Abstract
A large variety of peripheral neuropathies, myopathies, and central nervous system abnormalities cause dysphagia (Bucholz 1987). Dysphagia can result from any abnormality involving the peripheral or cranial sensory or motor nerves, the swallowing center in the brainstem, or the supratentorial regions of the brain controlling tongue function, cognitive function involved in swallowing or muscular movement of the bolus to the lips. In our practice, the most common neurogenic causes of dysphagia are acute cerebrovascular accidents, small vessel ischemic disease, Parkinson’s disease, multiple sclerosis, myasthenia gravis, muscular dystrophy, and dermatomyositis. Patients who have undergone cranial, neck, and thoracic operations may have direct intracranial, central cranial nerve or recurrent laryngeal nerve damage. Some postoperative patients have postoperative cerebrovascular damage. Any patient with a tracheostomy tube may have dysphagia due to impaired elevation of the pharynx/larynx with poor timing between the oral and pharyngeal phase and/or diminished epiglottic tilt.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Motor Disorders of the Pharynx
A large variety of peripheral neuropathies, myopathies, and central nervous system abnormalities cause dysphagia (Bucholz 1987). Dysphagia can result from any abnormality involving the peripheral or cranial sensory or motor nerves, the swallowing center in the brainstem, or the supratentorial regions of the brain controlling tongue function, cognitive function involved in swallowing or muscular movement of the bolus to the lips. In our practice, the most common neurogenic causes of dysphagia are acute cerebrovascular accidents, small vessel ischemic disease, Parkinson’s disease, multiple sclerosis, myasthenia gravis, muscular dystrophy, and dermatomyositis. Patients who have undergone cranial, neck, and thoracic operations may have direct intracranial, central cranial nerve or recurrent laryngeal nerve damage. Some postoperative patients have postoperative cerebrovascular damage. Any patient with a tracheostomy tube may have dysphagia due to impaired elevation of the pharynx/larynx with poor timing between the oral and pharyngeal phase and/or diminished epiglottic tilt.
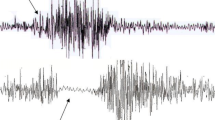
There is often very poor correlation between the clinically or radiologically perceived swallowing dysfunction and the presumed CNS or peripheral location of the disease. This reflects the complex nature of the swallowing system, the difficulty of clinical examination, and the low resolution of MRI in detecting disease in the bulbar tracts or the small sensory (nucleus fasciculus and tractus solitarius) and motor (nucleus ambiguous) regions of the brainstem. For example, aspiration is clinically silent in at least one third of patients who aspirate (Fig. 6.1).
Asymptomatic patient with laryngeal penetration and nasal regurgitation after radiotherapy for nasopharyngeal carcinoma. Radiograph obtained during swallowing with patient in right lateral position. The bolus has entered the oropharynx and hypopharynx. Barium is entering the nasopharynx (long arrow) around a bulbous, truncated soft palate (S). Barium penetrates into the laryngeal vestibule (short arrows), below a thick, bulbous epiglottis (e). The hyoid bone (H) and thyroid cartilage (T) are pulled normally together. Pharyngeal paresis is manifested as absence of the indentation on the posterior pharyngeal wall by one of the constrictor muscles
Pharyngography is used to determine (1) if there is a swallowing problem, (2) if the patient can swallow safely, and (3) the specific oral, pharyngeal, and/or esophageal location of the problem. When performed with a speech pathologist, the pharyngogram is used to determine modifications of swallowing that can provide the patient nutrition, hydration, and pleasurable eating. This radiologist believes that most modifications of swallowing do not contribute to healing of the underlying condition, but instead, prevent aspiration pneumonia, while the underlying disease hopefully improves or heals.
In some patients, the pattern of swallowing dysfunction suggests a specific location of disease. This specificity may uncover an etiology of swallowing dysfunction different than the clinical history suggests. For example, a recurrent laryngeal nerve may be temporarily or permanently damaged during cardiac or other forms of chest surgery (Fig. 6.2). Recurrent laryngeal nerve change results in abnormal epiglottic tilt (Fig. 6.3) and/or abnormal cricopharyngeal muscle function, resulting in subepiglottic laryngeal penetration or abnormal opening of the cricopharyngeus with stasis in the lower hypopharynx, respectively. Chest surgery or tracheostomy also results in poor elevation of the pharynx and larynx due to edema, hemorrhage, inflammation, or fibrosis in the soft tissues of the mediastinum or lower neck. Laryngeal and pharyngeal fixation results in poor epiglottic tilt related to poor hyoid elevation and diminished pull on the hyoepiglottic ligament. Poor pharyngeal and laryngeal elevation also results in diminished opening of the pharyngoesophageal segment. Therefore, a patient who has undergone chest surgery may have abnormal epiglottic tilt or abnormal function of the cricopharyngeus due to recurrent laryngeal nerve change or postoperative fixation of the laryngeal and pharynx. If a patient post chest surgery has tongue, palate, or middle constrictor dysfunction, however, the radiologist must suggest that another process is present, such as a perioperative stroke.
Stasis with overflow aspiration after chest surgery with left recurrent laryngeal nerve resection. (a) Radiograph obtained with the patient in the frontal position. A large volume of residual barium in the valleculae (left vallecula identified by V) results from absent epiglottic tilt. A large volume of residual barium in the left piriform sinus (P) is due to poor contraction of the left lower thyropharyngeal muscle. Barium flows from the left piriform sinus through the interarytenoid notch into the laryngeal vestibule (arrow). (b) Radiograph obtained with the patient in a lateral position shows a large volume of barium in the laryngeal vestibule (arrow) extending to the level of the anterior commissure. The lateral view shows residual barium in the piriform sinuses (P) but does not demonstrate that the barium is only in the left piriform sinus
Asymmetry of epiglottic tilt after cardiac surgery. Radiograph obtained with the patient in the frontal position as the bolus passes through the hypopharynx into the cervical esophagus. The left side of the epiglottis (short arrow) is tilting normally. The right side of the epiglottis (long arrow) is not tilting
Tongue dysfunction is usually related to supratentorial CNS disease, myopathy, or damage due to surgery or radiation therapy. However, the hypoglossal nerve (XII) crosses the superficial surface of the hyoglossus muscle and may be damaged during neck surgery or radiation therapy.
Abnormal closure of the velopharyngeal portal is due to soft palate (X) or superior constrictor (IX and X) dysfunction. Nasal regurgitation may occur in the presence of normal soft palate function, however, after the soft palate descends normally due to incomplete clearance of bolus from the oropharynx. Oropharyngeal stasis can be attributed to poor tongue base retraction (hyoglossus/styloglossus/XII) or tongue muscle loss or dysfunction.
Atrophy of the constrictor musculature is radiographically manifested as close apposition of the barium-coated posterior pharyngeal wall and the cervical spine. Poor contraction of the middle and inferior constrictor also suggests neuropathy or myopathy involving the pharynx. Therefore, when global constrictor paresis is seen in the absence of radiation therapy, a neuropathy (such as amyotrophic lateral sclerosis) or myopathy (such as polymyositis) is suggested.
Abnormal cricopharyngeal muscle function can be often attributed to recurrent laryngeal change or abnormal hyoid bone elevation due to various forms of chest or neck surgery, as described above. Abnormal cricopharyngeal muscle dysfunction also occurs with any other disorder that alters hyoid elevation. Any disorder that diminishes pressure of the bolus will also diminish cricopharyngeal muscle opening. Thus, the wide variety of diseases that alter abnormal tongue base retraction, abnormal seal of the palatoglossal isthmus or velopharyngeal portal, or constrictor muscle activity can affect opening of the cricopharyngeus. If no oral or pharyngeal cause of abnormal cricopharyngeal opening is seen, diseases of the esophagus are suspected. Abnormal cricopharyngeal muscle opening is seen in patients with gastroesophageal reflux disease (Brady et al. 1995) or any disease that causes functional or mechanical esophageal obstruction. Abnormal cricopharyngeal muscle opening associated with esophageal disease is a reflexive response to protect the pharynx from regurgitated gastric or esophageal contents (Fig. 6.4), rather than a “dysfunction.” The patient often has a globus sensation.
Incomplete opening of pharyngoesophageal segment. Radiograph obtained with the patient in a steep oblique position, enabling visualization “through the shoulders.” An incompletely opening cricopharyngeus (long arrow) is manifested as a smooth-surfaced, rounded “bar” of tissue narrowing the lumen of the pharyngoesophageal segment. A tiny web (thin arrow) in the cervical esophagus prevents the bolus from flowing down the anterior wall
Pharyngeal Pouches and Diverticula
Pharyngeal pouches are transient outpouchings of various depths of the pharyngeal wall through areas of muscle gaps. Pharyngeal diverticula are persistent outpouchings through the same regions.
Lateral Pharyngeal Pouches and Diverticula
The most common outpouchings of the pharynx are lateral pharyngeal pouches. These sacs form during swallowing on the anterolateral wall of the proximal hypopharynx just below the level of the hyoid bone (Bachman et al. 1968; Rubesin et al. 1987). The sacs bulge into a relatively weak area between the hyoid bone and thyroid cartilage, covered by the thyrohyoid membrane, but unsupported by muscle. Thus, the space of weakness is bounded superiorly by the greater cornu of the hyoid bone, anteriorly by the thyrohyoid muscle, inferiorly by the ala of the thyroid cartilage, and posteriorly by the superior cornu of the thyroid cartilage and the stylopharyngeal muscle (Bachman et al. 1968). The superior laryngeal artery and internal branch of the superior laryngeal nerve penetrate the upper posterior corner of this space.
Lateral pharyngeal pouches form during swallowing as the hyoid bone and thyroid cartilage are brought together by the thyrohyoid muscles. The pouches may be unilateral or bilateral. A transient, smooth-walled, 5–15 mm, hemispheric protrusion develops on the lateral upper hypopharyngeal wall, just below the level of the hyoid bone, just above the potentially calcified edge of the thyroid cartilage (Fig. 6.5). Barium that remains in the pouch spills into the ipsilateral piriform sinus after the swallow passes. This delayed spill of barium may lead to a sensation of incomplete swallowing, a need to double swallow, or rarely coughing or choking due to laryngeal penetration or the regurgitation of undigested food (Curtis et al. 1988; Lindbichler et al. 1998). On lateral views, the pouches are seen as transient barium-filled sacs on the anterior wall of the hypopharynx just below the hyoid bone, just behind the anterior wall of the laryngeal vestibule.
Lateral pharyngeal pouches. Radiograph obtained with the patient in the frontal position as the barium bolus flows through the hypopharynx into the cervical esophagus. Smoothly contoured, 1.3-cm round, barium-filled pouches (arrows) protrude outside the expected contour of the lateral wall of the pharynx, just below the hyoid bone
Lateral pharyngeal diverticula are persistent protrusions of non-keratinizing squamous epithelium surrounded by areolar connective tissue at the same site as lateral pharyngeal pouches (Bachman et al. 1968). It is not known whether lateral pharyngeal diverticula derive from lateral pharyngeal pouches. However, these diverticula reportedly arise in patients with long-standing increased intrapharyngeal pressure, such as wind instrument players. On barium studies, lateral pharyngeal diverticula are manifested as persistent sacculations of the anterolateral pharyngeal wall, just below the hyoid bone (Fig. 6.6).
Lateral pharyngeal diverticulum. (a) Radiograph obtained with the patient in a frontal position just as the patient is performing a second swallow. A 1.5-cm ovoid, smoothly contoured sac (arrow) lies outside the expected contour of the pharynx. (b) Spot radiograph obtained with the patient in a lateral position. The diverticulum (arrow) is seen arising from the anterolateral wall of the uppermost hypopharynx, just below the hyoid bone (H). The epiglottis (e) is just beginning to tilt
Congenital Abnormalities
Congenital remnants of pharyngeal development are rarely seen in adults. Four paired outpouchings of the endodermal origin of pharynx develop, termed branchial pouches (Maran and Buchanan 1978; Hyams et al. 1988). The branchial pouches grow outward to meet four paired grooves of ectodermal origin that develop in the neck, termed branchial clefts. The external auditory meatus is formed by the first branchial cleft. The middle ear, Eustachian tube, and the floor of the tonsillar fossa derive from the second branchial cleft. The piriform sinus is formed from the third and fourth branchial pouches.
Persistence of branchial cleft or pouches results in sinus tracts, fistulae, or cysts (Maran and Buchanan 1978). The most common remnant is a branchial cleft cyst, but these only rarely fill during pharyngography. Branchial pouch sinuses or fistulae may, however, fill during pharyngography, usually seen as blind ending tracks. Branch pouch sinuses or fistula may arise from the tonsillar fossa (second pouch), the upper anterolateral piriform sinus (third pouch), or the lower anterolateral piriform sinus (fourth pouch).
The thyroid gland arises in the base of the tongue with the thyroglossal duct and descends to its position inferior to the thyroid cartilage. Persistence of the thyroglossal duct may result in cysts, sinuses, or fistula, but these are rarely seen in adults or during pharyngography. A thyroglossal duct tract is seen arising from the base of the tongue, midline and extending inferiorly anterior to the lateral vestibule (Fig. 6.7).
Zenker’s Diverticulum
Zenker’s diverticulum (posterior hypopharyngeal diverticulum) is an acquired herniation of mucosa through an area of congenital muscle weakness near the cricopharyngeal muscle. The anatomy of the cricopharyngeus is complex and varies between individuals (Zaino et al. 1967, 1970). The cricopharyngeus portion of the inferior constrictor muscle arises on one lateral edge of the cricoid cartilage, encircles the pharyngoesophageal segment, and attaches on the opposite side of the cricoid cartilage. The cricopharyngeus has no midline raphe and is separate from the thyropharyngeus portion of the inferior constrictor. In about one third of individuals, there is a gap between the paired thyropharyngeal muscles and the cricopharyngeus or between the obliquely and horizontally oriented fibers of the cricopharyngeal muscle itself (Zaino et al. 1970). This gap is known as Killian’s dehiscence.
During swallowing, Zenker’s diverticulum appears as a variably sized outpouching of the posterior inferior hypopharyngeal wall descending a variable distance posterior to an incompletely opening cricopharyngeus and upper cervical esophagus (Fig. 6.8). The neck of the diverticulum is broad during swallowing, but narrows after the bolus passes. After swallowing, barium refluxes into the hypopharynx, to be swallowed at a second or later swallow. If a large amount of barium refluxes superior to the level of the interarytenoid notch, barium may enter the laryngeal vestibule during breathing or during a subsequent swallow. Images obtained with the patient in a frontal position show a diverticulum of varying size midline below the tips of the piriform sinus (Fig. 6.9). Images obtained in the lateral view demonstrate a sac posterior to the expected contour of the pharyngoesophageal segment and posterior to the soft tissue of the cricopharyngeus and fibers of the upper cervical esophagus (see Figs. 6.8 and 6.9).
Zenker’s diverticulum. (a) Spot radiograph obtained after swallowing shows a 2-cm, smooth, ovoid sac (Z) posterior to a collapsed pharyngoesophageal segment. (b) Spot radiograph obtained during swallowing demonstrates the diverticulum (Z) posterior to an incompletely opening cricopharyngeal bar (arrow). A jet of barium flows down the anterior wall of the cervical esophagus. The opening of the diverticulum is wide (double arrow). Also note a slight diminished tilt of the epiglottis (e) resulting in mild laryngeal penetration
Zenker’s diverticulum. (a) Spot radiograph obtained with the patient in a frontal position. A 4-cm, smoothly contoured, ovoid, partly barium-filled sac (Z) lies midline below the tips of the piriform sinuses (left piriform sinus identified by long arrow). The left vallecula is identified (v). (b) Spot radiograph obtained with the patient in a lateral position. The barium-filled sac (Z) is posterior to the expected course of the pharynx and cervical esophagus. The sac is separated from the collapsed lumen of the pharyngoesophageal segment (short arrows) by a thick radiolucent bar representing mucosa and the muscle fibers of the cricopharyngeus and the uppermost cervical esophagus. The valleculae (v) are identified
The pathogenesis of Zenker’s diverticulum is controversial (Knuff et al. 1982; Frieling et al. 1988). Opening of the tonically contracted cricopharyngeus depends on relaxation of the muscle (X via recurrent laryngeal nerve), pulling of the anterior wall of the pharyngoesophageal segment forward (suprahyoid muscles, thyrohyoid muscle, intrinsic pharyngeal elevators), and the pressure of the bolus (the weight of the bolus, preservation of the seal at the palatoglossal isthmus and nasopharynx, tongue base retraction, and contraction of the constrictor muscles). Thus, abnormalities in a variety of areas may lead to poor opening of the pharyngoesophageal segment and development of a diverticulum over time.
Almost all patients with a Zenker’s diverticulum have gastroesophageal reflux disease and a hiatal hernia (Smiley et al. 1970; Delahunty et al. 1971). It is this radiologist’s postulate that most patients with Zenker’s diverticulum have persistent closure of the cricopharyngeus as a reflexive response to protect the pharynx and larynx from gastroesophageal reflux. Manometric studies of the cricopharyngeus have not provided the answer, as there is variable resting or swallowing (relaxation) pressure of the cricopharyngeus and variable coordination of constrictor contraction with cricopharyngeal opening. Given the complexity of cricopharyngeal opening described above, a host of abnormalities may give rise to a Zenker’s diverticulum.
Clinically, patients with Zenker’s diverticulum complain of difficulty swallowing, regurgitation of undigested food, halitosis, choking, or a neck mass. Pulmonary complaints may be frequent due to aspiration pneumonia, bronchiectasis, or lung abscess. Other complications include ulceration due to stasis in the diverticulum, fistula formation, or development of carcinoma (less than 0.3% of patients) (Nanson 1976; Shirazi et al. 1977). A barium swallow demonstrating irregularity of the contour of the diverticulum suggests ulceration or tumor.
Proximal Lateral Cervical Esophageal Pouches and Diverticula
Pouches and diverticula of the proximal cervical esophagus may be confused with Zenker’s diverticulum; therefore, they are included in this chapter.
The longitudinal muscle of the esophagus is attached to the mid-posterior wall of the cricoid cartilage by a tendon (the suspensory tendon of the esophagus). The longitudinal muscle then descends and spreads laterally to envelop the cervical esophagus, forming the outer longitudinal muscle layer. As the larynx and pharynx rise during swallowing, the rising cricoid cartilage pulls the suspensory tendon superiorly, resulting in esophageal elevation. The Killian-Jamieson space (not to be confused with Killian’s dehiscence) is a triangular-shaped area just lateral to the suspensory tendon of the esophagus (Ekberg and Nylander 1983a). Thus, the Killian-Jamieson space is an area of esophageal muscle weakness bounded anteriorly by the inferior margin of the cricoid cartilage, inferomedially by the suspensory tendon of the esophagus, and superiorly by the cricopharyngeal muscle. Transient or persistent protrusions into the Killian-Jamieson space are termed proximal lateral cervical esophageal pouches or diverticula, respectively. These are also known as Killian-Jamieson pouches or diverticula.
Killian-Jamieson pouches are commonly seen during barium swallows as small (less than 1 cm) transient saccular protrusions of the lateral pharyngeal wall, just below the closing or closed cricopharyngeus. The pouches fill as the bolus passes, then empty, and disappear after the bolus passes.
Killian-Jamieson diverticula are not uncommon, seen with about one fourth the frequency of Zenker’s diverticulum (Rubesin 2001). These are bilateral or unilateral persistent sacculations that fill during swallowing. If unilateral, the pouch usually arises on the left side of the esophagus. With the patient in the frontal position, a Killian-Jamieson diverticulum appears a 3–20 mm round-oval smooth-surfaced outpouching of the lateral pharyngeal wall just below the cricopharyngeus muscle (Fig. 6.10). During swallowing, the neck of the diverticulum may be broad, but after swallowing, the neck narrows to several mm in luminal diameter. With the patient in a lateral position, the diverticulum appears as a sac partly anterior to the cervical esophagus. With the patient in a steep oblique position, the sac is anterior to the cervical esophagus (see Fig. 6.10). In contrast, Zenker’s diverticulum is a sac midline in the frontal view and, in the lateral view, originating superior to the cricopharyngeus and descending posterior to the wall of the cricopharyngeus and upper cervical esophagus.
Proximal lateral cervical esophageal diverticulum (Killian-Jamieson diverticulum). (a) Spot radiograph obtained with the patient in a frontal position. A smoothly contoured, 1×2 cm, partly barium-filled sac (K) is lateral to the uppermost cervical esophagus. The location of the closed cricopharyngeus is identified (short arrow). The opening of the diverticulum is seen on the lateral wall of the uppermost cervical esophagus (long arrow). The left piriform sinus is identified (P). (b) Spot radiograph obtained with the patient in a left posterior oblique position shows that the diverticulum (K) is anterior to the lumen of the collapsed cervical esophagus (arrow). The left piriform sinus is identified (P)
Inflammatory Disorders of the Pharynx
Acute or chronic inflammation of the pharynx may result in dysphagia. Edema and inflammation due to infection or severe gastroesophageal reflux may enlarge the epiglottis and stiffen its motion, leading to laryngeal penetration (Fig. 6.11). Laryngeal vestibule closure and vocal cord motion may be altered. Barium pharyngography may demonstrate pharyngeal candidal or herpetic infection in immunocompromised patients being studied to exclude candidal or herpes esophagitis (see Fig. 6.11).
