Abstract
Venous thromboembolism (VTE) which includes deep vein thrombosis (DVT) and pulmonary embolism (PE) is a severe complication in critically ill patients generally affected by multiorgan disfunction associated with immobilization also prolonged.
Nowadays, VTE prophylaxis is included in the requirements of hospital accreditation and evaluation of the maintenance of standards of quality of care. ICU patients are characterized by a dynamic day-to-day variation both of thromboembolic that bleeding risk and DVT incidence in presence of thromboprophylaxis ranges between 5 and 15 %.
Patient-centered methods for the assessment of both thrombotic and bleeding risk are recommended because pre-existent factors to ICU admission, diagnosis, emerging syndromes, invasive procedures and pharmacological treatments daily induce important changes in clinical condition.
General consensus currently establishes use of heparin in pharmacological prophylaxis at the time of admission to the ICU and the temporary suspension of heparin in patients with active bleeding or severe (<50,000/cc) thrombocytopenia. Individualized thromboprophylaxis regimens were proposed but there is still no consensus based on evidence.
DVT diagnosis is not clinical but imaging-based and in each ICU data on DVT incidence (DVT diagnosed 72 h after ICU admission) should be obtained by weekly ultrasound screening standardized for the anatomical sites of compression used, taking into account the persistence of DVT-risk throughout ICU stay. A role for mechanical thromboprophylaxis by elastic stockings or pneumatic compression was reported but no general consensus was reached about its use at the best. Much work has to be done but ICU remain the last frontier for VTE prophylaxis.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Deep vein thrombosis
- Thromboembolism
- Intensive care unit
- Critical care
- Thromboprophylaxis
- Heparin
- Ultrasonography
- Thrombotic risk
- Haemorrhagic risk
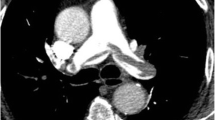
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a devastating complication for critical patients who have a baseline decrease in cardiopulmonary reserve. In six studies performed between 1978 and 2000 in medical-surgical intensive care unit (ICU) setting, autoptic diagnosis of pulmonary embolism was made in 13 (7–23) % of the 463 patients who died in ICU [1, 2] and all authors agreed on the fact that clinical suspicion was mentioned in a low minority. ICU patients with DVT have a longer duration of mechanical ventilation, ICU and hospital stay than patients without DVT even when DVT is not complicated (Fig. 1) [3, 4]. Four randomized controlled trials performed between 1981 and 2000 demonstrated the efficacy of unfractionated heparin (UH) or low molecular weight heparin (LMWH) thromboprophylaxis in ICU patients [5–8] and the 9th edition of the American College of Chest Physician’s (ACCP) Evidence-Based Clinical Practice Guidelines recommends prophylaxis of ICU patients with LMWH over no prophylaxis [9]. Nowadays venous thromboembolism (VTE) prophylaxis is incorporated into hospital accreditation and quality of care metrics all around the world.
The issue of “thromboembolism in intensive care units” deserves dedicated treatment because of some peculiar characteristics of critical patients. In this perspective we synthesize the most relevant: (a) critical patients are a heterogeneous population for thrombotic risk: in patients not receiving thromboprophylaxis was reported a DVT prevalence ranging between 10 and 80 % [10] that was usually observed in patients with major trauma or spinal cord injury, the two subpopulations at the highest risk of thrombosis. In medical-surgical ICU settings a failure rate of prophylaxis as high as 5–15 % was recently shown [11]; (b) in ICU DVT can rarely be diagnosed through clinical data: patients very often cannot communicate symptoms due to their underlying conditions, pharmacotherapy and mechanical ventilation. Signs associated with DVT such as oedema are common in the ICU setting and attributable to many other factors. Diagnosis of DVT needs imaging i.e. ultrasound screening that must be scheduled so that the cost/benefit ratio could be sustainable. (c) The individual risk stratification for DVT in ICU setting is difficult: risk assessment models for DVT diagnosis that are used for out-patients (Wells score) [12], hospitalized medical (Padua score) [13], surgical (Caprini modified score) [14] or trauma patients cannot be applied to critically ill patients. Pretest probability scores developed and validated outside ICU for diagnosis of pulmonary embolism (PE) do not correlated with clinically suspected PE in ICU [15]. In ICU patients not only risk factors such as personal or family history of VET or illness score severity at admission, but also time dependent factors due to newly acquired pathologies, iatrogen interventions or therapies concur to determine thrombotic risk which is dynamic and can change from day to day.; (d) ICU patients can also be at risk of major bleeding [16]. The balance between thrombotic and haemorrhagic risk must be evaluated daily, as it can change suddenly. In medical-surgical ICU patients on thromboprophylaxis the incidence of major bleeding was 6 % and was associated with a twofold increase of ICU and hospital mortality [17]. Dedicated strategies to improve compliance with thromboprophylaxis such as programs of continued education for physicians and nurses and /or electronic order sets and reminders are strongly recommended in ICU [11].
The goal of this review is to offer synthetic and critical knowledge on what we believe to be the main certainties and the main doubts regarding “DVT in ICU setting”.
1 How Many Deep Vein Thrombosis in ICU?
When the “DVT problem in ICU” is investigated, data must be separately analyzed according to (a) the evaluation of DVT clinically suspected or detected by ultrasound surveillance, (b) the use or not of thromboprophylaxis in ICU patients (c) the evaluation of spontaneous and/or CVC-related thrombosis. We remind that catheter-related DVT must be considered those DVT which occur within 72 h from CVC insertion. The difference between DVT prevalence and incidence is also to be taken into account.
