Abstract
Atrial fibrillation (AF) confers a raised risk of stroke, thromboembolism, and death, and this risk of adverse events is increased by the coexistence of other cardiovascular risk factors. Despite being easy to use for decision-making concerning oral anticoagulant therapy in AF, different clinical risk scores used for stratification have shown modest capability in predicting thromboembolic events, and biomarkers may improve our identification of “high-risk” patients. Biomarkers significantly improve risk stratification in addition to current clinical risk stratification models. These new findings may enable development of novel tools to improve clinical risk assessment in AF. This chapter will highlight novel associations of biomarkers and outcomes in AF as well as recent progress in the use of biomarkers for risk stratification, with focus on data from randomized prospective clinical trials and large community-based cohorts.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Key Facts of Stroke and Systemic Thromboembolism
-
The pathways underlying thrombogenesis in AF are complex. Abnormal changes are consistent with a prothrombotic or hypercoagulable state in AF.
-
Clinical scores such as CHADS2 or CHA2DS2–VASc have only modest predictive value for predicting “high-risk” subjects and could benefit from inclusion of biomarkers related to prothrombotic changes.
-
Several studies have reported troponins as an indicator of high risk of stroke or systemic embolism.
-
In the larger ARISTOTLE and RE-LY substudies, an especially strong association between increased risk of ischemic stroke and rising NT-proBNP levels was observed.
-
A recent study published by our group showed that adding CKD to the stroke risk scores did not independently improve the predictive value of current clinical scores.
-
Rising cystatin C levels were independently associated with increased rates of stroke or systemic embolism.
-
The addition of BTP improves the predictive value of a clinical risk score for the detection of thrombotic events.
-
The recent trials describe a significant association between baseline D-dimer levels and the risk of stroke independent of established risk factors including CHA2DS2–VASc variables.
-
Several studies have demonstrated an association between stroke and thromboembolism and endothelial damage biomarkers (vWF, sE-sel, sTM).
-
A small study reported the association between IL-6 and a composite outcome of stroke and death.
-
Platelet size, measured as mean platelet volume, has been associated with platelet reactivity and as an independent risk factor for future stroke.
-
Adiponectin could exert a protective role against cardiovascular diseases.
-
Although these markers are widely and effectively used in experimental research, their usage in everyday clinical practice remains limited.
Key Facts of Mortality
-
Isolated increases of troponin I concentrations generally seemed to be associated with higher risk of cardiac death and myocardial infarction compared with isolated increases in troponin T.
-
NT-proBNP was also predictive of all-cause mortality, suggesting that this biomarker may potentially be used to refine clinical risk stratification in anticoagulated patients with AF.
-
The presence of impaired renal function was also associated consistently with the development of adverse cardiovascular events and mortality, even after adjusting for the CHADS2 score.
-
CRP and IL-6 seem to be independent markers for mortality in patients with AF.
-
GDF-15 was shown to be an additive prognostic marker for death, even after adjusting for clinical variables, risk factors, and CHA2DS2–VASc score and other biomarkers.
Key Facts of Bleeding
-
The causality is unknown, but elevated troponin I levels might contribute to the identification of a more fragile AF subpopulation more likely to bleed during anticoagulation.
-
Higher baseline NT-proBNP concentration was strongly associated with each of the major clinical outcomes explored (like stroke or mortality), except major bleeding, even after adjustment for multivariable model.
-
Renal dysfunction has been associated with an increased risk of bleeding. The incidence of major bleeding increased significantly with the impairment of renal function.
-
Renal dysfunction may be associated with INR and worse the average percentage of the time in the optimal therapeutic INR (TTR).
-
High levels of cystatin C, when added to the eGFR equation, were associated with increased HR rates of major bleeding in patients taking warfarin.
-
BTP also improved the predictive value of the HAS-BLED score for major bleeding.
-
A high plasma vWF level showed an additive effect on the HAS-BLED score, for an intermediate-risk category for bleeding (HAS-BLED score 1–2 points).
-
DD levels at baseline, regardless OAC, were related to major bleeding.
-
GDF-15 was shown to be an additive prognostic marker for major bleeding in patients with AF receiving.
Definitions
Atrial fibrillation
An abnormal and irregular heart rhythm in which electrical signals are generated chaotically throughout the upper chambers (atria) of the heart.
Beta-thromboglobulin
A platelet-specific protein that indicates platelet activation and is released from alpha-granules during platelet aggregation and subsequent thrombus formation.
Biomarker
Any measurable indicator that are potentially useful along the whole spectrum of the disease process; research and development of new therapies; diagnosis, prognosis, and monitoring progression of a disease; or response to treatment.
B-type natriuretic peptide
A neurohormone synthesized by myocytes, predominantly in the left ventricle, in response to increased wall tension such as volume or pressure overload.
CHA2DS2–VASc score
A stroke risk score that assigns 1 point each for presence of congestive heart failure, hypertension, diabetes mellitus, vascular disease, age >65, and sex category (female gender) and 2 points to age >75 years and prior stroke/TIA. Patients with high CHADS2 scores (>2) are at significant risk for stroke: 5.9 % annual risk with a score of 3 and up to 18.2 % annual stroke risk for patients with a score of 6.
Cystatin C
A small protein, synthesized at a constant rate in all nucleated cells. It is freely filtered by the glomerulus and does not return to the blood flow.
HAS-BLED score
A new bleeding risk score, ranges from 0 to 9 that assigns 1 point for the presence of each of the following: hypertension (uncontrolled systolic blood pressure >160 mmHg), abnormal renal and/or liver function, previous stroke, bleeding history or predisposition, labile international normalized ratios, elderly, and concomitant drugs and/or alcohol excess. With scores of ≥3 indicating high risk of bleeding, caution and regular review of the patient are recommended.
Plasma D-dimer
A fibrin degradation product and is a marker of intravascular thrombogenesis and fibrin turnover.
TTR
Percentage of the time of INR in the therapeutic range (2.0–3.0).
von Willebrand factor
An established biomarker of endothelial damage/dysfunction. It is synthesized by vascular endothelial cells and promotes platelet adhesion and aggregation, leading to thrombus formation.
Introduction
Atrial fibrillation is the most common sustained cardiac arrhythmia which is associated with high risk of stroke, thromboembolism, and mortality (Wolf et al. 1991; Benjamin et al. 1998). In addition to these complications, many patients with AF have impaired cognitive function, impaired quality of life, and increased health care costs. The prevalence of AF increases with age and reaches 10 % in persons >80 years. The pathophysiology of AF is complex and multifactorial. The process involves a structural remodeling in which connective tissue deposition and fibrosis are the hallmarks (Fig. 1), as well as altered atrial electrophysiological properties facilitating the initiation and perpetuation of AF (Daoud et al. 1996; Frustaci et al. 1997). Besides, left ventricular dysfunction and elevated ventricular filling pressures contribute to atrial remodeling and may produce a substrate that predisposes for AF as well (Savelieva and Camm 2004). Many AF patients remain asymptomatic with an increase for fatal or disabling complications as first manifestation of this arrhythmia; consequently, improved diagnostic techniques have identified various biomarkers that may have an important role in prediction of AF and related outcomes (Tables 1, 2, and 3).
Otherwise, AF confers a prothrombotic or hypercoagulable state (Fig. 2), which participates in the two- to sevenfold increased risk for thromboembolic complications. AF fulfills the Virchow’s triad for thrombogenesis, including left atrial blood stasis (“flow abnormalities”), endothelial damage/dysfunction (“vessel wall abnormalities”), and abnormal blood constituents (Watson et al. 2009). Nonetheless, the precise mechanism(s) of how AF results in activation of the coagulation cascade are unclear.
In this setting, biomarkers could take an interesting role. The Food and Drug Administration defines biomarker as any measurable indicator that is potentially useful along the whole spectrum of the disease process; research and development of new therapies; diagnosis, prognosis, and monitoring progression of a disease; or response to treatment (Goodsaid and Frueh 2007). In the last decades, biomarkers have gained huge scientific and clinical value and interest in medical practice. The ideal biomarker should be easily obtained with minimum discomfort or risk to the patient, may also appear or disappear over the course of disease progression, and thus may be useful in determining the prognosis of a disease within an individual. Another biomarker may change as a drug therapy is started, adjusted, or discontinued, ultimately aiding in the monitoring of the patient’s response to that particular therapy. In addition, the rapid return of results for early initiation of treatment and monitoring effectiveness is highly desirable. This could be a test performed during a patient’s office visit with an immediate result. Finally, a reliable biomarker will have a detection method that could be both sensitive and specific and highly reproducible among clinical laboratories.
Renewed interest has arisen to study the different pathways that underlay this hypercoagulable state in AF. Figure 3 shows different pathways underlying hypercoagulable state in AF and their association with biomarkers (Vilchez et al. 2014).
Different pathways involved in the AF pathophysiology related to various biomarkers (Figure obtained from Vílchez et al. 2014)
Risk Stratification in AF
Oral anticoagulation (OAC) is highly effective in reducing stroke risk and mortality rates in patients with AF, but also increases the risk of bleeding (Singer et al. 2009). Assessment of AF- associated stroke risk is mainly based on clinical risk scores such as CHADS2 and CHA2DS2–VASc. The current guidelines on AF recommend the use of CHA2DS2–VASc score to assess thromboembolic risk (Craig et al. 2014; Camm et al. 2012). CHA2DS2–VASc score assigns 1 point each for presence of congestive heart failure, hypertension, diabetes mellitus, vascular disease, age >65, and sex category (female gender) and 2 points to age >75 years and prior stroke/TIA (Craig et al. 2014). AF patients with CHA2DS2–VASc ≥2 should be considered for starting OAC, and patients with CHA2DS2–VASc = 1 would have considered indication to initiate OAC for preventing stroke. Subjects categorized to be OAC eligible will be exposed to an increased risk of major bleeding (Providencia et al. 2012). The alternative would be to leave some patients untreated and exposed to the risk of fatal and devastating strokes. Stroke risk is also closely related to bleeding risk, and OAC therapy needs to weigh the benefit from stroke prevention against the bleeding risk. Many thromboembolic risk factors have also been identified as bleeding risk factors (e.g., advanced age or uncontrolled hypertension) (Lip et al. 2011). The HAS-BLED (Hypertension, Abnormal Renal/Liver Function, Stroke, Bleeding History or Predisposition, Labile International Normalized Ratio, Elderly, and Drugs/Alcohol Concomitantly) was proposed as a practical tool to assess the individual bleeding risk of “real-world” AF patients (Pisters et al. 2010). A score of >3 pointes indicates “high risk”; however, this score, as European guidelines state, does not contraindicate OAC therapy (Camm et al. 2012). In these patients with high bleeding risk, close monitoring is required after the initiation of antithrombotic therapy, as well as efforts to correct the potentially reversible risk factors for bleeding.
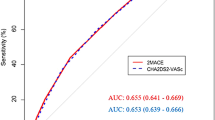
Although these scores are easy to apply, the clinical risk scores have limited capacity for prediction of thromboembolic events, with low values for the area under the receiver operating characteristic curve, known as the c-statistic. Numerous studies have highlighted the potential utility of biomarkers in enhancing risk stratification and improving the predictive power of clinical risk scores, such CHA2DS2–VASc (Hijazi et al. 2012). Advances in genomics, proteomics, and molecular pathology have generated many candidate biomarkers that might play an important role in prediction of related outcomes in AF (López-Cuenca et al. 2010; Hijazi et al. 2013a). There is much interest in blood-based biomarkers that could provide additional refinement to clinical risk stratification.
On the other hand, most of the interest has been focused on embolic risk and the development of major bleeds in patients under OAC. However, an increase on all-cause death in patients with AF has been observed (Camm et al. 2012). It probably merits to assess the risk of death of our patients in clinical practice.
We will review the published data about biomarkers in AF and focus on the predictive ability of the three most important cardiovascular events: thromboembolism, mortality, and major bleeding.
Cardiac Biomarkers and AF Outcomes
Stroke and Systemic Thromboembolism
Cardiac Troponins
Cardiac troponins are intracellular proteins involved in heart muscle contraction, and thus they are known as sensitive and specific biomarkers of myocardial injury (Roldán et al. 2012). Troponins as an indicator of high risk of stroke or systemic embolism were first reported from the Randomized Evaluation of Long-Term Anticoagulant Therapy (RE-LY) biomarker substudy performed in 6,189 patients with AF and treated with either warfarin or dabigatran (Hijazi et al. 2012). The Apixaban for the Prevention of Stroke in Subjects with Atrial Fibrillation (ARISTOTLE) troponin substudy results verified that the troponin levels were related to the risk of stroke, in a continuous fashion, independent of baseline characteristics and other biomarkers (Hijazi et al. 2014a). These two studies, therefore, provide firm evidence that patients classified as having elevated troponin levels based on the 99th percentile upper reference limit for healthy subjects (troponin I >0.04 μg/L or high-sensitivity troponin T >13 ng/L) had significantly increased risk of stroke and systemic embolism independent of clinical characteristics and other powerful biomarkers. Moreover, in comparison with CHADS2 and CHA2DS2–VASc, when adding information about troponin measurements to a predictive model for stroke outcomes, the troponin I level provided significant incremental prognostic information.
Interestingly, a recent ARISTOTLE substudy (Hijazi et al. 2014) assessed the distribution and compared and combined the prognostic value of cTnI and cTnT measured with high-sensitivity methods in patients with AF. Their findings show that the correlation between cTnI and cTnT concentrations was moderate and patients with both troponins above the median had significantly higher risk for stroke/systemic embolism than those with both troponins below median over a median 1.9 years of follow-up. However, intermediate risks were observed when only one assay of troponin was above the median; and when considered with information from other clinical risk factors, cTnI and cTnT provide similar prognosis information. Renal impairment was the most important determinant of increased troponin concentrations, with similar influence on both markers.
The underlying cause of the association between high troponin and stroke is not clearly elucidated. Troponin increase could be related to AF per se, or caused by coexistent cardiovascular risk factors, or troponin may simply reflect a sick heart. Even without a complete understanding of the mechanism, the firm evidence and the general availability of cardiac troponin measurements for routine care in most hospitals worldwide make it a very attractive candidate for use to improve prognostication of patients with AF, in addition to the currently recommended clinical stroke risk stratification.
Natriuretic Peptides
B-type natriuretic peptide (BNP) is a neurohormone synthesized by myocytes, predominantly in the left ventricle (LV), in response to increased wall tension such as volume or pressure overload (Daniels and Maisel 2007). BNP is secreted as an inactive prohormone. It is cleaved in equimolar amounts into the bioactive hormone, BNP, and the inactive N-terminal fragment (NT-proBNP) (Boomsma and van den Meiracker 2001). Although natriuretic peptides are excellent markers of LV function and considered as a simple and effective tool to diagnose heart failure or LV dysfunction, these indices have also been analyzed in different cardiovascular disorders.
Initial studies demonstrated elevated levels of BNP in patients with AF compared with matched controls in sinus rhythm (Ellinor et al. 2005; Shelton et al. 2006). Regarding the influence of these biomarkers, it was not until RE-LY results that the prognostic value of this information was highlighted (Hijazi et al. 2012). In the RE-LY substudy, the levels of NT-proBNP correlated with the risk of thromboembolic events and cardiovascular mortality with higher risk at rising levels. In the larger ARISTOTLE biomarker study was observed an especially strong association between increased risk of ischemic stroke and rising NT-proBNP levels (Hijazi et al. 2013). Recently our group showed that in a real-world cohort of anticoagulated patients with AF, NT-proBNP provided complementary prognostic information to an established clinical risk score (CHA2DS2–VASc) for the prediction of stroke/systemic embolism (Roldán et al. 2014).
The use of transesophageal echocardiography provides information of variables associated with thromboembolism, such as dense spontaneous echo contrast, low flow velocities in the left atrial appendage, or even the presence of left atrial thrombus. These parameters have been linked in small studies to elevated levels of natriuretic peptides and may contribute to the prognostic properties of these biomarkers in AF (Igarashi et al. 2001). Okada et al. (2011) showed that BNP levels can serve as a marker for left atrial thrombus in patients with AF who suffered acute ischemic stroke or transient ischemic attack. It has been suggested that the development of new onset AF in patients with acute ischemic stroke was strongly associated with higher BNP levels. This theory proposes that atrial dysfunction is an established risk factor of thrombus formation in AF and thereby represents plausible pathophysiologic mechanism for relation between natriuretic peptides and thromboembolic events in AF. The improved risk prediction by adding natriuretic peptides to clinical risk stratification models is substantial, and the availability of the analysis is widespread and easy accessible. Therefore, the opportunity to use measurements of NT-proBNP to improve risk stratification of AF patients in routine clinical practice is very attractive.
Renal Function Biomarkers in AF
Glomerular filtration rate (GFR) is accepted as useful index of renal function and is usually estimated from serum levels of endogenous filtration markers such as creatinine. The prevalence of AF is higher in end-stage renal disease populations compared with the general population, and the AF prevalence increases when GFR decreases in general chronic kidney disease (CKD) cohorts (Ananthapanyasut et al. 2010; Deo et al. 2010). Concerning renal function and stroke outcomes in AF, Go et al. reported an independent risk increase with reduced GFR or if proteinuria was present (Go et al. 2009). Hohnloser et al. reported similar findings based on ARISTOTLE trial population, in which increased rates of stroke occurred as renal function was deteriorated (Hohnloser et al. 2012). Remarkably, the recent study published by our group based on c-statistics and the integrated discrimination improvement showed that adding CKD to the stroke risk scores did not independently improve the predictive value of current clinical scores (Roldán et al. 2013a).
Cystatin C is a small protein, synthesized at a constant rate in all nucleated cells (Abrahamson et al. 1990). It is freely filtered by the glomerulus and does not return to the blood flow. Thus, this protein was proposed as a more reliable marker of renal function than serum creatinine, in particular for the detection of small reductions in GFR (Laterza et al. 2002; Newman et al. 1995). Cystatin C is a considered to reflect microvascular renal dysfunction and has been linked to elevated levels of markers of coagulation, raised levels of inflammatory markers, and severity of coronary artery disease (Dubin et al. 2011). Furthermore, cystatin C significantly improves risk stratification compared with creatinine-based estimation of GFR in both elderly and coronary artery disease populations (Ix et al. 2007). The significance of cystatin C in an AF population was recently reported from ARISTOTLE and RE-LY biomarker substudies (Hohnloser et al. 2012). Rising cystatin C levels were independently associated with increased rates of stroke or systemic embolism.
Beta-trace protein (BTP) is a lipocalin glycoprotein identified as lipocalin-type prostaglandin D synthase (Hoffmann et al. 1993). In the human heart, BTP is localized in myocardial cells and atrial and ventricular endocardial cells. BTP levels are elevated in the circulation of patients with severe coronary heart disease. In addition, BTP has been considered as an accurate biomarker of glomerular filtration, perhaps even more accurate than serum creatinine or eGFR in detecting impaired renal function, given that BTP has less dependence on extrarenal factors such as age, body dual-mass index, nutritional status, and sex. Our group demonstrated that the addition of BTP improves the predictive value of a clinical risk score (i.e., CHA2DS2–VASc) for the detection of thrombotic events (Vílchez et al. 2013). Thus, BTP may be another novel predictor of thromboembolism.
Thrombogenesis Biomarkers in AF
Plasma D-dimer is a fibrin degradation product and is a marker of intravascular thrombogenesis and fibrin turnover. Levels of D-dimer are elevated compared with matched controls in sinus rhythm and even seem to remain increased despite successful cardioversion (Asakura et al. 1992). Levels of D-dimer further seem to rise along with the accumulation of clinical risk factors for thromboembolism or by the presence of atrial appendage thrombi. The recent trials (RE-LY, ARISTOTLE) describe a significant association between baseline D-dimer levels and the risk of stroke independent of established risk factors including CHA2DS2–VASc variables (Eikelboom et al. 2010).
The risk increases with higher D-dimer levels as evidenced by a threefold increase of stroke or systemic embolism when the top vsersus bottom quartiles were compared. These results suggest that D-dimer may also be a clinically useful risk marker in AF. However, a study realized for our group did not find that D-dimer levels in an anticoagulated AF cohort were related to the prognosis (Roldán et al. 2011).
Prothrombin fragment 1 +2 (F1+2) reflects in vivo thrombin generation, is reported to be elevated in AF, and is suppressed by anticoagulation in a dose-dependent manner. F1+2 levels were independently associated with advanced age, female sex, systolic blood pressure, and heart failure and were not influenced by aspirin use. In the third Stroke Prevention in Atrial Fibrillation (SPAF III) study, elevated F1+2 levels, as index of thrombogenesis, were associated with a clinical risk factor for stroke in AF (Feinberg et al. 1999). Moreover, F1+2 levels measured were higher in participants who subsequently suffered thromboembolic events, but differences were only marginally statistically significant.
Fibrinolytic system dysfunction may contribute to increase risk of thrombosis. Plasma levels of modified antithrombin III (ATM), tissue plasminogen activator (tPA), its inhibitor (PAI-1), tPA–PAI-1 complexes, and plasmin–antiplasmin (PAP) complexes have been measured in plasma from patients with chronic atrial fibrillation compared with healthy subjects. The results showed a hypofibrinolytic state caused by elevated PAI-1 levels with no increase in PAP complex concentration (Roldán et al. 1998). Vene et al. observed that high levels of tPA antigen levels were significantly associated with combined cardiovascular events in AF patients (Vene et al. 2003). In conclusion, high levels of D-dimer and tPA antigen during oral anticoagulant therapy may be associated to combined cardiovascular events in AF patients and, on this basis, could be useful additional markers of cardiovascular risk in such patients.
Endothelial Damage Biomarkers
Plasma levels of von Willebrand factor (vWF), soluble thrombomodulin (sTM), and soluble E- selectin (sE-sel) are used as indexes of damage/dysfunction, endothelial damage, and endothelial activation. Indeed, vWF is an established biomarker of endothelial damage/dysfunction, as it is synthesized by vascular endothelial cells and promotes platelet adhesion and aggregation, leading to thrombus formation (Roldán et al. 2011). Plasma vWF levels have been associated with independent risk factors for stroke (heart failure, previous stroke, age, and diabetes) and stroke risk stratification schemes (Conway et al. 2004). Plasma vWF levels correlated with two risk stratification scores for stroke (CHADS2 and Framingham) in AF patients (Lip et al. 2006). Recent studies showing an association between AF and endothelial damage/dysfunction found that it is reversed after restoration of sinus rhythm by catheter ablation or electrical cardioversion. Despite the immediate improvement of endothelial function after sinus rhythm restoration, more sustained postcardioversion (delayed) injury and shedding of endothelial cells could be contributors to longer-term thromboembolic complications (Freestone et al. 2006). These changes in the hypercoagulable state and endothelial (dys)function occur within minutes of acute AF onset and appear to be persistent after sinus rhythm restoration. Roldán et al. confirmed that an increased plasma vWF levels were associated with adverse prognosis on “real-life” AF patients, mainly thrombotic events (Roldán et al. 2005). Therefore, the addition of vWF as a biomarker risk factor may help to refine these clinical risk stratification schemes for stroke.
A soluble form of thrombomodulin is a recognized marker of endothelial dysfunction and may contribute to the hypercoagulable state in AF. Plasma sTM levels are lower in patients with persistent AF (Freestone et al. 2007).
Freestone et al. hypothesized that endothelial dysfunction exists in AF and that this could be demonstrated by impaired flow-mediated dilatation (FMD) and related to plasma indices of endothelial damage/dysfunction plasma biomarkers, as well as total body nitrate/nitrite product (NOx, a measure of endothelial nitric oxide production) (Freestone et al. 2008). This study demonstrated that endothelial dysfunction, as demonstrated by impairment of FMD and raised vWF and E-selectin, is present in AF. Other studies reported that high plasma vWf and sE-sel levels are associated with an increased risk of ischemic stroke in “real-world” patients with AF with a median follow-up of 19 (9–31) months (Krishnamoorthy et al. 2013). These soluble biomarkers may potentially aid clinical risk stratification in this common arrhythmia.
Platelets
D ifferent platelet activation markers have been described in AF patients. However, many abnormal changes in platelets seen in AF could simply indicate underlying vascular comorbidities (Watson et al. 2009). It is uncertain if platelet activation might simply reflect the associated comorbidities with AF (e.g., hypertension and vascular disease) rather than be related to the prothrombotic state in AF per se. For example, Ferro et al. suggested that enhanced platelet activation might even play a role in clinical progression of AF because high soluble CD40L level was predictive for vascular events (stroke and myocardial infarction) in patients with AF (Ferro et al. 2007; Lip et al. 2007). In the Rotterdam Study, plasma-soluble P-selectin levels did predict clinical adverse outcomes in AF, suggesting a role of platelets in the prothrombotic state associated with this disorder (Heeringa et al. 2006). Also, platelet size, measured as mean platelet volume, has been associated with platelet reactivity and as an independent risk factor for future stroke and myocardial infarction.
Beta-thromboglobulin is a platelet-specific protein that indicates platelet activation and is released from alpha-granules during platelet aggregation and subsequent thrombus formation. In the SPAF III study have been shown that BTG levels were not predictive of thromboembolic events either when analyzed as a continuous variable or when those with BTG levels <42 ng/mL were compared with others (Feinberg et al. 1999).
Inflammation Biomarkers
C-reactive protein (CRP) is an established biomarker linked to inflammation and is predominantly synthesized in hepatocytes as an acute-phase reactant. CRP has been frequently studied in cardiovascular diseases and AF. In a small study, Conway et al. reported the association between CRP and a composite outcome of stroke and death in AF (Conway et al. 2004).
Interleukin-6 (IL-6) is circulating cytokine produced by monocytes, macrophages, T lymphocytes, and endothelial cells. IL-6 is the inflammation marker best related to AF that can induce a prothrombotic state (Kerr et al. 2001). Conway et al., based on a small study, reported the association between IL-6 and a composite outcome of stroke and death. Recently, our group showed that high IL6 and high TnT remained significantly associated with stroke/TIA or systemic embolic even after adjusting for CHADS2 score (17). Preliminary results from RE-LY biomarker substudy (Aulin et al. 2011) showed that in patients with top quartile levels compared with the bottom quartile, there was a doubling of stroke risk in adjusted analysis. These findings suggest that IL-6 may potentially be used to refine clinical risk stratification in AF.
Other Biomarkers
Adiponectin presents anti-inflammatory, atherogenic, and antihypertrophic functions, and both of them have been associated with multiple known risk factors for AF, including inflammation, diabetes, obesity, myocardial infarction, and incident heart failure (Rienstra et al. 2012). Hernández-Romero et al. found how low levels of adiponectin were independently associated with adverse cardiovascular events but only in female AF patients, and the lack of association in men could be because of testosterone decreasing adiponectin production (Hernández-Romero et al. 2013). These dates confirmed the importance of AF as a risk marker of atherosclerotic vascular damage, and adiponectin could exert a protective role against cardiovascular diseases.
Growth differentiation factor 15 (GDF-15) is a divergent member of the transforming growth factor-β family that can be secreted from a broad range of cells, for example, cytokine secreted from adipocytes and myocytes in response to, and may be protecting against, stress such as cellular ischemia and mechanical and oxidative stress. In the last months it has been described that the prognostic information provided by GDF-15 was independent of clinical characteristics and clinical risk scores (Wallentin et al. 2014). However, after adjustment for the other cardiac biomarkers, the prognostic value for stroke attenuated.
Mortality
Cardiac Troponins
These markers of myocardial injury and stress also play a relevant role in prediction of mortality in patients with AF. In routine daily practice, minor troponin elevation below the 99th percentile in patients with AF is attributed to the rapid or irregular ventricular response and does often not undergo stress testing and coronary angiography. Van der Bos demonstrated that troponin I release might detect additional or ongoing myocardial damage, ultimately leading to deterioration in cardiac function in patients hospitalized for atrial fibrillation, which constituted the first study that reported circulation troponin I levels were associated with mortality and major adverse cardiac events in AF (Van den Bos et al. 2011).
Later, in a substudy from the RE-LY trial, risk assessment for cardiovascular death was independently improved when troponin I was added to thromboembolic risk scores (Hijazi et al. 2012). These results were confirmed in the study by Roldán et al., in a stable and chronic anticoagulated AF cohort, whereby increased plasma troponin T levels were associated with an adverse prognosis in AF patients, with regard to cardiovascular events and mortality (Roldán et al. 2012). Recently, an ARISTOTLE substudy observed that the risk of cardiac death and myocardial infarction is highest in patients with increased concentrations of both troponins (Hijazi et al. 2014). Isolated increases of troponin I concentrations generally seemed to be associated with higher risk of cardiac death and myocardial infarction compared with isolated increases in troponin T (Hijazi et al. 2014). Despite the unknown exact underlying pathophysiological mechanism, as discussed above, therapies aimed at reducing ventricular rate, wall stress, or microperfusion might be useful to improve prognosis in the future.
Natriuretic Peptides
The role of natriuretic peptides as powerful prognostic markers for mortality was initially established in heart failure, thereafter in patients with acute coronary syndromes and later in stable coronary artery populations and in asymptomatic community-based elderly subjects (Frustaci et al. 1997).
In the RE-LY substudy (Hijazi et al. 2012), despite adjustment for known risk factors, the risk for cardiovascular mortality was fivefold higher in patients with the highest quartile levels of NT-proBNP in comparison with patients with normal NT-proBNP levels. Similar results have been shown in ARISTOTLE trial (Hijazi et al. 2014), which found improved risk stratification with NT-proBNP, doubling the risk of death. Thus, the addition of NT-proBNP to the risk stratification models resulted in significant improvements in the discrimination performance for mortality and cardiovascular events. Recently, our group showed NT-proBNP was also predictive of all-cause mortality, suggesting that this biomarker may potentially be used to refine clinical risk stratification in anticoagulated patients with AF (Roldán et al. 2014). So, NT-proBNP could give us valuable information about risk of death in patients with AF.
Renal Function Biomarkers
Renal impairment has been associated with an increased risk of death and adverse cardiovascular events in patients with coronary artery disease as well as in the general population (Go et al. 2004). Importantly, renal function may impair in AF patients; so, Roldán et al. showed a decreased eGFR >10 ml/min/1.73 m2 in 21 % of patients, with one fifth of followed-up patients developing severe CKD (<30 ml/min/1.73 m2) (Roldán et al. 2013). This study also demonstrated that the presence of impaired renal function was also associated consistently with the development of adverse cardiovascular events and mortality, even after adjusting for the CHADS2 score.
Cystatin C levels were independently associated with increased rates of major bleedings. The significance of cystatin C in AF population was recently reported on ARISTOTLE (Hohnloser et al. 2012) and RE-LY substudies.
On the other hand, BTP, a previously proposed as renal damage biomarker, could also be a predictor of mortality in patients with AF. Astor et al. compared the associations of BTP and other biomarkers with risks of mortality, coronary heart disease, heart failure, and chronic kidney disease and found higher BTP levels with decreasing eGFR and a significant P hazard ratio associated with the studied risk factors (Astor et al. 2012). In contrast, our results show how BTP levels are only slightly dependent upon renal function and, thus, justify the independent prognostic value of plasma BTP levels in patients with AF (Vílchez et al. 2013).
Inflammation Biomarkers
The prognostic value of CRP to all-cause mortality and a composite of ischemic stroke, myocardial infarction, or vascular death was displayed in a larger cohort based on the Stroke Prevention in Atrial Fibrillation III (trial) (Lip et al. 2007).
In a substudy of ARIC cohort, Hermida et al. (69) confirmed the results on hsCRP as a predictor of mortality with significant improvement on the CHA2DS2–VASc score by addition of this biomarker. Preliminary results from RE-LY biomarker substudy (Hijazi et al. 2012) showed that C-reactive protein quartile levels remained independently associated with cardiovascular mortality after multivariable adjustments.
Our group has demonstrated raised IL-6 levels in AF, which suggest the presence of an inflammatory state, although this fact appears to be related to clinical variables of the patients, rather than to the presence of AF per se. IL-6 provided prognostic information that was complementary to clinical risk scores for prediction of long-term cardiovascular events and death (Roldán et al. 2012). Thus, IL-6 was also independently and incrementally associated with cardiovascular mortality.
So, both inflammatory biomarkers, as CRP and IL-6, seem to be independent markers for mortality in patients with AF.
Growth Differentiation Factor 15
Plasma levels of GDF-15 are increased in response to inflammation and may be involved in maintaining the inflammatory activity. These experimental data and the results from this and other clinical studies suggest a link – protective or harmful – between GDF-15 and cellular stress as supported by the associations with age, diabetes mellitus, renal disease, smoking, congestive heart failure, and biomarkers of cardiac and renal dysfunction and inflammation. The understanding of the GDF-15 is limited because its receptor and the involved signaling pathways are unknown. Currently, the level of GDF-15 may be interpreted mainly as an integrative signal of severity of disease in several different pathological conditions.
The prognostic role of GDF-15 was presented as a substudy of the ARISTOTLE trial (64); GDF-15 was shown to be an additive prognostic marker for death, even after adjusting for clinical variables, risk factors, and CHA2DS2–VASc score and biomarkers (including troponin I, proBNP, cystatin C).
Major Bleeding
Cardiac Troponin
Various studies in acute coronary syndrome populations linking peak troponin I levels to subsequent increase bleeding rate. The Randomized Evaluation of Long-Term Anticoagulation Therapy (RE-LY) substudy also documents an association between elevated troponin I levels and risk of major bleeding (Hijazi et al. 2012). The causality is unknown, but elevated troponin I levels might contribute to the identification of a more fragile AF subpopulation more likely to bleed during anticoagulation.
On the other hand, isolated increases of troponin T displayed a stronger association with major bleeding events according to International Society on Thrombosis and Hemostasis criteria (Hijazi et al. 2014).
Natriuretic Peptides
Several studies (Hijazi et al. 2012, 2013) showed that there was no significant association between NT-proBNP levels and major bleeding. Higher baseline NT-proBNP concentration was strongly associated with each of the major clinical outcomes explored (like stroke or mortality), except major bleeding, even after adjustment for multivariable model.
Renal Function Biomarkers in AF
Major bleeding constitutes a major problem as patients with renal dysfunction currently tend to be undertreated with oral anticoagulation therapy due to the associated higher bleeding risk especially when treaded with vitamin K antagonist therapy (Piccini et al. 2009).
Renal dysfunction has been associated with an increased risk of bleeding (Hijazi et al. 2014; Santopinto et al. 2003); the incidence of major bleeding increased significantly with the impair of renal function. The association of a low eGFR and bleeding events was not surprising, and several studies have reported an association between a low GFR and a significantly increased risk of bleeding in patients with AF taking oral anticoagulation. Thus, renal impairment is an established risk factor for bleeding and has been included in the HAS-BLED bleeding score. Renal dysfunction may be associated with labile international normalized ratio (INR) and worse the average percentage of the time in the optimal therapeutic INR (TTR).
Cystatin C has also been studied related to risk of bleeding in the study by Hohnloser et al. (2012). They showed that high levels of cystatin C, when added to the eGFR equation, were associated with increased HR rates of major bleeding in patients taking warfarin. Although cystatin C achieved improved stroke risk stratification, creatinine-based estimates of renal function were better indicators of the risk of bleeding during OAC treatment in the ARISTOTLE study (Hijazi et al. 2014).
BTP also improved the predictive value of the HAS-BLED score for major bleeding. Of note, a recent analysis showed that the HAS-BLED score has already been shown to perform as well as a multivariate model for predicting major bleeding in patients with AF receiving anticoagulation treatment (Vílchez et al. 2013).
Endothelial Damage Biomarkers
High plasma vWF levels were also an independent predictor of major bleeding in anticoagulated permanent AF patients. These data were confirmed by Roldan et al. whereby an increased plasma vWF levels were associated major bleeding (Roldán et al. 2011). A high plasma vWF level showed an additive effect on the HAS-BLED score, for an intermediate-risk category for bleeding (HAS-BLED score 1–2 points), so that high plasma vWF levels changed the annual risk of a hemorrhagic event from 1.2 % (base on clinical criteria) to 4.7 %.
Thrombogenesis Biomarkers in AF
DD levels at baseline, regardless OAC, were related to major bleeding. These results were confirmed in the RE-LY or ARISTOTLE biomarker substudies, which described an association between DD levels and the risk of major bleeding outcome independent of established risk factors including the CHADS2 variables.
Growth Differentiation Factor 15
In a new study published in Circulation, GDF-15 was shown to be an additive prognostic marker for major bleeding in patients with AF receiving oral anticoagulation (Wallentin et al. 2014). The prognostic value for major bleeding remained even in the presence of NT-proBNP and high-sensitivity troponin I.
In this moment, there are no studies that show significant association between circulating adiponectin levels and major bleeding.
Potential Applications to Prognosis, Other Diseases, or Conditions
Several risk stratification scores have been developed to aid decision-making for thromboprophylaxis, which are currently in use and have limited capacity for prediction of thromboembolic events with low values for area under the receiver operating characteristic curve, known as c-statistic. The identification of new biomarkers could, therefore, provide an established clinical risk score like the CHA2DS2–VASc score with complementary prognostic information. However, the biomarker should not be expected to improve the identification of those patients with AF who will benefit from OAC. Biomarkers might be helpful in calculating the risk of major bleeding, by providing information on how to select patients who will derive the most benefit from reducing the composite end point, which includes both embolic and bleeding episodes. Tailoring different antithrombotic options to individuals based on biomarker expression has not been explored in patients with AF, but could be an interesting hypothesis for future trials (Marín et al. 2015). In Fig. 2 we may observe the past, present, and future role of biomarkers in AF.
Although several studies have demonstrated the usefulness of adding blood biomarkers to established clinical risk scores , the application of this approach to the daily clinical practice still remains uncertain. Indeed, some evidence for these biomarkers has been obtained from recent anticoagulation trials (which often have specific inclusion/exclusion criteria, leading to a selected trial cohort being studied), though the evidence for additive value of biomarkers from large non-anticoagulated “real-world” cohorts is more limited.
Summary Points
-
This chapter focuses on the biomarkers in relation to atrial fibrillation.
-
Atrial fibrillation is the most common sustained cardiac arrhythmia which is associated with high risk of stroke, thromboembolism, and mortality.
-
The prevalence AF increases with age. It is projected to increase in the coming decades.
-
The underlying mechanisms behind AF describe multiple pathological states leading to various remodeling processes in atrial myocardium.
-
The use of OAC significantly reduces the risk of stroke, thromboembolism, and all-cause mortality.
-
Improved diagnostic techniques have identified various biomarkers that might play an important role in prediction of AF and related outcomes (stroke, thromboembolism, and mortality).
-
The ideal biomarker should be easily obtained with minimum discomfort or risk to the patient, may also appear or disappear over the course of disease progression, and may thus be useful in determining the prognosis of a disease within an individual.
-
This would offer opportunities for personalized medicine and focused therapeutic approaches.
Abbreviations
- AF:
-
Atrial fibrillation
- ARISTOTLE trial:
-
Apixaban for the Prevention of Stroke in Subjects with Atrial Fibrillation trial
- ATM:
-
Antithrombin III
- BNP:
-
B-type natriuretic peptide
- BTG:
-
Beta-thromboglobulin
- BTP:
-
Beta-trace protein
- CKD:
-
Chronic kidney disease
- CRP:
-
C-reactive protein
- DD:
-
D-dimer
- F1+2:
-
Prothrombin fragment 1+2
- FMD:
-
Flow-mediated dilatation
- GDF-15:
-
Growth differentiation factor 15
- GFR:
-
Glomerular filtration rate
- IL-6:
-
Interleukin-6
- INR:
-
International normalized ratio
- LV:
-
Left ventricle
- NT-proBNP:
-
The inactive N-terminal fragment of B-type natriuretic peptide
- OAC:
-
Oral anticoagulation
- PAI-1:
-
Plasminogen activator inhibitor
- PAP complexes:
-
Plasmin–antiplasmin complexes
- RE-LY trial:
-
Randomized Evaluation of Long-Term Anticoagulant Therapy trial
- sE-sel:
-
Soluble E-selectin
- SPAF III study:
-
The third Stroke Prevention in Atrial Fibrillation study
- sTM:
-
Soluble thrombomodulin
- TIA:
-
Transient ischemic attack
- TnI:
-
Troponin I
- TnT:
-
Troponin T
- tPA:
-
Tissue plasminogen activator
- vWF:
-
von Willebrand factor
References
Abrahamson M, Olafsson I, Palsdottir A, Ulvsback M, Lundwall A, Jensson O, Grubb A. Structure and expression of the human cystatin C gene. Biochem J. 1990;268:287–94.
Ananthapanyasut W, Napan S, Rudolph EH, Harindhanavudhi T, Ayash H, Guglielmi KE, Lerma EV. Prevalence of atrial fibrillation and its predictors in non-dialysis patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5:173–81.
Asakura H, Hifumi S, Jokaji H, Saito M, kumabashiri Uotani C, Morishita E, Yamakazi M, Shibata K, Mizuhashi K. Prothrombin fragment F1+2 and thrombin-antithrombin III complex are useful markers of the hypercoagulable state in atrial fibrillation. Blood Coagul Fibrinolysis. 1992;3:469–73.
Astor BC, Shafi T, Hoogeveen RC, et al. Novel markers of kidney function as predictors of ESRD, cardiovascular disease, and mortality in the general population. Am J Kidney Dis. 2012;59(5):653–62.
Aulin JKEM, Andersson U, Connolly SJ, Huber K, Reilly PA, Siegbahn A, Wallentin L, Yusuf S, Oldgren J. Interleukin-6 and C-reactive protein and risk for death and cardiovascular events in patients with atrial fibrillation. J Am Coll Cardiol. 2011;57:E91.
Benjamin EJ, Wolf PA, D’ Agostino RB, Silbershatz H, Kannel WB, Levy D. Impact of atrial fibrillation on the risk of death. The Framingham Heart Study. Circulation. 1998;98:946–52.
Boomsma F, van den Meiracker AH. Plasma A- and B-type natriuretic peptides: physiology, methodology and clinical use. Cardiovasc Res. 2001;51:442–9.
Camm JA, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, Gerhard Hindricks G, Kirchhof P. Focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation – developed with the special contribution of the European Heart Rhythm Association. Europace. 2012;14(10):1385–413.
Conway DS, Buggins P, Hughes E, Lip GY. Prognostic significance of raised plasma levels of interleukin-6 and C-reactive protein in atrial fibrillation. Am Heart J. 2004;148(3):462–6.
Craig T, January L, Wann S, et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol. 2014;64(21):2246–80.
Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007;50:2357–68.
Daoud EG, Bogun F, Goyal R, Harvey M, Man KC, Strickberger SA, et al. Effect of atrial fibrillation on atrial refractoriness in humans. Circulation. 1996;94(7):1600–6.
Deo R, Katz R, Kestenbaum B, Fried L, Sarnak MJ, Psaty BM, Siscovick DS, Shlipak MG. Impaired kidney function and atrial fibrillation in elderly subjects. J Card Fail. 2010;16:55–60.
Dubin R, Cushman M, Folsom AR, Fried LF, Palmas W, Peralta CA, Wassel C, Shlipak MG. Kidney function and multiplate hemostatic markers: cross sectional associations in the multi-ethnic study of atherosclerosis. BMC Nephrol. 2011;12:3.
Eikelboom J, Hijazi Z, Oldgren J, Andersson U, Connolly SJ, Ezekowitz MD, Reilly PA, Yusuf S, Wallentin L, Siegbahn A. D-dimer is prognostic for stroke, major bleeding and death during anticoagulation of atrial fibrillation-a RELY substudy. Circulation. 2010;122:A18321.
Ellinor PT, Low AF, Patton KK, Shea MA, Macrae CA. Discordant atrial natriuretic peptide and brain natriuretic peptide levels in lone atrial fibrillation. J Am Coll Cardiol. 2005;45:82–6.
Feinberg WM, Pearce LA, Hart RG, Cushman M, Cornell ES, Lip GY, Bovill EG. Markers of thrombin and platelet activity in patients with atrial fibrillation. Stroke. 1999a;30:2547–53.
Feinberg WM, Pearce LA, Hart RG, Cushman M, Cornell ES, Lip GY, Bovill EG. Markers of thrombin and platelet activity in patients with atrial fibrillation: correlation with stroke among 1531 participants in the stroke prevention in atrial fibrillation III study. Stroke. 1999b;30(12):2547–53.
Ferro D, Loffredo L, Polimeni L, et al. Soluble CD40 ligand predicts ischemic stroke and myocardial infarction in patients with nonvalvular atrial fibrillation. Arterioscler Thromb Vasc Biol. 2007;27:2763–8.
Fonarow GC, Peacock WF, Phillips CO, Givertz MM, Lopatin M. Admission B-type natriuretic peptide levels and in-hospital mortality in acute decompensated heart failure. J Am Coll Cardiol. 2007;49:1943–50.
Freestone B, Chong AY, Blann AD, Lip GY. The effects of direct current cardioversion for persistent atrial fibrillation on indices of endothelial damage/dysfunction. Thromb Res. 2006;118:479–85.
Freestone B, Chong AY, Nuttall S, Blann AD, Lip GY. Soluble E-selectin, von Willebrand factor, soluble thrombomodulin, and total body nitrate/nitrite product as indices of endothelial damage/dysfunction in paroxysmal, persistent, and permanent atrial fibrillation. Chest. 2007;132(4):1253–8.
Freestone B, Chong AY, Nutall S, Lip GY. Impaired flow mediated dilatation as evidence of endothelial dysfunction in chronic atrial fibrillation: relationship to plasma von Willebrand factor and soluble E-selectin levels. Thromb Res. 2008;122(1):85–90.
Frustaci A, Chimenti C, Belocci F, Morgante E, Russo MA, Maseri A. Histological substrate of atrial biopsies in patients with lone atrial fibrillation. Circulation. 1997;96:1180–4.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risk of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305.
Go AS, Fang MC, Udaltsova N, Chang Y, Pomernacki NK, Borowsky L, Singer DE. Impact of proteinuria and glomerular filtration rate on risk of thromboembolism in atrial fibrillation (ATRIA) study. Circulation. 2009;119:1363–9.
Goodsaid F, Frueh F. Biomarker qualification pilot process at the US Food and Drug Administration. AAPS J. 2007;9(1):E105–8.
Heeringa J, Conway DS, van der Kuip DA, et al. A longitudinal population-based study of prothrombotic factors in elderly subjects with atrial fibrillation: the Rotterdam study 1990–1999. J Thromb Haemost. 2006;4:1944–9.
Hermida J, Lopez FL, Montes R, Matsushita K, Astor BC, Alonso A. Usefulness of high sensitivity C reactive protein to predict mortality in patients with atrial fibrillation (from the Atherosclerosis Risk in Communities, ARIC, Study). Am J Cardiol. 2012;109(1):95–9.
Hernández Romero D, Jover E, Marín F, Vilchez JA, Manzando-Fernández S, Romera M, et al. The prognostic role of the adiponectin levels in atrial fibrillation. Eur J Clin Invest. 2013;43(2):168–73.
Hijazi Z, Oldgren J, Andersson U, Connolly SJ, Ezekowitz MD, Hohnloser SH, Reilly PA, Vinereanu D, Siegbahn A, Yusuf S, Wallentin L. Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a randomized evaluation of long-term anticoagulation therapy (RE-LY) substudy. Circulation. 2012;125:1605–16.
Hijazi Z, Oldgren J, Siegbahn A, Granger CB, Wallentin L. Biomarkers in atrial fibrillation: a clinical review. Eur Heart J. 2013a;34(20):1475–80.
Hijazi Z, Wallentin L, Siegbahn A, Andersson U, Christersson C, Ekekowitz J, et al. N-terminal pro-B-type natriuretic peptide for risk assessment in patients with atrial fibrillation: insights form ARISTOTLE trial. J Am Coll Cardiol. 2013b;61(22):2274–84.
Hijazi Z, Walletin L, Siegbahn A, Schollin M, Andersson U, Alexander JH, et al. High-sensitivity troponin T and risk stratification in patients with atrial fibrillation during treatment with apixaban or warfarin (ARISTOTLE). J Am Coll Cardiol. 2014a;63(1):52–61.
Hijazi Z, Siegbahn A, Andersson U, Lindahl B, Granger CB, et al. Comparison of cardiac troponins I and T measured with high-sensitivity methods for evaluation of prognosis in atrial fibrillation: an ARISTOTLE substudy. Clin Chem. 2014b;61:2.
Hoffmann A, Conradt HS, Gross G, Nimtz M, Lottspeich F, Wurster U. Purification and chemical characterization of beta-trace protein from human cerebrospinal fluid: its identification as prostaglandin D synthase. J Neurochem. 1993;61(2):451–6.
Hohnloser SH, Hijazi Z, Thomas L, Alexander JH, Amerena J, Hanna M, Keltai M, Lanas F, Lopes RD, Lopez-Sendon J, Granger CB, Wallentin L. Efficacy of apixaban when compared with warfarin in relation to renal function in patients with atrial fibrillation: insights from the ARISTOTLE trial. Eur Heart J. 2012;33:2821–22830.
Igarashi Y, Kashimura K, Makiyama Y, Sato T, Ojima K, Aizawa Y. Left atrial appendage dysfunction in chronic nonvalvular atrial fibrillation is significantly associated with an elevated level of brain natriuretic peptide and a prothrombotic state. Jpn Circ J. 2001;65:788–92.
Ix JH, Shlipak MG, Chertow GM, Whooley MA. Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: data from the Heart and Soul Study. Circulation. 2007;115:173–9.
Kerr R, Stirling D, Ludlam CA. Interleukin 6 and haemostasis. Br J Haematol. 2001;115(1):3–12.
Krishnamoorthy S, Khoo CW, Lim HS, Lane DA, Pignatelli P, Basili S, Violi F, Lip GY. Prognostic role of plasma von Willebrand factor and soluble E-selectin levels for future cardiovascular events in a ‘real-world’ community cohort of patients with atrial fibrillation. Eur J Clin Invest. 2013;43(10):1032–8.
Laterza OF, Price CP, Scott MG. Cystatin C: an improved estimator of glomerular filtration rate? Clin Chem. 2002;48:699–707.
