Abstract
Epicardial adipose tissue is the visceral fat depot of the heart with unique anatomical and functional properties. Epicardial fat can be considered a novel biomarker of cardiovascular disease. Its thickness can be visualized and measured using standard two-dimensional echocardiography with several advantages, including its low cost, easy accessibility, and good reproducibility. Echocardiographic epicardial fat thickness reflects the intra-abdominal visceral fat and intramyocardial fat accumulation. Epicardial fat thickness is related to traditional and novel cardiovascular risk factors. Epicardial fat thickness correlates and predicts the risk of metabolic syndrome. Epicardial fat has been associated with the presence and severity of coronary artery disease, independent of traditional cardiometabolic risk factor and coronary calcification. Given its rapid metabolism and its simple objective measurability, epicardial fat can serve as target for pharmaceutical agents targeting the adipose tissue.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Key Facts of Epicardial Fat
-
Epicardial fat is the visceral fat depot of the heart with unique features.
-
Epicardial fat has physiological and pathological properties.
-
Epicardial fat can be easily measured with imaging techniques.
-
Epicardial fat is a marker of visceral fat and cardiovascular risk.
-
Epicardial fat thickness is a therapeutic target.
Introduction
Human body fat is functionally heterogeneous and not equally distributed. Local fat accumulation seems to be more important than overall body fat. If increased visceral fat is considered a major determinant of a poor cardiometabolic profile, the excessive intraorgan fat is recently thought to play a key role in cardiovascular diseases. Consistently with the emerging concept of organ-specific adiposity, I focused my attention on the epicardial fat, the visceral fat depot of the heart.
Anatomy and Embryology of the Epicardial Fat
The adipose tissue of the heart is divided into two layers: epicardial fat, the visceral layer, and pericardial fat, situated externally to the parietal layer of the pericardium (Iacobellis 2005, 2009). Epicardial and intra-abdominal fat evolve from brown adipose tissue during embryogenesis (Marchington et al. 1989). Epicardial fat is supplied by branches of the coronary arteries. In the adult human heart, epicardial fat is commonly found in the atrioventricular and interventricular grooves. As the amount of epicardial fat increases, it progressively fills the space between the ventricles, sometimes covering the entire epicardial surface. Notably, no muscle fascia divides epicardial fat and myocardium; therefore, the two tissues share the same microcirculation (Iacobellis 2005). This allows the hypothesis of a direct interaction between the epicardial fat and the myocardium.
Physiological and Biochemical Properties of the Epicardial Fat
A dichotomous role, both unfavorable and protective, has been attributed to epicardial fat, but its physiology in animals and humans is not completely clear (Iacobellis 2011).
Under normal physiological conditions epicardial fat could therefore serve several distinct functions – as a buffer, absorbing fatty acids and protecting the heart against high fatty acid levels, as a lipid storage and local energy source at times of high demand, channeling fatty acids to the myocardium, and perhaps as brown fat to defend the myocardium against hypothermia (Marchington and Pond 1990; Sacks et al. 2009; Pezeshkian et al. 2009). The brown fat properties of the epicardial fat are not fully elucidated and object of recent investigations (Sacks et al. 2013). Under pathological circumstances epicardial fat releases factors that promote harmful coronary artery and myocardial changes. A body of evidence shows that epicardial fat is an extremely active organ that produces several bioactive adipokines with both proinflammatory and anti-inflammatory properties (Mazurek et al. 2003). Nevertheless, what could influence this equilibrium between harmful and possible protective effects is still unknown. Because of its anatomical proximity to the heart and the absence of fascial boundaries, epicardial adipose tissue may interact locally and modulate the myocardium and coronary arteries through paracrine or vasocrine secretion of proinflammatory adipokines (Iacobellis 2011; Sacks 2007) (Fig. 1).
