Abstract
An important challenge to facing the epidemic of cardiovascular disease is the unpredictable nature of acute coronary events. Therefore, substantial research has been recently conducted in order to develop new methods to identify subjects at risk or atheromatous plaque that are prone to produce sudden major coronary events. Over the past two decades, the concept of “vulnerable plaque” has gained attention as a paradigm to improve risk stratification and potentially lead to the discovery of novel markers of risk to prevent cardiovascular disease.
We reviewed biochemical markers that have been investigated to date for the identification of coronary atherosclerotic plaque composition and early detection of their vulnerability. C-reactive protein and matrix metalloproteinases are the most commonly studied, but also novel biomarkers reflecting a variety of pathophysiologic pathways such as ischemia, inflammation, vascular dysfunction, biomechanical stress, hemostasis, and lipid metabolism have been reported to be potentially associated with increased risk of coronary events.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- C-reactive protein
- Coronary plaque
- Matrix metalloproteinases
- Percutaneous coronary intervention
- Vulnerable plaque
Definitions
Acute coronary syndrome
Any condition brought on by sudden, reduced blood flow to the heart
Culprit lesion
The coronary lesion involved in the initial myocardial infarction
Nonculprit lesion
Any lesion in the entire coronary tree outside the culprit lesion
Thin-cap fibroatheromas
Lesions with a fibrous cap <65 μm with macrophage infiltration (>25 cells/high-magnification field) and an underlying necrotic core
Vulnerable plaque
A kind of atheromatous plaque that is particularly unstable and prone to produce sudden major coronary events
Introduction
Atherosclerosis is a chronic condition with acute cardiovascular manifestations. For many patients, the first sign of atherosclerosis is an acute myocardial infarction (MI), sudden cardiac death, or a disabling stroke. An important challenge to facing the epidemic of cardiovascular disease is the unpredictable nature of its acute manifestations. Therefore, substantial research has been recently conducted in order to develop new methods to identify subjects at risk before the occurrence of a cardiovascular event. Furthermore, among patients who have survived a cardiovascular event, the risk for a subsequent event remains relatively high, despite aggressive treatment (Cannon et al. 2004). Such recurrence rates highlight the need for novel approaches to secondary prevention of cardiovascular disease and to the treatment of index events.
Pathophysiology of Atherosclerotic Plaque
There has been considerable progress in the identification of the molecular and cellular processes causing atherosclerosis and its clinical sequelae (Daugherty et al. 2005; Libby et al. 2002). Low-density lipoprotein (LDL) cholesterol is central to the development of the disease. In addition, it is now clearly established that inflammation plays an important role in the initiation of lesions and is likely to be responsible for the activation of the disease in more than a single plaque or artery (Hansson et al. 2005; Libby 2005).
Chronic endothelial injury eventually results in endothelial dysfunction and increased permeability and induces LDL oxidation and accumulation in the subendothelial space of the intima as well as the expression of adhesion molecules and chemokines that participate in platelet aggregation and lymphocyte and monocyte adhesion and infiltration, thus initiating the inflammatory process (Daugherty et al. 2005; Libby et al. 2002; Hansson et al. 2005; Libby 2005). As monocytes are attracted to the endothelium and migrate to the subendothelial space, they mature into macrophages and uptake oxidized LDL transforming into “foam” cells that eventually form the lipid core of the atherosclerotic plaque after apoptosis occurs. This inflammatory mediator cascade promotes a phenotype change of vascular smooth muscle cells (VSMCs) from the “contractile” phenotype state to the active “synthetic” state. VSMCs in the synthetic state can migrate and proliferate from the media to the intima, where they produce excessive amounts of extracellular matrix (e.g., collagen, elastin, and proteoglycans) that transforms the lesion into a fibrous plaque (Daugherty et al. 2005; Libby et al. 2002; Hansson et al. 2005; Libby 2005). The typical atherosclerotic plaque comprises of the lipid core and the fibrous cap and is the most commonly classified histologically by the American Heart Association-recommended Stary classification (Stary 2000).
Vulnerable atherosclerotic plaques (high-risk or unstable plaques) are associated with an increased risk of disruption, distal embolization and vascular events. They are histological lesions with a large lipid core and a thin fibrous cap and may contain ulceration, intraluminal thrombosis, and intraplaque hemorrhage, as well as intense infiltration of macrophages and other inflammatory cells (Fig. 1).
Schematic figure illustrating the most common type of vulnerable plaque characterized by thin fibrous cap, extensive macrophage infiltration, paucity of smooth muscle cells, and large lipid core, without significant luminal narrowing (Reprinted with permission from Naghavi et al. 2003)
Over the past two decades, the concept of “vulnerable plaque” has gained attention as a paradigm to improve risk stratification and potentially lead to newer invasive and noninvasive therapeutic options to prevent and treat cardiovascular disease (Alsheikh-Ali et al. 2010).
The Vulnerable Plaque
The term vulnerable plaque was first used more than two decades ago in the context of studying triggers of acute cardiovascular disease (Muller et al. 1989). Since its introduction, the term vulnerable plaque has been used interchangeably in reference to the concept of propensity to result in an acute cardiovascular event or to denote a plaque with the histologic hallmarks of culprit lesions from autopsy studies. A more broad definition was proposed in 2003 to include not only susceptibility to rupture but also susceptibility to thrombose or rapidly progress to a culprit lesion (Fig. 2), based on observations that rupture of plaques, although common in culprit lesions, is not universal (Naghavi et al. 2003). Indeed, almost one third of such lesions exhibit erosion or nodular calcification without rupture of the fibrous cap (Virmani et al. 2000). The introduction of this concept paralleled an increase in appreciation of the limitations of imaging arterial lumens and quantifying risk based merely on the severity of arterial stenoses. In several prospective and retrospective serial angiographic studies, the culprit lesion in nearly two thirds of patients with acute coronary events was shown to have less than 70 % (often <50 %) diameter narrowing on coronary angiography weeks or months before the index event (Ambrose et al. 1986; Little et al. 1988; Hackett et al. 1988; Giroud et al. 1992). In retrospective autopsy studies, three histologic features were more commonly observed in plaques thought to be responsible for most acute coronary events compared with stable plaques: a larger lipid core (>40 % of total lesion area), a thinner fibrous cap (<65 μ), and more inflammatory cells (about 26 % macrophage infiltration of fibrous cap compared with 3 % in stable plaques) (Kolodgie et al. 2004; Virmani et al. 2006). The major criteria to define a vulnerable plaque included active inflammation; a thin cap (<100 μ) with a large lipid core (>40 % of the plaque’s total volume); endothelial denudation with superficial platelet aggregation; fissured cap, which may indicate a recent rupture; or severe stenosis, which would make the plaque more prone to shear stress or may be a marker of other less stenotic but vulnerable plaques (Naghavi et al. 2003). According to this proposal, the presence of at least one of these major criteria may indicate a higher risk for plaque complication. The minor criteria for plaque vulnerability included the presence of superficial calcified nodules; yellow color, which may indicate a larger lipid core; intraplaque hemorrhage; endothelial dysfunction (impaired endothelial vasodilator function); and expansive (positive) remodeling, which refers to compensatory outward enlargement of the vessel wall without luminal compromise (Naghavi et al. 2003). Notably, several investigators have noted the presence of more than one vulnerable plaque in patients at risk ofcardiovascular events (Libby et al. 2002; Libby 2005; Eriksson 2004; Arbab-Zadeh 2015) underlying the importance of going beyond a vulnerable plaque and called for evaluating the total arterial tree as a whole. In addition, evidence suggests that systemic factors may play a role in plaque instability, including the presence of a systemic inflammatory state (Naghavi et al. 2003). This provides the rationale to studying serum biomarkers that may identify patients with high-risk lesions (vulnerable blood), which, along with vulnerable myocardium, form the triad of vulnerability that defines the vulnerable patient (Naghavi et al. 2003). Indeed, there is no conclusive evidence that individual plaque assessment better predicts acute coronary event risk than established risk factors, such as the extent and severity of coronary artery disease (Arbab-Zadeh 2015; Fig. 3). Current data suggest that rather than focusing on individual coronary arterial lesions, we need a comprehensive, integrative approach for identifying and managing patients at risk of adverse cardiovascular events (Arbab-Zadeh 2015).
Different types of vulnerable plaque as underlying cause of acute coronary events (ACS) and sudden cardiac death (SCD). (a) Rupture-prone plaque with large lipid core and thin fibrous cap infiltrated by macrophages. (b) Ruptured plaque with subocclusive thrombus and early organization. (c) Erosion-prone plaque with proteoglycan matrix in a smooth muscle cell-rich plaque. (d) Eroded plaque with subocclusive thrombus. (e) Intraplaque hemorrhage secondary to leaking vasa vasorum. (f) Calcific nodule protruding into the vessel lumen. (g) Chronically stenotic plaque with severe calcification, old thrombus, and eccentric lumen (Reprinted with permission from Naghavi et al. 2003)
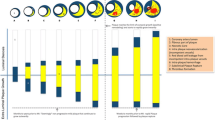
Annualized risk (percent) of myocardial infarction (MI) or cardiovascular (CV) death in 3,242 patients followed for a median of 3.6 years after baseline computed tomographic coronary angiography, according to the extent and severity of coronary artery disease. Risk is low in patients with nonobstructive disease (<50 % stenosis) involving four or fewer coronary artery segments (limited disease). Conversely, risk is similarly high in patients with nonobstructive disease if more than four segments are affected (extensive disease) compared with patients with obstructive disease (≥50 % stenosis) (Modified from Arbab-Zadeh et al. 2015)
Natural History of the Vulnerable Plaque
There are few longitudinal studies that investigated the natural history of plaque features that could be indicative of vulnerability or instability. Such studies involved a baseline imaging evaluation of the morphology of coronary (Motoyama et al. 2009; Kim et al. 2009; Bayturan et al. 2009; Ohtani et al. 2006; Lee et al. 2004) plaques and analyzed the occurrence of clinical events, imaging end points, or both in patients at follow-up. One of the largest studies to date (Motoyama et al. 2009) involved 1,059 patients with suspected or known disease who had computed tomography angiographic examinations and were followed for 27 months for the development of acute coronary syndrome (ACS). The coronary lesions were analyzed for the presence of two features of vulnerability: positive remodeling (>10 % diameter at the plaque site compared with the reference segment) and low attenuation plaques (non-calcified plaque with at low density). An ACS developed in 10 of 45 (22 %) patients that showed plaques with both vulnerability features, compared with 4 of 820 (0.5 %) patients that showed plaques without these features. None of the 167 patients with normal angiography results developed ACS. The presence of 1- or 2-feature positive plaques was the only significant independent predictor of ACS (hazard ratio, 22.8 [95 % CI, 6.9–75.2]) (Motoyama et al. 2009).
The PROSPECT (Providing Regional Observations to Study Predictors of Events in the Coronary Tree) was the first prospective, multicenter study of the natural history of coronary atherosclerosis, using multimodality intravascular imaging to identify the clinical and lesion-related factors that place patients at risk for adverse cardiac events (Stone et al. 2011). In this study, 697 patients with ACS underwent three-vessel coronary angiography and grayscale and radiofrequency intravascular ultrasonographic imaging after percutaneous coronary intervention (PCI) . Subsequent major adverse cardiovascular events (MACE) were adjudicated to be related to either originally treated (culprit) lesions or untreated (nonculprit) lesions (Stone et al. 2011). The 3-year cumulative rate of major adverse cardiovascular events was 20.4 %. Events were adjudicated to be related to culprit lesions in 12.9 % of patients and to nonculprit lesions in 11.6 %. Although the nonculprit lesions that led to major adverse cardiovascular events were frequently mild on angiographic assessment, most were characterized by a large plaque burden, a small luminal area, or both, as seen on grayscale intravascular ultrasonography but not on angiography; no major adverse cardiovascular events arose from untreated segments with a plaque burden resulting in less than 40 % loss of cross-sectional luminal area (Stone et al. 2011). The prospective identification of nonculprit lesions associated with major adverse cardiovascular events was further enhanced by the use of radiofrequency intravascular ultrasonography to characterize the morphologic features of plaques, with thin-cap fibroatheromas (TCFAs) representing the highest-risk phenotype, a finding that is consistent with the established concept of vulnerable plaque. Conversely, major adverse cardiovascular events related to nonculprit lesions rarely developed from non-fibroatheromas, regardless of the plaque burden or minimal luminal area (Stone et al. 2011; Fig. 4).
Event rates in the PROSPECT trial for lesions that were and those that were not thin-cap fibroatheromas, at a median follow-up of 3.4 years (Reprinted with permission from Stone et al. 2011)
Vulnerable Plaque Formation
Studies in genetically engineered mice deficient in apolipoprotein E, which develop advanced plaques similar to those in patients, have increased our understanding of certain clinical observations. An increase in T-helper type 1–like lymphocytes promoted TCFAs occurrence, indicating a possible role of the T-helper switch in the formation of these presumably vulnerable plaques.
Some authors (Sluijter et al. 2006) studied matrix metalloproteinases, which can degrade cap constituents, and an extracellular matrix metalloproteinase inducer in carotid endarterectomy specimens. Increased activity of matrix metalloproteinases 8 and 9 was associated with an inflammatory plaque phenotype, and different glycosylation forms of extracellular matrix metalloproteinase inducer were associated with varying degrees of matrix metalloproteinase activity. It was concluded that extracellular matrix metalloproteinase inducer glycosylation may play a role in plaque destabilization.
Vascular and hemodynamic forces are also likely to play a role in the formation and rupture of TCFAs. Several studies (Stone et al. 2003; Slager et al. 2005; Waxman et al. 2006) demonstrated that areas of low shear stress predispose to the formation of advanced plaques, presumably by creating conditions that favor transmigration of lipids and inflammatory cells into the vessel wall. High shear stress, on the other hand, can promote plaque rupture and platelet aggregability, leading to an occlusive thrombotic event (Stone et al. 2003; Slager et al. 2005; Waxman et al. 2006).
Biomarkers of Vulnerability and Their Potential Application to Prognosis
Increased understanding of the processes causing atherosclerosis has facilitated efforts to identify novel markers of risk that may be circulating in plasma and readily available for sampling.
To date, several biochemical markers have been investigated (Alsheikh-Ali et al. 2010; Seifarth et al. 2014; Battes et al. 2014; Ellims et al. 2014; Puri et al. 2013; Fuchs et al. 2012; Deftereos et al. 2012; Kubo et al. 2009; Hong et al. 2009; Rodriguez-Granillo et al. 2005; Van Mieghem et al. 2005; Drakopoulou et al. 2009; Table 1), C-reactive protein (CRP) and matrix metalloproteinases (MMPs) being the most commonly studied, and their concentrations were most commonly compared with imaging findings of plaques.
C-Reactive Protein
CRP is an acute-phase reactant and nonspecific marker of inflammation, produced predominantly in hepatocytes as a pentamer of identical subunits in response to several cytokines (Norata et al. 2009). Interleukin (IL)-6, one of the most potent drivers of CRP production, is released from activated leukocytes in response to infection or trauma and from vascular smooth muscle cells in response to atherosclerosis. CRP directly binds highly atherogenic oxidized LDL cholesterol and is present within lipid-laden plaques (Libby 2002).
The possible mechanistic role of CRP in plaque deposition is highly complex, exerting pro-atherogenic effects in many cells involved in atherosclerosis (Zhang et al. 1999). CRP may facilitate monocyte adhesion and transmigration into the vessel wall – a critical early step in the atherosclerotic process (Libby et al. 2008). Furthermore, M1 macrophage polarization, catalyzed by CRP, is a proinflammatory trigger in plaque deposition, leading to macrophage infiltration of both adipose tissue and atherosclerotic lesions (Kones 2011). Beyond its role in triggering immunity in plaque deposition, in vitro studies have also shown an association among CRP, inhibition of endothelial nitric oxide synthase, and impaired vasoreactivity 15 and 16. An isoform of CRP, monomeric CRP, is stimulated by platelet activation and has prothrombotic and inflammatory properties of its own (Eisenhardt et al. 2009). Monomeric CRP has also been found in plaques, particularly in regions of monocyte-mediated inflammatory activity, and within lipid microdomains of endothelial cells (Ji et al. 2009).
An association of CRP with risk for cardiovascular disease (CVD) has been described in many studies (Musunuru et al. 2008). The Multiple Risk Factor Intervention Trial (MRFIT) was the first of many primary prevention, prospective epidemiological studies to show a strong relationship between levels of CRP and mortality from CVD in high-risk middle-aged men (Kuller et al. 1996). A similar association between increasing CRP levels and subsequent rate of MI and stroke was found in an analysis of apparently healthy men (Ridker et al. 1997).
CRP has been evaluated extensively also in the setting of stable coronary artery disease (Tomai et al. 2005; Versaci et al. 2000; Gaspardone et al. 1998) and ACS (Morrow et al. 2007; Liuzzo et al. 1994; Biasucci et al. 1999). Elevated levels of CRP at the time of admission have been shown in multiple studies to be associated with poor outcomes in patients with ACS (Morrow et al. 2007; Liuzzo et al. 1994; Biasucci et al. 1999). The strength of that relationship varies depending of the degree of myocardial necrosis, the cut point applied, the timing of measurement, and the patient population (Morrow et al. 2007). Notably, elevated CRP concentrations are independently associated with enhanced vasoreactivity of the culprit lesion, but not in uninvolved epicardial coronary segments (Tomai et al. 2001; Fig. 5), supporting the concept that the increased vasoreactivity is a local plaque-related phenomenon (Tomai 2004). Assessing l e vels of CRP several weeks after ACS, when the acute inflammatory phase has subsided, may be more useful than in the acute setting. Patients with a CRP level >2 mg/L 1 month after admission for ACS were at significantly greater risk of death and heart failure (Scirica et al. 2009) compared with those with low levels of CRP.
Percent changes from baseline of minimal lumen diameter (MLD) (left) and of reference diameter (RD) (right) in patients with normal (open bars) and elevated (hatched bars) CRP serum levels during cold pressor test (CPT) and after intracoronary injection of nitroglycerin (NTG) (Reprinted with permission from Tomai et al. 2001)
Recently, the interaction of high-risk nonculprit lesions with CRP levels, which were measured at presentation, 1 month, and 6 months, then categorized at each time as normal (<3 mg/L), elevated (3–10 mg/L), or very elevated (>10 mg/L), has been examined among patients enrolled in the PROSPECT study (Kelly et al. 2014). Patients with elevated CRP levels at any time did not have more high-risk nonculprit lesions; however, untreated high-risk nonculprit lesions were more likely to cause subsequent MACE in patients with very elevated compared with normal 6-month CRP levels (for thin-cap fibroatheromas, 13.8 % vs. 1.9 %, p = 0.0003; for lesions with minimal luminal area ≤4.0 mm2, 15.6 % vs. 2.2 %, p < 0.0001). As expected, patients with very elevated 6-month CRP levels had higher rates of subsequent nonculprit lesion-related MACE (19.0 % vs. 7.2 %, p = 0.039) (Kelly et al. 2014).
Notably, wide variability of CRP levels exists among individuals (Yousuf et al. 2013). The interplay of CRP genetic polymorphisms, influence of genetic loci mediating CRP response, and lifestyle factors contributes to individual, ethnic, and sex-related variation in CRP concentration (Yousuf et al. 2013). A uniform cut point for CRP based on a single value should not be applied universally among all individuals. Body mass index, metabolic syndrome, diabetes mellitus, hypertension, oral contraceptive use, physical exercise, moderate alcohol consumption, periodontal disease, dietary patterns, environmental pollutant burden, and smoking cause significant baseline variation (Yousuf et al. 2013; Kones 2010).
Matrix Metalloproteinases
The MMPs comprise a fami ly of at least 23 active proteinases. MMPs and other proteinases can provoke net destruction of the vascular extracellular matrix in late-stage atherosclerosis, leading to plaque rupture (Galis et al. 1994). Importantly, loss of collagen in the shoulder regions of thin-cap fibroatheromas could reduce tensile strength and precipitate plaque rupture, leading to MI or strokes (Libby 2013). A broad spectrum of MMP inhibitors has been tested in preclinical studies without producing a net effect on atherosclerosis progression or histological features of instability, most likely because of the opposing roles of different MMPs. By contrast, two studies with selective MMP inhibitors showed favorable effects on plaque stability in apolipoprotein E-knockout mice models (Johnson et al. 2011; Quillard et al. 2011). However, translating this data into clinically useful therapies is hampered by the sheer numbers of MMPs and the conflicting results obtained in other animal models (Newby 2015).
Novel Biomarkers
There are several biomarkers reflecting a variety of pathophysiologic pathways that have been reported to be elevated in patients with ACS and potentially associated with increased risk. These include markers of ischemia and inflammation (ischemia-modified albumin, heart fatty acid-binding protein, myeloperoxidase), vascular dysfunction (pregnancy-associated plasma protein A0), biomechanical stress (copeptin, ST2, growth differentiation factor [GDF]-15), hemostasis (fibrinogen, plasminogen activator inhibitor-1), and lipid metabolism (lipoprotein-associated phospholipase A2) (Scirica 2010; Ferrante et al. 2010). Few of the novel biomarkers have been shown to consistently improve on established markers, and many lack confirmation in varied cohorts. In a study of 664 patients admitted with suspected ACS, for example, none of the more than ten novel markers tested approached the sensitivity of cardiac troponin in diagnosing MI (McCann et al. 2008).
Several authors have proposed analytical and clinical criteria that novel biomarkers must successfully meet before they can be fully integrated into clinical care (Jaffe et al. 2006). Of the novel markers, GDF-15, a member of the transforming growth factor family that is released by myocytes during ischemia and reperfusion, is one of the most promising. In several cohorts (Eggers et al. 2008; Wollert et al. 2007), elevated levels of GDF-15 are associated with increased risk of death and MI, independent of ECG changes, troponin level, or NP level. In one study, there was an interaction between randomization to an invasive strategy and elevated levels of GDF-15, which suggests that an invasive strategy may be preferential in patients with an increased concentration (Wollert et al. 2007), although prospective confirmatory studies are needed.
Proteomics, Metabolomics, Genomics, and Pharmacogenomics
Advances in proteomic, metabolic, and genomic profiling with high-throughput screening technology combined with advanced bioinformatic and statistical techniques may dramatically expand the number of novel markers of cardiac metabolism and pathology. For example, a study of serial blood samples from patients undergoing alcohol septal ablation, in other words a “planned MI,” revealed a specific profile of metabolites in pyrimidine metabolism, the tricarboxylic acid cycle, and the pentose phosphate pathway that were present within 10 min of the induced MI. The pattern was also present in patients with ACS undergoing PCI but not in patients with stable CAD undergoing PCI (Lewis et al. 2008). Genome-wide association studies, which evaluate hundreds of thousands of single nucleotide polymorphisms, have identified several potential variants such as those at chromosome 9p21 that are associated with an increased risk of incident CVD (Samani et al. 2007). Further studies are needed to determine whether individuals with single nucleotide polymorphisms at chromosome 9p21 are also at increased risk of secondary events after ACS.
Conclusions
In the quest for individualized medicine, biomarkers have emerged as a tool for improved risk prediction.
An ideal biomarker should demonstrate quantitative differences in patients with and without disease. Further, it should have predictive value in prospective studies and incremental benefit over standard clinical risk markers. The goal of measuring a biomarker should not only be risk assessment but rather ascertaining information that would alter the threshold of the pretest risk to change clinical management in a cost-effective manner. The ideal risk marker should demonstrate these features with rigorous evidence and independence (Hlatky et al. 2009).
During the last two decades, a number of biomarkers have been considered in the assessment of coronary plaque composition identifying the risk for primary and secondary prevention of cardiovascular diseases. However, further research is needed to undoubtedly determining a candidate that materially adds to established models of risk assessment and modification.
Summary Points
-
Substantial research has been recently conducted in order to develop new methods to identify subjects at risk before the occurrence of a cardiovascular event.
-
The concept of “vulnerable plaque” has gained attention as a paradigm to improve risk stratification and potentially lead to the discovery of novel markers of risk to prevent cardiovascular disease.
-
Biochemical markers have been investigated for the identification of coronary atherosclerotic plaque composition and early detection of their vulnerability.
-
C-reactive protein and matrix metalloproteinases are the most commonly studied, but also novel biomarkers reflecting a variety of pathophysiologic pathways have been reported to be potentially associated with increased risk of coronary events.
Abbreviations
- ACS:
-
Acute coronary syndrome
- CRP:
-
C-reactive protein
- CVD:
-
Cardiovascular disease
- LDL:
-
Low-density lipoprotein
- MACE:
-
Major adverse cardiovascular events
- MI:
-
Myocardial infarction
- MMP:
-
Matrix metalloproteinases
- PCI:
-
Percutaneous coronary intervention
- TCFA:
-
Thin-cap fibroatheromas
- VSMC:
-
Vascular smooth muscle cells
References
Alsheikh-Ali AA, Kitsios GD, Balk EM, et al. The vulnerable atherosclerotic plaque: scope of the literature. Ann Intern Med. 2010;153:387–95.
Ambrose JA, Winters SL, Arora RR, et al. Angiographic evolution of coronary artery morphology in unstable angina. J Am Coll Cardiol. 1986;7:472–8.
Arbab-Zadeh A, Fuster V. The myth of the “vulnerable plaque”. Transitioning from a focus on individual lesions to atherosclerotic disease burden for coronary artery disease risk assessment. J Am Coll Cardiol. 2015;65:846–55.
Battes LC, Cheng JM, Oemrawsingh RM, et al. Circulating cytokines in relation to the extent and composition of coronary atherosclerosis: results from the ATHEROREMO-IVUS study. Atherosclerosis. 2014;236:18–24.
Bayturan O, Tuzcu EM, Nicholls SJ, et al. Attenuated plaque at nonculprit lesions in patients enrolled in intravascular ultrasound atherosclerosis progression trials. JACC Cardiovasc Interv. 2009;2:672–8.
Biasucci LM, Liuzzo G, Grillo RL, et al. Elevated levels of C-reactive protein at discharge in patients with unstable angina predict recurrent instability. Circulation. 1999;99:855–60.
Cannon CP, Braunwald E, McCabe CH, Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 Investigators, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350:1495–504.
Daugherty A, Webb NR, Rateri DL, King VL. Thematic review series: the immune system and atherogenesis: cytokine regulation of macrophage functions in atherogenesis. J Lipid Res. 2005;46:1812–22.
Deftereos S, Giannopoulos G, Kossyvakis C, et al. Association of soluble tumour necrosis factor-related apoptosis-inducing ligand levels with coronary plaque burden and composition. Heart. 2012;98:214–8.
Drakopoulou M, Toutouzas K, Stefanadi E, et al. Association of inflammatory markers with angiographic severity and extent of coronary artery disease. Atherosclerosis. 2009;206:335–9.
Eggers KM, Kempf T, Allhoff T, et al. Growth-differentiation factor-15 for early risk stratification in patients with acute chest pain. Eur Heart J. 2008;29:2327–35.
Eisenhardt SU, Habersberger J, Murphy A, et al. Dissociation of pentameric to monomeric C-reactive protein on activated platelets localizes inflammation to atherosclerotic plaques. Circ Res. 2009;105:128–37.
Ellims AH, Wong G, Weir JM, et al. Plasma lipidomic analysis predicts non-calcified coronary artery plaque in asymptomatic patients at intermediate risk of coronary artery disease. Eur Heart J Cardiovasc Imaging. 2014;15:908–16.
Eriksson EE. Mechanisms of leukocyte recruitment to atherosclerotic lesions: future prospects. Curr Opin Lipidol. 2004;15:553–8.
Ferrante G, Nakano M, Prati F, et al. High levels of systemic myeloperoxidase are associated with coronary plaque erosion in patients with acute coronary syndromes: a clinicopathological study. Circulation. 2010;122:2505–13.
Fuchs S, Lavi I, Tzang O, et al. Intracoronary monocyte chemoattractant protein 1 and vascular endothelial growth factor levels are associated with necrotic core, calcium and fibrous tissue atherosclerotic plaque components: an intracoronary ultrasound radiofrequency study. Cardiology. 2012;123:125–32.
Galis ZS, Sukhova GK, Lark MW, Libby P. Increased expression of matrix metalloproteinases and matrix degrading activity in vulnerable regions of human atherosclerotic plaques. J Clin Invest. 1994;94:2493–503.
Gaspardone A, Crea F, Versaci F, et al. Predictive value of C-reactive protein after successful coronary-artery stenting in patients with stable angina. Am J Cardiol. 1998;82:515–8.
Giroud D, Li JM, Urban P, et al. Relation of the site of acute myocardial infarction to the most severe coronary arterial stenosis at prior angiography. Am J Cardiol. 1992;69:729–32.
Hackett D, Davies G, Maseri A. Pre-existing coronary stenoses in patients with first myocardial infarction are not necessarily severe. Eur Heart J. 1988;9:1317–23.
Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95.
Hlatky MA, Greenland P, Arnett DK, et al. Criteria for evaluation of novel markers of cardiovascular risk: a scientific statement from the American Heart Association. Circulation. 2009;119:2408–16.
Hong YJ, Jeong MH, Choi YH, et al. Plaque characteristics in culprit lesions and inflammatory status in diabetic acute coronary syndrome patients. JACC Cardiovasc Imaging. 2009;2:339–49.
Jaffe AS, Babuin L, Apple FS. Biomarkers in acute cardiac disease: the present and the future. J Am Coll Cardiol. 2006;48:1–11.
Ji SR, Ma L, Bai CJ, et al. Monomeric C-reactive protein activates endothelial cells via interaction with lipid raft microdomains. FASEB J. 2009;23:1806–16.
Johnson JL, Devel L, Czarny B, et al. A selective matrix metalloproteinase-12 inhibitor retards atherosclerotic plaque development in apolipoprotein E-knockout mice. Arterioscler Thromb Vasc Biol. 2011;31:528–35.
Kelly CR, Weisz G, Maehara A, et al. Relation of C-reactive protein levels to instability of untreated vulnerable coronary plaques (from the PROSPECT study). Am J Cardiol. 2014;114:376–83.
Kim SH, Hong MK, Park DW, et al. Impact of plaque characteristics analyzed by intravascular ultrasound on long-term clinical outcomes. Am J Cardiol. 2009;103:1221–6.
Kolodgie FD, Virmani R, Burke AP, et al. Pathologic assessment of the vulnerable human coronary plaque. Heart. 2004;90:1385–91.
Kones R. Rosuvastatin, inflammation, C-reactive protein, JUPITER, and primary prevention of cardiovascular disease a perspective. Drug Des Devel Ther. 2010;4:383–413.
Kones R. Primary prevention of coronary heart disease: integration of new data, evolving views, revised goals, and role of rosuvastatin in management. A comprehensive survey. Drug Des Devel Ther. 2011;5:325–80.
Kubo T, Matsuo Y, Hayashi Y, et al. High-sensitivity C-reactive protein and plaque composition in patients with stable angina pectoris: a virtual histology intravascular ultrasound study. Coron Artery Dis. 2009;20:531–5.
Kuller LH, Tracy RP, Shaten J, Meilahn EN. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Multiple Risk Factor Intervention Trial. Am J Epidemiol. 1996;144:537–47.
Lee SG, Lee CW, Hong MK, et al. Change of multiple complex coronary plaques in patients with acute myocardial infarction: a study with coronary angiography. Am Heart J. 2004;147:281–6.
Lewis GD, Wei R, Liu E, et al. Metabolite profiling of blood from individuals undergoing planned myocardial infarction reveals early markers of myocardial injury. J Clin Invest. 2008;118:3503–12.
Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–74.
Libby P. Collagenases and cracks in the plaque. J Clin Invest. 2013;123:3201–3.
Libby P, Theroux P. Pathophysiology of coronary artery disease. Circulation. 2005;111:3481–8.
Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–43.
Libby P, Nahrendorf M, Pittet MJ, et al. Diversity of denizens of the atherosclerotic plaque: not all monocytes are created equal. Circulation. 2008;117:3168–70.
Little WC, Constantinescu M, Applegate RJ, et al. Can coronary angiography predict the site of a subsequent myocardial infarction in patients with mild-to-moderate coronary artery disease? Circulation. 1988;78:1157–66.
Liuzzo G, Biasucci LM, Gallimore JR, et al. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331:417–24.
McCann CJ, Glover BM, Menown IB, et al. Novel biomarkers in early diagnosis of acute myocardial infarction compared with cardiac troponin T. Eur Heart J. 2008;29:2843–50.
Morrow DA, Cannon CP, Jesse RL, et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: clinical characteristics and utilization of biochemical markers in acute coronary syndromes. Circulation. 2007;115:e356–75.
Motoyama S, Sarai M, Harigaya H, et al. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54:49–57.
Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation. 1989;79:733–43.
Musunuru K, Kral BG, Blumenthal RS, et al. The use of high-sensitivity assays for C-reactive protein in clinical practice. Nat Clin Pract Cardiovasc Med. 2008;5:621–35.
Naghavi M, Libby P, Falk E, et al. From vulnerable plaque to vulnerable patient: a call for new definitions and risk assessment strategies: part I. Circulation. 2003;108:1664–72.
Newby AC. Metalloproteinases promote plaque rupture and myocardial infarction: a persuasive concept waiting for clinical translation. Matrix Biol. 2015. doi:10.1016/j.matbio.2015.01.015.
Norata GD, Marchesi P, Pulakazhi Venu VK, et al. Deficiency of the long pentraxin PTX3 promotes vascular inflammation and atherosclerosis. Circulation. 2009;120:699–708.
Ohtani T, Ueda Y, Mizote I, et al. Number of yellow plaques detected in a coronary artery is associated with future risk of acute coronary syndrome: detection of vulnerable patients by angioscopy. J Am Coll Cardiol. 2006;47:2194–200.
Puri R, Tuzcu EM, Nissen SE, et al. Exploring coronary atherosclerosis with intravascular imaging. Int J Cardiol. 2013;168:670–9.
Quillard T, Tesmenitsky Y, Croce K, et al. Selective inhibition of matrix metalloproteinase-13 increases collagen content of established mouse atherosclerosis. Arterioscler Thromb Vasc Biol. 2011;31:2464–72.
Ridker PM, Cushman M, Stampfer MJ, et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9.
Rodriguez-Granillo GA, Serruys PW, McFadden EP, et al. First-in-man prospective evaluation of temporal changes in coronary plaque composition by in vivo intravascular ultrasound radiofrequency data analysis: an Integrated Biomarker and Imaging Study (IBIS) substudy. EuroIntervention. 2005;1:282–8.
Samani NJ, Erdmann J, Hall AS, et al. Genomewide association analysis of coronary artery disease. N Engl J Med. 2007;357:443–53.
Scirica BM. Acute coronary syndrome. Emerging tools for diagnosis and risk assessment. J Am Coll Cardiol. 2010;55:1403–15.
Scirica BM, Cannon CP, Sabatine MS, et al. Concentrations of C-reactive protein and B-type natriuretic peptide 30 days after acute coronary syndromes independently predict hospitalization for heart failure and cardiovascular death. Clin Chem. 2009;55:265–73.
Seifarth H, Schlett CL, Lehman SJ, et al. Correlation of concentrations of high-sensitivity troponin T and high-sensitivity C-reactive protein with plaque progression as measured by CT coronary angiography. J Cardiovasc Comput Tomogr. 2014;8:452–8.
Slager CJ, Wentzel JJ, Gijsen FJ, et al. The role of shear stress in the generation of rupture-prone vulnerable plaques. Nat Clin Pract Cardiovasc Med. 2005;2:401–7.
Sluijter JP, Pulskens WP, Schoneveld AH, et al. Matrix metalloproteinase 2 is associated with stable and matrix metalloproteinases 8 and 9 with vulnerable carotid atherosclerotic lesions: a study in human endarterectomy specimens pointing to a role for different extracellular matrix metalloproteinase inducer glycosylation forms. Stroke. 2006;37:235–9.
Stary HC. Natural history and histological classification of atherosclerotic lesions: an update. Arterioscler Thromb Vasc Biol. 2000;20:1177–8.
Stone PH, Coskun AU, Yeghiazarians Y, et al. Prediction of sites of coronary atherosclerosis progression: in vivo profiling of endothelial shear stress, lumen, and outer vessel wall characteristics to predict vascular behavior. Curr Opin Cardiol. 2003;18:458–70.
Stone GW, Maehara A, Lansky AJ, PROSPECT Investigators, et al. A prospective natural-history study of coronary atherosclerosis. N Engl J Med. 2011;364:226–35.
Tomai F. C reactive protein and microvascular function. Heart. 2004;90:727–8.
Tomai F, Crea F, Gaspardone A, et al. Unstable angina and elevated C-reactive protein levels predict enhanced vasoreactivity of the culprit lesion. Circulation. 2001;104:1471–6.
Tomai F, Ribichini F, Ghini AS, et al. Elevated C-reactive protein levels and coronary microvascular dysfunction in patients with coronary artery disease. Eur Heart J. 2005;26:2099–105.
Van Mieghem CA, Bruining N, Schaar JA, et al. Rationale and methods of the integrated biomarker and imaging study (IBIS): combining invasive and non-invasive imaging with biomarkers to detect subclinical atherosclerosis and assess coronary lesion biology. Int J Cardiovasc Imaging. 2005;21:425–41.
Versaci F, Gaspardone A, Tomai F, et al. Predictive value of C-reactive protein in patients with unstable angina pectoris undergoing coronary artery stent implantation. Am J Cardiol. 2000;85:92–5.
Virmani R, Kolodgie FD, Burke AP, et al. Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol. 2000;20:1262–75.
Virmani R, Burke AP, Farb A, et al. Pathology of the vulnerable plaque. J Am Coll Cardiol. 2006;47:C13–8.
Waxman S, Ishibashi F, Muller JE. Detection and treatment of vulnerable plaques and vulnerable patients. Novel approaches to prevention of coronary events. Circulation. 2006;114:2390–411.
Wollert KC, Kempf T, Lagerqvist B, et al. Growth differentiation factor 15 for risk stratification and selection of an invasive treatment strategy in non ST-elevation acute coronary syndrome. Circulation. 2007;116:1540–8.
Yousuf O, Mohanty BD, Martin SS, et al. High-sensitivity C-reactive protein and cardiovascular disease: a resolute belief or an elusive link? J Am Coll Cardiol. 2013;62:397–408.
Zhang YX, Cliff WJ, Schoefl GI, et al. Coronary C-reactive protein distribution: its relation to development of atherosclerosis. Atherosclerosis. 1999;145:375–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
De Luca, L., Tomai, F. (2016). Biomarkers of Coronary Plaque Composition and Vulnerability. In: Patel, V., Preedy, V. (eds) Biomarkers in Cardiovascular Disease. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7678-4_44
Download citation
DOI: https://doi.org/10.1007/978-94-007-7678-4_44
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7677-7
Online ISBN: 978-94-007-7678-4
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences