Abstract
Liver transplantation is the standard therapy for many liver diseases. Despite being a considerable successful treatment, avoiding allograft rejection, among other complications, continues being one of the big challenges for physicians. Immunosuppression drugs significantly decrease rejection rates after liver transplantation; however, they have generally associated adverse effects which compromise liver transplantation outcome, increasing patients’ morbidity and mortality. So, a close monitoring of immunosuppression is essential to reduce drugs’ undesirable effects as long as allograft rejection is avoided. Nevertheless, monitoring of liver transplant recipients (LTRs) frequently entails the study of liver biopsies with its consequent inconvenience and risk for the patient. Identification of biomarkers that could diagnose or predict the risk of suffering allograft rejection (acute, chronic, or antibody mediated), or, on the contrary, the potential to achieve allograft tolerance, would represent a considerable progress in the managing and monitoring of LTRs. As the immune response of LTRs is responsible for the rejection or tolerance of the liver allograft, most of the potential biomarkers studied in this field are related to the immune system. For that reason, in this chapter, we attempt to review the state of the art in immunological biomarkers for the managing of patients after liver transplantation.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
Key Facts
Key Facts of Acute Rejection (AR)
-
AR is a T-cell-dependent immune response directed against donor tissues resulting from the recognition of alloantigens by recipient T cells.
-
AR after liver transplantation occurs in as much as 70% of patients within the first year.
-
Approximately 5–10% of liver transplant recipients who develop AR progress to severe ductopenic rejection despite antirejection therapy.
-
AR is generally suspected based upon the development of hepatic biochemical test abnormalities although histological study of liver biopsy is required to establish the diagnosis.
Key Facts of Chronic Rejection (CR)
-
CR can be broadly defined as a largely indolent but progressive form of allograft injury characterized histopathologically by two main features: severe damage and loss of small bile ducts and obliterative arteriopathy.
-
In comparison to acute rejection, CR is a more indolent but more progressive form of allograft injury, which is largely irreversible and eventually results in allograft failure.
-
Many cases of CR clearly evolve from severe or inadequately controlled AR episodes.
-
Often the only reliable early indicator of CR is persistent and preferential elevation of γ-glutamyl transpeptidase and alkaline phosphatase, which is related to bile duct damage and loss.
-
The gold standard of CR diagnosis is the histopathological study of liver biopsy.
Key Facts of Graft Tolerance
-
Life-long immunosuppression regimens are still required in transplant recipients, and these represent the standard treatment in daily practice despite their many side effects that increase morbidity and mortality.
-
Liver is considered as an immunologically privileged organ by its lowest incidence of rejection than other solid organ transplants.
-
Around 26% of adult liver transplant recipients may stop treatment without compromising the viability of the graft, and this phenomenon is known as spontaneous operational tolerance.
-
Pediatric population appears to develop tolerance more easily than adult recipients.
-
Whereas B cells participate in the maintenance of tolerance in other solid organ transplantations, like kidney, NK and T cells play an essential role in the development of tolerance in liver transplantation.
- Acute allograft rejection:
-
Allograft injury produced by the setting up of the cellular immunity of the recipient, usually known as acute rejection
- Allograft:
-
Whole or part of an organ or tissue that is transplanted from one individual to another of the same species with a different genotype, which generates an inmmunological response in the recipient
- Allograft tolerance:
-
Partial or complete acceptance of the allograft by the immune system of the recipient, which allows the immunosuppression withdrawal
- Antibody-mediated rejection:
-
Acute or chronic rejection of the allograft owing to the presence of DSAs, which produces an immune response against the allograft in the recipient
- Chronic allograft rejection:
-
Allograft injury produced by successive episodes of acute rejection
- Cytokines:
-
Broad and loose category of small proteins that are important in cell signaling during the immune response
- Donor-specific antibodies (DSAs):
-
Antibodies in the allograft recipient against specific HLA donor allograft antigens, formed in the recipient prior or after transplant
- Immunological markers:
-
Biomarkers related to the allograft recipient immune system
- Immunosuppression:
-
Inhibition of immune response in the allograft recipient in order to decrease allograft injury produced by the recipient immune system
- Orthotopic liver transplantation:
-
Replacement of a diseased liver with part or whole of a healthy liver from another person (allograft) in the same anatomic location as the original liver
Introduction
Liver transplantation is the standard therapy for many liver diseases. It is indicated for severe acute or chronic liver disease where the limits of medical therapy have been reached. Successful liver transplantation results in prolonged survival and improves quality of life of recipients. Nowadays in Europe the 5-year survival rate of liver transplantation recipients is around 75%, and the long-term management of these patients is a defiant challenge for the physicians (Adam et al. 2012).
Rejection was the biggest limitation to an acceptable survival in the beginning of liver transplantation era. The development of powerful immunosuppressant agents drove to a dramatical improvement in the recipients’ survival (Dienstag and Cosimi 2012).
Immunosuppression drugs significantly decrease rejection rates after liver transplantation. However, these agents have a poor safety profile, and in some cases, they are not well tolerated and require a close monitoring to prevent toxicity. Adverse effects associated with immunosuppressant therapy after liver transplantation include neurotoxicity, renal function impairment, increased risk of de novo cancer, or increased cardiovascular risk (Adams et al. 2015). These comorbidities are the main reason that transplant recipients still exhibit much higher morbidity and mortality than the general population (Londoño et al. 2012).
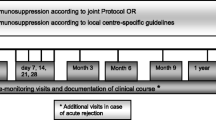
Lowering the dose or changing the immunosuppressant agent is frequent after liver transplantation to prevent or control adverse effects and to ease the development of acute or chronic rejection. Current immunological monitoring after orthotopic liver transplantation (OLT) relies mainly on clinical judgment and on measurement of immunosuppressive drug levels, without a real assessment of the immunological system suppression. Therefore, the evaluation of the immunosuppression state in liver transplanted patients is crucial for a correct posttransplant management and constitutes a major step toward the personalization of immunosuppressive therapy (Adams et al. 2015). The availability of biomarkers to identify patients in high risk of acute rejection (AR) could help to identify subjects that need an aggressive immunosuppressant therapy in the early posttransplant period. On the contrary, a biomarker to predict graft acceptance could allow using low dose of immunosuppressant drugs that could avoid or decrease the rate of adverse effects.
Despite the elevated interest in the evaluation of potential biomarkers of AR and graft acceptance, only a few of them are used routinely in the clinical practice.
Several biomarkers have been evaluated in the set of AR. Substances that increase during AR, such as liver enzymes and pro-inflammatory cytokines, have been the most studied ones. However most of them do not allow to differentiate AR from other OLT complications, as infections (Germani et al. 2015).
In the evaluation of graft acceptance, the results are more encouraging. Liver biopsy is the gold standard to assess graft status after liver transplantation, but is an invasive procedure, and it does not permit to identify the tolerant recipients (Germani et al. 2015). Several studies have been performed to identify biomarkers of tolerance after liver transplant. Patients undergoing immunosuppression withdrawal seem to present specific characteristics compared to non-tolerant patients. Most of them are based on the immunophenotyping of peripheral blood samples and nonspecific genome analysis (Londoño et al. 2012).
In this chapter, we attempt to review the state of the art of immunological biomarkers in liver transplantation.
Immunological Basis of Allograft Rejection in Liver Transplantation
Generally, liver allograft rejection involves predominantly graft-versus-host reactions after transplantation. The lymphocyte-mediated reactions from the recipient to the allogeneic cells (acquired as a graft) lead to injury and/or the destruction of the grafted cells. According with the time it takes to occur and the implicated causes, graft rejection has been divided into four groups (Table 1).
However, mechanisms that are at the genesis of rejection all are put in motion with transplantation of an allogeneic graft (Fig. 1). Following transplantation of liver or other solid organs, antibody-mediated hyperacute vasculitic rejection can develop in individuals with preformed antibodies targeting the donor’s major histocompatibility complex (MHC) class I-encoded antigens. However, in liver allograft transplant, owing to the liver tolerogenic capacity, hyperacute rejection is very unusual (Adams et al. 2015).
Mechanisms underlying liver allograft rejection. After liver transplant, recipient T cells are activated directly (acute rejection) or indirectly (chronic rejection), and proliferation of T cells and activation of effector cells by CD4+ T cells occur. CD8+ T cells and effector cells infiltrate and injure the graft developing rejection signs. Depending on the cytokine environment, activated CD4+ T cells can transform into graft-destructive or graft-tolerance phenotypes which balance the immunological response. CD4+T cells can also activate B cells, which can develop a further antibody-mediated response against antigens in the graft and generate antibody-mediated rejection (AMR)
Under most other circumstances, AR is initiated by the large number of the host’s T cells that recognize donor alloantigens (Afzali et al. 2008). Transplantation of MHC histo-incompatible organs and tissues therefore produces a strong, cytopathic T-cell-dependent immune response to donor tissues. In the direct pathway (dominant in AR), allogeneic MHC molecules on donor antigen-presenting cells (APCs) are recognized by recipient T cells without any previous processing. The initial T response in AR is characterized by infiltration of the graft by CD4+ and CD8+ T cells, but myeloid and innate lymphoid cells are involved and determine the outcome of the allorecognition.
Despite routine use of immunosuppressive therapy, AR is not uncommon. CD4+ and CD8+ T cells together contribute to AR, although CD4+ T cells primarily mediate the rejection response. Activation of CD4+ T cells is strongly influenced by the cytokine environment, and this contribute to the balance between rejection and tolerance, since CD4T cells can differentiate into effector (cells responsible of allograft rejection) or regulatory (cells responsible of allograft tolerance) phenotypes depending on the cytokines present during activation (Adams et al. 2015). Despite the importance of CD4+ T cells in rejection, many activated CD8+ (cytotoxic) T cells penetrate the transplant at the time of rejection, along with other mononuclear leukocytes. However, their exact role is still not completely clear. The hepatic sinusoidal endothelium presents some vascular adhesion proteins (VCAM-1, vascular cell adhesion protein 1), activated by injury or local inflammation, and mediates lymphocyte recruitment to the liver during graft rejection. Some chemokines are also critical for leukocyte recruitment (CXCL9 or CXCL10) and play an important role for compartmentalization of infiltrating leukocytes during graft rejection. Cytotoxic T cells and other effector leukocytes bind to bile ducts and hepatocytes by several molecular mechanisms causing hepatocyte and bile duct destruction during rejection .
Activated T cells also provide help for alloantibody production by B cells leading to antibody-mediated graft damage and complement deposition on graft endothelium (Adams et al. 2015).
Indirect antigen presentation (indirect pathway), in which donor alloantigens are processed by APCs, which internalize and process donor MHC molecules and subsequently present them to the recipient’s T cells (Afzali et al. 2008), dominates in chronic rejection (CR) and later immune response in the graft.
Immunological Biomarkers of Rejection
Biomarkers of Acute Rejection
Acute allograft rejection is a graft damage arising as a consequence of an immunological reaction to foreign antigens on the graft. The incidence of clinically significant rejection is 10–40% in most series. The majority of first acute rejection episodes are diagnosed in the first year after transplantation, usually within the first month after transplantation, although late acute rejection can occur more than 3 months after transplantation, normally as a consequence of inadequate immunosuppression (Thurairajah et al. 2013).
Clinical suspicion on one hand, based on nonspecific symptoms, as malaise, fever, abdominal pain, hepatomegaly, and increasing ascites, and biochemical alterations on the other hand, such as elevation of serum aminotransferases, alkaline phosphatases, g-glutamyl transferases, and bilirubin levels, can make suspect of AR after OLT. However, because of the nonspecificity of these signs and symptoms that do not correlate with the severity of rejection (Abraham and Furth 1995), anatomical pathology confirmation is required on liver biopsy, which results costly and may imply complications, as bleeding, infections, and so on.
Noninvasive diagnostic tools, as biomarkers, for the early diagnosis of AR would be very valuable. Considering that AR is a consequence of the recipient immune response, biomarkers related to this immune reaction have been studied in the last years; however, few of them have been validated and are used routinely in the clinical practice.
Serum Immunological Markers
The first potential immunological biomarkers being studied were cytokines and other proteins related to the inflammatory response.
The type 1 helper T cells (TH1) and cytokine interleukin 2 (IL-2) and its receptors (IL2-R) are well known to trigger acute allograft rejection. Perkins et al. (1989) studying 82 liver transplant recipients (LTRs) found that soluble IL2-R (sIL2-R) increased 17% per day in the 10 days prior to the diagnosis of AR episodes compared to the control group. Although sIL2-R also tended to increase in recipients developing cytomegalovirus (CMV) disease prior to the diagnosis, the increase was not as high as in the recipients with rejection . Even though other authors have found a raise in serum sIL2-R levels before diagnosis of AR, they have also observed higher serum sIL2-R levels in infection episodes after transplantation (Platz et al. 1997). In a study with 81 patients, Platz et al. (1997) found that sIL-2R increased 3 days prior to the onset of acute steroid resistant rejection. In this case, the increase in sIL-2R was similar to that in patients with serious infections and asymptomatic cholangitis. However, Ninova et al. (1994), in order to differentiate AR from CMV hepatitis after OLT, observed that patients with CMV showed a higher increased of sIL-2R and concomitant elevation of CD8+ T cells, not observed in AR patients.
Boleslawski et al. (2004) associated intracellular IL-2 expression in CD8+ T cells before transplantation with the later development of AR. These data were later confirmed by Akoglu et al. (2009), who observed that the percentage of CD8+ T cells with detectable intracellular IL-2 was significantly increased in patients with AR compared to recipients without rejection. Moreover, these authors found a good correlation between intracellular IL-2 and rejection severity, according to the Banff score (Spearmans-rho = 0.81, P < 0.05), showing good sensitivity and excellent specificity in AR (specificity of 95% for histologically proven AR). In a later study (Millán et al. 2013), LTRs who developed AR showed a significant increase in the percentage of CD8+IL-2+ T-cell levels during the early posttransplantation period (when there is a high incidence of AR) associated with lower susceptibility to immunosuppressive treatment. This increase was also accompanied by an increase in the percentage of interferon gamma (IFN-γ)-positive CD8+ T cells and soluble IFN-γ levels. The percentage of IFN-γ CD8+ T cells prior to transplantation was also higher in rejectors, and levels of soluble IFN-γ were also associated with severity of AR. Authors of this study suggested IFN-γ as a robust candidate biomarker of liver transplantation .
Other cytokines and growth factors have also been shown to increase in AR. In the study of Platz et al. (1997), mentioned before, also an elevation of tumor necrosis factor (TNF) receptor II (released upon stimulation of Th1 lymphocytes), interleukin-8 (IL-8), and interleukin-10 (IL-10) occurred in patients with steroid-resistant rejection 3 days prior to the onset of rejection ; however, as in the case of sIL-2R, similar increases were also observed in patients prior to severe infection. Neopterin (produced by IFN-γ-activated macrophages) levels increased before acute steroid-resistant rejection, although this increase was significantly lower than that observed prior to severe infection. In fact, a multivariate analysis revealed significant differences in cytokine pattern between rejection and infection for neopterin, IL-8, sTNF-RII, and IL-10, which may guide monitoring after OLT. This study also analyzed other cytokines including IFN-γ, interleukin-1-beta (IL-1β), interleukin 4 (IL-4), and interleukin 6 (IL-6), which also increased during severe rejection and infection, but, after the onset of other events, makes them of less clinical value in terms of early biomarkers.
Despite the results of Platz et al. (1997) measuring IL-6 levels in serum, Kita et al. (1994) found significantly higher serum levels of IL-6 up to 4 days prior to histopathological diagnosis of AR, and although patients with serious infections also presented higher levels of IL-6, the increase was distinguishable between both episodes.
Interleukin 15 (IL-15), produced by non-lymphatic cells as macrophages, with similar action to IL-2 and inducing proliferation of natural killer (NK) cells, increased in plasma during AR, especially in steroid-resistant rejection (Conti et al. 2003). Interleukin 23 (IL-23) and interleukin 17 (IL-17), produced by helper T cells and induced by IL-23, have been showed to be involved in the AR process after OLT. Although IL-23 and IL-17 serum levels are not different in the early posttransplantation period, they have been showed to increase at the diagnosis of AR (Fábrega et al. 2009). A later prospective study confirmed that levels of circulating CD4+IL-17+ T (Th17 cells) were higher during AR compared with LTRs without AR. This increase in the frequency of CD4+IL-17+ cells in peripheral blood was positively correlated with the rejection activity index (RAI) (r = 0.79, P = 0.0002) (Fan et al. 2012).
Apart from soluble cytokines, membrane proteins expressed on cells of the immune system have also been studied as potential markers of AR. Expression of CD28, protein expressed on the membrane of T cells that provides co-stimulatory signals required for T-cell activation and survival, has been showed to raise up to 6 days prior diagnosis of AR (García-Alonso et al. 1997). An upregulation of CD28 in CD4(+) lymphocytes in the periods of greatest AR has been observed, without being influenced by hepatitis B virus (HBV), hepatitis C virus (HCV), or CMV infections, which makes CD28 useful to discriminate between AR and the cellular activation induced by viral reinfection (García-Alonso et al. 1997; Minguela et al. 2006). Later, Boleslawski et al. (2008) studying prospectively the expression of CD25, CD28, and CD38 on CD3+, CD4+, and CD8+ cells in 52 LTRs found that in addition to the increase of CD28 expressing T cells during AR, there was also a raise in the frequency of CD38 expressing T cells. However, although they did not observed an elevation of CD28+ and CD38+ T cells during infection comparing to patients with an uneventful postoperative course, they could not exclude the possibility that infections themselves might alter the expression of CD28 and CD38, because the number of patients was too small.
On the other hand, circulating CD4+CD25highFoxP3+ regulatory T cells are regulatory T cells were showed to be significantly lower in liver allograft recipients with AR compared with patients without rejection. The frequency of circulating CD4+CD25highFoxP3+ T cells was also negatively correlated with the RAI (r = −0.80; P < 0.01) (He et al. 2011). These results were recently confirmed by Wang et al. (2014), who found that the frequency of circulating CD4+CD25+FoxP3+ cells decreased at the onset of AR whereas the frequency of circulating Th17 cells increased. They also observed that the Treg/Th17 ratio had a negative correlation with liver damage indices and the RAI. The increase of circulating Th17 cells during AR agrees with the study of Fan et al. (2012), as mentioned before. Thus, the Treg/Th17 ratio can be suggested as a candidate marker for the diagnosis of AR; however, there is a lack of data about the behavior of this ratio in other OLT complications.
Recently, Raschzok et al. (2015) in a prospective study with 94 LTRs observed lower CD44 and higher CXCL9 serum protein levels at day 1 posttransplantation in patients developing later AR. Even CXCL9 levels resulted higher before transplantation in these patients. CD44 values (cutoff <200.5 ng/mL) or CXCL9 values (cutoff >2.7 ng/mL) at the day after transplantation allowed to differentiate between rejection and no rejection with a sensitivity of 88% or 60% and a specificity of 61% or 79%, respectively. The combination of both biomarker cutoffs had a positive predictive value of 91% and a negative predictive value of 67% for clinically significant AR. Furthermore, CD44 levels were different in patients with graft dysfunction due to other reasons.
Toll-like receptor 4 (TLR4), with an important role in the activation of the innate immune system, has been showed to be related to acute liver rejection . Testro et al. (2011) studying 26 LTRs observed that patients experiencing AR showed higher levels of TLR4 in CD14+ cells prior to liver transplantation and a significant downregulation during the first week after transplantation.
Some cell adhesion molecules involved in the immune response have also been studied as potential biomarkers of AR. Intercellular adhesion molecule 1 (ICAM-1), cell surface glycoprotein regulating infiltration of leukocytes into the allograft during AR, E-selectin (expressed in endothelial cells recruiting leukocytes), and vascular cell adhesion protein 1 (VCAM-1) (also mediating adhesion of immune cells to the vascular endothelium) have been observed to be increased in serum of patients with AR, especially in acute steroid-resistant rejection. However, the increase of these molecules has also been observed in infectious episodes and other liver posttransplantation complications, not resulting practically as specific markers of AR (Goto et al. 1998).
Peripheral blood count of eosinophils has been suggested as a candidate biomarker for AR after liver transplantation. Foster et al. (1989) studying 60 LTRs found that blood eosinophilia (absolute eosinophil count >500 cells/mm3) occurred up to 5 days prior to AR diagnosis. In these cases of rejection , blood eosinophilia was followed by graft eosinophilia. Afterward, Barnes et al. (2003) in a cohort of 101 LTRs found that an elevated eosinophil count during or 1 day before biopsy had a positive predictive value of 82% for AR, whereas a normal eosinophil count excluded moderate/severe rejection with a predictive value of 86%. Nevertheless, in a recent study with a larger series of patients, it was found that although peripheral eosinophil count was strongly associated with moderate/severe rejection (OR = 2.15; P = 0.007), the area under ROC curve was only 0.58, concluding that peripheral eosinophilia was not sufficiently predictive of moderate/severe histological rejection. However, this study showed that changes (between the first and second biopsy) in eosinophil count over time can accurately predict the histological resolution of rejection (Rodríguez-Perálvarez et al. 2012).
In a study of Yu et al. (2013), the frequency of Vδ1+ T-cell subset was reduced during AR, whereas the frequency of Vδ2+ T-cell subset increased in these patients. Therefore, a reduction of the Vδ1+/Vδ2+ ratio during AR was observed, showing a negative correlation with alanine transaminase (ALT) and alanine aminotransferase (AST) levels. On the contrary, they did not found differences in frequency of γδ T cells. Considering that in CMV and HCV and other infections, an increase of Vδ1+ T-cell and a decrease Vδ2+ T-cell subset have been observed (Puig-Pey et al. 2010), the ratio Vδ1+/Vδ2+ ratio may act as a biomarker to predict the immunological situation of recipients after liver transplantation.
On the other hand, with pediatric patients following liver transplantation, a study revealed that serum plasminogen activator inhibitor 1 (PAI-1) levels at the time of AR were significantly higher than that after the rejection ending and those on days 14 and 28 in the group without rejection (Mimuro et al. 2010). Therefore, levels of PAI -1 in pediatric patients could be useful for suspecting AR after liver transplantation. However, no more studies have been performed in this sense to corroborate these results.
Bile Immunological Markers
Apart from serum biomarkers, some studies have focused on finding possible markers of AR in bile, though results are not very conclusive.
Some of the already mentioned cytokines and cell membrane proteins in serum have also been observed in bile. In that way, bile IL-6 levels were found to be significantly increased in patients with AR, decreasing in response to antirejection therapy, but these levels were also observed elevated in patients with cholangitis (Umeshita et al. 1996).
As in serum, Lang et al. (1995) observed that biliary ICAM-1 was specifically elevated during rejection and not during infection or when no rejection was apparent; however, in a later study, this increase was also found during infectious complications (Warlé et al. 2003). In the case of the IL-2R, bile IL-2R levels are increased in LTRs with AR, although comparing to serum levels, higher specificity and selectivity is reached (Adams et al. 1989).
Apart from the inconsistent results among studies, bile biomarkers present a clear limitation to be used in the clinical practice compared to serum biomarkers; bile sampling needs invasive procedures, whereas blood or serum samples are easily acquirable and do not represent any further risk for the patient.
Future Biomarkers
Permanent advances in analytical techniques, especially in the field of -omics (genomics, transcriptomics, proteomics) during the last decades, have opened new perspectives for the discovery of biomarkers.
Genomics
More advances in the identification of genes involved in allograft rejection have been carried out in the field of kidney transplantation; however, some studies have been developed in liver transplants. In a study performed by Berberat et al. (2006), they identified six genes related to the inflammatory response that significantly correlated with the occurrence of early graft dysfunction. Higher C-reactive protein gene expression levels correlated significantly with the need of therapeutic interventions due to graft-related complications, whereas the expression of five genes related to vascular endothelial cell physiology (connective tissue growth factor, CTGF; WW domain-containing protein 2, WWP2; programmed death ligand 1, CD274; vascular endothelial growth factor, VEGF; and its receptor FLT1) was significantly reduced in biopsies of patients with graft-related complications in the first month. Authors, using a risk score based on the expression of these five genes, determined that early allograft dysfunction could be predicted with 96% sensitivity. Nevertheless, authors did not differ among causes of allograft dysfunction, so these genes cannot be associated directly to AR.
Apart from wide genome studies, the polymorphisms of some genes related to the immune response have been identified to be associated with AR after OLT. In that way, Yu et al. (2014) in a study with 289 LTRs analyzing preoperative peripheral blood DNA of recipients found that interferon regulatory factor 5 (IRF5), which transcriptionally activates inflammatory cytokines, was genetically related to AR and could be considered a risk factor for AR after liver transplantations . In brief, the IRF5 gene polymorphism rs3757385 was found to be associated with AR, and homozygous individuals for this polymorphism were at higher risk of AR. However, polymorphism was not studied in patients with other complications after OLT.
Oetting et al. (2012), analyzing 37 different single nucleotide polymorphisms within the toll-like receptor 4 (TLR4) gene in 738 recipients LTRs, found that various donor polymorphisms of the TLR4 gene were clearly associated with AR and could be considered risk factors of graft loss. That would be in agreement with results of Testro et al. (2011), as mentioned before, who observed that levels of expression TLR4 in CD4+ (at protein level) cells were related to AR.
Transcriptomics
Asaoka et al. (2009), by microarray analysis of liver biopsies RNA, demonstrated novel transcriptome patterns for AR with recurrent hepatitis C and different from those in recipients with only recurrent hepatitis C without AR, suggesting that gene expression profiling may be useful in the diagnosis of AR in recipients with hepatitis C. In their study, they found 126 relatively overexpressed genes in the ACR, 15 of them involved in the inflammatory and immune response and antigen presentation.
Meanwhile, in peripheral blood, higher gene expression levels of guanylate-binding protein 2 (GBP2) and interferon regulatory factor 1 (IRF1) (genes mainly expressed in leukocytes) were observed in samples of patients with AR comparing with those from patients with other liver dysfunctions and normal liver after transplantation , but only GBP2 expression resulted significant. Using a cutoff of 20, the sensitivity and specificity of GBP2/GAPDH (glyceraldehyde-3-phosphate dehydrogenase) were 63% and 85%, respectively; as a result, authors concluded that GBP2 may be useful for the diagnosis of AR in patients with liver dysfunction after liver transplantation (Kobayashi et al. 2010).
On the other hand, circulating miRNAs that are extremely stable and protected from RNAses have emerged as candidate biomarkers for any disease. They fulfill many characteristics of ideal biomarkers: noninvasive, stable, and easily detected. In this sense, different studies have showed that some circulating miRNAs are associated with AR episodes after liver transplantation (Farid et al. 2012; Wei et al. 2013), some of them related to the immune system. As lymphocyte infiltration into the graft is a major pathological feature of AR after liver transplantation, the contribution of lymphocyte miRNAs during graft rejection have been evaluated. Wei et al. (2013) found that regulation of miR-142-3p expression in lymphocytes may impact graft outcomes.
In a previous study, serum levels of hepatocyte-derived miRNAs, miR-122, miR-148, and miR-194, correlated with hepatic injury and AR (Farid et al. 2012). In fact, expression was elevated earlier than aminotransferase levels during AR.
Nevertheless, miRNA have also been associated with other infectious diseases, as HBV and HCV, among them miRNA-122. Thus, although miRNA biomarkers clearly have potential for clinical application in the setting of liver transplantation, the number of studies on this topic should be expanded and validations should be carried out.
Proteomics
Considering that a wide range of proteins are related to the immune response in AR, proteomics seems a promising approach to determine new biomarkers.
Recently, Massoud et al. (2011) carried out a serum proteome profile in histologically confirmed AR patients, and afterward those identified proteins were validated by ELISA in another cohort of patients. This study showed that complement component 4 (C4) and complement component 1q (C1q) were both independent predictors of AR. C4 had the greatest predictivity for differentiating patients with or without AR (sensitivity = 97%; specificity = 62%; positive predictive value = 74%; negative predictive value = 94%). Combining levels of C4 and ALT improved these results (to 96%, 81%, 86% and 94%, respectively). So, serum C4 and ALT levels could be highly predictive of AR in LTRs; however, because of the reduced number of patients, this study should be validated in a larger multicenter trial.
Currently, only two noninvasive tests, approved by the US Food and Drug Administration, are commercialized. AlloMap (CareDx, San Francisco, USA) is intended to assess AR after heart transplantation, determining gene expression profile of RNA isolated from peripheral blood mononuclear cells (PBMC). ImmuKnow (Viracor-IBT Laboratories, Lee’s Summit, MO, USA) detects cell-mediated immunity in immunosuppressed patients. The assay detects cell-mediated immunity by measuring the concentration of ATP from CD4 cells following stimulation. A systematic review and meta-analysis carried out by Rodrigo et al. (2012) concluded that the ImmuKnow test was a valid tool for determining the risk of further infection in adult LTRs, but the elevated heterogeneity across studies did not allow to conclude the usefulness of ImmuKnow to predict AR. In a recent study of Ravaioli et al. (2015), results showed that ImmuKnow can provide additional data which can help to optimize immunosuppression and improve patient outcomes after liver transplantation, rather than discriminate the risk of AR.
Biomarkers of Chronic Rejection
Chronic liver rejection can be defined as an immunologic injury to the graft, which occurs after severe or persistent AR and results in irreversible loss of bile ducts, arteries, and veins (Neumann et al. 2002). Histologically, CR is characterized by destruction of interlobular bile ducts associated with cholestasis. Normally, it is associated with centrilobular inflammation and necrosis and with foam cell lesion within intrahepatic arterial branches. CR rejection can progress to bridging fibrosis and cirrhosis (Neuberger 1997).
There has been a progressive decrease in the prevalence of CR, being around 5–15%, and nowadays accounts for less than 2% of cases of graft failure. CR leading to re-transplantation is relatively rare, around 5%. However CR is probably underestimated due to the absence of routinely performed liver biopsies on the long term in most centers (Adams et al. 2015). The onset of the disease is during the first year posttransplant and occurs only in rare cases in the long term after OLT (Neuberger 1997). Late CR might also develop after a therapy refractory late acute rejection episode, normally in therapy noncompliant patients.
Because CR is a potentially reversible pathologic state at its onset, early diagnosis is very important. Generally, histopathologic diagnosis is carried out when CR is well established and results are irreversible; so as in AR, noninvasive diagnostic tools for early diagnosis of CR would be very valuable for the treatment of CR. Comparing with AR, few studies have been performed in the case of CR in order to study possible biomarkers, and all of them have been carried on liver biopsies, with no studies about biomarkers in serum. Thus, independent of the results, noninvasive procedures are not provided for CR diagnosis.
C4d has been proposed as a marker of CR. In a study of Lorho et al. (2006), searching for the presence of C4d in posttransplant hepatic biopsies, found that C4d expression appeared in 100% of biopsies classified as CR and in 33% of biopsies diagnosed as AR, being absent in biopsies of patients with recurrent hepatitis C infection without rejection.
The increase of p21 WAF1/Cip1 in liver biopsies has also been associated with early CR and suggested as a marker of this complication (Lunz et al. 2001). The percentage of p21 WAF1/Cip1 biliary epithelial cells (BECs) and the number of p21 WAF1/Cip1BECs per portal tract are significantly increased in early CR compared to BECs in normal liver allograft biopsies or those with nonspecific changes, chronic hepatitis C, or obstructive cholangiopathy. In fact, successful treatment of early CR is associated with a decrease in the percentage of p21 WAF1/Cip1BECs and the number of p21 WAF1/Cip1BECs per portal tract.
Recently, Wei et al. (2015) carried out a study in a rat model of CR after liver transplantation . In order to explore possible biomarkers of the disease, they performed a proteomic analysis of grafts samples 120 days after operation. Authors found that expression of 62 proteins significantly changed in CR. From them, finally they identified clusterin (CLU), lipocalin 2 (LCN2), and cytokeratin 19 (Krt19) as early and reliable biomarkers for chronic rejection on liver biopsies. Expressions of CLU and LCN2, a neutrophil gelatinase-associated lipocalin, were found to be upregulated both in AR and CR but more upregulated in CR. Krt19 expression was downregulated probably because of the disappearance of interlobular bile ducts.
DSAs: Potential Biomarkers for Allograft Rejection?
The adverse impact of donor-specific human alloantibodies (DSAs) in solid organ allografts has been widely demonstrated, such as the kidney, pancreas, or heart (Kaneku et al. 2013). Until recently, this impact has been considered irrelevant and ignored in OLT outcomes, since liver allografts possess some degree of alloantibody resistance (Pons et al. 2011). However, in the last few years, detailed studies have shown alloantibody-mediated adverse consequences in liver allografts (Castillo-Rama et al. 2008; Kozlowski et al. 2011; Kaneku et al. 2013), questioning the impact of DSAs on short- and long-term liver transplant outcomes. Currently, it is assumed that antibody-mediated rejection (AMR) can occur in the liver allograft, being involved in both acute and chronic rejections (Adams et al. 2015). Results from recent studies suggest that the presence of preformed or de novo DSAs is associated to AMR and a decrease in the liver allograft survival (Kozlowski et al. 2011; Kaneku et al. 2013). Nevertheless, not all DSAs have been seen to produce the same response after OLT and the mere presence of DSAs has entailed allograft injury, so that DSA concentration and DSA type seem to play an important role in the development of allograft injury and liver transplant outcomes. Considering these findings, certain circulating anti-HLA antibodies could be also suggested as potential biomarkers for the managing of immunosuppression after OLT.
DSAs and Liver Allograft Rejection
Only when AMR is accurately diagnosed early and successfully treated can graft outcomes improve because a delay in the diagnosis of AMR usually results in substantial allograft injury or failure. To date, liver acute AMR is diagnosed based on the following criteria: (1) the presence of DSAs in serum, (2) histopathologic evidence of diffuse microvascular endothelial cell injury and microvasculitis, (3) strong and diffuse C4d detection in tissue, and (4) reasonable exclusion of other causes of injury that might result in similar clinical signs. On the contrary, criteria for diagnosis of chronic AMR need to be further studied, although subsinusoidal and perivenular fibroses, associated with DSA and C4d staining, have been already described (O’Leary et al. 2014a). So, before liver biopsy, determination of serum DSAs can allow the identification of patients in higher risk of AMR after liver transplantation ; however, literature data pointed some considerations in order to use them as biomarkers of liver allograft rejection .
Although some studies have shown that the presence of preformed DSAs was not always associated to a decrease in the liver allograft survival rate or to a worse liver transplant outcome, recently, others have shown alloantibody-mediated adverse consequences in liver allografts (Castillo-Rama et al. 2008; Kozlowski et al. 2011; Kaneku et al. 2013). Thus, a clear controversy exists in the elucidation of the role of DSAs on the liver allograft injury and rejection.
Differences in preformed DSAs levels have been suggested as one of the reasons for the differences of effects between patients and the consequent appearance of clinically significant liver allograft injury and possible AMR. O’Leary et al. (2014b) observed LTRs with high preformed DSAs with higher mean fluorescence intensity (MFI) in its detection seemed to be at higher risk of suffering substantial early graft injury and consequent AMR.
Scornik et al. (2001) quantified by flow cytometry preformed IgG antibodies against donor cells in 465 LTRs and found that the incidence of rejection did not significantly differ between antibody-positive and antibody-negative patients. However, patients with higher antibody concentrations showed higher percentage of steroid-resistant rejection (31% at 1 year) than patients with lower antibody concentration (4%) or without antibodies (8%). These effects were mainly due to T-cell (HLA class I) antibodies. These authors concluded that the effect of preformed DSA on liver allograft outcomes depended on antibody concentration and the patient response to steroid treatment.
In another retrospective single-center study comprising 896 liver transplants, preformed HLA class I and II antibodies, detected by both complement-dependent cytotoxicity and multiple bead assay (Luminex xMAP), were found to be associated with shorter graft survival within the first year posttransplant, but in patients with anti-HLA class I antibodies, the decreased survival rate disappeared after the first year posttransplant and patients with preformed anti-HLA class II antibodies showed lower graft survival 5-year posttransplant (Castillo-Rama et al. 2008). These results are in accordance with those from the study of O’Leary et al. (2013) who observed that preformed class II DSAs were associated with an increased risk of early rejection.
Moreover, among DSAs, IgG subclasses have also been shown to have different effects on liver allograft outcomes. DSAs in chronic rejection patients have been found to be more often of multiple IgG subclasses including IgG3 compared to control group where most DSAs were of a single IgG subclass and without IgG3 (Kaneku et al. 2013). Recently, a retrospective study evaluating 1270 LTRs demonstrated the inferior survival associated with IgG3-positive DSA-positive patients and C1q-positive DSA-positive patients compared to DSA-negative patients. IgG3-positive DSA-positive patients had the highest hazard ratio for death, but its only analysis could not exclude standard DSA test since IgG3-negative DSA-positive patients remained at increased risk of death compared to DSA-negative patients. Nonetheless, IgG3 analysis is suggested as an independent predictor of allograft outcome. Meanwhile, the same study suggested that C1q-fixing DSA test could identify patients with preformed high MFI DSAs, who have been shown to have higher risk of rejection (O’Leary et al. 2015).
Apart from that, most studies have focused on preformed HLA antibodies, and little attention has been paid to de novo DSAs. Kaneku et al. (2013) considering 749 LTRs found that 8.1% of patients developed de novo DSAs 1 year after transplant, almost all de novo DSAs were against HLA class II antigens, and these patients had significantly lower patient and graft survival. This negative relation of de novo DSA and liver graft have been shown by others (Kozlowski et al. 2011).
Therefore, not all DSAs and levels produce the same effects on liver allograft, so differentiation among them should be made in order to be possible candidates as biomarkers of AMR. To date, literature shows that high preformed DSA levels, HLA class II DSAs, IgG3, and de novo DSAs are associated to allograft injury and AMR and could be suggested as biomarkers of AMR in LTRs. However, the development of analytical techniques for a further and more accurate discrimination and quantification of DSAs is required in order to progress in this field.
Current DSA Analytical Techniques
Techniques to detect DSAs have advanced spectacularly because of renal allograft transplantation. Firstly, cytotoxic crossmatch assay was used; however limited sensitivity and specificity did not allow to distinguish HLA from non-HLA antibodies, although performed pretransplantation allows to eliminate hyperacute renal allograft rejection .
This initial test was then supplemented by flow cytometry and solid-phase immunoassays (SPIs), such as ELISA, ELISPOT, and LUMINEX®. Flow cytometry lets differentiate HLA and non-HLA DSAs, even though it shows low sensitivity and specificity to characterize all HLA alloantibodies. This has been solved with the SPI technology based on the multi-analyte bead assays performed on LUMINEX® platforms. However, the latter assays can be influenced by substances in serum and reproducibility among lots and centers could be a considerable constraint. For these reasons, today cell-based assays and SPI are frequently performed in parallel (O’Leary et al. 2014a). In fact, Leonard et al. (2013) outlined an HLA antibody test algorithm for LTRs. Briefly, pretransplant patients were suggested for the analysis of HLA antibodies’ presence by solid-phase testing. If HLA antibodies’ presence resulted positive, a crossmatch by flow cytometry at the time of transplantation was recommended. Then, if a strongly positive crossmatch was detected (median channel shift, MCS > 200), evaluation of DSAs levels with both flow cytometry (MCS) and Luminex (MFI) was further accomplished. Thereafter, resulting the crossmatch strongly positive because of high levels of DSAs, DSAs should be tested for complement fixation and monitored after transplantation. These authors concluded that a strongly positive crossmatch, positive complement fixation, and persistent posttransplantation DSAs indicated an increased risk for AMR (Fig. 2).
Risk of AMR in LTRs. Monitoring antibody-mediated rejection in liver transplant recipients according to Leonard et al. (2013). Those authors proposed sequential analyses (pre- and posttransplantation) in liver transplant recipients in order to evaluate the risk of suffering antibody-mediated rejection; AMR antibody-mediated rejection, DSAs donor-specific human antibodies, HLA human leukocyte antigen, MCS median channel shift, C1q complement component 1q
Recently, molecular phenotyping has also been proposed as a technique to be able to differentiate patients with DSAs in serum who do not experience pathologic injury from those with DSA, experiencing subclinical pathologic injury that becomes apparent later, and those with clinically evident pathologic injury, opening a promising field in the use of DSAs in the monitoring of liver transplantation (O’Leary et al. 2014a).
There is an increasing need to characterize DSAs more accurately in order to clarify their role in AMR in liver transplantation and for the early diagnosis of AMR. That entails the development of new cross-platform analyses that can include routine and multiplex protein immunohistochemistry, messenger RNA and miRNA expression arrays, and proteomics and metabolomics techniques.
Immunological Biomarkers of Graft Acceptance/Tolerance
Allograft Tolerance
Successful immunosuppression (IS) withdrawal in LTRs occurs more frequently than in other solid organ transplantations. It has been showed both in noncompliant patients and in those with serious complications related to immunosuppression (IS) drugs, like lymphoproliferative disease (Lerut and Sánchez-Fueyo 2006). Thus, the liver is considered as an immunologically privileged organ by its intrinsic tolerogenic properties that make it the most amenable graft to IS withdrawal.
Literature data provides a percentage of successful weaning at around 20–33%, although the prevalence could be higher in pediatric population under 1 year, where this percentage could reach 64% (Li et al. 2012), and in adult recipients with more than 10 years of posttransplant follow-up (Sánchez-Fueyo 2011). This phenomenon is known as spontaneous operational tolerance, and these patients are considered as “operationally” tolerant recipients.
In the clinical setting, the state of tolerance can be achieved in two different ways: spontaneously or induced. The endpoint can be the complete IS drug withdrawal (operational tolerance) or minimization of this (“prope” tolerance), which is the most frequent situation in clinical practice (Table 2). To date, it is unknown whether minimally immunosuppressed patients actually will be able to complete the discontinuation of IS without developing rejection (Lerut and Sánchez-Fueyo 2006). Neither is clear whether “prope” tolerance is a previous step of operational tolerance or two independent conditions.
Since IS withdrawal has an inherent risk of AR, identifying biomarkers of graft acceptance is required in order to tailor IS therapy after liver transplantation (Germani et al. 2015).
Biomarkers of Graft Acceptance
In order to identify biomarkers of graft acceptance, several studies have employed blood samples of operationally tolerant recipients to perform gene expression profiling and immunophenotyping. In recent years, attention has been directed toward samples of liver tissue to find immune parameters associated with operational tolerance. The interest generated has made possible to identify several potential markers of allograft tolerance (Table 3).
NK Cells
Studies using gene expression analysis demonstrate that NK cells and related transcripts are upregulated in blood samples from operationally tolerant LTRs, determined by microarray and real-time PCR platforms. In fact, some authors, like Londoño et al. (2012), assert that NK-related transcripts seem to be the most robust markers of operational tolerance. These results have been confirmed not only in adults but also in pediatric LTRs (Li et al. 2012) and in operationally tolerant kidney recipients (Martínez-Llordella et al. 2007). Indeed, according to Bohne et al. (2012), tolerant recipients exhibit an expansion of NK cells in peripheral blood even before the initiation of drug minimization.
γδTCR+ Cells
Similar to NK cell-related transcripts, genes encoding for gamma-delta T cells (γδT-cell) and for proteins involved in the cycle cell proliferation arrest are upregulated in tolerant liver recipients compared to immunosuppression-dependent patients or healthy individuals. So they appear to be specifically related to the tolerant state and their expression seems to be independent on either HCV infection or IS treatment (Martinez-Llordella et al. 2008).
There are two kinds of γδTCR+ T-cell subsets in human peripheral blood; γδ2TCR+ T cells account for more than 70–80% of circulating T cells in healthy individuals, while Vδ1TCR+ subtype preferentially populates epithelial tissues such as the intestine, liver, and spleen (Martinez-Llordella et al. 2008). In contrast, a significant increase γδ1/γδ2 T-cell ratio has been found in operationally tolerant liver-transplanted patients when compared with liver-transplanted patients on immunosuppression and with age-matched healthy controls (Martinez-Llordella et al. 2007). Along these lines, Bohne et al. (2012) show a decreased proportion of γδ 2-TCR cells in tolerant patients as compared with non-tolerant recipients before the start of IS withdrawal.
Regulatory T Cells
Regulatory T cells (Treg cells) are characterized by the coexpression of CD4, CD25 (interleukin 2 [IL2] receptor α chain), and Forkhead box 3 (FOxP3) (Pons et al. 2008).
Several studies have shown an expansion of CD4+CD25high T cells in phenotypic analysis of PBMC of tolerant recipients for more than 2 years after liver transplantation than either non-tolerant patients or healthy individuals, but this increase does not seem to be present at the beginning of weaning. Castellaneta et al. (2011) suggest that CD4+CD25highCD127low would provide a better marker for tolerance.
Pons et al. (2008) described an increase of FoxP3 mRNA in blood samples of tolerant recipients and observed that FoxP3 intragraft transcript levels were 3.5-fold increase up to the beginning of the tolerance phenomenon, which is continued at the end of therapy. Li et al. (2008), following the same line, reported that FoxP3 mRNA is also higher in liver biopsies from tolerant transplanted patients compared with patients on immunosuppression, but mRNA levels were similar in operationally tolerant and chronic rejectors. However, while some authors report increased FoxP3+ transcript levels in peripheral blood and liver tissue of tolerant recipients, other authors did not observe differences between tolerant and non-tolerant patients, neither Foxp3 transcripts nor immunophenotyping analysis (Bohne et al. 2012).
It is noteworthy that Treg cell suppressor function and their survival depend on the presence of IL-2. Calcineurin inhibitors block IL-2 production, which may thereby negatively affect the homeostasis of Treg cells. Several reports support this hypothesis, as Pons et al. (2008) indicate. Therefore, up until today, the role of Treg cells in graft acceptance is less clear because the use of immunosuppressive drugs could alter their expression and by the disparity in the results found.
Dendritic Cells and HLA-G Expression
Dendritic cells (DC) are innate immune system cells that are also important in the regulation of adaptive immunity, including the ability to induce regulatory T cells (Treg cells). There are two types of DC: monocytoid DC (CD11c+), which induce Th1 cell differentiation in vitro, and plasmacytoid DC (CD123+), which promote Th2 cell responses. They are designated as DC1 (mDC) and DC2 (pDC), respectively.
Mazariegos et al. (2005) described an increased pDC/mDC ratio in tolerant recipients. According to their results, Reding et al. (2006) speculated that a pDC1/pDC2 subset ratio of 0.1 could serve as the threshold above which a patient might be considered for IS weaning. However, differences in the distribution of pDC in operationally tolerant LTRs have not been confirmed by all studies (Martinez-Llordella et al. 2007).
Moreover, mDC express higher levels of histocompatibility antigen, class I, G (HLA-G) in operational recipients than in IS-dependent patients or healthy controls, and these data are independent on the kind and dose of immunosuppressive drug. In addition, increased Foxp3 expression in Treg LTRs tolerant operationally correlated with the level of HLA-G expressed by mDC (Mazariegos et al. 2005).
Potential Applications to Prognosis, Other Diseases, or Conditions
AR and CR represent important complications in the managing and prognosis of OLT. After clinical suspicion, their diagnosis supposes the histopathological evaluation of liver biopsies. Liver biopsies are costly, result in being insidious, and represent a risk for patients; thus, the finding of biomarkers allowing the early detection of these liver transplantation complications, and their differentiation from others with similar clinical signs and biochemical alterations, will be of important value for the monitoring and the better immunosuppression managing of LTRs and therefore in the prognosis of the OLT outcome.
The review of the different potential immunological biomarkers that have been evaluated in the literature shows that most of the obtained results are inconclusive, either because biomarkers have not been studied in patients with other OLT complications, or, despite of doing it, they have showed similar patterns hampering the differentiation of rejection from other OLT complications; have been achieved from a reduced number of patients, since more studies, including higher number of patients, are needed; and require further validation, with the performance of prospective independent larger multicenter trials. Few of the reviewed biomarkers fulfill all these criteria and can be honestly considered as future potential AR biomarkers to be set up in the clinical practice. The most valuable of the reviewed biomarkers are summarized in Table 4. Despite the promising results of these biomarkers, its application to the clinics should entail further studies and validations.
Contrary to AR, where significant advances have been carried out in the discovery of biomarkers, in CR there is a considerable lack of studies in this sense, maybe because of its low prevalence and the variability among patients, which makes it impossible to suggest any future potential biomarker to diagnoses this complication. Therefore, the discovery of future noninvasive biomarkers of CR is a worthy field to investigate.
On the other hand, advances and studies using new techniques, in the fields of genomics, transcriptomics, and proteomics, have provided new potential biomarkers. And despite the few studies developed and the number of patients included, promising results have been obtained, especially in the field of proteomics. For sure, the revolution of the -omics era will allow the finding of more robust, sensitive, and specific biomarkers.
In relation to AMR of liver allografts, the identification of the impact of preformed and de novo DSAs in AMR would allow to differentiate this kind of complication that until now had been mistaken with other OLT complications, as AR. Moreover, preformed DSA analyses would help to predict LTRs at risk of rejection before transplant, percentage of graft survival, and therefore OLT outcome. As well, after transplantation, certain DSA identification would allow to identify patients that need a closer monitoring, in order to prevent rejection , before irreversible allograft injury is developed. However, the controversy of some studies makes mandatory the performance of further prospective multicenter studies to identify the class of DSAs implicated in AMR. Moreover, advances in analytical techniques will permit to progress in the use of DSAs. In the next years, DSAs will be very useful in the prognosis of liver transplantation outcomes, even prior to transplant. In other solid organ transplantations, as the kidney or heart, DSAs are widely accepted as a risk factor for decreased graft survival, and their determination helps to predict transplantation outcomes.
With regard to allograft tolerance , establishing biomarkers related with graft acceptance would allow assessing the real suppression state of the immune system after liver transplantation. In this way, transplant clinicians could modulate the immunosuppressive therapy depending on patients’ needs and identify liver transplant recipients who can discontinue or reduce the dosage of IS drugs without graft rejection. Indeed, this could allow the choice of immunosuppressor molecule, dosage adjustment, and target therapeutic window. Furthermore, establishing biomarkers of operational tolerance may provide tools to determine endpoints for tolerance induction trials, provide biological basis for guiding IS weaning protocols, and predict the success of withdrawal.
Against this background, the routine implementation of biomarkers and personalized therapy in patients would enable to revolutionize the quality of life of transplant recipients, with less exposure to toxicity or other adverse effects associated with immunosuppressive treatment, as well as a reduction in drug costs.
Summary Points
-
Biomarkers of liver allograft rejection and tolerance would be very useful in the managing of LTRs after transplantation, which would considerably improve liver transplantation outcomes.
-
Multiple potential biomarkers for liver AR, related to the immune system, have been studied; however, few of them permit to distinguish AR from other OLT complications or have been validated in later prospective multicenter trials.
-
There is a lack of studies about potential biomarkers for liver allograft CR, maybe because of its low prevalence in LTRs; however, considering that CR can be underestimated, it will be very worthy to invest efforts in their study.
-
As the role of DSAs (types of DSAs, levels needed, analyses) in liver AMR is elucidated, their use as biomarkers will allow to recognize LTRs in risk of suffering AMR, even before transplant, which will improve allograft survival and OLT outcomes.
-
Some potential biomarkers of allograft tolerance, as NK cells, have been identified. They will allow a better managing of patient immunosuppression reducing adverse effects of immunosuppressors.
-
Data available for biomarkers of graft acceptance are more encouraging compared to biomarkers of AR.
-
Development of analytical techniques will allow finding more specific and sensitive biomarkers for liver allograft rejection and tolerance.
-
More prospective and multicenter trials are required before the reliable implementation of biomarkers of rejection and tolerance in the clinical practice of LTRs.
Abbreviations
- ALT:
-
Alanine transaminase
- AMR:
-
Antibody-mediated rejection
- APCs:
-
Antigen-presenting cells
- AR:
-
Acute rejection
- BEC:
-
Biliary epithelial cells
- C1q:
-
Complement component 1q
- C4:
-
Complement component 4
- CLU:
-
Clusterin
- CMV:
-
Cytomegalovirus
- CR:
-
Chronic rejection
- DC:
-
Dendritic cells
- DSAs:
-
Donor-specific human alloantibodies
- GBP2:
-
Guanylate-binding protein 2
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HLA:
-
Human leukocyte antigen
- HLA-G:
-
Human leukocyte antigen, class I, G
- ICAM-1:
-
Intercellular adhesion molecule 1
- IFN-γ:
-
Interferon gamma
- IL-2:
-
Interleukin 2
- IL-6:
-
Interleukin 6
- IL-8:
-
Interleukin 8
- IL-10:
-
Interleukin 10
- IL-23:
-
Interleukin 23
- IRF5:
-
Interferon regulatory factor 5
- IS:
-
Immunosuppression)
- Krt19:
-
Cytokeratin-19
- LCN2:
-
Lipocalin-2
- LTRs:
-
Liver transplant recipients
- MCS:
-
Median channel shift
- MFI:
-
Mean fluorescent intensity
- MHC:
-
Major histocompatibility complex
- miRNA:
-
microRNA
- NK:
-
Natural killer cells
- OLT:
-
Orthotopic liver transplantation
- PBMC:
-
Peripheral blood mononuclear cell
- RAI:
-
Rejection activity index
- sIL2-R:
-
Soluble interleukin 2 receptor
- SPIs:
-
Solid-phase immunoassays
- Th1:
-
Type 1 helper T cells
- TLR4:
-
Toll-like receptor 4
- TNF-α:
-
Tumor necrosis factor-alpha
- Treg cells:
-
Regulatory T cells
- VCAM-1:
-
Vascular cell adhesion protein 1
References
Abraham SC, Furth EE. Receiver operating characteristic analysis of serum chemical parameters as tests of liver transplant rejection and correlation with histology. Transplantation. 1995;59:740–6.
Adam R, Karam V, Delvart V, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol. 2012;57:675–88. doi:10.1016/j.jhep.2012.04.015.
Adams DH, Wang L, Hubscher SG, Elias E, Neuberger JM. Soluble interleukin-2 receptors in serum and bile of liver transplant recipients. Lancet. 1989;1:69–71.
Adams DH, Sanchez-Fueyo A, Samuel D. From immunosuppression to tolerance. J Hepatol. 2015;62:S170–85. doi:10.1016/j.jhep.2015.02.042.
Afzali B, Lombardi G, Lechler RI. Pathways of major histocompatibility complex allorecognition. Curr Opin Organ Transplant. 2008;13:438–44. doi:10.1097/MOT.0b013e328309ee31.
Akoglu B, Kriener S, Martens S, et al. Interleukin-2 in CD8+ T cells correlates with Banff score during organ rejection in liver transplant recipients. Clin Exp Med. 2009;9:259–62. doi:10.1007/s10238-009-0042-4.
Asaoka T, Kato T, Marubashi S, et al. Differential transcriptome patterns for acute cellular rejection in recipients with recurrent hepatitis C after liver transplantation. Liver Transpl. 2009;15:1738–49. doi:10.1002/lt.21883.
Barnes EJ, Abdel-Rehim MM, Goulis Y, et al. Applications and limitations of blood eosinophilia for the diagnosis of acute cellular rejection in liver transplantation. Am J Transplant. 2003;3:432–8.
Berberat PO, Friess H, Schmied B, et al. Differentially expressed genes in postperfusion biopsies predict early graft dysfunction after liver transplantation. Transplantation. 2006;82:699–704.
Bohne F, Martínez-Llordella M, Lozano JJ, et al. Intra-graft expression of genes involved in iron homeostasis predicts the development of operational tolerance in human liver transplantation. J Clin Invest. 2012;122:368–82. doi:10.1172/JCI59411.
Boleslawski E, Conti F, Sanquer S, et al. Defective inhibition of peripheral CD8+ T cell IL-2 production by anti-calcineurin drugs during acute liver allograft rejection. Transplantation. 2004;77:1815–20.
Boleslawski E, BenOthman S, Grabar S, et al. CD25, CD28 and CD38 expression in peripheral blood lymphocytes as a tool to predict acute rejection after liver transplantation. Clin Transpl. 2008;22:494–501. doi:10.1111/j.1399-0012.2008.00815.x.
Castellaneta A, Mazariegos GV, Nayyar N, Zeevi A, Thomson AW. HLA-G level on monocytoid dendritic cells correlates with regulatory T cell Foxp3 expression in liver transplant tolerance. Transplantation. 2011;91:1132–40. doi:10.1097/TP.0b013e31821414c9.
Castillo-Rama M, Castro MJ, Bernardo I, et al. Preformed antibodies detected by cytotoxic assay or multibead array decrease liver allograft survival: role of human leukocyte antigen compatibility. Liver Transpl. 2008;14:554–62. doi:10.1002/lt.21408.
Conti F, Calmus Y, Rouer E, et al. Increased expression of interleukin-4 during liver allograft rejection. J Hepatol. 1999;30:935–43.
Conti F, Frappier J, Dharancy S, et al. Interleukin-15 production during liver allograft rejection in humans. Transplantation. 2003;76:210–6.
Dienstag JL, Cosimi AB. Liver transplantation – a vision realized. N Engl J Med. 2012;367:1483–5. doi:10.1056/NEJMp1210159.
Fábrega E, López-Hoyos M, San Segundo D, Casafont F, Pons-Romero F. Changes in the serum levels of interleukin-17/interleukin-23 during acute rejection in liver transplantation. Liver Transpl. 2009;15:629–33. doi:10.1002/lt.21724.
Fan H, Li LX, Han DD, Kou JT, Li P, He Q. Increase of peripheral Th17 lymphocytes during acute cellular rejection in liver transplant recipients. Hepatobiliary Pancreat Dis Int. 2012;11:606–11.
Farid WR, Pan Q, van der Meer AJ, et al. Hepatocyte-derived microRNAs as serum biomarkers of hepatic injury and rejection after liver transplantation. Liver Transpl. 2012;18:290–7. doi:10.1002/lt.22438.
Foster PF, Sankary HN, Hart M, Ashmann M, Williams JW. Blood and graft eosinophilia as predictors of rejection in human liver transplantation. Transplantation. 1989;47:72–4.
García-Alonso AM, Minguela A, Muro M, et al. CD28 expression on peripheral blood T lymphocytes after orthotopic liver transplant: upregulation in acute rejection. Hum Immunol. 1997;53:64–72.
Germani G, Rodriguez-Castro K, Russo FP, et al. Markers of acute rejection and graft acceptance in liver transplantation. World J Gastroenterol. 2015;21:1061–8. doi:10.3748/wjg.v21.i4.1061.
Girmanova E, Hruba P, Viklicky O. Circulating biomarkers of tolerance. Transplant Rev. 2015;29:68–72. doi:10.1016/j.trre.2015.01.003.
Goto S, Noguchi T, Lynch SV, et al. Is regular measurement of adhesion molecules and cytokines useful to predict post-liver transplant complications? Transplant Proc. 1998;30:2975–6.
He Q, Fan H, Li JQ, et al. Decreased circulating CD4+CD25highFoxp3+ T cells during acute rejection in liver transplant patients. Transplant Proc. 2011;43:1696–700. doi:10.1016/j.transproceed.2011.03.084.
Kaneku H, O’Leary JG, Banuelos N, et al. De Novo donor-specific HLA antibodies decrease patient and graft survival in liver transplant recipients. Am J Transplant. 2013;13:1541–8. doi:10.1111/ajt.12212.
Kita Y, Iwaki Y, Demetris AJ, Starzl TE. Evaluation of sequential serum interleukin-6 levels in liver allograft recipients. Transplantation. 1994;57:1037–41.
Kobayashi S, Nagano H, Marubashi S, et al. Guanylate-binding protein 2 mRNA in peripheral blood leukocytes of liver transplant recipients as a marker for acute cellular rejection. Transpl Int. 2010;23:390–6. doi:10.1111/j.1432-2277.2009.00991.x.
Kozlowski T, Rubinas T, Nickeleit V, et al. Liver allograft antibody-mediated rejection with demonstration of sinusoidal C4d staining and circulating donor-specific antibodies. Liver Transpl. 2011;17:357–68. doi:10.1002/lt.22233.
Lalli E, Meliconi R, Conte R, et al. Serum markers of immune activation and liver allograft rejection. Dig Dis Sci. 1992;37:1116–20.
Lang T, Krams SM, Villanueva JC, Cox K, So S, Martinez OM. Differential patterns of circulating intercellular adhesion molecule-1 (cICAM-1) and vascular cell adhesion molecule-1 (cVCAM-1) during liver allograft rejection. Transplantation. 1995;59:584–9.
Leonard GR, Shike H, Uemura T, et al. Liver transplantation with a strongly positive crossmatch: case study and literature review. Liver Transpl. 2013;19:1001–10. doi:10.1002/lt.23694.
Lerut J, Sanchez-Fueyo A. An appraisal of tolerance in liver transplantation. Am J Transplant. 2006;6:1774–80.
Li Y, Zhao X, Cheng D, et al. The presence of Foxp3 expressing T cells within grafts of tolerant human liver transplant recipients. Transplantation. 2008;86:1837–43. doi:10.1097/TP.0b013e31818febc4.
Li L, Wozniak LJ, Rodder S, et al. A common peripheral blood gene set for diagnosis of operational tolerance in pediatric and adult liver transplantation. Am J Transplant. 2012;12:1218–28. doi:10.1111/j.1600-6143.2011.03928.x.
Londoño MC, Danger R, Giral M, Soulillou JP, Sánchez-Fueyo A, Brouard S. A need for biomarkers of operational tolerance in liver and kidney transplantation. Am J Transplant. 2012;12:1370–7. doi:10.1111/j.1600-6143.2012.04035.x.
Lorho R, Turlin B, Aqodad N, et al. C4d: a marker for hepatic transplant rejection. Transplant Proc. 2006;38:2333–4.
Lunz JG, Contrucci S, Ruppert K, et al. Replicative senescence of biliary epithelial cells precedes bile duct loss in chronic liver allograft rejection: increased expression of p21(WAF1/Cip1) as a disease marker and the influence of immunosuppressive drugs. Am J Pathol. 2001;158:1379–90.
Martínez-Llordella M, Puig-Pey I, Orlando G, et al. Multiparameter immune profiling of operational tolerance in liver transplantation. Am J Transplant. 2007;7:309–19.
Martínez-Llordella M, Lozano JJ, Puig-Pey I, et al. Using transcriptional profiling to develop a diagnostic test of operational tolerance in liver transplant recipients. J Clin Invest. 2008;118:2845–57. doi:10.1172/JCI35342.
Massoud O, Heimbach J, Viker K, et al. Noninvasive diagnosis of acute cellular rejection in liver transplant recipients: a proteomic signature validated by enzyme-linked immunosorbent assay. Liver Transpl. 2011;17:723–32. doi:10.1002/lt.22266.
Mazariegos GV, Zahorchak AF, Reyes J, Chapman H, Zeevi A, Thomson AW. Dendritic cell subset ratio in tolerant, weaning and non-tolerant liver recipients is not affected by extent of immunosuppression. Am J Transplant. 2005;5:314–22.
Millán O, Rafael-Valdivia L, Torrademé E, et al. Intracellular IFN-γ and IL-2 expression monitoring as surrogate markers of the risk of acute rejection and personal drug response in de novo liver transplant recipients. Cytokine. 2013;61:556–64. doi:10.1016/j.cyto.2012.10.026.
Mimuro J, Mizuta K, Kawano Y, et al. Impact of acute cellular rejection on coagulation and fibrinolysis biomarkers within the immediate post-operative period in pediatric liver transplantation. Pediatr Transplant. 2010;14:369–76. doi:10.1111/j.1399-3046.2009.01248.x.
Minguela A, Miras M, Bermejo J, et al. HBV and HCV infections and acute rejection differentially modulate CD95 and CD28 expression on peripheral blood lymphocytes after liver transplantation. Hum Immunol. 2006;67:884–93.
Neuberger J. Incidence, timing, and risk factors for acute and chronic re-jection. Liver Transpl Surg. 1997;5:S30–6.
Neumann UP, Langrehr JM, Neuhaus P. Chronic rejection after human liver transplantation. Graft. 2002;5:102–7.
Ninova DI, Wiesner RH, Gores GJ, Harrison JM, Krom RA, Homburger HA. Soluble T lymphocyte markers in the diagnosis of cellular rejection and cytomegalovirus hepatitis in liver transplant recipients. J Hepatol. 1994;21:1080–5.
O’Leary JG, Kaneku H, Jennings LW, et al. Preformed class II donor-specific antibodies are associated with an increased risk of early rejection after liver transplantation. Liver Transpl. 2013;19:973–80. doi:10.1002/lt.23687.
O’Leary JG, Demetris AJ, Friedman LS, et al. The role of donor-specific HLA alloantibodies in liver transplantation. Am J Transplant. 2014a;14:779–87. doi:10.1111/ajt.12667.
O’Leary JG, Kaneku H, Demetris AJ, et al. Antibody-mediated rejection as a contributor to previously unexplained early liver allograft loss. Liver Transpl. 2014b;20:218–27. doi:10.1002/lt.23788.
O’Leary JG, Kaneku H, Banuelos N, Jennings LW, Klintmalm GB, Terasaki PI. Impact of IgG3 subclass and C1q-fixing donor-specific HLA alloantibodies on rejection and survival in liver transplantation. Am J Transplant. 2015;15:1003–13. doi:10.1111/ajt.13153.
Oetting WS, Guan W, Schladt DP, et al. Donor polymorphisms of TLR4 associated with graft failure in liver transplant recipients. Liver Transpl. 2012;18:1399–405. doi:10.1002/lt.23549.
Perkins JD, Nelson DL, Rakela J, Grambsch PM, Krom RA. Soluble interleukin-2 receptor level as an indicator of liver allograft rejection. Transplantation. 1989;47:77–81.
Platz KP, Mueller AR, Haller GW, et al. Determination of alpha- and Pi-glutathione-S-transferase will improve monitoring after liver transplantation. Transplant Proc. 1997;29:2827–9.
Pons JA, Revilla-Nuin B, Baroja-Mazo A, et al. FoxP3 in peripheral blood is associated with operational tolerance in liver transplant patients during immunosuppression withdrawal. Transplantation. 2008;86:1370–8. doi:10.1097/TP.0b013e318188d3e6.
Pons JA, Revilla-Nuin B, Ramírez P, Baroja-Mazo A, Parrilla P. Development of immune tolerance in liver transplantation. Gastroenterol Hepatol. 2011;34:155–69. doi:10.1016/j.gastrohep.2010.11.007.
Puig-Pey I, Bohne F, Benitez C, et al. Characterization of gammadelta T cell subsets in organ transplantation. Transpl Int. 2010;23:1045–55. doi:10.1111/j.1432-2277.2010.01095.x.
Raschzok N, Reutzel-Selke A, Schmuck RB, et al. CD44 and CXCL9 serum protein levels predict the risk of clinically significant allograft rejection after liver transplantation. Liver Transpl. 2015. doi:10.1002/lt.24164.
Ravaioli M, Neri F, Lazzarotto T, et al. Immunosuppression modifications based on an immune response assay: results of a randomized. Control Trial Transplant. 2015. doi:10.1097/TP.0000000000000650.
Reding R, Gras J, Truong DQ, Wieërs G, Latinne D. The immunological monitoring of alloreactive responses in liver transplant recipients: a review. Liver Transpl. 2006;12:373–83.
Rodrigo E, López-Hoyos M, Corral M, et al. ImmuKnow as a diagnostic tool for predicting infection and acute rejection in adult liver transplant recipients: a systematic review and meta-analysis. Liver Transpl. 2012;18:1245–53. doi:10.1002/lt.23497.
Rodríguez-Perálvarez M, Germani G, Tsochatzis E, et al. Predicting severity and clinical course of acute rejection after liver transplantation using blood eosinophil count. Transpl Int. 2012;25:555–63. doi:10.1111/j.1432-2277.2012.01457.x.
Sánchez-Fueyo A. Hot-topic debate on tolerance: immunosuppression withdrawal. Liver Transpl. 2011;17:S69–73. doi:10.1002/lt.22421.
Scornik JC, Soldevilla-Pico C, Van der Werf WJ, et al. Susceptibility of liver allografts to high or low concentrations of preformed antibodies as measured by flow cytometry. Am J Transplant. 2001;1:152–6.
Testro AG, Visvanathan K, Skinner N, et al. Acute allograft rejection in human liver transplant recipients is associated with signaling through toll-like receptor 4. J Gastroenterol Hepatol. 2011;26:155–63. doi:10.1111/j.1440-1746.2010.06324.x.
Thurairajah PH, Carbone M, Bridgestock H, et al. Late acute liver allograft rejection; a study of its natural history and graft survival in the current era. Transplantation. 2013;95:955–9. doi:10.1097/TP.0b013e3182845f6c.
Umeshita K, Monden M, Tono T, et al. Determination of the presence of interleukin-6 in bile after orthotopic liver transplantation. Its role in the diagnosis of acute rejection. Ann Surg. 1996;223:204–11.
Wang Y, Zhang M, Liu ZW, et al. The ratio of circulating regulatory T cells (Tregs)/Th17 cells is associated with acute allograft rejection in liver transplantation. PLoS One. 2014;9:e112135. doi:10.1371/journal.pone.0112135.
Warlé MC, Metselaar HJ, Hop WC, et al. Early differentiation between rejection and infection in liver transplant patients by serum and biliary cytokine patterns. Transplantation. 2003;75:146–51.
Wei L, Gong X, Martinez OM, Krams SM. Differential expression and functions of microRNAs in liver transplantation and potential use as non-invasive biomarkers. Transpl Immunol. 2013;29:123–9. doi:10.1016/j.trim.2013.08.005.
Wei W, Huang XH, Liang D, Zeng YY, et al. A proteomic analysis of transplanted liver in a rat model of chronic rejection. Clin Res Hepatol Gastroenterol. 2015;39:340–50. doi:10.1016/j.clinre.2014.10.005.
Yu X, Liu Z, Wang Y, et al. Characteristics of Vδ1(+) and Vδ2(+) γδ T cell subsets in acute liver allograft rejection. Transpl Immunol. 2013;29:118–22. doi:10.1016/j.trim.2013.09.001.
Yu X, Wei B, Dai Y, et al. Genetic polymorphism of interferon regulatory factor 5 (IRF5) correlates with allograft acute rejection of liver transplantation. PLoS One. 2014;9:e94426. doi:10.1371/journal.pone.0094426.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media Dordrecht
About this entry
Cite this entry
Solanas, E., Martínez-Crespo, E., Lue, A., Baptista, P., Serrano, M.T. (2017). Immunological Biomarkers in Liver Transplantation. In: Patel, V., Preedy, V. (eds) Biomarkers in Liver Disease. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-7675-3_17
Download citation
DOI: https://doi.org/10.1007/978-94-007-7675-3_17
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-7674-6
Online ISBN: 978-94-007-7675-3
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences