes onset of disability . It is conceivable that depression is a causal factor in functional decline through its underlying pathology of diminished interest and motivation.
In addition to chronic diseases, causal factors for functional decline are usually sought in physiological parameters. Various so-called biomarkers are independent determinants of decline in functional ability . Markers of inflammation (interleukin-6, C-reactive protein, and alpha1-antichymotrypsin) were shown to be predictive of function loss (Schaap et al. 2006). As these markers are implicated in the pathogenesis of a number of chronic diseases, they are indicative of sub-clinical disease. Raised levels of inflammation furthermore decrease the level of serum albumin and total cholesterol , which biomarkers can be easily determined in general practice. Serum albumin is involved in the transport of various substances through the bloodstream, and cholesterol has a role in the production of hormones and in cell membrane permeability. Low levels of both markers proved predictive of functional decline, especially in combination with each other (Schalk et al. 2004). Both albumin and total cholesterol are synthesised in the liver, and it is suggested that an overall deterioration in the liver function might be associated with a poor health status, and might therefore contribute to functional decline. With proper nutrition, adequate levels of albumin and cholesterol can be maintained. Other nutrition-related biomarkers such as vitamin D are more difficult and thus more expensive to assess, but also were found to predict decline in functioning (Wicherts et al. 2007). Vitamin D deficiency is common among older people and can cause bone loss and muscle weakness. Genetic make-up was found to be of additional importance: the e4 variant of the apolipoprotein-E gene (ApoE) , well-known for its predictive ability for cognitive decline and dementia , was also found to be predictive of physical decline, regardless of cognitive functioning (Henderson et al. 1995; Melzer et al. 2005). ApoE has a role in the clearance of lipoproteins such as cholesterol . The predictive ability of biomarkers appears to be stronger for objective , performance-based mobility impairment than for disability in daily activities, i.e. for the earlier stages of disability.
From the social factors that have been examined in relation to functional decline, socio-economic status plays an important role. Both a low educational level and a low income increase the risk of incident disability in 3 years time (Broese van Groenou et al. 2003; Huisman et al. 2005). The chance of recovery, however, proved not to be influenced by socio-economic status. In searching for explanations for socio-economic differences in functional decline, Koster et al. (2006) found different explanatory factors in subjects younger and older than 70 years. In the younger age group, lifestyle proved to be of predominant importance, whereas in the older age group lifestyle appeared to have no explanatory value. In contrast, psychosocial factors such as a low sense of mastery and lack of social engagement proved to contribute to the explanation of socio-economic differences in physical function loss in the older age group. In particular in men, a low sense of self-efficacy was shown to be associated with functional decline (Cooper et al. 2011).
Of lifestyle factors, especially physical inactivity and poor nutrition resulting in obesity were important predictors of function loss. Smoking and excessive alcohol use did not play a significant role. It was noted that physical inactivity was an equally important predictor of functional decline in chronically ill and in healthy older adults (Visser et al. 2002). Moreover, not only current intensity of physical activity, but also physical activity intensity during young adulthood proved to be predictive of functional decline in later life (Pluijm et al. 2007). A similar life course effect was found for body weight: obesity at middle age was equally predictive of functional decline in later life as obesity in late life itself.
In addition to the physical and psychosocial factors already discussed, one LASA-based study showed that lack of social support was predictive of function loss (Bisschop et al. 2003). Social support was detailed as partner support and support by other relatives and by non-kin. If present, the partner is generally the most important source of support, so that partner support would be expected to protect against function loss. However, partner support appeared to be protective only in those older people who did not yet have a chronic disease at baseline, i.e. in the case of first-onset disease and disability. In contrast, those who already had chronic diseases at baseline benefited from contacts with daughters and non-kin in terms of better maintenance of functioning.
Consequences of Changes in Functional Ability
Decline in functional ability may have a range of adverse consequences . It means having more difficulty moving about, moving more slowly and being less able to compensate in unexpected circumstances. The risk of fall accidents is therefore strongly increased in the presence of function loss (Stel et al. 2004; Pluijm et al. 2006). In addition, function loss may lead to decreased self-rated health, more psychological distress and loneliness (Dykstra et al. 2005; Jonker et al. 2008; van de Kamp et al. 2008). Moreover, in spouses one partner’s function loss increases the feelings of loneliness in the other partner (Korporaal et al. 2008). Longitudinal analyses showed that physical function loss increases the probability of chronic depression (Beekman et al. 2002; Geerlings et al. 2000). Depressive symptoms proved to decrease, however, when older people who had experienced function loss were admitted to a care institution (Thomése and Broese van Groenou 2006). Physical function loss also affects social functioning: social networks become smaller, disabled older adults receive more instrumental support but provide less support to others and participation in social activities decreases (Van Tilburg and Broese van Groenou 2002; Aartsen et al. 2004; Broese van Groenou and Deeg 2006). Especially, sport activities were reported to decline in the face of function loss.
Considering the effects of function loss on the utilisation of health and social services, a distinction can be made between acute care, i.e. out-patient care and hospital admission, and long-term care, i.e. informal or formal care in the home and institutionalised care. Although function loss is associated with the use of acute care (Pot et al. 2009), this association is temporary in many cases as the aim of hospital care is to treat the health condition, and recovery is mostly achieved. However, the use of long-term care is often permanent, so that when people start using some type of long-term care, we can speak of a ‘transition’ to this type of care.
In older people who in a 3-year period experienced a first onset of function loss, 17 % made a transition to informal care, 5 % to subsidised professional home care, 9 % contracted home help paid for out-of-the-pocket and 2 % were admitted to a care institution (Geerlings et al. 2004, 2005). It was thus demonstrated that at first onset of function loss, older people generally look for care in their own informal network or pay for help out of their pockets, and only a small minority look for government-provided care. A different picture arises for older people who have experienced function loss for a longer period of time. Among them, 25 % made a transition to informal care, 15 % to subsidised professional home care, 11 % contracted home help paid for out-of-the-pocket and 6 % were admitted to a care institution. At this stage, informal care is still the type of care used most often. However, subsidised professional home care takes a second place, while the transition to a care institution is more often made than among those with a recent onset of function loss.
An ultimate consequence of decline in functional ability is mortality . Disability, in particular performance-based functional impairment, is a powerful predictor of mortality (Smits et al. 1999; Deeg and Kriegsman 2003). However, not all older people experience a similar decline in functioning prior to death (Deeg 2005). Klinkenberg (2004) showed that in the last phase of life of older persons, four different trajectories can be distinguished. Nineteen per cent died without experiencing any disability and 26 % experienced disability only in the last week before death. A gradual, protracted decline was experienced by another 24 %. The largest group, 31 %, experienced disability at the severest level measured already more than 3 months before death. This group was on average older, had a larger share of women, and was more often institutionalised than the other groups. Moreover, this group relatively often had suffered a stroke or had osteo-arthritis , and more often was cognitively impaired. Thus, this high-cost group with severe, long-standing disability was characterised by notoriously disabling chronic conditions.
Conclusions
In this overview of findings concerning changes in functional ability in the older population over time and in individuals as they age, functional ability was shown to be influenced by and to have influence on many factors, from the micro to the macro level. From the data on trends in the prevalence of disability , it can be concluded that the extent of disability in the older population is not a fixed fact, but changes over time. Similar to several other studies in Europe , the LASA study indicates that the prevalence of mild disability increases over time , whereas the prevalence of severe disability stays the same or slightly decreases. These trends are not observed in all European countries, as recent data show that, for example, in Norway, mild disability decreased in prevalence, and in France, severe but not mild disability showed increasing prevalences (Moe and Hagen 2011; Cambois et al. 2008). Moreover, in Sweden a reversal from a positive to a negative trend in the prevalence of mobility disability was seen in the late 1990s (Parker et al. 2008). To explain such discrepancies, cross-national research is needed with exactly the same measures of disability as well as of potential explanatory factors. Although such studies now exist, they are relatively recent and cannot yet address time trends over a period of sufficient length.
From the longitudinal findings, it can be concluded that a sizeable proportion of the older population experiences function loss, especially at higher ages. Several factors, such as a decreased lung function, may be considered as causal factors. Other factors, such as depressive symptoms or a low level of education, may be regarded as factors accelerating function loss. This accelerating effect may be due to an unhealthy lifestyle, for example, malnutrition or non-compliance with treatment regimens, such as intake of medications that are prescribed to counteract the consequences of a disease. Regarding depression , it is, nevertheless, conceivable that this is a causal factor in functional decline through underlying pathology. In either case, the findings emphasise that depressed older adults and older adults with a low level of education are risk groups with increased probability of function loss.