Paracrine pathological effects of epicardial fat. Under pathological conditions epicardial adipose tissue (EAT) can locally affect myocardium and coronary arteries by a complex interplay of mechanisms. EAT displays a dense inflammatory infiltrate, mainly represented by macrophages. Both macrophages and EAT adipocytes can release pro-inflammatory and atherogenic cytokines, such as Tumor Necrosis Factor-alpha (TNF-a), Interleukin 1 and 6 (IL1, IL6) and Monocyte Chemoattractant Protein-1 (MCP-1), regulated upon activation t-cell and secreted (RANTES) and soluble intercellular adhesion molecule (ICAM). Increased EAT reactive oxygen species (ROS) also contribute to activate inflammatory signals. EAT Type II secretory phospholipase A2 (sPLA2-II) secretion facilitates lipid accumulation within the atherosclerotic plaque. A local insulin resistance status is also due to the lower EAT glucose transporter-4 (GLUT4) expression. EAT also affect local coagulation and hemostasis by expressing tissue plasminogen activator (PLAT) and other coagulation factors
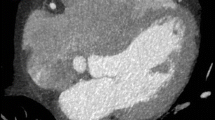
Echocardiographic epicardial fat thickness. Epicardial fat (epi fat) is generally identified as the echo-free space between the outer wall of the myocardium and the visceral layer of pericardium and its thickness is measured perpendicularly on the free wall of the right ventricle at end-systole in three cardiac cycles from the parasternal long axis view, as first proposed by Iacobellis
Echocardiographic Epicardial Fat Thickness
Epicardial fat thickness can be visualized and measured with two-dimensional guided M-mode echocardiography using commercially available equipments, as first proposed and validated by Iacobellis (Iacobellis 2003, 2009) (Fig. 3). Standard parasternal long- and short-axis views permit the most accurate measurement of epicardial fat thickness on the right ventricle. Echocardiographically, epicardial fat is generally identified as the echo-free space between the outer wall of the myocardium and the visceral layer of pericardium and its thickness is measured perpendicularly on the free wall of the right ventricle at end-systole in three cardiac cycles. The majority of population-based clinical studies have reported excellent interobserver and intraobserver agreement on epicardial fat thickness measurement. Echocardiographic epicardial fat thickness range varies from a minimum of 1 mm to a maximum measured value of almost 25 mm. The wide range of epicardial fat thickness likely reflects the substantial variation in abdominal visceral fat distribution (Iacobellis 2003).
Epicardial Fat Is a New Marker of Visceral Fat
Echocardiographic epicardial fat is a marker of visceral fat . In fact, echocardiographic epicardial fat strongly reflects the intra-abdominal visceral fat as measured by magnetic resonance imaging and better than waist circumference does (Iacobellis 2003; Iacobellis 2003). In a multiple regression analysis that included waist circumference and epicardial fat thickness, intra-abdominal visceral fat was better and independently predicted by the epicardial fat thickness (Iacobellis 2003) (Fig. 2).
Epicardial fat as new cardiovascular risk factor. Individuals with excessive intra-abdominal fat accumulation, such as the one depicted here, have large epicardial adipose tissue, as shown in this cardiac surgery picture, and higher risk of developing cardiovascular diseases and major cardiovascular events
Echocardiographic epicardial fat thickness as therapeutic target. Echocardiographic epicardial fat can serve as marker of visceral fat changes during pharmaceutical or lifestyle interventions targeting the adipose tissue. These images show a significant and rapid decrease of epicardial fat thickness, within the yellow line, after a 3-month very low calorie diet program.
Bland test confirmed the good agreement between the two methods. Other studies confirmed this finding in different populations. Echocardiographic epicardial fat thickness is therefore an independent predictor of visceral adiposity and weakly reflects the obesity degree. Subjects with higher waist circumference clearly show higher epicardial fat thickness, as previously reported. Recent evidences showed that obesity leads not only to increased fat depots in classical adipose tissue locations but also to significant lipid accumulation and infiltration within and around other tissues and internal organs (Iozzo 2011, Kankaanpää et al. 2006). Ectopic fat deposition may occur within the heart and affect cardiovascular function. Myocardial lipid content increases with the degree of adiposity and may contribute to the adverse structural and functional cardiac adaptations seen in obese persons. Echocardiographic epicardial fat is associated with intramyocardial and intrahepatic fat accumulation, as measured by proton magnetic resonance spectroscopy, Malavazos et al. 2010.
Epicardial Fat Is a New Cardiovascular Risk Factor
An escalating number of evidences indicate that epicardial fat measurement may play a role in the stratification and prediction of the cardiometabolic risk. Several clinical studies showed that epicardial fat thickness is also related to traditional and novel cardiovascular risk factors. Epicardial fat thickness is significantly higher in subjects with metabolic syndrome than in those without (Iacobellis 2008; Pierdomenico et al. 2012). When cardiometabolic parameters are considered separately, epicardial fat is independently associated with inflammatory markers, fatty liver, and liver enzymes. A recent meta-analysis reported a significant variability of epicardial fat with ethnicity, with a greater difference in Caucasian subjects than in other ethnic groups, Pierdomenico et al. 2012. Different cutoff points of high-risk epicardial fat thickness for the prediction of metabolic syndrome have been proposed (Iacobellis 2008).
Epicardial fat has been associated with the presence and severity of coronary artery disease in a large number of studies. Epicardial fat contributes to the development and progression of atherosclerosis, independent of traditional cardiometabolic risk factors (Iacobellis 2011) (Fig. 4). The relationship of epicardial fat thickness and coronary artery disease is driven by local mechanisms and is not fully explained by the concurrence of excess visceral fat accumulation or obesity in general. The association of epicardial fat with the risk of coronary artery disease seems to be independent also of coronary calcification. However, further studies to better explain the role of epicardial fat in coronary artery disease would be desirable. Epicardial fat has been also associated with markers of subclinical atherosclerosis, such as carotid intima media thickness, in high-risk individuals. Epicardial fat thickness is also associated with diabetes and insulin resistance in diabetics and no diabetic subjects (Iacobellis 2003, 2008; Momesso et al. 2011). Interestingly, echocardiographic epicardial fat has been reported as the best predictor of ultrasound measured liver steatosis.
Epicardial Fat and Heart Morphology and Function
Increased epicardial fat thickness is related with increased left ventricular mass and abnormal right ventricle geometry, as detected by echocardiography (Iacobellis et al. 2004; Iacobellis 2009). Echocardiographic findings are in agreement with autoptic studies. Mechanical and biomolecular mechanisms have been evoked to explain these correlations. Increased epicardial fat by adding to the mass of the ventricles may increase the work of pumping. Increased left ventricular mass in morbidly obese subjects could be due to a direct effect of excess epicardial fat. Increase in epicardial fat thickness is also significantly correlated with enlarged atria and impaired right and left ventricular diastolic filling in morbidly obese subjects. Epicardial fat may directly contribute to impair diastolic function in subjects with increased visceral adiposity. A mechanical obstacle to diastolic filling due to the excess epicardial fat pad could explain these findings.
Epicardial Fat as New Therapeutic Target
Interestingly, echocardiographic epicardial fat has been reported to significantly and quickly decrease after a very low-calorie diet and bariatric surgery in morbidly obese subjects (Iacobellis 2009; Willens et al. 2007) (Fig. 5). Changes in epicardial fat thickness were significantly higher than changes in BMI and waist circumference after the very low-calorie diet program. Changes in epicardial fat thickness were consensually and independently associated with the improvement in cardiac parameters in these subjects. Given its rapid metabolism and its simple objective measurability, epicardial fat can serve as target for pharmaceutical agents targeting the adipose tissue, such as statins, oral and injectable antidiabetes medications (Alexopoulos et al. 2013; Kim et al. 2009; Park et al. 2010) (Fig. 6). Future studies in this direction are warranted.
Epicardial fat as target of drugs modulating the fat. Given its rapid metabolism and rapid changes, epicardial adipose tissue (EAT) is a therapeutic target of medications targeting the fat, such statins, thiazolidinediones (TZDs), dipeptidyl peptidase-4 (DPP4) inhibitors, recombinant growth hormone (rGH), and potentially of glucagon like peptide-1 (GLP-1) analogs and thyroid hormones. These drugs can modulate EAT, reduce its thickness or volume and restore its physiological role
Potential Applications
Epicardial fat is an emerging biomarker of visceral adiposity and cardiovascular risk. Its simple and readily available measurement provides both clinician and researcher with a new diagnostic tool. The potential of modulating the epicardial fat to its physiological functions with targeted pharmacological agents can open new avenues in the pharmacotherapy of cardiometabolic diseases.
Summary Points
-
Epicardial fat plays a role in the development and progression of cardiometabolic diseases.
-
Epicardial fat and its secretosome display local and systemic effects.
-
Epicardial fat can be easily measured with imaging procedures, such as echocardiography, magnetic resonance, and computed tomography.
-
Epicardial fat assessment is an additional tool for the cardiovascular risk stratification and prediction.
-
Epicardial fat measurement can serve as therapeutic target during weight loss and pharmacological interventions targeting the adipose tissue.
References
Alexopoulos N, Melek BH, Arepalli CD, et al. Effect of intensive versus moderate lipid-lowering therapy on epicardial adipose tissue in hyperlipidemic post-menopausal women: a substudy of the BELLES trial (Beyond Endorsed Lipid Lowering with EBT Scanning). J Am Coll Cardiol. 2013;61:1956–61.
Iacobellis G. Relation of epicardial fat thickness to right ventricular cavity size in obese subjects. Am J Cardiol. 2009a;104:1601–2.
Iacobellis G. Epicardial and pericardial fat: close, but very different. Obesity. 2009b;17:625.
Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab. 2011;22:450–7.
Iacobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab. 2005;90:6300–2.
Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009;22:1311–9.
Iacobellis G, Ribaudo MC, Assael F, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003a;388:5163–8.
Iacobellis G, Assael F, Ribaudo MC, et al. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res. 2003b;11:304–10.
Iacobellis G, Ribaudo MC, Zappaterreno A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. Am J Cardiol. 2004;94:1084–7.
Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005;2:536–43.
Iacobellis G, Barbaro G, Gerstein HC. Relationship of epicardial fat thickness and fasting glucose. Int J Cardiol. 2008a;128:424–6.
Iacobellis G, Singh N, Wharton S, Sharma AM. Substantial changes in epicardial fat thickness after weight loss in severely obese subjects. Obesity. 2008b;16:1693–7.
Iacobellis G, Willens HJ, Barbaro G, Sharma AM. Threshold values of high-risk echocardiographic epicardial fat thickness. Obesity (Silver Spring). 2008c;16:887–92.
Iacobellis G, Lonn E, Lamy A, Singh N. Sharma AM epicardial fat thickness and coronary artery disease correlate independently of obesity. Int J Cardiol. 2011;146:452–4.
Iozzo P. Myocardial, perivascular, and epicardial fat. Diabetes Care. 2011;34 Suppl 2:S371–9.
Kankaanpää M, Lehto HR, Pärkkä JP, et al. Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab. 2006;91:4689–95.
Kim MK, Tomita T, KimMJ SH, Maeda S, Tanaka K. Aerobic exercise training reduces epicardial fat in obese men. J Appl Physiol. 2009;106:5–11.
Malavazos AE, Di Leo G, Secchi F, et al. Relation of echocardiographic epicardial fat thickness and myocardial fat. Am J Cardiol. 2010;105:1831–5.
Marchington JM, Pond CM. Site-specific properties of pericardial and epicardial adipose tissue. the effects of insulin and high-fat feeding on lipogenesis and the incorporation of fatty acids in vitro. Int J Obes. 1990;14:1013–22.
Marchington JM, Mattacks CA, Pond CM. Adipose tissue in the mammalian heart and pericardium; structure, foetal development and biochemical properties. Comp Biochem Physiol. 1989;94B:225–32.
Mazurek T, Zhang L, Zalewski A, Mannion JD, Diehl JT, Arafat H. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003;108:2460–6.
Momesso DP, Bussade I, Epifanio MA, Schettino CD, Russo LA, Kupfer R. Increased epicardial adipose tissue in type 1 diabetes is associated with central obesity and metabolic syndrome. Diabetes Res Clin Pract. 2011;91:47–53.
Park JH, Park YS, Kim YJ, et al. Effects of statins on the epicardial fat thickness in patients with coronary artery stenosis underwent percutaneous coronary intervention: comparison of atorvastatin with simvastatin/ezetimibe. J Cardiovasc Ultrasound. 2010;18:121–6.
Pezeshkian M, Noori M, Najjarpour-Jabbari H, et al. Fatty acid composition of epicardial and subcutaneous human adipose tissue. Metab Syndr Relat Disord. 2009;7:125–31.
Pierdomenico SD, Pierdomenico AM, Cuccurullo F, Iacobellis G. Metaanalysis of the relation of echocardiographic epicardial adipose tissue thickness and the metabolic syndrome. Am J Cardiol. 2012;15:1234–6.
Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007;153:907–17.
Sacks HS, Fain JN, Holman B, Cheema P, Chary A, Parks F. Uncoupling protein-1 and related mRNAs in human epicardial and other adipose tissues: epicardial fat functioning as brown fat. J Clin Endocrinol Metab. 2009;94:3611–5.
Sacks HS, Fain JN, Cheema P, Bahouth SW, Garrett E, Wolf RY. Inflammatory genes in epicardial fat contiguous with coronary atherosclerosis in the metabolic syndrome and type 2 diabetes: changes associated with pioglitazone. Diabetes Care. 2011;34:730–3.
Sacks HS, Fain JN, Bahouth SW, et al. Adult epicardial fat exhibits beige features. J Clin Endocrinol Metab. 2013;98:E1448–55.
Willens HJ, Byers P, Chirinos JA, Labrador E, Hare JM, de Marchena E. Effects of weight loss after bariatric surgery on epicardial fat measured using echocardiography. Am J Cardiol. 2007;99:1242–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
Iacobellis, G. (2016). Epicardial Fat Thickness as a Biomarker in Cardiovascular Disease. In: Patel, V., Preedy, V. (eds) Biomarkers in Cardiovascular Disease. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7678-4_13
Download citation
DOI: https://doi.org/10.1007/978-94-007-7678-4_13
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7677-7
Online ISBN: 978-94-007-7678-4
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences