Abstract
For more than 25 years, researchers have made advances in developing medications to treat alcohol use disorder (AUD), highlighted by the US Food and Drug Administration’s (FDA’s) approval of disulfiram, naltrexone (oral and long-acting), and acamprosate. These medications are also approved in Europe, where the European Medicines Agency (EMA) recently added a fourth medication, nalmefene, for AUD. Despite these advances, today’s medications have a small effect size, showing efficacy for only a limited number of individuals with AUD. However, a host of new medications, which act on variety of pharmacologic targets, are in the pipeline and have been evaluated in numerous human studies. This article reviews the efficacy and safety of medications currently being tested in human trials and looks at ongoing efforts to identify candidate compounds in human studies. As mentioned in the National Institute on Alcohol Abuse and Alcoholism’s Strategic Plan 2017–2021 (https://www.niaaa.nih.gov/sites/default/files/StrategicPlan_NIAAA_optimized_2017-2020.pdf), medications development remains a high priority. By developing more effective and safe medications, and identifying those patients who will benefit the most from these treatments, we can provide clinicians with the tools they need to treat this devastating disorder, providing relief for patients and their families and markedly improving public health and safety.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
In the United States, three medications have been approved by the US Food and Drug Administration (FDA) for the treatment of alcohol use disorder (AUD): disulfiram, naltrexone (oral and extended-release injectable), and acamprosate. Yet most people, less than 20%, seek treatment for AUD during their lifetime, and of these less than 4% receive FDA-approved medications (Grant et al. 2015; Litten 2016). Medications for AUD have been available to clinicians for decades but remain underutilized. In an effort to better inform clinicians about the benefits of medications for treating AUD, the Substance Abuse and Mental Health Services Administration (SAMHSA) and National Institute on Alcohol Abuse and Alcoholism (NIAAA) recently published practical guidelines for prescribing these FDA-approved medications in clinical practice (http://store.samhsa.gov/shin/content//SMA15-4907/SMA15-4907.pdf).
Raising awareness about the medications available and offering guidelines for prescribing them may help. Still, clinicians’ reluctance to make full use of pharmacotherapies may be, in part, because the existing medications have such small effect sizes, on average, and show a wide range of efficacy across patients. Some of this variability is due to the significant heterogeneity of AUD itself. We simply do not know which type of patient is most likely to respond to each of these medications. Severity, duration, and family history of the disorder, co-occurring disorders, demographic characteristics, and genetic markers, among other factors, all can impact how a patient responds to medication. In other words, there is no silver bullet for the treatment of this complex disorder.
Because of this, in recent years, the search for medications to treat AUD has undergone a paradigm shift toward precision medicine. Medications development is now actively seeking to identify subgroups of patients who will benefit the most from specific compounds and have the fewest side effects. The goal is to provide clinicians with a full menu of medication options from which to choose. This is not an entirely new concept. Over two decades ago, NIAAA first explored the idea of “matching” specific treatments to specific types of patients with AUD in a series of groundbreaking studies conducted through the Project Match initiative (Project MATCH Research Group 1997). Since then, with advances in neuroscience and the underlying etiology of AUD, clinical trials have focused not only on whether a medication works “on average” across a patient population but also if it works better in certain patient subgroups based on a purported mechanism of action.
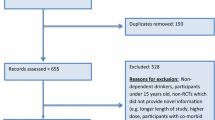
Most encouraging is the diversity and number of targets being studied today, as well as the number of potential compounds currently in development. Preclinical work is summarized in another chapter of this book (see Egli, M). Here we detail the latest research on these medications, including their mechanism of action, efficacy, and safety in treating AUD in humans. We include medications that have exhibited efficacy in alcohol treatment clinical trials, medications that initially showed promise but failed in subsequent multisite clinical trials, as well as medications which are still in the early stages of evaluation in human studies (Table 1).
1.1 Medications Exhibiting Efficacy in Alcohol Treatment Clinical Trials
1.1.1 Nalmefene
1.1.1.1 Molecular and Functional Mechanisms of Action
Nalmefene is an opioid antagonist approved by the FDA to treat opioid overdose. Although structurally similar to naltrexone, nalmefene has several differences that may have advantages over naltrexone. It has a higher affinity for mu and kappa opioid receptors, a lower likelihood to induce liver toxicity, and higher bioavailability than naltrexone (Mann et al. 2016; Mason et al. 1999). In a three-group (nalmefene, naltrexone, and placebo) human laboratory study, nalmefene reduced alcohol-induced craving and stimulation compared with placebo. Similar results also were found for naltrexone (Drobes et al. 2004).
1.1.1.2 Results of Clinical Trials
In a single-site 12-week randomized clinical trial (RCT), Mason et al. (1999) first showed that alcohol-dependent patients who received either 20 mg or 80 mg of nalmefene per day were less likely to relapse to drinking or to drink heavily, compared with patients who were treated with placebo. Results were not significantly different between the 20- and 80-mg doses, with both nalmefene groups showing similar efficacy. In another 12-week multisite RCT in 270 alcohol-dependent patients, nalmefene, evaluated at three different doses (5, 20, and 40 mg per day), failed to show a difference in the number of heavy-drinking days (defined as five or more drinks per day for men and four or more drinks per day for women), alcohol craving, gamma-glutamyl transpeptidase (GGT), and carbohydrate-deficient transferrin (CDT) levels (GGT and CDT are biomarkers of alcohol consumption) (Anton et al. 2004). In contrast to the Anton et al. (2004) study, three recent large RCTs of nalmefene showed a positive effect on drinking outcome, which, subsequently, led to approval of this medication for treatment of AUD in Europe. The first 24-week RCT was conducted in 604 alcohol-dependent patients across 39 sites in Austria, Finland, Germany, and Sweden (Mann et al. 2013). Nalmefene was taken as needed (one 18-mg tablet per day) if the patient perceived a risk of relapse. Patients taking nalmefene significantly reduced the number of days they drank heavily and the total amount of alcohol they consumed compared with the placebo group (8.2 versus 10.7 heavy-drinking days; 33.3 versus 45.5 g of alcohol per day, respectively). The design of the second 24-week RCT was similar to the first, with 718 alcohol-dependent patients recruited across 57 sites in Belgium, the Czech Republic, France, Italy, Poland, Portugal, and Spain (Gual et al. 2013). Again, patients taking nalmefene as needed showed a significant reduction in the number of heavy-drinking days and a reduction (nonsignificant) in the amount of alcohol they consumed compared with the placebo group (6.6 versus 7.5 heavy-drinking days; 30 versus 33 g of alcohol per day, respectively). Interestingly, a secondary analysis of a subgroup of the heaviest drinkers in the two trials showed even larger nalmefene treatment effects (van den Brink et al. 2013). A year-long RCT trial was also conducted in 675 alcohol-dependent patients across 60 sites in the Czech Republic, Estonia, Hungary, Latvia, Lithuania, Poland, Russia, Slovakia, Ukraine, and the United Kingdom (van den Brink et al. 2014). Although there was no significant difference in drinking outcomes between those taking nalmefene as needed and the placebo groups at 6 months, there was a significant reduction in heavy-drinking days and alcohol consumption in the nalmefene group at 12 months. Nalmefene was well-tolerated across the three studies, with the most common side effects being nausea, vomiting, fatigue, insomnia, and dizziness. Although the oral formulation of nalmefene is not yet available or approved for use in AUD in the United States, it is approved for use in alcohol dependence in Europe.
1.1.2 Varenicline
1.1.2.1 Molecular and Functional Mechanisms of Action
Varenicline is a partial agonist at the α4β2 and a full agonist at α7 nicotinic acetylcholine receptor (Mihalak et al. 2006). It has been approved by the FDA for smoking cessation. Recent evidence indicates that varenicline also attenuates drinking in alcohol-dependent individuals. In several human laboratory studies, varenicline reduced alcohol craving and the subjective reinforcing effects of alcohol in non-alcohol-dependent heavy-drinking smokers, heavy-drinking smokers and nonsmokers, and non-treatment-seeking alcohol-dependent individuals (McKee et al. 2009; Roberts et al. 2017a, b; Schacht et al. 2014). Interestingly, in one human laboratory study, varenicline was most effective in heavy drinkers with high levels of depressive symptoms, in both reducing alcohol craving and alcohol self-administration (Roberts et al. 2017b). Finally, Vatsalya et al. (2015) showed that varenicline decreases activity in the striato-cortico-limbic regions of the brain, which are associated with alcohol craving/urges in heavy drinkers.
1.1.2.2 Results of Clinical Trials
Several small RCTs of varenicline showed efficacy in problematic drinkers. Fucito et al. (2011) conducted an 8-week RCT of varenicline (titrated up to 2 mg per day) in 30 heavy-drinking smokers. Varenicline was effective in reducing alcohol craving, resulting in fewer heavy-drinking days compared with those who received placebo. In a 16-week RCT with 64 heavy-drinking smokers, varenicline (2 mg per day) significantly reduced alcohol consumption compared with placebo (Mitchell et al. 2012b). In a 13-week RCT of 40 alcohol-dependent individuals, varenicline (2 mg per day) reduced alcohol craving compared with placebo, but drinking outcomes were similar (Plebani et al. 2013). However, smokers were less likely to report heavy drinking when taking varenicline compared with those taking placebo.
Results of these small RCTs were confirmed by a larger 13-week multisite RCT of varenicline (2 mg per day) in 200 alcohol-dependent individuals, approximately 40% of whom were smokers (Litten et al. 2013). Compared with the placebo group, the varenicline group had significantly fewer heavy-drinking days (37.9% each week versus 48.4%), drinks per day (4.4 versus 5.3), and drinks per drinking day (5.8 versus 6.8). Furthermore, varenicline also reduced alcohol craving. The efficacy was the same among smokers and nonsmokers. Notably, although the subgroup of alcoholic smokers was not seeking treatment for smoking, varenicline still reduced the number of cigarettes per day among smokers. A moderator analysis indicated that varenicline was most effective in individuals with less severe AUD and in those who reduced their smoking (Falk et al. 2015). Varenicline was well-tolerated. The most common adverse effects were nausea, abnormal dreams, and constipation. In another multisite RCT conducted in Sweden, 160 alcohol-dependent individuals were given either varenicline (2 mg per day) or placebo for 12 weeks (de Bejczy et al. 2015). In this study, there were no differences in self-reported drinking outcomes or reduction in smoking between the varenicline and placebo groups. However, there were significant reductions in alcohol craving, the number of reported AUD symptoms (measured using the Alcohol Use Disorders Identification Test [AUDIT]), and blood levels of phosphatidyl ethanol (PEth), a specific biomarker of alcohol consumption – all supporting an effect of varenicline on alcohol consumption.
The FDA recently removed the Box Warning about possible neuropsychiatric side effects on mood, behavior, or thinking when taking varenicline (https://www.fda.gov/Drugs/DrugSafety/ucm532221.htm). However, the FDA has issued a warning that varenicline may change the way patients respond to alcohol, affecting their ability tolerate its effects. Moreover, in rare accounts, seizures have been reported in patients taking varenicline (https://www.fda.gov/Drugs/DrugSafety/ucm436494.htm). However, none of these side effects were observed in the above RCTs.
1.1.3 Topiramate
1.1.3.1 Molecular and Functional Mechanisms of Action
Topiramate is an anticonvulsant approved by the FDA for treatment of seizures, migraines, and obesity (combined with phentermine for the latter indication). It has multiple pharmacologic effects in the brain. Topiramate antagonizes α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) and kainate receptors, facilitates GABA activity, blocks L-type calcium channels, reduces voltage-dependent sodium channel activity, and inhibits carbonic anhydrase (Arnone 2005). In two human laboratory studies, topiramate reduced the frequency of heavy drinking and the stimulating effects of alcohol in one study (Miranda et al. 2008) and alcohol craving in the other (Miranda et al. 2016).
1.1.3.2 Results of Clinical Trials
Several clinical trials showed topiramate was effective in reducing drinking in alcohol-dependent individuals, which was summarized by a recent meta-analysis (Blodgett et al. 2014). Johnson et al. (2003) first demonstrated the efficacy of topiramate in a single-site 12-week RCT with 150 alcohol-dependent individuals. Individuals receiving topiramate (up to 300 mg per day) had fewer drinks per day, more days abstinent, less heavy-drinking days, lower GGT, and less alcohol craving than those treated with placebo. Notably, unlike previous alcohol pharmacotherapy RCTs, this study did not require participants to be abstinent from alcohol before starting the trial. Therefore, the study assessed when abstinence began rather than how well it was maintained (i.e., abstinence initiation versus abstinence persistence). Side effects included dizziness, paresthesia, psychomotor slowing, memory or concentration impairment, nervousness, taste perversion, pruritus, and weight loss. The results of this study were replicated in a larger 14-week multisite RCT with 371 alcohol-dependent individuals (Johnson et al. 2007). Again, topiramate (titrated up to 300 mg per day) significantly reduced the number of heavy-drinking days, drinks per drinking day, and serum GGT levels and increased the number of days abstinent. The side-effect profile was similar to the original study.
Several smaller RCTs of topiramate have since followed. Knapp et al. (2015) conducted a single-site 14-week RCT in 21 alcohol-dependent individuals and found that topiramate (300 mg per day) significantly reduced the number of drinks per day, drinking days, and heavy-drinking days compared with placebo. Martinotti et al. (2014) conducted a low-dose topiramate (100 mg per day) RCT in 52 alcohol-dependent individuals and found it was effective in reducing daily alcohol consumption and alcohol craving and increasing the number of days abstinent. The side-effect profile for this lower dosage was more favorable than studies using 200 mg per day and 300 mg per day. In another study, Kranzler et al. (2014) conducted a 12-week RCT of topiramate (200 mg per day) in 138 alcohol-dependent individuals. Those receiving topiramate experienced fewer heavy-drinking days, reduced serum levels of GGT, and more abstinent days relative to placebo. Moreover, a post hoc analysis revealed that topiramate’s increased efficacy was moderated by a single nucleotide polymorphism (SNP). Patients with the CC genotype of the rs2832407 GRIK1 gene encoding the glutamate kainate GluK1 receptor showed improvement in drinking outcomes, whereas the other genotypes (AC and AA genotype) did not show efficacy with topiramate. Notably, a previous small laboratory study with heavy drinkers showed that individuals with the CC genotype of the rs2832407 GRIK1 gene had significantly fewer topiramate-related side effects and lower topiramate blood concentrations (Ray et al. 2009). A two-site RCT currently is being conducted in alcohol-dependent European-Americans and African-Americans to see if these promising findings can be replicated, both in terms of efficacy and safety/tolerability (ClinicalTrials.gov NCT02371889).
Interestingly, Anthenelli et al. (2017) recently conducted a 12-week RCT of topiramate (200 mg per day) in 129 alcohol-abstinent (mean of ~6 months) alcohol-dependent male smokers (80% had other substance use disorders). In this population, topiramate was not effective in reducing relapse to alcohol or smoking or other drug use. Thus, topiramate may be more useful in preventing or reducing alcohol consumption in current drinkers than in preventing relapse to drinking in individuals with AUD who are abstinent. This finding was consistent with other positive RCTs (Johnson et al. 2003, 2007) where abstinence initiation rather than abstinence persistence was assessed.
As a final note, it appears that topiramate has gained acceptance with some large clinical care provider organizations, such as the Veterans Health Administration (Del Re et al. 2013). Nonetheless, research continues to explore other medications with similar mechanisms of action but with a more favorable safety profile, particularly regarding cognitive dysfunction (see zonisamide and levetiracetam below).
1.1.4 Zonisamide
1.1.4.1 Molecular and Functional Mechanisms of Action
Zonisamide is approved by the FDA as an adjunct treatment for partial seizures. Like topiramate, it has multiple molecular actions in the brain, including blocking voltage-sensitive sodium channels and T-type calcium channels, facilitating GABA activity, and serving as a weak inhibitor of carbonic anhydrase (Kothare and Kaleyias 2008). However, the side-effect profile of zonisamide appears to be more favorable than topiramate, with the most common being somnolence, anorexia, dizziness, decreased cognitive dysfunction, headache, nausea, and agitation/irritability (Kothare and Kaleyias 2008; https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/020789s019lbl.pdf). In a human laboratory study of risky drinkers, zonisamide reduced alcohol craving and alcohol intake in a self-administration paradigm compared with placebo (Sarid-Segal et al. 2009).
1.1.4.2 Results of Clinical Trials
Several open-label trials (no placebo group) suggest that zonisamide may be effective in reducing alcohol consumption and craving in alcohol-dependent individuals (Knapp et al. 2010; Rubio et al. 2010). Zonisamide was well-tolerated in these studies. This preliminary work was followed by a 12-week RCT of zonisamide (up to 500 mg per day) in 40 alcohol-dependent individuals (Arias et al. 2010). Zonisamide significantly reduced the number of heavy-drinking days, drinks per week, and alcohol craving compared with placebo. It was well-tolerated with no serious side effects. In another RCT, 85 alcohol-dependent individuals were administered either zonisamide (400 mg per day), topiramate (300 mg per day), levetiracetam (200 mg per day), or placebo for 14 weeks (Knapp et al. 2015). Zonisamide and topiramate significantly reduced the percent of drinking days per week, drinks per day, and heavy drinking per week compared with placebo (results were slightly more favorable for topiramate). Levetiracetam was only effective in decreasing the percent of heavy-drinking days per week. Neurotoxicity and cognitive function were also evaluated for the three compounds. Individuals treated with zonisamide or topiramate were more likely to experience impairments in verbal fluency and verbal working memory. Those treated with topiramate also had visual memory impairments, and were slower to recall events, compared with zonisamide. This indicates less severe side effects with zonisamide compared with topiramate. Levetiracetam did not produce any performance decreases on the neuropsychological tests.
Several ongoing trials are being conducted with zonisamide in veteran and non-veteran AUD patients with and without posttraumatic stress disorder (ClinicalTrials.gov NCT02368431, NCT01847469, NCT02901041, and NCT02900352).
1.1.5 Gabapentin
1.1.5.1 Molecular and Functional Mechanisms of Action
Gabapentin is approved by the FDA for the treatment of epileptic seizures, neuropathic pain, and restless legs syndrome. Its mechanism of action is thought to be related to its inhibition of voltage-gated calcium channels, which indirectly modulate GABA activity (Sills 2006). In a human laboratory study, Mason et al. (2009) demonstrated that gabapentin (1,200 mg per day) was effective in reducing alcohol craving and improving sleep quality.
1.1.5.2 Results of Clinical Trials
Several single-site RCTs of gabapentin have been conducted in alcohol-dependent patients. Furieri and Nakamura-Palacios (2007) conducted a 4-week RCT of gabapentin (600 mg per day) in 60 male alcohol-dependent patients from a Brazilian public outpatient drug treatment center. Gabapentin significantly reduced the number of drinks per day and number of heavy-drinking days and increased the percent of days abstinent. Brower et al. (2008) conducted a small 6-week RCT trial of gabapentin (titrated to 1,500 mg per day) in 21 alcohol-dependent individuals who also were diagnosed with insomnia. Gabapentin significantly delayed the onset of heavy drinking compared with placebo, but did not differ from the placebo group in improving insomnia. In another RCT, gabapentin (up to 1,200 mg per day for 39 days) was combined with flumazenil (20 mg per day for first 2 days) in 60 alcohol-dependent patients (44 with relatively fewer and 16 with relatively more pretreatment alcohol withdrawal symptoms) (Anton et al. 2009). Individuals with more alcohol withdrawal symptoms before treatment had an increase in the percent of days abstinent and a longer delay to heavy drinking when taking combined gabapentin and flumazenil compared with placebo. On the other hand, those with fewer alcohol withdrawal symptoms before treatment did not differ in drinking outcomes compared with the placebo groups. In another RCT, 150 alcohol-dependent individuals received either 16 weeks of naltrexone (50 mg per day) or naltrexone (50 mg per day) combined with gabapentin (up to 1,200 mg per day for the first 6 weeks) or double placebo (Anton et al. 2011). During the first 6 weeks, the combined medication group experienced a longer delay to heavy drinking, less heavy-drinking days, and fewer drinks per drinking day than the group taking naltrexone alone or those receiving the placebo. In addition, the naltrexone/gabapentin group reported significantly better sleep than the other two groups. Finally, Mason et al. (2014) conducted a 12-week RCT of gabapentin (900 mg per day and 1,800 mg per day) in 150 patients with alcohol dependence. Gabapentin significantly improved the rates of abstinence and no heavy drinking. The abstinence rate was 4.1% for the placebo group, 11.1% for the 900 mg group, and 17.0% for the 1,800 mg group, while the rate of no heavy drinking was 22.5% for the placebo group, 29.6% for the 900 mg group, and 44.7% in the 1,800 mg group. Gabapentin also showed a dose effect on alcohol craving, mood, and sleep. Gabapentin was well-tolerated with the most common side effects being fatigue, insomnia, and headaches.
Although gabapentin is considered to have no abuse potential, a recent report indicates that gabapentin potentially may be misused in substance abuse populations, especially those who abuse opioids (Smith et al. 2016). NIAAA currently is conducting a multisite RCT on enacarbil gabapentin, an extended-release prodrug (a medication that is metabolized into a pharmacologically active drug after administration) designed to increase its bioavailability (ClinicalTrials.gov: NCT02252536).
1.1.6 Baclofen
1.1.6.1 Molecular and Functional Mechanisms of Action
Baclofen is a GABAB agonist approved by the FDA for the treatment of muscle spasticity. Several human laboratory studies suggest that baclofen may affect alcohol drinking behavior by changing the subjective effects of alcohol (Evans and Bisaga 2009; Farokhnia et al. 2017; Leggio et al. 2013).
1.1.6.2 Results of Clinical Trials
Several RCTs have provided mixed results on the efficacy, optimal dose, and safety of baclofen. Addolorato et al. (2002) conducted a 4-week RCT of baclofen (30 mg per day) in 39 alcohol-dependent individuals. The results showed that baclofen increased abstinence rates and the number of days abstinent compared with placebo. The medication also reduced alcohol craving and state anxiety levels. The same group conducted a larger 12-week RCT of baclofen (30 mg per day) in 84 alcohol-dependent individuals with co-occurring liver cirrhosis (Addolorato et al. 2007). Individuals treated with baclofen experienced a higher rate of abstinence compared with placebo (71% versus 29%, respectively). Baclofen also significantly increased number of days abstinent and reduced alcohol craving. Baclofen was well-tolerated with no additional hepatic side effects. Indeed, there was an improvement of blood liver tests in the baclofen group versus placebo, most likely because of baclofen’s effects in facilitating alcohol abstinence. In contrast, Garbutt et al. (2010) found no effect of baclofen (30 mg per day) in a 12-week RCT with 80 alcohol-dependent individuals. There were no differences in number of heavy-drinking days, percent of days abstinent, time to first drink, or time to relapse to heavy drinking between the baclofen and placebo groups. However, baclofen reduced the level of anxiety state, consistent with its mechanism of reducing the symptoms of alcohol withdrawal. Baclofen was well-tolerated with the most common side effect being drowsiness. Morley et al. (2014) conducted a 12-week RCT with 42 alcohol-dependent individuals using 30 mg per day of baclofen, 60 mg per day of baclofen, or placebo. There were no differences in time to first heavy-drinking day, time to first drink, number of heavy-drinking days, drinks per drinking day, or percent of days abstinent between the baclofen and placebo groups. In a subgroup analysis, individuals who received 30 mg per day of baclofen and who had a lifetime or current anxiety disorder experienced a significant increase in the time to first drink and time to first heavy-drinking day. Again, the major side effect of baclofen was drowsiness. Finally, a small 12-week RCT was conducted to determine if baclofen (80 mg per day) was effective in treating alcohol-dependent individuals who also were smokers (n = 30) (Leggio et al. 2015). Baclofen, compared with placebo, significantly increased the number of days abstinent from alcohol and tobacco co-use, but did not significantly increase the number of days abstinent from alcohol use alone.
Two anecdotal reports showing that high doses of baclofen [up to 140 mg per day (Bucknam 2007) and up to 300 mg per day (Ameisen 2005)] resulted in abstinence from alcohol led researchers to wonder if it was more effective in these higher amounts. Muller et al. (2015) conducted a RCT with a high dose of baclofen (up to 250 mg per day) in 56 alcohol-dependent individuals. Those treated for 12 weeks with 250 mg per day had a greater abstinence rate (68.2% versus 23.8% for placebo) and more cumulative abstinence duration (67.8 versus 51.8 for placebo). No serious adverse events were observed. In contrast to these findings, Beraha et al. (2016) conducted a RCT of baclofen in 151 alcohol-dependent individuals who were administered a high dose (150 mg per day; 6 weeks titration, 10 weeks of high dose), a low dose (30 mg per day), or placebo. There were no differences in time to first relapse or abstinence rates among the three groups (although only 15.5% of those in the high dose group reached the 150 mg per day). The high dose group experienced more adverse events, particularly fatigue, sleepiness, drowsiness, dizziness, and dry mouth. In another multisite RCT, baclofen (180 mg per day) or placebo was administered to 320 alcohol-dependent individuals for 24 weeks (Reynaud et al. 2017). Although baclofen significantly reduced alcohol craving, there were no significant differences in percent of abstinence and drinks per day between the baclofen and placebo groups. However, in a subgroup analysis, baclofen was more effective than placebo in reducing drinking in individuals who were drinking heavily at the start of the study. There were no major adverse effects; the most common were somnolence, sleep disorders, asthenia, and dizziness.
The mixed results of these RCTs suggest that baclofen works in a subgroup of patients. In particular, it is conceivable that baclofen might be an effective medication in those patients with higher severity of alcohol dependence (Leggio et al. 2010). Whether higher doses are more effective remains unclear and controversial, although higher doses may have a greater risk of adverse events. For example, Rolland et al. (2015), in a study of 253 alcohol-dependent individuals, found a positive relationship between the dose of baclofen and the likelihood of major sedation. In addition, Boels et al. (2017) reported that baclofen, prescribed in high doses, may lead to severe poisoning (cardiovascular, neurological metabolic, respiratory symptoms), particularly in patients with psychiatric illnesses. Currently, several RCTs are being conducted using baclofen, which may shed light on its efficacy, optimal dose (high versus low), safety, and possible subgroups who may respond more favorably to this medication (ClinicalTrials.gov NCT02835365, NCT 03034408, NCT01980706, NCT02723383, and NCT02596763).
1.1.7 Ondansetron
1.1.7.1 Molecular and Functional Mechanisms of Action
Ondansetron is a selective serotonin 5-HT3 antagonist approved by the FDA for the treatment of nausea and vomiting. Several laboratory studies have shown that ondansetron reduces the desire to drink and augments the stimulating and sedating effects of alcohol (Johnson et al. 1993; Kenna et al. 2009; Swift et al. 1996).
1.1.7.2 Results of Clinical Trials
In a groundbreaking RCT, Sellers et al. (1994) administered 0.25 mg or 2.0 mg per day of ondansetron or placebo to 71 alcohol-dependent individuals. After 6 weeks of treatment, the 0.25 mg ondansetron group significantly decreased drinks per drinking day compared with placebo (35% versus 21% reduction) in people consuming ten or less drinks per drinking day at baseline. Interestingly, the daily 0.25 mg dose of ondansetron was more effective than the 2.0 mg dose. In a subsequent 11-week RCT, 271 alcohol-dependent individuals were randomized to receive 2 μg/kg, 8 μg/kg, or 32 μg/kg per day of ondansetron or placebo (Johnson et al. 2000). An equal number of patients with early (25 years of age or younger) and late (>25 years) onset of alcoholism were recruited. Ondansetron significantly reduced the number of drinks per day and the number of drinks per drinking day compared with placebo, but only in people with early onset of alcoholism. The 8 μg/kg dose of ondansetron was the most effective dose, increasing the percent of days abstinent and total abstinence compared with placebo. Ondansetron was well-tolerated with no serious adverse events. Kranzler et al. (2003) later confirmed these results by conducting an open-label trial of ondansetron (8 μg per kg per day) in 40 early and late-onset alcohol-dependent individuals. The early-onset individuals experienced a greater decrease in drinks per day, drinks per drinking day, and alcohol-related consequences compared with late-onset alcoholic individuals.
These clinical studies led researchers to question if a biological marker might be able to predict a response to ondansetron. In particular, Johnson et al. (2011) hypothesized that there might be a pharmacogenetic interaction between ondansetron and the SLC6A4 gene. That gene encodes the serotonin transporter, 5-HTT, which is associated with several psychiatric disorders. The SLC6A4 consists of two types of alleles, a long form (L) and a short form (S) consisting of 44 less base pairs. Johnson et al. (2011) conducted an 11-week RCT of ondansetron (8 μg/kg per day) in 283 dependent individuals randomized to three different genotypes: LL, LS, and SS genotypes of 5-HTT. Individuals with the LL genotype who received ondansetron had a significantly lower number of drinks per drinking day and a higher percent of days abstinent than those treated with the LS/SS genotypes who received the medication or those who received placebo regardless of their genotype. The research team also discovered another functional single nucleotide polymorphism (T/G) rs1042173, in the 3′-untranslated region of the SLC6A4 gene. Individuals with the LL/TT genotype experienced a significantly lower number of drinks per drinking day and higher percent of days abstinent than all other genotypes and treatment groups combined. In a later analysis from the same RCT, Johnson et al. (2013) found additional functional genetic polymorphisms in the HTR3A and HTR3B genes, including AC in the rs17614942 in the HTR3B gene and AG in the rs1150226 and GG in the rs1176713 portion of the HTR3A gene. Ondansetron was more effective in reducing the number of drinks per drinking day and the number of heavy-drinking days and increasing the percent of days abstinent in people carrying one or more of these genetic variants. Kenna et al. (2014a) conducted a laboratory study of ondansetron and sertraline in 77 non-treatment-seeking alcohol-dependent individuals. Consistent with Johnson et al. (2011), Kenna et al. (2014a) found a pharmacogenetic interaction between the LL genotype and ondansetron, but no effect was found for sertraline. Specifically, ondansetron was effective in reducing the amount of drinks per drinking day in people with the LL genotype. In a later analysis from the same human laboratory study, Kenna et al. (2014b) found that women (not men) who had the LL genotype and equal or greater than 7 exon III repeats on the dopamine receptor D4 gene (DRD4) experienced less alcohol intake after taking ondansetron (0.5 mg per day for 3 weeks).
Finally, ondansetron given in doses cited above was much lower than that required to treat nausea and vomiting (approximately 10 times less). The FDA has issued a safety warning for ondansetron, indicating it may increase the risk of abnormal electrical activity in the heart (https://www.fda.gov/Drugs/DrugSafety/ucm271913.htm). However, this side effect may not be evident at the low doses required to treat AUD.
NIAAA is currently supporting a two-site RCT of ondansetron to confirm these promising genetic findings of Johnson et al. (2011, 2013) (ClinicalTrials.Gov NCT02354703).
1.1.8 Prazosin and Doxazosin
1.1.8.1 Molecular and Functional Mechanisms of Action
Prazosin and doxazosin are both selective α-1 adrenergic antagonists approved by the FDA to treat hypertension and benign prostatic hyperplasia. Fox et al. (2011) conducted a human laboratory study on prazosin (16 mg daily) in 17 recently abstinent, treatment-seeking alcohol-dependent individuals. Following cue and stress exposure, the prazosin group significantly reduced alcohol craving and reported lower levels of anxiety and negative emotions compared with the placebo group.
1.1.8.2 Results of Clinical Trials
A 6-week study by Simpson et al. (2009) found that prazosin (16 mg per day), compared with placebo, reduced drinking days per week and drinks per week in 24 alcohol-dependent patients without posttraumatic stress disorder (PTSD). Subsequently, Simpson et al. (2015) conducted a small 6-week RCT of prazosin (16 mg per day) in 30 individuals with co-occurring alcohol dependence and PTSD. Individuals treated with prazosin experienced a reduction in the percent of drinking days and percent of heavy-drinking days compared with placebo. No significant differences were found between the prazosin and placebo groups in terms of the PTSD symptoms. This is surprising because prazosin has been shown to be effective in treating PTSD (Green 2014). The most common side effects of prazosin were drowsiness, dizziness on standing, and fatigue. Petrakis et al. (2016) later conducted a 13-week RCT of prazosin (16 mg per day) in 96 veterans with co-occurring alcohol dependence and PTSD. There were no significant differences between the prazosin and placebo groups in the drinking outcomes, alcohol craving, or the PTSD symptoms. The mixed results of these studies suggest that the medication may be effective only in subgroups. Raskind et al. (2016), for example, reported that prazosin worked best in reducing PTSD symptoms in patients who had a higher baseline standing blood pressure. Current studies are investigating this compound in people with comorbid alcohol dependence and PTSD (ClinicalTrials.gov NCT00585780 and NCT02226367).
Alcohol researchers also are investigating doxazosin, another α-1 adrenergic antagonist. The advantage of doxazosin over prazosin is that given its significantly longer half-life, doxazosin requires only once-a-day dosing compared with prazosin’s two to three dosages per day; frequency of side effects is lower; and, unlike prazosin, doxazosin may be taken with or without food (Leggio and Kenna 2013). All these properties are important in RCTs and in clinical practice as they could potentially increase medication adherence. Kenna et al. (2015) conducted a 10-week RCT of doxazosin (up to 16 mg per day) in 41 alcohol-dependent individuals. In the main analysis, no significant differences were found in the drinking outcomes between the doxazosin and placebo groups. However, in a priori moderator analyses, doxazosin-treated individuals with a greater family history of alcoholism experienced a significant decrease in the number of drinks per week and in the number of heavy-drinking days per week compared with placebo-treated, high-family-history individuals. In a later analysis from the same RCT, Haass-Koffler et al. (2017) found that doxazosin, compared with placebo, reduced the number of drinks per week and heavy-drinking days per week in a subgroup of patients who had higher baseline standing blood pressure.
These studies suggest that precision medicine may be important in using α-1 adrenergic antagonists to treat AUD.
1.1.9 ABT-436 (Vasopressin V1b Receptor Antagonist)
1.1.9.1 Molecular and Functional Mechanisms of Action
Vasopressin, a peptide released from the hypothalamus, acts on the type 1b receptor (V1b) at the pituitary, activating the hypothalamic-pituitary-adrenal (HPA) axis, which, in turn, regulates the body’s stress response (Milivojevic and Sinha 2017). In addition, vasopressin acts on the extra-hypothalamic stress system, especially in the extended amygdala. Blocking the V1b receptors in various animal models has resulted in decreased alcohol intake (Edwards et al. 2011; Zhou et al. 2011).
1.1.9.2 Results of a Clinical Trial
In a recent 12-week multisite RCT, ABT-436, a novel selective V1b receptor antagonist, was evaluated in 150 alcohol-dependent individuals (Ryan et al. 2017). ABT-436 (titrated to 800 mg per day) significantly increased the percent of days abstinent compared with placebo (51.2 versus 41.6, respectively). The percent of heavy-drinking days was lower in people receiving ABT-436 compared with placebo, although the difference was not statistically significant. Other measures of drinking, alcohol craving, and alcohol-related consequences did not differ between the ABT-436 and placebo groups. However, in smokers, the compound significantly reduced the number of cigarettes consumed compared with placebo. In moderator analyses, individuals reporting higher baseline levels of stress responded better to ABT-436 than to placebo on drinking outcomes. ABT-436 was well-tolerated, with diarrhea (mild-to-moderate severity) being the most common side effect. Unfortunately, AbbVie, Inc. has recently discontinued development of this compound.
1.1.10 Aripiprazole
1.1.10.1 Molecular and Functional Mechanisms of Action
Aripiprazole is an atypical, antipsychotic medication approved by the FDA for the treatment of schizophrenia, bipolar disorder, and for use as adjunct treatment for major depression (Litten et al. 2016a). It has multiple pharmacological mechanisms in the brain, including acting as a partial agonist for the dopamine D2 and serotonin 5-HT1A receptors and as an antagonist to the 5-HT2 receptors (Fleischhacker 2005). Several human laboratory studies suggest that aripiprazole may affect drinking behavior. Kranzler et al. (2008) reported that aripiprazole (2.5 mg and 10 mg per day) increased the sedating effects of alcohol and, to a lesser degree, reduced the euphoric effects. In another human laboratory study, Voronin et al. (2008) reported that aripiprazole (up to 15 mg per day) reduced drinking in non-treatment-seeking alcohol-dependent individuals, but had no effect on self-reported “high,” intoxication, or alcohol craving when compared with the placebo group. Finally, Myrick et al. (2010) showed that aripiprazole (15 mg per day) blunted alcohol-cue-induced brain activity in the right ventral striatum. Anton et al. (2017) recently completed a human laboratory study of aripiprazole (15 mg per day) in 99 non-treatment-seeking alcohol-dependent individuals. In a bar-lab setting, aripiprazole significantly decreased alcohol self-administration among individuals with low self-control and delayed the return to drinking in those with high impulsivity compared with placebo.
1.1.10.2 Results of Clinical Trials
Martinotti et al. (2009) conducted a 16-week RCT of aripiprazole (up to 15 mg per day) and naltrexone (50 mg per day) in 75 alcohol-dependent subjects. During treatment, the aripriprazole and naltrexone groups displayed similar reductions on measures of abstinence, percent days abstinent and number of heavy drinking days. However, patients treated with aripiprazole remained abstinent for a longer period of time than those treated with naltrexone. Anton et al. (2008) conducted a 12-week multisite RCT of aripiprazole with mixed results. Aripiprazole (titrated up to 30 mg per day) was effective in reducing the number of drinks per drinking day compared with the placebo group and reduced CDT at weeks 4 and 8. However, the aripiprazole group did not differ from the placebo group in percent of days abstinent, number of heavy-drinking days, and time to first drinking day. The authors postulated that these lackluster results possibly were related to dose-related attrition, as the aripiprazole group had a higher dropout rate than the placebo group, especially with the 30 mg dose. The most common side effects from aripiprazole were fatigue, insomnia, restlessness, somnolence, anxiety, and disturbances in attention. It has been suggested that aripiprazole may be efficacious at lower doses (15 mg per day). NIAAA is currently supporting an aripiprazole RCT in individuals with AUD and bipolar disorder, comparing the 15 and 30 mg daily doses (NCT02918370).
1.1.11 LY 2940094 (Nociceptin Receptor Antagonist)
1.1.11.1 Molecular and Functional Mechanisms of Action
The nociceptin (NOP) receptor (formerly known as opioid receptor-like) belongs to the opioid receptor family. Several studies have shown that targeting this receptor modifies alcohol drinking behavior in animal models (Aziz et al. 2016; Ciccocioppo et al. 2004; Economidou et al. 2008, 2011). Recently, Lilly Research Laboratories synthesized a NOP antagonist, LY2940094, that demonstrated an antidepressant effect in individuals with major depressive disorder (Post et al. 2016a). In addition, Rorick-Kehn et al. (2016) reported that LY2940094 was effective in decreasing alcohol intake in animal models bred to show a preference for alcohol.
1.1.11.2 Results of a Clinical Trial
Post et al. (2016b) conducted an 8-week multisite RCT trial of LY2940094 (40 mg per day) in 88 alcohol-dependent individuals. LY2940094 reduced the number of heavy-drinking days compared with placebo (−24.5% versus −15.7%, respectively) and increased the percent of days abstinent (9.1% versus 1.9%, respectively). Although the primary endpoint, drinks per day, did not differ between the two groups in the full sample, the compound did reduce drinks per day in two subgroups: those who drank less at baseline and women. Because most of the women had lower baseline drinking, it was difficult to determine which moderator had the most effect. The compound was well-tolerated with no serious adverse effects. The most common side effects were insomnia, anxiety, and vomiting. Currently, BlackThorn Therapeutics has licensed the compound from Lilly for further development.
1.1.12 LY2196044 (Opioid Receptor Antagonist)
1.1.12.1 Molecular and Functional Mechanisms of Action
The novel compound LY2196044, synthesized by Eli Lilly and Company, is an opioid receptor antagonist at the mu, kappa, and delta receptors. This compound has been shown to reduce drinking in animal models (Wong et al. 2014) through a mechanism similar to naltrexone and nalmefene.
1.1.12.2 Results of a Clinical Trial
In a 16-week multisite trial in 375 alcohol-dependent individuals, LY2196044 (up to 250 mg per day) significantly reduced the number of drinks per day from baseline compared with placebo (−5.4 versus −4.7, respectively) (Wong et al. 2014). However, the number of heavy-drinking days and percent of days abstinent did not differ significantly between the two groups. In a subgroup analysis, LY2196044 significantly improved the drinking outcomes in people with the dopamine receptor type 4 (DRD4) gene carrying tandem repeat L (which occurred in 39% of the subjects), compared with L carriers who received only the placebo. LY2196044-treated individuals had more gastrointestinal-related adverse events than did placebo-treated individuals, a finding similar to other opioid antagonists, such as naltrexone and nalmefene.
1.2 Medications That Have Shown Poor Efficacy in Multisite Alcohol Pharmacotherapy Clinical Trials Despite Promising Preliminary Studies
1.2.1 Quetiapine
1.2.1.1 Molecular and Cellular Mechanisms of Action
Quetiapine is an atypical antipsychotic medication approved by the FDA for treatment of schizophrenia, manic episodes associated with bipolar I disorder, depressive episodes associated with bipolar disorder, and as an adjunct treatment for major depression (Litten et al. 2016a). Quetiapine has multiple actions in the brain, blocking the serotonin 5-HT1A and 5-HT2A receptors, the dopamine D1 and D2 receptors, the histamine H1 receptors, and the adrenergic α1 and α2 receptors (Ray et al. 2010). Two human laboratory studies have found that non-treatment-seeking alcohol-dependent individuals treated with quetiapine (400 mg per day) experienced reduced alcohol craving and alcohol-induced sedation and impulsivity, compared with placebo (Moallem and Ray 2012; Ray et al. 2011).
1.2.1.2 Results of Clinical Trials
In three open-label studies, alcohol-dependent individuals who were treated with quetiapine improved their drinking outcomes (Martinotti et al. 2008; Monnelly et al. 2004; Sattar et al. 2004). Kampman et al. (2007) conducted a 12-week pilot RCT of quetiapine (400 mg per day) in 61 Type A and Type B alcohol-dependent individuals. [Type A alcoholics are characterized by late age of onset of problem drinking, low severity of alcohol dependence, few childhood risk factors, less concomitant psychopathology, and reduced drug use. In contrast, Type B alcoholics are characterized by early age of onset of alcohol problems, high severity of alcohol dependence, polydrug use, and a high degree of concomitant psychopathology (Babor et al. 1992).] Quetiapine-treated Type B alcoholic individuals experienced fewer days of drinking and days of heavy drinking and less alcohol craving than Type B alcoholic individuals treated with placebo. In contrast, among the Type A alcoholic individuals, there were no differences between the quetiapine and placebo groups.
To confirm these findings, Litten et al. (2012) conducted a multisite 12-week RCT of quetiapine (titrated to 400 mg per day) in 224 alcohol-dependent individuals. Surprisingly, there were no differences between the quetiapine and placebo groups in percent of heavy-drinking days, drinks per day, drinks per drinking day, percent of days abstinent, and percent of abstinent individuals. In a subgroup analysis, Type B alcoholic individuals, regardless of whether they took quetiapine or placebo, did not differ in drinking outcome. As expected, quetiapine improved sleep and symptoms of depression. Quetiapine was well-tolerated, with the most common side effects being dizziness, dry mouth, dyspepsia, increased appetite, sedation, and somnolence. This study was followed by another 12-week RCT of quetiapine (titrated to 600 mg per day) in 90 alcohol-dependent individuals diagnosed with comorbid bipolar I or II disorders and depressed or mixed mood state (Brown et al. 2014). The quetiapine group did not differ from the placebo group in drinks per day, percent of days abstinent, drinks per drinking day, and percent of heavy-drinking days. Finally, in another 12-week RCT, Stedman et al. (2010) found that quetiapine (300–800 mg per day, flexible dosing) when added as an adjunct therapy with lithium or divalproex, was no better than placebo in reducing alcohol use in 362 individuals with comorbid alcohol dependence and bipolar I disorder. Together, these RCTs do not support the use of quetiapine for AUD.
1.2.2 Levetiracetam
1.2.2.1 Molecular and Functional Mechanisms of Action
Like topiramate and zonisamide, levetiracetam is approved by the FDA to treat seizures, yet it has fewer reported side effects (Litten et al. 2016a). It targets multiple mechanisms in the brain, including activating the GABA and glycine systems, inhibiting glutamate AMPA receptors, decreasing sodium/calcium channel currents, and modulating the synaptic vesicle protein 2A (Abou-Khalil 2008; De Smedt et al. 2007, Fertig et al. 2012).
1.2.2.2 Results of Clinical Trials
Two open-label trials indicated that levetiracetam reduced alcohol consumption in alcohol-dependent individuals (Mariani and Levin 2008; Sarid-Segal et al. 2008). This was followed by multiple RCTs. As mentioned previously (in the topiramate and zonisamide sections), Knapp et al. (2015) conducted a 14-week single-site RCT with zonisamide (400 mg per day), topiramate (300 mg per day), and levetiracetam (2,000 mg per day) in 85 alcohol-dependent individuals. Levetiracetam showed less efficacy than zonisamide and topiramate in reducing drinking (only reducing the number of heavy-drinking days compared with placebo). Unlike zonisamide and topiramate, levetiracetam showed no cognitive impairment. This confirmed an earlier study by Gomer et al. (2007) that also found no cognitive impairment from levetiracetam. Fertig et al. (2012) conducted a 16-week multisite trial of levetiracetam (2,000 mg per day) in 130 alcohol-dependent individuals. There were no differences on any drinking outcomes (percent of heavy-drinking days, drinks per day, drinks per drinking day, or percent of days abstinent) between the levetiracetam and the placebo groups. The medication was well-tolerated, with fatigue being the only significant side effect. In another 16-week multisite RCT of levetiracetam (2,000 mg per day) in 201 recently detoxified alcohol-dependent individuals, Richter et al. (2012) found the compound did not affect the rate/time of relapse compared with the placebo. In addition, Mitchell et al. (2012a) conducted a 6-week single-site RCT of levetiracetam in 46 moderate-to-heavy drinkers. Individuals were given a 500–1,000 mg dose per day, a 1,000–2,000 mg dose per day, or placebo. Levetiracetam had no effect on drinking outcome. Interestingly, individuals who initially were drinking less actually experienced an increase in drinking with levetiracetam, compared with placebo. Thus, these RCTs indicate that levetiracetam has very limited efficacy, if any, for treating AUD individuals.
1.3 Promising Medications: Ongoing Human Studies
1.3.1 Mifepristone
1.3.1.1 Molecular and Functional Mechanisms of Action
Mifepristone is a glucocorticoid receptor antagonist approved by the FDA for terminating pregnancy (together with misoprostol) and for treating hyperglycemia in patients with Cushing syndrome and type 2 diabetes mellitus and endometriosis. Alterations in the brain glucocorticoid system are believed to drive compulsive-like alcohol consumption in rats (Richardson et al. 2008; Simms et al. 2012; Vendruscolo et al. 2012). Recently, Vendruscolo et al. (2015) tested the efficacy of mifepristone in both rats and humans. Mifepristone reduced alcohol intake in alcohol-dependent rats but not in non-dependent rats. Vendruscolo et al. (2015) then tested the medication (600 mg daily for 1 week) in a laboratory setting in 56 non-treatment-seeking alcohol-dependent people. Mifepristone significantly reduced alcohol-induced craving during the laboratory session and reduced alcohol consumption during the 1-week treatment phase and 1-week posttreatment phase compared with placebo. There were no serious adverse effects, and there were no differences in the type or severity of adverse events during treatment between the mifepristone and placebo groups. Currently, human laboratory and RCT studies are evaluating the efficacy and safety of mifepristone (ClinicalTrials.gov: NCT02243709 and NCT02179749).
1.3.2 Oxytocin
1.3.2.1 Molecular and Functional Mechanisms of Action
Oxytocin is a nine-amino acid polypeptide hormone approved by the FDA for inducing labor and terminating pregnancy and as an adjunctive therapy in the management of incomplete or inevitable abortion. It also plays a role in the brain’s reward and stress systems, as well as in networks that have a role in social affiliations, learning, and memory. Recent studies show that oxytocin affects alcohol drinking behavior in animal models (Lee et al. 2016; Lee and Weerts 2016). In particular, King et al. (2017) demonstrated reduced alcohol consumption in different models of alcohol self-administration in mice, and Peters et al. (2016) reported that oxytocin inhibited alcohol consumption and alcohol-induced dopamine release in the nucleus accumbens of rats. A pilot RCT of oxytocin (48 IU per day, intranasal) was conducted in 11 alcohol-dependent individuals admitted for medical detoxification (Pedersen et al. 2013). Oxytocin was more effective than placebo in reducing craving and the symptoms of alcohol withdrawal. Mitchell et al. (2016) conducted a human laboratory study of oxytocin (40 IU, intranasal) in 32 non-treatment-seeking individuals with alcohol abuse. Subjects receiving oxytocin had significant improvements in social perception, compared with those receiving placebo, but there was no effect on alcohol-induced craving. However, in a subgroup analysis, oxytocin reduced alcohol craving in people with higher levels of attachment anxiety and increased alcohol craving in those with lower levels of attachment anxiety. Several human laboratory studies are currently underway to study the effects of oxytocin in AUD individuals (ClinicalTrials.gov NCT03046836, NCT02407340, and NCT02711189).
1.3.3 Ibudilast
1.3.3.1 Molecular and Functional Mechanisms of Action
Ibudilast (AV-411) is a nonselective phosphodiesterase inhibitor known to suppress glial cell activation and neuroinflammation (Ledeboer et al. 2007). Bell et al. (2013) showed that ibudilast reduced drinking in multiple animal models of alcohol dependence. In a crossover human laboratory study, ibudilast (100 mg per day) was no better than placebo in reducing subjective measures such as alcohol craving, stimulation, sedation, positive mood, and negative mood (Ray et al. 2017). However, ibudilast, compared with placebo, was associated with improvements in mood during stress- and alcohol-cue exposure. In a subgroup analysis, individuals with elevated depression had reduced stimulant and mood-altering effects of alcohol when given ibudilast, compared with those receiving placebo.
1.3.4 D-Cycloserine
1.3.4.1 Molecular and Functional Mechanisms of Action
D-cycloserine is a partial agonist at the glycine modulatory site of the glutamate NMDA receptor. It is FDA approved for the treatment of tuberculosis and urinary tract infection. The compound is also thought to enhance learning, memory, and decision making because of its action on the NMDA receptor (Kelley 2004; Scholl et al. 2014). In addition, D-cycloserine has been shown to reduce alcohol intake in rats (Seif et al. 2015). Several human studies have been conducted with D-cycloserine to determine if the medication enhances cue-exposure therapy in alcohol-dependent and problem-drinking individuals. Watson et al. (2011) conducted a small human laboratory study in 16 abstinent alcohol-dependent individuals. D-cycloserine (single dose of 250 mg) did not differ from placebo in reducing the alcohol-induced cue response. However, because a high percentage of individuals had little or no response to the cue exposure, it was difficult for D-cycloserine to actually show an effect. In another human laboratory study, Hofmann et al. (2012) found that D-cycloserine (50 mg) increased alcohol craving compared with placebo in 20 non-treatment-seeking problem drinkers during an alcohol-cue paradigm. In contrast, MacKillop et al. (2015) later reported that D-cycloserine (50 mg) lowered cue-elicited craving for alcohol in 37 treatment-seeking AUD individuals. In addition, D-cycloserine reduced drinking during the 1-week interval between the cue-extinction paradigms. Finally, Kiefer et al. (2015) conducted a human laboratory study of D-cycloserine (50 mg) in 76 recently detoxified abstinent alcohol-dependent individuals. Using functional magnetic resonance imaging (fMRI), D-cycloserine, compared with placebo, decreased brain activation in the ventral and dorsal striatum, areas of the mesolimbic system associated with addiction. Further studies are needed to validate the efficacy of this compound for the treatment of AUD.
1.4 Other Promising Medications (Preclinical or Theoretical)
In addition to the medications above, NIAAA is supporting initial human studies of compounds that have shown promise in preclinical studies and/or have rational theory for efficacy in alleviating drinking in AUD individuals. These include the following medications along with their cllinicaltrials.gov number: PF-5190457 (ghrelin receptor inverse agonist) (NCT02707055), N-acetylcysteine (NAC) (precursor to glutathione) (NCT02966873), guanfacine (α2A adrenoceptor agonist) (NCT02164422 and NCT03137082), minocycline (inhibitor of 5-lipoxygenase) (NCT02187211), citicoline (biosynthesis of phosphatidylcholine) (NCT02582905), dutasteride (5α-reductase inhibitor) (NCT01758523), pregabalin (inhibitor of voltage-gated calcium channel) (NCT02884908), and kudzu extract (mechanism unknown) (NCT03099590).
2 Final Remarks
From this review, it is clear that advances are being made in developing medications to treat AUD, and researchers are exploring numerous targets involved in alcohol-seeking and drinking behavior. Although progress has been made, the challenge over the next decade will be to develop medications that are more effective than the current ones and without serious side effects. To accomplish this, NIAAA has identified two long-range goals to increase the effectiveness of alcohol treatment medications (Litten et al. 2016b): (1) advancing precision medicine and (2) discovering more effective targets.
Advancing precision medicine (or personalized medicine) is an essential step in identifying and targeting specific phenotypes that are most likely to respond favorably to a given medication. Although precision medicine is in its early stages, progress already is being made, especially in pharmacogenetics (Garbutt et al. 2014; Jones et al. 2015; Sun et al. 2016; see topiramate and ondansetron sections above). Still, given the complexities of AUD, it is doubtful that one factor, such as a person’s genetic makeup, will be sufficient to predict a positive outcome for that individual (Litten et al. 2015). Most likely, multiple factors will need to be considered to successfully “match” an individual to a specific medication. Such factors include biomarker signatures from the various “-omics,” including epigenomics, transcriptomics, proteomics, and metabolomics (Litten et al. 2016b). Other factors include biomarkers from brain imaging and electrophysiological variations, as well as patients’ characteristics, such as demographics, drinking patterns, family history, AUD severity, and psychiatric/medical comorbidity. Using this “treatment fingerprint,” an algorithm then could be established to describe a specific set of rules for matching individuals with medications. NIH’s new groundbreaking initiative, the “All of Us Program” (formerly known as the Precision Medicine Initiative) (https://allofus.nih.gov), offers a tremendous resource for this. The program is drawing together data on more than 1 million individuals. It will be useful not only for identifying different phenotypes and genotypes but also will enable scientists to test new information and computational approaches for deciphering the heterogeneity of complex diseases like AUD.
A second long-range goal in discovering medications is to identify targets in the brain that will be effective across the multiple phenotypes of AUD. During the past two decades, scientists have focused their research on targets that affect craving and the urge/desire to drink. So far, these efforts have produced alcohol treatment medications that have only small effect sizes (Zindel and Kranzler 2014). As we begin to better understand the mechanisms underlying brain function, this undoubtedly will lead to new druggable targets. To help accomplish this goal, NIH has initiated several major programs, including the “Brain Research through Advancing Innovative Neurotechnologies (BRAIN) initiative.” Supporting research on innovative technologies will enable us to examine how individual brain cells and neural circuits interact to produce specific behaviors, such as AUD, which can disrupt normal function (https://www.braininitiative.nih.gov/).
Another potential target involves the enzymes implicated in alcohol metabolism. We know that a genetic variant of the alcohol dehydrogenase gene (ADH1B*2) results in a more rapid alcohol metabolism, elevating acetaldehyde levels in the body (Hurley and Edenberg 2012). Because of the toxic and aversive actions of acetaldehyde, people with this genetic variant, which is common in Asian populations, are less likely to drink heavily and to become dependent on alcohol (Hurley and Edenberg 2012). Disulfiram, the first medication approved by the FDA for use in AUD, uses a similar mechanism of action, increasing acetaldehyde levels and making it uncomfortable to drink alcohol. However, disulfiram often is not effective because patient adherence tends to be low, probably because this medication does not reduce alcohol craving (Johnson 2008). One strategy is to develop a compound that interferes with the alcohol metabolism, producing the desired aversive effect while, at the same time, reducing craving for alcohol (Diamond and Yao 2015). Another strategy is to produce a long-lasting compound that is active for weeks or perhaps months, eliminating the need to take daily dosages.
And finally, developing a rational, systematic way to identify druggable targets will be vital in the hunt for new medications. Currently, more than 30 targets have been identified that appear to influence alcohol-seeking and drinking behavior (Litten et al. 2016b). To better understand these targets, we need to know their role in causing and/or maintaining problematic drinking, whether they are related or independent of each other, and how they fit within the different domains of AUD (e.g., incentive salience/reward, negative affect/emotionality, and cognitive function) to produce the wide variety of responses to alcohol that we see across the population. It is particularly important to identify how these targets interrelate with molecular pathways and other brain circuits. One approach is to develop, integrate, and data mine biomolecular and cellular networks to discover druggable targets (Hopkins 2008; Masoudi-Nejad et al. 2013; Yildirim et al. 2007). Those networks are highly complex and include gene-gene, gene-protein, and protein-protein interactions, metabolic differences, and variations in gene expression and regulatory networks (Gebicke-Haerter 2016; Robinson and Nielsen 2016; Tang et al. 2013). Researchers examining other complex disorders are using this approach, including cancer, endocrine disorders, Huntington’s disease, mood disorders, and schizophrenia (Collier et al. 2016; Morrow et al. 2010; Pirhaji et al. 2016; Yildirim et al. 2007). Many believe complex diseases like AUD cannot be effectively treated with one target–one medication; instead, successful treatment depends on multiple targets and combinations of medications. To date, there is a paucity of clinical studies where combined pharmacotherapies have been tested in AUD (Lee and Leggio 2014). To facilitate this line of research in the alcohol field, NIAAA recently issued a guide, Development, Integration, and Data Mining of Biomolecular and Cellular Networks for Discovering Druggable Targets for Alcohol Use Disorder and Alcohol-Induced Organ Damage (https://grants.nih.gov/grants/guide/notice-files/NOT-AA-17-007.html).
Ultimately, the success of our medications development program rests on our ability to get people into treatment. In any given year, less than 10% of individuals with AUD are offered or seek treatment (Grant et al. 2015). This meager rate would not be acceptable if these individuals were affected by cancer or another chronic medical condition. AUD is a chronic brain disorder. All patients suffering from AUD need to receive adequate treatment. By providing addiction-oriented education and training during medical school, clinical training, and beyond, we can help physicians better understand the pharmacotherapy options available to them, making AUD medications a routine part of standard practice.
In summary, the goals outlined above will be challenging but certainly are attainable. The NIAAA, the alcohol research community, the pharmaceutical industry, the clinicians, and the patients themselves all have a role in identifying, developing, and implementing the next generation of medications. By developing more effective medications, with few side effects, and identifying the patients who will benefit the most from these treatments, we can provide clinicians with the tools they need to treat this devastating disorder, providing relief for patients and their families, and markedly improving public health and safety.
References
Abou-Khalil B (2008) Levetiracetam in the treatment of epilepsy. Neuropsychiat Dis Treat 4:507–523
Addolorato G, Caputo F, Capristo E, Domenicali M, Bernardi M, Janiri L, Agabio R, Colombo G, Gessa GL, Gasbarrini G (2002) Baclofen efficacy in reducing alcohol craving and intake: a preliminary double-blind randomized controlled study. Alcohol Alcohol 37:504–508
Addolorato G, Leggio L, Ferrulli A, Cardone S, Vonghia L, Mirijello A, Abenavoli L, D’Angelo C, Caputo F, Zambon A, Haber PS, Gasbarrini G (2007) Effectiveness and safety of baclofen for maintenance of alcohol abstinence in alcohol-dependent patients with liver cirrhosis: randomised, double-blind controlled study. Lancet 370:1915–1922
Ameisen O (2005) Complete and prolonged suppression of symptoms and consequences of alcohol-dependence using high-dose baclofen: a self-case report of a physician. Alcohol Alcohol 40:147–150
Anthenelli RM, Heffner JL, Wong E, Tibbs J, Russell K, Isgro M, Dinh E, Wehrle C, Worley MJ, Doran N (2017) A randomized trial evaluating whether topiramate aids smoking cessation and prevents alcohol relapse in recovering alcohol-dependent men. Alcohol Clin Exp Res 41:197–206
Anton RF, Pettinati H, Zweben A, Kranzler HR, Johnson B, Bohn MJ, McCaul ME, Anthenelli R, Salloum I, Galloway G, Garbutt J, Swift R, Gastfriend D, Kallio A, Karhuvaara S (2004) A multi-site dose ranging study of nalmefene in the treatment of alcohol dependence. J Clin Psychopharmacol 24(4):421–428
Anton RF, Kranzler H, Breder C, Marcus RN, Carson WH, Han J (2008) A randomized, multicenter, double-blind, placebo-controlled study of the efficacy and safety of aripiprazole for the treatment of alcohol dependence. J Clin Psychopharmacol 28:5–12
Anton RF, Myrick H, Baros AM, Latham PK, Randall PK, Wright TM, Stewart SH, Waid R, Malcolm R (2009) Efficacy of a combination of flumazenil and gabapentin in the treatment of alcohol dependence: relationship to alcohol withdrawal symptoms. J Clin Psychopharmacol 29:334–342
Anton RF, Myrick H, Wright TM, Latham PK, Am B, Waid LR, Randall PK (2011) Gabapentin combined with naltrexone for the treatment of alcohol dependence. Am J Psychiatry 168:709–717
Anton RF, Schacht JP, Voronin KE, Randall PK (2017) Aripiprazole suppression of drinking in a clinical laboratory paradigm: influence of impulsivity and self-control. Alcohol Clin Exp Res 41(7):1370–1380
Arias A, Feinn R, Oncken C, Covault J, Kranzler HR (2010) Placebo-controlled trial of zonisamide for the treatment of alcohol dependence. J Clin Psychopharmacol 30:318–322
Arnone D (2005) Review of the use of topiramate for treatment of psychiatric disorders. Ann Gen Psychiatry 4:5
Aziz AMA, Brothers S, Sartor G, Holm L, Heilig M, Wahlestedt C, Thorsell A (2016) The nociception/orphanin FQ receptor agonist SR-8993 as a candidate therapeutic for alcohol use disorders: validation in rat models. Psychopharmacology (Berl) 233(19–20):3553–3563
Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, Rounsaville B (1992) Types of alcoholics, I: evidence for an empirically derived typology based on indicators of vulnerability and severity. Arch Gen Psychiatry 49:599–608
de Bejczy A, Lof E, Walther L, Gutertstam J, Hammarbeg A, Ansanovska G, Franck J, Isaksson A, Soderpalm B (2015) Varenicline for treatment of alcohol dependence: a randomized, placebo-controlled trial. Alcohol Clin Exp Res 39:2189–2199
Bell RL, Lopez MF, Cui C, Egli M, Johnson KW, Franklin KM, Becker HC (2013) Ibudilast reduces alcohol drinking in multiple animal models of alcohol dependence. Addict Biol 20:38–42
Beraha EM, Salemink E, Goudriaan AE, Bakker A, de Jong D, Smits N, Zwart JW, van Geest D, Bodewits P, Schiphof T, Defourny H, van Tricht M, van den Brink W, Rw W (2016) Efficacy and safety of high-dose baclofen for the treatment of alcohol dependence: a multicenter, randomized, double-blind controlled trial. Eur Neuorpsychopharmacol 26:1950–1959
Blodgett JC, Del Re AC, Maisel NC, Finney JW (2014) A meta-analysis of topiramate’s effects for individuals with alcohol use disorders. Alcohol Clin Exp Res 38:1481–1488
Boels D, Victorri-Vigneau C, Grall-Bronnec M, Toure A, Garnier A, Turcant A, Le Roux G (2017) Baclofen and alcohol-dependent patients: a real risk of severe self-poisoning. Basic Clin Pharmacol Toxicol 121(4):353–359
van den Brink W, Aubin HJ, Bladstrom A, Torup L, Gual A, Mann K (2013) Efficacy of as-needed nalmefene in alcohol-dependent patients with at least a high drinking risk level: results from a subgroup analysis of two randomized controlled 6-month studies. Alcohol Alcohol 48:570–578
van den Brink W, Sorensen P, Torup L, Mann K, Gual A (2014) Long-term efficacy, tolerability and safety of nalmefene as-needed in patients with alcohol dependence: a 1-year, randomized controlled study. J Psychopharmacol 28:733–744
Brower KJ, Myra Kim H, Strobbe S, Karam-Hage MA, Consens F, Zucker RA (2008) A randomized double-blind pilot trial of gabapentin versus placebo to treat alcohol dependence and comorbid insomnia. Alcohol Clin Exp Res 32(8):1429–1438
Brown ES, Davila D, Nakamura A, Carmody TJ, Rush AJ, Lo A, Holmes T, Adinoff B, Caetano R, Swann AC, Sunderajan P, Bret ME (2014) A randomized, double-blind, placebo-controlled trial of quetiapine in patients with bipolar disorder, mixed or depressed phase, and alcohol dependence. Alcohol Clin Exp Res 38:2113–2118
Bucknam W (2007) Suppression of symptoms of alcohol dependence and craving using high-dose baclofen. Alcohol Alcohol 42:158–160
Ciccocioppo R, Economidou D, Fedeli A, Angeletti S, Weiss F, Heilig M, Massi M (2004) Attenuation of ethanol self-administration and of conditioned reinstatement of alcohol-seeking behaviour by the antiopioid peptide nociception/orphanin FZ in alcohol-preferring. Psychopharmacology 172:170–178
Collier DA, Bj E, Malki K, Mokrab Y (2016) Advances in the genetics of schizophrenia: toward a network and pathway view for drug discovery. Ann N Y Acad Sci 1366:61–75
De Smedt T, Raedt R, Vonck K, Boon P (2007) Levetiracetam: the profile of a novel anticonvulsant drug-part I: preclinical data. CNS Drug Rev 13:43–56
Del Re AC, Gordon AJ, Lembke A, Harris AHS (2013) Prescription of topiramate to treat alcohol use disorders in the Veterans Health Administration. Addict Sci Clin Pract 8:12
Diamond I, Yao L (2015) From ancient Chinese medicine to a novel approach to treat cocaine addiction. CNS Neurol Disord Drug Targets 14:716–726
Drobes DJ, Anton RF, Thomas SE, Voronin K (2004) Effects of naltrexone and nalmefene on subjective response to alcohol among non-treatment-seeking alcoholics and social drinkers. Alcohol Clin Exp Res 28:1362–1370
Economidou D, Hansson AC, Weiss F, Terasmaa A, Sommer WH, Cippitelli A, Fedeli A, Martin-Fardon R, Massi M, Ciccocioppo R, Heilig M (2008) Dysregulation of nociception/orphanin FZ activity in the amygdala is linked to excessive alcohol drinking in the rat. Biol Psychiatry 64:211–218
Economidou D, Cippitelli A, Stopponi S, Braconi S, Clementi S, Ubaldi M, Martin-Fardon R, Weiss F, Massi M, Ciccocioppo R (2011) Activation of brain NOP receptors attenuates acute and protracted alcohol withdrawal symptoms in the rat. Alcohol Clin Exp Res 35:747–755
Edwards S, Guerrero M, Ghoneim OM, Roberts E, Koob GF (2011) Evidence that vasopressin V1b receptors mediate the transition to excessive drinking in ethanol-dependent rats. Addict Biol 17:76–85
Evans SM, Bisaga A (2009) Acute interaction of baclofen in combination with alcohol in heavy social drinkers. Alcohol Clin Exp Res 33:19–30
Falk DE, Castle IJP, Ryan M, Fertig J, Litten RZ (2015) Moderators of varenicline treatment effects in a double-blind, placebo-controlled trial for alcohol dependence: an exploratory analysis. J Addict Med 9:296–303
Farokhnia M, Schwandt ML, Lee MR, Bollinger JW, Farinelli LA, Amodio JP, Sewell L, Lionetti TA, Spero DE, Leggio L (2017) Biobehavioral effects of baclofen in anxious alcohol-dependent individuals: a randomized, double-blind, placebo-controlled, laboratory study. Transl Psychiatry 7(4):e1108
Fertig JB, Ryan ML, Falk DE, Litten RZ, Mattson ME, Ransom J, Rickman WJ, Scott C, Ciraulo D, Green AI, Tiouririne NA, Johnson B, Pettinati H, Strain EC, Devine E, Brunette MF, Kampman K, Tompkins DA, Stout R (2012) A double-blind, placebo-controlled trial assessing the efficacy of levetiracetam extended-release in very heavy drinking alcohol-dependent patients. Alcohol Clin Exp Res 6(8):1421–1430
Fleischhacker WW (2005) Aripiprazole. Expert Opin Pharmacolther 6:2091–2101
Fox HC, Anderson GM, Tuit K, Hansen J, Kimmerling A, Siedlarz KM, Morgan PT, Sinha R (2011) Prozosin effects on stress-and cue-induced craving and stress response in alcohol-dependent individuals: preliminary findings. Alcohol Clin Exp Res 36:351–360
Fucito LM, Toll BA, Wu R, Romano DM, Tek E, O’Malley SS (2011) A preliminary investigation of varenicline for heavy drinking smokers. Psychopharmacology (Berl) 215:655–663
Furieri FA, Nakamura-Palacios EM (2007) Gabapentin reduces alcohol consumption and craving: a randomized, double-blind, placebo-controlled trial. J Clin Psychiatry 68(11):1691–1700
Garbutt JC, Kampov-Polevoy AB, Gallop R, Kalka-Juhl L, Flannery BA (2010) Efficacy and safety of baclofen for alcohol dependence: a randomized, double-blind, placebo-controlled trial. Alcohol Clin Exp Res 34(11):1849–1857
Garbutt JC, Greenblatt AM, West SL, Morgan LC, Kampov-Polevoy A, Jordan HS, Bobashev GV (2014) Clinical and biological moderators of response to naltrexone in alcohol dependence: a systematic review of the evidence. Addiction 109:1274–1284
Gebicke-Haerter PJ (2016) Systems psychopharmacology: a network approach to developing novel therapies. World J Psychiatr 6:66–83
Gomer B, Wagner K, Frings L, Saar J, Carius A, Harle M, Steinhjoff BJ, Schulze-Bonhage A (2007) The influence of antiepileptic drugs on cognition: a comparison of levetiracetam with topiramate. Epilepsy Behav 10:486–494
Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, Pickering RP, Ruan WJ, Smith SM, Huang B, Hasin DS (2015) Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiat 72(8):757–766
Green B (2014) Prazosin in the treatment of PTSD. J Psychiatr Pract 20:253–259
Gual A, He Y, Torup L, van den Brink W, Mann K (2013) A randomised, double-blind, placebo-controlled, efficacy study of nalmefene, as-needed use, in patients with alcohol dependence. Eur Neuropsychopharmacol 23(11):1432–1442
Haass-Koffler CL, Goodyear K, Zywiak WH, Magill M, Eltinge SE, Wallace PM, Long VM, Jayaram-Lindstrom N, Swift RM, Kenna GA, Leggio L (2017) Higher pressure in associated with greater alcohol drinking reduction in alcohol-dependent individuals treated with doxazosin. Drug Alcohol Depend 177:23–28
Hofmann SG, Huweler R, MacKillop JM, Kantak K (2012) Effects of D-cycloserine on craving to alcohol cues in problem drinkers: preliminary findings. Am J Drug Alcohol Abuse 38:101–107
Hopkins AL (2008) Network pharmacology: the next paradigm in drug discovery. Nat Chem Biol 4:682–690
Hurley TD, Edenberg HJ (2012) Genes encoding enzymes involved in ethanol metabolism. Alcohol Res Curr Rev 34:339–344
Johnson BA (2008) Update on neuropharmacological treatments for alcoholism: scientific basis and clinical findings. Biochem Pharmacol 75:34–56
Johnson BA, Campling GM, Griffiths P, Cowen PJ (1993) Attention of some alcohol-induced mood changes and the desire to drink by 5-HT3 receptor blockade: a preliminary study I healthy male volunteers. Psychopharmacology (Berl) 112:142–144
Johnson BA, Roache JD, Javors MA, DiClemente CC, Cloninger CR, Prihoda TJ, Bordnick PS, Ait-Daoud N, Hensler J (2000) Ondansetron for reduction of drinking among biologically predisposed alcoholic patients: a randomized controlled trial. JAMA 284(8):963–971
Johnson BA, Ait-Daoud N, Bowden CL, DiClemente CC, Roache JD, Lawson K, Javors MA, Ma JZ (2003) Oral topiramate for treatment of alcohol dependence: a randomised controlled trial. Lancet 361:1677–1685
Johnson BA, Rosenthal N, Capece JA, Wiegund F, Mao L, Beyers K, McKay A, Ait-Daoud N, Anton RF, Ciraulo DA, Kranzler HR, Mann K, O’Malley SS, Swift RM (2007) Topiramate for treating alcohol dependence: a randomized controlled trial. JAMA 198(14):1641–1651
Johnson BA, Ait-Daoud N, Seneviratne C, Roach JD, Javors MA, Wang XQ, Liu L, Penberthy JK, DiClemente CC, Li MD (2011) Pharmacogenetic approach at the serotonin transporter gene as a method of reducing the severity of alcohol drinking. Am J Psychiatry 168:265–275
Johnson BA, Seneviratne C, Wang XQ, Ait-Daoud LMD (2013) Determination of genotype combinations that can predict the outcome of the treatment of alcohol dependence using the 5-HT3 antagonist ondansetron. Am J Psychiatry 170:1020–1031
Jones JD, Comer SD, Kranzler HR (2015) The pharmacogenetics of alcohol use disorder. Alcohol Clin Exp Res 39:391–402
Kampman KM, Pettinati HM, Lynch KG, Whittingham T, Macfadden W, Dackis C, Tirado C, Oslin DW, Sparkman T, O’Brien CP (2007) A double-blind, placebo-controlled pilot trial of quetiapine for the treatment of type A and type B alcoholism. J Clin Psychopharmacol 27(4):344–351
Kelley AE (2004) Memory and addiction: shared neural circuitry and molecular mechanisms. Neuron 44:161–179
Kenna GA, Zywiak WH, McGeary JE, Leggio L, McGeary C, Wang S, Grenga A, Swift RM (2009) A within-group design of nontreatment seeking 5-HTTLPR genotyped alcohol-dependent subjects receiving ondansetron and sertraline. Alcohol Clin Exp Res 33:315–323
Kenna GA, Zywiak WH, Swiftt RM, McGeary JE, Cliifford JS, Shoaff JR, Vuittonet C, Fricchione S, Brickley M, Beaucage K, Haass-Koffler CL, Leggio L (2014a) Ondansetron reduces naturalistic drinking in nontreatment-seeking alcohol-dependent individuals with the LL 5/-HTTLPR genotype: a laboratory study. Alcohol Clin Exp Res 38:1567–1574
Kenna GA, Zwiak WH, Swift RM, McGeary JE, Clifford JS, Shoaff JR, Fricchione S, Brickley M, Beaucage K, Haass-Koffler CL, Leggio L (2014b) Ondansetron and sertraline may interact with 5-HTTLPR and DRD4 polymorphisms to reduce drinking in non-treatment seeking alcohol-dependent women: exploratory findings. Alcohol 48:515–522
Kenna GA, Haass-Koffler CL, Zywiak WH, Edwards SM, Brickley MB, Swift RM, Leggio L (2015) Role of the α1 blocker doxazosin in alcoholism: a proof-of-concept randomized controlled trial. Addict Biol 21:904–914
Kiefer F, Kirsch M, Bach P, Hoffmann S, Reinhard I, Jorde A, von der Goltz C, Spanagel R, Mann K, Loeber S, Vollstadt-Klein S (2015) Effects of D-cycloserine on extinction of mesolimbic cue reactivity in alcoholism: a randomized placebo-controlled trial. Psychopharmacology (Berl) 232(13):2353–2362
King CE, Griffin WC, Luderman LN, Kates MM, McGinty JF, Becker HC (2017) Oxytocin reduces ethanol self-administration in mice. Alcohol Clin Exp Res 41:955–964
Knapp CM, Sarid-Segal O, Richardson MA, Sickles Colaneri L, Afshar M, Devine E, Streeter CC, Piechniczek-Buczek J, Ciraulo DA (2010) Open label trial of the tolerability and efficacy of zonisamide in the treatment of alcohol dependence. Am J Drug Alcohol Abuse 36:102–105
Knapp CM, Ciraulo DA, Sarid-Segal O, Richardson MA, Devine E, Streeter CC, Oscar-Berman M, Surprise C, Colaneri L, Putnam M, Waters M, Richambault C (2015) Zonisamide, topiramate, and levetiracetam: efficacy and neuropsychological effects in alcohol use disorders. J Clin Psychopharmacol 35:1–9
Kothare S, Kaleyias J (2008) Zonisamide: review of pharmacology, clinical efficacy, tolerability, and safety. Expert Opin Drug Metab Toxicol 4:493–506
Kranzler HR, Piernucci-Lagha A, Feinn R, Hernandez-Avila C (2003) Effects of ondansetron in early-versus late-onset alcoholics: a prospective, open-label study. Alcohol Clin Exp Res 27:1150–1155
Kranzler HR, Covault J, Pierucci-Lagha A, Chan G, Douglas K, Arias AJ, Oncken C (2008) Effects of aripiprazole on subjective and physiological responses to alcohol. Alcohol Clin Exp Res 32:1–7
Kranzler HR, Covault J, Feinn R, Armeli S, Tennen H, Arias AJ, Gelernter J, Pond T, Oncken C, Kampman KM (2014) Topiramate treatment for heavy drinkers: moderation by a GRIK1 polymorphism. Am J Psychiatry 171:445–452
Ledeboer A, Hutchinson MR, Watkins LR, Johnson KW (2007) Ibudilast (AV-411): a new class therapeutic candidate for neuropathic pain and opioid withdrawal syndromes. Expert Opin Investig Drugs 16:935–950
Lee MR, Leggio L (2014) Combined pharmacotherapies for the management of alcoholism rationale and evidence to date. CNS Drugs 28:107–119
Lee MR, Weerts EM (2016) Oxytocin for the treatment of drug and alcohol use disorders. Behav Pharmacol 27:640–648
Lee MR, Rohn MCH, Tanda G, Leggio L (2016) Targeting the oxytocin system to treat addictive disorders: rationale and progress to date. CNS Drugs 30:109–123
Leggio L, Kenna GA (2013) Commentary: doxazosin for alcoholism. Alcohol Clin Exp Res 37:191–193
Leggio L, Garbutt JC, Addolorato G (2010) Effectiveness and safety of baclofen in the treatment of alcohol dependent patients. CNS Neurol Disor 9:33–44
Leggio L, Zywiak WH, McGeary JE, Edwards S, Fricchione SR, Shoaff JR, Addolorato G, Swift RM, Kenna GA (2013) A human laboratory pilot study with baclofen in alcoholic individuals. Pharmacol Biochem Behav 103:784–791
Leggio L, Zywiak WH, Edwards SM, Tidey JW, Swift RM, Kenna G (2015) A preliminary double-blind, placebo-controlled randomized study of baclofen effects in alcoholic smokers. Psychopharmacology (Berl) 232:233–243
Litten RZ (2016) Nociceptin receptor as a target to treat alcohol use disorder: challenges in advancing medications development. Alcohol Clin Exp Res 40:2299–2304
Litten RZ, Fertig JB, Falk DE, Ryan ML, Mattson ME, Collins JF, Murtaugh C, Ciraulo D, Green AI, Johnson BA, Pettinati H, Swift R, Afshar M, Brunette MF, Tiouririne NAD, Kampman K, Stout R (2012) Study Group. A double-blind, placebo-controlled trial to assess the efficacy of quetiapine fumarate XR in very heavy-drinking alcohol-dependent patients. Alcohol Clin Exp Res 36(3):406–416
Litten RZ, Ryan ML, Fertig JB, Falk DE, Johnson B, Dunn KE, Green AI, Pettinati HM, Ciraulo DA, Sarid-Segal O, Kampman K, Brunette MF, Strain EC, Tiouririne NA, Ransom J, Scott C, Stout R (2013) A double-blind, placebo-controlled trial assessing the efficacy of varenicline tartrate for alcohol dependence. J Addict Med 7:277–286
Litten RZ, Ryan ML, Falk DE, Reilly M, Fertig JB, Koob GF (2015) Heterogeneity of alcohol use disorder: understanding mechanisms to advance personalized treatment. Alcohol Clin Exp Res 39:579–584
Litten RZ, Wilford BB, Falk DE, Ryan ML, Fertig JB (2016a) Potential medications for the treatment of alcohol use disorder: an evaluation of clinical efficacy and safety. Subs Abuse 37:286–298
Litten RZ, Falk DE, Ryan ML, Fertig JB (2016b) Discovery, development, and adoption of medications to treat alcohol use disorder: goals for the phases of medications development. Alcohol Clin Exp Res 40:1368–1379
MacKillop J, Few LR, Stojek MK, Murphy CM, Malutinok SF, Johnson FT, Hofmann SG, McGeary JE, Swift RM, Monti PM (2015) Transl Psychiatry 5(4):e544
Mann K, Bladstrom A, Torup L, Gual A, van den Brink W (2013) Extending the treatment options in alcohol dependence: a randomized controlled study of as-needed nalmefene. Biol Psychiatry 73:706–713
Mann K, Torup L, Sorensen P, Gual A, Swift R, Walker B, van den Brink W (2016) Nalmefene for the management of alcohol dependence: review on its pharmacology, mechanism of action and meta-analysis on its clinical efficacy. Eur Neuoropsychopharmacol 26(12):1941–1949
Mariani JJ, Levin FR (2008) Levetiracetam for the treatment of co-occurring alcohol dependence and anxiety: case series and review. Am J Drug Alcohol Abuse 34:683–691
Martinotti G, Andreoli S, Di Nicola M, Di Giannantonio M, Sarchiapone M, Janiri L (2008) Quetiapine decreases alcohol consumption, craving, and psychiatric symptoms in dually diagnosed alcoholics. Psychopharmacol Clin Exp 23:417–424
Martinotti G, Di Nicola M, Di Giannantonio M, Janiri L (2009) Aripiprazole in the treatment of patients with alcohol dependence: a double-blind, comparison trial vs naltrexone. J Psychopharmacol 23:123–129
Martinotti G, DiNicola M, De Vita O, Hatzigiakoumis DS, Guglielmo R, Santucci B, Aliotta F, Romanelli R, Verrastro V, Petruccelli F, Di Giannantonio M, Janiri L (2014) Low-dose topiramate in alcohol dependence: a single-blind, placebo-controlled study. J Clin Psychopharmacol 34:709–715
Mason BJ, Salvato FR, Williams LD, Ritvo EC, Cutler RB (1999) A double-blind, placebo-controlled study of oral nalmefene for alcohol dependence. Arch Gen Psychiatry 56(8):719–724
Mason BJ, Light JM, Williams LD, Drobes DJ (2009) Proof-of-concept human laboratory study for protracted abstinence in alcohol dependence: effects of gabapentin. Addict Biol 14(1):73–83
Mason BJ, Quello S, Goodell V, Shadan F, Kyle M, Begovic A (2014) Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med 174:70
Masoudi-Nejad A, Mousavian Z, Bozorgmehr JH (2013) Drug-target and disease networks: polypharmacology in the post-genomic era. Silico Pharmacol 1:17
McKee SA, Harrison ELR, O’Malley SS, Krishnan-Sarin S, Shi J, Tetrault JM, Picciotto MR, Petrakis IL, Estevez N, Balchunas E (2009) Varenicline reduces alcohol self-administration in heavy-drinking smokers. Biol Psychiatry 66:185–195
Mihalak KB, Carroll FI, Luetje CW (2006) Varenicline is a partial agonist at α4β2 and a full agonist at α7 neuronal nicotinic receptors. Mol Pharmacol 70:801–805
Milivojevic V, Sinha R (2017) Targeting stress pathophysiology to improve alcoholism relapse outcomes. Neuropsychopharmacology 42:987–988
Miranda R, MacKillop J, Monti PM, Rohsenow DJ, Tidey J, Gwaltney C, Swift R, Ray L, McGeary J (2008) Effects of topiramate on urge to drink and the subjective effects of alcohol: a preliminary laboratory study. Alcohol Clin Exp Res 32:489–497
Miranda R, MacKillop J, Treloar H, Blanchard A, Tidey JW, Swift R, Chun T, Rohsenow DJ, Monti PM (2016) Biobehavioral mechanisms of topiramate’s effects on alcohol use: an investigation pairing laboratory and ecological momentary assessments. Addict Biol 21:171–182
Mitchell JM, Grossman LE, Coker AR, Messing RO (2012a) The anticonvulsant levetiracetam potentiates alcohol consumption in non-treatment seeking alcohol abusers. J Clin Psychopharmacol 32:269–272
Mitchell JM, Teague CH, Kayser AS, Bartlett SE, Fields HL (2012b) Varenicline decreases alcohol consumption in heavy-drinking smokers. Psychopharmacology (Berl) 223:299–306
Mitchell JM, Arcuni PA, Weinstein D, Woolley JD (2016) Intranasal oxytocin selectively modulates social perception, craving, and approach behavior in subjects with alcohol use disorder. J Addict Med 10:182–189
Moallem N, Ray LA (2012) Quetiapine improves response inhibition in alcohol dependent patients: a placebo-controlled pilot study. Pharmacol Biochem Behav 100:490–493
Monnelly EP, Ciraulo DA, Knapp C, LoCastro J, Sepulveda I (2004) Quetiapine for treatment of alcohol dependence. J Clin Psychopharmacol 24:532–535
Morley KC, Baillie A, Leung S, Addolorato G, Leggio L Haber PS (2014) Baclofen for the treatment of alcohol dependence and possible role of comorbid anxiety. Alcohol Alcohol 49:654–660
Morrow JK, Tian L, Zhang S (2010) Molecular networks in drug discovery. Crit Rev Biomed Eng 38:143–156
Muller CA, Geisel O, Petz P, Higl V, Kruger J, Stickel A, Beck A, Wernecke KD, Hellweg R, Heinz A (2015) High-dose baclofen for the treatment of alcohol dependence (BACLAD study): a randomized, placebo-controlled trial. Europ Neuropsychopharm 25:1167–1177
Myrick H, Li X, Randall PK, Henderson S, Voronin K, Anton RF (2010) The effect of aripiprazole in cue-induced brain activation and drinking parameters in alcoholics. J Clin Psychopharmacol 30:365–372
Pedersen CA, Smedley KL, Leserman J, Jarskog LF, Rau SW, Kampov-Polevoi A, Casey RL, Fender T, Garbutt JC (2013) Intranasal oxytocin blocks alcohol withdrawal in human subjects. Alcohol Clin Exp Res 37:484–489
Peters ST, Bowen MT, Bohrer K, McGregor IS, Neumann ID (2016) Oxytocin inhibits ethanol consumption and ethanol-induced dopamine release in the nucleus accumbens. Addict Biol 22:702–711
Petrakis IL, Desai N, Gueorguieva R, Arias A, O’Brien E, Jane JS, Sevarino K, Southwick S, Ralevski E (2016) Prazosin for veterans with posttraumatic stress disorder and comorbid alcohol dependence: a clinical trial. Alcohol Clin Exp Res 40:178–186
Pirhaji L, Milani P, Leidl M, Curran T, Avila-Pacheco J, Clish CB, White FM, Saghatelian A, Fraenkel E (2016) Revealing disease-associated pathways by network integration of untargeted metabolomics. Nat Methods 13(9):770–776
Plebani JG, Lynch KG, Rennert L, Pettinati HM, O’Brien CP, Kampman KM (2013) Results from a pilot clinical trial of varenicline for the treatment of alcohol dependence. Drug Alcohol Depend 133(2):754–758
Post A, Smart TS, Krikke-Workel J, Dawson GR, Harmer CJ, Browning M, Jackson K, Kakar R, Mohs R, Statnick M, Wafford K, McCarthy A, Barth V, Witkin JM (2016a) A selective nociception receptor antagonist to treat depression: evidence from preclinical and clinical studies. Neurophsychopharmaclogy 41:1803–1812
Post A, Smart T, Jackson K, Wilson J, Mohs R, Rorick-Kehn L, Statnick M, Anton R, O’Malley S, Wong C (2016b) A proof-of-concept study to assess the nociception receptor antagonist LY2940094 as a new treatment for alcohol dependence. Alcohol Clin Exp Res 40:1935–1944
Project MATCH Research Group (1997) Matching alcoholism treatments to client heterogeneity: project MATCH posttreatment drinking outcomes. J Stud Alcohol 58:7–29
Raskind MA, Millard SP, Petie EC, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, Hill J, Daniels C, Hendrickson R, Er P (2016) Higher pretreatment blood pressure is associated with greater posttraumatic stress disorder symptom reduction in soldiers treated with prazosin. Biol Psychiatry 80(10):736–742
Ray LA, Miranda R, MacKillop J, McGeary J, Tidey JW, Rohsenow DJ, Gwaltney C, Swift RW, Monti PM (2009) A preliminary pharmacogenetic investigation of adverse events from topiramate in heavy drinkers. Exp Clin Psychopharmacol 17:122–129
Ray LA, Heydari A, Zorick T (2010) Quetiapine for the treatment of alcoholism: scientific rationale and review of the literature. Drug Alcohol Rev 29:568–575
Ray LA, Chin PF, Heyari A, Miotto K (2011) A human laboratory study of the effects of quetiapine on subjective intoxication and alcohol craving. Psychopharmacology (Berl) 317:341–351
Ray LA, Bujarski S, Shoptaw S, Roche DJO, Heinzerling K, Miotto K (2017) Development of the neuroimmune modulator ibudilast for the treatment of alcoholism: a randomized, placebo-controlled, human laboratory trial. Neuropsychopharmacology 42(9):1776–1788
Reynaud M, Aubin HJ, Trinquet F, Zakine B, Dano C, Dematteis M, Trojak B, Paille F, Detilleux M (2017) A randomized, placebo-controlled study of high-dose baclofen in alcohol-dependent patients – the ALPADIR study. Alcohol Alcohol 52(4):439–446
Richardson HN, Lee SY, O’Dell LE, Koob GF, Rivier CL (2008) Alcohol self-administration acutely stimulates the hypothalamic-pituitary-adrenal axis, but alcohol dependence leads to a dampened neuroendocrine state. Eur J Neurosci 28:1641–1653
Richter C, Effenberger S, Bschor T, Bonnet U, Haasen C, Preuss UW, Heinz A, Forg A, Volkmar K, Glauner T, Schaefer M (2012) Efficacy and safety of levetiracetam for the prevention of alcohol relapse in recently detoxified alcohol-dependent patients: a randomized trial. J Clin Psychopharmacol 32(4):558–562
Roberts W, Harrison ELR, McKee SA (2017a) Effects of varenicline on alcohol cue reactivity in heavy drinkers. Psychopharmacology. doi: https://doi.org/10.1007/s00213-017-4667-9. [Epub ahead of print]
Roberts W, Verplaetse TL, Moore K, Oberleitner L, Picciotto MR, McKee SA (2017b) Effects of varenicline on alcohol self-administration and craving in drinkers with depressive symptoms. J Psychopharmacol 31:906–914
Robinson JL, Nielsen J (2016) Integrative analysis of human omics data using biomolecular networks. Mol Biosyst 12(10):2953–2964
Rolland B, Labreuche J, Duhame A, Deheul S, Gautier S, Auffret M, Pignon B, Valin T, Bordet R, Cottencin O (2015) Baclofen for alcohol dependence: relationships between baclofen and alcohol dosing and the occurrence of major sedation. Eur Neuropsychopharmacol 25:1631–1636
Rorick-Kehn LM, Ciccocioppo R, Wong CJ, Witkin JM, Martinez-Grau MA, Stopponi S, Adams BL, Katner JS, Perry KW, Toledo MA, Diaz M, Lafuente C, Jimenez A, Benito A, Pedregal C, Weiss F, Statnick MA (2016) A novel, orally bioavailable nociception receptor antagonist, LY2940094, reduces ethanol self-administration and ethanol seeking in animal models. Alcohol Clin Exp Res 40:945–954
Rubio G, Lopez-Munoz F, Ferre F, Martinez-Gras I, Ponce G, Pascual JM, Jimenez-Arriero MA, Alamo C (2010) Effects of zonisamide in the treatment of alcohol dependence. Clin Neuropharmacol 33:250–253
Ryan ML, Falk DE, Fertig JB, Rendenbach-Mueller B, Katz DA, Tracy KA, Strain EC, Dunn KE, Kampman K, Mahoney E, Ciraulo DA, Sickles-Colaneri L, Ait-Daoud N, Johnson BA, Ransom J, Scott C, Koob GF, Litten RZ (2017) A phase2, double-blind, placebo-controlled randomized trial assessing the efficacy of ABT-436, a novel V1b receptor antagonist, for alcohol dependence. Neuropsychopharmacology 42:1012–1023
Sarid-Segal O, Piechniczek-Buczek J, Knapp C, Afshar M, Devine E, Sickles L, Uwodukunda E, Richambault C, Koplow J, Ciraulo D (2008) The effects of levetiracetam on alcohol consumption in alcohol-dependent subjects: an open label study. Am J Drug Alcohol Abuse 34:441–447
Sarid-Segal O, Cm K, Burch W, Richardson MA, Bahtia S, DeQuattro K, Afshar M, Richambault C, Sickels L, Devine E, Ciraulo D (2009) The anticonvulsant zonisamide reduces ethanol self-administration by risky drinkers. Am J Drug Alcohol Abuse 35:316–319
Sattar SP, Bhatia SC, Petty F (2004) Potential benefits of quetiapine in the treatment of substance dependence disorders. J Psychiatry Neurosci 29:452–4457
Schacht JP, Anton RF, Randall PK, Li X, Henderson S, Myrick H (2014) Varenicline effects on drinking, craving and neural reward processing among non-treatment-seeking alcohol-dependent individuals. Psychopharmacology (Berl) 231:3799–3807
Scholl J, Gunthner J, Kollling N, Favaron E, Rushworth FS, Cj H, Reinecke A (2014) Arole beyond leaning for NMDA receptors in reward-based decision-making-a pharmacological study using d-cycloserine. Neuropsychopharmacology 39(12):2900–2909
Seif T, Simms JA, Lei K, Wegner S, Bonci A, Messing RO, Hopf FW (2015) D-serine and D-cycloserine reduce compulsive alcohol intake in rats. Neuropyschopharmacology 40(10):2357–2367
Sellers EM, Toneatto T, Romach MK, Somer GR, Sobell LC, Sobell MB (1994) Clinical efficacy of the 5-HT3 antagonist ondansetron in alcohol abuse and dependence. Alcohol Clin Exp Res 18(4):879–885
Sills GJ (2006) The mechanisms of action of gabapentin and pregabalin. Curr Opin Pharmacol 6:108–113
Simms JA, Haass-Koffler CL, Bito-Onon J, Li R, Bartlett SE (2012) Mifepristone in the central nucleus of the amygdala reduces yohimbine stress-induced reinstatement of ethanol-seeking. Neuropsychopharmacology 37:906–918
Simpson TL, Saxon AJ, Meredith CW, Malte CA, McBride B, Ferguson LC Gross CA, Hart KL, Raskind M (2009) A pilot trial of the alpha-1 adrenergic antagonist, prazosin for alcohol dependence. Alcohol Clin Exp Res 33:255–263
Simpson TL, Malte CA, Dietel B, Tell D, Pocock I, Lyons R, Varon D, Raskind M, Saxon AJ (2015) A pilot trial of prazosin, an alpha-1 adrenergic antagonist, for comorbid alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res 39:808–817
Smith RV, Havens JR, Walsh SL (2016) Gabapentin misuse, abuse and diversion: a systematic review. Addiction 111:1160–1174
Stedman M, Pettinati HM, Brown ES, Kotz M, Calabrese JR, Raines S (2010) A double-blind, placebo-controlled study with quetiapine as adjunct therapy with lithium or divalproex in bipolar I patients with coexisting, alcohol dependence. Alcohol Clin Exp Res 34:1822–1831
Sun Y, Zhang Y, Wang F, Sun Y, Shi J, Lu L (2016) From genetic studies to precision medicine in alcohol dependence. Behav Pharmacol 27(2–3 Spec Issue):87–99
Swift RM, Davidson D, Whelihan W, Kuznetsov O (1996) Ondansetron alters human alcohol intoxication. Biol Psychiatry 40:514–521
Tang J, Karhinen L, Xu T, Szwajda A, Yadav B, Wennerberg K, Aittokallio T (2013) Target inhibition networks: predicting selective combinations of druggable targets to bl9ck cancer survivial pathways. PLoS Comput Biol (9):e1003226
Vatsalya V, Gowin JL, Schwandt ML, Momenan R, Coe MA, Hommer DW, Bartlett S, Heilig M, Ramchandani VA (2015) Effects of varenicline on neural correlates of alcohol salience in heavy drinkers. Int J Neuropsychopharmacol 18(12). pii: pyv068. doi: https://doi.org/10.1093/ijnp/pyv068
Vendruscolo LF, Barbier E, Schlosburg JE, Misra KK, Whitfield TW, Logrip ML, Rivier C, Repunte-Canonigo V, Zorrilla EP, Sanna PP, Heilig M, Koob GF (2012) Corticosteroid-dependent plasticity medicates compulsive alcohol drinking in rats. J Neurosci 32:7563–7571
Vendruscolo LF, Estey D, Goodell V, Macshane LG, Logrip ML, Schlosburg JE, McGinn MA, Zamora-Martinez ER, Belanoff JK, Hunt HJ, Sanna PP, George O, Koob GF, Edwards S, Mason BJ (2015) J Clin Invest 125:3193–3197
Voronin K, Randall P, Myrick H, Anton R (2008) Aripiprazole effects on alcohol consumption and subjective reports in a clinical laboratory paradigm–possible influence of self-control. Alcohol Clin Exp Res 32:1954–1961
Watson BJ, Wilson S, Griffin L, Kalk NJ, Taylor LG, Munafo MR, Lingford-Hughes AR, Nutt DJ (2011) A pilot study of the effectiveness of D-cycloserine during cue-exposure therapy in abstinent alcohol-dependent subjects. Psychopharmacology (Berl) 216:121–129
Wong CJ, Witcher J, Mallinckrodt C, Dean RA, Anton RF, Chen Y, Fijal BA, Ouyang H, Dharia S, Sundseth SS, Schuh KJ, Kinon BJ (2014) A phase 2, placebo-controlled study of the opioid receptor antagonist LY2196044 for the treatment of alcohol dependence. Alcohol Clin Exp Res 38:511–520
Yildirim MA, Goh KL, Cusick ME, Barabasi AL, Vidal M (2007) Drug-target network. Nat Biotechnol 25:1119–1126
Zhou Y, Colombo G, Carai MAM, Ho A, Gessa GL, Kreek MJ (2011) Involvement of arginine vasopressin and V1b receptor in alcohol drinking in Sardinian alcohol-preferring rats. Alcohol Clin Exp Res 35:1876–1883
Zindel LR, Kranzler HR (2014) Pharmacotherapy of alcohol use disorders: Seventy-five years of progress. J Stud Alcohol Drugs 75(Suppl)17):79–88
Acknowledgement
The authors thank Barbara Vann of CSR, Incorporated for her review, edits, and thoughtful comments.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Litten, R.Z., Falk, D.E., Ryan, M.L., Fertig, J., Leggio, L. (2017). Advances in Pharmacotherapy Development: Human Clinical Studies. In: Grant, K., Lovinger, D. (eds) The Neuropharmacology of Alcohol . Handbook of Experimental Pharmacology, vol 248. Springer, Cham. https://doi.org/10.1007/164_2017_79
Download citation
DOI: https://doi.org/10.1007/164_2017_79
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-96522-2
Online ISBN: 978-3-319-96523-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)