Abstract
*Also termed “electrophrenic ventilation”, while “diaphragm pacing” depicts both phrenic nerve stimulation and muscle stimulation using electrodes directly implanted in the diaphragm. The latter is not in the scope of the present overview.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Historical Notes
Already more than a hundred years ago electric stimulation of the phrenic nerves was discussed as a possibility for reanimation of breathing and resuscitation [1–4]. At the Harvard School of Public Health, JS Sarnoff and collaborators in the late 1940s, after a series of animal experiments, were able to show that “electrophrenic respiration” could maintain adequate breathing in man for considerable time periods [5,6]. In 1968 the first patient with chronic phrenic nerve stimulation for primary alveolar hypoventilation was published [7]. Subsequently, in collaboration with the Avery LaboratoryFootnote 1 (Avery Biomedical Devices, Inc., Commack, NY, USA), William Glenn developed a commercially available diaphragm pacing system based upon permanently implanted phrenic nerve electrodes. These electrodes are connected to a subcutaneously placed radio frequency receiver controlled by an external transmitter supplying the electrical energy. Later other stimulators like Atrostim® (Atrotech Oy., Tampere, Finland) and MedImplant (Vienna, Austria) were constructed and introduced into the market [8,9]. The different types of equipment have now been available for the treatment of patients for more than 30 years. Despite the relatively few number of patients needing diaphragm pacing, it can be estimated that at present more than 2,500 operations have been performed worldwide, the majority of which with the Avery system. Essentially the devices consist of an implanted electrode connected to an implanted radiofrequency receiver in contact transcutaneously, via an antenna, with an external transmitter (Figure 180-1 ). Repetitive stimuli activate the nerve resulting in contractions of the diaphragm muscle (Figure 180-2 ). These rhythmic contractions will cause downward movements of the diaphragm and thereby mimic normal breaths. Respiratory frequency, progressive increase in amplitude (slope of the curve), pulse width and interval, inspiratory and expiratory times can be varied and optimized for each patient by programing the device.
Physiology and Anatomy
Normal breathing is accomplished by active inspiration of air by increase of the thoracic volume creating a negative intrathoracic pressure for filling the lungs with air. The expansion of the chest needs activation of the breathing muscles, the most important of which being the intercostal muscles increasing the horizontal and the diaphragm muscle increasing the vertical chest volume. Expiration is passive and implies a relaxation of these muscles. While the intercostal muscles receive innervations from the thoracic spinal nerves, the phrenic nerves supply the diaphragm muscle.
The phrenic nerves emanate from cell bodies in the anterior horn of the cervical spinal cord segments C3–C5 and descend in close vicinity of the truncs of the cervical plexus, frontal to the anterior scalenus muscle and posterior to the jugular vein before entering the thoracic aperture. The nerves then pass through the mediastinum close to the pleura and pericardium on either side of the heart for finally splitting up in a number of branches innervating the hemidiaphragms. The respiratory nerves are controlled mainly from the autonomic respiratory centre situated in the brainstem, but also from cortical neurons enabling a voluntary control of breathing. The most important of the neuronal control is the autonomic one efficacious also during sleep and at lower degrees of unconsciousness. The brainstem respiratory centre is mainly responsive to changes in blood PCO2 –levels and hypercapnia will stimulate while hypocapnia will inhibit respiration but to a lesser degree by the arterial PO2. Any block in the neuronal circuitry connecting the central nervous control system with the respiratory muscles will cause impaired breathing, hypoxia and, if total, lead to apnoea and death.
Indications and Patient Selection
Diaphragm pacing by stimulation of the phrenic nerves is more a physiologic alternative for artificial respiration than positive pressure insufflations of air by means of a mechanical respirator in patients with chronic neurogenic ventilatory failure. Main candidates for diaphragm pacing are patients suffering from an insensitive respiratory centre, either congenital or acquired, as well as high spinal cord lesions (above the C3 –level). Absolute conditions for the method to be applicable include intact phrenic nerve function and absence of significant atrophy of the diaphragm. Another important condition is that the patient and his/her closely related are willing and motivated for taking active part in the pacing treatment.
Central Alveolar Hypoventilation (CAHV, Ondine’s Curse)
CAHV is caused by insensitivity of the respiratory center to increases in blood PCO2 resulting in progressive hypercapnia to levels inducing a state of general anesthesia, apnoea, hypoxia, and finally death. Voluntary respiration is not affected and, therefore, this deleterious development only arises during sleep, in fact, at deeper sleep than REM-sleep since the cortical activity during REM-sleep will stimulate voluntary respiration mechanisms. The name Ondine’s curse emanates from mythology. There are several versions in folklore about a mermaid called Ondine (or Undine) who, because of her husbands’ unfaithfulness, delivered him a curse that he should stop breathing and die if he ever fell asleep. The most widely known version of this tale was written in 1811 by Friedrich de la Motte Fouquet and stimulated Severinghaus and Mitchell to use her name for CAHV [10]. The congenital form of CAHV is assumed to be caused by a sporadic gene mutation [11] and may be one cause of the sudden infant death syndrome. Acquired CAHV may arise as a consequence of vascular brain stem lesion, tumor, and encephalitis. Correct diagnosis implies a thorough examination at a sleep laboratory with EEG, PCO2, and PO2 analyses during different sleep levels as well as tests of respiratory responses to increased PCO2.
Spinal Cord Lesions
Spinal cord lesions at the C1–C2 levels may typically be results of traumatic injuries to the spine after diving-, traffic- and fall accidents. If severe, this may cause a functionally complete or close-to-complete transversal section of the medulla and block of the nervous communication between brain and body with quadriplegia and loss of voluntary as well as automatic respiration. These patients will permanently be dependant on artificial respiration but retain the function of the peripheral phrenic nerves, which can be used for electric pacing of the diaphragm. Severe spinal cord lesions at the levels C3–C5 in most cases also lose the majority of cell bodies of the phrenic nerves, which will rapidly degenerate and are impossible to stimulate. This problem may however be overcome by a combined surgical technique anastomosing intercostal nerves to the distal portion of the phrenic nerve and implanting a nerve stimulator [12]. In lesions below C5 the patients retain adequate phrenic nerve function and their ability for both voluntary and automatic diaphragmal respiration, which eliminates the need for artificial respiration.
Presurgical Evaluations
Before surgery it should be first ensured that pulmonary function with gas exchange is adequate and that no primary lung disease exists. Second the function of the phrenic nerves must be evaluated. This is done with EMG measurement of the nerve conduction time combined with fluoroscopic measurements of diaphragmal contraction upon percutaneous nerve stimulation. The phrenic nerves are easily accessed for test stimulation at 2–3 cm above the clavicles at the posterior border of the sternocleidomastoideus muscles. As measured fluoroscopically the dome of the diaphragm muscle should descend at least 4 cm upon stimulation of the nerve if permanent pacing should be considered [4,13,14]. Simultaneous spirometric measurement of the tidal volume is valuable, but may not be necessary. During fluoroscopy, a possible pulling of the mediastinum to the side ipsilateral to stimulation may diminish the space for filling the lung, should be observed. This is not unusual in small children and, if so, bilateral phrenic nerve stimulation activated simultaneously must be considered.
Surgical Techniques
There a few fundamental differences between different models of phrenic nerve stimulators concerning implantation procedures. We, therefore, here summarize the original techniques as developed by Glenn [15] and used at our own departments. Two different approaches can be recommended: the cervical (often preferred by neurosurgeons) and the thoracic (often preferred by thoracic surgeons) approaches. General anesthesia is used but, muscle relaxants should be omitted to allow intraoperative nerve test stimulation and spirometry during stimulation.
The Cervical Approach
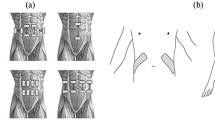
With the patient in prone position, head slightly turned backwards and rotated contralaterally, skin is opened by a five cm incision 2–4 cm above and in parallel to the clavicle passing over the posterior border of the sternocleidomastoid muscle. Platysma is opened and the sternocleidomastoid muscle retracted frontally and medially, exposing the scalenus anterior muscle and, frontal-medial, to the jugular vein. A small fat pad is usually located over the muscle and has to be retracted for exposing the phrenic nerve lying closely under the muscle facia and crossing the muscle from superior-lateral to inferior-medial (Figure 180-3a ). For localizing the nerve a bipolar nerve stimulator may be used for electrical testing and observing the muscle response from the diaphragm. After 5–6 mm incisions through the scalenus fascia on both sides of and in parallel to the nerve, the electrode is placed under the nerve so that the nerve will be located into the electrode semicircular groove (Figure 180-3b ). Finally the electrode wings are sutured to the muscle fascia on both sides (Figure 180-3c ). The extension wire from the electrode is passed subcutaneously to a small new thoracic skin incision some distance below. A subcutaneous pocket is formed for implanting the transmitter, which will be connected to the lead extension wire. For the monopolar mode the electrode connects with the cathode while the anode contact is built-in into the transmitter.
Bipolar electrodes are implanted similarly and they differ only with respect to that both the negative and positive contacts are placed in the phrenic nerve electrode for a narrow electric field. The advantage with this is that it can be used in patients with cardiac pacemakers.
The Thoracic Approach
This is essentially similar to what has been seen earlier and was also originally described by Glenn et al [15], and modified by Miller et al [16]. The thoracic approach was advocated mainly because of three reasons. First, in some (roughly 25%) the phrenic nerve may receive an accessory branch joining the main trunk below the clavicle [14,17]. Second, to avoid a risk of undesired sensory effects and muscular twitches in the arm because of the stimulation of the lower nerve trunks of the cervical plexus. Third, the great mobility of the head and neck could contribute to electrode dislocation or break.
With this approach the skin is incised (about 10–15 cm) on the anterior-lateral thorax between the second and third ribs. The ribs are spread and the lung retracted for access to the anterior mediastinum and the phrenic nerves, situated at a depth of around 5 cm. This technique may have advantages, but the disadvantage is that a thoracotomy with some risk for complications may be detrimental in a patient with already impaired respiratory function. The surgical complications reported have, however, been few and recently, minor traumatic approaches were suggested by using endoscopic and robotic techniques [18,19].
The timing of surgery is important and must be individualized especially for patients requiring full time mechanical ventilatory support. After a traumatic high cervical cord lesion with initial quadriplegia, some neuronal recovery may occur after several months with a possibility of partly return of ability of spontaneous breathing. In the early course of events, it is impossible to judge to which extent this capacity will be functionally sufficient. Therefore, a period of waiting before arriving at a definite decision is motivated. On the other hand due to disuse, atrophy of the diaphragm starts very early and may by time reach levels difficult to recondition [20]. It is not unlikely that early surgery should promote an optimal result of the treatment.
Postimplantation Management
After surgery the patient should be allowed a 12–14 day period of rest for wound healing and postoperative tissue edema to resolve, before starting the stimulation. During fluoroscopic observation of the diaphragm contractions, the amplitude threshold for muscle response is recorded, with spirometry the amplitude is now increased until maximal tidal volume is obtained. The transmitter is set at the lowest value for obtaining maximum tidal volume. The slope of the amplitude as well as the respiratory rate is set (usually 12–14 per min). Since patients with central hypoventilation syndromes retain their capacity of voluntary breathing, there are seldom any or only little diaphragma atrophy and the muscle does not need to be trained. Phrenic nerve stimulation can, therefore, be started with long time periods almost directly. However, it is recommended that the patients in the beginning use pacing in 1–3 h periods while awake for habituation before using continuous pacing for maximal 12 h during sleep. Usually these patients only need a unilateral phrenic nerve stimulator, since only pacing is necessary during the sleeping hours and the risk of muscular fatigue is little.
In patients totally dependent of artificial respiration, there is always atrophy of the diaphragm which needs training. For each patient an individual conditioning program should be made up starting pacing in 3–5 min periods per hour and prolonging these periods successively to the point when continuous pacing can be used. Usually this conditioning period will take 3–6 months. In quadriplegic patients bilateral implants are necessary and in order to prevent muscle fatigue the patient should stimulate unilaterally maximally for 12 h and then switch to stimulate the other side. The alternative is alternate stimulation of the two sides in shorter intervals (2–3 h) in accordance with individual preferences.
Outcomes
Several papers published during the 1970s verified the efficacy of phrenic nerve stimulation for the treatment of neurogenic respiratory failure in central hypoventilation syndromes and in quadriplegic patients [21–24]. In 1988 Glenn et al [25] reviewed the records of 165 patients treated in six centers included in a cooperative study. Sixty-five patients received unilateral stimulators and 100 bilateral, 37% were men and 64% women. Diagnoses were: cervical cord and brain stem lesions (64%); hypoventilation syndromes (35%), and 1% peripheral lesions. Wound infections were seen in 4.5% of all implantation procedures. In seven cases removal of the device was necessary, but pacing could be reinstituted after reimplantations. Surgical risk for nerve injury was lower with the monopolar electrode than with bipolar and the lowest risk of injury to the nerve was found with monopolar electrodes implanted with the thoracic approach. At follow up close to 80% of the patients were either independent of ventilation or needed minimal periods of support with mechanical ventilation. The majority (65%) lived at home, while 23% were hospitalized and 13% stayed in rehabilitation units. Fodstad [26] reported postoperative results follow-up ranging from 2 months to 10 years in thirty-five patients with either central hypoventilation or spinal cord lesions treated with phrenic nerve mediated diaphragm pacing. Seven patients died because of reasons not related to stimulation and five stopped pacing. Fifteen patients were totally independent while eight were partly dependent on mechanical ventilation. In another long-term follow-up study of 12 patients with complete respiratory paralysis from high cervical spinal cord lesions, all treated with stimulation of the thoracic phrenic nerves, full time pacing was accomplished from 0.5 to 16 years [27]. Nine of the patients could live at home; one of them married and was able to work full time; two completed collage studies. A recently published study [28] prospectively collected data from 64 patients with high spinal cord lesions and compared the outcome of phrenic nerve stimulation with the outcome of mechanical ventilation support. Data from the study period of more than 20 years show a statistically significant lower incidence of respiratory infections; significantly better quality of speech; and more patients managing employments in the 32 patients with stimulator controlled breathing than the 32 with mechanical ventilators. Subjective evaluations of quality of life by the patients and their doctors also favored the stimulation treatment and SCIM (the Spinal Cord Independence Measure) increased by a factor four as compared to mechanical respiratory treatment.
The incidence of long-term pacer complications (intermittent or absent pacing) was similar in a pediatric patient group (n = 35) and an adult group (n = 29), but higher in active children with Ondine’s curse than in adult or children with quadriplegia [29]. After interventions successful pacing was reached in 94% of the children and 86% of the adult patients.
Concluding Remarks
In highly selected patients with central hypoventilation syndromes and spinal cord lesions above the C3 level, support of respiration by permanently implanted phrenic nerve stimulators may be of great value. The technique affords a possibility for more independency, reduces the incidence respiratory infections, may reduce the need for permanent tracheotomy, and reduces nursing care. Despite a significant financial investment for each system to be implanted, calculations indicate that initial costs may be paid off within 1–3 years [28,30]. Furthermore, for the individual sufferer benefits to costs ratio may well be favorable.
Future improvements of the technique should take measures to develop fully implantable system including built-in energy source in similarity to deep brain and dorsal column stimulator devices. This would avoid risks for unintentional decoupling of antennas connecting the external transmitter with the internal receiver. Closed loop systems that could respond to changes in the patients’ actual metabolic needs and automatically adapt to the ventilation accordingly would also be a target for future research efforts. For patients with some retained capacity of voluntary breathing, a system that could synchronize stimulation-initiated breaths with voluntary initiation of breaths is warranted.
Notes
- 1.
*Also termed “electrophrenic ventilation”, while “diaphragm pacing” depicts both phrenic nerve stimulation and muscle stimulation using electrodes directly implanted in the diaphragm. The latter is not in the scope of the present overview.
References
Hufeland CW. Usum uis electriciae in asphyxia experimentis illustratum. Göttingen, Germany: Dissertatio Inauguralis Medica; 1783.
Duchenne GBA. De l’Electrisation Localisee et de son Application a la Pathologie et a le Therapeutique par Courant Induits et apr Courants Galvanique Inerrompus et Continus par le Dr. Duchenne. Paris, France: Bailliere; 1872.
Beard GM, Rockwell AD. A practical treatise on the medical and surgical uses of electricity. New York: William Wood; 1886. p. 664.
Creasey G, Elefteriades J, DiMarco A, Talonen P, Bijak M, Girsch W, et al. Electrical stimulation to restore respiration. J Rehabil Res Dev. 1996;33:123–32.
Sarnoff SJ, Hardenbergh E, Whittenberger JL. Electrophrenic respiration. Science 1948;108:482.
Whittenberger JL, Sarnoff SJ, Hardenbergh E. Electrophrenic respiration. II. Its use in man. J Clin Invest. 1949;28:124–28.
Judson JP, Glenn WW. Radio-frequency electrophrenic respiration. Long-term application to a patient with primary hypoventilation. JAMA 1968;203:1033–37.
Talonen PP, Baer GA, Häkkinen V, Ojala JK. Neurophysiological and technical considerations for the design of an implantable phrenic nerve stimulator. Med Biol Eng Comput. 1990;28:31–37.
Holle J, Mortiz E, Thoma H, Lischka A. Karusselstimulation, a new metod of electrophrenic long-term nerve stimulation. Wien Klin Wochenschr 1974;86:23–27.
Severinghaus JW, Mitchell RA. Ondine’s curse – failure of respiratory center automaticity while awake. Clin Res. 1962;10:122.
Dubreuil V, Ramanantsoa N, Trochet D, Vaubourg V, Amiel J, Gallego J, et al. A human mutation in Phox2b causes lack of CO2 chemosensitivity, fatal apnea, and specific loss of parafacial neurons. Proc Natl Acad Sci. 2008;105:1067–72.
Krieger LM, Krieger AJ. The intercostals to phrenic nerve transfer: An effective means of reanimating the diaphragm in patients with high cervical spine injury. Plast Reconstr Surg. 2000;105:1255–61.
Devine A, Watt JWH. Anaesthesia and diaphragmatic pacing in patients with tetraplegia. A review of peri-operative management in patients over a 10-year period. Eur J Anaesthesiol. 1966;13:553–61.
Glenn WWL, Sairenji H. Diaphragm pacing in the treatment of chronic ventilatory insufficiency. In: Roussos C, Macklem PT, editors, The thorax: lung biology in health and disease, Marcel Dekker; New York, NY: 1985. p. 1407–440.
Glenn WWL, Hogan JF, Phelps ML. Ventilatory support of the quadriplegic patient with respiratory paralysis by diaphragm pacing. Surg Clin North Am. 1980;60:1055–78.
Miller JI, Farmer JA, Stuart W, Apple D. Phrenic nerve pacing of the quadriplegic patient. J Thoracic Cardiovasc Surg. 1990;99:35–40.
Oda T, Glenn WWL, Fukuda Y, Hogan JF, Gorfien J. Evaluation of electrical parameters for diaphragm pacing: an experimental study. J Surg Res. 1981;30:142–53.
Shaul DB, Danielson PD, McComb JG, Keens TG. Thoracoscopic placement of phrenic nerve electrodes for diaphragmatic pacing in children. J Pediatr Surg. 2002;37:974–78.
Morgan JA, Morales DL, John R, Ginsburg ME, Kherani AR, Vigilance DW, et al. Endoscopic, robotically assisted implantation of phrenic pacemakers. J Thorac Cardiovasc Surg. 2003;126:582–83.
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P, et al. Rapid disuse atrophy of diaphragm of fibers in mechanically ventilated humans. N Engl J Med. 2008;358:1327–35.
Glenn WW, Holcomb WG, Gee JB, Rath R. Central hypoventilation: long-term ventilation assistance by radiofrequency electrophrenic respiration. Ann Surg. 1970;172:755–73.
Glenn WW, Holcomb WG, McLaughlin AJ, O’Hare JM, Hogan JF. Yasuda R. Total ventilatory support in a quadriplegic patient with radiofrequency electrophrenic respiration. N Engl J Med. 1972;286:513–16.
Glenn WW, Holcomb WG, Shaw RK, Hogan JF, Holschuh KR. Long-term ventilation support by diaphragm pacing in quadriplegia. Ann Surg. 1976;183:566–77.
Fodstad H, Blom S, Linderholm H. Artificial respiration by phrenic nerve stimulation (diaphragm pacing) in patients with cervical cord and brain stem lesions. Scand J Rehabil Med. 1983;15:173–81.
Glenn WWL, Brouillette RT, Dentz B, Fodstad H, Hunt CE, Keens TG, et al. Fundamental considerations in pacing of the diaphragm for chronic ventilatory insufficiency: A multi-center study. PACE 1988;11:2121–27.
Fodstad H. Pacing of the diaphragm to control breathing in patients with paralysis of central nervous system origin. Stereotact Funct Neurosurg. 1989;53:209–22.
Elefteriades JA, Quin JA, Hogan JF, Holcoomb WG, Letsou GV, Chlosta WF, et al. Long-term follow up of pacing of the conditioned diaphragm in quadriplegia. PACE 2002;25:897–906.
Hirschfeld S, Exner G, Luukkaala T, Baer GA. Mechanical ventilation or phrenic nerve stimulation for trearment of spinal cord injury-induced respiratory insufficiency. Spinal Cord, advance online publ, 13 May 2008;doi:10.1038/sc.2008.43.
Weese-Mayer DE, Silvestri JM, Kenny AS, Ilbawi MN, Hauptman SA, Lipton JW, et al. Diaphragm pacing with a quadripolar phrenic nerve electrode: an international study. PACE 1996;19:1311–19.
Similowski T, Derenne JP. Stimulation phrénique implantée. Medicine et Terapeutique 2001;7:457–695.
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer-Verlag Berlin Heidelberg
About this entry
Cite this entry
Rehncrona, S., Sedin, G., Fodstad, H. (2009). Apnea: Phrenic Nerve Stimulation*. In: Lozano, A.M., Gildenberg, P.L., Tasker, R.R. (eds) Textbook of Stereotactic and Functional Neurosurgery. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-69960-6_180
Download citation
DOI: https://doi.org/10.1007/978-3-540-69960-6_180
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-69959-0
Online ISBN: 978-3-540-69960-6
eBook Packages: MedicineReference Module Medicine