Abstract
Islet cell or pancreas transplantation is the only long-term diabetes treatment that consistently results in normal hemoglobin A1c levels without the risk of severe hypoglycemia. Additionally, islet cell or pancreas transplantation may prevent, halt, or even reverse the complications of diabetes. Consequently, it is an important part of the management of a subset of patients with diabetes, namely, those in renal failure and those with life-threatening complications of their diabetes such as hypoglycemic unawareness. Here, we explore the indications, options, and outcomes of islet cell or pancreas transplantation as a treatment for diabetes mellitus. The morbidity of solid-organ pancreas transplantation restricts pancreas transplantation to relatively younger and fitter patients. Islet cell transplantation is less invasive and, therefore, more appealing to patients, endocrinologists, and diabetologists. Pancreas transplants and islet transplants should be considered complementary, not mutually exclusive, procedures that are chosen on the basis of the individual patient’s surgical risk. As the mortality and morbidity of solid pancreas transplantation diminish and the longer-term outcomes of both solid-organ and islet transplantation improve, the appropriate indications for both procedures will expand, particularly with the increasing incidence of diabetes as well as evidence that transplantation is suitable not only for type 1 diabetics but also for selected insulin-dependent patients with type 2 diabetes.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
Beta-Cell Replacement Therapies as Treatment Options for Type 1 Diabetes Patients
The ultimate treatment goal for type 1 diabetes is to re-create normal (nondiabetic) or nearly normal blood sugar levels to assure a long healthy life. In healthy subjects under everyday life conditions, the mean 24-hour interstitial fluid glucose concentration is about 90 mg/dl, and the mean fasting glucose concentration is about 80 mg/dl with a mean peak tissue glucose concentration of about 120–130 mg/dl and mean time to peak glucose between 46 and 50 min (Freckmann et al. 2007). Moreover, tissue glucose concentrations in nondiabetic subjects were below 100 mg/dl and 140 mg/dl during 80% and 99.2% of the total day, respectively (Freckmann et al. 2007). In the last decades, significant improvements in insulin therapy thanks to new preparations (i.e., ultrafast and long-lasting insulin analogues) and the adoption of intensive diabetes management have resulted in an overall improvement of patients’ glycemic control and a decreased incidence of chronic complications of diabetes (Gregg et al. 2014). In spite of this, the treatment is still far from being optimal. Studies investigating continuous glucose profiles in diabetic patients demonstrated that glucose concentrations were above 140 mg/dl during about 60% of the total day (Garg et al. 2006) or above 180 mg/dl during about 30% of the total day (Bode et al. 2005). The majority of people with type 1 diabetes have higher HbA1c levels than recommended in guidelines based on the published evidence from registries (McKnight et al. 2015), and roughly only about one-fourth of patients with type 1 gains therapeutic target (Mannucci et al. 2014). High proportions of individuals not achieving glycemic targets with current therapies are also reported for patients treated at centers that focus on the care of type 1 diabetes (Miller et al. 2015). In fact, only a minority of children and adults with type 1 diabetes participating in the T1D Exchange clinic registry achieve HbA1c targets, despite insulin pump being used by 60% of participants (Miller et al. 2015). Moreover, the data indicate that acute complications of insulin treatment remain a problem (Weinstock et al. 2013) in a substantial percentage of patients: 6% reported having had a seizure or loss of consciousness due to hypoglycemia, and 3% reported having DKA event in the prior 3 months. Advanced technologies [insulin pumps (CSII), bolus calculators (BC), real-time continuous glucose monitors (RT-CGM), sensor-augmented pumps (SAP), low-glucose threshold suspend (LGTS) systems, low-glucose predictive suspend (LGPS) systems, and artificial pancreas (AP) systems] are becoming more prevalent in diabetes management, but the limitations of advanced technologies in reducing both A1c and hypoglycemia rates are relevant (Vigersky 2015). CSII reduces A1c in some (Pickup and Sutton 2008; Fatourechi et al. 2009; Bonfanti et al. 2015; Ross et al. 2015) but not all studies (Golden and Sapir 2012), while it improves hypoglycemia in patients with high baseline rates (Pickup and Sutton 2008). BC improve A1c and improve the fear of hypoglycemia but not hypoglycemia rates (Schmidt and Norgaard 2014). RT-CGM alone and when combined with CSII improves A1c with a neutral effect on hypoglycemia rates (Floyd et al. 2012; Golden and Sapir 2012). SAP improves A1c but not hypoglycemia rates (Bergenstal et al. 2010). LGTS reduces hypoglycemia with a neutral effect on A1c (Bergenstal et al. 2013), and LGPS reduces hypoglycemia with a small increase in plasma glucose levels (Maahs et al. 2014). In short-term studies, artificial pancreas systems reduce both hypoglycemia rates and plasma glucose levels (Phillip et al. 2013; Russell et al. 2014). CSII and RT-CGM are cost-effective technologies, but their wide adoption is limited by cost and psychosocial and educational factors. Exogenous insulin administration cannot avoid the long-term complications of diabetes in all patients, and the life expectancy of patients with diabetes is still much shorter compared to that of the general population (Hu et al. 2001; Franco et al. 2007; Lind et al. 2014; Livingstone et al. 2015). Diabetes is one of the leading causes of end-stage renal disease, blindness, and amputation (Gregg et al. 2014). In principle, the treatment for type 1 diabetes, type 3c diabetes, and many cases of type 2 diabetes lies in the possibility of replacing destroyed or exhausted beta-cell mass in order to restore two essential functions: sensing blood sugar levels and secreting appropriate amounts of insulin in the vascular bed, ideally into the portal system. Currently, the only available clinical approach of restoring beta-cell mass in patients with diabetes is the transplantation of beta cells (i.e., pancreas or islet transplantation). The goals of beta-cell replacement are to restore glucose-regulated endogenous insulin secretion with normalization of glucose levels, arresting the progression of the complications of diabetes and improving quality of life. In the allogenic setting, both pancreas and islet transplantation require lifelong immunosuppression to prevent rejection of the graft and recurrence of the autoimmune process. Current immunosuppressive regimens are capable of preventing beta-cell failure for months to years, but the agents used expose to several side effects and increase the risk for specific malignancies (Geissler 2015) and opportunistic infections (Helfrich and Ison 2015). In addition the most commonly used agents – calcineurin inhibitors and rapamycin – are also known to impair normal islet function and/or insulin action (Rangel 2014). Furthermore, these agents have other toxicities, including the harmful effect on renal function (de Mattos et al. 2000). Differently that for uremic patients in which chronic immunosuppression is already present because of concurrent or previous kidney transplantation, a specific assessment of the risk of the initiation of a long-term immunosuppressive therapy in islet or pancreas transplantation alone should be considered only in patients with serious progressive complications of diabetes in whom the quality of life is very limited by a poor glycemic control or a high number of severe hypoglycemic events notwithstanding optimized intensive insulin therapy or clinical and emotional problems with exogenous insulin therapy that are so severe as to be incapacitating.
Pancreas and Islet Cell Transplantation: Indication
Pancreas or islet transplantation can be performed simultaneously with kidney transplantation, after kidney transplantation or alone, depending on the clinical condition of the patient and on organ availability. A general overview of indications for pancreas or islet transplantation is provided in the Table 1. Within these general indications, some differences are observed in different countries, and there are important issues that are still to be addressed.
Indication in Uremic Patient
In general, patients who develop chronic end-stage renal failure, secondary to either type 1 or type 2 diabetes, who are on insulin and are not obese, are considered for simultaneous pancreas–kidney (SPK) transplantation (Robertson et al. 2006; Jahansouz et al. 2011; Gruessner and Gruessner 2013a). This indication is well defined and without controversy as the “gold standard” when the vascular status of the patient can support two organ transplants instead of one (Chiang et al. 2014). In fact diabetic subjects with end-stage renal failure have a high mortality risk (van Dellen et al. 2013). Kidney transplant alone confers a survival benefit compared with dialysis (Port et al. 1993), but the survival after SIK is superior to survival after cadaveric kidney transplant alone (Tyden et al. 1999; Ojo et al. 2001; Mohan et al. 2003), despite added surgical risk (Smets et al. 1999). Survival after living kidney transplantation alone was described to be equivalent to that after SPK (Rayhill et al. 2000), but there is strong evidence that successful pancreas transplantation still increases life expectancy. In fact, although patients undergoing SPK had a higher mortality risk compared with those undergoing living kidney transplantation in the first 18 months, this early survival disadvantage is lost after because of the effects of good metabolic control obtained by SPK (Reddy et al. 2003; Morath et al. 2008). Although stabilization of renal function contributes significantly to improved life expectancy after SPK, studies comparing SPK recipients with functioning grafts, those with either kidney or pancreas graft failure, and recipients of living and cadaveric kidney transplantation have demonstrated that the pancreas graft confers significant additional benefit beyond that offered by the kidney transplant alone (Salvalaggio et al. 2009; Weiss et al. 2009; Norman et al. 2011). Pancreas after kidney (PAK) is an alternative option to SPK. Patients who undergo PAK transplantation commonly have an identified living kidney donor and undergo cadaveric pancreas transplantation later on. PAK is also an option for diabetic patients with unstable glycemic control who have already had kidney transplantation with stable graft function and sufficient cardiac reserve to receive a second transplantation or in patients who received SPK and lose the pancreas for technical reasons, mainly thrombosis, shortly after transplantation. PAK is becoming increasingly used due to shorter waiting lists for kidney availability compared to SPK (Jahansouz et al. 2011). The main advantage of SPK is the high success rate of the pancreas graft, which contrasts with PAK and mainly pancreas transplant alone (PTA). One of the main reasons suggested for this success rate is the possibility of an early detection of acute rejection in concomitant transplanted kidney (which often is associated with rejection in the transplanted pancreas) by monitoring serum creatinine; this allows a quick treatment with immunosuppressant therapy (Jahansouz et al. 2011). Where a living donor option for kidney transplantation is available, PAK may be preferred in order to achieve earlier independence from dialysis; however, in light of the inferior pancreas graft survival outcomes of PAK compared with those of SPK, the former remains controversial, and the decision on how best to proceed must be made with careful consideration of the individual patient’s circumstances and their likely waiting time on the combined pancreas–kidney list. Data on the outcomes of SPK and PAK transplantation compared directly with simultaneous islet–kidney (SIK) and islet-after-kidney (IAK) transplantation are rare. There are no direct, randomized trials comparing the outcomes, and there are few observational studies (Gerber et al. 2008; Maffi et al. 2011; Lehmann et al. 2015; Moassesfar et al. 2016).
The available data on a long-term follow-up suggest that the combination of kidney transplantation with pancreas transplantation as well as with isolated islet transplantation results in significant and sustained improvement of glucose control without the occurrence of severe hypoglycemia. While insulin independence is more common in SPK/PAK recipients, SIK/IAK can be conducted with a lower complication rate. No difference in the decline of kidney function between the two groups is evident (Lehmann et al. 2015). A careful selection of the adequate procedure by interdisciplinary transplantation teams may help to ensure optimal care for patients with diabetes undergoing combined transplantation. The decision should be influenced by the assessment of pretransplant surgical risk and the definition of treatment goals. Both SPK and PAK should be undertaken in patients who are relatively young (<50 years) and nonobese (<30 kg/m2) and who do not have coronary artery disease and with vascular conditions capable to support double transplantation. These patient selection criteria minimize operative mortality (<1%) and reduce early technical pancreas graft loss (∼10%). Patients beyond 50 years require critical evaluation, because benefit for survival is not evident for this group (Ojo et al. 2001). Islet transplantation (SIK and IAK), a minimally invasive procedure, allows for inclusion of older patients and patients with coronary and peripheral artery disease who would be ineligible for a whole-pancreas transplant. Moreover islet recipients must consider glycemic control and absence of hypoglycemia as their primary therapeutic goal rather than insulin independence. Malignancies, chronic infections, and insufficient compliance are contraindications for both SPK/PAK and SIK/IAK transplantation.
Indication in Non-Uremic Patients
There has been debate about beta-cell replacement therapies (PTA and ITA) in the absence of an indication for kidney transplantation because of the risks of mortality, morbidity, and immunosuppression. Established indications for PTA and ITA have been developed by the American Diabetes Association (ADA) in 2004 (Robertson et al. 2004, 2006): “In the absence of indications for kidney transplantation, pancreas transplantation should only be considered a therapy in patients who exhibit these three criteria: (1) a history of frequent, acute, and severe metabolic complications (hypoglycemia, hyperglycemia, ketoacidosis) requiring medical attention; (2) clinical and emotional problems with exogenous insulin therapy that are so severe as to be incapacitating; and (3) consistent failure of insulin-based management to prevent acute complications.” The indications for PTA and ITA reported by ADA are generally associated to the concept of “brittle” diabetes. A proportion of T1D patients experience a highly instable form of the disease known as “brittle” and characterized by a severe instability of blood glucose levels with frequent and unpredictable episodes of severe hypoglycemia and/or ketoacidosis (Voulgari and Tentolouris 2011; Voulgari et al. 2012). Due to this unpredictable large variability in blood glucose levels, brittle T1D patients often report difficulties in finding an optimal insulin dosing schedule to normalize glucose levels (Bertuzzi et al. 2007). The definition of brittle diabetes has evolved since it was first introduced in the 1930s by Woodyatt to describe patients with excessive fluctuations of blood sugar which could not be explained by patient or physician errors and that unpredictability and unexpectedly led to hypoglycemic reactions (Tattersall 1997). Nowadays, a generally accepted definition of brittle diabetes could be a severe instability of blood glucose levels with frequent and unpredictable episodes of severe hypoglycemia and/or ketoacidosis that disrupts quality of life. The high incidence of severe hypoglycemia episodes observed in the brittle population and, in general, the metabolic instability lead to a reduction in the physiological response to these events and to a certain degree of impairment in the ability to identify further episodes, which is known as hypoglycemia unawareness (Cryer 2013). Several different etiologies have been described for brittle diabetes, although in a significant number of patients, the cause remains unknown. Organic causes explain brittleness in some occasions, and psychosocial factors have also been described in some patients (Gill 1992; Vantyghem and Press 2006; Voulgari et al. 2012). The main organic causes of brittleness include malabsorption, certain drugs (including alcohol and antipsychotics), defective insulin absorption or accelerated degradation, defect of hyperglycemic hormones especially glucocorticoids and glucagon, and above all autonomic neuropathy resulting in changed (delayed or fastened) gastric emptying and hypoglycemic unawareness. Apart from organic causes, psychosocial factors that seem to cause brittle diabetes are complex and diverse. The deliberate induction of factitious brittleness (i.e., hypoglycemia and/or ketoacidosis events) has been described as a response to intolerable life stress (Gill 1992). Furthermore obsessive control and frequent doses adjustments can in some instances increase blood glucose instability, instead of improving metabolic control. Eating disorders like anorexia nervosa in patients with T1D might lead to insulin dose reduction or omission by the patient as a method of weight control. The natural history of the condition remains largely unknown. A few long-term follow-up studies of brittle patients provide some insight on the course of the disease (Tattersall et al. 1991; Kent et al. 1994; Cartwright et al. 2011). According to these studies, the high frequency of hypoglycemia and/or diabetic ketoacidosis events in brittle patients translates in the development of diabetes complications in the long term including nephropathy, retinopathy, and neuropathy, which show an increased incidence compared to non-brittle patients. Unnoticed severe hypoglycemia events are life-threatening and one of the major determinants of quality of life impairment in brittle diabetes patients. Diabetes-related complications are also the main cause of death of brittle patients (Cartwright et al. 2011). Available literature on the epidemiology of brittle T1D is scarce. One of the main reasons for this is probably the lack of a clear definition of diagnostic criteria for the condition. A prevalence rate of 1.2/1,000 diabetic patients and of 2.9/1,000 insulin-treated diabetic patients was reported (Gill et al. 1996). Brittle diabetes is associated with a substantial humanistic burden to patients, caregivers, and family. The frequency of acute events like hypoglycemia or diabetic ketoacidosis and the subsequent hospital admissions, as well as the incidence of complications, have a major impact in the quality of life of patients. When compared to patients with “stable” T1D, the number of emergency admissions and the length of in-hospital stay due to poor diabetic control are much more frequent in brittle patients, in some cases resulting in patients spending up to several months each year in the hospital (Voulgari and Tentolouris 2011). Lifestyle disruption is also induced by other aspects like pregnancy complications and a higher risk of death due to diabetes complications (Voulgari et al. 2012). Most studies assessing the characteristics of brittle diabetes have also identified a high prevalence of psychosocial disruptions and psychiatric disorders, especially mood and anxiety disorders (Tattersall et al. 1991). Patients with brittle diabetes are generally terrified by the condition and resist with psychotic-type defense reactions when psychotherapeutic approaches are performed commonly driving to deep regression, suicidal feelings, and mistreatment of diabetes. Several measures and methodologies have been introduced in order to quantify metabolic instability, including the assessment of the mean amplitude of the largest glycemic excursions or the mean of daily differences between blood glucose values, among others (McDonnell et al. 2005; Baghurst 2011). Recently, beta-cell replacement therapies were indicated in the treatment algorithm of “problematic hypoglycemia” (Choudhary et al. 2015). Hypoglycemia is a common and greatly feared complication of T1D (Seaquist et al. 2013; Frier 2014). The term severe hypoglycemia is used for episodes with such a degree of cognitive impairment that the patient needs assistance from another person in order to achieve normal glycemia (Workgroup on Hypoglycemia, American Diabetes Association 2005). Many severe hypoglycemia events are single episodes caused by insulin dosing errors, exercise, and alcohol. Conversely, problematic hypoglycemia is a condition in which episodes of severe hypoglycemia are unpredictable, cannot be easily explained or prevented, and, therefore, have a significant negative impact on health and quality of life. The criteria of problematic hypoglycemia include two or more episodes of severe hypoglycemia in the past 12 months or one episode of severe hypoglycemia in the past 12 months associated with impaired awareness of hypoglycemia, extreme glycemic lability, or major fear and maladaptive behavior. Simple tools are available clinically to quantitate awareness of hypoglycemia (Gold et al. 1994; Clarke et al. 1995), hypoglycemia severity (Ryan et al. 2004b), and glycemic lability (Ryan et al. 2004b). Scores and indexes have been developed to quantify hypoglycemic frequency and hypoglycemic awareness, including the low blood glucose index (LBGI), the Clarke score, or the HYPO score:
-
The LBGI is a summary statistic used to assess the risk for severe hypoglycemia based on the percentage of low self-monitored blood glucose readings and their magnitude in the lower blood glucose range, thus integrating the frequency and severity of hypoglycemia events. Based on the LBGI score, patients are classified as having a low (<2.5), moderate (2.5–5), and high (>5) risk of severe hypoglycemia (Kovatchev et al. 1998).
-
The Clarke score is based on an eight-question survey to patients aimed at assessing patients’ hypoglycemia awareness. The final score may range between 0 and 7. A score ≤2 would classify patients as aware, while a score ≥4 indicates reduced awareness of hypoglycemia and therefore an increased risk of severe hypoglycemic episodes (Clarke et al. 1995).
-
The HYPO score used a complex scoring system that takes into account the frequency, the severity, and the loss of symptoms of hypoglycemia. It combines the data obtained from records of capillary blood glucose levels over a 4-week period and the number of self-reported hypoglycemic events during this period and during the past year. Points are awarded for each documented episode of hypoglycemia with extra points depending on the severity of the associated neurologic symptoms and if additional help was required within the episode. If autonomic symptoms provided adequate warning of impending hypoglycemia, no points are awarded to the episode. Normal subjects usually show a HYPO score of 0, while stable diabetes patients’ scores are around 200. A HYPO score ≥1047 (ninetieth percentile) indicate that the patient has severe problems with hypoglycemia (Ryan et al. 2004b).
The epidemiology of severe hypoglycemia in T1D patients has been widely described in the literature. Studies identified in a comprehensive review of evidence report a yearly prevalence of severe hypoglycemia of 7–66% in T1D patients (Pedersen-Bjergaard et al. 2003; Giorda et al. 2015), although in most cases, prevalence ranges from 30% to 40% (Pedersen-Bjergaard et al. 2004; UK Hypoglycaemia Study Group 2007; Gruden et al. 2012; Weinstock et al. 2013; Frier 2014). In terms of incidence, the number of severe hypoglycemia episodes per patient-year generally ranges between 1.0 and 1.7, although some variability exists, and one episode of severe hypoglycemia is experienced by one-third of patients with T1D at least once a year. Comparatively fewer studies have been identified specifically addressing hypoglycemia unawareness, in part, due to a lack of an agreed definition (Graveling and Frier 2010; Hoi-Hansen et al. 2010). Hypoglycemia unawareness is found in 20–40% of patients with T1D (Gold et al. 1994; Geddes et al. 2008; Choudhary et al. 2010; Ogundipe et al. 2011; Hopkins et al. 2012) and increases the risk of severe hypoglycemia by 6–20-fold (Gold et al. 1994; Clarke et al. 1995; Pedersen-Bjergaard et al. 2004). Prevalence of impaired awareness of hypoglycemia increased with diabetes duration and ageing (Olsen et al. 2014). Recurrent hypoglycemia can cause significant morbidity (Frier 2004, 2014) and mortality. Among individuals with T1D, 4–10% of all deaths are attributed to severe hypoglycemia (Skrivarhaug et al. 2006; Feltbower et al. 2008), and risk of death 5 years after an episode of severe hypoglycemia is increased 3.4-fold (McCoy et al. 2012). A four-stage treatment algorithm was recently proposed for “problematic hypoglycemia.” All patients with problematic hypoglycemia should undergo structured or hypoglycemia-specific education programs (stage 1). Glycemic and hypoglycemia treatment targets should be individualized and reassessed every 3–6 months. If targets are not met, one diabetes technology – continuous subcutaneous insulin infusion or continuous glucose monitoring – should be added (stage 2). For patients with continued problematic hypoglycemia despite education (stage 1) and one diabetes technology (stage 2), sensor-augmented insulin pumps preferably with an automated low-glucose suspend feature and/or very frequent contact with a specialized hypoglycemia service can reduce hypoglycemia (stage 3). For patients whose problematic hypoglycemia persists, ITA or PTA should be considered (stage 4). Because PTA (Gruessner and Gruessner 2013b) and ITA (Markmann 2016) outcomes have gradually improved and are both effective in preventing severe hypoglycemia and achieving near-normoglycemia, the optimal treatment option will require an individualized discussion of multiple factors, including the procedural risks (which are higher for a pancreas transplant), importance of insulin independence, waiting time, and sensitization. Some contraindications to a pancreas transplant (age >50 years, high cardiac risk) are common in patients with problematic hypoglycemia; they may only be eligible for an islet transplant. Yet, a small proportion of patients may be ineligible for an islet transplant because of their weight or insulin requirements. The transplant team should consider each patient’s preferences and perceptions of risks and benefits. A summary of indications and contraindications of SPK, PAK, PTA, and ITA is provided in Table 2. If the patient has advanced renal disease and is undergoing a renal transplant, a SPK or PAK is reasonable especially if there are problems with lability or hypoglycemia. If the center has local expertise in preparing islets, SIK or IAK transplants could be considered. If the patient has a kidney transplant and has stable diabetes, performing a pancreas transplant, in addition, increases the risk of surgery and requires full discussion with the patient in regard to short- and long-term risks/benefits. If the patient has labile diabetes and no renal disease, the choice between ITA and PTA should be done together with the patients, according to expectations, psychological conditions, and propensity to risk. The burden of procedure-related adverse events, which is clearly higher for PTA than for ITA, should be carefully weighted up, and the patient might be recommended to the more suitable indication, in the center with the best expertise. The most challenging patients are those with unstable diabetes (lability or hypoglycemia problems) and some renal dysfunction. If the renal dysfunction is limited to the presence of microalbuminuria, then islet transplantation is reasonable. If there is macroproteinuria present, the outcomes are less certain, and a pancreas or islet transplant alone can be considered in the light of the possibility that the immunosuppressive drugs may hasten the decline of renal function. A particular subgroup is represented by brittle diabetic patients with chronic kidney disease in an intermediate stage (III and IV, GFR 15–30), when the proposal of SPK seems too early and the proposal of PTA too risky for the progression of kidney disease, thanks to nephrotoxic immunosuppressants. In patients in stage III (GFR 30–60), PTA can be safely and reasonably proposed once assured that a potential kidney living donor is available, useful in case of progression of kidney disease. In patients in stage IV (GFR 15–30), SPK can be proposed if risk equations to predict kidney failure (Tangri et al. 2016) can envisage early and rapid progression of ESRD .
Current Status of Pancreas Transplantation
Surgical Technique and History of Pancreas Transplantation
Most transplant units around the world transplant the whole pancreas together with a segment of donor duodenum (Han and Sutherland 2010). The arterial inflow is usually from the recipient common iliac artery with venous drainage to the common iliac vein. Pancreas transplantation was first used for the treatment of diabetes in humans in 1966 (Kelly et al. 1967). In the 1970s the pancreas transplant development was continued with the first urinary drainage via the ureter (Gliedman et al. 1973), segmental PTA with end-to-side ductoenterostomy (Merkel et al. 1973), and injection of neoprene (Dubernard et al. 1978). In the 1980s, the bladder drainage technique was reported and developed (Cook et al. 1983; Starzl et al. 1984; Nghiem and Corry 1987). From the mid-1980s to mid-1990s, the anastomosis of the donor duodenum was usually to the bladder drainage and was the most common technique worldwide (Prieto et al. 1987). This technique has the advantage of enabling urinary amylase to be used as a biochemical marker of pancreatic function and fewer complications with regard to contamination from enterotomy or duodenal leaks (Sollinger et al. 2009); however, bladder drainage has the disadvantage of being associated with metabolic and urological complications including dehydration, metabolic acidosis, and irritation from cystitis. For this reason, the enteric drainage became the routine method in the late 1990s (Gruessner and Sutherland 2000). This technique is more physiological but renders the pancreas less easily monitored. Despite this, as a result of improvements in surgical technique, radiological imaging and antimicrobial prophylaxis, outcomes after pancreas transplantation with enteric drainage, are equivalent to those after bladder drainage. The first large case series of living donor segmental transplantation – a technique started in the late 1970s (Sutherland et al. 1980) – was reported in the 1990s (Gaber et al. 1995b). The use of portal drainage in recipients of enterically drained whole-organ pancreaticoduodenal transplants was described in the 1990s (Rosenlof et al. 1992). This approach, although associated with more physiological systemic levels of insulin, is not supported by evidence of substantial benefit with respect to graft or patient survival (Bazerbachi et al. 2012). Although there has been concern that the hyperinsulinemia associated with systemic venous drainage may be associated with adverse events such as an increased risk of atherosclerosis, there is no convincing evidence that systemic venous drainage places pancreas recipients at a disadvantage (Stadler et al. 2010) .
Clinical Outcomes of Pancreas Transplantation
From 1966 to 2012, >42,000 pancreas transplants performed worldwide were reported to the International Pancreas Transplant Registry (IPTR), the majority of which reported diabetes as underlying disease (over 90% T1D) (Gruessner 2011; Gruessner and Gruessner 2013a). The most frequently used modality of pancreatic transplant was SPK (75%), followed by PAK (12%) and PTA (7%). The number of pancreatic transplants grew until 2004, and since then, it has gradually diminished (Gruessner and Gruessner 2014; Kandaswamy et al. 2015).
Patient and Graft Survival
Patient survival is equivalent after SPK, PAK, and PTA (Gruessner and Gruessner 2013a). Patient survival rates have continued to improve over time in all three categories, reaching 96% at 1 year and 80% at 5 years posttransplantation (Gruessner and Gruessner 2013a). In all three recipient categories, cardiovascular and/or cerebrovascular problems and infections were the leading causes of early (<3 months posttransplant) and late (>1 year posttransplant) death after transplant surgery (Gruessner and Gruessner 2012). Pancreas graft survival (defined as insulin independence) rates have also improved significantly over time in all three categories but remains higher with SPK transplantation. Graft survival rates at 1 year were 89% (SPK), 86% (PAK), and 82% (PTA). The figures at 5 years were 71% (SPK), 65% (PKT), and 58% (PTA). The estimated half-life (50% function) of pancreas grafts is 14 years (SPK), 7 years (PAK), and 7 years (PTA). In case of pancreas failure, the organ can be removed, when necrosis or colliquation is envisaged or maintained when it becomes fibrotic, without further risk of colliquation. In case of failure, a second pancreas transplant can be considered. In this case immunosuppression should be maintained in order to avoid appearance of DSA. In this case retransplantation must be done in a timely manner. Absolute contraindications to pancreas retransplantation are poor cardiovascular conditions, impairment of kidney function, and high percentage of panel reactive antibody (PRA) or high level of donor-specific alloantibodies (DSA).
Complications
Pancreas transplantation is a major surgical procedure associated with several technical complications. In general, the primary complication related to pancreatic graft loss is technical failure, followed by acute or chronic rejection. The rate of technical failure has declined across all recipient categories and is currently about 9% (Kandaswamy et al. 2016). Considering transplants performed between 2007 and 2011, technical complications were the most common reasons for graft loss posttransplant in all three categories (63% for SIK, 75% for PAK, and 77% for PTA). Technical failure is understood as the loss of the graft in the first 3 months of transplant due to vascular thrombosis (50%), pancreatitis (20%), infection (18%), fistulas (6.5%), and hemorrhage (2.4%). The rate of graft loss owing to acute rejection peaked between 3 and 12 months posttransplant, while the rate of graft loss owing to chronic rejection constantly increased from time since surgery (18% for SIK, 14% for PAK, and 36% for PTA >1 year posttransplant). Chronic rejection (18% for SIK, 14% for PAK, and 36% for PTA) and death with a functioning graft (38% for SIK, 18% PAK, and 13% for PTA) are the two most common causes of long-term graft loss (>1 year posttransplant) (Gruessner and Gruessner 2012). Pancreatic transplant presents 10–20% of surgical complications that require review laparotomy. The risk factors for surgical complications include prolonged time in peritoneal dialysis, donor or recipient with a body mass index >28 kg/m2, donor or recipient age over 45 years, cerebrovascular disease as cause of donor death, prolonged preservation time (>20 h), retransplantation, and prior abdominal surgery (Sutherland et al. 2001; Gruessner and Gruessner 2012, 2014). One of the most feared complications in pancreatic transplant with enteric drainage is intestinal leak, since it poses risks to patient’s survival (Jahansouz et al. 2011). The incidence of intestinal leak ranges from 5% to 8%, and most occur during the immediate postoperative period. The early leak is related to technical problems, such as impaired blood irrigation and ischemia. The potential risk factors for the occurrence of early intestinal leak are prolonged cold ischemia time, duodenal trauma, postreperfusion pancreatitis, and intra-abdominal infection. Its treatment generally leads to the removal of the pancreatic graft (Nath et al. 2005). Pancreatic transplants with bladder drainage imply frequent and severe urological and metabolic complications. Approximately 10–25% of patients submitted to pancreatic transplant with bladder drainage need to be submitted to intestinal conversion of the graft’s exogenous drainage (Stratta 2005). The main metabolic complications are metabolic acidosis and dehydration due to loss of water and sodium bicarbonate in the urine. These patients should receive adequate fluid and bicarbonate replacement in the follow-up of pancreatic transplant with bladder drainage. Despite better pancreatic transplant results, infectious complications continue to be the primary causes of morbidity and mortality. In fact, the use of immunosuppressant drugs in pancreas transplantation recipients is associated with an increased incidence of infections. Infections are more common in the first months following transplantation. The main pathogens involved are bacterial (Staphylococcus sp., Pseudomonas aeruginosa, Clostridium difficile) and viral (mainly Cytomegalovirus), although some fungal infections may be observed (Candida sp.). The urinary tract and abdominal wall are the most affected sites. Infection rates tend to decline after the first 3 months. In the long term, a retrospective cohort study including 216 pancreas transplant recipients identified a 63% incidence of infections (mainly of bacterial origin) requiring hospitalization during a >5-year follow-up period resulting in an increased risk of mortality (Rostambeigi et al. 2010). Patients submitted to pancreas transplant have a high risk of developing infection by Cytomegalovirus due to the use of antilymphocyte serum in immunosuppression protocols. The mean incidence is 25%. The incidence of malignancies secondary to immunosuppression is also increased in pancreas or kidney–pancreas transplant recipients. Data reported in the literature show similar long-term figures compared to those reported for other solid organ transplantation recipients (Stratta 1998). A retrospective single-center study including 360 diabetic patients who had undergone SPK transplantation reported an overall incidence of malignant tumors of 6.2% (n = 25) after a median follow-up period of 8 years posttransplant. Most common tumor types were non-melanoma skin cancers, lymphomas and lung adenocarcinoma, bladder carcinoma, and peritoneal carcinoma (Girman et al. 2011).
Immunosuppression
Immunosuppressant induction and maintenance regimens to avoid graft rejection in pancreas transplant recipients have evolved over time, resulting in improved outcomes in terms of patient and graft survival. The majority of units use biological antibody induction (thymoglobulin, alemtuzumab, or basiliximab) to achieve profound immune cell depletion lasting for the first 3 months when the risk of rejection is greatest. There is no difference in patient or graft outcomes according to which induction they received, although a tendency toward less acute rejection with alemtuzumab was described (Hao et al. 2012). Induction is followed by a maintenance combination of tacrolimus (a calcineurin inhibitor, CNI) and mycophenolate mofetil (an antiproliferative agent) to block T-cell activation and expansion, respectively. There is an increasing trend toward the use of steroid-free regimens in all areas of transplantation, and steroids are early or delayed withdrawal or not routinely used at all in either pancreas or islet cell transplantation (Gruessner and Gruessner 2012). The advent of inhibitors of the mammalian target of rapamycin inhibitors (mTORI), such as sirolimus and everolimus, provided an opportunity to reduce both the diabetogenic and nephrotoxic potential of the immunosuppression, although it later transpired that mTORIs do have some nephrotoxicity manifesting as proteinuria (Letavernier and Legendre 2008), as well as a potential to cause diabetes (Johnston et al. 2008). Tolerability of mTORI, particularly their tendency to cause mouth ulcers, rashes, joint pain, and edema, has prevented their wider use (Campistol et al. 2010). Nevertheless, where they are tolerated, they provide a good alternative to CNI-based immunosuppression. The mTORI have a theoretical advantage over tacrolimus for recipients of a pancreas transplant alone (PTA), in whom preservation of renal function is important, and latest data suggest that 18% of PTA recipients are on mTORI (Gruessner and Gruessner 2013b). The combination of CNI and mTORI can provide enhanced immunosuppression (McAlister et al. 2000) but was associated with a risk of enhanced nephrotoxicity and other complications(Feldmeyer et al. 2012) and has proved useful to rescue patients with difficult-to-manage rejection. The other area where mTORI may have a role is in the management of transplant patients who develop a malignancy, since mTORI have been shown to have antineoplastic properties (Hasskarl 2014). The most recent addition to the immunosuppressive armory is belatacept, a biological agent which blocks the CD28 co-stimulatory pathway (Larsen et al. 2005). Results of its use in pancreas transplantation are awaited, but it may be a good alternative to mTORIs in patients with CNI nephrotoxicity (Mujtaba et al. 2014) .
