Abstract
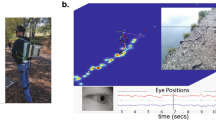
Visual information is crucial for safe locomotion because it allows individuals to adjust their stepping patterns to deal with environmental demands. Deficits in the ability to visually sample the environment expose walkers to an increased risk of falling, which have motivated researchers to investigate the visual control of locomotion. Portable eye tracking technologies allow researchers to quantify eye movements and determine how, when and what individuals look at during locomotion. However, appropriate methodological approaches are required to understand the complex link between eye movements and locomotion. This book chapter explores methodological aspects required to assess the visual control of locomotion. To offer readers examples of how we applied eye tracking technologies to investigate the role of visual information during locomotor tasks, we revisit two previous studies published by our group involving older adults and patients with Parkinson’s disease.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Vitório R, Gobbi LT, Lirani-Silva E, Moraes R, Almeida QJ (2016) Synchrony of gaze and stepping patterns in people with Parkinson’s disease. Behav Brain Res 307:159–164. https://doi.org/10.1016/j.bbr.2016.04.010
Lord SR, Ward JA, Williams P, Anstey KJ (1994) Physiological factors associated with falls in older community-dwelling women. J Am Geriatr Soc 42(10):1110–1117. https://doi.org/10.1111/j.1532-5415.1994.tb06218.x
Ivers RQ, Cumming RG, Mitchell P, Attebo K (1998) Visual impairment and falls in older adults: the Blue Mountains eye study. J Am Geriatr Soc 46(1):58–64. https://doi.org/10.1111/j.1532-5415.1998.tb01014.x
Lord SR, Clark RD, Webster IW (1991) Visual acuity and contrast sensitivity in relation to falls in an elderly population. Age Ageing 20(3):175–181. https://doi.org/10.1093/ageing/20.3.175
Lord SR, Dayhew J (2001) Visual risk factors for falls in older people. J Am Geriatr Soc 49(5):508–515. https://doi.org/10.1046/j.1532-5415.2001.49107.x
Moraca GAG, Beretta VS, Dos Santos PCR, Nóbrega-Sousa P, Orcioli-Silva D, Vitório R, Gobbi LTB (2021) Center of pressure responses to unpredictable external perturbations indicate low accuracy in predicting fall risk in people with Parkinson’s disease. Eur J Neurosci 53(8):2901–2911. https://doi.org/10.1111/ejn.15143
Rubenstein LZ, Josephson KR (2002) The epidemiology of falls and syncope. Clin Geriatr Med 18(2):141–158. https://doi.org/10.1016/s0749-0690(02)00002-2
Chapman GJ, Hollands MA (2006) Evidence for a link between changes to gaze behaviour and risk of falling in older adults during adaptive locomotion. Gait Posture 24(3):288–294. https://doi.org/10.1016/j.gaitpost.2005.10.002
Chapman GJ, Hollands MA (2007) Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait Posture 26(1):59–67. https://doi.org/10.1016/j.gaitpost.2006.07.010
Marigold DS, Patla AE (2007) Gaze fixation patterns for negotiating complex ground terrain. Neuroscience 144(1):302–313. https://doi.org/10.1016/j.neuroscience.2006.09.006
Matthis JS, Yates JL, Hayhoe MM (2018) Gaze and the control of foot placement when walking in natural terrain. Curr Biol 28(8):1224–1233.e1225. https://doi.org/10.1016/j.cub.2018.03.008
Patla AE, Vickers JN (1997) Where and when do we look as we approach and step over an obstacle in the travel path? Neuroreport 8(17):3661–3665. https://doi.org/10.1097/00001756-199712010-00002
Tilley BC, LaPelle NR, Goetz CG, Stebbins GT, Force M-UT (2014) Using cognitive pretesting in scale development for Parkinson’s disease: the Movement Disorder Society unified Parkinson’s disease rating scale (MDS-UPDRS) example. J Parkinsons Dis 4(3):395–404. https://doi.org/10.3233/JPD-130310
Patla AE (1997) Understanding the roles of vision in the control of human locomotion. Gait Posture 5(1):54–69. https://doi.org/10.1016/S0966-6362(96)01109-5
Marigold DS (2008) Role of peripheral visual cues in online visual guidance of locomotion. Exerc Sport Sci Rev 36(3):145–151. https://doi.org/10.1097/JES.0b013e31817bff72
Vitório R, Lirani-Silva E, Pieruccini-Faria F, Moraes R, Gobbi LT, Almeida QJ (2014) Visual cues and gait improvement in Parkinson’s disease: which piece of information is really important? Neuroscience 277:273–280. https://doi.org/10.1016/j.neuroscience.2014.07.024
Srivastava A, Ahmad OF, Pacia CP, Hallett M, Lungu C (2018) The relationship between saccades and locomotion. J Mov Disord 11(3):93–106. https://doi.org/10.14802/jmd.18018
Stuart S, Galna B, Lord S, Rochester L, Godfrey A (2014) Quantifying saccades while walking: validity of a novel velocity-based algorithm for mobile eye tracking. Annu Int Conf IEEE Eng Med Biol Soc 2014:5739–5742. https://doi.org/10.1109/embc.2014.6944931
Stuart S, Alcock L, Galna B, Lord S, Rochester L (2014) The measurement of visual sampling during real-world activity in Parkinson’s disease and healthy controls: a structured literature review. J Neurosci Methods 222:175–188. https://doi.org/10.1016/j.jneumeth.2013.11.018
Stuart S, Hunt D, Nell J, Godfrey A, Hausdorff JM, Rochester L, Alcock L (2018) Do you see what I see? Mobile eye-tracker contextual analysis and inter-rater reliability. Med Biol Eng Comput 56(2):289–296. https://doi.org/10.1007/s11517-017-1669-z
Freedman EG (2008) Coordination of the eyes and head during visual orienting. Exp Brain Res 190(4):369–387. https://doi.org/10.1007/s00221-008-1504-8
Cognolato M, Atzori M, Müller H (2018) Head-mounted eye gaze tracking devices: an overview of modern devices and recent advances. J Rehabil Assist Technol Eng 5:2055668318773991. https://doi.org/10.1177/2055668318773991
Hollands MA, Marple-Horvat DE, Henkes S, Rowan AK (1995) Human eye movements during visually guided stepping. J Mot Behav 27(2):155–163. https://doi.org/10.1080/00222895.1995.9941707
Moraes R, Lewis MA, Patla AE (2004) Strategies and determinants for selection of alternate foot placement during human locomotion: influence of spatial and temporal constraints. Exp Brain Res 159(1):1–13. https://doi.org/10.1007/s00221-004-1888-z
Hollands MA, Marple-Horvat DE (2001) Coordination of eye and leg movements during visually guided stepping. J Mot Behav 33(2):205–216. https://doi.org/10.1080/00222890109603151
Hausdorff JM (2005) Gait variability: methods, modeling and meaning. J Neuroeng Rehabil 2:19. https://doi.org/10.1186/1743-0003-2-19
Rubenstein LZ, Josephson KR (2006) Falls and their prevention in elderly people: what does the evidence show? Med Clin North Am 90(5):807–824. https://doi.org/10.1016/j.mcna.2006.05.013
Conceição NRD, Nóbrega de Sousa P, Pereira MP, Gobbi LTB, Vitório R (2019) Utility of center of pressure measures during obstacle crossing in prediction of fall risk in people with Parkinson’s disease. Hum Mov Sci 66:1–8. https://doi.org/10.1016/j.humov.2019.03.010
Allen NE, Schwarzel AK, Canning CG (2013) Recurrent falls in Parkinson’s disease: a systematic review. Parkinsons Dis 2013:906274. https://doi.org/10.1155/2013/906274
Stegemöller EL, Buckley TA, Pitsikoulis C, Barthelemy E, Roemmich R, Hass CJ (2012) Postural instability and gait impairment during obstacle crossing in Parkinson’s disease. Arch Phys Med Rehabil 93(4):703–709. https://doi.org/10.1016/j.apmr.2011.11.004
Vitório R, Pieruccini-Faria F, Stella F, Gobbi S, Gobbi LT (2010) Effects of obstacle height on obstacle crossing in mild Parkinson’s disease. Gait Posture 31(1):143–146. https://doi.org/10.1016/j.gaitpost.2009.09.011
Vitório R, Lirani-Silva E, Baptista AM, Barbieri FA, dos Santos PC, Teixeira-Arroyo C, Gobbi LT (2014) Disease severity affects obstacle crossing in people with Parkinson’s disease. Gait Posture 40(1):266–269. https://doi.org/10.1016/j.gaitpost.2014.03.003
Stolze H, Klebe S, Zechlin C, Baecker C, Friege L, Deuschl G (2004) Falls in frequent neurological diseases--prevalence, risk factors and aetiology. J Neurol 251(1):79–84. https://doi.org/10.1007/s00415-004-0276-8
Almeida QJ, Frank JS, Roy EA, Jenkins ME, Spaulding S, Patla AE, Jog MS (2005) An evaluation of sensorimotor integration during locomotion toward a target in Parkinson’s disease. Neuroscience 134(1):283–293. https://doi.org/10.1016/j.neuroscience.2005.02.050
Konczak J, Corcos DM, Horak F, Poizner H, Shapiro M, Tuite P, Volkmann J, Maschke M (2009) Proprioception and motor control in Parkinson’s disease. J Mot Behav 41(6):543–552. https://doi.org/10.3200/35-09-002
Lee EY, Cowan N, Vogel EK, Rolan T, Valle-Inclán F, Hackley SA (2010) Visual working memory deficits in patients with Parkinson’s disease are due to both reduced storage capacity and impaired ability to filter out irrelevant information. Brain J Neurol 133(9):2677–2689. https://doi.org/10.1093/brain/awq197
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Science+Business Media, LLC, part of Springer Nature
About this protocol
Cite this protocol
Lirani-Silva, E., Vitorio, R. (2022). Eye Tracking Application to Understand the Visual Control of Locomotion. In: Stuart, S. (eds) Eye Tracking. Neuromethods, vol 183. Humana, New York, NY. https://doi.org/10.1007/978-1-0716-2391-6_9
Download citation
DOI: https://doi.org/10.1007/978-1-0716-2391-6_9
Published:
Publisher Name: Humana, New York, NY
Print ISBN: 978-1-0716-2390-9
Online ISBN: 978-1-0716-2391-6
eBook Packages: Springer Protocols