Lip GY, Lane D, Van WC, Hart RG. Additive role of plasma von Willebrand factor levels to clinical factors risk stratification of patients with atrial fibrillation. Stroke. 2006;37(9):2294–300.
Lip GY, Patel JV, Hughes E, Hart RG. High-sensitivity C-reactive protein and soluble CD40 ligand as indices of inflammation and platelet activation in 880 patients with nonvalvular atrial fibrillation: relationship to stroke risk factors, stroke risk stratification schema, and prognosis. Stroke. 2007;38(4):1229–37. Epub 2007 Mar 1.
Lip GY, Andreotti F, Fauchier L, Huber K, Hylek E, Knight E, et al. Bleeding risk assessment and management in atrial fibrillation patients. Executive summary of a position document from the European Heart Rhythm Association (EHRA), endorsed by the European Society of Cardiology (ESC) working group on thrombosis. Thromb Haemost. 2011;106(6):997–1011.
López-Cuenca A, Marín F, Roldán V, González-Conejero R, Hernández- Romero D, Valdés M, Lip GY. Genetic polymorphisms and atrial fibrillation: insights into the prothrombotic state and thromboembolic risk. Ann Med. 2010;42(8):562–75.
Marín F, Roldán V. GDF-15 and risk stratification in atrial fibrillation. Nat Rev Cardiol. 2015;12:8–9.
Newman DJ, Thakkar H, Edwards RG, Wilkie M, White T, Grubb AO, Price CP. Serum Cystatin C measured by automated immunoassay: a more sensitive marker of changes in GFR than serum creatinine. Kidney Int. 1995;47:312–8.
Okada Y, Shibazaki K, Kimura K, et al. Brain natriuretic peptide is a marker associated with thrombus in stroke patients with atrial fibrillation. J Neurol Sci. 2011;301:86–9.
Piccini JP, Hernandez AF, Zhao X, Patel MR, Lewis WR, Peterson ED, Fonarow GC. Quality of care for atrial fibrillation among patients hospitalized for heart failure. J Am Coll Cardiol. 2009;54:1280–9.
Pisters R, Lane DA, de Vos Nieuwlaat CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138(5):1093–100.
Providencia R, Paiva L, Barra S. Risk stratification of patients with atrial fibrillation biomarkers and other future perspectives. World J Cardiol. 2012;4(6):195–200.
Rienstra M, Sun JX, Lubitz SA, Frankel DS, Vasan RS, Levy D, et al. Plasma resistin, adiponectin, and risk of incident atrial fibrillation: the Framingham Offspring Study. Am Heart J. 2012;163(1):119–24.
Roldán V, Marín F, Marco P, Martínez JG, Calatayud R, Sogorb F. Hypofibrinolysis in atrial fibrillation. Am Heart J. 1998;136(6):956–60.
Roldán V, Marín F, García-Herola A, Lip G. Correlation of plasma von Willebrand factor levels, an index of endothelial damage/dysfunction, with two point-based stroke risk stratification scores in atrial fibrillation. Thromb Res. 2005;116(4):321–5.
Roldán V, Marín F, Muiña B, Torregrosa JM, Hernández-Romero D, et al. Plasma von Willebrand factor levels are an independent risk factor for adverse events including mortality and major bleeding in anticoagulated atrial fibrillation patients. J Am Coll Cardiol. 2011;57(25):2496–504.
Roldán V, Marín F, Diaz J, Gallego P, Jover E, Romera M, et al. High sensitivity cardiac troponin T and interleukin-6 predict adverse cardiovascular events and mortality in anticoagulated patients with atrial fibrillation. J Thromb Haemost. 2012;10(8):1500–7.
Roldán V, Marín F, Manzano-Fernández S, Fernández H, Gallego P, Valdés M, et al. Does chronic kidney disease improve the predictive value of CHADS2 and CHA2DS2-VASc stroke stratification risk scores for atrial fibrillation? Thromb Haemost. 2013a;109(5):956–60.
Roldán V, Marín F, Fernández H, Manzano-Fernández S, Gallego P, Valdés M, et al. Renal impairment in a “real-life” cohort of anticoagulated patients with atrial fibrillation (implications for thromboembolism and bleeding). Am J Cardiol. 2013b;111(8):1159–64.
Roldán V, Vílchez JA, Manzano-Fernández S, Jover E, Gálvez J, Puche CM, Valdés M, et al. Usefulness of N-terminal pro–B-type natriuretic peptide levels for stroke risk prediction in anticoagulated patients with atrial fibrillation. Stroke. 2014;45(3):696–701.
Santopinto JJ, Fox KA, Goldberg RJ, Budaj A, Pinero G, Avezum A, Gulba D, Esteban J, Gore JM, Johnson J, Gurfinkel EP. Creatinine clearance and adverse hospital outcomes in patients with acute coronary events (GRACE). Heart. 2003;89:1003–8.
Savelieva I, John Camm A. Atrial fibrillation and heart failure: natural history and pharmacological treatment. Europace. 2004;5 Suppl 1:S5–19.
Shelton RJ, Clark AL, Goode K, Rigby AS, Cleland JG. The diagnostic utility of N-terminal pro-B-type natriuretic peptide for the detection of major structural heart disease in patients with atrial fibrillation. Eur Heart J. 2006;27:2353–61.
Singer DE, Chang Y, Fang MC, Borowsky LH, Pomenarcki NK, Udaltasova N, et al. Should patient characteristics influence target anticoagulation intensity for stroke prevention in nonvalvular atrial fibrillation? The ATRIA study. Circ Cardiovasc Qual Outcome. 2009;2(4):297–304.
Van den Bos EJ, Constantinescu AA, van Domburg RT, Akin S, Jordaens LJ, Kofflard MJ. Minor elevations in troponin I are associated with mortality and adverse cardiac events in patients with atrial fibrillation. Eur Heart J. 2011;32(5):611–7.
Vene N, Mavri A, Kosmelj K, Stegnar M. High D-dimer levels predict cardiovascular events in patients with chronic atrial fibrillation during oral anticoagulant therapy. Thromb Haemost. 2003;90(6):1163–72.
Vílchez JA, Roldán V, Manzano-Fernández S, Fernández H, Avilés-Plaza F, et al. β-Trace protein and prognosis in patients with atrial fibrillation receiving anticoagulation treatment. Chest. 2013;144(5):1564–70.
Vilchez JA, Roldan V, Hernandez-Romero D, Valdes M, Lip GY, Marin F. Biomarkers in atrial fibrillation: an overview. Int J Clin Pract. 2014;68:434–43.
Wallentin L, et al. Growth differentiation factor 15, a marker of oxidative stress and inflammation, for risk assessment in patients with atrial fibrillation: insights from ARISTOTLE trial. Circulation. 2014;130(21):1847–58.
Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet. 2009;373(9658):155–66.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
Rodríguez-Serrano, A.I., Esteve-Pastor, M.A., Hernández-Romero, D., Valdés, M., Roldán, V., Marín, F. (2016). New Role of Biomarkers in Atrial Fibrillation. In: Patel, V., Preedy, V. (eds) Biomarkers in Cardiovascular Disease. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7678-4_36
Download citation
DOI: https://doi.org/10.1007/978-94-007-7678-4_36
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7677-7
Online ISBN: 978-94-007-7678-4
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences