Abstract
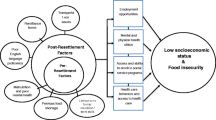
The socioeconomic growth of some countries is impacted by immigration. For example, Canada has sheltered numerous refugees and promptly responded to the global refugee crisis. Food insecurity, dietary acculturation, inadequate access to healthcare, and poor nutrition are major contributing factors to newcomer health. For refugees, compared to immigrants, barriers to health include pre- and postmigration factors such as language, trauma, social stratification, and lack of access to healthcare. Newcomer children can be negatively affected by these inequities. Refugee children, specifically, are at higher risk of poor nutritional health. Studies on refugee children showed they were vulnerable to excess weight, chronic conditions, mental health issues, poor education, and poverty. Newcomer health decreases over time, which can increase the burden on the Canadian healthcare system. Limited information is available regarding the relationship between food security and social determinants of heath and how this affects unique subgroups of newcomers. Research is required to identify culturally appropriate and cost-effective ways to promote traditional food, and to assess nutritional quality and safety in Canada. Although Canada is used as an example, there is wide applicability to other countries where refugees have similar experiences and data regarding children is lacking.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
International migration occurred at a faster rate than the world’s population growth (United Nations 2016). As of 2015, there were approximately 244 million migrants worldwide (United Nations High Commissioner for Refugees [UNHCR] 2017). There were 65.3 million people forcibly displaced from homes around the world, among them, nearly 21.3 million were refugees, which is more than the number of people displaced after World War II (UNHCR 2017). More than ten million of these refugees were children and youth (UNHCR 2017). Ten million people worldwide have been denied a nationality and lack access to basic necessities including employment, food, education, and healthcare (UNHCR 2017). Immigrant is often used for immigrants and refugees. However, these two populations differ due to cause of migration, different countries of origin, cultures, pre- and postmigration factors, and socioeconomic status, all of which affect quality of life and integration into a new society (Nisbet 2011). Immigrants choose to migrate for a better future while refugees are forcefully displaced from their homeland.
Canada is thought of as the land of immigrants since the majority of its population is new immigrants or descendants of previous immigrants (Fig. 1) (Government of Canada 2011). People migrate to Canada for multiple reasons including job opportunities, health, and ultimately a desire for a better life. Canada’s first Governor General, John Buchan, stated that immigrants “should retain their individuality and each make its contribution to the national character” (Government of Canada 2011). This philosophy has been maintained throughout the years in Canada’s Multiculturalism Policy (Government of Canada 2011). Immigration has had a major impact on the population and socioeconomic growth of Canada. Statistics Canada (2011) states the level of education is higher among immigrants than Canadian-born. Politicians at all levels of government believe immigration is necessary for economic growth and stability (Statistics Canada 2011). The racial diversity of Canada’s immigrants may be responsible for the superior social cohesion compared to other developed nations (Statistics Canada 2011).
The number of immigrants and immigrant children to Canada according to period of immigration. This figure indicates a rise in the total number of people who have immigrated to Canada as well as the number of children who have immigrated to Canada from 1971 to 2011. (*Data retrieved from Statistics Canada (2017))
According to the 2011 census, 6.8 million people living in Canada are foreign born, which accounts for 21% of the total population. People migrate to Canada as individuals or families and are grouped into four categories: economic, families, refugees, and others (Pottie et al. 2015). Based on available data, as of 2011, there were more than one million newcomers in Canada who immigrated between 2006 and 2011, out of which 19% were children aged 14 years and under (Fig. 1) (Statistics Canada 2016). Another 15% were youth between the ages of 15 and 24 years (Statistics Canada 2016).
Refugees entering Canada come with hopes, experiences, and skills, which contribute to a wealthy and affluent society. Canada, in the past, has responded on various occasions to the global refugee crisis and sheltered numerous refugees. From November 2015 to January 2017, approximately 40,081 Syrian refugees arrived in Canada (Government of Canada 2017a). In 2016 (January–September) alone, there were 16,369 in-person refugee claims (Government of Canada 2017b).
Health of Newcomers to Canada
Newcomer health is influenced by culture including knowledge, skills, practices, beliefs, and experiences associated with traditional, complementary, or alternative medicines (World Health Organization [WHO] 2000). Social determinants of health include income, education, employment, social structures, culture, gender, and child development. They play an important role in the health status of newcomers, particularly regarding food security, which is discussed later in this chapter.
Immigrants with a higher socioeconomic status possess more knowledge about health and follow the Western medicine system (Rothstein and Rajapaksha 2003). Highly educated and wealthy immigrants are more likely to maintain a healthy body weight, adhere to preventive health advice, and exercise more frequently (Rothstein and Rajapaksha 2003). Those who are not satisfied with Western healthcare, whether due to high costs, long wait times, or perceived discrimination, have a tendency to use traditional or complementary medicine more than those who are satisfied (Ku 2007). Exposure to factors such as past harmful exposure from war, lack of nutritious food, violence, trauma, poor sanitation, socioeconomic status, English- or French-language proficiency, limited access to preventive services, and specific disease vectors exposure, put refugee s at higher risk of ill health and poor nutrition when compared to immigrants (Ng et al. 2011). English language proficiency was greater in immigrant children compared to refugees (Hoover et al. 2016). Refugee newcomer children to Canada were significantly more likely to come from families where neither parent had a secondary level education and where their main source of income was social assistance compared to immigrants (Nisbet 2011). Newcomer immigrant and refugee families with children found themselves in the lowest income category at 49% and 62%, respectively (Nisbet 2011).
The Healthy Immigrant Effect
Previous literature suggests the health status of immigrants upon arrival is high, eventually deteriorating over a period of 5 years postmigration before matching that of native-born Canadians (Newbold 2009). This healthy immigrant effect is associated with three hypotheses, selective immigration, better access to healthcare services over time, and acculturation (Antecol and Bedard 2006; Gushulak 2007). In order to understand the healthy immigrant effect, these hypotheses need to be investigated further.
Selective Immigration
Self-selection is a term that describes individuals who are economically affluent and healthy in their home countries and more likely to migrate due to better opportunities. Immigrants must pass a screening process, including a medical examination, which removes those with severe medical conditions who pose a danger to public health or safety and strain the healthcare system more than the average Canadian, which was $5,292USD per capita in 2014 (Antecol and Bedard 2006; WHO 2014). However, refugee s are “protected by law from exclusion on the basis of noninfectious burden of illness” (Government of Canada 2017c). Immigrants from Asia, Africa, and South America were not as likely to indicate excellent/very good health compared to immigrants from Europe, the United States, Australia, and Mexico combined (Ali et al. 2004). The definition of health changes for immigrants and refugees over time due to acculturation, as they compare themselves to the general population, which affects their perceived health (Newbold 2005).
Although self-selection exists, it is likely only one contributing factor to the healthy immigrant effect and may not be applicable to all immigrants. This theory does not consider the weakening health of refugees after migration. Investigation of other hypotheses is necessary.
Healthcare
Large scale migration inevitably impacts migrants’ health as well as the healthcare system of the host country. Compared to native-born Canadians, immigrants and refugees healthcare needs can vary drastically, and they seek access to medical care less, although, they do not necessarily have better health even though their self-perceived health is higher upon entry (Gushulak 2007). Although self-assessed health of immigrants to Canada decreased, their utilization of hospitals did not increase from 1994/1995 to 2000/2001 (Newbold 2009). Barriers to healthcare affecting immigrants can include poor socioeconomic status, loss of social networks, use of traditional medicine, familial and cultural responsibilities, hesitation providing personal information, perceived discrimination, weak language skills, and poor working environments related to “deskilling” (Newbold 2009; Canadian Paediatric Society 2013). The Canadian healthcare system can be difficult to understand as it is not consistent throughout the country. Some provinces have a waiting period of 3 months, which may contribute to lower usage of the healthcare system upon entry (Government of Canada 2016a). For protected persons like refugees, a temporary health card and programs are available (Government of Canada 2016b).
The decline of newcomer health after migration is not limited to poor healthcare access. Healthcare services utilization by immigrants increases with length of stay. This could possibly increase identifying, diagnosing, reporting, and treating health-related issues (Newbold 2009). Certain groups of refugees are given immediate access to healthcare services upon arrival in Canada; hence the hypothesis of self-selection and poor access to healthcare does not apply to them. Therefore, the healthy immigrant effect could be associated with several other factors.
Dietary Acculturation
Adaptation of an individual of a particular ethnicity to a new culture is known as acculturation. Acculturation in itself is a combination of various stages. Typically, the last stage is “assimilation,” which occurs when someone from a different ethnicity completely adopts the norms of their new culture, leaving their own behind (Kittler and Sucher 2012). Those who migrate at an older age are less likely to adopt the new culture when compared to those who migrate at a younger age (Kaushal 2009). It is important to note that acculturation is complex and nonlinear, occurring along a spectrum (Berry et al. 2006). A balance should be maintained between the traditional culture and the new culture.
Obesity is a serious condition that can increase the risk of chronic conditions including, certain cancers, coronary heart diseases, hypertension, elevated blood cholesterol, and type 2 diabetes. These conditions could be attributed to poor dietary choices. The possibility of becoming obese increases during the process of acculturation (Kittler and Sucher 2012). When an individual or group of immigrants adopts the eating patterns of the host country, dietary acculturation occurs (Satia-Abouta et al. 2002). Dietary acculturation is important among immigrants to developed countries as diets are high in fat and sugar, which negatively affects their health as their length of stay increases in the host country (Satia-Abouta et al. 2002). Poor accessibility to traditional food items, lack of nutrition education, and convenience of Western food results in increased consumption of prepackaged items or fast food and can be attributed to dietary acculturation (Kittler and Sucher 2012). Dietary acculturation has been associated with increased chronic conditions among adults; hence health could be negatively affected among those children who experience dietry acculturation.
Food Security
One of the most common approaches to evaluate income-related household food security is using a questionnaire developed by the United States Department of Agriculture (2016) and adapted by Statistics Canada (Tarasuk et al. 2014). The United States classifies responses to these questions into four categories whereby households, adults, or children with high or marginal food security are considered food secure and those with low or very low food security are food insecure. Canada uses the same questionnaire and classifies households as food secure, marginally, moderately, and severely food insecure. Food security is directly related to income. Nonvisible minority Canadians are more likely to receive a higher wage job when compared to that of visible minority immigrants (Simich and Jackson 2010). Higher income, greater food security, and better opportunities are typically associated with higher education levels. However, for immigrants, higher education levels do not result in better job opportunities due to deskilling. This explains why immigrants have lower levels of food security when compared to native Canadians. Recent immigrants, even those with postsecondary education, were more likely to be underemployed, low-income, and need housing compared to the Canadian-born (Simich and Jackson 2010).
Since 2004, Statistics Canada has collected information on the food security status of Canadians by means of the Canadian Community Health Survey. Almost 13% of Canadian households (four million individuals) experienced some form of food insecurity, which included 16% (1.15 million) of children (Tarasuk et al. 2014). Food insecurity was more prevalent in households with low income, children, and single-mothers, and where the respondent was Black or Aboriginal (Tarasuk et al. 2014). Recent immigrant households had a higher prevalence of food insecurity (20%) compared to nonrecent immigrants (11.8%) and Canadian-born (12.4%) (Tarasuk et al. 2014). A pilot study, Healthy Immigrant Children (HIC), examined newcomer immigrant and refugee children in Saskatchewan, Canada, and found the prevalence of household food security was 62% and 34%, respectively (Fig. 2) (Nisbet 2011). Child food security status was 51% compared to household food security at 46% (Nisbet 2011). Although a higher prevalence of household food insecurity was observed in refugee newcomer families, child food security was not significantly different between immigrant and refugee families (Nisbet 2011). As the duration of stay in Canada increased, the risk of food insecurity in children decreased (Nisbet 2011). The study also noted that children living in households with more than two children were more likely to be food insecure (Nisbet 2011).
Prevalence of household food security among households with children. This figure compares national data (Tarasuk et al. 2014) to local data from Saskatchewan in immigrant and refugee children in the Healthy Immigrant Children study (Nisbet 2011) (*Data retrieved from Tarasuk et al. (2014) and Nisbet (2011))
Food insecure individuals can binge eat, consume high-calorie food, and, therefore, develop overweight/obesity (Che and Chen 2001). Children living in households where high school is the highest level of education are at greater risk of being overweight/obese in comparison with those living in households with a postsecondary degree (Shields 2005). Studies also showed that 21% of people in food insecure households had at least three chronic conditions and 15% of these people were obese (Che and Chen 2001).
Nutritional Health of Newcomers
The health status of individuals is strongly affected by the food they consume. Culture strongly influences people’s food choices. Healthy food choices can be limited by the ability to purchase expensive food items (Kittler and Sucher 2012). Data gathered by Statistics Canada (2014) using body mass index (BMI) showed nearly 20% (5.3 million) of Canadian adults were obese (self-reported height and weight). Estimates suggest that Canadians consume about 13% of their caloric intake from added sugar. High sugar consumption is frequently associated with adverse health outcomes including cancer, dental caries, diabetes, heart disease, high blood cholesterol, overweight/obesity, and stroke. Figure 3 portrays overweight and obesity according to immigration status. Culture influences newcomer food choices, possibly due to lack of access to traditional food items. Newcomers also witness differences in schedules, such as working long hours, which results in minimal time to prepare food in a traditional manner. Immigrant children tend to prefer Western food, while parents particularly prefer traditional food items (Gray et al. 2005). Income, country of origin, city of relocation and comprehension of its primary language all affect the likelihood of food habits changing postmigration (Gray et al. 2005).
Classification of overweight and obese according to immigration status. Overweight and obesity is shown for adult non-immigrants, long-term immigrants, and recent immigrants. This figure supports the healthy immigrant effect, as overweight and obesity increases with length of stay in Canada (*Long-term immigrants were in Canada 11 years and longer and recent were in Canada less than 11 years. Data retrieved from Tremblay et al. (2005))
Health of Newcomer Children
Detailed information on health and nutritional status of newcomer children is not available in Canadian literature. A large number of youth (37%) acculturate by being involved in activities of both traditions (Berry et al. 2006). The Canadian Institute of Child Health reported that immigrant children and youth were less likely to consume alcohol, smoked less, and had lower suicidal behavior when compared to native-born Canadian children (Pottie et al. 2015). A huge proportion of immigrant youth reported being in good stable physical and mental health (Kukaswadia et al. 2014). Also, 88% of immigrant youth aged 12–14 years reported having a strong sense of belonging to their community compared to 82% of native-born Canadian youth (Pottie et al. 2015). Canada’s vision is dependent on the well-being of children and youth who are the future of the country, and the diversity of immigrant and refugee children plays a vital role.
Refugees, particularly children, are prone to infection, which is only heightened by unsanitary living conditions and malnutrition (Food and Agriculture Organization 1995). Unfortunately, many immigrant and refugee children face serious issues with poverty, education, dietary needs, and emotional changes while coping with North American culture (Tienda and Haskins 2011). Immigrant children and youth are subjected to a wide range of mental health issues. Causes for mental health issues were a combination of several complex factors including language barriers, loss of friends or family members, living in poor neighborhoods, and cultural discordance or dissonance (Canadian Paediatric Society 2016). Cultural discordance occurs when a child perceives divergence between two cultures. This discordance is greater for children who migrate at a younger age and can have a negative impact on various aspects of their lives including relationships with peers, mental health, and tension with family (Rohmann et al. 2006).
Prevalence of nutritional anemia, growth abnormalities, malnutrition, dental caries, enteric parasites, and psychiatric disorders among the children of recent immigrants is high (Pottie et al. 2015). The term “malnutrition” comprises both under- and overnutrition and develops due to poor nutrient absorption within the body and inadequate or excess intake of protein, energy, and micronutrients (WHO 2001). Malnutrition causes deficiencies, which can affect children’s physical development/growth, increase their risk of diseases, and decrease their concentration levels/performance at school (International Development Committee 2008; WHO 2001). The likelihood of being malnourished increases among families who have lower household incomes and poor health education (e.g., newcomer refugees) (WHO 2001). A study conducted in Toronto, Ontario, showed 7% of immigrant children were below the third percentile for height-for-age and 12% for weight-for-age (Salehi et al. 2015). The same study also showed the prevalence of anemia and iron deficiency among immigrant children was 23% and 53%, respectively (Salehi et al. 2015). Health issues in children postmigration can arise because of poor dietary choices leading to overweight/obesity, and eventually chronic diseases (Shields 2005).
Nutritional Health of Newcomer Children
Diversity in diet is important to ensure adequate intake of all nutrients for optimal growth and development. Children have specific requirements as they go through this particular stage of life. Over the last three decades, the prevalence of overweight/obesity has increased among children in Canada. The possibility of being an obese adult increases if obesity is acquired during childhood. Research on immigrant and refugee children in Canada is lacking in the literature.
The predisposition to numerous negative health outcomes associated with obesity makes childhood obesity a serious public health concern. From 2005 to 2014, 29% of boys and 17% of girls were classified as overweight/obese (Statistics Canada 2014). In 2011–2012, immigrant youth were less likely to be overweight (15%) when compared to their Canadian counterparts (19%) (Pottie et al. 2015). The chance of being overweight/obese was higher among refugees compared to immigrants (Nisbet 2011). Hypertensive levels were reported in 26% of overweight/obese newcomer children (Nisbet 2011). Table 1 displays indices of disease in newcomer children to Canada.
In 2004, 71% of Canadian children 4–8 years and 62% of girls and 68% of boys 9–13 years were lacking the daily recommended servings of fruit and vegetables (Garriguet 2007). This value jumps to 80% for newcomer children 7–11 years (Nisbet 2011). Reduced intake of fruit and vegetables depletes nutrients from the body; this decreases immune system function and increases the chance of developing chronic conditions (Kirkpatrick and Tarasuk 2008). Also, 37% of children 4–9 years and 61% of boys and 83% of girls 10–16 years were not getting the daily recommended milk and alternatives servings (Garriguet 2007). When examining newcomer children 7–11 years of age, 76% did not meet recommendations for milk and alternatives (Nisbet 2011). Over 25% of children aged 4–8 years and 89% of newcomers aged 7–11 years were not consuming enough whole grains (Garriguet 2007; Nisbet 2011). Another 14–18% of girls aged 9–18 years were not getting the recommended amount of meat and alternatives (Garriguet 2007).
Prevalence of food insecurity negatively impacts nutrient consumption among Canadian children. Food insecure children were more likely than food secure children to consume energy-dense food and have lower protein, milk, and vegetable and fruit intake (Kirkpatrick and Tarasuk 2008). In 2004, the average HEIC score for children aged 4–8 years was 65.4, 59.7 for boys aged 9–13 years, and 60.0 for girls in that same age range (Garriguet 2009). More than 90% of Canadian children aged 4–13 years and newcomer children aged 7–11 years had diets classified as needing improvement (Garriguet 2009; Nisbet 2011). Newcomer refugee children to Saskatchewan had a significantly lower mean score (60.4) compared to newcomer immigrant children (65.4) (Vatanparast et al. 2013). Refugees had a poor diet at 14% compared to zero immigrants (Vatanparast et al. 2013).
Nutrients of Concern
Immigrant and refugee children can be at greater risk for nutrient intake inadequacies due to previously discussed pre- and postmigration factors compared to Canadian-born children. Prevalence of intake inadequacy was <10% for all nutrients for children 1–8 years of age (Kirkpatrick and Tarasuk 2008). Among children aged 9–18 years who were food insecure, the prevalence of nutrient intake inadequacy for protein, vitamin A, and magnesium was greater compared to food secure children (Kirkpatrick and Tarasuk 2008). Newcomer children to Canada are particularly at risk for nutrient inadequacies of folate (DFE), iron, vitamin B12, zinc, calcium, and vitamin D as found in HIC study (Fig. 4) (Nisbet 2011). The prevalence of intake inadequacy of both folate (DFE) and iron was significantly greater among refugee compared to immigrant children (Nisbet 2011).
Prevalence of nutrient intake inadequacy in Canadian and newcomer children. Prevalence of nutrient intake inadequacy for vitamin A, folate, vitamin B12, vitamin D, calcium, magnesium, phosphorous, and iron are compared amongst Canadian children 9-13 years of age and immigrant and refugee children to Canada, 7-11 years of age. (*Significant difference between immigrant and refugee children. 1Canadian data obtained from Health Canada (2008). 2Newcomer data obtained from Nisbet (2011))
Vitamin D is important during the developmental stage of childhood. It is a major nutrient for bone mineral accrual. The majority of requirements, 80–90%, must be synthesized from the sun (Hintzpeter et al. 2008). It is available through consumption of food such as oily fish, cod liver oil, and egg yolk. A deficiency in vitamin D involves deterioration of cortical bone, which progresses to osteoporosis (Institute of Medicine 2010). Some noncalciotropic functions of vitamin D, primarily those with an immune regulatory role, are associated with cancer, multiple sclerosis, and types 1 and 2 diabetes (Whiting and Calvo 2005). Calcium deficiencies are often found among those who are also vitamin D deficient (Nellen et al. 1996). Hyperparathyroidism has been noted in individuals whose regular diets contain high amounts of unrefined cereals. These cereals have a high content of phytates, which hinder calcium absorption (Pettifor 2004).
Immigrants to developed countries, including Canada, are at greater risk for vitamin D and calcium deficiencies. Vitamin D deficiency is often found in female immigrants and refugees. Some females have minimal sun exposure due to cultural beliefs associated with full-body veils, darker skin pigmentation, which decreases the dermal synthesis of vitamin D, and higher parity (number of births) (Nellen et al. 1996). Other risk factors for vitamin D deficiency, relevant to the general population, include genetics, use of sunscreen, living in areas of high latitude (around 37° latitude in the winter months), and insufficient dietary vitamin D (Hintzpeter et al. 2008).
A vitamin D deficiency less than 25–27.5 nmol/L is considered representative of rickets (Roth 2007; Ward et al. 2007). Individuals with darker skin represented 89% of children with rickets while 24% were immigrants (Ward et al. 2007). As children age, vitamin D concentrations decrease. This may be associated with poor milk consumption, higher consumption of sugar-sweetened beverages, low sun exposure, and decreased activity levels (Roth 2007). In Canada, children who live at greater than 55 degrees latitude are more likely to be vitamin D deficient (Ward et al. 2007). A study using data from 2005 to 2010 in Calgary showed 42% of newcomer refugee children had lower than adequate vitamin D and 10% were deficient (Aucoin et al. 2013). It also showed the refugee population had lower levels of vitamin D when compared to the general Canadian population (Aucoin et al. 2013). Prevalence of intake inadequacy was significantly higher in newcomer refugee (97%) children to Saskatchewan compared to newcomer immigrant children (81%) (Vatanparast et al. 2013). Females were at greater risk of deficiency, likely due to cultural practices limiting skin exposure to the sun (Vatanparast et al. 2013). Prevalence of calcium intake inadequacy in newcomer immigrant and refugee children was 76%. This could be associated with only 24% meeting Canada’s Food Guide recommendations for milk and alternatives (Vatanparast et al. 2013). Total serum 25(OH)D (nmol/L) was significantly higher in newcomer immigrant children compared to refugees (Table 1) (Nisbet 2011). Low levels of vitamin D were noted among individuals who had been living longer in Canada, particularly females (Nisbet 2011). Height and serum vitamin D status were significant determinants of TBBMC in newcomer children (Nisbet 2011).
Research Gaps and Recommendations
The health of immigrants decreases over time. However, many factors come into play and must be considered when investigating this population’s health. In order to appropriately influence policy, we must turn to research to understand how and why this decline in health manifests. Research has shown that certain measures of health are poor for newcomers, particularly refugees compared to the Canadian-born. The Canadian health system could be negatively impacted. Therefore, evidence-based interventions should be carried out to mitigate the growing burden of disease. In Canada, little is known regarding the dietary transition that newcomers face postmigration. Information is particularly sparse when it comes to children and differentiating between varied experiences of immigrants and refugees.
Further investigation is required to identify culturally appropriate and cost-effective ways to promote traditional food and to assess their nutritional quality and safety in Canada. It is also imperative to identify the most important influential factors in nutrition-specific health promotion as well as priority subgroups such as culture, gender, age, and immigration status.
The relationship between food security and the social determinants of health is important to determine how they affect acculturation, immigrant dietary behaviors, and resultant health outcomes. The impact of food security on health and diet in the newcomer population is unknown as is the extent of its reach.
Literature is lacking any sort of measurement for acculturation, which would be beneficial to understand where along the acculturation spectrum immigrants find themselves and how that relates to dietary behaviors (Table 2). Further research is required when it comes to how, and to what extent, Canadian culture influences the nutrition knowledge, perceptions, beliefs, and behaviors of immigrants. The challenges of accessing and maintaining a traditional diet and how to incorporate nutrition knowledge into a traditional diet should be explored.
Nutrient deficiencies specific to immigrants and the role they play in diet-related health outcomes requires further investigation. With a wide range of cultural groups, it is important to identify the role of genetics and if these groups have unique standards in regards to health measurement tools. Further exploration is required into dietary risk factors for chronic conditions, especially among newcomer children, and how they vary across age groups, cultures, immigration status, gender, and time since migration. When it comes to providing culturally appropriate nutritional care and services, cultural competency skills among registered dietitians and the care they provide is essential.
Protocols
Anthropometry: Anthropometrics included measured height, weight, and waist circumference. BMI was assessed using the age- and sex-specific BMI calculator from the WHO (2007).
Blood Pressure: A child with a blood pressure measurement greater or equal to the 95th percentile on three occasions was deemed hypertensive (NHBPEP 2004).
Dietary Intake: The average of three 24-h dietary recalls was used to obtain usual dietary intake. Food was entered into a diet analysis program and classified in groups according to Eating Well with Canada’s Food Guide (Health Canada 2007). For nutrient intake inadequacy, see the Mini-Dictionary of Terms. The Canadian Healthy Eating Index was based on recommendations for age and sex from Eating Well with Canada’s Food Guide as illustrated by Garriguet (2009). Based on a total score out of one hundred, a person’s diet was classified as poor (<50), needing improvement (50–80), and good (>80).
Food Security: Food security was assessed using a validated questionnaire, adapted from Health Canada (2007), whereby participants were food secure (0–1), moderately food insecure (2–5), and severely food insecure (6–10).
Serum Measures: Serum was collected on blood spot cards using a finger prick. Nonfasting total cholesterol was classified as acceptable (<4.4 mmol/L), borderline (4.4–5.1 mmol/L), and high (≥5.2 mmol/L) (American Heart Association 2011). Vitamin D was defined as deficient (<30 nmol/L), inadequate (30–50 nmol/L), and sufficient (>50 nmol/L) according to the IOM (2010).
TBBMC: Values were obtained using dual-energy x-ray absorptiometry and compared to estimated normal values for each child’s age, sex, and ethnicity based on longitudinal studies (Baxter-Jones et al. 2009).
Dictionary of Terms
-
Deskilling – Deskilling occurs when the host country does not acknowledge immigrants’ education from their native country (Newbold 2005).
-
Food Insecurity – The Food and Agricultural Organization (2003) states “Food insecurity exists when people do not have adequate physical, social or economic access to [sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life].”
-
Food Security – The Food and Agricultural Organization (2003) states “Food security [is] a situation that exists when all people, at all times, have physical, social and economic access to sufficient, safe and nutritious food that meets their dietary needs and food preferences for an active and healthy life.”‖
-
Health – The World Health Organization (2004) defines health as “the state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity…and [it] is largely culturally defined.”
-
Healthy Eating Index – “The Healthy Eating Index (HEI) uses a point system on a scale of 1–100 to evaluate certain aspects of a person’s diet to conclude if their diet is good (>80pts), needing improvement (50-80pts), or poor (<50pts)” (Garriguet 2009). The HEI was originally developed by the United States Department of Agriculture and adapted by Canada (HEIC) (Garriguet 2009).
-
Healthy Immigrant Effect – Immigrants are healthier upon arrival to the host country compared to the native-born population (Newbold 2009; Kaushal 2009). The healthy immigrant effect is influenced by self-selection, access to healthcare, acculturation, and other factors (Newbold 2009; Kaushal 2009).
-
Immigrant – “A person who has come to a different country in order to live there” (UNHCR 2017).
-
Newcomers (recent immigrant/refugees) – People who migrated to their host country less than 5 years ago.
-
Prevalence of Inadequacy – The prevalence of inadequacy is the percentage of a group’s intake below the estimated average requirement (EAR) for a specific nutrient (Health Canada 2012). The EAR is the “average daily nutrient intake level that is estimated to meet the requirement of half the healthy individuals in a life-stage and gender group” (Health Canada 2012).
-
Refugee – A refugee is someone who “…owing to well-founded fear of being persecuted for reasons of race, religion, nationality, membership of a particular social group or political opinion…is unable or unwilling to return to his/her country of birth due to fear for their safety” (UNHCR 1951).
Summary Points
-
In 2011, 6.8 million people living in Canada were foreign born with more than one million being newcomers. Children aged 14 years and under made up 19% of the total newcomers and youth aged 15–24 years made up 15%.
-
Canada has welcomed several refugees in the past, responding to the global refugee crisis. In the last 1.5 years, 40,081 Syrian refugees arrived in Canada and in 2016 (January–September), there were 16,369 in-person refugee claims.
-
The health status of immigrants upon arrival is high. However, it eventually deteriorates over time before matching that of native-born Canadians.
-
Refugees are at greater risk of poor nutrition and health compared to immigrants due, in part, to premigration exposures. Refugee children, specifically, are at greater risk.
-
Dietary acculturation could be due to expensive or less available traditional food items, a lack of nutrition education, and convenience in preparation of Western food, resulting in increased consumption of prepackaged energy-dense items, which contribute to elevated overweight and obesity levels.
-
Newcomer households had a higher prevalence of food insecurity, less access to healthcare, and lower than recommended levels of required nutrients.
-
Immigrant and refugee children face issues with poverty, education, food security, nutritional requirements, and mental health while acculturating to North American culture, which results in poor health outcomes.
-
Canada lacks comprehensive information on the health and nutritional status of immigrant and refugee children. However, immigrant and refugee children were found to have higher rates of food insecurity and be at greater risk for vitamin D and calcium deficiencies.
-
Continued research on food security and the identification of culturally appropriate food with consideration for availability, accessibility, quality, and affordability is important to address these issues.
-
Further investigation is required to identify culturally appropriate and cost-effective ways to promote traditional food and assess their nutritional quality and safety in Canada.
Abbreviations
- BMI:
-
Body mass index
- DFE:
-
Dietary folate equivalents
- HEI:
-
Healthy eating index
- HEIC:
-
Canada’s healthy eating index
- TBBMC:
-
Total body bone mineral content
- UNHCR:
-
United Nations High Commissioner for Refugees
- WHO:
-
World Health Organization
References
Ali JS, McDermott S, Gravel RG (2004) Recent research on immigrant health from Statistics Canada’s population surveys. Can J Public Health 95(3):I9–I13
American Heart Association (2011) Children and cholesterol. http://www.heart.org/HEARTORG/Conditions/Cholesterol/UnderstandYourRiskforHighCholesterol/Children-and-Cholesterol_UCM_305567_Article.jsp. Accessed 24 Feb 2017
Antecol H, Bedard K (2006) Unhealthy assimilation: why do immigrants converge to American health status levels? Demography 43(2):337–360
Aucoin M, Weaver R, Thomas R, Jones L (2013) Vitamin D status of refugees arriving in Canada: findings from the Calgary refugee health program. Can Fam Physician 59(4):e188–e194
Baxter-Jones ADG, Burrows M, Bachrach LK, Lloyd T, Petit M, Macdonald H, Mirwald RL, Bailey D, McKay H (2009) International longitudinal pediatric reference standards for bone mineral content. Bone 46(1):208
Berry JW, Phinney JS, Sam DL, Vedder P (2006) Immigrant youth: acculturation, identity, and adaptation. Appl Psychol Int Rev 55(3):303–332
Canadian Paediatric Society (2013) Adaptation and acculturation. http://www.kidsnewtocanada.ca/culture/adaptation. Accessed 20 Mar 2017
Canadian Paediatric Society (2016) Depression in children and youth. http://www.kidsnewtocanada.ca/mental-health/depression. Accessed 20 Mar 2017
Che J, Chen J (2001) Food insecurity in Canadian households. Health Rep 2(4):11–22
Food and Agricultural Organization (1995) FAO corporate repository. http://www.fao.org/docrep/U8480E/U8480E05.htm. Accessed 8 Mar 2011
Food and Agricultural Organization (2003) Trade reforms and food security-Part I: Chapter 2. http://www.fao.org/DOCREP/005/Y4671E/y4671e06.htm. Accessed 15 Oct 2010
Garriguet D (2007) Canadian’s eating habits. Health Rep 18(2):17–32
Garriguet D (2009) Diet quality in Canada. Health Rep 20(3):41
Government of Canada (2011) Backgrounder-facts in Canada’s immigration history. http://www.cic.gc.ca/english/department/media/backgrounders/2011/2011-06-27.asp. Accessed 21 Mar 2017
Government of Canada (2016a) Health care in Canada. http://www.cic.gc.ca/english/newcomers/after-health.asp. Accessed 21 Mar 2017
Government of Canada (2016b) Health care-refugees. http://www.cic.gc.ca/english/refugees/outside/arriving-healthcare.asp. Accessed 21 Mar 2017
Government of Canada (2017a) #WelcomeRefugees: key figures. http://www.cic.gc.ca/english/refugees/welcome/milestones.asp. Accessed 27 Mar 2017
Government of Canada (2017b) Refugee claims. http://open.canada.ca/data/en/dataset/8a136ac4-951b-43fe-bac9-15d5b71a6f5c?_ga=1.24378682.1671602258.1489417970. Accessed 27 Mar 2017
Government of Canada (2017c) Immigration and Refugee protection act. http://laws.justice.gc.ca/eng/acts/i-2.5/. Accessed 21 Mar 2017
Gray VB, Cossman JS, Dodson WL, Byrd SH (2005) Dietary acculturation of Hispanic immigrants in Mississippi. Salud Publica Mex 47(5):351–360
Gushulak B (2007) Healthier on arrival? Further insight into the “healthy immigrant effect”. CMAJ 176(10):1439–1440
Health Canada (2007) Income-related household food security in Canada. http://www.hc-sc.gc.ca/fn-an/alt_formats/hpfb-dgpsa/pdf/surveill/income_food_sec-sec_alim-eng.pdf. Accessed 10 Feb 2011
Health Canada (2008) Canadian Community Health Survey Cycle 2.2, Nutrition (2004)-Nutrient intakes from food: provincial, regional and national summary data tables, volumes 1, 2, and 3. www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/index-eng.php. Accessed 30 Mar 2017
Health Canada (2012) Do Canadian adults meet their nutrient requirements through food intake alone? http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/art-nutr-adult-eng.php. Accessed 30 Mar 2017
Hintzpeter B, Scheidt-Nave C, Muller MJ, Schenk L, Mensink GB (2008) Higher prevalence of vitamin D deficiency is associated with immigrant background among children and adolescents in Germany. J Nutr 138(8):1482–1490
Hoover J, Vatanparast H, Uswak G (2016) Risk determinants of dental caries and oral hygiene status in 3–15 year-old recent immigrant and refugee children in Saskatchewan, Canada: a pilot study. J Immigr Minor Health. https://doi.org/10.1007/s10903-016-0452-9
Institute of Medicine (2010) Dietary reference intakes for calcium and vitamin D. The National Academies Press, Washington, DC
International Development Committee (2008) International development: Chapter 2 (Tenth report). http://www.parliament.the-stationery-office.co.uk/pa/cm200708/cmselect/cmintdev/493/49302.htm. Accessed 23 Feb 2011
Kaushal N (2009) Adversities of acculturation? Prevalence of obesity among immigrants. Health Econ 18(3):291–303
Kirkpatrick SI, Tarasuk V (2008) Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. J Nutr 138:604–612
Kittler PG, Sucher KP (2012) Food and culture, 6th edn. Thomson Wadsworth, Belmont
Ku L (2007) Improving health insurance and access to care for children in immigrant families. Ambul Pediatr 7(6):412–420
Kukaswadia A, Pickett W, Janssen I (2014) Time since immigration and ethnicity as predictors of physical activity among Canadian youth: a cross-sectional study. PLoS One 9(2):e89509. https://doi.org/10.1371/journal.pone.0089509
National High Blood Pressure Education Program (2004) The fourth Report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 114(2):555–576
Nellen JFJB, Smulders YM, Frissen PHJ, Slaats EH, Silberusch J (1996) Hypovitaminosis D in immigrant women: slow to be diagnosed. BMJ Clin Res 312(7030):570–572
Newbold KB (2005) Self-rated health within the Canadian immigrant population: risk and the healthy immigrant effect. Soc Sci Med 60(6):1359–1370
Newbold KB (2009) Health care use and the Canadian immigrant population. Int J Health Serv 39(3):545–565
Ng E, Pottie K, Spitzer D (2011) Limited official language proficiency and decline in health status: a dynamic view from the longitudinal survey of immigrants to Canada. Health Rep 22(4)
Nisbet C (2011) Have we forgotten the children? Health and nutrition issues in refugee and immigrant newcomer children. Master’s thesis, University of Saskatchewan, Saskatoon. http://library2.usask.ca/etd. Accessed 24 Mar 2017
Pettifor JM (2004) Nutritional rickets: deficiency of vitamin D, calcium, or both? Am J Clin Nutr 80(6 Suppl):1725S–1729S
Pottie K, Dahal G, Hanvey L, Marcotte M (2015) Health profile on immigrant and Refugee children and Youth in Canada. In: The health of Canada’s children and youth: a CICH profile. http://profile.cich.ca/en/index.php/chapter4. Accessed 27 Mar 2017
Rohmann A, Florack A, Piontkowski U (2006) The role of discordant acculturation attitudes in perceived threat: an analysis of host and immigrant attitudes in Germany. Int J Intercult Rel 30:683–702
Roth DE (2007) Bones and beyond: an update on the role of vitamin D in child and adolescent health in Canada. Appl Physiol Nutr Metab 32(4):770–777
Rothstein WG, Rajapaksha S (2003) Health beliefs of college students born in the United States, China, and India. J Am Coll Heal 51(5):189–194
Salehi L, Lofters AK, Hoffmann SM, Polsky JY, Rouleau KD (2015) Health and growth status of immigrant and refugee children in Toronto, Ontario: a retrospective chart review. Paediatr Child Health 20(8):e38–e42
Satia-Abouta J, Patterson RE, Neuhouser ML, Elder J (2002) Dietary acculturation: applications to nutrition research and dietetics. J Am Diet Assoc 102(8):1105–1118
Shields M (2005) Measured obesity: overweight Canadian children and adolescents. Nutrition: Findings from the Canadian Community Health Survey
Simich L, Jackson B (2010) Social determinants of immigrant health in Canada: what makes some immigrants healthy and others not? Migr Health 17:26–29
Statistics Canada (2011) The effect of immigration on social cohesion in Canada. http://www.statcan.gc.ca/pub/11f0019m/2008319/s13-eng.htm. Accessed 28 Mar 2017
Statistics Canada (2014) Overweight and obese youth (self-reported). http://www.statcan.gc.ca/pub/82-625-x/2015001/article/14186-eng.htm. Accessed 28 Mar 2017
Statistics Canada (2016) Immigration and ethnocultural diversity in Canada. Migration health http://www12.statcan.gc.ca/nhs-enm/2011/as-sa/99-010-x/99-010-x2011001-eng.cfm. Accessed 28 Mar 2017
Statistics Canada (2017) 2011 National Household Survey: data tables. http://www12.statcan.gc.ca/nhs-enm/2011/dp-pd/dt-td/Rp-eng.cfm?TABID=2&LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GK=0&GRP=1&PID=105470&PRID=0&PTYPE=105277&S=0&SHOWALL=0&SUB=0&Temporal=2013&THEME=95&VID=0&VNAMEE=&VNAMEF=. Accessed 30 Mar 2017
Tarasuk V, Mitchell A, Dachner N (2014) Household food insecurity in Canada, 2012. Toronto: Research to identify policy options to reduce food insecurity (PROOF). http://nutritionalsciences.lamp.utoronto.ca/. Accessed 29 Mar 2017
Tienda M, Haskins R (2011) Immigrant children: introducing the issue. Futur Child 21(1):3
Tremblay MS, Perez CE, Ardern CI, Bryan SN, Katzmarzyk PT (2005) Obesity, overweight, and ethnicity. Health Rep 16(4):23
United Nations (2016) International migration report 2015. http://www.un.org/en/development/desa/population/migration/index.shtml. Accessed 27 Mar 2017
United Nations High Commissioner for Refugees (1951) Convention relating to the status of Refugees Article 1. http://www2.ohchr.org/English/law/refugees.htm#wp1037003. Accessed 4 Feb 2011
United Nations High Commissioner for Refugees (2017) Figures at a glance. http://www.unhcr.org/figures-at-a-glance.html. Accessed 27 Mar 2017
United States Department of Agriculture (2016) Food security in the U.S.: measurement. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/measurement/. Accessed 18 May 2017
Vatanparast H, Nisbet C, Gushulak B (2013) Vitamin D insufficiency and bone mineral status in a population of newcomer children in Canada. Forum Nutr 5(5):1561–1572. https://doi.org/10.3390/nu5051561
Ward LM, Gaboury I, Ladhani M, Zlotkin S (2007) Vitamin D-decifiency rickets among children in Canada. CMAJ 177(2):161–166
Whiting SJ, Calvo MS (2005) Dietary recommendations for vitamin D: a critical need for functional end points to establish an estimated average requirement. J Nutr 135(2):304–309
World Health Organization (2000) General guidelines for methodologies on research and evaluation of traditional medicine. http://whqlibdoc.who.int/hq/2000/WHO_EDM_TRM_2000.1.pdf. Accessed 28 Mar 2017
World Health Organization (2001) Water-related diseases: malnutrition. http://www.who.int/water_sanitation_health/diseases/malnutrition/en/. Accessed 15 Nov 2010
World Health Organization (2004) A glossary of terms for community health care and services for older persons. http://www.who.int/kobe_centre/ageing/ahp_vol5_glossary.pdf?ua=1. Accessed 28 Mar 2017
World Health Organization (2007) WHO AnthroPlus. http://www.who.int/childgrowth/software/en/. Accessed 8 Jan 2011
World Health Organization (2014) Global health expenditure database. http://apps.who.int/nha/database. Accessed 29 Mar 2017
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this entry
Cite this entry
Vatanparast, H., Nisbet, C., Patil, R. (2019). Food Security and Nutritional Health of Newcomer Children. In: Preedy, V., Patel, V. (eds) Handbook of Famine, Starvation, and Nutrient Deprivation. Springer, Cham. https://doi.org/10.1007/978-3-319-55387-0_48
Download citation
DOI: https://doi.org/10.1007/978-3-319-55387-0_48
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-55386-3
Online ISBN: 978-3-319-55387-0
eBook Packages: MedicineReference Module Medicine