Abstract
Incidental small-volume renal tumors are a growing clinical problem, and while partial nephrectomy – open or laparoscopic – remains the standard of care, radiofrequency ablation for sub-4 cm disease has been increasingly confirmed as a viable treatment alternative. This chapter looks at the suitability of renal tumors to percutaneous ablation, radiofrequency ablation equipment, and ablation techniques including imaging, patient sedation, and follow-up regimes. The chapter concludes with a review of the current evidence for RFA and how it compares to surgical treatments of renal cancer.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Trends in Renal Cancer Epidemiology
The incidence of renal cell carcinoma (RCC) has increased in recent years, notably in the USA, from 31,200 in 2000 to 57,760 new cases in 2009 [1, 2]. This has largely been attributed to the incidental detection of small renal cancers by the virtue of increased abdominal imaging [3, 4]. However, even accounting for this increase in imaging-detected tumors, there appears to be an additional background increase in renal cancer incidence [3], which appears to be attributable to increased longevity [4, 5], obesity, and hypertension [6]. The largest rise has been seen in the western hemisphere where the age-standardized incidence rates are currently 11–12 per 100,000 compared with 1–3 per 100,000 in China [5].
Contrary to widespread opinion, not all of the increase in renal mass incidence is due to small clinically irrelevant disease. Indeed, there has been an increase in renal cancer-specific mortality from 4.3 per 100,000 in 1971 to 6.0 per 100,000 in 2008 in males in England and Wales [5]. Despite this, overall renal cancer survival rates have improved from 53.2 % in 1975 to 68.8 % in 2002 [1]. In the background, there is an undoubted stage migration toward smaller, more treatable, sub-4 cm stage T1a disease.
Natural History of Renal Cell Carcinoma
Most incidental renal masses detected on imaging for alternative symptomatology are small in size, (<4 cm). Despite optimal imaging it is often not possible to distinguish benign from malignant lesions in this group of lesions. Clinicians must seek to avoid unnecessary, even though minimally invasive, therapies for benign masses.
Frank et al. [7] compared preoperative imaging of solid renal masses with postoperative histology in 2,770 patients. 12.8 % of the 2,935 tumors were benign, largely oncocytomas, and angiomyolipomas. Size has a significant bearing on malignancy risk. In this series, 25 % of sub-3 cm and 46 % of sub-1 cm masses were benign. Ninety percent of masses greater than 4 cm were malignant with 30 % demonstrating high-grade histology (Fuhrman grade 2 and above).
In 1995, Bosniak et al. reviewed historic imaging of 37 patients who had subsequently gone on to have renal lesions removed and reported average growth rate of 3.6 mm/year with a range of 0–11 mm/year [8]. Although the numbers were small, Bosniak noted that those with the most histologically malignant features were toward the upper end of this range of growth rates, whereas those with less malignant features grew more slowly. A meta-analysis by Chawla et al. [9] of 286 lesions demonstrated an average renal mass growth of 2.8 mm/year while the subset histologically proven to be RCC had an average growth rate of 4.0 mm/year. Overall it appears that there is a range of growth patterns with follow-up data suggesting higher histological grades seen in faster growing lesions [9]. Conversely, Kunkle et al. [10] demonstrated 83 % of enhancing renal masses followed up for at least 12 months demonstrating no measurable growth were eventually histologically proven to be RCC.
The meta-analysis by Cary et al. in 2009 with a total of 441 patients [11] found significant rates of malignancy (>60 %) in all renal masses, regardless of size or growth rate. They also reported a 1 % distant metastasis rate during watchful waiting, although these two cases were at 5 and 10 years.
Most authors [12, 13] conclude that renal masses in fit patients should be removed/ablated, while there may be some scope for watchful waiting in less-fit patients where slow-growing renal masses are unlikely to diminish patient longevity (Fig. 46.1).
Should Renal Masses Be Biopsied?
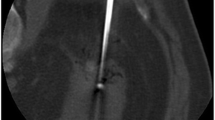
With significant rates of benignity for small renal masses, clinicians should always seek histological verification of the nature of a small renal mass. This can be done either before or, at the very least, immediately prior to the planned ablation. Definitive benign diagnoses of angiomyolipoma or focal infection can be made though there are risks to relying on negative biopsy results. Dechet [14] demonstrated some of the uncertainties of renal biopsy. Intraoperative frozen section results, when compared with extirpative histology, had negative predictive values by two histologists of 69 % and 73 % [14]. Additional more recent renal mass biopsy studies have shown significant improvements in diagnostic accuracy largely due to the advances in immunohistochemistry [15, 16]. Ablation in particular is a non-extirpative technique, and therefore, histological proof of the nature of the treated lesion becomes more critical. For the purposes of treatment planning and follow-up, a histological biopsy should always be sought even though on occasion it will yield a false-negative result (Fig. 46.2).
Device
Radiofrequency ablation causes cell death through heating and tissue coagulation. Radiofrequency ablation utilizes high-frequency alternating current to cause ion agitation of polarized water molecules and subsequent heating through frictional heat loss. There is a concentration of current flux density and thus heating effect around the antenna tip. Most monopolar systems use a single-exposed probe antenna placed within the target lesion. The electrical circuit is completed by large grounding pads applied to the patient’s thighs. When the alternating current is applied, the heating effect is concentrated within 2–3 mm of the probe tip reaching 80–100 °C, whereas the tissue adjacent to the much larger surface area of the grounding pad usually barely records a temperature rise. Although the tissue immediately next to the probe tip is actively heated, the process is otherwise considerably reliant on conductive heating to achieve the overall thermal ablation zone. In order to achieve greater ablation volumes, manufactures have designed clustered or expandable monopolar probes [17]. Hollow probes have also been made which can be coaxially perfused with chilled saline in order to increase the efficiency of heat deposition.
Alternatively the circuit can be completed with multiple bipolar probes instead grounding pads or multiple monopolar probes. This allows one or more probes to be placed (bipolar or multipolar RF ablation) within the target lesion with the current between them resulting in a larger volume of lethal heating [17].
Most authors report using RFA safely in patients with in situ cardiac pacemakers [18, 19], as long as the treatment zone is adequately remote from the pacemaker. A magnet can be placed over the pacemaker to deactivate rhythm sense function. The cardiac devices require formal resetting and checking following the RFA procedure.
Is Renal Cell Cancer Suited to Image-Guided Ablation?
Ignoring the specifics of renal tumors for one moment, we can consider which tumor characteristics imply suitability for image-guided ablation.
Given current RFA device capabilities, an ideal target tumor would be a well-defined, focal tumor of less than 4 cm in size. It should be targetable without critical intervening structures. The tumor should be surrounded by relatively thermally insensitive tissue so as to permit adequate thermal tumor destruction. Lastly, the target lesion itself should be amenable to thermal injury. T1a renal masses [6] fulfill all these physical criteria and are eminently suited to currently available devices and thereby image-guided thermal ablation (Box 46.1).
Treatment Trends
The first standardized, low-mortality nephrectomy technique was described by Robson as recently as 1969 [20]. With most other cancers, the intention is to remove the cancer and not the whole organ; however, radical nephrectomy has persisted as an oncologically effective operation due to the availability of a contralateral functioning kidney. Advanced patient age and renal impairment at time of diagnosis have increased the need to preserve functioning renal parenchyma, and thus, the partial nephrectomy was developed. In the1990s, Van Poppel et al. compared open partial renal resection with open radical nephrectomy [21] and confirmed the technical efficacy of partial resection, albeit with an increase in the complication rates. The oncological efficacy of partial nephrectomy was subsequently confirmed by Weight et al. who demonstrated 5-year overall survival rates of 95 % [22].
Laparoscopic partial nephrectomy is a technically demanding procedure occasionally requiring intracorporeal pelvicalyceal suturing. The procedure usually incurs some degree of warm ischemic injury by virtue of the necessity to clamp the renal hilum for the purposes of intraoperative hemostasis [23]. This can be detrimental to the function of the remaining renal parenchyma and thereby overall renal function if it exceeds 20–30 min [24]. On the other hand, focal renal tumor ablation in patients with single kidneys has been reported to cause no significant functional renal injury [25].
Surgical resection is a well-established treatment which permits histological confirmation of complete tumor removal. Image-guided ablation is inherently an in situ tumor destruction process which relies upon subsequent radiological confirmation of treatment adequacy. Tumor ablation was first reported with an open and then laparoscopic approach using either heat coagulation in the form of radiofrequency ablation or cryotherapy [26]. As ablative probes became smaller, the percutaneous approach became increasingly feasible but highly dependent on accurate image guidance.
There are several advantages to image-guided ablation. Image-guided ablation uses rapid 3-D image reconstruction, usually CT, which can be supplemented with US or MRI, using image fusion technology. This imaging permits precise probe positioning and improves prediction of the ablation zone. From a patient point of view, the percutaneous approach has several advantages. It results in less postoperative pain, can, on occasion, be done with sedation if unable to tolerate a general anesthetic, and is even being performed in many centers as a day-case procedure [18].
In order for image-guided renal tumor ablation to achieve similar outcomes to resectional surgery, it requires precise probe placement or even multiple probe placements with a tolerance of +/−3 mm. This requires the patient to be very still, often for 90–120 min, lying in a prone or prone-oblique position. Although some centers have used RFA under heavy sedation in patients not suitable for general anesthesia, the risks of heavy sedation are often similar. The risks may even be increased as the airway is poorly controlled especially in the prone position with the stomach being compressed. These authors feel strongly that general anesthesia or intravenous (TIVA – total intravenous anesthesia) should be used as it allows complete control, with arrested ventilation permitting a largely stationary target with reproducible organ positioning. As yet, there have been no direct studies comparing general anesthesia to sedation because most centers use either one method or the other. There do not appear to be demonstrable differences in oncological outcome to date [18, 22, 27, 28].
Surgical resection of renal masses yields prognostically important histological information, including the resection margins. RFA cannot provide the physician with that immediate feedback and reassurance. RFA requires serial imaging to assess ablation zone shrinkage, to confirm accepted radiologic surrogates of complete treatment, and to look for tumor recurrence/margin regrowth. This all takes time. For RFA to become successful and widespread, there will have to be sufficient evidence of good long-term oncological outcomes and negligible late local recurrences comparable with the current very low rates of local recurrence after clear margin resectional surgery for small-volume disease.
Image Guidance
While US-guided renal tumor ablation is practiced without significant undertreatment compared to CT guidance [27], the authors feel strongly that US should at least be used in conjunction with CT for confirmation of accurate 3-dimensional probe position. However, in larger patients, US may not be well suited. Furthermore, the echogenic treatment response visualized at US may make it difficult to see the electrode if additional overlapping ablations are to be performed in larger tumors. Also multiprobe placement may be difficult with US as the US transducer may not be able to easily appreciate the position of multiple electrodes. Therefore, deployed electrode positioning is currently best confirmed by orthogonal CT/MRI reformatting. CT also permits careful assessment of tine position in the case of expandable probes. Importantly if all renal tumors are to be targeted, CT most easily allows for careful assessment of adjacent thermally sensitive structures such as colon, adrenal, and the renal hilum. The former can be displaced from the ablation zone by means of hydrodissection (see later).
Patient Positioning and Technique
To achieve accurate electrode position and therefore good outcomes, it is essential to make the electrode placement as straightforward as possible. Although there are software and technologies in development to dictate electrode position within a volume, most procedures are currently best carried out by a combination of US and CT or CT guidance alone. The patient should be placed in an optimized prone-oblique position, and the spine flexed over pillows (a nephrostomy-style position). This usually ensures that straightforward direct or minimally oblique intercostal puncture can be made to the tumor mass.
Even with the patient and electrodes positioned perfectly, there can be thermally sensitive tissue such as bowel adjacent to the renal mass especially in thinner patients. Laparoscopic ablation allows these tissues to be mechanically moved out of the ablation zone. RFA still requires these tissues to be moved, but this is achieved using fluid or gas (often carbon dioxide) injected into retroperitoneal fat planes to displace adjacent structures. The technique is widely known as “hydrodissection” [29]. The fluid used is typically 5 % dextrose solution, in order to prevent any aberrant electrical conduction. Two to three percent of intravenous iodinated contrast can be added to this fluid to facilitate assessment of the dispersal of the dissection fluid [30]. The ureteropelvic junction (UPJ) is thermally sensitive but cannot be easily displaced using hydrodissection. Tumors close to the collecting system and UPJ are increasingly being treated by RFA and cryoablation. In addition to seeking to displace structures, the ureter and collecting system can, to some extent, be protected if actively cooled. This can be achieved by means of the pressure-bagged circulation of chilled normal saline via a cystoscopically placed retrograde ureteric catheter with “piggy-backed” urethral catheter drainage [31]. There is some anecdotal evidence that this can reduce the risk of thermal injury but the operator should still pay careful attention to the likely ablation zone with particular reference to major vessels and the UPJ [32] (Fig. 46.3).
(a) Exophytic renal tumor suitable for image-guided ablation but note the close proximity of the adjacent colon. (b) Hydrodissection fluid has been injected into the perirenal fat to displace the colon from the ablation zone. The addition of 2 % contrast to the hydrodissection fluid enhances visualization of the dissection process with regard to adjacent bowel, kidney, or even hematoma
Renal artery or segmental renal artery embolization prior to RFA may have two potential benefits. Early animal models have shown increased ablation volume in pre-embolized renal tissue [33]. Practice suggests pre-embolization may reduce treatment bleeding and lead to a more effective ablation zone. Larger flowing vessels of greater than 3 mm can cause a heat-sink effect which segmental pre-embolization may help diminish. However pre-embolization is not used routinely as it comes with its own risks including inadvertent renal and/or vascular injury (Fig. 46.4).
(a) Small cortical renal mass; (b) post procedure, the patient became hypotensive with severe flank pain. Portal venous phase images show a large post-procedural renal capsular hematoma; (c) delayed phase images show a small pool of extravasated contrast. This was treated conservatively, but if it had been more brisk, it could have been embolized/coiled angiographically
Minimizing Complications
The vascular nature of RCCs means any needling procedure carries a risk of bleeding. Pre-procedural checks should include any patient or family history of bleeding problems and any current medication. The authors’ practice is to ensure the platelets are greater than 100 and INR equal to or less than 1.4 [27]. Minimizing the number of passes of the RF probe by using a combination of US and CT for placement, and as discussed earlier, reduces probe placements and the risk of obscuring hematoma. At the end of the procedure, RF-induced tumor coagulation and track ablation are thought to help reduce bleeding risk. Overall significant bleeding is seen in less than 1 % of patients [18] and is usually self-limiting.
Tumors in differing positions within the kidney require different strategies to prevent complication. During treatment of lower pole lesions, care must be taken to prevent injury to the ureteropelvic junction; this can be achieved by careful planning of the ablation zone but also ureteric cooling via ureteric catheters as described earlier. Despite these precautions authors have still reported a ureteral stricture rate of 2 % [18]. One should take similar precautions when dealing with lesions deep within the parenchyma and close to the collecting system to reduce the small risk of pelvicalyceal leak or urinoma, even though this has only been rarely reported. Upper pole lesions may be near the adrenal glands; even with the best ablation zone planning, it is essential to have good communication with the anesthetist who should watch for transient hypertension [34] and be prepared with hypotensive anesthesia. All anterior renal lesions bring the ablation zone near the small or large bowel. The authors currently prescribe an enema pre-procedure to help reduce colon loading and particularly gas. Even after the enema, it is often necessary to carefully consider the ablation zone and perform hydrodissection to displace the bowel in up to 50 % of cases in the authors’ experience. Lesions lying anteriorly within the right kidney need special consideration as the duodenum is often in close proximity. If suitable precautions are taken, the position of the lesion within the kidney does not affect the complication rate [18, 35, 36].
It is vital that the ablation process is performed in a sterile manner as post ablation, the tumor undergoes necrosis and becomes temporarily vulnerable to opportunistic infection, although this complication has been rarely reported without associated gut injury. It is important to ensure the patient is not systemically unwell pre-procedure and in particular does not have active urinary infection. Most authors use prophylactic antibiotics; the authors regime is 24 h of broad-spectrum intravenous antibiotic cover starting at induction (metronidazole 500 mg and cefuroxime 750 mg tds) followed by a 10-day course of oral antibiotics (ciprofloxacin 500 mg bd), although there is little evidence of an absolute requirement for this prophylactic cover.
Immediate Follow-Up
Diligent imaging follow-up of patients post RFA is the only way to ensure complete tumor treatment or to detect incomplete treatment. The first post-ablation imaging assessment is usually carried out at 24 h to 30 days after RFA. Immediate post-ablation CTs are reserved for those with a suspected acute complication and are less accurate in detecting undertreatment as an irregular margin of the ablation zone enhances acutely [37], and the ablation zone becomes better defined over the subsequent 3–14 days. CT densitometry – i.e., assessment of target tumor enhancement – remains central to the determination of treatment success and has been validated by several studies [38]. This is usually performed by careful volumetric CT comparison of unenhanced images with late arterial phase and to a lesser extent nephrographic phase images [39]. Subtotal treatments are usually manifest as marginal crescents or focal areas of persistent enhancement often at the peri-cortical or deep aspects of the tumor. Other CT features help to confirm treatment adequacy [39], a subjacent crescent or wedge of cortical coagulation usually signifies adequate treatment of the cortical margin, and over time a fibrotic halo is often seen (approximately 70 %) in the peri-renal fat and has been confirmed as a feature supporting complete treatment [40, 41] (Fig. 46.5).
(a) Lower pole RCC; (b) follow-up imaging after the first ablation, note the crescentic enhancement of local recurrence. (c) Immediate post re-ablation confirms subjacent crescent of cortical infarction, treatment margin; (d, e) longer-term follow-up shows non-enhancing ablation zone reducing in size
In 1.9 % of patients, Lokken [42] described enhancing nodules along the ablation track post RFA which were concerning for track seeding. Some of these lesions were sampled and found to be inflammatory or a small abscess. All lesions subsequently became smaller or resolved completely. Lokken concluded that even though the imaging was initially suspicious for track seeding, the lesions should be biopsied and not diagnosed as tumor seeding which is rare especially with track ablation.
Long-Term Follow-Up Regimes
Radiofrequency-ablated tumors will often appear slightly enlarged at initial post-procedural imaging but do not enhance. The treated tumor slowly diminishes in size and exophytic tumors often “auto-amputate.” In the case of RFA, the thermal scar can form a chronic granulomatous nodule and persist for years as a small, stable, and non-enhancing nodule. This is in contradistinction to cryoablation where the nodule appears to involute more quickly and often completely involutes over 2–3 years. In the case of renal failure, MR can be utilized to avoid the risk of contrast-induced nephropathy with attention to the relative risks of nephrogenic systemic fibrosis. Early studies [43] have suggested arterial spin labeling can identify viable tumor as well as contrast-enhanced MRI and may negate the need for IV contrast in future follow-up studies. In severe renal failure, GFR < 25 contrast-enhanced US can be utilized for follow-up. However, US contrast is not approved in the United States (Fig. 46.6).
A multicenter review concluded that follow-up in the first year should consist of imaging at 1, 3, and 12 months with most people also imaging at 6 months [37]. Follow-up regimes are currently intense for the purposes of data collection and validation of RFA outcomes. Some published series have however noted [44] a small (3–4 %) but significant incidence of late local recurrence as late as 2–4 years after treatment. These recurrences are very uncommon and slow growing. As such most centers still perform at least annual imaging out to 5 years.
Radiologic and Oncologic Outcomes for Small Renal Tumors
Radiofrequency ablation (RFA) is a maturing technology, and undoubtedly the clinical effectiveness of these devices, in terms of lethal thermal ablation volumes, has improved significantly over the last 15 years. Similarly, as with any surgical techniques, there is a clearly identifiable learning curve with optimal outcomes dependent upon a standardized technique with appropriate treatment dosimetry and diligent imaging follow-up. Recent natural history papers [45] have also emphasized the relatively indolent growth pattern of many small, incidentally detected renal tumors in older patients, often meaning the growth rate at ∼3 mm/year with a low metastatic potential.
It remains the case that some 20–30 % of renal tumors exhibit a significantly faster doubling time and therefore pose a higher risk of progression and metastasis [46]. The decision to treat must, however, be judged against the overall relatively slow growth of these often incidentally detected tumors.
Partial nephrectomy – laparoscopic or open – has been shown to achieve excellent 5- and 10-year cancer-specific survivals [47, 48]. However, given the low metastatic potential of sub-4 cm, T1a tumors, it can be difficult to demonstrate survival differences between treatment modalities. Studies will have to be adequately powered to detect these differences. The reported experience in the literature is confounded by a number of factors:
-
(a)
Often single-center retrospective cases series
-
(b)
Tendency toward biased case selection with percutaneous procedures reserved for patients with significant comorbidities
-
(c)
Some centers comparing mixed modalities of treatment such as laparoscopic cryoablation (CRA) compared with percutaneous radiofrequency ablation (RFA)
For the purposes of this review, we have therefore drawn together larger, more substantial RFA case series and reported longer-term oncologic outcomes.
In 2005, Gervais et al. [28] reported their experience of 100 renal tumors treated by percutaneous, CT-guided RFA in 85 patients. The mean tumor size was 32 mm (90 % biopsy-proven renal cell carcinoma), and they were followed up for a mean of 28 months. Overall 90 % were completely ablated. Multivariate analysis found that small (<3 cm), exophytic tumors were straightforwardly treated but that larger (>3 cm), more deeply set tumors often required additional treatment sessions (Fig. 46.7).
A report by Park et al. [49] in 2006 reported on a mixed series of percutaneous and laparoscopic RFA in 78 patients with 94 tumors, with a mean size of 24 mm. Some 75 % of these tumors were biopsy-proven renal cancer, and the mean follow-up of this cohort was 25 months. The authors reported a cancer-specific survival rate of 98.5 % and an overall survival rate of 92.3 %. They concluded that RFA was comparable with traditional surgical resection for solitary renal masses.
A further large series by Zagoria et al. [18] reported CT-guided renal tumor RFA outcomes in 104 patients with 125 renal tumors. All were biopsy-proven RCC with a mean diameter of 27 mm and a mean follow-up of 13.8 months. Ninety three percent of these tumors were treated in a single session. On subgroup analysis, straightforward, single-session treatment occurred up to a threshold of 37 mm. Increasingly larger tumors resulted in higher level of subtotal treatment, with every 1 cm increase in size-decreasing tumor-free survival by a factor of 2.19.
Breen et al. reported the technical outcomes from the RFA of 105 tumors in 97 patients with a mean tumor size of 32 mm and mean follow-up of 16.7 months [27]. The biopsy outcomes in this cohort were not detailed. They reported an overall technical success rate of 90.5 %, and again logistic regression analysis confirmed 37 mm as an important threshold for single-session treatment success (given technology present during the study period, 1999–2005).
A multicenter, collaborative study by Matin et al. reviewed the experience of seven institutions in terms of residual posttreatment and recurrent disease following percutaneous and laparoscopic radiofrequency and cryoablation of renal tumors [37]. (The cryoablation results are dealt with in a separate chapter). The authors chose to report together residual and recurrent disease rates akin to the practice in the liver of reporting “local tumor progression,” making no distinction between primary subtotal treatment and late local recurrence. Of 616 patients treated, 63 patients were found to have residual/recurrent disease of which 8 had undergone cryoablation and 55 RFA. However, these combined cohorts obscured a significant bias with the vast majority of CRA cases performed via a laparoscopic approach and almost certainly the vast majority of those unsuitable for laparoscopic CRA being offered percutaneous RFA. Unfortunately, these selection biases plague the reported renal tumor ablation literature. Most incomplete treatments (70 %) were detected within the first three months – i.e., were likely reportable as primary “subtotal treatments.”
Despite reasonable intermediate term results, the long-term oncologic outcome data for renal tumor RFA remains sparse. In 2005, the MGH Boston group reported the 5-year outcome of 16 patients following RFA for biopsy-proven RCC [50]. Five patients had died before completing 4 years of follow-up from unrelated causes. All except one tumor was completely ablated for a cancer-specific survival rate of 93.8 %.
The most substantive long-term data comes from Levinson et al. [44]. Thirty one patients with 34 tumors of between 1 and 4 cm (median 2 cm) were followed up for a mean of 61.6 months. One subtotal treatment was successfully retreated. There were three late local recurrences notably at 7, 13, and 31 months yielding an overall recurrence-free survival of 90.3 %. Of the 18 pathologically confirmed RCCs, the disease-specific, metastasis-free, and recurrence-free survivals were 100 %, 100 %, and 79.9 % at a mean of 57.4 months of follow-up.
Recent studies have continued to show consistent results. Tracy et al. [51] followed 160 patients who had RFA for biopsy-proven RCC for 5 years; their overall 5-year recurrence-free survival was 90 %. Zagoria et al. [36] followed up 41 patients with 48 RCCs; they found no recurrences in those tumors less than 4 cm at time of treatment and an overall 5-year recurrence-free survival of 88 %.
In summary, RFA appears to yield disease-specific survivals comparable with more onerous surgical resection. This is, however, a coarse measure of outcome in a relatively indolent disease. Larger cohorts with longer follow-up after RFA are required to ensure there is not a small but significant incidence of unacceptable late local recurrence [44] which would question the oncological merit of even this minimally invasive intervention.
References
National Cancer Institute. Surveillance, epidemiology and end results. http://seer.cancer.gov. Accessed June 2010.
American Cancer Society. Facts and figures downloads. http://www.cancer.org. Accessed June 2010.
Chow W, Devesa S, et al. Rising incidence of renal cell cancer in the United States. JAMA. 1999;281:1628–31.
Jayson M, Sanders H. Increased incidence of serendipitously discovered renal cell carcinoma. Urology. 1998;51(2):203–5.
Quinn M, Babb P, et al. Cancer trends in England and Wales 1950–1999, National statistics. http://www.statistics.gov.uk/downloads/theme_health/cancertrends_5099.pdf. Accessed June 2010. or Vol. SMPS No. 66. 2001: TSO.
Adams KF, Leitzmann MF, Albanes D, et al. Body size and renal cell cancer incidence in a large US cohort study. Am J Epidemiol. 2008;168(3):268–77. Epub 9 Jun 2008.
Frank I, Blute M, Cheville J, et al. Solid renal tumors: an analysis of pathological features related to tumor size. J Urol. 2003;170(6 Pt 1):2217–20.
Bosniak MA, Birnbaum BA, Krinsky GA, Waisman J. Small renal parenchymal neoplasms: further observations on growth. Radiology. 1995;197(3):589–97.
Chawla SN, Crispen PL, Hanlon AL, Greenberg RE, Chen DY, Uzzo RG. The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J Urol. 2006;175(2):425–31.
Kunkle DA, Crispen PL, Chen DY, Greenberg RE, Uzzo RG. Enhancing renal masses with zero net growth during active surveillance. J Urol. 2007;177(3):849–53. discussion 853–4.
Cary KC, Sundaram CP. Watchful waiting in the treatment of the small renal mass. Indian J Urol. 2009;25(4):489–93.
Mattar K, Jewett MA. Watchful waiting for small renal masses. Curr Urol Rep. 2008;9(1):22–5.
Mues AC, Landman J. Small renal masses: current concepts regarding the natural history and reflections on the American Urological Association guidelines. Curr Opin Urol. 2010;20(2):105–10.
Dechet CB, Sebo T, Farrow G, Blute ML, Engen DE, Zincke H. Prospective analysis of intraoperative frozen needle biopsy of solid renal masses in adults. J Urol. 1999;162(4):1282–4. discussion 1284–5.
Beland MD, Mayo-Smith WW, Dupuy DE, Cronan JJ, DeLellis RA. Diagnostic yield of 58 consecutive imaging-guided biopsies of solid renal masses: should we biopsy all that are indeterminate? AJR. 2007;188:792–7.
Rybicki FJ, Shu KM, Cibas ES, Fielding JR, vanSonnenberg E, Silverman SG. Percutaneous biopsy of renal masses: sensitivity and negative predictive value stratified by clinical setting and size of masses. AJR Am J Roentgenol. 2003;180(5):1281–7.
Goldberg SN, Gazelle GS, Dawson SL, Rittman WJ, Mueller PR, Rosenthal DI. Tissue ablation with radiofrequency using multiprobe arrays. Acad Radiol. 1995;2(8):670–4.
Zagoria RJ, Traver MA, Werle DM, Perini M, Hayasaka S, Clark PE. Oncologic efficacy of CT-guided percutaneous radiofrequency ablation of renal cell carcinomas. AJR Am J Roentgenol. 2007;189(2):429–36.
Skonieczki BD, Wells C, Wasser EJ, Dupuy DE. Radiofrequency and microwave tumor ablation in patients with implanted cardiac devices: is it safe? Eur J Radiol. 2011;79(3):343–6. Epub ahead of print.
Robson CJ, Churchill BM, Anderson W. The results of radical nephrectomy for renal cell carcinoma. J Urol. 1969;101(3):297–301.
Van Poppel H, Bamelis B, Oyen R, Baert L. Partial nephrectomy for renal cell carcinoma can achieve long-term tumor control. J Urol. 1998;160(3 Pt 1):674–8.
Weight CJ, Lieser G, Larson BT, Gao T, Lane BR, Campbell SC, Gill IS, Novick AC, Fergany AF. Partial nephrectomy is associated with improved overall survival compared to radical nephrectomy in patients with unanticipated benign renal tumours. Eur Urol. 2010;58(2):293–8 [Epub ahead of print].
Marszalek M, Meixl H, Polajnar M, Rauchenwald M, Jeschke K, Madersbacher S. Laparoscopic and open partial nephrectomy: a matched-pair comparison of 200 patients. Eur Urol. 2009;55(5):1171–8. Epub 2009 Feb 20.
Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, Gill IS, Campbell SC, Blute ML. Comparison of warm ischemia versus no ischemia during partial nephrectomy on a solitary kidney. Eur Urol. 2010;58(3):331–6 [Epub].
Krambeck AE, Farrell MA, Callstrom MR, Atwell TD, Charboneau JW, Chow GK, Dimarco DS, Patterson DE. Radiofrequency ablation of renal tumors in the solitary kidney. Can J Urol. 2008;15(4):4163–8. discussion 4168.
Zlotta AR, Wildschutz T, Raviv G, Peny MO, van Gansbeke D, Noel JC, Schulman CC. Radiofrequency interstitial tumor ablation (RITA) is a possible new modality for treatment of renal cancer: ex vivo and in vivo experience. J Endourol. 1997;11(4):251–8.
Breen D, Rutherford E, Steadman B, et al. Management of renal tumours by image-guided radiofrequency ablation: experience in 105 tumours. CVIR. 2007;30:936–42.
Gervais DA, McGovern FJ, Arellano RS, McDougal WS, Mueller PR. Radiofrequency ablation of renal cell carcinoma: part 1, Indications, results, and role in patient management over a 6-year period and ablation of 100 tumors. AJR Am J Roentgenol. 2005;185(1):64–71.
Ginat DT, Saad WE. Bowel displacement and protection techniques during percutaneous renal tumor thermal ablation. Tech Vasc Interv Radiol. 2010;13(2):66–74.
DeBenedectis CM, Beland MD, Dupuy DE, et al. Utility of iodinated contrast medium in hydrodissection fluid when performing renal tumor ablation. J Vasc Interv Radiol. 2010;21(5):745–7.
Cantwell CP, Wah TM, Gervais DA, Eisner BH, Arellano R, Uppot RN, Samir AE, Irving HC, McGovern F, Mueller PR. Protecting the ureter during radiofrequency ablation of renal cell cancer: a pilot study of retrograde pyeloperfusion with cooled dextrose 5 % in water. J Vasc Interv Radiol. 2008;19:1034–40.
Morales JP, Sabharwal T, Georganas M, Dourado R, Cahill D, Adam A. Cold saline irrigation of the renal pelvis during radiofrequency ablation of a central renal neoplasm: a case report. J Med Case Reports. 2008;2:40.
Sommer CM, Kortes N, Zelzer S, Arnegger FU, Stampfl U, Bellemann N, Gehrig T, Nickel F, Kenngott HG, Mogler C, Longerich T, Meinzer HP, Richter GM, Kauczor HU, Radeleff BA. Renal artery embolization combined with radiofrequency ablation in a porcine kidney model: effect of small and narrowly calibrated microparticles as embolization material on coagulation diameter, volume, and shape. Cardiovasc Intervent Radiol. 2011;34(1):156–65 [Epub].
Mayo-Smith WW, Dupuy DE, Parikh PM, Pezzullo JA, Cronan JJ. Imaging-guided percutaneous radiofrequency ablation of solid renal masses: techniques and outcomes of 38 treatment sessions in 32 consecutive patients. AJR. 2003;180(6):1503–8.
Atwell TD, Carter RE, Schmit GD, Carr CM, Boorjian SA, Curry TB, Thompson RH, Kurup AN, Weisbrod AJ, Chow GK, Leibovich BC, Callstrom MR, Patterson DE. Complications following 573 percutaneous renal radiofrequency and cryoablation procedures. J Vasc Interv Radiol. 2012;23(1):48–54.
Zagoria RJ, Pettus JA, Rogers M, Werle DM, Childs D, Leyendecker JR. Long-term outcomes after percutaneous radiofrequency ablation for renal cell carcinoma. Urology. 2011;77(6):1393–7.
Matin SF, Ahrar K, Cadeddu JA, Gervais DA, McGovern FJ, Zagoria RJ, Uzzo RG, Haaga J, Resnick MI, Kaouk J, Gill IS. Residual and recurrent disease following renal energy ablative therapy: a multi-institutional study. J Urol. 2006;176(5):1973–7.
Gervais DA, McGovern FJ, Wood BJ, et al. Radio-frequency ablation of renal cell carcinoma: early clinical experience. Radiology. 2000;217:665–72.
Rutherford EE, Cast JE, Breen DJ. Immediate and long-term CT appearances following radiofrequency ablation of renal tumours. Clin Radiol. 2008;63(2):220–30. Epub 2007 Nov 7.
Davenport MS, Caoili EM, Cohan RH, Ellis JH, Higgins EJ, Willatt J, Fox GA. MRI and CT characteristics of successfully ablated renal masses: imaging surveillance after radiofrequency ablation. AJR Am J Roentgenol. 2009;192(6):1571–8.
Schirmang TC, Mayo-Smith WW, Dupuy DE, Beland MD, Grand DJ. Kidney neoplasms: renal halo sign after percutaneous radiofrequency ablation – incidence and clinical importance in 101 consecutive patients. Radiology. 2009;253:263–9.
Lokken RP, Gervais DA, Arellano RS, Tuncali K, Morrison PR, Tatli S, Mueller PR, Silverman SG. Inflammatory nodules mimic applicator track seeding after percutaneous ablation of renal tumors. AJR Am J Roentgenol. 2007;189:845–8.
Boss A, Martirosian P, Schraml C, Clasen S, Fenchel M, Anastasiadis A, Claussen CD, Pereira PL, Schick F. Morphological, contrast-enhanced and spin labeling perfusion imaging for monitoring of relapse after RF ablation of renal cell carcinomas. Eur Radiol. 2006;16(6):1226–36.
Levinson AW, Su LM, Agarwal D, Sroka M, Jarrett TW, Kavoussi LR, Solomon SB. Long-term oncological and overall outcomes of percutaneous radio frequency ablation in high risk surgical patients with a solitary small renal mass. J Urol. 2008;180(2):499–504. discussion 504. Epub 2008 Jun 11.
Kunkle DA, Egleston RG. Excise, ablate or observe: the small renal mass dilemma – a meta-analysis and review. J Urol. 2008;179:1227–33.
Volpe A, Panzarella T, Rendon RA, Haider MA, Kondylis FI, Jewett MA. The natural history of incidentally detected small renal masses. Cancer. 2004;100:738.
Fergany AF, Hafez KS, Novick AC. Long-term results of nephron sparing surgery for localized renal cell carcinoma: 10-year follow up. J Urol. 2000;163(2):442–5.
Aron M, Gill IS. Partial nephrectomy–why, when, how…? J Urol. 2008;179(3):811–2. Epub 2008 Jan 25.
Park S, Anderson JK, Matsumoto ED, et al. Radiofrequency ablation of renal tumours: intermediate-term results. J Endourol. 2006;20:569–73.
McDougal WS, Gervais DA, McGovern FJ, Mueller PR. Long-term follow up of patients with renal cell carcinoma treated with radiofrequency ablation with curative inter. J Urol. 2005;174:61–3.
Tracy CR, Raman JD, Donnally C, Trimmer CK, Cadeddu JA. Durable oncologic outcomes after radiofrequency ablation. Experience from treating 243 small renal masses over 7.5 years. Cancer. 2010;116(13):3135–42.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this entry
Cite this entry
Osborn, P., Breen, D.J. (2013). Image-Guided Radio Frequency Ablation of Renal Cancer. In: Dupuy, D., Fong, Y., McMullen, W. (eds) Image-Guided Cancer Therapy. Springer, New York, NY. https://doi.org/10.1007/978-1-4419-0751-6_48
Download citation
DOI: https://doi.org/10.1007/978-1-4419-0751-6_48
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4419-0750-9
Online ISBN: 978-1-4419-0751-6
eBook Packages: MedicineReference Module Medicine