In light of the absolute and relative increase of older people in the populations of European countries, it is paramount to prevent onset and further decline of function loss, or at least to postpone these to older ages than the ages at which they now occur. To this end, causal factors such as lifestyle , chronic diseases or biomarkers can be targeted. Sufficient physical activity is a likely candidate to postpone function loss, especially in chronically ill older people. Also, better disease management is highly likely to postpone functional decline. Several biomarkers found to predict function loss are indicative of undernutrition. Thus, the nutritional status of older people needs due attention. However, it is at least as productive to identify groups of older people with increased risk of function loss. Improvement of the recognition of depression in older people is an example. Finally, helping older people to improve their sense of mastery or to maintain a social network of sufficient diversity are other interventions highly likely to have a beneficial effect on their level of daily functioning.
References
Aartsen, M. J., Tilburg, T. G. van, Smits, C. H. M., & Knipscheer, C. P. M. (2004). A longitudinal study on the impact of physical and cognitive decline on the personal network in old age. Journal of Social and Personal Relationships, 21, 249–266.
Appels, A., Bosma, H., Grabuskas, V., Gostautas, A., & Sturmans, F. (1996). Self-rated health and mortality in a Lithuanian and a Dutch population. Social Science and Medicine, 42, 681–689.
Beekman, A. T. F., Geerlings, S. W., Deeg, D. J. H., Smit, J. H., Schoevers, R. A., De Beurs, E., Braam, A. W., Penninx, B. W. J. H., & Van Tilburg, W. (2002). The natural history of late-life depression: A 6-year prospective study in the community. Archives of General Psychiatry, 59, 605–611.
Bisschop, M. I., Kriegsman, D. M. W., Deeg, D. J. H., Tilburg, T. G. van, & Penninx, B. W. J. H. (2003). The influence of differing social ties on decline in physical functioning among older people with and without chronic diseases: The longitudinal aging study Amsterdam. Aging Clinical and Experimental Research, 2003, 15, 164–173.
Börsch-Supan, A., Hank, K., & Jürges, H. (2005). A new comprehensive and international view on ageing: Introducing the ‘Survey of health, ageing and retirement in Europe’. European Journal of Ageing, 2(4), 245–253.
Broese van Groenou, M. I., Penninx, B. W. J. H., & Deeg, D. J. H. (2003). Socio-economic inequalities in health decline and mortality in an older population. Aging Clinical and Experimental Research, 15, 174–183.
Broese van Groenou, M., & Deeg, D. (2006). Veranderingen in sociale participatie. Hoofdstuk 10. In De Boer, A. (Ed.), Rapportage Ouderen 2006; veranderingen in de leefsituatie en de levensloop [Report on the Elderly 2006; Changes in living conditions and the life course] (pp. 215–238). The Hague: Social and Cutural Planning Bureau.
Broese van Groenou, M., Deeg, D., & de Boer, A. (2006). Veranderingen in de levensloop. Hoofdstuk 8. In De Boer, A. (Ed.), Rapportage Ouderen 2006; veranderingen in de leefsituatie en de levensloop [Report on the Elderly 2006; Changes in living conditions and the life course] (pp. 167–193). The Hague: Social and Cutural Planning Bureau.
Cambois, E., Clavel, A., Romieu, I., & Robine, J.-M. (2008). Trends in disability-free life expectancy at age 65 in France: Consistent and diverging patterns according to the underlying disability measure. European Journal of Ageing, 5, 287–298.
Comijs, H. C., Dik, M. G., Aartsen, M. J., Deeg, D. J. H., & Jonker, C. (2005). The impact of change in cognitive functioning and cognitive decline on disability, well-being and utilization of health care services in older persons. Results of the longitudinal aging study Amsterdam. Dementia and Geriatric Cognitive Disorders, 19, 316–323.
Cooper, R., Huisman, M., Kuh, D., & Deeg, D. J. H. (2011). Do positive psychological characteristics modify the associations of physical performance with functional decline and institutionalization? Findings from the longitudinal aging study Amsterdam. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 66(4), 468–477.
Crimmins, E. M., & Saito, Y. (2001). Trends in healthy life expectancy in the United States, 1970–1990: Gender, racial, and educational differences. Social Science and Medicine, 52, 1629–1641.
Deeg, D. J. H. (2005). Longitudinal characterization of course types of functional limitations. Disability and Rehabilitation, 27, 253–261.
Deeg, D. J. H., & Kriegsman, D. M. W. (2003). Concepts of self-rated health: Specifying the gender difference in mortality risk. The Gerontologist, 43, 376–386.
Deeg, D. J. H., & Broese van Groenou, M. I. (2007). Health services use by older peolpe after discharge from hospital: Developments in 1992–2002. Tijdschrift voor Gezondheidswetenschappen (TSG) 85, 174–182. (In Dutch, abstract in English).
Deeg, D. J. H., Huisman, M. (2010). Cohort differences in 3-year adaptation to health problems among Dutch middle-aged, 1992–1995 and 2002–2005. European Journal of Ageing, 7, 157–165.
Deeg, D. J. H., Kriegsman, D. M. W., & van Zonneveld, R. J. (1994). Prevalence of four chronic diseases and their impact on health in older persons in the Netherlands between 1956–1993. Tijdschr Soc Gezonheidsz, 72, 434–41 (In Dutch, abstract in English).
Dykstra, P. A., Van Tilburg, T. G., & Gierveld, J. D. (2005). Changes in older adult loneliness—Results from a seven-year longitudinal study. Research on Aging, 27, 725–747.
Fleming, D. M., Cross, K. W., & Barley, M. A. (2005). Recent changes in the prevalence of diseases presenting for health care. The British Journal of General Practice, 55, 589–595.
Fors, S., Lennartsson, C., & Lundberg, O. (2008). Health inequalities among older adults in Sweden 1991–2002. European Journal of Public Health, 18(2):138–43.
Freedman, V. A., & Martin, L. G. (2000). Contribution of chronic conditions to aggregate changes in old-age functioning. American Journal of Public Health, 90, 1755–1760.
Freedman, V. A., Crimmins, E., Schoeni, R. F. et al (2004). Resolving inconsistencies in trends in old-age disability: Report from a technical working group. Demography, 41, 417–441.
Fried, L. P., Tangen, C. M., Walston, J., Newman, A. B., Hirsch, C., Gottdiener, J. et al (2001). Frailty in older adults: Evidence for a phenotype. The Journal of Gerontology: Medical Sciences, 56A, M146–M156.
Galenkamp, H., Braam, A. W., Huisman, M., Deeg, D. J. H. (2012). Seventeen-year time trend in poor self-rated health in older adults: changing contributions of chronic diseases and disability. European Journal of Public Health, In press:doi:10.1093/eurpub/cks031.
Geerlings, S. W., Beekman, A. T. F., Deeg, D. J. H., & Van Tilburg, W. (2000). Physical health and the onset and persistence of depression in older adults: An eight-wave prospective community based study. Psychological Medicine, 30, 369–380.
Geerlings, S. W., Beekman, A. T. F., Deeg, D. J. H., Twisk, J. W. R., & Van Tilburg, W. (2001). The longitudinal effect of depression on functional limitations and disability in older adults: An eight-wave prospective community-based study. Psychological Medicine, 31, 1361–1371.
Geerlings, S., Broese van Groenou, M., & Deeg, D. (2004). Determinanten van veranderingen in zorggebruik [Determinants of changes in the use of care]. In De Klerk, M. M. Y. (Ed.), Zorg en wonen voor kwetsbare ouderen. Rapportage ouderen 2004 [Care and residence of frail older persons. Report on older persons 2004] (pp. 81–111). Den Haag: Sociaal en Cultureel Planbureau.
Geerlings, S. W., Pot, A. M., Twisk, J. W. R., Deeg, & D. J. H. (2005). Predicting transitions in the use of informal and professional care by older adults. Ageing and Society, 25, 111–130.
Guralnik, J. M., Simonsick, E. M., Ferrucci, L., Glynn, R. J., Berkman, L. F., Blazer D. G., Scherr, P. A., & Wallace, R. B. (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology Medical Sciences, 49, 85–94.
Guralnik, J. M., Fried, L. P., & Salive, M. E. (1996). Disability as a public health outcome in the aging population. Annual Review of Public Health, 17, 25–46.
Henderson, A. S., Easteal, S., Jorm, A. F., et al. (1995). Apolipoprotein E allele epsilon 4, dementia, and cognitive decline in a population sample. Lancet, 346, 1387–1390.
Hoeymans, N., Wong, A., van Gool, C. H., Deeg, D. J. H., Nusselder, W. J., de Klerk, M. M. Y., van Boxtel, M. P. J., & Picavet, H. S. J. (2012). The disabling effect of diseases: A study on trends in diseases, activity limitations and their interrelationships. American Journal of Public Health, 102(1), 160–173.
Hoogendijk, E., Broese van Groenou, M., Van Tilburg, T., & Deeg, D. (2008). Educational differences in functional limitations: Comparisons of 55–65-year-olds in the Netherlands in 1992 and 2002. International Journal of Public Health, 53, 281–289.
Huisman, M., Kunst, A., Deeg, D., Grigoletto, F., Nusselder, W., & Mackenbach, J. (2005). Educational inqualities in the prevalence and incidence of disability in Italy and the Netherlands were observed. Journal of Clinical Epidemiology, 58, 1058–1063.
Huisman, M., Poppelaars, J., van der Horst, M., Beekman, A., Brug, J., van Tilburg, T., & Deeg, D. (2011). Cohort profile: The longitudinal aging study Amsterdam. International Journal of Epidemiology, 40(4):868–876.
Jonker, A. A., Comijs, H. C., Knipscheer, K. C., & Deeg, D. J. (2008). Persistent deterioration of functioning (PDF) and change in well-being in older persons. Aging Clinical and Experimental Research, 20, 461–468.
Jylhä, M., Guralnik, J. M., Ferrucci, L., Jokela, J., & Heikkinen, E. (1998). Is self-rated health comparable across cultures and genders? Journal of Gerontology: Social Sciences, 53B, S144–S152.
Kamp, K. van de, Braam, A. W., & Deeg, D. J. (2008). Shifts in the self-perceived health of 55–64-year olds between 1992 and 2002. Tijdschr Gerontol Geriatr 39, 182–192 (In Dutch, abstract in English).
Klinkenberg, M. (2004). The last phase of life of older people: Health, preferences and care. Amsterdam: Drukkerij WC den Ouden B. V. (ISBN: 90-5669-077-9).
Knoops, K. T. B., De Groot, L. C. P. G. M., Kromhout, D., Perrin, A. E., Moreiras-Varela, O., Menotti, A., & Van Staveren, W. (2004). Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women—The HALE project. Journal of the American Medical Association, 292, 1433–1439.
Korporaal, M., Broese van Groenou, M. I., & Van Tilburg, T. G. (2008). Effects of own and spousal disability on loneliness among older adults. Journal of Aging and Health, 20, 306–325.
Koster, A., Bosma, H., Broese van Groenou, M. I., Kempen, G. I., Penninx, B. W., van Eijk, J. T., & Deeg, D. J. H. (2006). Explanations of socioeconomic differences in changes in physical function in older adults: Results from the Longitudinal aging study Amsterdam. BMC Public Health, 6, 244.
Kriegsman, D. M. W., Deeg, D. J. H., & Stalman, W. A. B. (2004). Comorbidity of somatic chronic diseases and decline in physical functioning. The longitudinal aging study Amsterdam. Journal of Clinical Epidemiology, 57, 55–65.
Lafortune, G., Balestat, G, & The Disability Study Expert Group Members. (2007). Trends in severe disability among elderly people: Assessing the evidence in 12 OECD countries and the future implication (OECD Health Working Papers No. 26). Paris: OECD.
Manton, K. G. (1982). Changing concepts of morbidity and mortality in the elderly population. Milbank Quarterly, 60, 183–244.
Melzer, D., Dik, M. G., Van Kamp, G. J., Jonker, C., & Deeg, D. J. H. (2005). The APOE e4 polymorphism is strongly associated with poor mobility performance test results but not self-reported limitation in older people. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 60A, 1319–1323.
Minicuci, N., Noale, M., Bardage, C., Blumstein, T., Deeg, D. J. H., Gindin, J., Jylhä, M., Nikula, S., Otero, A., Pedersen, N. L., Pluijm, S. M. F., Zunzunegui, M. V., & Maggi, S., for the CLESA Working Group (2003). Cross-national determinants of quality of life from six longitudinal studies on aging: The CLESA project. Aging Clinical and Experimental Research, 15, 187–202.
Moe, J. O., & Hagen, T. P. (2011). Trends and variation in mild disability and functional limitations among older adults in Norway, 1986–2008. European Journal of Ageing, 8(1), 49–61.
Morley, J. E., Perry, H. M III, & Miller, D. K. (2002). Editorial: Something about frailty. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 57(11), M698–M704.
Parker, M. G., Ahacic, K., & Thorslund, M. (2005). Health changes among Swedish oldest old: Prevalence rates from 1992 and 2002 show increasing health problems. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 60, 1351–1355.
Parker, M. G., Schön, P., Lagergren, M., & Thorslund, M. (2008). Functional ability in the elderly Swedish population from 1980 to 2005. European Journal of Ageing, 5, 299–309.
Pluijm, S. M. F., Bardage, C., Nikula, S., Blumstein, T., Jylhä, M., Minicuci, N., Zunzunegui, M. V., Pedersen, N. L., & Deeg, D. J. H., for the CLESA Study Working Group. (2005). A harmonized measure of activities of daily living was a reliable and valid instrument for comparing disability in older people across countries. Journal of Clinical Epidemiology, 58, 1015–1023.
Pluijm, S. M., Smit, J. H., Tromp, E. A., Stel, V. S., Deeg, D. J., Bouter, L. M., & Lips, P. (2006). A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: Results of a 3-year prospective study. Osteoporosis International, 17, 1–9.
Pluijm, S. M. F., Visser, M., Puts, M. T. E., Dik, M. G., Schalk, B. W. M., Van Schoor, N. M., Schaap, L. A., Bosscher, R. J., & Deeg, D. J. H. (2007). Unhealthy lifestyles during the life course: Associations with physical decline in late life. Aging Clinical and Experimental Research, 19, 75–83.
Portrait, F., Alessie, R., & Deeg, D. (2010). Do early life and contemporaneous macroconditions explain health at older ages? Journal of Population Economics, 23(2), 617–642.
Pot, A. M., Portrait, F., Visser, G., Puts, M., van Groenou, M. I., & Deeg, D. J. H. (2009). Utilization of acute and long-term care in the last year of life: Comparison with survivors in a population-based study. BMC Health Services Research, 9, 139.
Puts, M. T. E., Lips, P., & Deeg, D. J. H. (2005). Static and dynamic measures of frailty predict decline in a performance-based and self-reported measure of physical functioning. Journal of Clinical Epidemiology, 58, 1188–1198.
Puts, M. T., Deeg, D. J., Hoeymans, N., Nusselder, W. J., & Schellevis, F. G. (2008). Changes in the prevalence of chronic disease and the association with disability in the older Dutch population between 1987 and 2001. Age and Ageing, 37, 187–193.
Robine, J. M., & Michel, J. P. (2004). Looking forward to a general theory on population aging. The Journals of Gerontology: Series A, Biological Sciences and Medical Sciences, 59, M590–M597.
Robine, J. M., Mormiche, P., & Sermet, C. (1998). Examination of the causes and mechanisms of the increase in disability-free life expectancy. Journal of Aging and Health, 10, 171–191.
Sagardui-Villamor, J., Guallar-Castillon, P., Garcia-Ferruelo, M., Banegas, J. R., Rodriguez-Artalejo, F. (2005). Trends in disability and disability-free life expectancy among elderly people in Spain: 1986–1999. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 60, 1028–34.
Schaap, L. A., Pluijm, S. M. F., Deeg, D. J. H., & Visser, M. (2006). Inflammatory markers and loss of muscle mass (sarcopenia) and strength. American Journal of Medicine, 119, 526.e9–526.e17.
Schalk, B. W. M., Visser, M., Deeg, D. J. H., & Bouter, L. M. (2004). Lower levels of serum albumin and total cholesterol and future decline in functional performance in older persons: The longitudinal aging study Amsterdam. Age Ageing, 33, 266–272.
Schram, M. T., Frijters, D., Lisdonk, E. H. van de, Ploemacher, J., Craen, A. J. de, Waal, M. W. de, Rooij, F. J. van, Heeringa, J., Hofman, A., Deeg, D. J., & Schellevis, F. G. (2008). Setting and registry characteristics affect the prevalence and nature of multimorbidity in the elderly. Journal of Clinical Epidemiology, 61, 1104–1112.
Smits, C. H. M., Deeg, D. J. H., Kriegsman, D. M. W., & Schmand, B. (1999). Cognitive functioning and health as determinants of mortality in an older population. American Journal of Epidemiology, 150, 978–986.
Sonnenberg, C. M., Deeg, D. J. H., Comijs, H. C., van Tilburg, W., Beekman, A. T. F. (2008). Trends in antidepressant use in the older population: Results from the LASA-study over a period of 10 years. Journal of Affective Disorders, 111, 299–305
Stel, V. S., Pluijm, S. M. F., Deeg, D. J. H., Smit, J. H., Bouter, L. M., & Lips, P. (2004). Functional limitations and poor physical performance as independent risk factors fors elf-reported fractures in older persons. Osteoporos International, 15, 742–750.
Thomése, F., & Broese van Groenou, M. I. (2006). Adaptive strategies after health decline in later life: Increasing the person-environment fit by adjusting the social and physical environment. European Journal of Ageing, 3, 169–177.
Van den Brink, C. L., Tijhuis, M., Kalm, S., Klazinga, N. S., Nissinen, A., Giampaoli, S., Kivinen, P., Kromhout, D., & Van den Bos, G. (2003). Self-reported disability and its associates with performance-based limitation in elderly men: A comparison of three European countries. Journal of the American Geriatrics Society, 51, 782–788.
Van Gool, C. H., Kempen, G. I. J. M., Penninx, B. W. J. H., Deeg, D. J. H., Beekman, A. T. F., & Van Eijk, J. T. M. (2005). Impact of depression on disablement in late middle aged and older persons: Results from the longitudinal aging study Amsterdam. Social Science & Medicine, 60, 25–36.
Van Tilburg, T. G., & Broese van Groenou, M. I. (2002). Network and health changes among older Dutch adults. Journal of Social Issues, 58, 697–713.
Verbrugge, L. M., & Jette, A. (1994). The disablement process. Social Science and Medicine, 38, 1–14.
Visser, M., Stel, V. S., Pluijm, S. M. F., Bosscher, R. J., & Deeg, D. J. H. (2002). Physical activity as a determinant of change in mobility performance: The longitudinal aging study Amsterdam. Journal of American Geriatric Association, 50, 1774–1781.
Visser, M., Pluijm, S. M. F., van der Horst, M. H. L., Poppelaars, J. L., Deeg, & D. J. H. (2005). Lifestyle of Dutch people aged 55–64 years less healthy in 2002/’03 than in 1992/’93. Nederlands Tijdschrift voor Geneeskunde, 149, 2973–2978 (In Dutch, abstract in English).
Wicherts, I. S., Van Schoor, N. M., Boeke, A. J., Visser, M., Deeg, D. J. H., Smit, J., Knol, D. L., & Lips, P. (2007). Vitamin D status predicts physical performance and its decline in older persons. Journal of Clinical Endocrinology & Metabolism, 92, 2058–2065.
Wolf, D. A., Hunt, K., & Knickman, J. (2005). Perspectives on the recent decline in disability at older ages. The Milbank Quarterly, 83, 365–395.
World Health Organisation (WHO). (2002). Towards a common language for functioning, disability and health: ICF. The international classification of functioning, disability and health. Geneva: World Health Organization.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Deeg, D., Huisman, M., Terwee, C., Comijs, H., Thomese, G., Visser, M. (2013). Changes in Functional Ability with Ageing and Over Time. In: Phellas, C. (eds) Aging in European Societies. International Perspectives on Aging, vol 6. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-8345-9_8
Download citation
DOI: https://doi.org/10.1007/978-1-4419-8345-9_8
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-8344-2
Online ISBN: 978-1-4419-8345-9
eBook Packages: Humanities, Social Sciences and LawSocial Sciences (R0)