Abstract
The variety of brain tumors with different histology, localization, age distribution, and prognosis might be confusing. The WHO Classification of Tumours of the Central Nervous system (2007) includes more than 100 different entities (Louis et al. 2007). The comparison of primary brain and CNS tumors by site and by histology facilitates a first insight (Ostrom et al. 2014). Moreover, this reflects the incidence rates of specific brain tumors. Besides metastatic tumors of the CNS, meningeal tumors and glioma account for more than 60 % of all primary brain tumors. Regarding malignant tumors, gliomas even represent 80 % of all primary brain tumors. From 45 years of age and older, meningioma is the most frequent and glioblastoma the second most frequent brain tumor. In children and adolescents, pilocytic astrocytoma and embryonal tumors are more relevant (Ostrom et al. 2014).
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 Overview
The variety of brain tumors with different histology, localization, age distribution, and prognosis might be confusing. The WHO Classification of Tumours of the Central Nervous system (2007) includes more than 100 different entities (Louis et al. 2007). The comparison of primary brain and CNS tumors by site and by histology facilitates a first insight (Ostrom et al. 2014). Moreover, this reflects the incidence rates of specific brain tumors. Besides metastatic tumors of the CNS, meningeal tumors and glioma account for more than 60 % of all primary brain tumors. Regarding malignant tumors, gliomas even represent 80 % of all primary brain tumors. From 45 years of age and older, meningioma is the most frequent and glioblastoma the second most frequent brain tumor. In children and adolescents, pilocytic astrocytoma and embryonal tumors are more relevant (Ostrom et al. 2014).
Taken together, this illustrates that gliomas besides brain metastases are the most challenging entities in adult neurooncology.
Another important point is the differentiation of extra- and intracerebral localization of brain tumors. This usually allows an early distinction between meningiomas and gliomas or brain metastasis. As the clinical management differs substantially, this radiological differentiation is important. Small meningiomas in uncomplicated locations might not need an early histological diagnosis and can be followed by MRI scans. On the other hand, gliomas or brain metastasis usually need an immediate histological diagnosis. Further, the early radiological differentiation between gliomas, metastasis, and lymphomas is equally essential as the clinical management differs. For primary CNS lymphomas, steroids should be avoided before histological diagnostics and have traditionally been preferred over resection (Weller et al. 2012a). If brain metastases are suspected, systemic diagnostics are essential, and brain surgery may not always be necessary.
The current WHO classification from 2007 tries to indicate the prognosis of primary brain tumors by grading tumors from I° (benign) to IV° (malignant) primarily based on morphology (Louis et al. 2007). However, it is clear that the progress in molecular analyses will profoundly alter and refine this classification. In the future, prognostic and predictive markers and profiles will have practical importance for the vast majority of patients. Accordingly, a number of established molecular markers will be integrated in the upcoming WHO classification (Louis et al. 2014; Weller et al. 2012b, 2013; Wick et al. 2014).
In this chapter, we will focus on glioma, lymphoma, and brain metastasis.
2 Clinical Management
As the location of brain tumors is variable, the clinical presentation can be heterogeneous. Neurological or neuropsychological deficits, epileptic seizures, and symptoms of increased intracranial pressure are guiding symptoms. Symptomatic treatment includes, but is not limited to, anticonvulsive drugs for symptomatic epilepsy and dexamethasone for the treatment of symptomatic peritumoral edema (Soffietti et al. 2010; Weller et al. 2012c, 2014).
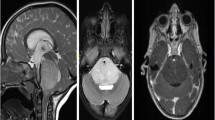
After medical history taking and the neurological examination, MRI of the brain with contrast-enhancing agent is the most important diagnostic procedure. Lumbar puncture to allow the evaluation of the cerebrospinal fluid (CSF) can be helpful in primary CNS lymphoma where tumor cells or tumor-specific molecular alterations can be detected in CSF or in germ cell tumors where elevated amounts of AFP or β-HCG can be found. In almost all other cases, the diagnosis should be confirmed via a stereotactic biopsy or, when appropriate, via resection. Despite all innovative imaging, the procurement of tumor tissue has gained particular relevance in the era of molecular diagnostic (Weller et al. 2014).
Nonetheless, innovative imaging has gained a lot of attention in the last decade. Before confirmation of the diagnosis via tissue analysis, MR spectroscopy, MR perfusion, and positron emission tomography (PET) imaging can be helpful for specific topics (Suchorska et al. 2014, 2015). Spectroscopy and perfusion can be helpful to distinguish between neoplastic lesions and other possible diagnoses. Some of the most important differential diagnoses are infectious or inflammatory causes and postischemic lesions. Moreover, metabolic imaging might show “hot spots” inside a tumor mass that can be targeted by stereotactic biopsy, thereby increasing the chance to get the most accurate diagnosis (Hermann et al. 2008). PET imaging using amino acid tracers also supports the diagnostic workup or can guide stereotactic biopsy to hot spots.
After the diagnosis has been confirmed pathologically, these innovative imaging modalities can be even more valuable. In particular, they may be useful for planning of radiotherapy (Revannasiddaiah et al. 2014). The irradiated field can be tailored to include areas with elevated PET tracer uptake, and radiation dose may be increased at hot spots seen on MR spectroscopy/perfusion or on amino acid PET.
Even more established in clinical practice is the use of innovative imaging for the monitoring during therapy and follow-up. MRI and PET can both be useful to distinguish between progressive tumor and pseudoprogression (Hutterer et al. 2014).
Functional MRI and fiber tracking using diffusion tensor imaging (DTI) might help to identify eloquent areas and improve results of surgery. Intraoperative brain mapping and awake surgery can be of further benefit. This may help to increase the extent of resection and improve progression-free survival (PFS) and overall survival (OS) while reducing perioperative morbidity.
3 Glial Tumors
3.1 Focal Glial and Glioneuronal Tumors Versus Diffuse Gliomas
Compared to focal glial tumors like pilocytic astrocytomas of the WHO grade I, grade II gliomas show diffuse infiltrative growth patterns and a propensity to evolve into grade III or grade IV gliomas. Therefore, and in contrast to pilocytic astrocytomas, a surgical cure is not possible in these (Louis et al. 2007).
Like pilocytic astrocytomas, glioneuronal tumors like dysembryoplastic neuroepithelial tumors (DNET) or ganglioglioma show a benign course. If clinically necessary, these glioneuronal tumors can usually be resected completely.
3.2 Low-Grade Versus High-Grade Gliomas
Neuropathological analyses of diffuse astrocytomas (WHO grade II) reveal well-differentiated fibrillary or gemistocytic neoplastic astrocytes on a loosely structured and often microcystic tumor matrix. Cellularity is only moderately increased. There is no mitotic activity, and proliferation rate determined by Ki-67/MIB-1 labeling index is usually below 4 % (Louis et al. 2007).
Histopathology of anaplastic astrocytomas shows the same features as those for diffuse astrocytoma. In addition, anaplastic astrocytoma shows increased cellularity, distinct nuclear atypia, and mitotic activity. Proliferation rate ranges from 5 to 10 %, but might overlap with low-grade gliomas and glioblastomas. Microvascular proliferation and necrosis are still absent (Louis et al. 2007).
Glioblastomas show a remarkable regional heterogeneity with anaplastic, poorly differentiated pleomorphic astrocytic tumor cells. Nuclear atypia is common, and mitotic activity is high. Proliferation rates range between 10 and 20 %, again with high regional heterogeneity. Microvascular proliferation and/or necrosis is essential for the diagnosis of glioblastoma (Louis et al. 2007).
Regarding prognosis, the WHO classification has obvious limitations. First, oligodendroglial tumors, anaplastic or not, have a similar clinical course that is superior to that of astrocytoma of the corresponding WHO grade. Molecular markers like 1p/19q deletions, IDH1/2 mutations, and MGMT promotor methylation are of prognostic value as they define subgroups of favorable survival. In addition, they are of predictive value and necessary for therapy decisions. It is now clear that true oligodendroglial tumors are characterized by 1p/19q codeletions and uniformly carry IDH1/2 mutations (Weller et al. 2012b, 2013; Reuss et al. 2015).
Moreover, anaplastic gliomas with favorable clinical and molecular markers can show superior survival compared to low-grade gliomas with unfavorable markers. On the other hand, anaplastic glioma with unfavorable constellation can have a prognosis inferior to that of patients with glioblastoma and favorable markers. This elucidates that molecular markers should be incorporated into an upcoming WHO classification (Louis et al. 2014; Reuss et al. 2015; Hartmann et al. 2010).
3.3 Astrocytomas Versus Oligodendroglial Tumors
In contrast to astrocytomas (see above), oligodendroglial tumor cells are monomorphic cells that show uniform round nuclei and perinuclear halos on paraffin sections (“honeycomb”). Microcalcifications, mucoid/cystic degenerations, and a dense network of branching capillaries (chicken wire) are frequently observed. Again, the presence of microvascular proliferation or necrosis is not compatible with the diagnosis of a low-grade glioma (Louis et al. 2007).
Compared to the corresponding low-grade gliomas, mitotic activity, microvascular proliferation, and areas of necrosis are frequent in anaplastic oligodendroglial tumors. A diagnosis of so-called mixed oligoastrocytoma has been established for tumors with both morphological features of oligodendroglioma and astrocytoma (Louis et al. 2007). However, the definition of oligoastrocytoma, low grade or anaplastic, is under heavy debate, and molecular markers are likely to lead to the omission of this diagnosis (Louis et al. 2007).
The mentioned calcifications in histology of oligodendroglial tumors are relevant for clinical management as they often can be detected on CT and MRI scans.
As shown by the NOA-04 trial, anaplastic oligodendroglioma and anaplastic oligoastrocytoma display a favorable outcome compared to anaplastic astrocytoma (Wick et al. 2009). This is also true for low-grade gliomas. As response rates to radiotherapy or chemotherapy in oligodendroglial tumors are higher than in astrocytic tumors, the avoidance of perioperative morbidity has even higher importance.
3.4 Low-Grade Glioma (WHO Grade II)
The absence of neurological symptoms and the presence of younger age or oligodendroglial histology are favorable clinical prognostic factors (Pignatti et al. 2002). However, even when short-term MRI scans (e.g., 3 months) suggest stable tumor size, all low-grade gliomas constantly grow in the long run (Mandonnet et al. 2003). Consequently, adjuvant treatment will be necessary at a certain time point in the course of the disease for all patients. Resection improves seizure control and may reduce the risk of malignant transformation (Soffietti et al. 2010).
3.4.1 Diffuse Astrocytoma (WHO Grade II)
After gross total resection, adjuvant treatment can be postponed at least in patients younger than 40 years of age with no neurological symptoms and a favorable location of the tumor (Pignatti et al. 2002). Regarding all other patients, there is an ongoing debate on which patients to treat and on the best time point of treatment. Radiotherapy prolongs PFS but not OS (van den Bent et al. 2005). Therefore, the EORTC defined five prognostic factors useful to identify low-risk and high-risk patients, the latter being treated with early radiotherapy (Pignatti et al. 2002). Prognostic favorable factors are age < 40 years, largest tumor diameter < 6 cm, tumor not crossing the midline, oligodendroglial or oligoastrocytic histology, and absence of a neurological deficit. Patients with two or fewer unfavorable factors are low-risk patients where therapy might be postponed unless their tumor is located in eloquent brain areas or patients suffer from untreatable epilepsy. Patients with three or more risk factors have dismal prognosis and might be treated immediately unless gross total resection was possible. In these cases, therapy might still be postponed. Chemotherapy also has activity in diffuse astrocytoma (Pace et al. 2003; Quinn et al. 2003; Brada et al. 2003). It is well established for patients who progressed after initial radiotherapy and can be an alternative as initial treatment in some patients. PCV (procarbazine, CCNU, and vincristine) and temozolomide seem to be comparable regarding efficacy with a better toxicity profile for temozolomide.
Recently, the updated results of the RTOG 9802 trial have been presented, although not published in detail yet (Shaw et al. 2012). This trial compared 54 Gy of radiotherapy with 54 Gy of radiotherapy followed by adjuvant chemotherapy with six cycles of PCV. In this regimen, procarbazine, CCNU, and vincristine are combined to a 6-week cycle. This trial included high-risk patients with low-grade glioma > 40 years of age and/or less than total resection. Median OS increased from 7.8 to 13.3 years in the combination therapy group although, interestingly, 77 % of the patients that progressed after radiotherapy had received salvage chemotherapy. A detailed analysis on histology subtypes and especially on molecular markers is lacking.
Whether these rather low-threshold criteria to define high-risk patients will translate to everyday practice is under debate. Further, it remains unanswered whether PCV alone would be equivalent and whether temozolomide could safely replace PCV in combination with radiotherapy. Therefore, many centers recommend the combination of radiotherapy and PCV.
3.4.2 Oligodendroglioma and Oligoastrocytoma (WHO Grade II)
After resection or diagnostic biopsy, the considerations for adjuvant treatment are similar to those for astrocytomas. The prognostic factors defined by the EORTC and mentioned above also apply to oligodendroglioma and oligoastrocytoma. As oligodendroglial tumors more often respond to chemotherapy, this is a more common choice for initial treatment in many centers (van den Bent et al. 1998, 2003). Nonetheless, the emerging standard of care is radiotherapy followed by chemotherapy with PCV according to the RTOG 9802 trial (Shaw et al. 2012).
3.5 Anaplastic Glioma (WHO Grade III)
In contrast to low-grade gliomas, adjuvant treatment is mandatory for patients with anaplastic glioma. The limitations of the current WHO classification are obvious in these tumors as mentioned above. Molecular markers have already entered diagnostic workup and therapeutic decision making (Weller et al. 2014).
3.5.1 Anaplastic Astrocytoma (WHO Grade III)
For adjuvant treatment, radiotherapy (60 Gy) was traditionally applied. According to the results of the NOA-04 trial, primary chemotherapy with temozolomide or with PCV seems to be equivalent regarding PFS and OS (Wick et al. 2009). Many brain tumor centers treat patients with anaplastic astrocytomas with radiochemotherapy according to the EORTC NCIC protocol with concomitant temozolomide and six cycles of adjuvant temozolomide. While reasonable, the evidence for this approach is limited and might be provided by the CATNON trial (EORTC 26053–22054). In this ongoing trial, the addition of temozolomide to first-line radiotherapy of anaplastic gliomas without 1p/19q deletion (mostly anaplastic astrocytoma) will be evaluated. In a 2 × 2 design, this study compares radiotherapy alone with radiotherapy plus concomitant temozolomide, radiotherapy plus adjuvant temozolomide, and radiotherapy plus concomitant and adjuvant temozolomide.
In the recurrent situation, treatment is less firmly established, and randomized controlled trials are rare. Second surgery might be an option if possible. Further treatment will depend on first-line treatment. Patients that progress after radiotherapy will be treated with either temozolomide chemotherapy or nitrosourea-based chemotherapy. If first-line treatment consisted of chemotherapy, radiotherapy is an option. Depending on availability, bevacizumab is often applied at progression after radiotherapy and alkylating chemotherapy, with modest PFS rates at 6 months (Weller et al. 2014).
3.5.2 Anaplastic Oligodendroglioma and Oligoastrocytoma
Radiotherapy has long been the standard of care in anaplastic oligodendroglioma and anaplastic oligoastrocytoma. However, these tumors not just frequently respond to radiotherapy, but also to chemotherapy. Especially in tumors with loss of 1p and 19q (LOH 1p/19q), PCV chemotherapy shows response rates of up to 100 % (Cairncross et al. 1994; Buckner et al. 2003). The NOA-04 trial showed that radiotherapy, PCV chemotherapy, and temozolomide are comparable in first-line treatment (Wick et al. 2009). Therefore, many centers recommended temozolomide as first-line therapy in the past, as it shows a superior tolerability profile compared to PCV. The sequence of therapeutic options (RT, PCV, TMZ) was the main focus in this trial.
In 2013, the long-term results of two large randomized controlled trials were published. Both the RTOG 9402 and the EORTC 26951 trial evaluated the combination of radiotherapy and PCV chemotherapy compared to radiotherapy alone in patients with anaplastic oligodendroglioma or oligoastrocytoma (Cairncross et al. 2006; van den Bent et al. 2006). Only after a follow-up of 6 years it became obvious that patients with LOH 1p/19q showed a dramatic benefit in OS when treated with radiotherapy and PCV (Cairncross et al. 2013; van den Bent et al. 2013). Hence, the 1p/19q status is not just prognostic but also predictive, requiring the testing for this marker before treatment planning. As for low-grade glioma, it remains unclear whether PCV alone would achieve similar results and whether temozolomide could safely replace PCV.
3.5.3 Gliomatosis Cerebri
Gliomatosis cerebri is a rare and controversial diagnosis and might be revised in future WHO classifications. This tumor cannot be defined by the neuropathologist alone. The diagnosis requires a combination of glioma histology and the radiological involvement of at least three cerebral lobes (Louis et al. 2007).
As this entity is the prototype of an infiltrative tumor, surgical resection is usually no option, and stereotactic biopsy leads to the diagnosis.
Histological features and prognosis are highly variable since any glioma histology together with radiology can lead to the diagnosis. Usually, all patients receive treatment after diagnosis.
Large randomized trials for adjuvant treatment are lacking. Radiotherapy, PCV, and temozolomide are active treatments (Herrlinger 2012; Sanson et al. 2004). Due to the diffuse growth, radiotherapy usually results in whole brain radiotherapy and is therefore frequently postponed. Instead, chemotherapy is frequently recommended for first-line treatment. The NOA-05 trial is one of the few prospective trials on chemotherapy in gliomatosis cerebri (Glas et al. 2011). Chemotherapy with PC (procarbazine + CCNU) resulted in prolonged tumor control in some patients in this trial, and the median OS was only 30 months.
3.6 Glioblastoma (WHO Grade IV)
Glioblastoma is the most frequent malignant primary brain tumor. Several studies suggest that the extent of resection is relevant for prognosis, although class I evidence is still lacking (Sanai et al. 2011; Kreth et al. 2013). Surgery using 3D navigation systems and intraoperative monitoring is standard in most centers. With 5-ALA-guided resection and intraoperative MRI, two techniques to improve extent of resection have been evaluated in a randomized controlled setting (Senft et al. 2011; Stummer et al. 2006). Both studies showed an increase of patients with gross total resection and superior survival. Awake surgery is done by some centers but cannot be regarded as a standard for patients with glioblastoma.
The current standard of care was defined in 2005 with the results of the EORTC 26981–22981 NCIC CE.3 (Stupp et al. 2005, 2009). This trial compared radiotherapy, the former standard of care, with radiotherapy plus concomitant and adjuvant chemotherapy with temozolomide. Median OS was prolonged from 12.1 to 14.6 months. Two-year survival rate increased from 10.4 to 26.5 %. In addition, a companion paper reported on the predictive value of the MGMT promoter methylation status (Hegi et al. 2005). The benefit of the addition of temozolomide was far lower when the MGMT promotor was not methylated. Patients with a methylated MGMT promotor showed a median OS of 15.3 months when they received radiotherapy alone and 21.7 months after combined treatment. Importantly, the majority of patients had alkylating agent chemotherapy at progression, diluting the survival benefit afforded by temozolomide in the experimental arm. When the MGMT promotor was unmethylated, median OS reached 11.8 and 12.7 months for radiotherapy alone and combined treatment, respectively. This benefit in patients with unmethylated MGMT promotor was small but still significant. Therefore, and because of missing alternatives as well as a certain amount of uncertainty regarding the procedures for testing the MGMT promotor, most patients are treated with a combined radiochemotherapy irrespective of the MGMT promotor status (Weller et al. 2014).
In elderly patients with glioblastoma, the MGMT status is more relevant. The NOA-08 trial randomized patients older than 65 years between radiotherapy alone and temozolomide alone (Wick et al. 2012). For the whole cohort, there was no significant difference in PFS and OS, suggesting that temozolomide is equally active in these patients. When analyzing the subgroups of patients with methylated and unmethylated MGMT promotor, however, significant and clinically relevant differences were observed. In patients with methylated MGMT promotor temozolomide resulted in an event-free survival (EFS) of 8.4 months compared to 4.6 months for radiotherapy. In contrast, in patients with unmethylated MGMT promotor, temozolomide showed an EFS of 3.3 months and radiotherapy of 4.6 months. Similar results were observed in the Nordic trial (Malmstrom et al. 2012). As a result of these studies, treatment planning in older patients depends on MGMT status (Wick et al. 2014; Weller et al. 2012b, 2014). Patients with methylated MGMT promotor should receive temozolomide, either alone or in combination with radiotherapy for patients with a good clinical status. Radiotherapy alone is not sufficient for these patients. When the MGMT promotor is unmethylated, radiotherapy is the therapy of choice. Temozolomide seems to have no or only minimal efficacy in these patients.
In the recurrent situation, no formal standard is established. If possible, second surgery and second radiotherapy are regularly applied even if evidence for efficacy is low (Fogh et al. 2010; Grosu et al. 2005). Regarding chemotherapy, nitrosourea-based protocols and temozolomide are frequently used and approved by authorities (Batchelor et al. 2013; Wick et al. 2010; Perry et al. 2010; Norden et al. 2013). The antiangiogenic drug bevacizumab has resulted in unprecedented response rates and promising PFS times in patients with recurrent glioblastoma in the BRAIN trial (Friedman et al. 2009). As large randomized and controlled trials are missing, the influence on OS is unclear. Nonetheless, the FDA approved bevacizumab for the treatment of recurrent glioblastoma in 2009. The European authorities have refused approval in the same year.
A small but randomized phase II study (BELOB trial) conducted in the Netherlands compared CCNU (n = 46) with bevacizumab (n = 50) and the combination of both (n = 52) in patient with recurrent glioblastoma (Taal et al. 2014). The combination of bevacizumab and CCNU resulted in a median OS of 12 months whereas CCNU and bevacizumab alone only reached 8 months, respectively. A large randomized controlled phase III trial comparing CCNU with CCNU plus bevacizumab has just finished recruitment, and results are expected in late 2015.
Regarding the use of bevacizumab in first-line treatment, two randomized controlled trials showed 4 months benefit for PFS but no benefit for OS (Chinot et al. 2014; Gilbert et al. 2014). Therefore, bevacizumab has no role in first-line therapy.
As antiangiogenic agents often abrogate contrast enhancement and edema of glioblastoma, this might in part explain the discrepancy between effects on PFS and OS. Furthermore, even T2-weighted MRI sequences are influenced by bevacizumab (Hattingen et al. 2013). This emphasizes the need for innovative imaging for the follow-up of patients on antiangiogenic therapy (Hutterer et al. 2014).
4 Primary CNS Lymphomas
Primary CNS lymphomas are malignant lymphomas, usually B-cell lymphomas, arising in the CNS without lymphoma manifestations outside the nervous system (Louis et al. 2007). This is a rare entity with a much higher incidence in AIDS patients. With the introduction of highly active antiretroviral therapy (HAART), the occurrence in AIDS patients has markedly dropped.
Primary CNS lymphomas typically involve the supratentorial brain parenchyma, but can also occur in the spinal cord and the posterior fossa. In rare cases, lymphoma cells can be found in the cerebrospinal fluid (CSF). Ocular disease can be detected in up to 15 % of all cases. Some primary CNS lymphomas show a perivascular growth pattern and thereby result in atypical MRI findings. In less than 10 %, occult systemic lymphomas are present.
This possible dissemination defines the diagnostic workup (Korfel & Schlegel 2013). Besides cerebral MRI, at least systemic staging with computed tomography, CSF analysis (if safely possible) and ophthalmologic examination are recommended. For the clinical management, it is essential to early consider a possible diagnosis of CNS lymphoma. Steroids, as often applied for symptomatic therapy in patients with malignant glioma or brain metastases, must be avoided in lymphoma patients before histological diagnosis. Steroids are cytotoxic to lymphoma cells and can thereby impede a clear histological diagnosis.
Diagnosis is still commonly made via stereotactic biopsy, although the best contemporary evidence indicates a benefit from open surgical resection at least with unifocal disease (Weller et al. 2012a). The therapy usually consists of high-dose methotrexate chemotherapy for all patients who can tolerate it (Korfel & Schlegel 2013). The monoclonal CD20 antibody rituximab and dexamethasone are frequently combined with chemotherapy. High-dose chemotherapy followed by autologous stem-cell transplantation can be considered in younger patients (Illerhaus et al. 2006). Intrathecal/intraventricular chemotherapy is part of some protocols (Pels et al. 2003). Whole brain radiotherapy is active in primary CNC lymphomas but is associated with delayed neurotoxicity (Doolittle et al. 2013). Therefore, radiotherapy should be reserved for patients who cannot receive chemotherapy or in the recurrent setting (Korfel et al. 2015; Thiel et al. 2010).
5 Metastatic Tumors of the CNS
Brain metastases are approximately five times more frequent than primary brain tumors, and 25 % of all patients dying because of malignancies show metastatic involvement of the brain in autopsies (Louis et al. 2007). The frequency of underlying cancer entities depends on their respective incidence and tropism for CNS. Non-small cell lung cancer (NSCLC) accounts for 50 % of all patients with brain metastasis, followed by breast cancer (~15 %), melanoma (~10 %), and renal cancer (~10 %) (Ostrom et al. 2014). In general, the prognosis for patients with metastatic tumors of the CNS is unfavorable. The incidence of brain metastasis is increasing due to improved systemic therapies with sometimes limited CNS activity (Ahluwalia et al. 2014).
The clinical presentation does not differ from primary brain tumors, and in cases of single metastasis, MRI scans might also be similar to a malignant glioma. When numerous tumors are visible on MRI, the diagnosis is usually easy with infectious diseases being the relevant differential diagnosis.
All therapeutic considerations regarding brain metastases must account for the systemic situation of the underlying cancer entity (Ahluwalia et al. 2014). Neurosurgical resections can be considered in patients with solitary or singular brain metastases and lesions causing mass effects or neurological symptoms (Patchell et al. 1990). Stereotactic radiosurgery is an active alternative to surgery and is typically applied in patients with up to five small metastases (<3 cm) (Aoyama et al. 2006; Kocher et al. 2011). The maximum number of metastases that can be treated with radiosurgery has increased during the last years (Yamamoto et al. 2014; Hunter et al. 2012). When neurosurgery and focal radiotherapy are not possible, whole brain radiotherapy (WBRT) is an active option. WBRT prolongs PFS but not OS and is associated with a relevant cognitive decline in some patients (Chang et al. 2009; Aoyama et al. 2007). Therefore, WBRT can be postponed in patients where all brain metastases can be sufficiently treated with a local treatment modality (surgery or radiosurgery). Systemic chemotherapy is frequently applied according to the underlying cancer type (Ahluwalia et al. 2014). Usually, systemic chemotherapy does not render one of the aforementioned brain-directed therapies unnecessary. This might be different for some targeted therapies like BRAF inhibitors for malignant melanoma (Ahluwalia et al. 2014).
In general, the number and efficacy of therapeutic options are often limited, and therefore, the intensification of preclinical and clinical research in this rather neglected field is warranted.
References
Ahluwalia MS, Vogelbaum MV, Chao ST, Mehta MM (2014) Brain metastasis and treatment. F1000Prime Rep 6:114
Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, Hatano K, Kenjyo M, Oya N, Hirota S, Shioura H, Kunieda E, Inomata T, Hayakawa K, Katoh N, Kobashi G (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. JAMA 295(21):2483–2491
Aoyama H, Tago M, Kato N, Toyoda T, Kenjyo M, Hirota S, Shioura H, Inomata T, Kunieda E, Hayakawa K, Nakagawa K, Kobashi G, Shirato H (2007) Neurocognitive function of patients with brain metastasis who received either whole brain radiotherapy plus stereotactic radiosurgery or radiosurgery alone. Int J Radiat Oncol Biol Phys 68(5):1388–1395
Batchelor TT, Mulholland P, Neyns B, Nabors LB, Campone M, Wick A, Mason W, Mikkelsen T, Phuphanich S, Ashby LS, Degroot J, Gattamaneni R, Cher L, Rosenthal M, Payer F, Jurgensmeier JM et al (2013) Phase III randomized trial comparing the efficacy of cediranib as monotherapy, and in combination with lomustine, versus lomustine alone in patients with recurrent glioblastoma. J Clin Oncol 31(26):3212–3218
Brada M, Viviers L, Abson C, Hines F, Britton J, Ashley S, Sardell S, Traish D, Gonsalves A, Wilkins P, Westbury C (2003) Phase II study of primary temozolomide chemotherapy in patients with WHO grade II gliomas. Ann Oncol 14(12):1715–1721
Buckner JC, Gesme D Jr, O’Fallon JR, Hammack JE, Stafford S, Brown PD, Hawkins R, Scheithauer BW, Erickson BJ, Levitt R, Shaw EG, Jenkins R (2003) Phase II trial of procarbazine, lomustine, and vincristine as initial therapy for patients with low-grade oligodendroglioma or oligoastrocytoma: efficacy and associations with chromosomal abnormalities. J Clin Oncol 21(2):251–255
Cairncross G, Macdonald D, Ludwin S, Lee D, Cascino T, Buckner J, Fulton D, Dropcho E, Stewart D, Schold C Jr et al (1994) Chemotherapy for anaplastic oligodendroglioma. National Cancer Institute of Canada Clinical Trials Group. J Clin Oncol 12(10):2013–2021
Cairncross G, Berkey B, Shaw E, Jenkins R, Scheithauer B, Brachman D, Buckner J, Fink K, Souhami L, Laperierre N, Mehta M, Curran W (2006) Phase III trial of chemotherapy plus radiotherapy compared with radiotherapy alone for pure and mixed anaplastic oligodendroglioma: Intergroup Radiation Therapy Oncology Group Trial 9402. J Clin Oncol 24(18):2707–2714
Cairncross G, Wang M, Shaw E, Jenkins R, Brachman D, Buckner J, Fink K, Souhami L, Laperriere N, Curran W, Mehta M (2013) Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol 31(3):337–343
Chang EL, Wefel JS, Hess KR, Allen PK, Lang FF, Kornguth DG, Arbuckle RB, Swint JM, Shiu AS, Maor MH, Meyers CA (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, Nishikawa R, Carpentier AF, Hoang-Xuan K, Kavan P, Cernea D, Brandes AA, Hilton M, Abrey L, Cloughesy T (2014) Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 370(8):709–722
Doolittle ND, Korfel A, Lubow MA, Schorb E, Schlegel U, Rogowski S, Fu R, Dosa E, Illerhaus G, Kraemer DF, Muldoon LL, Calabrese P, Hedrick N, Tyson RM, Jahnke K, Maron LM et al (2013) Long-term cognitive function, neuroimaging, and quality of life in primary CNS lymphoma. Neurology 81(1):84–92
Fogh SE, Andrews DW, Glass J, Curran W, Glass C, Champ C, Evans JJ, Hyslop T, Pequignot E, Downes B, Comber E, Maltenfort M, Dicker AP, Werner-Wasik M (2010) Hypofractionated stereotactic radiation therapy: an effective therapy for recurrent high-grade gliomas. J Clin Oncol 28(18):3048–3053
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, Yung WK, Paleologos N, Nicholas MK, Jensen R, Vredenburgh J, Huang J, Zheng M, Cloughesy T (2009) Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol 27(28):4733–4740
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, Vogelbaum MA, Colman H, Chakravarti A, Pugh S, Won M, Jeraj R, Brown PD, Jaeckle KA, Schiff D, Stieber VW, Brachman DG et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370(8):699–708
Glas M, Bähr O, Felsberg J, Rasch K, Wiewrodt D, Schabet M, Simon M, Urbach H, Steinbach JP, Rieger J, Fimmers R, Bamberg M, Nagele T, Reifenberger G, Weller M, Herrlinger U (2011) NOA-05 phase 2 trial of procarbazine and lomustine therapy in gliomatosis cerebri. Ann Neurol 70(3):445–453
Grosu AL, Weber WA, Franz M, Stark S, Piert M, Thamm R, Gumprecht H, Schwaiger M, Molls M, Nieder C (2005) Reirradiation of recurrent high-grade gliomas using amino acid PET (SPECT)/CT/MRI image fusion to determine gross tumor volume for stereotactic fractionated radiotherapy. Int J Radiat Oncol Biol Phys 63(2):511–519
Hartmann C, Hentschel B, Wick W, Capper D, Felsberg J, Simon M, Westphal M, Schackert G, Meyermann R, Pietsch T, Reifenberger G, Weller M, Loeffler M, von Deimling A (2010) Patients with IDH1 wild type anaplastic astrocytomas exhibit worse prognosis than IDH1-mutated glioblastomas, and IDH1 mutation status accounts for the unfavorable prognostic effect of higher age: implications for classification of gliomas. Acta Neuropathol 120(6):707–718
Hattingen E, Jurcoane A, Daneshvar K, Pilatus U, Mittelbronn M, Steinbach JP, Bähr O (2013) Quantitative T2 mapping of recurrent glioblastoma under bevacizumab improves monitoring for non-enhancing tumor progression and predicts overall survival. Neuro Oncol 15(10):1395–1404
Hegi ME, Diserens AC, Gorlia T, Hamou MF, de Tribolet N, Weller M, Kros JM, Hainfellner JA, Mason W, Mariani L, Bromberg JE, Hau P, Mirimanoff RO, Cairncross JG, Janzer RC, Stupp R (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352(10):997–1003
Hermann EJ, Hattingen E, Krauss JK, Marquardt G, Pilatus U, Franz K, Setzer M, Gasser T, Tews DS, Zanella FE, Seifert V, Lanfermann H (2008) Stereotactic biopsy in gliomas guided by 3-tesla 1H-chemical-shift imaging of choline. Stereotact Funct Neurosurg 86(5):300–307
Herrlinger U (2012) Gliomatosis cerebri. Handb Clin Neurol 105:507–515
Hunter GK, Suh JH, Reuther AM, Vogelbaum MA, Barnett GH, Angelov L, Weil RJ, Neyman G, Chao ST (2012) Treatment of five or more brain metastases with stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(5):1394–1398
Hutterer M, Hattingen E, Palm C, Proescholdt MA and Hau P (2014) Current standards and new concepts in MRI and PET response assessment of antiangiogenic therapies in high-grade glioma patients. Neuro Oncol 1–16, doi:10.1093/neuonc/nou322
Illerhaus G, Marks R, Ihorst G, Guttenberger R, Ostertag C, Derigs G, Frickhofen N, Feuerhake F, Volk B, Finke J (2006) High-dose chemotherapy with autologous stem-cell transplantation and hyperfractionated radiotherapy as first-line treatment of primary CNS lymphoma. J Clin Oncol 24(24):3865–3870
Kocher M, Soffietti R, Abacioglu U, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, van den Berge D, Collette S, Collette L et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952–26001 study. J Clin Oncol 29(2):134–141
Korfel A, Schlegel U (2013) Diagnosis and treatment of primary CNS lymphoma. Nat Rev Neurol 9(6):317–327
Korfel A, Thiel E, Martus P, Mohle R, Griesinger F, Rauch M, Roth A, Hertenstein B, Fischer T, Hundsberger T, Mergenthaler HG, Junghanss C, Birnbaum T, Fischer L, Jahnke K, Herrlinger U, et al (2015) Randomized phase III study of whole-brain radiotherapy for primary CNS lymphoma. Neurology 84(12):1242–1248
Kreth FW, Thon N, Simon M, Westphal M, Schackert G, Nikkhah G, Hentschel B, Reifenberger G, Pietsch T, Weller M, Tonn JC (2013) Gross total but not incomplete resection of glioblastoma prolongs survival in the era of radiochemotherapy. Ann Oncol 24(12):3117–3123
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, Scheithauer BW, Kleihues P (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol 114(2):97–109
Louis DN, Perry A, Burger P, Ellison DW, Reifenberger G, von Deimling A, Aldape K, Brat D, Collins VP, Eberhart C, Figarella-Branger D, Fuller GN, Giangaspero F, Giannini C, Hawkins C, Kleihues P et al (2014) International Society of Neuropathology–Haarlem consensus guidelines for nervous system tumor classification and grading. Brain Pathol 24(5):429–435
Malmstrom A, Gronberg BH, Marosi C, Stupp R, Frappaz D, Schultz H, Abacioglu U, Tavelin B, Lhermitte B, Hegi ME, Rosell J, Henriksson R (2012) Temozolomide versus standard 6-week radiotherapy versus hypofractionated radiotherapy in patients older than 60 years with glioblastoma: the Nordic randomised, phase 3 trial. Lancet Oncol 13(9):916–926
Mandonnet E, Delattre JY, Tanguy ML, Swanson KR, Carpentier AF, Duffau H, Cornu P, Van Effenterre R, Alvord EC Jr, Capelle L (2003) Continuous growth of mean tumor diameter in a subset of grade II gliomas. Ann Neurol 53(4):524–528
Norden AD, Lesser GJ, Drappatz J, Ligon KL, Hammond SN, Lee EQ, Reardon DR, Fadul CE, Plotkin SR, Batchelor TT, Zhu JJ, Beroukhim R, Muzikansky A, Doherty L, Lafrankie D, Smith K et al (2013) Phase 2 study of dose-intense temozolomide in recurrent glioblastoma. Neuro Oncol 15(7):930–935
Ostrom QT, Gittleman H, Liao P, Rouse C, Chen Y, Dowling J, Wolinsky Y, Kruchko C, Barnholtz-Sloan J (2014) CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol 16(Suppl 4):iv1–iv63
Pace A, Vidiri A, Galie E, Carosi M, Telera S, Cianciulli AM, Canalini P, Giannarelli D, Jandolo B, Carapella CM (2003) Temozolomide chemotherapy for progressive low-grade glioma: clinical benefits and radiological response. Ann Oncol 14(12):1722–1726
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500
Pels H, Schmidt-Wolf IG, Glasmacher A, Schulz H, Engert A, Diehl V, Zellner A, Schackert G, Reichmann H, Kroschinsky F, Vogt-Schaden M, Egerer G, Bode U, Schaller C, Deckert M, Fimmers R et al (2003) Primary central nervous system lymphoma: results of a pilot and phase II study of systemic and intraventricular chemotherapy with deferred radiotherapy. J Clin Oncol 21(24):4489–4495
Perry JR, Belanger K, Mason WP, Fulton D, Kavan P, Easaw J, Shields C, Kirby S, Macdonald DR, Eisenstat DD, Thiessen B, Forsyth P, Pouliot JF (2010) Phase II trial of continuous dose-intense temozolomide in recurrent malignant glioma: RESCUE study. J Clin Oncol 28(12):2051–2057
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P, Afra D, Cornu P, Bolla M, Vecht C, Karim AB (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20(8):2076–2084
Quinn JA, Reardon DA, Friedman AH, Rich JN, Sampson JH, Provenzale JM, McLendon RE, Gururangan S, Bigner DD, Herndon JE 2nd, Avgeropoulos N, Finlay J, Tourt-Uhlig S, Affronti ML, Evans B, Stafford-Fox V et al (2003) Phase II trial of temozolomide in patients with progressive low-grade glioma. J Clin Oncol 21(4):646–651
Reuss DE, Sahm F, Schrimpf D, Wiestler B, Capper D, Koelsche C, Schweizer L, Korshunov A, Jones DT, Hovestadt V, Mittelbronn M, Schittenhelm J, Herold-Mende C, Unterberg A, Platten M, Weller M et al (2015) ATRX and IDH1-R132H immunohistochemistry with subsequent copy number analysis and IDH sequencing as a basis for an “integrated” diagnostic approach for adult astrocytoma, oligodendroglioma and glioblastoma. Acta Neuropathol 129(1):133–146
Revannasiddaiah S, Susheela SP, Kallur KG (2014) Integration of methionine-PET into the radiotherapy planning process for high grade glioma: prospects against non-central and central failures. Radiother Oncol 113(2):296
Sanai N, Polley MY, McDermott MW, Parsa AT, Berger MS (2011) An extent of resection threshold for newly diagnosed glioblastomas. J Neurosurg 115(1):3–8
Sanson M, Cartalat-Carel S, Taillibert S, Napolitano M, Djafari L, Cougnard J, Gervais H, Laigle F, Carpentier A, Mokhtari K, Taillandier L, Chinot O, Duffau H, Honnorat J, Hoang-Xuan K, Delattre JY (2004) Initial chemotherapy in gliomatosis cerebri. Neurology 63(2):270–275
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12(11):997–1003
Shaw EG, Wang M, Coons SW, Brachman DG, Buckner JC, Stelzer KJ, Barger GR, Brown PD, Gilbert MR, Mehta MP (2012) Randomized trial of radiation therapy plus procarbazine, lomustine, and vincristine chemotherapy for supratentorial adult low-grade glioma: initial results of RTOG 9802. J Clin Oncol 30(25):3065–3070
Soffietti R, Baumert BG, Bello L, von Deimling A, Duffau H, Frenay M, Grisold W, Grant R, Graus F, Hoang-Xuan K, Klein M, Melin B, Rees J, Siegal T, Smits A, Stupp R et al (2010) Guidelines on management of low-grade gliomas: report of an EFNS-EANO Task Force. Eur J Neurol 17(9):1124–1133
Stummer W, Pichlmeier U, Meinel T, Wiestler OD, Zanella F, Reulen HJ (2006) Fluorescence-guided surgery with 5-aminolevulinic acid for resection of malignant glioma: a randomised controlled multicentre phase III trial. Lancet Oncol 7(5):392–401
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, Curschmann J, Janzer RC, Ludwin SK, Gorlia T, Allgeier A, Lacombe D et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352(10):987–996
Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, Ludwin SK, Allgeier A, Fisher B, Belanger K, Hau P, Brandes AA, Gijtenbeek J, Marosi C, Vecht CJ, Mokhtari K et al (2009) Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol 10(5):459–466
Suchorska B, Tonn JC, Jansen NL (2014) PET imaging for brain tumor diagnostics. Curr Opin Neurol 27(6):683–688
Suchorska B, Jansen NL, Linn J, Kretzschmar H, Janssen H, Eigenbrod S, Simon M, Popperl G, Kreth FW, la Fougere C, Weller M, Tonn JC (2015) Biological tumor volume in 18FET-PET before radiochemotherapy correlates with survival in GBM. Neurology 84(7):710–719
Taal W, Oosterkamp HM, Walenkamp AM, Dubbink HJ, Beerepoot LV, Hanse MC, Buter J, Honkoop AH, Boerman D, de Vos FY, Dinjens WN, Enting RH, Taphoorn MJ, van den Berkmortel FW, Jansen RL, Brandsma D et al (2014) Single-agent bevacizumab or lomustine versus a combination of bevacizumab plus lomustine in patients with recurrent glioblastoma (BELOB trial): a randomised controlled phase 2 trial. Lancet Oncol 15(9):943–953
Thiel E, Korfel A, Martus P, Kanz L, Griesinger F, Rauch M, Roth A, Hertenstein B, von Toll T, Hundsberger T, Mergenthaler HG, Leithauser M, Birnbaum T, Fischer L, Jahnke K, Herrlinger U et al (2010) High-dose methotrexate with or without whole brain radiotherapy for primary CNS lymphoma (G-PCNSL-SG-1): a phase 3, randomised, non-inferiority trial. Lancet Oncol 11(11):1036–1047
van den Bent MJ, Kros JM, Heimans JJ, Pronk LC, van Groeningen CJ, Krouwer HG, Taphoorn MJ, Zonnenberg BA, Tijssen CC, Twijnstra A, Punt CJ, Boogerd W (1998) Response rate and prognostic factors of recurrent oligodendroglioma treated with procarbazine, CCNU, and vincristine chemotherapy. Dutch Neuro-oncology Group. Neurology 51(4):1140–1145
van den Bent MJ, Taphoorn MJ, Brandes AA, Menten J, Stupp R, Frenay M, Chinot O, Kros JM, van der Rijt CC, Vecht Ch J, Allgeier A, Gorlia T (2003) Phase II study of first-line chemotherapy with temozolomide in recurrent oligodendroglial tumors: the European Organization for Research and Treatment of Cancer Brain Tumor Group Study 26971. J Clin Oncol 21(13):2525–2528
van den Bent MJ, Afra D, de Witte O, Ben Hassel M, Schraub S, Hoang-Xuan K, Malmstrom PO, Collette L, Pierart M, Mirimanoff R, Karim AB (2005) Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: the EORTC 22845 randomised trial. Lancet 366(9490):985–990
van den Bent MJ, Carpentier AF, Brandes AA, Sanson M, Taphoorn MJ, Bernsen HJ, Frenay M, Tijssen CC, Grisold W, Sipos L, Haaxma-Reiche H, Kros JM, van Kouwenhoven MC, Vecht CJ, Allgeier A, Lacombe D et al (2006) Adjuvant procarbazine, lomustine, and vincristine improves progression-free survival but not overall survival in newly diagnosed anaplastic oligodendrogliomas and oligoastrocytomas: a randomized European Organisation for Research and Treatment of Cancer phase III trial. J Clin Oncol 24(18):2715–2722
van den Bent MJ, Brandes AA, Taphoorn MJ, Kros JM, Kouwenhoven MC, Delattre JY, Bernsen HJ, Frenay M, Tijssen CC, Grisold W, Sipos L, Enting RH, French PJ, Dinjens WN, Vecht CJ, Allgeier A et al (2013) Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol 31(3):344–350
Weller M, Martus P, Roth P, Thiel E, Korfel A (2012a) Surgery for primary CNS lymphoma? Challenging a paradigm. Neuro Oncol 14(12):1481–1484
Weller M, Stupp R, Hegi ME, van den Bent M, Tonn JC, Sanson M, Wick W, Reifenberger G (2012b) Personalized care in neuro-oncology coming of age: why we need MGMT and 1p/19q testing for malignant glioma patients in clinical practice. Neuro Oncol 14(Suppl 4):iv100–iv108
Weller M, Stupp R, Wick W (2012c) Epilepsy meets cancer: when, why, and what to do about it? Lancet Oncol 13(9):e375–e382
Weller M, Pfister SM, Wick W, Hegi ME, Reifenberger G, Stupp R (2013) Molecular neuro-oncology in clinical practice: a new horizon. Lancet Oncol 14(9):e370–e379
Weller M, van den Bent M, Hopkins K, Tonn JC, Stupp R, Falini A, Cohen-Jonathan-Moyal E, Frappaz D, Henriksson R, Balana C, Chinot O, Ram Z, Reifenberger G, Soffietti R, Wick W (2014) EANO guideline for the diagnosis and treatment of anaplastic gliomas and glioblastoma. Lancet Oncol 15(9):e395–e403
Wick W, Hartmann C, Engel C, Stoffels M, Felsberg J, Stockhammer F, Sabel MC, Koeppen S, Ketter R, Meyermann R, Rapp M, Meisner C, Kortmann RD, Pietsch T, Wiestler OD, Ernemann U et al (2009) NOA-04 randomized phase III trial of sequential radiochemotherapy of anaplastic glioma with procarbazine, lomustine, and vincristine or temozolomide. J Clin Oncol 27(35):5874–5880
Wick W, Puduvalli VK, Chamberlain MC, van den Bent MJ, Carpentier AF, Cher LM, Mason W, Weller M, Hong S, Musib L, Liepa AM, Thornton DE, Fine HA (2010) Phase III study of enzastaurin compared with lomustine in the treatment of recurrent intracranial glioblastoma. J Clin Oncol 28(7):1168–1174
Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M, Nikkhah G, Papsdorf K, Steinbach JP, Sabel M, Combs SE, Vesper J, Braun C, Meixensberger J, Ketter R, Mayer-Steinacker R et al (2012) Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: the NOA-08 randomised, phase 3 trial. Lancet Oncol 13(7):707–715
Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, Plass C, Hegi M, Platten M, Reifenberger G (2014) MGMT testing–the challenges for biomarker-based glioma treatment. Nat Rev Neurol 10(7):372–385
Yamamoto M, Serizawa T, Shuto T, Akabane A, Higuchi Y, Kawagishi J, Yamanaka K, Sato Y, Jokura H, Yomo S, Nagano O, Kenai H, Moriki A, Suzuki S, Kida Y, Iwai Y et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Bähr, O., Steinbach, J.P., Weller, M. (2015). Brain Tumor Imaging. In: Hattingen, E., Pilatus, U. (eds) Brain Tumor Imaging. Medical Radiology(). Springer, Berlin, Heidelberg. https://doi.org/10.1007/174_2015_1072
Download citation
DOI: https://doi.org/10.1007/174_2015_1072
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-45039-6
Online ISBN: 978-3-642-45040-2
eBook Packages: MedicineMedicine (R0)