2 The Difference Between Prevalence and Incidence of DVT in ICU
Cook et al [3] well describe the difference between prevalence and incidence of DVT in ICU: prevalence takes into account those DVTs that are diagnosed within 48–72 h from ICU admission and that started before admission either during the preceding hospital stay or from trauma or individual thrombotic risk. Data on DVT prevalence are obtainable only when an ultrasound exam for DVT is scheduled within 48–72 h from admission. DVT prevalence depends on factors preceding ICU admission and is independent of ICU quality of care.
DVT incidence in ICU shows how many DVTs are diagnosed 72 h after ICU admission and is the result of the imbalance between prothrombotic stimuli and antithrombotic defence that can occur any time during ICU stay. Indeed, observational studies showed that new-onset DVT can occur at every day independently of the length of ICU stay [4]. No ICU patient can be considered free from risk of DVT (Fig. 2).
New-onset DVT can occur at every day independently of the length of ICU stay [4]. During the prospective phase of the study tromboprophylaxis was optimized and DVT incidence decreased from 11 to 4 %, but no difference was observed on the time of occurrence between the prospective and retrospective phase
3 Criticism About Clinical and Ultrasound Diagnosis of DVT in ICU
(a) In the ICU setting, the clinical suspicion of DVT is made difficult by the fact that patients with impaired consciousness through the effect of drugs or simply through their conditions often cannot refer symptoms. Signs that are part of risk assessment models for DVT in hospitalized or out-patients are therefore not easily detectable in ICU patients. Physical examination proved to have no diagnostic utility for DVT in medical-surgical patients [18]. Venous compression ultrasonography (CUS) is the most accurate non invasive test for DVT diagnosis [19, 20], even if CUS has reduced sensitivity in patients with minimal symptoms [21, 22]. Concern about underdiagnosed DVT in the medical-surgical ICU setting is highlighted by studies showing that 10 % [16, 17] to 100 % [23] of DVTs identified by ultrasound screening were clinically unsuspected. Screening test is not recommended by guidelines for DVT prevention [24], but given the common lack of clinical symptoms and signs for DVT in critical patients, DVT diagnosis can only be made by ultrasound screening that allows strict monitoring of the changes in DVT incidence related to the different interventions adopted for prophylaxis improvement. In our opinion a scheduled ultrasound screening program would increase awareness for the need of daily assessment of individual DVT risk burden. Moreover, nowadays in the ICU setting ultrasound is part of the daily clinical assessment of patients and its use for DVT ultrasound screening does not represent a supplementary cost in term of human and tool resources. Finally, we strongly encourage the use of a standard technique for Doppler ultrasound exam through (a) the application of ultrasound compression at six fixed locations from the popliteal trifurcation to the common femoral vein, (b) the measurement of residual thrombus in mm in short axis at each of the CUS fixed locations and (c) scheduled ultrasound test once or twice/a week till discharge (Fig. 3). A standardized methodology would permit optimization of DVT follow-up [3, 4] not only during ICU and hospital stay but also after hospital discharge.
Standardization of ultrasound exams for the diagnosis of DVT is a key point and is based on (a) the definition of anatomical points on which compressive ultrasound is to be performed, (b) the measurement at of the residual thrombus in mm at each CUS point and (c) the scheduled time of ultrasound exams during ICU stay
It is to be underlined that DVT frequency varies among different studies because of heterogeneity in populations enrolled but most importantly because of the methods of surveillance used and when ultrasound screening is used, because of the frequency of ultrasound test. It is well known that an increased number of ultrasound test in a week, results in a higher number of diagnosed DVT [25]. This means that only studies reporting similar frequency of ultrasound screening are comparable. According to data reported by Cook et al [3] the best risk/benefit ratio is obtained when ultrasound screening is performed twice a week; ultrasound screening carried out less than once a week is therefore unadvisable for a correct control of DVT prophylaxis. When ultrasound screening is scheduled once or twice a week, an incidence of 5–10 % is reported in medical-surgical ICU [3, 4, 26].
4 Does Differentiating Between Symptomatic and Asymptomatic DVT in ICU Have Sence?
Early studies reported that symptomatic or asymptomatic DVT without thromboprophylaxis develops in 13–31 % of medical –surgical critically ill patients [27], whereas in ICU patients receiving LMWH the frequency of DVT at any site ranged between 5.1 and 15.5 % [11]. Due to the extreme difficulty in clinical diagnosis already cited many times, we believe that a reliable distinction between symptomatic and asymptomatic DVT is impossible in ICU settings and that the need for ultrasound screening is absolute when the issue “DVT in ICU” is investigated.
5 What About CVC-Related Thrombosis?
Central venous catheter (CVC)-related DVTs are to be considered those diagnosed within 72 h of CVC insertion. CVCs are included among time dependent acquired DVT risk factors in ICU in all dedicated studies, but some issues must be considered that differentiate CVC-related DVT from idiopathic DVT. The majority of studies on DVT in ICU investigated DVT of the lower limbs, whereas CVC-related thromboses are located in the veins of the upper limbs [28]. The veins of upper limbs are usually not evaluated during ultrasound screening except under specific clinical questions. In patients enrolled in the PROTECT study the incidence of non leg DVT diagnosed in patients with clinical signs or symptoms that prompted ultrasound screening was 2 % [29]. Most importantly, CVC related DVT are mainly due to endothelial damage and in the pathophysiology of CVC-related DVT the role of other risk factors can be different when compared to the role played in idiopathic thrombosis. This is very true when we consider the cannula-related DVT during Extra Corporeal Membrane Oxygenation (ECMO) treatment: the cannulas used in ECMO, expecially the venous cannulas, have a diameter very close to that of the affected vessels with a marked increase in the endothelial damage [30]. Considering all the above points, we believe that CVC-related DVT in ICU deserves dedicated treatment that is beyond the goals of this review.