Candida pharyngitis. Spot radiograph obtained with the patient in a lateral position. The pharyngeal mucosa is not smooth. Discrete 2-mm ovoid elevations (short arrows) are seen in the depths of the valleculae and posterior to the epiglottis. Barium-coating the laryngeal vestibule and laryngeal ventricle (long arrow) is the result of poor epiglottic tilt due to the inflammatory process
Barium pharyngography, however, is not a technique used in most patients with severe, acute sore throats. Theoretically, barium studies may exacerbate edema in patients with stridor, severe sore throat, and acute epiglottis. In patients with suspected acute epiglotitis, plain radiographs may be indicated to show enlargement of the epiglottis and aryepiglottic folds. Barium studies are utilized, however, to demonstrate the sequelae of chronic gastroesophageal reflux, scarring due to corrosive ingestion, or scarring due to severe ulcerative skin disease.
Pharyngeal mucosal ulceration occurs in patients with Behçet’s syndrome, Reiter’s syndrome, epidermolysis bullosa, benign mucous membrane pemphigoid, bullous pemphigoid, and corrosive ingestion (Bosma et al. 1968; Agha et al. 1983). With severe ulceration, the uvula or the tip of the epiglottis may be amputated. Healing may result in pharyngeal deformity and dysmotility.
Lymphoid Hyperplasia
The lingual tonsil is composed of 30–100 lymph follicles beneath the squamous mucosa of the base of the tongue, extending from the circumvallate papillae to the root of the epiglottis. Hypertrophy of the lingual tonsil is a response to aging, infection, and chronic allergic states, and is a compensatory response to palatine and adenoid tonsillectomy. Patients complain of throat discomfort and rarely dysphagia.
Radiographically, in the frontal view, many, 3–8 mm, smooth, ovoid nodules are symmetrically distributed across the base of the tongue (Fig. 6.12) (Gromet et al. 1982). On lateral images, the nodules protrude posteriorly. There is, however, no dividing line of nodularity in the base of the tongue, distinguishing normal lingual tonsil from lymphoid hyperplasia. With severe lymphoid hyperplasia, smooth nodules may extend onto the lingular surface of the epiglottis or into the uppermost hypopharynx. If the nodules are asymmetrically enlarged, mass-like, or asymmetrically distributed, endoscopy should be performed to exclude carcinoma.
Webs
A web is a thin fold composed of epithelium and lamina propria with underlying blood vessels (Clements et al. 1974). Webs are most frequently seen on the anterior wall of the lower hypopharynx and cervical esophagus, but are also found in the valleculae and lower lateral piriform sinuses (Ekberg 1981). Webs are seen in at least 10% of esophagrams and were found in 16% of patients at autopsy. It is not known whether webs are normal variants or due to healing after chronic inflammation (Nosher et al. 1975). Some webs are seen in patients with scarring due to epidermolysis bullosa, benign mucous membrane pemphigoid, lye ingestion, or radiation therapy (Agha et al. 1983; Scott et al. 1992). There is an association between patients with gastroesophageal reflux and cervical esophageal webs (Gordon et al. 2001). There is a weak association of cervical esophageal webs, iron deficiency anemia, and pharyngoesophageal junction squamous cell carcinoma (Plummer–Vinson syndrome/Patterson Kelly syndrome).
Radiographically, a web is a thin radiolucent mucosal shelf, either seen in the barium column (Fig. 6.13) or coated in barium. Webs may partly or fully encircle the cervical esophagus. Obstructive symptoms only occur when the lumen is markedly narrowed by a deep, shelf-like web or by a circumferential ring. Obstruction is implied radiographically by luminal narrowing greater than 50%, by dilatation of the cervical esophagus proximal to the web, and by a “jet” of barium spurting around or through the web (Shauffer et al. 1977). This radiologist does not test obstruction of cervical esophageal webs by using barium tablets or unchewed food. Instead, the luminal diameter is measured by placing a radioopaque object of known size at the same height from the fluoroscopic tabletop as the midneck/esophagus.
Cervical esophageal web. Spot radiograph obtained with the patient in a steep obliquity to “see through the shoulders.” A 3 mm deep by 0.5 mm in height radiolucent filling defect (arrow) is seen in the barium column passing through the pharyngoesophageal segment. The cricopharyngeus (arrowhead) does not completely open. The relationship of the web to the cricopharyngeus identifies its location in the pharyngoesophageal segment
Tumors of the Pharynx
Benign Tumors
Benign, non-epithelial tumors of the pharynx are uncommon. However, tumor-like cysts, such as retention cysts, are common (Bachman 1978). A retention cyst is lined by squamous epithelium, with its cystic center filled with desquamated debris.
Patients with base of tongue lesions are usually asymptomatic, but may complain of throat discomfort or dysphagia. The most common benign tumors of the base of the tongue are retention cysts (Woodfield et al. 2005) and granular cell tumors. Ectopic thyroid tissue and thyroglossal duct cysts are rare in adults.
Tumors in the aryepiglottic folds cause dysphonia, stridor, coughing, or dysphagia due to laryngeal penetration. The most common benign tumors of the aryepiglottic folds are retention cysts and saccular cysts. Saccular cysts arise from the mucus-secreting glands of the appendix of the laryngeal ventricle and are filled with mucoid secretions. Saccular cysts are a mucus-filled variant of an internal laryngocele.
Pedunculated tumors (papilloma, lipoma, and fibrovascular polyp) may cause choking, coughing, and dysphagia (Mansson et al. 1978). Large, pedunculated tumors may be coughed up into the oral cavity or cause sudden death through asphyxiation.
Patients with neurofibromatosis may have neurofibromas involving the aryepiglottic folds and submucosa overlying the muscular processes of the arytenoids (Chang-Lo 1977). About 40% of tumors arising from minor serous salivary glands are benign. Minor salivary gland tumors typically arise in the soft palate, oropharynx, and base of tongue (Fig. 6.14). Benign (chondroma) or malignant cartilaginous tumors usually arise in the posterior lamina of the cricoid cartilage.
A benign tumor, regardless of its histology, usually appears radiographically as a smooth-surfaced, round, sharply circumscribed mass en face, and as a hemispheric protrusion into the lumen in profile (see Fig. 6.14) (Seaman 1974; Rubesin and Glick 1988; Woodfield et al. 2005). These tumors, covered by normal, smooth appearing squamous mucosa, may be missed at endoscopy. Pedunculated tumors are rare.
Malignant Tumors
Squamous Cell Carcinoma
Squamous cell carcinoma accounts for greater than 90% of malignant oropharyngeal and hypopharyngeal tumors. Most squamous cell carcinomas are detected when patients are 50–70 years. More than 95% of patients have used alcohol and/or tobacco. Synchronous or metachronous squamous cell cancers of the oral cavity, pharynx, esophagus, and lung are seen in more than 20% of patients (Goldstein and Zornoza 1978). One to fifteen percent of patients with pharyngeal squamous cell carcinoma will develop a squamous cell carcinoma in the esophagus.
Squamous cell carcinoma has two main macroscopic forms: ulcerative tumors that penetrate deep into local soft tissue, cartilage, and bone and exophytic tumors that spread over the mucosa and into the pharyngeal lumen (Hyams et al. 1988). The ulcerative form of squamous cell carcinoma is radiographically manifested as an irregular, barium-filled contour extending beyond the expected smooth pharyngeal contour (Fig. 6.15) (Rubesin and Glick 1988). The normally smooth mucosal surface is disrupted by small elevated nodules or by small barium-filled crevices (Rubesin and Laufer 1991).
Ulcerated squamous cell carcinoma left piriform sinus. (a) Spot radiograph with the patient in a frontal position shows expansion of the left piriform sinus and mild irregularity of its contour (arrows). (b) Spot radiograph obtained with the patient in a near lateral position shows a 7-mm irregular contrast collection (arrow) arising from the tip of the piriform sinus (p). This ulcerated squamous cell carcinoma was not seen at endoscopy or a CT scan. A repeat endoscopy with biopsy proved the diagnosis
The exophytic form of squamous cell carcinoma is radiographically manifested as an intraluminal mass (Fig. 6.16). The expected smooth pharyngeal contour is lost. A soft tissue mass coated by barium extends into the pharyngeal air space. The surface of the mass is coarsely nodular, finely nodular, or granular (Rubesin and Laufer 1991). Barium fills crevices between tumor nodules or areas of ulceration. If a barium pool is present, the exophytic tumor is seen as a radiolucent filling defect in the barium pool.
Exophytic squamous cell carcinoma right lateral oropharyngeal wall. (a) Spot radiograph obtained with the patient in a frontal view shows loss of the contour of the lower right lateral oropharyngeal wall (arrowhead). Lobulated, barium-coated lines (arrows) are superimposed over the normal lymphoid tissue of the base of the tongue. (b) Spot radiograph obtained with the patient in a lateral position. The barium-coated edges of a mass (arrows) lie posterior to the tip of the epiglottis (e). Barium enters interstices of the tumor, manifested as barium lines and tiny collections, seen en face
With dynamic imaging, pharyngeal structures obliterated by tumor move poorly. For example, squamous cell carcinoma involving the epiglottis disrupts epiglottic tilt, resulting in laryngeal penetration. Images obtained during phonation show loss of distensibility of lateral pharyngeal walls.
Nasopharyngeal squamous cell carcinomas are usually undifferentiated tumors with a reactive lymphoid stroma. Poor ventilation, inhaled carcinogens, upper respiratory viruses, and nasal balms have been implicated as causative factors, as well as alcohol and tobacco use. Nasopharyngeal cancers typically occur at a younger age than most squamous cell carcinomas, with 20% of patients less than 30 years old. Barium studies evaluate symptoms of nasal regurgitation and dysphonia related to soft palate infiltration.
The palatine tonsil is the most common location for development of squamous cell carcinoma. These tumors spread to the base of tongue, soft palate, and posterior pharyngeal wall. A small squamous cell carcinoma may easily be missed on a pharyngogram in the normally nodular palatine tonsil.
Squamous cell carcinoma arising in the base of the tongue is typically a tumor that deeply infiltrates the tongue (Apter et al. 1984). Patients with base of tongue carcinoma often have few swallowing symptoms, but present with cervical lymphadenopathy. Small tumors may be difficult to detect endoscopically, as they are hidden in the valleculae or glossotonsillar recess. Flat or ulcerative lesions may be missed radiographically, as they are difficult to distinguish from the normally nodular vertical surface of the tongue.
Supraglottic squamous cell carcinomas are typically poorly differentiated tumors of the epiglottis (Fig. 6.17), aryepiglottic folds, mucosa overlying the muscular process of the arytenoids cartilages, false vocal cords and laryngeal ventricles. These tumors spread widely to the tongue and through the epiglottic cartilage to the pre-epiglottic space (Balfe and Heiken 1986). Supraglottic cancers rarely spread to the true vocal cords. Patients typically complain of dysphagia, choking, or coughing due to abnormal epiglottic tilt and laryngeal penetration.
Small epiglottic carcinoma missed on ENT examination. Spot radiograph obtained with the patient in a lateral position. A 7-mm finely lobulated mass (long arrow) expands the vallecular surface of the epiglottis. The tip and posterior surface of the epiglottis are smooth and normal (short arrows). The valleculae are identified (v). A biopsy on repeat endoscopy revealed a squamous cell carcinoma. This case illustrates the occasional difficulty of evaluating the valleculae
Squamous cell cancers of the piriform sinus are typically large lesions. Tumors of the medial wall of the piriform sinus may invade the ipsilateral aryepiglottic fold, arytenoid cartilage, and paraglottic space (Balfe and Heiken 1986). Invasion of the supraglottis results in hoarseness or symptoms of laryngeal penetration. Squamous cell carcinoma involving the lateral piriform sinus wall infiltrates the thyrohyoid membrane, thyroid cartilage, and neck, including the carotid sheath.
Patients with squamous cell carcinoma of the posterior pharyngeal wall are typically asymptomatic, presenting with bulky cervical nodal metastases. Posterior pharyngeal wall tumors are the form of pharyngeal squamous cell carcinoma most frequently associated with synchronous or metachronous lesions. Posterior wall tumors infiltrate superiorly into the nasopharynx, inferiorly into the cervical esophagus, and posteriorly into the prevertebral soft tissue. Tumors located in the depths of the piriform sinuses or lowermost hypopharyngeal wall may be missed at endoscopy (Fig. 6.18).
Squamous cell carcinoma of lower hypopharynx missed on ENT examination. Radiograph obtained with the patient in a lateral position. Most of the bolus is in the oropharynx. The soft palate (s) is elevating. A 3 cm in length radiolucency (arrowheads) is present in the lower hypopharynx. Tiny drops of barium and a small barium-filled ulcer (arrow) demonstrate the irregular surface of the tumor. This patient had one ENT exam 3 months before the pharyngogram and a second ENT examination 1 week before the study. Neither had seen the depths of the hypopharynx or diagnosed a tumor. A repeat ENT exam showed a posterior wall pharyngeal tumor, with a biopsy positive for squamous cell carcinoma
Squamous cell carcinoma arising in the post-cricoid region is the form of carcinoma most frequently associated with iron deficiency anemia and cervical esophageal webs (Plummer–Vinson syndrome.) This form of tumor is rare, except in Scandinavia. These annular, infiltrating lesions are best detected at pharyngography as the barium column traverses and distends the pharyngoesophageal segment.
Other Malignant Tumors
The lymphoid tissue of Waldeyer’s ring—the adenoids, palatine tonsils, and lingual tonsil—may give rise to non-Hodgkin’s lymphoma. Only 1–2% of patients with Hodgkin’s disease have pharyngeal involvement, despite the fact that Hodgkin’s disease often originates in cervical lymph nodes.
Pharyngeal lymphoma accounts for less than 10% of pharyngeal malignancies, with most patients presenting between 50 and 70 years of age. The palatine tonsil is the most frequent site of origin (about 60% of patients) (Hyams et al. 1988). Lymphoma involves right and left palatine tonsils in about 15% of these patients. The nasopharynx is involved in 18–28% of patients, the lingual tonsil in 10% of patients. Involvement of two or more sites is seen in 25% of patients.
Lymphomas are typically lobulated, smooth-surfaced masses involving the nasopharynx, base of tongue, or palatine tonsil (Fig. 6.19). The normal lymphoid pattern of the base of tongue may be obliterated by the infiltrating tumor. Despite the smooth submucosal infiltrating nature of the tumor, lymphoma may easily be confused radiographically with squamous cell carcinoma, given the lobulated surface and the infrequent incidence of lymphoma.
Non-Hodgkin’s lymphoma of lingual and right palatine tonsil. (a) Spot radiograph obtained with the patient in a frontal position shows a large, coarsely lobulated mass (arrows) involving the right oropharynx. (b) Spot radiograph obtained with the patient in a steep right posterior oblique position shows that the mass is composed of smooth 1-cm ovoid lobules involving the base of the tongue (small arrows) and right lateral oropharyngeal wall (long arrows)
Rare tumors of the pharynx include carcinoma arising in minor salivary glands, synovial sarcoma, malignant fibrous histiocytoma, chondrosarcoma, and Kaposi’s sarcoma (Hyams et al. 1988; Lakhani et al. 2005; Emery et al. 1986). Most minor salivary gland tumors are malignant (65–88%) and arise in the soft palate. The most frequent histologic types are adenoid cystic carcinoma (35%), solid adenocarcinoma (22%), and mucoepidermoid carcinoma (16%).
Chondrosarcoma typically arises in the posterior lamina of the cricoid cartilage (Hyams and Rabuzzi 1970). The tumor is usually detected on plain radiography or CT as a mass with central or peripheral stippled calcification. During pharyngography, this tumor compresses the pharyngoesophageal segment resulting in dysphagia.
Radiation Change
Radiation therapy is used as primary or adjuvant therapy for primary pharyngeal tumors such as squamous cell carcinoma or lymphoma. The pharynx may also be included in the radiation field during treatment of tumors of the larynx or cervical lymph nodes. Pharyngeal irradiation results in acute epithelial necrosis, ulceration, and submucosal edema. Long-term capillary and lymphatic damage leads to skin atrophy and fibrosis in subcutaneous, submucosal tissue and muscle. Thus, chronic radiation leads to persistent edema. Osteonecrosis and chondronecrosis with secondary infection may also occur.
Hoarseness, xerostomia, dysphagia, or a globus sensation usually subside 2–6 weeks after radiotherapy. Pharyngography performed during or immediately after radiation therapy may help determine if the patient is able to swallow safely. Pharyngography performed after acute radiation changes have subsided is helpful in determining whether persistent dysphagia is the result of pharyngeal dysfunction or due to a complication such as stricture formation or tumor recurrence.
Pharyngeal dysfunction is due to abnormal epiglottic tilt and laryngeal vestibule closure and pharyngeal constrictor paresis. The epiglottis is smooth and bulbous and the aryepiglottic folds are smooth, and thickened by submucosal edema (Fig. 6.20) (Goldstein et al. 1975). The edematous pharyngoepiglottic and median glossoepiglottic folds cause the vallecula to have a flat, effaced contour. The mucosa overlying the muscular processes of the arytenoids cartilage is elevated, swollen by edema. The global supraglottic edema results in poor or absent epiglottic tilt (Fig. 6.21) with subsequent laryngeal penetration. Poor pharyngeal constrictor muscle contraction is present. With long-standing disease, the soft palate is atrophic and the thickness of the retropharyngeal space is small due to constrictor muscle atrophy.
Radiation changes, pharynx. Spot radiographs of the pharynx obtained with patient in a frontal (a) and lateral (b) position. The soft palate is enlarged and smooth, with a bulbous uvular tip (s). The valleculae are flattened (right vallecula identified by v). The epiglottis is enlarged, with a smooth bulbous tip (e). The aryepiglottic folds are markedly thickened, but smooth (left aryepiglottic fold identified between arrows). The mucosa overlying the muscular processes of the arytenoids cartilages is elevated, worse on the right (right arytenoid identified by arrowhead). The right piriform sinus (p) is dilated, indicating muscle weakness. Barium-coating the laryngeal vestibule and laryngeal ventricle was due to laryngeal penetration related to absent epiglottic tilt
Abnormal epiglottic tilt due to radiation therapy. Radiograph obtained with the patient in a lateral position demonstrates an enlarged, bulbous soft palate (S). The epiglottis (arrow) is enlarged, markedly thickened, but smooth and shows moderately diminished tilt. This results in small volume subepiglottic laryngeal penetration (arrowhead). However, with repeat swallowing, barium is seen in the proximal trachea
Stricture formation may occur near the pharyngoesophageal segment after radiation therapy. Long, smooth strictures or thick webs (Fig. 6.22) narrow the lumen, resulting in dysphagia.
A post-radiation pharyngogram demonstrating tumor nodules or barium-filled crevices between nodules suggests the possibility of persistent or recurrent cancer (Quillen et al. 1993). Radiation-induced ulceration, however, may have similar radiographic findings.
The Postoperative State
This chapter will not discuss the wide variety of surgical procedures used to treat structural pharyngeal abnormalities. The reader is referred to several references for a detailed discussion (Rubesin et al. 2003; Ekberg and Nylander 1983b; Balfe et al. 1982; DiSantis et al. 1983). This chapter will focus on total laryngectomy and surgery for Zenker’s diverticulum as examples of how to approach the postoperative state.
Ideally, the radiological request slip describes the type of surgery performed and the information needed by the surgeon. In reality, the radiologist benefits from electronic access to the operative and pathology reports. In the immediate postoperative state, the pharyngogram helps determine whether the patient is swallow-safe and if a complication is present, such as laryngeal penetration or leak with fistula or abscess formation. In the remote postoperative state, the complications include persistent leak, ischemia of a muscle flap, stricture formation, abnormal function of the constrictor musculature, and persistent or recurrent tumor.
Total Laryngectomy
Advanced laryngeal cancer, subglottic carcinoma, and small carcinomas of the tongue base are treated by total laryngectomy. Total laryngectomy may be performed for recurrent tumor or osteonecrosis/chondronecrosis after radiation therapy or voice conserving surgery. An extended total laryngectomy and partial pharyngectomy is performed for cancers of the piriform sinus, lateral and posterior pharyngeal walls, and post-cricoid area.
During total laryngectomy, the surgeon removes the epiglottis, thyroid cartilage, arytenoid cartilages, cricoid cartilage, and internal soft tissues related to these structures. The hyoid bone may be removed or spared. Many of the muscles of the pharynx are detached from their bony or cartilaginous insertions. The suprahyoid and infrahyoid muscles are transected. The thyropharyngeus and cricopharyngeus are detached from the thyroid and cricoid cartilages, respectively. A tracheostoma is required for breathing. The ipsilateral lobe of the thyroid gland and nearby parathyroid glands may be removed. A neck dissection may be performed unilaterally or bilaterally. Depending on tumor size and spread, the submandibular gland, internal jugular vein, spinal accessory or hypoglossal nerves, external carotid artery and sternocleidomastoid muscle may be spared or removed.
Removal of epiglottis, aryepiglottic folds, mucosa overlying the arytenoid cartilages, and the anterior pharyngeal wall results in a large gap in the anterior and anterolateral wall of the pharynx. This gap is closed by approximating the residual pharyngeal mucosa and constrictor musculature. In some patients, the gap is so large that it must be closed by a free flap or myocutaneous flap.
The residual neopharynx is manifested radiographically as a tubular structure devoid of its original anterior pharyngeal wall (Fig. 6.23) (Balfe et al. 1982). The tubular neopharynx begins at the base of the tongue and extends to the cervical esophagus. Sacculations normally seen at the junction of the neopharyngeal tube and the base of the tongue mimic valleculae, hence the term pseudovalleculae. The neopharyngeal tube may be focally angulated as it is attached to the base of the tongue. The epiglottis, aryepiglottic folds, laryngeal vestibule, laryngeal ventricle, vocal cords, and proximal cervical trachea are missing. The soft tissues of the neck are narrowed; the anterior wall of the neopharyngeal tube lies just below the skin and the posterior wall of the neopharyngeal tube abuts the vertebral column. In some patients, a fold of tissue angles from the posterior oropharynx to the base of the tongue. The course of this lateral pharyngeal wall fold mimics the angle of the original epiglottis, hence the term pseudoepiglottis (Moses et al. 1993). When the patient is turned to the frontal position, the neopharyngeal tube is with 0.5 cm of the midline.
Total laryngectomy. (a) Spot radiograph obtained with the patient in a frontal position shows a tubular-shaped neopharynx. There is mild sacculation where the tube joins the tongue base (arrowhead). A voice prosthesis is seen in the upper thoracic esophagus. There is a small leak (arrow) around the voice prosthesis. (b) Spot radiograph performed with the patient in a lateral position demonstrates the tubular-shaped neopharynx. The hyoid bone, epiglottis, muscular processes of the arytenoids are not present, having been resected. The larynx and proximal trachea are not seen due to surgical resection. The skin of the anterior neck closes approximates the neopharyngeal tube
The larynx is gone, so there is no concern for aspiration in the post-total laryngectomy patient. However, a leak with fissure or pharyngocutaneous fistula formation is seen in 6–21% of patients, usually within 10–14 days after surgery. Leaks arise at sites of mucosal approximation: the base of the tongue, the anterior neopharyngeal wall, the junction with cervical esophagus, the tracheostoma, and, if used, the margin of a flap. Leaks end blindly in the residual soft tissues of the neck or extend as a fistula to the skin or carotid sheath. Leaks developing in the remote postoperative period suggest recurrent carcinoma. Leaks appear radiographically as contrast-filled tracks or ulcers originating at the base of the tongue or anterior neopharyngeal wall (Fig. 6.24).
In the remote postoperative period, the most common complications are stricture formation and constrictor muscle dysfunction. A “normal” neopharyngeal may be as narrow as 7 mm in luminal diameter, given the lack of tissue to close the surgically created anterior wall gap. Short, less than 5 mm in length web or ring-like strictures at the base of tongue or in the neopharyngeal tube are usually the sequelae of leaks. Long (>3 cm in length), smooth symmetric tubular strictures are usually the result of insufficient mucosa at the time of neopharyngeal tube closure or radiation therapy. Recurrent carcinoma is suggested by any narrowing that has nodular mucosa or mass effect.
Abnormal bolus transfer through the neopharyngeal tube may result from muscular detachment from bony, cartilaginous, or ligamentous structures or partial or complete muscular denervation at surgery. Poor coordination of muscular contraction between the intact superior constrictor muscle and the middle constrictor, thyropharyngeus, and cricopharyngeus muscle is not infrequent. With the patient in a lateral position, constrictor muscle dysfunction appears radiographically as a persistent or poorly time smooth extrinsic mass impression on the posterior neopharyngeal wall (Muller-Miny et al. 1993). The mass impression changes size and shape with swallowing. Dilatation of the neopharyngeal tube and incomplete clearance of the bolus are associated with muscle dysfunction.
Severe smokers/alcoholics often have poor dentition and missing teeth. Teeth may be removed prior to radiation therapy. Therefore, some total laryngectomy patients are unable to chew solid food fully. This food can impact in normal sacculations at the base of the tongue, in the normally narrow neopharyngeal tube, or above a stricture or poorly functioning constrictor muscle.
Other complications include poor tongue motion due to hypoglossal nerve damage, tracheostoma stenosis, and tumor recurrence. Failure to achieve satisfactory voice rehabilitation may be the result of poor cricopharyngeal muscle function, voice prosthesis malposition, gastroesophageal reflux, or esophageal motor disorder.
Procedures for Zenker’s Diverticulum
Diverticulectomy with cricopharyngeal myotomy is the most successful surgery for treatment of Zenker’s diverticulum. The diverticulum is removed. The fibers of the lowermost thyropharyngeus and the cricopharyngeus are divided from behind, sparing the mucosa of the pharyngoesophageal segment. At postoperative pharyngography, a diverticulum should not be visible. The pharyngoesophageal segment opens widely. A beak-like deformity may be seen on the posterior pharyngeal wall near the site of diverticulectomy. However, no leak should be present.
Several other procedures have been devised when the patient is a poor operative risk. Cricopharyngeal myotomy with diverticulopexy avoids cutting the pharyngeal mucosa. A cricopharyngeal myotomy is performed. The apex of the Zenker’s diverticulum is pulled superiorly and sutured to the prevertebral fascia. During pharyngography, the diverticulum may partly fill, but the barium drains through the patent cricopharyngeus (Fig. 6.25).
Diverticulopexy with cricopharyngeal myotomy. (a) Spot radiograph obtained with the patient in a steep oblique (near lateral) position demonstrates a wide-open pharyngoesophageal segment (arrowhead). A beak-like outpouching (arrow) indicates barium barely refluxing into a collapsed Zenker’s diverticulum that has been pulled superiorly. (b) Spot radiograph obtained just after the image in (a) demonstrates slight increased filling of the diverticulum (long arrows). A non-obstructive web (short arrow) is seen in the cervical esophagus
An endoscopically performed division of the cricopharyngeal bar is another alternative treatment for Zenker’s diverticulum in high-risk patients. The anterior tip of a specially designed endoscope is passed into the pharyngoesophageal segment and upper cervical esophagus, while the posterior tip is passed into the Zenker’s diverticulum. The cricopharyngeus is then divided and stapled so that the upper portion of the diverticulum widely communicates with the cervical esophagus. The Zenker’s diverticulum is not excised. During pharyngography (Fig. 6.26), there should be less filling of the Zenker’s diverticulum with barium, as the pharyngoesophageal segment is transected and widened, improving clearance through the pharyngoesophageal segment (Hadley et al. 1997). The barium level in the Zenker’s diverticulum is lower than the level in a preoperative study (Sydow et al. 2001).
Endoscopically performed division of the “cricopharyngeus” in a patient with a Zenker’s diverticulum. (a) Spot radiograph obtained with the patient in a frontal position while drinking barium shows a bilobed sac (arrows) midline. (b) Spot radiograph obtained with the patient in a frontal position shows a bilobed sac (arrows). Midline, the staple line that partially divided the diverticulum is barely visible (arrowhead). The right vallecula (V) and right piriform sinus (P) are identified. (c) Spot radiograph obtained while the patient drinks while standing in a lateral position demonstrates the bilobed diverticulum (short arrows). The staple line is barely visible (long arrow). The portion of the pharyngoesophageal segment that has not been endoscopically divided is narrow (arrowhead)
Cricopharyngeal myotomy alone, endoscopic dilatation of the cricopharyngeal bar, and Botox injection of the cricopharyngeus are ineffective procedures for Zenker’s diverticulum.
References
Agha FP, Francis IR, Ellis CN. Esophageal involvement in epidermolysis bullosa dystrophica: clinical and roentgenographic manifestations. Gastrointest Radiol. 1983;8:111–7.
Apter AJ, Levine MS, Glick SN. Carcinomas of the base of the tongue: diagnosis using double-contrast radiography of the pharynx. Radiology. 1984;151:123–6.
Bachman AL, Seaman WB, Macken KL. Lateral pharyngeal diverticula. Radiology. 1968;91:774–82.
Bachman AL. Benign, non-neoplastic conditions of the larynx and pharynx. Radiol Clin North Am. 1978;16:273–90.
Balfe DM, Koehler RE, Setzen M, et al. Barium examination of the esophagus after total laryngectomy. Radiology. 1982;143:501–8.
Balfe DM, Heiken JP. Contrast evaluation of structural lesions of the pharynx. Curr Probl Diagn Radiol. 1986;15:73–160.
Bosma JF, Gravkowski EA, Tryostad CW. Chronic ulcerative pharyngitis. Arch Otolaryngol. 1968;87:85–96.
Brady AP, Stevenson GW, Somers S, et al. Premature contraction of the cricopharyngeus: new sign of gastroesophageal reflux disease. Abdom Imaging. 1995;20:225–9.
Bucholz D. Neurologic causes of dysphagia. Dysphagia. 1987;1:152–6.
Chang-Lo M. Laryngeal involvement in Von Recklinghausen’s disease. Laryngoscope. 1977;87:435–42.
Clements JL, Cox GW, Torres WE, et al. Cervical esophageal webs—a roentgen-anatomic correlation. AJR. 1974;121:221–31.
Curtis DJ, Cruess DF, Crain M, et al. Lateral pharyngeal outpouchings: a comparison of dysphagic and asymptomatic patients. Dysphagia. 1988;2:156–61.
Delahunty JE, Margulies SE, Alonso UA, et al. The relationship of reflux esophagitis to pharyngeal pouch (Zenker’s diverticulum). Laryngoscope. 1971;81:570–7.
DiSantis DJ, Balfe DM, Koehler RE, et al. Barium examination of the pharynx after vertical hemilaryngectomy. AJR. 1983;141:335–9.
Ekberg O. Cervical oesophageal webs in patients with dysphagia. Clin Radiol. 1981;32:633–41.
Ekberg O, Nylander G. Lateral diverticula from the pharyngoesophageal junction area. Radiology. 1983a;146:117–22.
Ekberg O, Nylander G. Pharyngeal dysfunction after treatment for pharyngeal cancer with surgery and radiotherapy. Gastrointest Radiol. 1983b;8:97–104.
Emery CD, Wall S, Federle MP, et al. Pharyngeal Kaposi’s sarcoma in patients with AIDS. AJR. 1986;147:919–22.
Frieling T, Berges W, Lubke HJ, et al. Upper esophageal sphincter function in patients with Zenker’s diverticulum. Dysphagia. 1988;3:90–2.
Goldstein HM, Rogers LF, Fletcher GH, Dodd GD. Radiological manifestations of radiation-induced injury to the normal upper gastrointestinal tract. Radiology. 1975;117:135–40.
Goldstein HM, Zornoza J. Association of squamous cell carcinoma of the head and neck with cancer of the esophagus. AJR. 1978;131:791–4.
Gordon AR, Levine MS, Redfern RO, Rubesin SE, Laufer I. Cervical esophageal webs: association with gastroesophageal reflux. Abdom Imaging. 2001;26:574–7.
Gromet M, Homer MJ, Carter BL. Lymphoid hyperplasia at the base of the tongue. Radiology. 1982;144:825–8.
Hadley JM, Ridley N, Djazaeri B, Glover G. The radiological appearances after endoscopic cricopharyngeal myotomy: Dohlman’s procedure. Clin Radiol. 1997;52:613–5.
Hyams VJ, Rabuzzi DD. Cartilaginous tumors of the larynx. Laryngoscope. 1970;80:755–67.
Hyams VJ, Batsakis JG, Michaels L. Tumors of the upper respiratory tract and ear. In: Atlas of tumor pathology, Fascicle 25, vol. 2. Bethesda: Armed Forces Institute of Pathology; 1988.
Knuff TE, Benjamin SB, Castell DO. Pharyngoesophageal (Zenker’s) diverticulum: a reappraisal. Gastroenterology. 1982;82:734–6.
Lakhani P, Rubesin SE, Zhang PJ. Malignant fibrous histiocytoma of the pharynx. AJR. 2005;184:S12–3.
Lindbichler F, Raith J, Uggowitzer M, et al. Aspiration resulting from lateral hypopharyngeal pouches. AJR. 1998;170:129–32.
Mansson T, Wilske J, Kindblom L-G. Lipoma of the hypopharynx: a case report and a review of the literature. J Laryngol Otol. 1978;92:1037–43.
Maran AGD, Buchanan DR. Branchial cysts, sinuses and fistulae. Clin Otolaryngol. 1978;3:77–92.
Moses BL, Eisele DW, Jones B. Radiologic assessment of the early postoperative total-laryngectomy patient. Laryngoscope. 1993;103:1157–60.
Muller-Miny H, Eisele DW, Jones B. Dynamic radiographic imaging following total laryngectomy. Head Neck. 1993;15:342–7.
Nanson EM. Carcinoma in a long-standing pharyngeal diverticulum. Br J Surg. 1976;63:417–9.
Nosher JL, Campbell WL, Seaman WB. The clinical significance of cervical esophageal and hypopharyngeal webs. Radiology. 1975;117:45–7.
Quillen SP, Balfe DM, Glick SN. Pharyngography after head and neck irradiation: differentiation of postirradiation edema from recurrent tumor. AJR. 1993;161:1205–8.
Rubesin SE, Jessurun J, Robertson D, et al. Lines of the pharynx. Radiographics. 1987;7:217–37.
Rubesin SE, Glick SN. The tailored double-contrast pharyngogram. Crit Rev Diagn Imaging. 1988;28:133–79.
Rubesin SE, Laufer I. Pictorial review: principles of double contrast pharyngography. Dysphagia. 1991;6:170–8.
Rubesin SE. Killian-Jamieson diverticula: radiographic findings in 16 patients. AJR. 2001;177:85–9.
Rubesin SE, Eisele DW, Jones B. Pharyngography in the postoperative patient. In: Jones B, editor. Normal and abnormal swallowing. 2nd ed. New York: Springer; 2003. p. 167–203.
Shauffer IA, Phillips HE, Sequeira J. The jet phenomenon: a manifestation of esophageal web. AJR. 1977;129:747–8.
Scott JC, Jones B, Eisele DW, Ravich WJ. Caustic ingestion injuries of the upper aerodigestive tract. Laryngoscope. 1992;102:1–8.
Seaman WB. Contrast radiography in neoplastic disease of the larynx and pharynx. Semin Roentgenol. 1974;9:301–9.
Shirazi KK, Daffner RH, Gaede JT. Ulcer occurring in Zenker’s diverticulum. Gastrointest Radiol. 1977;2:117–8.
Smiley TB, Caves PK, Porter DC. Relationship between posterior pharyngeal pouch and hiatus hernia. Thorax. 1970;25:725–31.
Sydow BD, Levine MS, Rubesin SE, Laufer I. Radiographic findings and complications after surgical or endoscopic repair of Zenker’s diverticulum in 16 patients. AJR. 2001;177:1067–71.
Woodfield C, Levine MS, Rubesin SE, Laufer I, Mirza N. Pharyngeal retention cysts: radiographic findings in seven patients. AJR. 2005;184:793–6.
Zaino C, Jacobson HG, Lepow H, et al. The pharyngoesophageal sphincter. Radiology. 1967;89:639–45.
Zaino C, Jacobson HG, Lepow H, et al. The pharyngoesophageal sphincter. Springfield: Charles C Thomas; 1970.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Rubesin, S.E. (2013). Pharynx: Benign and Malignant Conditions. In: Hamm, B., Ros, P.R. (eds) Abdominal Imaging. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-13327-5_3
Download citation
DOI: https://doi.org/10.1007/978-3-642-13327-5_3
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-13326-8
Online ISBN: 978-3-642-13327-5
eBook Packages: MedicineReference Module Medicine