Abstract
Functional characterization of endolysosomal ion channels is challenging due to their intracellular location. With recent advances in endolysosomal patch clamp technology, it has become possible to directly measure ion channel currents across endolysosomal membranes. Members of the transient receptor potential (TRP) cation channel family, namely the endolysosomal TRPML channels (TRPML1-3), also called mucolipins, as well as the distantly related two-pore channels (TPCs) have recently been characterized in more detail with endolysosomal patch clamp techniques. However, answers to many physiological questions require work in intact cells or animal models. One major obstacle thereby is that the known endogenous ligands of TRPMLs and TPCs are anionic in nature and thus impermeable for cell membranes. Microinjection, on the other hand, is technically demanding. There is also a risk of losing essential co-factors for channel activation or inhibition in isolated preparations. Therefore, lipophilic, membrane-permeable small-molecule activators and inhibitors for TRPMLs and TPCs are urgently needed. Here, we describe and discuss the currently available small-molecule modulators of TRPMLs and TPCs.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Transient receptor potential (TRP) channels represent potential targets for the treatment of various diseases. Several members of the TRP channel family have been investigated as potential targets for the treatment of neuropathic and other pain conditions and more than 20 drugs targeting TRPV1, TRPV2, TRPM8, or TRPA1 are still under active clinical development (Weyer-Menkhoff and Lotsch 2018; Dietrich 2019). Other disease areas with TRP channels as potential drug targets are: bladder dysfunctions (Birder 2007), inflammatory bowel disease (Zhang and Li 2014), pulmonary oedema (TRPV4) (Thorneloe et al. 2012), hyperkeratosis, inflammatory skin disorders with itch and/or pain (TRPV3) (Imura et al. 2009; Yoshioka et al. 2009; Lin et al. 2012), prostate cancer (TRPM8) (Zhang and Barritt 2006), inflammation, infection (Parenti et al. 2016), ischaemia reperfusion (Ma et al. 2017), Alzheimer’s disease (TRPM2) (Jiang et al. 2018a), chronic cough and asthma (TRPA1) (Belvisi and Birrell 2017), lysosomal storage disorders and neurodegenerative diseases (TRPML1; (Huang and Szallasi 2017)).
In the past decade, remarkably many highly potent and efficacious agonists and antagonists for TRP channels have been developed by the pharmaceutical industry. Meanwhile, many of these compounds have become commercially available. Some of them, e.g. PF-4840154 (TRPA1 agonist) (Ryckmans et al. 2011), GSK1016790A (TRPV4 agonist) (Thorneloe et al. 2008), WS-12 (TRPM8 agonist) (Sherkheli et al. 2008), AMG9810 and AMG517 (TRPV1 antagonists) (Gavva et al. 2005, 2008), GSK2193874 (TRPV4 antagonist) (Cheung et al. 2017), ML204 and HC-070 (TRPC4/5 antagonists) (Miller et al. 2011; Just et al. 2018) are presented in Fig. 1.
For the endolysosomal TRPML channels (TRPML1-3; mucolipins 1-3) and the distantly related two-pore channels (TPCs) no agonists/antagonists, albeit under development have been released by the pharmaceutical industry so far. Several compounds are however available as a result of high-throughput screening (HTS) efforts by academic institutions. Here, we describe and discuss in the first part the currently available TRPML channel agonists and antagonists and give an overview of the general characteristics of the three TRPML channel subfamily members. In the second part, we focus on general characteristics of the endolysosomal TPCs (TPC1 and TPC2) and present small molecules, which are currently available for their activation or inhibition.
2 Small-Molecule Tools for the Modulation of TRPMLs
The TRPML subfamily of TRP channels comprises three members in mammals. Loss or mutation of TRPML1 in humans and mice results in severe neurodegeneration as well as corneal clouding and retinal degeneration, which eventually leads to blindness (mucolipidosis type IV phenotype; (Bargal et al. 2000)). Gain-of-function mutations in TRPML3 cause deafness and circling behaviour in mice (varitint-waddler phenotype; (Di Palma et al. 2002; Xu et al. 2007; Nagata et al. 2008; Kim et al. 2007; Grimm et al. 2007, 2009)). TRPML2 enhances viral entry, viral trafficking, and thus infection with viruses such as yellow fever virus, Dengue virus, influenza A virus, or equine arteritis virus. The mutation K370Q within TRPML2 is found at higher frequencies in African populations compared to other geographic populations and leads to a loss of viral enhancement (Rinkenberger and Schoggins 2018).
The phosphoinositide phosphatidylinositol 3,5-bisphosphate (PI(3,5)P2; Fig. 2), a major constituent of endolysosomal membranes has been described in 2010 as the first endogenous activator of TRPML channels (Dong et al. 2010). In contrast, phosphatidylinositol 4,5-bisphosphate (PI(4,5)P2; Fig. 2), which mainly occurs in the plasma membrane, was identified as an inhibitor of TRPML channels (Zhang et al. 2012); Tables 1, 2, and 3.
PI(3,5)P2 is present in both Rab5 positive early endosomes (EE) as well as Rab7 positive late endosomes (LE) and lysosomes (LY; (Takatori et al. 2016)). Defects in PI(3,5)P2 signalling are linked to human diseases such as Charcot–Marie–Tooth disease and amyotrophic lateral sclerosis. Cryo electron microscopy (Cryo-EM) revealed that PI(3,5)P2 and PI(4,5)P2 bind to the extended helices of transmembrane domains S1, S2, and S3 of TRPML1. The phosphate group of PI(3,5)P2 induces amino acid Y355 to form a π–cation interaction with R403, moving the S4–S5 linker, thus allosterically activating the channel (Fine et al. 2018). This is different from the PI(3,5)P2 binding observed in TPC1. Here PI(3,5)P2 binds to the first S6 domain (She et al. 2018).
In addition to phosphoinositides in the membrane of endo-lysosomes, the proton concentration in the lumen of endo-lysosomes controls TRPML channel activity. TRPML1 activity is enhanced by protons (acidic pH; (Dong et al. 2008; Chen et al. 2014)), while TRPML2 and TRPML3 activity is reduced by protons (Kim et al. 2008; Grimm et al. 2012; Miao et al. 2015; Lev et al. 2010; Plesch et al. 2018). Further regulators of TRPML1 channel activity are sphingomyelin, which inhibits TRPML1 activity in NPC1 (Niemann Pick type C1) cells (Shen et al. 2012), adenosine (Zhong et al. 2017), reactive oxygen species (ROS; (Zhang et al. 2016)), and TOR kinase via phosphorylation of the TRPML1 channel (Onyenwoke et al. 2015).
Several synthetic ligands have become available in recent years for TRPML1, 2, and 3 as a result of high-throughput screening (HTS) and medicinal chemistry efforts, which have been discussed in detail before (Grimm et al. 2010, 2012, 2014a; Yamaguchi and Muallem 2010; Saldanha et al. 2011; Shen et al. 2012; Cuajungco et al. 2014; Chen et al. 2014; Kilpatrick et al. 2016). TRPML channel activators identified in the HTS belong to different substance families including (hetero)arylsulfonamides (e.g. SN-1, SF-11, SF-21, SF-22, and MK6-83; (Chen et al. 2014)), phthalimidoacetamides (SF-51 and ML-SA1; (Shen et al. 2012)), isoxazol(in)es (e.g. SN-2, ML2-SA1, EVP-21), and others (Grimm et al. 2010, 2012, 2014a; Saldanha et al. 2011, 2013; Cuajungco et al. 2014; Kilpatrick et al. 2016); Fig. 3).
Small-molecule TRPML activators. (a) TRPML3 activators with the structural motif of (hetero)arylsulfonamides (highlighted in pink). SN-1, SF-11, and SF-21 only share an aryl sulfonamide moiety, whereas SF-22 and MK6-83 only differ in the substituent at the thiophene residue. (b) The dihydroquinoline SF-51 and the tetrahydroquinoline ML-SA1 both sustain phthalimidoacetamide moieties (blue) and only differ in one double bond. ML1-SA1 (= EVP-169) contains a tetrachlorophthalimidoacetamide moiety instead of a phthalimidoacetamide moiety in SF-51 and ML-SA1. ML-SA1 activates all human TRPML isoforms while SF-51 preferentially activates TRPML3 and ML1-SA1 selectively TRPML1. (c) The isoxazoline (green) SN-2 and selective TRPML2 activator ML2-SA1 (= EVP-22) differ merely in the substitution pattern of the phenyl ring. ML3-SA1 (= EVP-77) is a selective activator for mouse TRPML3 and contains a fused oxane ring instead of a fused norbornane ring in SN-2. (d) Selective TRPML3 activator EVP-21 with an isoxazole (orange) as structural motif (selective for human TRPML3)
Besides their structural differences, these activators also differ in activity and selectivity. While the tetrahydroquinoline ML-SA1 activates all human TRPML channel isoforms, and TRPML1 and TRPML3 in mouse, its dehydro analogue SF-51 preferentially activates TRPML3 (Grimm et al. 2010). A small modification of SF-22 (from 2-chlorothiophene in SF-22 into 2-methylthiophene in MK6-83) results in strongly increased activity. Nevertheless, both SF-22 and MK6-83 activate mouse and human TRPML1 and TRPML3 (Chen et al. 2014).
Although the structural differences between SN-2 and ML2-SA1 are rather small, they result in this case in very different selectivities within the TRPML family. SN-2, however, is preferentially activating TRPML3, while ML2-SA1 (EVP-22) is a selective agonist of TRPML2. All modifications are a result of systematic analysis of structure–activity relationships (Plesch et al. 2018; Grimm et al. 2010; Chen et al. 2014). MK6-83 has an EC50 of 0.1 μM for hTRPML1 in calcium imaging experiments (i.e. in intact cells), while ML2-SA1 has an EC50 of 1.2 μM for hTRPML2, and SN-2 showed an EC50 of 1.8 μM for hTRPML3 (Grimm et al. 2010, 2014a; Chen et al. 2014). A further modified congener of the isoxazoline SN-2, which selectively activates hTRPML3, is the isoxazole EVP-21, an aromatic analogue of SN-2 with an annulated cyclohexane moiety instead of a bicycloheptane moiety (Plesch et al. 2018). Although EVP-21 has a higher EC50 (4.3 μM in calcium imaging experiments), it shows an increased efficacy and selectivity on human TRPML3 over human TRPML1 and human TRPML2 compared to SN-2. EVP-21 can elicit TRPML3 currents in both LE/LY and EE (Fig. 4).
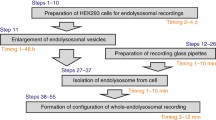
TRPML3 agonist EVP-21. Characteristics assessed in calcium imaging as well as in endolysosomal patch clamp experiments. (a) Structures of SN-2 and its analogous compound EVP-21. (b) Concentration-effect curves (CEC) obtained from Fura-2-AM calcium imaging experiments after application of EVP-21 at different concentrations. CEC shows the effect of EVP-21 on hTRPML1, 2, and 3. (c, d) Results of whole-LE/LY patch clamp recordings and (e, f) whole-EE patch clamp recordings using ramp protocols (−100 to +100 mV in 500 ms, every 5 s, holding potential 0 mV). For measurement, organelles (LE/LY (YM201636-enlarged) and EE (wortmannin/latrunculin B-enlarged)) were isolated from hTRPML3-YFP stably expressing HEK293 cells. Shown are representative EVP-21 stimulated TRPML3 currents in LE/LY (c) and EE (e). Pipette (luminal) solution contained 140 mM K-MSA, 5 mM Na-MSA, 2 mM Ca-MSA, 1 mM CaCl2, and 10 mM HEPES. Bath (cytoplasmic) solution contained 140 mM K-MSA, 5 mM KOH, 4 mM NaCl, 0.39 mM CaCl2, 1 mM EGTA, and 10 mM HEPES. The current amplitudes at −100 mV were extracted from individual ramp current recordings with and without agonist. In (d) currents were normalized to those obtained without agonists. (f) Statistical analysis of currents as shown in (e). In all statistical analysis of endo-lysosome recordings, mean values of n (in parentheses) independent experiments are shown as indicated. ***p < 0.001, *p < 0.05, Student’s t test, unpaired
Very recently, new selective agonists for TRPML1 and mouse TRPML3 were published (Spix et al. 2022). Thus, EVP-169 (ML1-SA1) selectively activates human and mouse TRPML1. EVP-77 (ML3-SA1) selectively activates mouse TRPML3 (Spix et al. 2022) (Fig. 3).
Wang et al. (2015) further published a TRPML activator, the aryl-bis-sulfonamide ML-SA3 with increased potency compared to ML-SA1. However, the stereochemistry of this compound on the cyclohexane ring was not further specified. More recently, another TRPML activator, ML-SA5, another aryl-bis-sulfonamide, was described ((Yu et al. 2020), Fig. 5).
Besides TRPML channel agonists, synthetic small molecules for TRPML channel inhibition named ML-SI1, ML-SI2, and ML-SI3 were reported (Samie et al. 2013; Chen et al. 2014; Wang et al. 2015; Zhang et al. 2016; Kilpatrick et al. 2016). Only for two of these three compounds (ML-SI1 and ML-SI3) the chemical structures have been released (Wang et al. 2015). Unfortunately, it remained unclear from the original publication which of the stereoisomers of ML-SI1 and ML-SI3 are functionally active. Possible diastereomers would have cis or trans configuration and each of them can further occur in two enantiomeric forms (R,R or S,S for trans; R,S or S,R for cis) for its absolute configuration. We have synthesized both compounds, compared them with commercially available variants and analysed their activity on the TRPML isoforms.
ML-SI1, as published by Wang et al. (2015), is based on an indoline moiety and cannot be purchased from commercial providers. In contrast, commercially available GW405833 (CAS number: 18002-83-9), which was formerly (erroneously) offered as ML-SI1, is based on a fully aromatic indole framework (Fig. 6a). To elucidate which one of the two structures is able to block TRPML channels, we synthesized the indoline version of ML-SI1 and purchased the indole version (GW405833) of ML-SI1. ML-SI1 was synthesized as a racemic mixture of diastereomers, containing four different stereoisomers (cis/trans and enantiomers of each). Calcium imaging experiments confirmed blocking effect of indoline ML-SI1 on TRPML1 (32% inhibition) and TRPML2 (33% inhibition) after activation with ML-SA1, whereas TRPML3 could not be blocked. Further experiments showed different blocking activities after activation with MK6-83. While ML-SI1 can block 45% of TRPML1 activity after stimulation with ML-SA1, the blocking effect after activation with MK6-83 is only around 20%. These results indicate that the antagonistic effect of ML-SI1 depends on the mode of activation. The commercially available indole analogue GW405833 showed no effect in patch clamp experiments on TRPML1 after activation with ML-SA1 (Fig. 6). There are, up to now, no data for the four single stereoisomers of the active indoline ML-SI1 available.
Small-molecule TRPML inhibitor ML-SI1 and its indole-type analogue GW405833. Characteristics assessed in calcium imaging as well as in endolysosomal patch clamp experiments. (a) Structure of racemic cis/trans-ML-SI1, with an indoline scaffold and commercially available, achiral indole GW405833. (b) In contrast to ML-SI1 GW405833 (10 μM) has no effect on hTRPML1-YFP transfected HEK-293 cells after activation with ML-SA1 (10 μM) in patch clamp experiments. Experimental conditions were applied as in Fig. 4c with the exception that pipette (luminal) solution contained 140 mM Na-MSA (Chen et al. 2017), 5 mM K-MSA, 2 mM Ca-MSA, 1 mM CaCl2, 10 mM HEPES, and 10 mM MES at pH 4.6 (Chen et al. 2017). (c) Statistical analysis of the inhibitory effect on TRPMLs in Fura-2-AM calcium imaging experiments (normalized activation). Experiments were carried out as previously described (Plesch et al. 2018) on a Polychrome IV monochromator (for hTRPML1) or a Leica DMi8 live cell microscope (for TRPML2 and 3). After stimulation with ML-SA1 (10 μM, activation) for 200 s, the inhibitor ML-SI1 (10 μM) was applied for further 200 s. For measurements HEK-293 cells stably expressing hTRPML2-YFP or hTRPML3-YFP, and transiently transfected hTRPML1-YFP cells were used (Grimm et al. 2010). Stably expressing hTRPML2-YFP cells were generated as previously described (Chen et al. 2014). (d) Statistical analysis as in (c), using ML-SA1 (10 μM, red) or MK6-83 (10 μM, green) for activation of hTRPML1ΔNC-YFP (plasma membrane variant of TRPML1) transiently transfected HEK-293 cells, followed by inhibition using ML-SI1 (10 μM). (e) Representative Ca2+ signals recorded from hTRPML1-YFP transiently transfected HEK-293 cells, loaded with Fura-2-AM and stimulated with ML-SA1 (10 μM, red) or MK6-83 (10 μM, green), followed by addition of the inhibitor ML-SI1 (10 μM). Highlighted lines represent means, shaded lines single cell traces. In all statistical analyses of calcium imaging experiments, mean values of n (in parentheses) independent experiments are shown as indicated. *** indicates p < 0.001, ** indicates p < 0.01, * indicates p < 0.05, ns = not significant, one-way ANOVA test followed by Tukey’s post-hoc test
The second TRPML inhibitor published by Wang et al. (2015) is the aryl-sulfonamide ML-SI3. Commercially available ML-SI3 (CAS No.: 891016-02-7) was identified as racemic mixture of trans-isomers by NMR spectrometry. Further confirmation of the stereochemistry was provided by independent synthesis of (±)-trans-ML-SI3 in our laboratory (Leser et al. 2021). Inhibitory effects of ML-SI3 were analysed via calcium imaging and endolysosomal patch clamp experiments. Like ML-SI1, ML-SI3 is inhibiting ML-SA1 activated TRPML1 and 2 channels (55% and 66% inhibition), but not TRPML3. Also, in endolysosomal patch clamp experiments, ML-SI3 showed strong inhibitory effect on hTRPML2 after activation with the TRPML2 specific agonist ML2-SA1. Furthermore, no difference in the inhibitory effect was observed after activation with different TRPML activators. ML-SI3 was able to block hTRPML1 after activation with both ML-SA1 and MK6-83 (Fig. 7). Furthermore, an activating effect of the racemic mixture of trans-ML-SI3 on hTRPML2 could be observed. Separation of the enantiomers of trans-ML-SI3 by chiral HPLC showed that exclusively the (+)-trans-ML-SI3 is responsible for this activation, which in enantiopure form activates hTRPML2 (EC50: 2.8 μM) and hTRPML3 (EC50: 11 μM) whereas it inhibits hTRPML1 (IC50: 5.6 μM). Very recently, we assigned the (R,R)-configuration to the active (+)-trans enantiomer by unambiguous chiral synthesis and single-crystal X-ray structure analysis (Kriegler et al. 2022). The (−)-trans-ML-SI3 has, however, a pure inhibitory effect on all three subtypes (IC50 (hTRPML1):1.4 μM; IC50 (hTRPML2): 2.2 μM; IC50 (hTRPML3):11 μM) and is also the eutomer on TRPML1 (IC50 of the racemic mixture: 2.7 μM). The racemic mixture of cis-ML-SI3 has a weaker inhibitory effect on hTRPML1 (IC50: 19 μM) and activates TRPML2 (EC50: 8.9 μM) and TRPML3 (EC50: 27 μM). All EC50 and IC50 values were determined by a Fluo-4 calcium-imaging based FLIPR (Fluorescence Imaging Plate Reader) system using ML-SA1 as activator (Leser et al. 2021).
Small-molecule TRPML inhibitor ML-SI3. Characteristics assessed in calcium imaging as well as in endolysosomal patch clamp experiments. (a) Racemic mixture of trans-isomers of ML-SI3 identified as an active species. (b) Patch clamp experiments show block of hTRPML2-YFP transiently transfected HEK-293 cells with ML-SI3 (10 μM) after activation with the TRPML2 selective agonist ML2-SA1 (10 μM) as described in Fig. 4c. Pipette (luminal) solution contained 140 mM Na-MSA, 5 mM K-MSA, 2 mM Ca-MSA, 1 mM CaCl2, 10 mM HEPES, and 10 mM MES at pH 7.2. (c) Statistical analysis of ML-SI3 (10 μM) after activation of hTRPML1, 2, or 3 with ML-SA1 (10 μM, activation), as described in Fig. 5c. (d) Statistical analysis as in (c), using ML-SA1 (10 μM, blue) or MK6-83 (10 μM, green) for activation of hTRPML1-YFP transiently transfected HEK-293 cells, followed by inhibition using ML-SI3 (10 μM). (e) Representative Ca2+ signals recorded from hTRPML1-YFP transiently transfected HEK-293 cells, loaded with Fura-2-AM and stimulated with ML-SA1 (10 μM, blue) or MK6–83 (green, 10 μM), followed by addition of the inhibitor ML-SI3 (10 μM). Highlighted lines represent means, shaded lines single cell trances. In all statistical analyses of calcium imaging experiments, mean values of n (in parentheses) independent experiments are shown as indicated. *** indicates p < 0.001, ** indicates p < 0.01, ns = not significant, one-way ANOVA test followed by Tukey’s post-hoc test
Comparing the two TRPML inhibitors, ML-SI3 seems more potent, as its blocking effect on hTRPML1 is about 55% while the blocking effect of ML-SI1 on hTRPML1 is around 32%. Drawbacks of these compounds are their lack of selectivity and the activator-dependent effects.
Ou et al. (2020) have used a not further specified TRPML(1) inhibitor named “130” without disclosing its structure or source, and without any information on isoform selectivity.
Very recently (Rühl et al. 2021), we have presented novel TRPML1 isoform selective blockers which are based on the identification of a steroidal lead structure (EDME, 17β-estradiol methyl ether) in a high-throughput screening of a library of drug-like small-molecule compounds containing numerous FDA-approved drugs. Based on this screening hit we developed, by systematic structure variations, the advanced analogues PRU-10 and PRU-12 (Fig. 8). In whole-cell patch clamp experiments using EDME and the plasma membrane variant of TRPML1 (TRPML1ΔNC) the IC50 measured for TRPML1 was 0.22 μM. No block for TRPML3 was found with this compound. TRPML2 was blocked with an IC50 of 3.8 μM. For comparison, in analogous patch clamp experiments ML-SI3 blocked TRPML1 with an IC50 of 4.7 μM and TRPML2 with an IC50 of 1.7 μM, suggesting that ML-SI3 has an almost threefold stronger effect on TRPML2 compared to TRPML1 and is >20-fold weaker on TRPML1 than EDME. The synthetic analogues PRU-10 and PRU-12 showed a further improved selectivity profile compared to EDME (Rühl et al. 2021).
In the following, we present a summary of the characteristics of the three TRPML isoforms and the presently available modulators.
3 Small-Molecule Tools for the Modulation of TPCs
Two-pore channels (TPCs, TPCNs) are only distantly related to the TRPML channels in terms of sequence similarities, but both channel families share a number of functional features. Both TRPMLs and TPCs are non-selective cation channels in endo-lysosomes, they are permeable to sodium and calcium, they are activated by PI(3,5)P2, and both are involved in endolysosomal trafficking, autophagy, TFEB (Transcription Factor EB) and mTOR signalling (Grimm et al. 2018). TPCs have been shown to be activated by NAADP (nicotinic acid adenine dinucleotide phosphate; (Brailoiu et al. 2010; Calcraft et al. 2009; Ogunbayo et al. 2011; Grimm et al. 2014b; Jha et al. 2014; Pitt et al. 2014; Ruas et al. 2015a)), although it remained unclear until recently whether activation is mediated directly or indirectly, e.g. via an auxiliary subunit (Walseth et al. 2012; Lin-Moshier et al. 2012; Morgan and Galione 2014; Morgan et al. 2015; Ruas et al. 2015b; Gerasimenko et al. 2015; Pitt et al. 2016; Grimm et al. 2017; Nguyen et al. 2017; Jiang et al. 2018b). In 2021, two groups have published independently neurological expressed 1-like protein (HN1L) or Jupiter microtubule-associated homologue 2 (JPT2) as NAADP binding protein. However, interaction was only confirmed for TPC1 but not TPC2, leaving open the question how NAADP acts on TPC2 (Gunaratne et al. 2021; Roggenkamp et al. 2021). Both activators PI(3,5)P2 and NAADP are not plasma membrane permeable. A commercially available variant of NAADP, NAADP-AM (a lipophilic acetoxymethyl (AM) ester prodrug, Fig. 9) is plasma membrane permeable (Parkesh et al. 2008; Galione et al. 2014), but due to its instability very limited in use. Hence, there was an urgent need for lipophilic, plasma membrane-permeable small-molecule activators of TPCs.
Recently, small-molecule activators for TPCs have been identified by two independent groups. Zhang et al. (2019) identified tricyclic antidepressants (TCAs: clomipramine, desipramine, imipramine, amitriptyline, and nortriptyline), phenothiazines (chlorpromazine, triflupromazine), and the benzothiazole riluzole by screening Sigma’s LOPAC library (Fig. 10). All of these compounds are registered drugs and are able to activate TPC2 with EC50 values between 43 and 112 μM in whole-cell patch clamp experiments. While clomipramine and desipramine can additionally activate TPC1, chlorpromazine and riluzole inhibit TPC1. Furthermore, currents evoked with the TCAs and phenothiazines were strongly voltage-dependent while the activation using riluzole was voltage-independent. This suggests different agonist-specific gating mechanisms within one ion channel. TCAs were introduced to treat depression, bipolar and panic disorder, chronic pain, and insomnia. Additionally, they block monoamine (dopamine, norepinephrine, and serotonin) reuptake and inhibit cholinergic, histaminic, and alpha-adrenergic transmission. Due to the broad range of adverse effects TCAs were meanwhile mostly replaced as antidepressants by the selective serotonin reuptake inhibitors (Trindade et al. 1998; Shelton 2019). For amitriptyline, imipramine, and clomipramine it is reported that they are potent CYP450 inhibitors, that block CYP450 2C19 and 1A2, which raises the risk of undesired drug–drug interactions (Gillman 2007; Gerndt et al. 2020b). Riluzole is an FDA-approved drug, which is used for the treatment of amyotrophic lateral sclerosis (ALS) (Bissaro and Moro 2019; Liu and Wang 2018) and furthermore blocks tetrodotoxin-sensitive Na+ channels (Song et al. 1997), kainite and NMDA (N-methyl-D-aspartate) receptors (Hubert et al. 1994; Debono et al. 1993; Malgouris et al. 1994).
hTPC2 agonists published by Zhang et al. (2019). (a) Structures of the TCAs as hTPC2 activators and EC50 values. (b) Structures of the phenothiazines and their EC50 values as hTPC2 activators. (c) Structure of the hTPC2 agonist riluzole
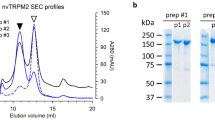
Another HTS was performed by our consortium (Gerndt et al. 2020a), screening the 80.000 compound-strong Roche Explore libraries. Two differentially acting lipophilic small-molecule agonists of TPC2, namely TPC2-A1-N and TPC2-A1-P (Fig. 11a, b) were identified in calcium imaging experiments using the calcium indicator dye Fluo-4-AM, followed by re-evaluation in single cell calcium imaging using Fura-2-AM (Fig. 11 a, b). EC50 values in fluorescence-based calcium imaging experiments were 7.8 μM (TPC2-A1-N) and 10.5 μM (TPC2-A1-P), while EC50 values in electrophysiological endolysosomal patch clamp experiments were both 0.6 μM. Both compounds neither activated TPC1 nor activated TRPML1, 2, and 3 (Fig. 11c–f). In addition, it was shown that the activators mimicked the activation of NAADP (TPC2-A1-N) and PI(3,5)P2 (TPC2-A1-P), respectively, rendering the channel either more calcium-(TPC2-A1-N) or more sodium-(TPC2-A1-P) permeable. TPC2-A1-N itself is known as anthelmintic agent (Sjogren et al. 1991), while there is no previous report on TPC2-A1-P in literature.
Confirmation of TPC2-A1-N and TPC2-A1-P as TPC2 activators (Gerndt et al. 2020a). (a, b) Structures of the activators and representative calcium signals, recorded from HEK-293 cells transiently transfected with plasma membrane targeted human TPC2 (hTPC2L11A/L12A) and loaded with Fura-2-AM. Cells were activated with TPC2-A1-N (10 μM) or TPC2-A1-P (10 or 30 μM). Highlighted lines represent the mean response from a population of cells. Shaded traces represent responses of single cells. (c, d) Experiments as in a-b but cells were transiently transfected with human hTRPML1ΔNC-YFP (plasma membrane variant of TRPML1) and sequentially stimulated with TPC2-A1-N (10 μM) or TPC2-A1-P (30 μM) and the TRPML agonist ML-SA1 (10 μM). (e, f) Experiments as in (c, d), but cells were transiently transfected with human TRPML2, or TRPML3. Cells were sequentially stimulated with TPC2-A1-N (10 μM) or TPC2-A1-P (30 μM) and the TRPML agonist ML-SA1 (10 μM) or the TRPML2 selective agonist ML2-SA1 (10 μM)
While there is comprehensive knowledge on the pharmacological profiles of TCAs, phenothiazines, and riluzole, due to their long-term application in therapy, the newly identified activators TPC2-A1-N and TPC2-A1-P (Fig. 11) require an in-depth pharmacokinetic and pharmacological characterization. On the other hand, TCAs are known for their unwanted side effects and also seem to be less potent activators of TPC2 with much higher EC50 values compared to TPC2-A1-N and TPC2-A1-P.
Several TPC inhibitors have been proposed in the past. TPC activity can be blocked by commercially available trans-Ned-19 ((Naylor et al. 2009; Kelu et al. 2015; Nguyen et al. 2017); Fig. 12). In 2016, Kintzer and Stroud presented an X-ray structure of trans-Ned-19 bound to TPC1 from Arabidopsis thaliana and claimed direct interaction with the ligand involving F229 in S5, W232 in S5, L255 in P1, F444 in S7, and W647 in S12, thus clamping the pore domains and VSD2 (voltage-sensing domain 2) together (Kintzer and Stroud 2016). This results in an allosteric block of channel activation. The validity of these data has however been a matter of debate since then.
Besides trans-Ned-19, several other compounds have been shown to block TPCs: ATP (via mTOR (Cang et al. 2013)), the bisbenzylisoquinoline alkaloid tetrandrine (Sakurai et al. 2015; Nguyen et al. 2017), the flavonoids naringenin (Pafumi et al. 2017), pratensein (MT-8), and duartin (UM-9) (Netcharoensirisuk et al. 2021) as well as the marketed drugs fluphenazine and raloxifene ((Penny et al. 2019); Fig. 12).
The herbal alkaloid tetrandrine (isolated from Stephania tetrandra, Menispermaceae) is known to also block voltage-gated Ca2+ channels, large-conductance Ca2+-activated K+ (BK) channels, and intracellular Ca2+ pumps (sarcoplasmic reticulum Ca2+-ATPase pumps; (Wang et al. 2004)). For naringenin it has been shown that it also blocks TRPM3 (Straub et al. 2013), voltage-gated sodium channels (Gumushan Aktas and Akgun 2018), cardiac HERG (human Ether-à-go-go-Related Gene; Kv11.1) channels (Scholz et al. 2005), HMG-CoA (3-hydroxy-3-methylglutaryl-CoA) reductase, and ACAT (acetyl-CoA-acetyltransferase; (Lee et al. 1999)), and it enhances the activity of large-conductance Ca2+-activated K+ (BK) channels (Hsu et al. 2014). Likewise, the flavonoids pratensein and duartin may have other channel and non-channel targets. However, in contrast to naringenin (IC50 = 74 μM for hTPC2), the IC50s for pratensein and duartin are much lower, 2.6 μM and 9.5 μM, respectively (Netcharoensirisuk et al. 2021). Fluphenazine is an anti-psychotic drug used to treat psychotic disorders such as schizophrenia. Fluphenazine, like chlorpromazine and haloperidol, belongs to the first generation of antipsychotics and has a number of severe adverse effects, in particular extrapyramidal effects including acute dystonia, akathisia, Parkinsonism, and tardive dyskinesia (Divac et al. 2014). Fluphenazine blocks postsynaptic mesolimbic dopaminergic D1 and D2 receptors in brain. It also blocks neuronal voltage-gated sodium channels (Zhou et al. 2006) and the ATP-sensitive K+ channel (Müller et al. 1991). Penny et al. 2019 reported an IC50 of 8.2 μM in patch clamp experiments after TPC2 stimulation with PI(3,5)P2. Raloxifene has an IC50 of 0.63 μM in patch clamp experiments after TPC2 stimulation with PI(3,5)P2 (Penny et al. 2019). Raloxifene belongs to the class of selective oestrogen receptor modulators (SERM) and is used for the treatment and prevention of osteoporosis in postmenopausal women, for reduction in risk of invasive breast cancer in postmenopausal women with osteoporosis and those at high risk for breast cancer. Raloxifene also inhibits L-type and T-type voltage-sensitive Ca2+ channels (Tsang et al. 2004; Wang et al. 2011) as well as Kv4.3 channels (Chae et al. 2015).
Other reported compounds which interfere with NAADP-mediated calcium signalling are BZ194, an N-alkylated nicotinic acid derivative (Dammermann et al. 2009), and pyridoxalphosphate-6-azophenyl-2′,4′-disulfonic acid (PPADS; (Singaravelu and Deitmer 2006; Billington and Genazzani 2007)). For both compounds, no direct measurements of TPC inhibition are published, in particular no endolysosomal patch clamp recordings are currently available.
In 2021, Müller et al. reported about novel TPC2 blockers SG-005 and SG-094, which represent truncated analogues of the bisbenzylisoquinoline alkaloid tetrandrine. These quite easily accessible compounds block TPC2 with an increased potency compared to tetrandrine and at the same time show less toxicity. SG-005 additionally blocked the activation of TRPML1 and TPC1, whereas SG-094 had no considerable inhibitory effect on TRPML1, only on TPC1.
In sum, for none of the currently available TPC antagonists isoform selectivity has been demonstrated and target selectivity needs to be further improved.
In the following, we present a summary of the characteristics of the two TPC isoforms (Tables 4 and 5).
References
Arlt E, Fraticelli M, Tsvilovskyy V, Nadolni W, Breit A, O'Neill TJ, Resenberger S, Wennemuth G, Wahl-Schott C, Biel M, Grimm C, Freichel M, Gudermann T, Klugbauer N, Boekhoff I, Zierler S (2020) TPC1 deficiency or blockade augments systemic anaphylaxis and mast cell activity. Proc Natl Acad Sci U S A 117(30):18068–18078. https://doi.org/10.1073/pnas.1920122117
Bargal R, Avidan N, Ben-Asher E, Olender Z, Zeigler M, Frumkin A, Raas-Rothschild A, Glusman G, Lancet D, Bach G (2000) Identification of the gene causing mucolipidosis type IV. Nat Genet 26(1):118–123. https://doi.org/10.1038/79095
Belvisi MG, Birrell MA (2017) The emerging role of transient receptor potential channels in chronic lung disease. Eur Respir J 50(2). https://doi.org/10.1183/13993003.01357-2016
Billington RA, Genazzani AA (2007) PPADS is a reversible competitive antagonist of the NAADP receptor. Cell Calcium 41(6):505–511. https://doi.org/10.1016/j.ceca.2006.10.002
Birder LA (2007) TRPs in bladder diseases. Biochim Biophys Acta 1772(8):879–884. https://doi.org/10.1016/j.bbadis.2007.04.003
Bissaro M, Moro S (2019) Rethinking to riluzole mechanism of action: the molecular link among protein kinase CK1delta activity, TDP-43 phosphorylation, and amyotrophic lateral sclerosis pharmacological treatment. Neural Regen Res 14(12):2083–2085. https://doi.org/10.4103/1673-5374.262578
Böck J, Krogsaeter E, Passon M, Chao YK, Sharma S, Grallert H, Peters A, Grimm C (2021) Human genome diversity data reveal that L564P is the predominant TPC2 variant and a prerequisite for the blond hair associated M484L gain-of-function effect. PLoS Genet 17(1):e1009236. https://doi.org/10.1371/journal.pgen.1009236
Brailoiu E, Hooper R, Cai X, Brailoiu GC, Keebler MV, Dun NJ, Marchant JS, Patel S (2010) An ancestral deuterostome family of two-pore channels mediates nicotinic acid adenine dinucleotide phosphate-dependent calcium release from acidic organelles. J Biol Chem 285(5):2897–2901. https://doi.org/10.1074/jbc.C109.081943
Calcraft PJ, Ruas M, Pan Z, Cheng X, Arredouani A, Hao X, Tang J, Rietdorf K, Teboul L, Chuang KT, Lin P, Xiao R, Wang C, Zhu Y, Lin Y, Wyatt CN, Parrington J, Ma J, Evans AM, Galione A, Zhu MX (2009) NAADP mobilizes calcium from acidic organelles through two-pore channels. Nature 459(7246):596–600. https://doi.org/10.1038/nature08030
Cang C, Zhou Y, Navarro B, Seo YJ, Aranda K, Shi L, Battaglia-Hsu S, Nissim I, Clapham DE, Ren D (2013) mTOR regulates lysosomal ATP-sensitive two-pore Na(+) channels to adapt to metabolic state. Cell 152(4):778–790. https://doi.org/10.1016/j.cell.2013.01.023
Castonguay J, Orth JHC, Muller T, Sleman F, Grimm C, Wahl-Schott C, Biel M, Mallmann RT, Bildl W, Schulte U, Klugbauer N (2017) The two-pore channel TPC1 is required for efficient protein processing through early and recycling endosomes. Sci Rep 7(1):10038. https://doi.org/10.1038/s41598-017-10607-4
Chae YJ, Kim DH, Lee HJ, Sung KW, Kwon OJ, Hahn SJ (2015) Raloxifene inhibits cloned Kv4.3 channels in an estrogen receptor-independent manner. Pflugers Arch 467(8):1663–1676. https://doi.org/10.1007/s00424-014-1602-3
Chao YK, Schludi V, Chen CC, Butz E, Nguyen ONP, Muller M, Kruger J, Kammerbauer C, Ben-Johny M, Vollmar AM, Berking C, Biel M, Wahl-Schott CA, Grimm C (2017) TPC2 polymorphisms associated with a hair pigmentation phenotype in humans result in gain of channel function by independent mechanisms. Proc Natl Acad Sci U S A 114(41):E8595–E8602. https://doi.org/10.1073/pnas.1705739114
Chen CC, Keller M, Hess M, Schiffmann R, Urban N, Wolfgardt A, Schaefer M, Bracher F, Biel M, Wahl-Schott C, Grimm C (2014) A small molecule restores function to TRPML1 mutant isoforms responsible for mucolipidosis type IV. Nat Commun 5:4681. https://doi.org/10.1038/ncomms5681
Chen CC, Butz ES, Chao YK, Grishchuk Y, Becker L, Heller S, Slaugenhaupt SA, Biel M, Wahl-Schott C, Grimm C (2017) Small molecules for early endosome-specific patch clamping. Cell Chem Biol 24(7):907–916.e904. https://doi.org/10.1016/j.chembiol.2017.05.025
Cheung M, Bao W, Behm DJ, Brooks CA, Bury MJ, Dowdell SE, Eidam HS, Fox RM, Goodman KB, Holt DA, Lee D, Roethke TJ, Willette RN, Xu X, Ye G, Thorneloe KS (2017) Discovery of GSK2193874: an orally active, potent, and selective blocker of transient receptor potential vanilloid 4. ACS Med Chem Lett 8(5):549–554. https://doi.org/10.1021/acsmedchemlett.7b00094
Cuajungco MP, Basilio LC, Silva J, Hart T, Tringali J, Chen CC, Biel M, Grimm C (2014) Cellular zinc levels are modulated by TRPML1-TMEM163 interaction. Traffic 15(11):1247–1265. https://doi.org/10.1111/tra.12205
Dammermann W, Zhang B, Nebel M, Cordiglieri C, Odoardi F, Kirchberger T, Kawakami N, Dowden J, Schmid F, Dornmair K, Hohenegger M, Flugel A, Guse AH, Potter BV (2009) NAADP-mediated Ca2+ signaling via type 1 ryanodine receptor in T cells revealed by a synthetic NAADP antagonist. Proc Natl Acad Sci U S A 106(26):10678–10683. https://doi.org/10.1073/pnas.0809997106
Debono M-W, Le Guern J, Canton T, Doble A, Pradier L (1993) Inhibition by riluzole of electrophysiological responses mediated by rat kainate and NMDA receptors expressed in xenopus oocytes. Eur J Pharmacol 235(2–3):283–289. https://doi.org/10.1016/0014-2999(93)90147-a
Di Palma F, Belyantseva IA, Kim HJ, Vogt TF, Kachar B, Noben-Trauth K (2002) Mutations in Mcoln3 associated with deafness and pigmentation defects in varitint-waddler (Va) mice. Proc Natl Acad Sci U S A 99(23):14994–14999. https://doi.org/10.1073/pnas.222425399
Dietrich A (2019) Transient receptor potential (TRP) channels in health and disease. Cell 8(5):413. https://doi.org/10.3390/cells8050413
Divac N, Prostran M, Jakovcevski I, Cerovac N (2014) Second-generation antipsychotics and extrapyramidal adverse effects. Biomed Res Int 2014:1–6. https://doi.org/10.1155/2014/656370
Dong XP, Cheng X, Mills E, Delling M, Wang F, Kurz T, Xu H (2008) The type IV mucolipidosis-associated protein TRPML1 is an endolysosomal iron release channel. Nature 455(7215):992–996. https://doi.org/10.1038/nature07311
Dong XP, Shen D, Wang X, Dawson T, Li X, Zhang Q, Cheng X, Zhang Y, Weisman LS, Delling M, Xu H (2010) PI(3,5)P(2) controls membrane trafficking by direct activation of mucolipin Ca2+ release channels in the endolysosome. Nat Commun 1:38. https://doi.org/10.1038/ncomms1037
Favia A, Desideri M, Gambara G, D'Alessio A, Ruas M, Esposito B, Del Bufalo D, Parrington J, Ziparo E, Palombi F, Galione A, Filippini A (2014) VEGF-induced neoangiogenesis is mediated by NAADP and two-pore channel-2-dependent Ca2+ signaling. Proc Natl Acad Sci U S A 111(44):E4706–E4715. https://doi.org/10.1073/pnas.1406029111
Fine M, Schmiege P, Li X (2018) Structural basis for PtdInsP2-mediated human TRPML1 regulation. Nat Commun 9(1):4192. https://doi.org/10.1038/s41467-018-06493-7
Galione A, Chuang KT, Funnell TM, Davis LC, Morgan AJ, Ruas M, Parrington J, Churchill GC (2014) Synthesis of NAADP-AM as a membrane-permeant NAADP analog. Cold Spring Harb Protoc 2014(10). https://doi.org/10.1101/pdb.prot076927
Gavva NR, Tamir R, Qu Y, Klionsky L, Zhang TJ, Immke D, Wang J, Zhu D, Vanderah TW, Porreca F, Doherty EM, Norman MH, Wild KD, Bannon AW, Louis JC, Treanor JJ (2005) AMG 9810 [(E)-3-(4-t-butylphenyl)-N-(2,3-dihydrobenzo[b][1,4] dioxin-6-yl)acrylamide], a novel vanilloid receptor 1 (TRPV1) antagonist with antihyperalgesic properties. J Pharmacol Exp Ther 313(1):474–484. https://doi.org/10.1124/jpet.104.079855
Gavva NR, Treanor JJ, Garami A, Fang L, Surapaneni S, Akrami A, Alvarez F, Bak A, Darling M, Gore A, Jang GR, Kesslak JP, Ni L, Norman MH, Palluconi G, Rose MJ, Salfi M, Tan E, Romanovsky AA, Banfield C, Davar G (2008) Pharmacological blockade of the vanilloid receptor TRPV1 elicits marked hyperthermia in humans. Pain 136(1–2):202–210. https://doi.org/10.1016/j.pain.2008.01.024
Gerasimenko JV, Charlesworth RM, Sherwood MW, Ferdek PE, Mikoshiba K, Parrington J, Petersen OH, Gerasimenko OV (2015) Both RyRs and TPCs are required for NAADP-induced intracellular Ca2+ release. Cell Calcium 58(3):237–245. https://doi.org/10.1016/j.ceca.2015.05.005
Gerndt S, Chen CC, Chao YK, Yuan Y, Burgstaller S, Scotto Rosato A, Krogsaeter E, Urban N, Jacob K, Nguyen ONP, Miller MT, Keller M, Vollmar AM, Gudermann T, Zierler S, Schredelseker J, Schaefer M, Biel M, Malli R, Wahl-Schott C, Bracher F, Patel S, Grimm C (2020a) Agonist-mediated switching of ion selectivity in TPC2 differentially promotes lysosomal function. eLife 9:e54712. https://doi.org/10.7554/eLife.54712
Gerndt S, Krogsaeter E, Patel S, Bracher F, Grimm C (2020b) Discovery of lipophilic two-pore channel agonists. FEBS J. https://doi.org/10.1111/febs.15432
Gillman PK (2007) Tricyclic antidepressant pharmacology and therapeutic drug interactions updated. Br J Pharmacol 151(6):737–748. https://doi.org/10.1038/sj.bjp.0707253
Grimm C, Cuajungco MP, van Aken AF, Schnee M, Jors S, Kros CJ, Ricci AJ, Heller S (2007) A helix-breaking mutation in TRPML3 leads to constitutive activity underlying deafness in the varitint-waddler mouse. Proc Natl Acad Sci U S A 104(49):19583–19588. https://doi.org/10.1073/pnas.0709846104
Grimm C, Jors S, Heller S (2009) Life and death of sensory hair cells expressing constitutively active TRPML3. J Biol Chem 284(20):13823–13831. https://doi.org/10.1074/jbc.M809045200
Grimm C, Jors S, Saldanha SA, Obukhov AG, Pan B, Oshima K, Cuajungco MP, Chase P, Hodder P, Heller S (2010) Small molecule activators of TRPML3. Chem Biol 17(2):135–148. https://doi.org/10.1016/j.chembiol.2009.12.016
Grimm C, Jörs S, Guo Z, Obukhov AG, Heller S (2012) Constitutive activity of TRPML2 and TRPML3 channels versus activation by low extracellular sodium and small molecules. J Biol Chem 287(27):22701–22708. https://doi.org/10.1074/jbc.M112.369876
Grimm C, Barthmes M, Wahl-Schott C (2014a) Trpml3. Handb Exp Pharmacol 222:659–674. https://doi.org/10.1007/978-3-642-54215-2_26
Grimm C, Holdt LM, Chen CC, Hassan S, Muller C, Jors S, Cuny H, Kissing S, Schroder B, Butz E, Northoff B, Castonguay J, Luber CA, Moser M, Spahn S, Lullmann-Rauch R, Fendel C, Klugbauer N, Griesbeck O, Haas A, Mann M, Bracher F, Teupser D, Saftig P, Biel M, Wahl-Schott C (2014b) High susceptibility to fatty liver disease in two-pore channel 2-deficient mice. Nat Commun 5:4699. https://doi.org/10.1038/ncomms5699
Grimm C, Chen CC, Wahl-Schott C, Biel M (2017) Two-pore channels: catalyzers of endolysosomal transport and function. Front Pharmacol 8:45. https://doi.org/10.3389/fphar.2017.00045
Grimm C, Bartel K, Vollmar AM, Biel M (2018) Endolysosomal cation channels and cancer-a link with great potential. Pharmaceuticals (Basel) 11(1). https://doi.org/10.3390/ph11010004
Grishchuk Y, Sri S, Rudinskiy N, Ma W, Stember KG, Cottle MW, Sapp E, Difiglia M, Muzikansky A, Betensky RA, Wong AM, Bacskai BJ, Hyman BT, Kelleher RJ 3rd, Cooper JD, Slaugenhaupt SA (2014) Behavioral deficits, early gliosis, dysmyelination and synaptic dysfunction in a mouse model of mucolipidosis IV. Acta Neuropathol Commun 2:133. https://doi.org/10.1186/s40478-014-0133-7
Grishchuk Y, Pena KA, Coblentz J, King VE, Humphrey DM, Wang SL, Kiselyov KI, Slaugenhaupt SA (2015) Impaired myelination and reduced brain ferric iron in the mouse model of mucolipidosis IV. Dis Model Mech 8(12):1591–1601. https://doi.org/10.1242/dmm.021154
Grishchuk Y, Stember KG, Matsunaga A, Olivares AM, Cruz NM, King VE, Humphrey DM, Wang SL, Muzikansky A, Betensky RA, Thoreson WB, Haider N, Slaugenhaupt SA (2016) Retinal dystrophy and optic nerve pathology in the mouse model of mucolipidosis IV. Am J Pathol 186(1):199–209. https://doi.org/10.1016/j.ajpath.2015.09.017
Gumushan Aktas H, Akgun T (2018) Naringenin inhibits prostate cancer metastasis by blocking voltage-gated sodium channels. Biomed Pharmacother 106:770–775. https://doi.org/10.1016/j.biopha.2018.07.008
Gunaratne GS, Brailoiu E, He S, Unterwald EM, Patel S, Slama JT, Walseth TF, Marchant JS (2021) Essential requirement for JPT2 in NAADP-evoked Ca(2+) signaling. Sci Signal 14(675). https://doi.org/10.1126/scisignal.abd5605
Hsu HT, Tseng YT, Lo YC, Wu SN (2014) Ability of naringenin, a bioflavonoid, to activate M-type potassium current in motor neuron-like cells and to increase BKCa-channel activity in HEK293T cells transfected with alpha-hSlo subunit. BMC Neurosci 15:135. https://doi.org/10.1186/s12868-014-0135-1
Huang S, Szallasi A (2017) Transient receptor potential (TRP) channels in drug discovery: old concepts & new thoughts. Pharmaceuticals (Basel) 10(3). https://doi.org/10.3390/ph10030064
Hubert JP, Delumeau JC, Glowinski J, Premont J, Doble A (1994) Antagonism by riluzole of entry of calcium evoked by NMDA and veratridine in rat cultured granule cells: evidence for a dual mechanism of action. Br J Pharmacol 113(1):261–267. https://doi.org/10.1111/j.1476-5381.1994.tb16203.x
Imura K, Yoshioka T, Hirasawa T, Sakata T (2009) Role of TRPV3 in immune response to development of dermatitis. J Inflamm (Lond) 6:17. https://doi.org/10.1186/1476-9255-6-17
Jha A, Brailoiu E, Muallem S (2014) How does NAADP release lysosomal Ca2+? Channels (Austin) 8(3):174–175. https://doi.org/10.4161/chan.28995
Jiang LH, Li X, Syed Mortadza SA, Lovatt M, Yang W (2018a) The TRPM2 channel nexus from oxidative damage to Alzheimer's pathologies: an emerging novel intervention target for age-related dementia. Ageing Res Rev 47:67–79. https://doi.org/10.1016/j.arr.2018.07.002
Jiang Y, Zhou Y, Peng G, Tian H, Pan D, Liu L, Yang X, Li C, Li W, Chen L, Ran P, Dai A (2018b) Two-pore channels mediated receptor-operated Ca2+ entry in pulmonary artery smooth muscle cells in response to hypoxia. Int J Biochem Cell Biol 97:28–35. https://doi.org/10.1016/j.biocel.2018.01.012
Just S, Chenard BL, Ceci A, Strassmaier T, Chong JA, Blair NT, Gallaschun RJ, Del Camino D, Cantin S, D'Amours M, Eickmeier C, Fanger CM, Hecker C, Hessler DP, Hengerer B, Kroker KS, Malekiani S, Mihalek R, McLaughlin J, Rast G, Witek J, Sauer A, Pryce CR, Moran MM (2018) Treatment with HC-070, a potent inhibitor of TRPC4 and TRPC5, leads to anxiolytic and antidepressant effects in mice. PLoS One 13(1):e0191225. https://doi.org/10.1371/journal.pone.0191225
Kelu JJ, Chan HL, Webb SE, Cheng AH, Ruas M, Parrington J, Galione A, Miller AL (2015) Two-Pore Channel 2 activity is required for slow muscle cell-generated Ca2+ signaling during myogenesis in intact zebrafish. Int J Dev Biol 59(7–9):313–325. https://doi.org/10.1387/ijdb.150206am
Kilpatrick BS, Yates E, Grimm C, Schapira AH, Patel S (2016) Endo-lysosomal TRP mucolipin-1 channels trigger global ER Ca2+ release and Ca2+ influx. J Cell Sci 129(20):3859–3867. https://doi.org/10.1242/jcs.190322
Kim HJ, Li Q, Tjon-Kon-Sang S, So I, Kiselyov K, Muallem S (2007) Gain-of-function mutation in TRPML3 causes the mouse Varitint-Waddler phenotype. J Biol Chem 282(50):36138–36142. https://doi.org/10.1074/jbc.C700190200
Kim HJ, Li Q, Tjon-Kon-Sang S, So I, Kiselyov K, Soyombo AA, Muallem S (2008) A novel mode of TRPML3 regulation by extracytosolic pH absent in the varitint-waddler phenotype. EMBO J 27(8):1197–1205. https://doi.org/10.1038/emboj.2008.56
Kintzer AF, Stroud RM (2016) Structure, inhibition and regulation of two-pore channel TPC1 from Arabidopsis thaliana. Nature 531(7593):258–262. https://doi.org/10.1038/nature17194
Kriegler K, Leser C, Mayer P, Franz Bracher F (2022) Effective chiral pool synthesis of both enantiomers of the TRPML inhibitor trans-ML-SI3. Arch Pharm 355:e2100362. https://doi.org/10.1002/ardp.202100362
Lear PV, Gonzalez-Touceda D, Porteiro Couto B, Viano P, Guymer V, Remzova E, Tunn R, Chalasani A, Garcia-Caballero T, Hargreaves IP, Tynan PW, Christian HC, Nogueiras R, Parrington J, Dieguez C (2015) Absence of intracellular ion channels TPC1 and TPC2 leads to mature-onset obesity in male mice, due to impaired lipid availability for thermogenesis in brown adipose tissue. Endocrinology 156(3):975–986. https://doi.org/10.1210/en.2014-1766
Lee SH, Park YB, Bae KH, Bok SH, Kwon YK, Lee ES, Choi MS (1999) Cholesterol-lowering activity of naringenin via inhibition of 3-hydroxy-3-methylglutaryl coenzyme A reductase and acyl coenzyme A:cholesterol acyltransferase in rats. Ann Nutr Metab 43(3):173–180. https://doi.org/10.1159/000012783
Leser C, Keller M, Gerndt S, Urban N, Chen CC, Schaefer M, Grimm C, Bracher F (2021) Chemical and pharmacological characterization of the TRPML calcium channel blockers ML-SI1 and ML-SI3. Eur J Med Chem 210:112966. https://doi.org/10.1016/j.ejmech.2020.112966
Lev S, Zeevi DA, Frumkin A, Offen-Glasner V, Bach G, Minke B (2010) Constitutive activity of the human TRPML2 channel induces cell degeneration. J Biol Chem 285(4):2771–2782. https://doi.org/10.1074/jbc.M109.046508
Lin Z, Chen Q, Lee M, Cao X, Zhang J, Ma D, Chen L, Hu X, Wang H, Wang X, Zhang P, Liu X, Guan L, Tang Y, Yang H, Tu P, Bu D, Zhu X, Wang K, Li R, Yang Y (2012) Exome sequencing reveals mutations in TRPV3 as a cause of Olmsted syndrome. Am J Hum Genet 90(3):558–564. https://doi.org/10.1016/j.ajhg.2012.02.006
Lin-Moshier Y, Walseth TF, Churamani D, Davidson SM, Slama JT, Hooper R, Brailoiu E, Patel S, Marchant JS (2012) Photoaffinity labeling of nicotinic acid adenine dinucleotide phosphate (NAADP) targets in mammalian cells. J Biol Chem 287(4):2296–2307. https://doi.org/10.1074/jbc.M111.305813
Liu J, Wang LN (2018) The efficacy and safety of riluzole for neurodegenerative movement disorders: a systematic review with meta-analysis. Drug Deliv 25(1):43–48. https://doi.org/10.1080/10717544.2017.1413446
Ma J, Yang L, Ma Y, Wang X, Ren J, Yang J (2017) Targeting transient receptor potential channels in cardiometabolic diseases and myocardial ischemia reperfusion injury. Curr Drug Targets 18(15):1733–1745. https://doi.org/10.2174/1389450116666151019102052
Malgouris C, Daniel M, Doble A (1994) Neuroprotective effects of riluzole on or veratridine-induced neurotoxicity in rat hippocampal slices. Neurosci Lett 177(1–2):95–99. https://doi.org/10.1016/0304-3940(94)90053-1
Miao Y, Li G, Zhang X, Xu H, Abraham SN (2015) A TRP channel senses lysosome neutralization by pathogens to trigger their expulsion. Cell 161(6):1306–1319. https://doi.org/10.1016/j.cell.2015.05.009
Micsenyi MC, Dobrenis K, Stephney G, Pickel J, Vanier MT, Slaugenhaupt SA, Walkley SU (2009) Neuropathology of the Mcoln1(−/−) knockout mouse model of mucolipidosis type IV. J Neuropathol Exp Neurol 68(2):125–135. https://doi.org/10.1097/NEN.0b013e3181942cf0
Miller M, Shi J, Zhu Y, Kustov M, Tian JB, Stevens A, Wu M, Xu J, Long S, Yang P, Zholos AV, Salovich JM, Weaver CD, Hopkins CR, Lindsley CW, McManus O, Li M, Zhu MX (2011) Identification of ML204, a novel potent antagonist that selectively modulates native TRPC4/C5 ion channels. J Biol Chem 286(38):33436–33446. https://doi.org/10.1074/jbc.M111.274167
Morgan AJ, Galione A (2014) Two-pore channels (TPCs): current controversies. Bioessays 36(2):173–183. https://doi.org/10.1002/bies.201300118
Morgan AJ, Davis LC, Ruas M, Galione A (2015) TPC: the NAADP discovery channel? Biochem Soc Trans 43(3):384–389. https://doi.org/10.1042/BST20140300
Müller M, De Weille JR, Lazdunski M (1991) Chlorpromazine and related phenothiazines inhibit the ATP-sensitive K+ channel. Eur J Pharmacol 198(1):101–104. https://doi.org/10.1016/0014-2999(91)90569-c
Müller M, Gerndt S, Chao YK, Zisis T, Nguyen ONP, Gerwien A, Urban N, Muller C, Gegenfurtner FA, Geisslinger F, Ortler C, Chen CC, Zahler S, Biel M, Schaefer M, Grimm C, Bracher F, Vollmar AM, Bartel K (2021) Gene editing and synthetically accessible inhibitors reveal role for TPC2 in HCC cell proliferation and tumor growth. Cell Chem Biol. https://doi.org/10.1016/j.chembiol.2021.01.023
Nagata K, Zheng L, Madathany T, Castiglioni AJ, Bartles JR, Garcia-Anoveros J (2008) The varitint-waddler (Va) deafness mutation in TRPML3 generates constitutive, inward rectifying currents and causes cell degeneration. Proc Natl Acad Sci U S A 105(1):353–358. https://doi.org/10.1073/pnas.0707963105
Naylor E, Arredouani A, Vasudevan SR, Lewis AM, Parkesh R, Mizote A, Rosen D, Thomas JM, Izumi M, Ganesan A, Galione A, Churchill GC (2009) Identification of a chemical probe for NAADP by virtual screening. Nat Chem Biol 5(4):220–226. https://doi.org/10.1038/nchembio.150
Nguyen ON, Grimm C, Schneider LS, Chao YK, Atzberger C, Bartel K, Watermann A, Ulrich M, Mayr D, Wahl-Schott C, Biel M, Vollmar AM (2017) Two-pore channel function is crucial for the migration of invasive cancer cells. Cancer Res 77(6):1427–1438. https://doi.org/10.1158/0008-5472.CAN-16-0852
Ogunbayo OA, Zhu Y, Rossi D, Sorrentino V, Ma J, Zhu MX, Evans AM (2011) Cyclic adenosine diphosphate ribose activates ryanodine receptors, whereas NAADP activates two-pore domain channels. J Biol Chem 286(11):9136–9140. https://doi.org/10.1074/jbc.M110.202002
Onyenwoke RU, Sexton JZ, Yan F, Diaz MC, Forsberg LJ, Major MB, Brenman JE (2015) The mucolipidosis IV Ca2+ channel TRPML1 (MCOLN1) is regulated by the TOR kinase. Biochem J 470(3):331–342. https://doi.org/10.1042/BJ20150219
Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, Guo L, Guo R, Chen T, Hu J, Xiang Z, Mu Z, Chen X, Chen J, Hu K, Jin Q, Wang J, Qian Z (2020) Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nat Commun 11(1):1620. https://doi.org/10.1038/s41467-020-15562-9
Pafumi I, Festa M, Papacci F, Lagostena L, Giunta C, Gutla V, Cornara L, Favia A, Palombi F, Gambale F, Filippini A, Carpaneto A (2017) Naringenin impairs two-pore channel 2 activity and inhibits VEGF-induced angiogenesis. Sci Rep 7(1):5121. https://doi.org/10.1038/s41598-017-04974-1
Parenti A, De Logu F, Geppetti P, Benemei S (2016) What is the evidence for the role of TRP channels in inflammatory and immune cells? Br J Pharmacol 173(6):953–969. https://doi.org/10.1111/bph.13392
Parkesh R, Lewis AM, Aley PK, Arredouani A, Rossi S, Tavares R, Vasudevan SR, Rosen D, Galione A, Dowden J, Churchill GC (2008) Cell-permeant NAADP: a novel chemical tool enabling the study of Ca2+ signalling in intact cells. Cell Calcium 43(6):531–538. https://doi.org/10.1016/j.ceca.2007.08.006
Penny CJ, Vassileva K, Jha A, Yuan Y, Chee X, Yates E, Mazzon M, Kilpatrick BS, Muallem S, Marsh M, Rahman T, Patel S (2019) Mining of Ebola virus entry inhibitors identifies approved drugs as two-pore channel pore blockers. Biochim Biophys Acta Mol Cell Res 1866(7):1151–1161. https://doi.org/10.1016/j.bbamcr.2018.10.022
Pitt SJ, Lam AK, Rietdorf K, Galione A, Sitsapesan R (2014) Reconstituted human TPC1 is a proton-permeable ion channel and is activated by NAADP or Ca2+. Sci Signal 7(326):ra46. https://doi.org/10.1126/scisignal.2004854
Pitt SJ, Reilly-O'Donnell B, Sitsapesan R (2016) Exploring the biophysical evidence that mammalian two-pore channels are NAADP-activated calcium-permeable channels. J Physiol 594(15):4171–4179. https://doi.org/10.1113/JP270936
Plesch E, Chen CC, Butz E, Scotto Rosato A, Krogsaeter EK, Yinan H, Bartel K, Keller M, Robaa D, Teupser D, Holdt LM, Vollmar AM, Sippl W, Puertollano R, Medina D, Biel M, Wahl-Schott C, Bracher F, Grimm C (2018) Selective agonist of TRPML2 reveals direct role in chemokine release from innate immune cells. eLife 7:e39720. https://doi.org/10.7554/eLife.39720
Rinkenberger N, Schoggins JW (2018) Mucolipin-2 cation channel increases trafficking efficiency of endocytosed viruses. MBio 9(1):e02314–e02317. https://doi.org/10.1128/mBio.02314-17
Roggenkamp HG, Khansahib I, Hernandez CL, Zhang Y, Lodygin D, Kruger A, Gu F, Mockl F, Lohndorf A, Wolters V, Woike D, Rosche A, Bauche A, Schetelig D, Werner R, Schluter H, Failla AV, Meier C, Fliegert R, Walseth TF, Flugel A, Diercks BP, Guse AH (2021) HN1L/JPT2: a signaling protein that connects NAADP generation to Ca(2+) microdomain formation. Sci Signal 14(675). https://doi.org/10.1126/scisignal.abd5647
Ruas M, Chuang KT, Davis LC, Al-Douri A, Tynan PW, Tunn R, Teboul L, Galione A, Parrington J (2014) TPC1 has two variant isoforms, and their removal has different effects on endo-lysosomal functions compared to loss of TPC2. Mol Cell Biol 34(21):3981–3992. https://doi.org/10.1128/MCB.00113-14
Ruas M, Davis LC, Chen CC, Morgan AJ, Chuang KT, Walseth TF, Grimm C, Garnham C, Powell T, Platt N, Platt FM, Biel M, Wahl-Schott C, Parrington J, Galione A (2015a) Expression of Ca2+-permeable two-pore channels rescues NAADP signalling in TPC-deficient cells. EMBO J 34(13):1743–1758. https://doi.org/10.15252/embj.201490009
Ruas M, Galione A, Parrington J (2015b) Two-pore channels: lessons from mutant mouse models. Messenger (Los Angel) 4(1):4–22. https://doi.org/10.1166/msr.2015.1041
Rühl P, Scotto Rosato A, Urban N, Gerndt S, Tang R, Abrahamian C, Leser C, Sheng J, Jha A, Vollmer G, Schaefer M, Bracher F, Grimm C (2021) Estradiol analogs attenuate autophagy, cell migration and invasion by direct and selective inhibition of TRPML1, independent of estrogen receptors. Sci Rep 11(1):8313
Ryckmans T, Aubdool AA, Bodkin JV, Cox P, Brain SD, Dupont T, Fairman E, Hashizume Y, Ishii N, Kato T, Kitching L, Newman J, Omoto K, Rawson D, Strover J (2011) Design and pharmacological evaluation of PF-4840154, a non-electrophilic reference agonist of the TrpA1 channel. Bioorg Med Chem Lett 21(16):4857–4859. https://doi.org/10.1016/j.bmcl.2011.06.035
Sakurai Y, Kolokoltsov AA, Chen CC, Tidwell MW, Bauta WE, Klugbauer N, Grimm C, Wahl-Schott C, Biel M, Davey RA (2015) Ebola virus. Two-pore channels control Ebola virus host cell entry and are drug targets for disease treatment. Science 347(6225):995–998. https://doi.org/10.1126/science.1258758
Saldanha S, Grimm C, Mercer BA, Choi JY, Allais C, Roush WR, Heller S, Hodder P (2011) Campaign to identify agonists of transient receptor potential channels 3 and 2 (TRPML3 & TRPML2). Probe Rep
Saldanha PA, Cairrao E, Maia CJ, Verde I (2013) Long- and short-term effects of androgens in human umbilical artery smooth muscle. Clin Exp Pharmacol Physiol 40(3):181–189. https://doi.org/10.1111/1440-1681.12047
Samie M, Wang X, Zhang X, Goschka A, Li X, Cheng X, Gregg E, Azar M, Zhuo Y, Garrity AG, Gao Q, Slaugenhaupt S, Pickel J, Zolov SN, Weisman LS, Lenk GM, Titus S, Bryant-Genevier M, Southall N, Juan M, Ferrer M, Xu H (2013) A TRP channel in the lysosome regulates large particle phagocytosis via focal exocytosis. Dev Cell 26(5):511–524. https://doi.org/10.1016/j.devcel.2013.08.003
Scholz EP, Zitron E, Kiesecker C, Luck S, Thomas D, Kathofer S, Kreye VA, Katus HA, Kiehn J, Schoels W, Karle CA (2005) Inhibition of cardiac HERG channels by grapefruit flavonoid naringenin: implications for the influence of dietary compounds on cardiac repolarisation. Naunyn Schmiedebergs Arch Pharmacol 371(6):516–525. https://doi.org/10.1007/s00210-005-1069-z
She J, Guo J, Chen Q, Zeng W, Jiang Y, Bai XC (2018) Structural insights into the voltage and phospholipid activation of the mammalian TPC1 channel. Nature 556(7699):130–134. https://doi.org/10.1038/nature26139
Shelton RC (2019) Serotonin and norepinephrine reuptake inhibitors. Handb Exp Pharmacol 250:145–180. https://doi.org/10.1007/164_2018_164
Shen D, Wang X, Li X, Zhang X, Yao Z, Dibble S, Dong XP, Yu T, Lieberman AP, Showalter HD, Xu H (2012) Lipid storage disorders block lysosomal trafficking by inhibiting a TRP channel and lysosomal calcium release. Nat Commun 3:731. https://doi.org/10.1038/ncomms1735
Sherkheli M, Gisselmann G, Vogt-Eisele AK, Doerner JF, Hatt H (2008) Menthol derivative WS-12 selectively activates transient receptor potential melastatin-8 (TPPM8) ion channels. Pak J Pharm Sci 21:370–378
Singaravelu K, Deitmer JW (2006) Calcium mobilization by nicotinic acid adenine dinucleotide phosphate (NAADP) in rat astrocytes. Cell Calcium 39(2):143–153. https://doi.org/10.1016/j.ceca.2005.10.001
Sjogren EB, Rider MA, Nelson PH, Bingham S Jr, Poulton AL, Emanuel MA, Komuniecki R (1991) Synthesis and biological activity of a series of diaryl-substituted alpha-cyano-beta-hydroxypropenamides, a new class of anthelmintic agents. J Med Chem 34(11):3295–3301. https://doi.org/10.1021/jm00115a020
Song JH, Huang CS, Nagata K, Yeh JU, Narahashi T (1997) Differential action of riluzole on tetrodotoxin-sensitive and tetrodotoxin-resistant sodium channels. J Pharmacol Exp Ther 282:707–714
Spix B, Butz ES, Chen C-C, Scotto Rosato A, Tang R, Jeridi A, Kudrina V, Plesch E, Wartenberg P, Arlt E, Briukhovetska D, Ansari M, Günes Günsel G, Conlon TM, Wyatt A, Wetzel S, Teupser D, Holdt LM, Ectors F, Boekhoff I, Boehm U, García Añoveros J, Saftig P, Giera M, Kobold S, Schiller HB, Zierler S, Gudermann T, Wahl-Schott C, Bracher F, Yildirim AÖ, Biel M, Grimm C (2022) Lung emphysema and impaired macrophage elastase clearance in mucolipin 3 deficient mice. Nat Commun 13(1):318
Straub I, Krugel U, Mohr F, Teichert J, Rizun O, Konrad M, Oberwinkler J, Schaefer M (2013) Flavanones that selectively inhibit TRPM3 attenuate thermal nociception in vivo. Mol Pharmacol 84(5):736–750. https://doi.org/10.1124/mol.113.086843
Sulem P, Gudbjartsson DF, Stacey SN, Helgason A, Rafnar T, Jakobsdottir M, Steinberg S, Gudjonsson SA, Palsson A, Thorleifsson G, Palsson S, Sigurgeirsson B, Thorisdottir K, Ragnarsson R, Benediktsdottir KR, Aben KK, Vermeulen SH, Goldstein AM, Tucker MA, Kiemeney LA, Olafsson JH, Gulcher J, Kong A, Thorsteinsdottir U, Stefansson K (2008) Two newly identified genetic determinants of pigmentation in Europeans. Nat Genet 40(7):835–837. https://doi.org/10.1038/ng.160
Takatori S, Tatematsu T, Cheng J, Matsumoto J, Akano T, Fujimoto T (2016) Phosphatidylinositol 3,5-bisphosphate-rich membrane domains in endosomes and lysosomes. Traffic 17(2):154–167. https://doi.org/10.1111/tra.12346
Thorneloe KS, Sulpizio AC, Lin Z, Figueroa DJ, Clouse AK, McCafferty GP, Chendrimada TP, Lashinger ES, Gordon E, Evans L, Misajet BA, Demarini DJ, Nation JH, Casillas LN, Marquis RW, Votta BJ, Sheardown SA, Xu X, Brooks DP, Laping NJ, Westfall TD (2008) N-((1S)-1-{[4-((2S)-2-{[(2,4-dichlorophenyl)sulfonyl]amino}-3-hydroxypropanoyl)-1 -piperazinyl]carbonyl}-3-methylbutyl)-1-benzothiophene-2-carboxamide (GSK1016790A), a novel and potent transient receptor potential vanilloid 4 channel agonist induces urinary bladder contraction and hyperactivity: part I. J Pharmacol Exp Ther 326(2):432–442. https://doi.org/10.1124/jpet.108.139295
Thorneloe KS, Cheung M, Bao W, Alsaid H, Lenhard S, Jian MY, Costell M, Maniscalco-Hauk K, Krawiec JA, Olzinski A, Gordon E, Lozinskaya I, Elefante L, Qin P, Matasic DS, James C, Tunstead J, Donovan B, Kallal L, Waszkiewicz A, Vaidya K, Davenport EA, Larkin J, Burgert M, Casillas LN, Marquis RW, Ye G, Eidam HS, Goodman KB, Toomey JR, Roethke TJ, Jucker BM, Schnackenberg CG, Townsley MI, Lepore JJ, Willette RN (2012) An orally active TRPV4 channel blocker prevents and resolves pulmonary edema induced by heart failure. Sci Transl Med 4(159):159ra148. https://doi.org/10.1126/scitranslmed.3004276
Trindade E, Menon D, Tropfer LA, Coloma C (1998) Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. CMAJ 159:1245–1252
Tsang SY, Yao X, Essin K, Wong CM, Chan FL, Gollasch M, Huang Y (2004) Raloxifene relaxes rat cerebral arteries in vitro and inhibits L-type voltage-sensitive Ca2+ channels. Stroke 35(7):1709–1714. https://doi.org/10.1161/01.STR.0000131479.08005.ca
Walseth TF, Lin-Moshier Y, Jain P, Ruas M, Parrington J, Galione A, Marchant JS, Slama JT (2012) NAADP does not directly bind to two-pore channels to release calcium. J Biol Chem 287(4):2316–2316. https://doi.org/10.1074/jbc.P111.305813
Wang G, Lemos JR, Iadecola C (2004) Herbal alkaloid tetrandrine: from an ion channel blocker to inhibitor of tumor proliferation. Trends Pharmacol Sci 25(3):120–123. https://doi.org/10.1016/j.tips.2004.01.009
Wang Q, Lu L, Gao X, Wang C, Wang J, Cheng J, Gao R, Xiao H (2011) Effects of raloxifene on voltage-dependent T-type Ca2+ channels in mouse spermatogenic cells. Pharmacology 87(1–2):70–80. https://doi.org/10.1159/000321726
Wang W, Gao Q, Yang M, Zhang X, Yu L, Lawas M, Li X, Bryant-Genevier M, Southall NT, Marugan J, Ferrer M, Xu H (2015) Up-regulation of lysosomal TRPML1 channels is essential for lysosomal adaptation to nutrient starvation. Proc Natl Acad Sci U S A 112(11):E1373–E1381. https://doi.org/10.1073/pnas.1419669112
Weyer-Menkhoff I, Lotsch J (2018) Human pharmacological approaches to TRP-ion-channel-based analgesic drug development. Drug Discov Today 23(12):2003–2012. https://doi.org/10.1016/j.drudis.2018.06.020
Xu H, Delling M, Li L, Dong X, Clapham DE (2007) Activating mutation in a mucolipin transient receptor potential channel leads to melanocyte loss in varitint-waddler mice. Proc Natl Acad Sci U S A 104(46):18321–18326. https://doi.org/10.1073/pnas.0709096104
Yamaguchi S, Muallem S (2010) Opening the TRPML gates. Chem Biol 17(3):209–210. https://doi.org/10.1016/j.chembiol.2010.02.009
Yoshioka T, Imura K, Asakawa M, Suzuki M, Oshima I, Hirasawa T, Sakata T, Horikawa T, Arimura A (2009) Impact of the Gly573Ser substitution in TRPV3 on the development of allergic and pruritic dermatitis in mice. J Invest Dermatol 129(3):714–722. https://doi.org/10.1038/jid.2008.245
Yu L, Zhang X, Yang Y, Li D, Tang K, Zhao Z, He W, Wang C, Sahoo N, Converso-Baran K, Davis CS, Brooks SV, Bigot A, Calvo R, Martinez NJ, Southall N, Hu X, Marugan J, Ferrer M, Xu H (2020) Small-molecule activation of lysosomal TRP channels ameliorates Duchenne muscular dystrophy in mouse models. Sci Adv 6(6):eaaz2736. https://doi.org/10.1126/sciadv.aaz2736
Zhang L, Barritt GJ (2006) TRPM8 in prostate cancer cells: a potential diagnostic and prognostic marker with a secretory function? Endocr Relat Cancer 13(1):27–38. https://doi.org/10.1677/erc.1.01093
Zhang YZ, Li YY (2014) Inflammatory bowel disease: pathogenesis. World J Gastroenterol 20(1):91–99. https://doi.org/10.3748/wjg.v20.i1.91
Zhang X, Li X, Xu H (2012) Phosphoinositide isoforms determine compartment-specific ion channel activity. Proc Natl Acad Sci U S A 109(28):11384–11389. https://doi.org/10.1073/pnas.1202194109
Zhang X, Cheng X, Yu L, Yang J, Calvo R, Patnaik S, Hu X, Gao Q, Yang M, Lawas M, Delling M, Marugan J, Ferrer M, Xu H (2016) MCOLN1 is a ROS sensor in lysosomes that regulates autophagy. Nat Commun 7:12109. https://doi.org/10.1038/ncomms12109
Zhang X, Chen W, Li P, Calvo R, Southall N, Hu X, Bryant-Genevier M, Feng X, Geng Q, Gao C, Yang M, Tang K, Ferrer M, Marugan JJ, Xu H (2019) Agonist-specific voltage-dependent gating of lysosomal two-pore Na(+) channels. eLife 8:e51423. https://doi.org/10.7554/eLife.51423
Zhong XZ, Zou Y, Sun X, Dong G, Cao Q, Pandey A, Rainey JK, Zhu X, Dong XP (2017) Inhibition of transient receptor potential channel mucolipin-1 (TRPML1) by lysosomal adenosine involved in severe combined immunodeficiency diseases. J Biol Chem 292(8):3445–3455. https://doi.org/10.1074/jbc.M116.743963
Zhou X, Dong XW, Priestley T (2006) The neuroleptic drug, fluphenazine, blocks neuronal voltage-gated sodium channels. Brain Res 1106(1):72–81. https://doi.org/10.1016/j.brainres.2006.05.076
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rautenberg, S., Keller, M., Leser, C., Chen, CC., Bracher, F., Grimm, C. (2022). Expanding the Toolbox: Novel Modulators of Endolysosomal Cation Channels. In: Wahl-Schott, C., Biel, M. (eds) Endolysosomal Voltage-Dependent Cation Channels. Handbook of Experimental Pharmacology, vol 278. Springer, Cham. https://doi.org/10.1007/164_2022_605
Download citation
DOI: https://doi.org/10.1007/164_2022_605
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-31522-0
Online ISBN: 978-3-031-31523-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)