6 What Is Important to Know About DVT Incidence in ICU?
Data on DVT frequency are extensively reported in literature and according to recent trials DVT incidence in ICU patients under thromboprophylaxis ranges between 5 and 15 %; this means that if in an ICU DVT incidence is above 15 %, an optimization of thromboprophylaxis is called for. Further, it is no longer acceptable for an ICU not to record and not to report the relative data on DVT incidence. A retrospective investigation of what has taken place in the past is necessary in order to form the basis for creating a quality improvement program for the future [4, 26].
6.1 Risk Factors for DVT in ICU
Recognized risk factors for DVT are related to one or more elements of Virchow’s triad (flow stasis, vessel injury and hypercoagulability). In ICU patients, flow stasis plays a major role because of immobility due to trauma, use of sedatives and neuromuscular block that markedly decreases the velocity of limb venous blood flow [31, 32]. In addition, mechanical ventilation and abdominal hypertension, found in many situations, decrease venous return of blood to the heart and can further facilitate the stasis of venous blood in veins of the lower limbs [33] Vessel injuries are mainly due to catheter insertion in central and peripheral veins and/or surgical interventions. Finally, hypercoagulability can be due to sepsis, renal failure or hemodynamic impairment with administration of vasoactive drugs. Under such pathophysiological conditions, the occurrence of additional DVT risk factors during ICU stay added to risk factors present at admission can precipitate thrombosis.
Figure 4 shows that according to the triad of Virchow in ICU setting, several factors occur contemporarily in each patient that facilitate flow stasis and/or endothelial damage and/or hypercoagulabity. We should wonder why not all ICU patients develop DVT. Really, humans are endowed with a very good fibrinolytic system.
To calculate the risk for DVT in ICU patients a risk assessment model must be used that takes into account not only the thrombophilic profile of each patient at ICU admission with different items for medical, surgical and trauma patients, but also transient risk factors acquired during ICU stay, the major part related to iatrogenic interventions. In the ICU setting thrombofilic profile is not static, but dynamic; the persistence of DVT occurrence shown in all studies performed in ICU despite an extensive application of thromboprophylaxis, can be partly due to the variability of the thrombotic threshold that is hardly detectable compared with a fixed dosage of anticoagulants. ICU has been called the last frontiere of prophylaxis” [34].
7 DVT Risk Assessment Model in ICU-One for Each ICU?
-
pre-existent risk factors-a proposal for calculating DVT risk at admission
Pre-existent risk factors are in major part common to the risk factors that in recent years have been included in models for the assessment of thrombotic risk in hospitalized medical and surgical patients. Among those available in literature, the Padua score for medical patients [13] and the Caprini [14] modified score for surgical patients, also applied in the PROF-ETEV study [35] are the most extensively used and we propose that they would be applied in the evaluation of individual thrombotic risk at ICU admission. Remarkably, both Padua and Caprini modified models classify as at high thrombotic risk those patients who have a positive history for TEV, that was also selected together with end-stage renal failure as strongest pre-existent risk factor in ICU medical surgical setting by Cook et al 2005. Moreover, chronic cardiac and/or respiratory failure that select ICU patients at very high DVT risk are identified by Padua and Caprini scores [36]. In ICU intensivists have too short time to do too many things and having an electronic format for thrombotic scoring to complete could be a good methodological approach for the standardized calculation of individual thrombotic profile. In ICU patients the thrombotic risk scoring at admission would not have the goal to decide the start of anticoagulation, but could help to quickly calculate a baseline individual risk threshold which should be daily modified according with the evolution of clinical conditions.
-
specific of admission diagnosis
Dedicated score are available for hospitalized medical, surgical o trauma patients each taking into account DVT risk factors that play the major role in that specific subpopulation such as underlying inflammatory conditions, minor or major surgery due or not to cancer, number and kind of injured bones. However when patients are admitted to ICU beyond the mentioned risk factors, hemodynamic instability with the need of vasopressor therapy and/or compromised ventilation with the need of mechanical ventilation complicate the clinical picture of the majority of patients. These acute illness are always associated with a very high risk of thrombosis and determine per se the immediate start of anticoagulation [36].
-
newly acquired and not specific of admission diagnosis
As a whole newly acquired risk factors in ICU can be differentiated in those related to the evolution of the clinical conditions, or secondary to pharmacological or invasive or surgical iatrogenic interventions, as below shown, or rather according to the component of the Virchow’s triad they mainly act on.
-
(a)
Related to onset of new medical pathologies
Sepsis, kidney failure, systemic hypotension-hypoperfusion, abdominal hypertension
-
(b)
Related to procedures
surgical procedures, peripheral or central catheter insertion
-
(c)
Related to mechanical ventilation
-
(d)
Related to pharmacological therapies-amine neuromuscular blockers
-
(e)
Related to hemoderivate administration.
Risk factors described according to the effect on each component of the Virchow’s triad
-
Negative action on flow stasis:
-
Abdominal hypertension, mechanical ventilation, amine, neuromuscular blockers
-
Negative action on hypercoagulability:
-
Sepsis, renal failure, amine, hemoderivate, erythropoietin
-
Negative action on endothelium:
-
For direct endothelium damage:surgical intervention, CVC
-
For endothelium dysfunction: sepsis renal failure amine
In recent years a protective effect of statins on DVT was reported and related with their positive effect on endothelial dysfunction; the clinical relevance of these data for thromboprophylaxis in ICU needs dedicated studies [37].
We think that when the pathophysiologic mechanisms of the different DVT risk factors is considered, the dynamic change in individual thrombotic threshold would be better assayed during ICU stay. Dedicated studies are needed to understand whether this approach could have clinical relevance supporting the individual adjustment of pharmacological and/or mechanical prophylaxis.
No “official” risk assessment model is available for ICU patients. Given the high number of risk factors for DVT that may differently coexist and concur to lower the threshold of the risk of thrombosis, risk factors are reported in different studies as having different impact. It is always difficult to apply recommendations by trials or meta-analysis to real clinical practice but it is even more difficult in ICU setting.
We suggest that a specific model should be prepared in each ICU according to the risk factors that characterize that specific population taking into account but not rigidly applying the indications given in the literature.
7.1 DVT Prophylaxis in ICU
-
(A)
Pharmacological prophylaxis is recommended in medical-surgical ICU patients
Starting from the first trial by Kapoor et al in 1999 [7] that reported a 50 % risk reduction of screening detected VTE vs placebo, in medical-surgical ICU patients randomly selected and treated with UFU 5,000 units subcutaneously twice daily, in these decades an evidence-based efficacy of pharmacological UFH or LVWH prophylaxis in reducing the risk of VTE in ICU patients has been clearly shown [11, 37]. In a recent systematic review and meta-Analysis of randomized trials on the efficacy and safety of any heparin (UFH or LMWH) thromboprophylaxis vs no anticoagulant prophylaxis, that enrolled 7,226 medical surgical ICU patients, any heparin compared with no heparin was associated with a 50 % lower risk of DVT and of PE with a number needed to prophylax to prevent one DVT of 20, using an assumed control risk of 10 %, and to a number needed to prophylax to prevent one PE of 52, using an assumed control risk of 4 %[38]. Heparin thromboprophylaxis did not influence the risk of major bleeding or mortality.
Laboratory-based variables to define optimal thromboprophylaxis such as thrombin generation and thromboelastometric assay of hypercoagulability have been proposed but dedicated studies are needed to understand how and whether use these data in clinical practice [37].
-
(B)
Which heparin?
LWMHs are prepared from UFH by different chemical or enzymatic processes and we know that they have different physical, biochemical and pharmacological properties but we do not know whether this translates in different clinical outcome, specifically in ICU setting. In absence of comparative data among different LWMH, each LWMH should be used at the recommended doses when efficacy and safety data exist [39]. The major advantage of UFH over LMWH is that it avoids a renal clearance that allows UFH administration in patients with impaired renal function. LMWH are associated with a reduced likelihood of heparin-induced thrombocytopenia, that requires administration only once-daily and is commercially available in a unit dose. All the three randomized controlled trials performed between 2000 and 2011 that compared UFH with LMWH for VTE prophylaxis in ICU patients, did not find significant difference in the DVT rate between the two groups [40–42]. Only the multicentric Prophylaxis for Thromboembolism in Critical Care Trial (PROTECT) reported a significant lower incidence of PE (2.3 vs 1.3 %, p = 0.01) in the dalteparin group [43]. Pooled outcomes from the meta-analysis of Alhazzani et al are in agreement with the PROTECT’s results that LMWH was not associated with a lower risk of DVT, but with a reduction of asymptomatic and symptomatic pulmonary embolism when compared with UFH. The risk of DVT, major bleeding, mortality and HIT was similar in the two groups [38].
A recent systematic review with meta-analysis and trial sequential analysis by Beitland et al [44] that included also ICU patients with trauma showed that LMWH compared with UFH reduced the risk of any DVT (RR 0.84,95 % CI 0.71–0.98), p = 0.03) and resulted in a net clinical benefit. There were no statistically significant differences in the risk of any PE, major bleeding or mortality.
The different findings reported by these two meta-analyses highlight the importance of a critical interpretation of all data reported by meta-analysis of trials performed in ICU patients when we want to transfer reported results into clinical practice. We should consider whether and how much the characteristics of ICU patients enrolled in studies or meta-analysis fit with those of our ICU.
8 Heparin Thromboprophylaxis in High Risk Subgroups
8.1 Sepsis
Heparin at prophylactic dosage can significantly reduce 28-day mortality in patients with severe sepsis i.e. sepsis complicated by organ dysfunction and tissue hypoperfusion; the use of heparin for sepsis is not associated to an increased risk of bleeding (Wang et al Critical Care 2014;18:563) [45]. Heparin has no effect on 28-day mortality in patients with no severe sepsis. The positive effect of heparin on mortality in ICU patients with severe sepsis can be explained by (a) the reduced occurrence of deep venous thromboembolism, (b) the negative modulation of coagulation activation and (c) the heparin anti-inflammatory effect through the reduction of inflammatory mediators (histamine) and the increase in TFPI release.
8.2 Renal Failure
Patients with renal failure have an increase of both thrombotic and hemorrhagic risks, with the transitional prevalence of one over the other depending on underlying nephropathies (nephrotic or nephritic syndrome), hemodialysis treatment, eritropoietin administration and associated comorbidities. End-stage renal failure was selected with a positive familial or individual history of VET as the two strongest risk factors for DVT pre-existent to ICU admission in medical-surgical critical ill patients [3]. No specific indications are reported about the role of renal failure in the thrombotic risk stratification by the algorithm proposed by Laport and Mismetti [36] that is dedicated to medical critically ill patients and by Caprini modified score [14] that is used in the surgical setting. It must be underlined that beyond the effect on haemostatic balance, renal failure signifies a reduction of creatinine clearance and often results in the anticoagulant therapy to be stopped or in its excessive reduction without proven data on possible bioaccumulation. Heparin bioaccumulation would be investigated through the determination of anti-Xa units after the third heparin dose when the steady state has been achieved. Regarding prophylaxis, data on bioaccumulation are reported only for enoxaparin that should be used at reduced dose (30 mg once daily) for VET prophylaxis. Therapeutic doses of enoxaparin were associated with increased in major bleeding in patients with a creatinine clearance of 30 ml/min or less compared with UFH (8.3 % vs 2.4 %,95 % CI 1.78–8.45) in a meta-analysis of 12 studies that had enrolled about 5000 patients [39].
9 What About Obesity?
No doubts remain about the role of obesity as independent risk factor for DVT in all hospitalized patients and also in ICU patients, but whether or not a patient with a BMI >30 need a higher dosage of heparin is still a matter of debate [46]. Increasing BMI demonstrates the strongest relationship with thromboprophylaxis failure, suggesting an underdosing of anticoagulants with a fixed dose regimen (36a). Due to the lability of thrombotic threshold in ICU patients, we suggest that in these patients heparin concentration should be monitorized by the dosage of anti Xa levels. The decision to increase heparin dosage would be taken account of the level of global individual DVT risk.
10 When the Bleeding Risk Is Not Acceptable for Prophylaxis-Major Bleeding
The absolute contraindication to anticoagulation in patients at high risk for DVT are active bleeding and severe thrombocytopenia (<50000/cc); both are transient controindications and prophylaxis or therapy must be started immediately after these controindications are corrected [9]. All other clinical situations that are associated with increased risk of bleeding do not represent an absolute controindication for heparin prophylaxis but a daily individual evaluation of bleeding risk is needed in ICU patients. According to what indicated in the paragraph for the evaluation of the thrombotic risk, we think that the use of bleeding risk assessment models proposed for hospitalized medical patients could be also applied for ICU patients [47]; to answer to a standardized electronic form for bleeding scoring would shorten the dedicated time and undoubtedly would reduce the intra and interassay variability.
11 Only Heparin as Anticoagulant for DVT Prophylaxis in ICU?
Recently, new oral anticoagulants (NAO) that are direct thrombin or factor Xa inhibitors, have become available for primary and secondary prevention of venous thrombosis and of embolization in atrial fibrillation. None of the new anticoagulants have been studied in the ICU population and the results of the MAGELLAN trial, rivaroxaban vs enoxaparin,[48] and the ADOPT trial, apixaban vs enoxaparin,[49] studies performed in acute medical illness cannot be transferred tout-court to ICU setting. At the moment the lack of data on efficacy and safety of NAO in ICU setting and of antidote for controlling bleeding, are against the use of NAO in critical ill patients.
12 Doubts on the Role of Mechanical Thromboprophylaxis in ICU Patients
Mechanical prophylaxis includes graduated compression stocking (GCS) and intermittent pneumatic compression (IPC) devices; however, for their use in ICU setting, general agreement only exists for patients at very high risk for VET in association with pharmacological prophylaxis or in patients for whom contraindications to pharmacological prophylaxis exists. These indications are reported in ACCP guidelines. Vignon et al [50] randomized ICU patients with high risk of bleeding to IPC plus GCS or GCS alone and found no difference in the DVT rate between the two groups (5,6 vs 9.2 %).In only one two-phase study that examined the effect of an educational program on the implementation of DVT prophylaxis in medical-surgical-trauma patients, the increased use of graduated compression stockings combined with pharmacological prophylaxis was associated with a significant reduction in DVT incidence during ICU stay from 11.6 to 4.7 %, p = 0.017despite no changes in the LWMH dosage and in the use of pneumatic mechanical compression [4]. These findings had had scarce relevance in the scientific community, but they sound not surprising taking into account the pathophysiology of DVT (i.e. Virchow’s triad): ICU patients have a marked decrease in venous blood flow velocity because they are immobile, under sedation and/or often ventilated. When a neuromuscolar block is activated the venous blood velocity falls to about zero. In these unfavourable conditions the application of graduated compression stockings can be effective in increasing blood velocity in veins of the lower limbs so that the key event for the start of thrombus formation can be limited, especially when anticoagulation is administered contemporarily [51]. Moreover, the daily application of compression stockings is necessarily associated with an increased passive mobilization of ICU patients.
Recently two randomized controlled trials analyzed the efficacy of pneumatic compression in reducing thrombotic risk in medical surgical ICU patients when compared with no anticoagulation and showed that pneumatic compression significantly reduced DVT (3.8 vs 19.28 %, p < 0.0), PE (0 vs 9.64 %, p < 0.01), separately analyzed in the first study, and VTE from 7.2 to 4.8 % in the second study [52, 53].
13 Strategies to Improve Thromboprophylaxis Compliance in ICU
Nowadays DVT incidence during ICU hospital stay is used as a marker of quality care and given the epidemiology and the clinical impact of DVT in ICU population, clear evidence exists that DVT prophylaxis must be optimized by dedicated educational programs. On the contrary, the passive dissemination of guidelines has little effect on the improvement and maintenance of DVT prophylaxis prescription [54]. In ICU setting the presence of combined active and dynamic clinical conditions influencing the attention of the medical staff, together with the complexity and heterogeneity of medical in-patients, hinder the systematic application of prophylaxis. Remarkably, Ho et al [55] showed that omission of thromboprophylaxis within the first 24 h following ICU admission was associated with an increased risk of mortality in 175,665 critically ill adult patients admitted to 134 ICUs in Australia and New Zealand between 2006 and 2010, despite patients with early omission of prophylaxis being associated with a slightly lower acuity of illness (mean APACHE [Acute Physiology and Chronic Health Evaluation] III model predicted mortality, 13 % vs 14 %; P 5.001). The estimated attributable mortality effect of omitting early prophylaxis was more relevant in patients with high acuity of illness such as multiple trauma, sepsis, cardiac arrest, and pre-existing metastatic cancer.
A recent review on venous thromboembolism prophylaxis [11] in critically ill patients clearly summarizes that studies performed all around the world- Asia, Australia and New Zeland, China, Japan, Spain and United States- have shown that more than 80 % ICU patients received appropriated prophylaxis; principal barriers to prophylaxis are fear of bleeding and underestimated risk of thrombosis.
Among studies based on the activation of educational programs for physicians and nurses, a three-phase prospective longitudinal study investigated the implementation of pharmacological prophylaxis in medical-surgical ICU by minimizing errors of omission through a 1-year period of interactive multidisciplinary educational in-services, verbal reminders to ICU team, computerized daily nurse recording of prophylaxis, weekly graphic feedback, publicly displayed graphic feedback on group performance. At the end of the educational period, days of heparin administration increased from 60 % observed under baseline period (phase 1) to 100 % (p < 0.01) [56]. The use of a daily quality round checklist (QRC) including DVT prophylaxis in a surgical ICU during a 2-year program with routine implementation of QCR, was associated to a final DVT prophylaxis compliance of 98 % [57].
Boddi et al [4] showed that a-1 year ICU-based educational program aimed at optimization of pharmacological and mechanical prophylaxis, combined with a twice a week scheduled ultrasound screening, was significantly associated with a marked decrease in DVT incidence from 11.6 to 4.7 %.
Several studies have demonstrated that electronic reminders associated with educational programs clearly improved the use of both pharmacological and mechanical DVT prophylaxis through the direct involvement of ICU clinicians and daily assessment of prophylaxis prescription [11]. Recently, an Italian study by Peris’s group [26] showed that multiple interventions aimed at improving DVT prophylaxis rate ( electronic alert for automatic pharmacological prophylaxis activation at ICU admission, nurse protocol with check list including graduated compression stockings application to be applied within 12 h from ICU admission) can reduce DVT incidence to low levels (2.6 %) in high risk ICU patients and result in a decrease in ICU length of stay. Most importantly, the 4-year-long quality improvement program of DVT prophylaxis was sustained and was active in a busy 10-bed mixed trauma, medical and surgical ICU despite the high turnover of patients.
14 Additional Problems Due to the Increased Dosage of Heparin from Prophylaxis to Therapy
The diagnosis of DVT is associated with the need of increasing dosage of anticoagulants and a higher risk of over dosing in patients with impaired renal function, peripheral hypoperfusion because of low cardiac output, hypotension and vasopressor use, altered binding to albumin, acute phase reactants and generalized edema. Risk factors that may be associated with under dosing are multiple organ dysfunction, high body mass index and the use of vasodepressor.
To monitor the LWMH anticoagulant effect the dosage of anti-Xa levels is used but a correlation between bleeding and thrombosis and anti Xa levels was not clearly proved (r na). Indeed, anti-factor Xa measure a drug concentration, not an effect [37]. Recently, the use of a weight-based LMWH dosing regime has been reported to avoid subtherapeutic anti-factor Xa levels in critically ill population [58]. In clinical conditions with risk of over or underdosing of heparin, the use of mechanical prophylaxis should be optimized and additional risk of bleeding such as thrombocytemia, antiplatelet therapy and surgical intervention that should be delayed whenever possible.
15 Key Messages
Main Certainties
-
(a)
ICU patients are at high risk for DVT thrombosis and ICU population is characterized by a dynamic day-to-day variation in the thrombotic threshold and bleeding risk. Pharmacological prophylaxis by heparin should be immediately start at ICU admission and stopped only in those few patients at very high bleeding risk, till the risk is not resolved (Fig. 5).
-
(b)
In each ICU data on DVT prevalence and incidence obtained by scheduled ultrasound screening should be available and regularly (monthly) updated.
-
(c)
Electronic form for individual thrombotic and bleeding risk assessment models should be available in every ICU and used daily. The models for calculating thrombotic risk would consider the additive effect of the different risk factors on each of three components of the Virchow‘s triad. The application of pharmacological and mechanical prophylaxis should be optimized by individual checklist-form for intensivists and nurses.
Doubts
-
(a)
Individualized thromboprophylaxis regimens in ICU is invoked, expecially in renal failure and obesity, but how to monitor is still a matter of debate.
-
(b)
A role for mechanical thromboprophylaxis in ICU is proved, but how to standardize its use at the best is a question to be addressed.
References
Geerts W, Selby R (2003) Prevention of venous thromboembolism in the ICU. Chest 124(6 Suppl):357S
McLeod AG, Geerts W (2011) Venous thromboembolism prophylaxis in critically ill patients. Crit Care Clin 27(4):765–780
Cook D, Crowther M, Meade M et al (2005) Deep vein thrombosis in medical-surgical critically ill patients: prevalence, incidence, and risk factors. Crit Care Med 33(7):1565–1571
Boddi M, Barbani F, Abbate R, Bonizzoli M, Batacchi S, Lucente E, Chiostri M, Gensini GF, Peris A (2010) Reduction in deep vein thrombosis incidence in intensive care after a clinician education program. J Thromb Haemost 8:121–128
Moser KM, Le Moine JR, Natchwey FJ, Spragg RG (1981) Deep venous thrombosis and pulmonary embolism. Frequency in respiratory intensive care unit. JAMA 246(13):1422–1424
Cade JF (1982) High risk of the critically ill for venous thromboembolism. Crit Care Med 10(7):448–450
Kapoor M, Kupfer YY, Tessler S (1999) Subcutaneously heparin prophylaxis significantly reduces the incidence of venous thromboembolic events in critically ill. Crit Care Med 27(Suppl 12):A69
Fraisse F, Holzapfel L, Couland JM et al (2000) The Association of Non-University Affiliated Intensive Care Specialist Physician of France. Naproparin in the prevention of deep vein thrombosis in acute decompensated COPD. Am J Respir Crit Care Med 161(4, Pt 1):1109–1114
Kahn SR, Lim W, Dunn AS, et al (2012) American College of chest physicians. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed. American College of Chest Physicians. Evidence-Based Clinical Practice Guidelines. Chest 141(2, Suppl):e1955–e2265
Geerts WH, Pineo GF, Bergqvist D, Lassen CCW, Ray J (2004) Prevention of venous thromboembolism:the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest 126:338S–400S
Boonyawat K, Crowther MA (2015) Venous thromboembolism prophylaxis in critically ill patients. Semin Thromb Hemost 41:68–74
Wells PS, Owen C, Doucette S, Fergusson D, Tran H (2006) Does this patient have deep vein thrombosis? JAMA 295:199–207
Barbar S, Noventa F, Rossetto V, Ferrari A, Brandolin B, Perlati M et al (2010) A risk assessment model for the identification of hospitalized medical patients at risk for venous thromboembolism: the Padua Prediction Score. J Thromb Haemost 8(11):2450–2457
Caprini JA, Arcelus JI, Reyna JJ (2001) Effective risk stratification of surgical and not surgical patients for venous thromboembolic disease. Semin Hematol 38:12S–19S
Katsios CM, Donadini M, Meade M, Mehta S, Granton J, Kutsiogiannis J et al (2014) Prediction scores do not correlate with clinically adjudicated categories of pulmonary embolism in critically ill patients. Can Respir J 21(1):36–42
Williamson DR, Albert M, Heels-Ansdell D, Arnold DM, Lauzier F, Zarychanski R et al (2013) Thrombocytopenia in critically ill patients receiving thromboprophylaxis. Chest 144(4):1207–1215
Lauzier F, Arnold DM, Rabbat C, Heels-Ansdell D, Zarychanski R, Dodek P et al (2013) Risk factors and impact of major bleeding in critically ill patients receiving heparin thromboprophylaxis. Intensive Care Med 39:2135–2143
Crowther MA, Cook DJ, Griffith LE, Devereaux PJ, Rabbat CC, Clarke FJ, Hoad N, McDonald E, Meade MO, Guyatt GH, Geerts WH, Wells PS (2005) Deep venous thrombosis: clinically silent in the intensive care unit. J Crit Care 20(4):334–340
Kearon C, Ginsberg JS, Hirsh J (1998) The role of venous ultrasonography in the diagnosis of suspected deep vein thrombosis and pulmonary embolism. Ann Intern Med 129:1044–1049
Blann AD, Lip GYH (2006) Venous thromboembolism. BMJ 332:215–219
Shellong SM, Beyer J, Kakkar AK, Halbritter K, Eriksson BI, Turpie ACG et al (2007) Ultrasound screening for asymptomatic deep vein thrombosis after major orthopedic surgery: the VENUS study. J Thromb Haemost 5:1431–1437
Cook DJ, Rocker G, Meade M, Guyatt G, Geerts WH (2005) Andersond, et al. PROTECT Investigators; Canadian Critical Care Trials Group. Prophylaxis of Thromboembolism in Critical Care (PROTECT) Trial: a pilot sudy. J Crit Care 20:364–372
Hirsch DR, Ingenito EP, Goldhaber SZ (1995) Prevalence of deep venous thrombosis among patients in medical intensive care. JAMA 274:335–337
The Intensive Care Society (2008) Guidelines for Venous Thromboprophylaxis in Critical Care. http://www.ics.ac.uk/icmprof/downloads/2008102336_Thromboprophylaxis%2027%2010%2008.pdf
Pierce CA, Haut ER, Kardooni S, Chang DC, Efron DT, Haider A, Pronovost PJ (2008) Cornwell EE 3rd.Surveillance bias and deep vein thrombosis in the national trauma data bank; the more we look, the more we find. J Trauma 64:932–936
Boddi M, Cecchi A, Bonizzoli M, Barbani F, Franci A, Anichini V, Batacchi S, Parodo J, Gensini GF, Peris A (2014) Follow-up after four-year quality improvement program to prevent inferior limb deep vein thrombosis in intensive care unit. Thromb Res 134(3):578–583
Geerts W(1), Cook D, Selby R, Etchells E (2002) Venous thromboembolism and its prevention in critical care. J Crit Care 17(2):95–104
Bonizzoli M, Batacchi S, Cianchi G, Zagli G, Lapi F, Tucci V et al (2011) Peripherally inserted central venous catheters and central venous catheters related thrombosis in post-critical patients. Intensive Care Med 37(2):284–289
Lamontagne F, McIntyre L, Dodek P, Heels-Ansdell D, Meade M, Pemberton J et al (2014) Nonleg venous thrombosis in critically ill adults: a nested prospective cohort study FREE.JAMA. Intern Med 174(5):689–696
Migliaccio ML, Zagli G, Cianchi G, Lazzeri C, Bonizzoli M, Cecchi A, Anichini V, Gensini GF, Peris A (2013) Extracorporeal membrane oxygenation in brain-death organ and tissues donors: a single-centre experience. Br J Anaesth 111(4):673–674
Mammen EF (1992) Pathogenesis of venous thrombosis. Chest 102:640S–644S
Miranda AR, Hassouna HI (2000) Mechanisms of thrombosis in spinal cord injury. Hematol Oncol Clin North Am 14:401–416
Ibrahim EH, Irequi M, Prentice D, Sherman G, KollefMH SW (2002) Deep vein thrombosis during prolonged mechanical ventilation despite prophylaxis. Crit Care Med 30:771–774
Cook DJ, Crowther MA, Geerts WH (2005) On the need for a workshop on venous thromboembolism in critical care. J Crit Care 20(4):306–308
Garcia-Olivares P, Guerrero JE, Galdos P, Carriedo D, Murillo F (2014) Rivera A.PROF-ETEV study: prophylaxis of venous thromboembolic disease in critical care units in Spain. Intensive Care Med 40:1698–1708
Laporte S, Mismetti P (2010) Epidemiology of thrombotic risk factors:the difficulty of using clinical trials to develop a risk assessment model. Crit Care Med 38(2 Suppl):S10–S17
Welsby I, Ortel T (2015) Is the time for individualized thromboprophylaxis regimens in ICU? Crit Care Med 43:500–501
Alhazzani W, Lim W, Jaeschke RZ, Murad MH, Cade J, CooK DJ (2013) Heparin thromboprophylaxis in medical-surgical critically ill patients:a systematic review and meta-analysis of randomized trials. Crit Care Med 41(9):2088–2098
Rajasekhar A, Beyth R, Crowther MA (2012) Newer anticoagulants in critically ill patients. Crit Care Clin 28:427–451
De A, Roy P, Garg VK, Pandey NK (2010) Low-molecular-weight –heparin and unfractionated heparin in prophylaxis against deep vein thrombosis in critically ill patients undergoing major surgery. Blood Coagul Fibrinolysis 21(1):57–61
Cook D, Meade M, Guyatt G et al (2011) PROTECT Investigators for the Canadian Critical Care Trials Group and the Austalian and New Zeland Intensive Care Society Clinical Trials Group. Deltaparin versus unfractionated heparin in critically ill patients. N Engl J Med 364(14):1305–1314
Goldhaber SZ, Kett DH, Cusumano CJ et al (2000) Low molecular weight heparin versus minidose unfractionated heparin for prophylaxis against venous thromboembolism in medical intensive care unit patients: A randomized controlled trial. J Am Coll Cardiol 35(suppl):325 A
Lin W, Meade M, Lauzier F, Zarychanski R, Mehta S (2015) Lamontagne F for the PROTECT Trial Group. Failure of anticoagulant thromboprophylaxis:risk factors in medical-surgical critically ill patients. Crit Care Med 43:4001–4410
Beitland S, Sandven I, Kjærvik LK, Sandset PM, Sunde K, Eken T (2015) Thromboprophylaxis with low molecular weight heparin versus unfractionated heparin in intensive care patients: a systematic review with meta-analysis and trial sequential analysis. Intensive Care Med [Epub ahead of print]
Wang C, Chi C, Guo L, Wang X, Sun J, Liu S et al (2014) Heparin therapy reduces 28-day mortality in adult severe sepsis patients: a systematic review and meta-analysis. Crit Care 18:563–572
Severinsen MT, Kristensen SR, Johensen SP et al (2009) Anthropometry, body fat, and venous thromboembolism.A Danish follow-up study. Circulation 120:1850–1857
Decousus H, Tapson VF, Bergmann JF, Chong BH, Froehlich JB, Kakkar AK (2011) Factors at admission associated with Bleeding risk in medical patients.Findings from the IMROVE Investigators. Chest 139:69–79
Cohen AT, Spiro TE, Spyropoulos AC, MAGELLAN Steering Committee (2013) Rivaroxaban for thromboprophylaxis in acutely ill medical patients. N Engl J Med 368(20):1945–1946. doi:10.1056/NEJMc1303641
Goldhaber SZ(1), Leizorovicz A, Kakkar AK, Haas SK, Merli G, Knabb RM, Weitz JI (2011) ADOPT trial investigators. N Engl J Med. 365(23):2167–2177. doi:10.1056/NEJMoa1110899
Vignon P, Dequin PF, Renault A et al (2013) Clinical Research in Intensive Care and Sepsis Group ( CRICS Group). Intermittent pneumatic compression to prevent venous thromboembolism in patients at high risk of bleeding hospitalized in intensive care units: the CIREA1 randomized trial. Intensive Care Med 39(5):872–880
Cipolle MD, Wojcik R, Seislove E, Waaser T, Pasquale MD (2002) The role of surveillance duplex scanning in preventing venous thromboembolism in trauma patients. J Trauma 52:453–462
Zhang C, Zeng W, Zhou H et al (2011) The efficacy of intermittent pneumatic compression in the prevention of venous thromboembolism in medical critically ill patients. Zhongguo Wei Zhong Bing Ji Jiu Yi Xue 23(9):563–565
Arabi YM, Khedr M, Dara SI et al (2013) Use of intermittent pneumatic compression and not graduated compression stockings is associated with lower incident VTE in critically ill patients: a multiple propensity score analysis. Chest 144(1):152–159
Sharif-Kashani B, Shahabi P, Raeissi S, Behzadnia N, Shoaraka A, Shahrivari M et al (2012) ProphylAxis for VenouS ThromboembolIsm in hospitalized patients: the MASIH study. Clin Appl Thromb Hemost 18(5):462–468
Ho KM, Chavan S, Pilcher D (2011) Omission of early thromboprophylaxis and mortality in critically ill patients: a multi center registry study. Chest 140(6):51–57
McMullin J, Cook D, Griffith L et al (2006) Minimizing errors of omission: behavioural re-enforcement of heparin to avoid venous emboli:the BEHAVE study. Crit Care Med 8(1):121–128
Teixera PG, Inaba K, Dubose J et al (2013) Measurable outcomes of quality improvement using a daily quality rounds checklist:two year prospective analysis of sustainability in a surgical intensive care unit. J Trauma Acute Care Surg 75(4):717–721
Robinson S, Zincuk A, Larsen UL et al (2013) A comparative study of varying doses of enoxaparin for thromboprophylaxis in critically ill patients:A double-blinded, randomized controlled trial. Crit Care 17:R75–R79
Crowther MA, Cook DJ (2008) Thromboprophylaxis in medical-surgical critically ill patients. Curr Opin Crit Care 14:520–523
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Boddi, M., Peris, A. (2016). Deep Vein Thrombosis in Intensive Care. In: Islam, M. (eds) Thrombosis and Embolism: from Research to Clinical Practice. Advances in Experimental Medicine and Biology(), vol 906. Springer, Cham. https://doi.org/10.1007/5584_2016_114
Download citation
DOI: https://doi.org/10.1007/5584_2016_114
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22107-6
Online ISBN: 978-3-319-22108-3
eBook Packages: MedicineMedicine (R0)