Abstract
This review article focuses on occurrence, imaging, and differential diagnosis of insufficiency fractures. Prevalence and the most common sites of insufficiency fractures and their clinical implications are discussed. Insufficiency fractures are due to normal stress exerted on weakened bone. Most commonly, postmenopausal osteoporosis is the cause for insufficiency fractures. Additional conditions affecting bone turnover include osteomalacia, chronic renal failure, and high dose corticosteroid therapy. It is a challenge for the radiologist to detect and diagnose insufficiency fractures as well as to differentiate them from malignant fractures. Radiographs are the basic modality used for screening of insufficiency fractures, yet depending on the location of the fractures sensitivity is limited. Magnetic resonance imaging (MRI) is a very sensitive tool to visualize bone marrow abnormalities associated with insufficiency fractures and has allowed differentiation of benign versus malignant fractures. Thin section Multidetector CT depicts subtle fracture lines allowing direct visualization of cortical and trabecular bone. Dedicated Mikro-CTs (Xtreme-CT) can detect subtle fractures reaching an in-plane resolution of 80 μm. Bone scintigraphy still plays a role in detecting fractures, with good sensitivity but unsatisfactory specificity. PET-CT with hybrid scanners has been the upcoming modality for the differentiation of benign from malignant fractures. Bone densitometry and clinical fracture history may determine the future risk of possible insufficiency fractures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vertebral Fracture
- Distal Radius Fracture
- Acetabular Fracture
- Insufficiency Fracture
- Renal Osteodystrophy
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 Background
Insufficiency fractures are stress fractures that occur when stress is applied to abnormal, weakened bone with less than the normal elastic resistance. The most prevalent disease leading to insufficiency fractures is postmenopausal osteoporosis, followed by osteomalacia. Unlike the other subtype of stress fractures fatigue fractures are due to normal or physiologic stress on weakened bone. They result from the application of abnormal stress or torque on a bone with normal elastic resistance and strength. Loss of bone trabeculae decreases the bone’s elastic resistance. Awareness is increasing concerning the occurrence of these fractures among older persons. The prevalence of both osteoporosis and osteomalacia increases with age and, in subjects over the age of 90, osteoporosis is found in 71 % of patients and osteomalacia is found in 29 % of patients (Hordon and Peacock 1990). Insufficiency fractures occur most commonly at the pelvic girdle including the sacrum, followed by the proximal femur and the vertebral bodies in particular at the lumbar spine and the lower thoracic spine. Other sites frequently affected by insufficiency fractures are the tibia, fibula, and calcaneus and metatarsal bones (Soubrier et al. 2003). Insufficiency fractures of the femoral diaphyses are rare. Most frequently insufficiency fractures are due to undiagnosed or untreated osteoporosis.
1.2 Pathophysiology
A fracture represents the end result of the spectrum of a bone’s response to an increasing level of stress. According to Wolff’s law, stress that occurs beyond the bone’s elastic range causes persistent plastic deformity as a result of microfractures. In this situation, osteoclastic resorption exceeds osteoblastic activity. A strong association exists between fractures of the sacrum and those of the pubic bone. They can often be found in a symmetrical fashion and are often due to osteomalacia. Pubic fractures may develop as a result of increased anterior arch strain secondary to initial failure of the posterior arch (sacrum). There are many causes of insufficiency fractures including postmenopausal osteoporosis, rheumatoid arthritis, Paget’s disease, osteomalacia, hyperparathyroidism, renal osteodystrophy, osteogenesis imperfecta, osteopetrosis, and fibrous dysplasia. Other important causes are senile osteoporosis or pelvic irradiation and corticosteroid therapy leading to secondary osteoporosis. Also reported are total hip replacement, scurvy, osteopetrosis, primary biliary cirrhosis, organ transplantation, tabes dorsalis, and high dose fluoride therapy (Soubrier et al. 2003).
1.3 Frequency
Most patients with insufficiency fractures are older than 60 years. The mean age ranges from 62 to 74 years (Frey et al. 2007; Peh and Evans 1993; Grasland et al. 1996; Soubrier et al. 2003). Women predominantly are affected especially in the postmenopausal state. On the average insufficiency fractures are estimated to occur in 1–5 % of the population, depending on the referral population (Kanis and Pitt 1992). In most patients, insufficiency fractures resolve or improve significantly with conservative management. However, in recent years interventional procedures using percutaneous cement application have been suggested, in particular of vertebral bodies and the sacrum (Brook et al. 2005; Cho et al. 2010).
1.4 Clinical Presentation
Typically, patients present with acute pain in the groin, back, or buttock, resp. foot or around the knee, depending on the site of the fracture. Twenty-five percent of patients have multiple sites of pain. In many patients, pain is severe enough to render the patient nonambulatory. Usually, patients present with either no history of trauma or a history of low impact trauma. On physical examination usually, signs of insufficiency fracture are nonspecific or nonexistent. Neurologic deficits are rarely found. Typically, a discordance exists between the severe symptoms and the mild or absent physical signs. Management is conservative and consists initially of bed rest, reduced weight bearing, and simple analgesics for pain relief. In severe cases a more aggressive approach can be performed. Imaging-guided sacroplasty for treatment of sacral insufficiency fractures has been described (Frey et al. 2007). Vertebroplasty or kyphoplasty to treat vertebral insufficiency fractures is a common procedure in radiology or orthopaedic departments.
1.5 Locations
1.5.1 Pelvis
Insufficiency fractures of the pelvis are being increasingly recognized as a major cause of low back pain in elderly women with osteoporosis (Fig. 1). Fractures in the sacrum are difficult to diagnose, as plain radiographic findings are sometimes unhelpful or misleading. Bone scintigraphy is very sensitive for the detection of fractures in the sacrum, with demonstration of the H-shaped (or butterfly) sacral pattern or the combination of concomitant sacral and parasymphyseal uptake being considered as a typical finding of insufficiency fractures (Fujii et al. 2005). MRI is a very sensitive method for detecting insufficiency fractures visualizing bone marow edema pattern and frequently also fracture lines. It can be helpful in distinguishing insufficiency from pathologic fractures due to tumour infiltration (Figs. 2, 3). The majority of patients respond well to periods of enforced bed rest and administration of analgesics. Recognition of the spectrum of imaging findings for this entity should lead to its correct identification and the institution of appropriate treatment (Peh et al. 1996). Insufficiency fractures following total hip arthroplasty (THA) frequently occur in the superior and inferior pubic ramus, the puboischial rami, or the ischium around the obturator foramen, while they rarely occur in the medial wall of the acetabulum (Kanaji et al. 2007) (Fig. 4). Computed tomography (CT) is helpful for confirming the presence of fractures in cases with atypical scintigraphic patterns, particularly in those with a known primary malignant neoplasm. CT is especially useful in the further evaluation of parasymphyseal and pubic rami lesions (Figs. 5, 6). Radiotherapy is a well-known risk factor for pelvic insufficiency fractures in postmenopausal women. Recognition of insufficiency fractures helps to avoid the pitfalls of misdiagnosing tumour recurrence or bony metastases (Peh et al. 1995) (Fig. 7).
It should also be noted that multiple pelvic insufficiency fractures are frequently found, particularly in the presence of pubic or acetabular fractures, and careful search for concomitant fractures is warranted. In a previous study in 70.3 % of cases with pelvic insufficiency fractures, multiple fracture sites were present. In the case of pubic fractures in 90 % concomitant fractures were present. Also, 76 % of acetabular fractures had concomitant fractures present (Cabarrus et al. 2008).
1.5.2 Lower Extremity
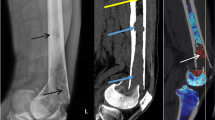
Insufficiency fractures of the fibula are typically found in patients with underlying rheumatic diseases, mainly rheumatoid arthritis (Alonso-Bartolome et al. 1999; Yamamoto et al. 2002) (Figs. 8, 9). Insufficiency fractures are also frequently found at the metatarsal bones in particular in the setting of inflammatory arthropathies (Fig. 10). Also these may be diagnosed in patients with severe osteoporosis, high-dose corticosteroids, or methotrexate therapy. Patients with marked joint deformity are also at high risk for developing insufficiency fractures (Maenpaa et al. 2002). Less frequently, in up to 25 %, insufficiency fractures at the femoral shaft can occur, predominately in elderly patients with osteoporosis (Martin-Hunyadi et al. 2000) (Fig. 11). Insufficiency fractures at the tibia (Fig. 12a–c) may be found as an early manifestation of bone failure in patients after renal transplantation as reported by a previous study (Franco et al. 2003). The main causes are preexisting renal osteodystrophy, glucocorticoid therapy, and hyperparathyroidism, whether residual or secondary to imperfect graft function (Franco et al. 2003). Longitudinal stress fractures of the tibia can also occur in patients with healed chronic osteomyelitis (Feydy et al. 2000). Even postpartum osteoporosis was found to be a cause of insufficiency fractures around the knee (Clemetson et al. 2004).
Patient with history of tumor endoprosthesis at the proximal femur and insufficiency fracture at the proximal tibia. Lateral radiograph of the distal femur and knee shows severe osteopenia but no fracture a. The coronal STIR sequence shows significant bone marrow edema pattern and subtle fracture line at the lateral tibia b. The sagittal T1-w image better demonstrates the fracture line in the same patient c
One of the important differential diagnoses of subchondral insufficiency fractures of the femoral head may include osteonecrosis. Typical MRI findings in insufficiency fractures include a pattern of bone marrow edema with a low-signal-intensity line (resp. fracture) on the T1-weighted images parallel to the subchondral bone. In general, the circumscribed lesions on MRI, which are commonly observed in osteonecrosis, are not found (Yamamoto et al. 2007). Histopathologically fracture callus, reactive cartilage, and granulation tissue is seen without any evidence of antecedent osteonecrosis. The subchondral insufficiency fracture of the femoral head (SIF) is a recently recognized cause of acute onset arthritis mostly in elderly women, which previously had been commonly considered either as osteonecrosis or osteoarthritis.
1.5.3 Spine
Insufficiency fractures at the spine are a leading cause for acute low back pain without an acute traumatic event. Usually a concave or wedge-shaped deformity of the affected vertebra is found and a wide range of the vertebral height ratios and fracture distribution were reported (Kawaguchi et al. 2001). Once an initial vertebral fracture is sustained, the risk of subsequent vertebral fracture increases significantly. However, this effect cannot be explained by low bone mass alone, suggesting that factors independent of this parameter contribute to this occurrence (Briggs et al. 2007). The assessment of vertebral fractures using a semiquantitative approach has been described, grading osteoporotic fractures into type 1 (20–25 % deformity), type 2 (25–40 %), and type 3 (>40 %) (Genant et al. 1993). Accurate radiographic diagnosis of osteoporotic vertebral fractures is important. Several studies indicated a false-negative rate of up to 34 % in reports of lateral radiographs of the thoracolumbar spine (Delmas et al. 2005). Radiologists should be aware of the importance of vertebral fracture diagnosis in assessing future osteoporotic fracture risk. Vertebral fractures incidental to radiologic examinations done for other reasons should be identified and reported, in particular vertebral fractures should be assessed in lateral chest radiographs. Proper training of radiologists is necessary to improve detection of vertebral fractures (Lentle et al. 2007). In oncologic patients differentiation from benign and malignant vertebral fractures is important and can be achieved by MRI or PET-CT (Figs. 13, 14).
Same patient as in Fig. 13 demonstrating multiple vertebral fractures with gibbus at the thoracic spine
1.5.4 Upper Extremity
A common site of fragility fractures is the distal forearm. In addition, fractures involving the wrist are known to be strongly associated with osteoporosis. It is well-known that patients with distal radius fracture who are otherwise healthy have a preferential bone loss at the distal forearm. Distal radius fractures are also associated with generally low bone mass and elevated fracture risk at other skeletal sites. In these subjects pharmacotherapy for osteoporosis is warranted (Mallmin and Ljunghall 1994). Interestingly in osteoporosis the proximal humerus may also be a fracture site at risk (Guggenbuhl et al. 2005).
1.6 Differential Diagnosis
An important differential diagnosis of a stress/insufficiency fracture is a fracture due to malignant disease. MRI features of a malignant fracture are diffusely or focally abnormal bone marrow signal which may be either well-defined or ill-defined and does not follow fracture lines. In addition abnormal intracortical, periosteal, or muscle signal intensity are found as well as endosteal scalloping and soft-tissue masses. The features seen on CT are bone marrow abnormality which may be well-defined, ill-defined, permeative or moth-eaten, endosteal scalloping, periosteal reaction, and a soft-tissue mass. Accuracy for differentiating malignant fractures from stress fractures was reported to be highest with MRI (93–98 %) followed by CT (82–88 %) and radiographs (88–94 %) (Fayad et al. 2005).
1.7 Imaging Methods and Limitations
Radiographs are the initial imaging test in patients with pain localized to the skeleton. If the radiographs are inconclusive and pain persists, either MRI or CT will be performed. Multidetector computed tomography (MDCT) is currently standard and allows multiplanar reconstruction, near isotropic 3D reconstructions of anatomical structures, reduction of artefacts as well as thin-section high-resolution imaging which is beneficial to visualizing also subtle fracture lines. It should be considered, however, that MRI is more sensitive and the imaging modality of choice if the patient history suggests malignant disease and metastasis may be responsible for fracture. Though MRI is very sensitive for detection of fractures, bone marrow changes, and related soft-tissue edema, it should be considered that in the absence of fractures lines or a typical history MRI may also be misleading and suggest other bone marrow pathology such as malignant infiltration. While MRI is the most sensitive technique in the visualization of insufficiency fractures, CT sometimes tends to depict the extent and stability of these fractures better. Bone scintigraphy is highly sensitive, but not specific. Atypical uptake patterns may be difficult to interpret and abnormal uptake may persist for several months.
1.7.1 Radiographs
Radiographic findings depend on the site of the fracture. Parasymphyseal and pubic ramus fractures may have an aggressive appearance that depends on the stage of fracture maturity. Findings include sclerosis, lytic fracture line, bone expansion, exuberant callus, and osteolysis. The most common finding is a sclerotic band or line. A lytic fracture line or cortical break rarely is observed. The degree of confidence is low in sacral fractures because of osteoporosis, overlying bowel gas, and calcified vessels and is better at peripheral sites like in long bones and the metatarsal bones. Parasymphyseal and pubic ramus fractures often are misinterpreted as malignant lesions. Sacral, iliac, and supra-acetabular fractures often are difficult to detect.
1.7.2 Multidetector Computed Tomography
On CT images a linear fracture line with surrounding sclerosis may be observed, but depending on the age of the fracture sometimes only sclerosis may be demonstrated. Pubic fractures may be seen as a lytic fracture line often surrounded by callus. Typically, a soft-tissue mass is absent, bone destruction is lacking, and adjacent fascial planes are preserved. MDCT also is useful for detecting large bony sacral defects such as Tarlov cysts and for the diagnosis of coexisting malignant lesions. MDCT is very specific for the definitive diagnosis of an insufficiency fractures of the pelvis but may have limitations with sensitivity. MDCT is useful as an alternative to bone scintigraphy when radiographs are inconclusive and MRI is not available (Soubrier et al. 2003). Multiplanar CT reformats are essential for the diagnosis of insufficiency fractures of the long bones and pelvic girdle (Junila et al. 1996). Dedicated MDCT-protocols using thin-section MPR’s with adequate overlap and reconstruction kernels are essential for detecting even subtle fractures (Philipp et al. 2003).
In the diagnosis and staging of osteoporosis the 3D bone structure has been shown to be an important predictor of bone strength in addition to bone mass or the mineral content of the bone. Micro-CT scanning has shown promising results in the differentiation of osteoporotic and nonosteoporotic individuals with respect to histomorphometry and quality of trabecular fractures (Heiss et al. 2005).
1.7.3 Magnetic Resonance Imaging
MRI shows decreased signal on T1-weighted images and increased signal on T2-weighted images. In the sacrum, signal changes are seen as linear bands within the sacral ala and body and are parallel to the sacroiliac joints. On T2-weighted images, the fracture line may be seen if it is surrounded by adjacent marrow edema pattern. MRI is highly sensitive and highly specific. MRI cannot be used in patients with pacemakers, a significant limitation in the elderly population. Iliac and sacral bones are frequently involved in patients with osteomalacia. MRI can determine the clinical activity of the disease, and can monitor the response to treatment of insufficiency fractures (Kanberoglu et al. 2005). Diffusion-weighted MRI pulse sequences are capable of differentiating malignant from benign lesions and may be the modality of choice in the near future (Byun et al. 2007).
1.7.4 Nuclear Medicine
In nuclear studies, the typical H-shaped or butterfly pattern of uptake in the sacrum is diagnostic of insufficiency fracture (Abe et al. 1992). The vertical limbs of the H lie within the sacral ala, parallel to the sacroiliac joints, while the transverse limb of the H extends across the sacral body. Other sacral variant uptake patterns occur frequently and include the unilateral ala, incomplete H, and horizontal linear dot patterns. Iliac fractures are seen as linear areas of uptake. PET-CT using F18-FDG combined with MDCT gives metabolic and morphologic information at the same time, allowing the differentiation of pathologic fractures and insufficiency fractures (Figs. 15, 16) (Tsuchida et al. 2006; Halac et al. 2007). Pubic and supra-acetabular fractures produce areas of linear or focal uptake. Concomitant findings of two or more areas of uptake in the sacrum and at another pelvic site are considered diagnostic of insufficiency fractures of the pelvis. Nuclear studies are highly sensitive and highly specific when a typical pattern of sacral uptake or concomitant sacral and pubic uptake is observed. If a typical pattern of abnormality is not present, the bone scan is much less specific. If abnormal or incomplete patterns of uptake are observed, findings may be mistaken for malignancy and other diseases. CT or MR imaging are useful in these cases.
Same patient as in Fig. 13 shows bilateral sclerosis compatible with bilateral insufficiency fractures
1.7.5 Interventional Radiology
Sacroplasty is a variation of the vertebroplasty technique for treatment of a sacral insufficiency fracture. Sacroplasty is a procedure in which polymethylacrylate, a quick-setting bone cement, is injected into the fractured bone. This technique appears to be useful in providing symptomatic relief to affected patients (Garant 2002). Other authors proposed a novel technique in which guidance with CT fluoroscopy allows placement of a transiliosacral bar in conjunction with sacroplasty combining the use of metallic hardware and bone cement for stabilization (Sciubba et al. 2007). There exist numerous publications about the treatment of vertebral fractures with vertebroplasty. Percutaneous vertebroplasty (PV) is a safe and effective treatment for relieving pain in patients complaining of severe back pain induced by osteoporotic compression fractures (Fig. 17). The success rate exceeds 90 % and the complication rate is lower than 1 % (Deramond and Mathis 2002). A substantial number of patients with osteoporosis develop new fractures after undergoing PV; two-thirds of these new fractures occur in vertebrae adjacent to those previously treated (Uppin et al. 2003).
1.8 Summary and Conclusion
Due to the increase in the average age of the population, the number of insufficiency fractures is steadily increasing. The majority of insufficiency fractures is due to weakened bone by osteoporosis. Usually, patients experience the acute onset of pain after an inadequate trauma. Insufficiency fractures can initially be missed on standard radiographs due to subtle findings. It is important to know the most commonly affected sites and the appearance with different radiological modalities. MDCT is superior to radiographs in the diagnosis of insufficiency fractures and should be used, in the case of negative radiographs exams, but high clinical suspicion of an insufficiency fracture. As insufficiency fractures usually occur in elderly patients, radiation dose is not a major concern. MRI should be used as a problem solver to distinguish between pathologic fractures and insufficiency or stress fractures and to monitor the bone marrow edema pattern. Radiographs can also be used for the follow-up of insufficiency fractures and the monitoring of callus formation and bone healing. Nuclear medicine studies gained a big role in the diagnosic work-up, due to the introduction of PET-CT with hybrid scanners in clinical routine. The radiologist’s role nowadays also includes treatment of fractures with an increasing number of vertebroplasties performed each year. Other sites, such as the sacrum, have also been treated and the results seem promising.
References
Abe H et al (1992) Radiation-induced insufficiency fractures of the pelvis: evaluation with 99mTc-methylene diphosphonate scintigraphy. Am J Roentgenol 158(3):599–602
Alonso-Bartolome P et al (1999) Insufficiency fractures of the tibia and fibula. Semin Arthritis Rheum 28(6):413–420
Briggs AM, Greig AM, Wark JD (2007) The vertebral fracture cascade in osteoporosis: a review of aetiopathogenesis. Osteoporos Int 18(5):575–584
Brook AL, Mirsky DM, Bello JA (2005) Computerized tomography guided sacroplasty: a practical treatment for sacral insufficiency fracture: case report. Spine 30(15):E450–E454
Byun WM et al (2007) Diffusion-weighted magnetic resonance imaging of sacral insufficiency fractures: comparison with metastases of the sacrum. Spine 32(26):E820–E824
Cabarrus MC et al (2008) MRI and CT of pelvic insufficiency fractures: morphology, location and associated clinical findings. Am J Roentgenol 191(4):995–1001
Cho CH, Mathis JM, Ortiz O (2010) Sacral fractures and sacroplasty. Neuroimaging Clin N Am 20(2):179–186
Clemetson IA et al (2004) Postpartum osteoporosis associated with proximal tibial stress fracture. Skeletal Radiol 33(2):96–98
Delmas PD et al (2005) Underdiagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res 20(4):557–563
Deramond H, Mathis JM (2002) Vertebroplasty in osteoporosis. Semin Musculoskelet Radiol 6(3):263–268
Fayad LM et al (2005) Distinction of long bone stress fractures from pathologic fractures on cross-sectional imaging: how successful are we? Am J Roentgenol 185(4):915–924
Feydy A et al (2000) A longitudinal insufficiency fracture of the tibia in association with a healed chronic osteomyelitis. Eur Radiol 10(12):1929–1931
Franco M et al (2003) Longitudinal bone insufficiency fracture of the tibia in a renal transplant recipient. Joint Bone Spine 70(4):296–299
Frey ME et al (2007) Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J 8(2):367–373
Fujii M et al (2005) Honda sign and variants in patients suspected of having a sacral insufficiency fracture. Clin Nucl Med 30(3):165–169
Garant M (2002) Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol 13(12):1265–1267
Genant HK et al (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1148
Grasland A et al (1996) Sacral insufficiency fractures: an easily overlooked cause of back pain in elderly women. Arch Intern Med 156(6):668–674
Guggenbuhl P, Meadeb J, Chales G (2005) Osteoporotic fractures of the proximal humerus, pelvis, and ankle: epidemiology and diagnosis. Joint Bone Spine 72(5):372–375
Halac M et al (2007) Avoidance of misinterpretation of an FDG positive sacral insufficiency fracture using PET/CT scans in a patient with endometrial cancer: a case report. Clin Nucl Med 32(10):779–781
Heiss C et al (2005) Micro-CT analysis of cancellous bone fragments from the distal radius fracture zone in osteoporosis. Biomed Tech (Berl) 50(3):60–65
Hordon LD, Peacock M (1990) Osteomalacia and osteoporosis in femoral neck fracture. Bone Miner 11(2):247–259
Junila J, Lakovaara M, Lahde S (1996) Diagnosis of longitudinal stress fracture of the tibia with multiplanar CT reformats: a case report. Rofo 165(3):303–304
Kanaji A et al (2007) Insufficiency fracture in the medial wall of the acetabulum after total hip arthroplasty. J Arthroplasty 22(5):763–767
Kanberoglu K et al (2005) Magnetic resonance imaging in osteomalacic insufficiency fractures of the pelvis. Clin Radiol 60(1):105–111
Kanis JA, Pitt FA (1992) Epidemiology of osteoporosis. Bone 13(Suppl 1):S7–S15
Kawaguchi S et al (2001) Insufficiency fracture of the spine: a prospective analysis based on radiographic and scintigraphic diagnosis. J Bone Miner Metab 19(5):312–316
Lentle BC et al (2007) Recognizing and reporting vertebral fractures: reducing the risk of future osteoporotic fractures. Can Assoc Radiol J 58(1):27–36
Maenpaa HM et al (2002) Insufficiency fractures in patients with chronic inflammatory joint diseases. Clin Exp Rheumatol 20(1):77–79
Mallmin H, Ljunghall S (1994) Distal radius fracture is an early sign of general osteoporosis: bone mass measurements in a population-based study. Osteoporos Int 4(6):357–361
Martin-Hunyadi C et al (2000) Spontaneous insufficiency fractures of long bones: a prospective epidemiological survey in nursing home subjects. Arch Gerontol Geriatr 31(3):207–214
Peh WC, Evans NS (1993) Pelvic insufficiency fractures in the elderly. Ann Acad Med Singapore 22(5):818–822
Peh WC et al (1995) Sacral and pubic insufficiency fractures after irradiation of gynaecological malignancies. Clin Oncol (R Coll Radiol) 7(2):117–122
Peh WC et al (1996) Imaging of pelvic insufficiency fractures. Radiographics 16(2):335–348
Philipp MO et al (2003) Four-channel multidetector CT in facial fractures: do we need 2 × 0.5 mm collimation? Am J Roentgenol 180(6):1707–1713
Sciubba DM et al (2007) CT fluoroscopically guided percutaneous placement of transiliosacral rod for sacral insufficiency fracture: case report and technique. Am J Neuroradiol 28(8):1451–1454
Soubrier M et al (2003) Insufficiency fracture. A survey of 60 cases and review of the literature. Joint Bone Spine 70(3):209–218
Tsuchida T et al (2006) Sacral insufficiency fracture detected by FDG-PET/CT: report of 2 cases. Ann Nucl Med 20(6):445–448
Uppin AA et al (2003) Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology 226(1):119–124
Yamamoto T, Takabatake K, Iwamoto Y (2002) Subchondral insufficiency fracture of the femoral head resulting in rapid destruction of the hip joint: a sequential radiographic study. Am J Roentgenol 178(2):435–437
Yamamoto T et al (2007) Histopathologic prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis 67(2):150–153
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Krestan, C.R., Nemec, U., Nemec, S. (2013). Imaging of Insufficiency Fractures. In: Guglielmi, G. (eds) Osteoporosis and Bone Densitometry Measurements. Medical Radiology(). Springer, Berlin, Heidelberg. https://doi.org/10.1007/174_2012_613
Download citation
DOI: https://doi.org/10.1007/174_2012_613
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-27883-9
Online ISBN: 978-3-642-27884-6
eBook Packages: MedicineMedicine (R0)