Life Expectancy
To this day, both ethical and practical considerations have prevented randomized controlled trials comparing the outcomes of simultaneous pancreas and kidney transplants versus kidney-only transplants, pancreas after kidney transplants versus kidney-only transplants, and pancreas transplants alone versus intensive insulin therapy. The three different modalities of pancreas transplantation (SPK, PAK, and PTA) have been suggested to have long-term mortality benefit compared to continuous insulin treatment in patients who are on waiting list for transplantation (Gruessner et al. 2004; Siskind et al. 2014), although this benefit has been more demonstrated in patients undergoing SPK (Smets et al. 1999; Becker et al. 2000; Ojo et al. 2001; Reddy et al. 2003; Kleinclauss et al. 2009). The survival benefit achieved by SPK, when compared to waiting-list patients, is 14.4 versus 3.7 years, in terms of median survival (propensity score matching) (Rana et al. 2015). In a previous study conducted in 2004 with data from the UNOS/IPTR database on 13,467 patients, Gruessner et al. (2004) reported significantly decreased mortality after the first year posttransplant among patients who had undergone SPK, PAK, and PTA compared with patients who remained on the waiting lists (SPK, HR 0.04 [CI, 0.03–0.04; p < 0.0001)]; PAK, HR, 0.18 [CI, 0.13–0.25; p < 0.0001]; PTA, 0.15 [CI, 0.08–0.29; p < 0.0001] (Gruessner et al. 2004). The patient survival rate at 10 years posttransplant is significantly higher in recipients of a SPK than of a kidney transplant from a deceased donor. Recipients of a SPK had the greatest longevity (23.4 years), as compared with 20.9 years for recipients of a kidney transplant from a living donor and 12.8 years for recipients of a kidney transplant from a deceased donor (Gruessner and Gruessner 2013a). The survival benefit of isolated pancreas transplant (after kidney transplant and alone) is more controversial. Earlier reports stating a survival disadvantage for recipients of solitary pancreas transplants (PAK and PTA) compared with patients on the waiting list for a transplant (Venstrom et al. 2003) now seem to be unsubstantiated (Gruessner et al. 2004; Siskind et al. 2014). Recently UNOS data have shown that pancreas transplantation alone, when compared to waiting list patients, confers a survival benefit of 6.7 years (14.5 vs. 7.8) in terms of median survival (propensity score matching) (Rana et al. 2015). In recipients of PAK, evidence shows that the pancreas transplant improves long-term patient and kidney graft survival rates. Also, glomerular filtration rates appear significantly higher in the kidney graft of recipients of pancreas after kidney transplants than in recipients of kidney transplants alone (Kleinclauss et al. 2009). The survival benefit of PTA is debated. The benefit for the individual patient must be considered by weighing the incapacities experienced with insulin-based treatments against the risks of surgery and immunosuppression. For patients who have experienced frequent and significant hypoglycemic episodes, particularly those requiring third-party assistance, pancreas transplant can be a lifesaving procedure.
No specific quality-of-life questionnaire for use in transplantation currently exists, and so most studies have been limited not only by size but also by the use of generic and heterogeneous quality-of-life measures (Gross and Zehrer 1992; Dew et al. 2000; Speight et al. 2010). A successful simultaneous pancreas and kidney transplant with sustained graft function leads to a large improvement in quality of life, including greater satisfaction with life and health, more feelings of control and independence, and perceptions of better physical, mental, and social health and functioning (Nakache et al. 1994; Isla Pera et al. 2009; Ziaja et al. 2009; Smith et al. 2010). The effect of pancreas after kidney transplants and pancreas transplants alone on quality of life is more difficult to determine because of the much smaller numbers of recipients. Freedom from insulin is exchanged for the complications of immunosuppression, and the short-term difficulties of postoperative recovery are balanced against the long-term benefits .
Metabolic and Functional Outcomes After Pancreas Transplantation
When a segment of the pancreas is transplanted, as it was in the early period of pancreas transplantation, mild metabolic abnormalities were observed, such as impaired glucose tolerance and delayed insulin response to glucose (Pozza et al. 1983). Whole-organ pancreas transplantation achieves a high degree of insulin independence, usually with normalization of many of the frequently measured variables of metabolic function including HbA1c and appropriate insulin, C-peptide, and glucagon responses to circulating blood glucose levels; however, the physiology of glucose homeostasis after pancreas transplantation is not fully understood. A successful pancreas transplant seems to more effectively lower the levels of HbA1c than intensive insulin therapy, and even 10 years posttransplant, a successful pancreas transplant can preserve insulin secretion and provide good glycemic control (Dieterle et al. 2007). Restoration of β-cell secretory capacity, improvement in glucose counter-regulation, and return to hypoglycemia awareness can all be achieved with a successful pancreas transplant (Rickels 2012). Several studies (White et al. 2009; Gruessner and Gruessner 2013a) have reported long-term beneficial effects of the different types of pancreas transplantation on chronic microvascular diabetes complications including diabetic nephropathy (Fioretto et al. 1998, 2006; Fiorina et al. 2007), neuropathy autonomic and peripheral (Kennedy et al. 1990; Martinenghi et al. 1997; Navarro et al. 1997), gastroparesis (Gaber et al. 1991), retinopathy (Koznarova et al. 2000; Giannarelli et al. 2005, 2006), microvascular and macrovascular disease including cerebral vasculopathy and morphology (La Rocca et al. 1995, 2001; Morrissey et al. 1997; Jukema et al. 2002; Larsen et al. 2002, 2004; Biesenbach et al. 2005), cardiac function (Gaber et al. 1995a; Fiorina et al. 2000, 2012; Coppelli et al. 2003; Folli et al. 2010), and sexual function (Salonia et al. 2011). Despite such encouraging results, caution must be exercised for a number of reasons. It has been acknowledged that there is a paucity of long-term, prospective randomized studies of sufficient size to draw meaningful conclusions and that at the present time much of the benefit is circumstantial with most evidence limited to single-center studies. Exposure to calcineurin inhibitors and dehydration can result in impaired kidney function (Boggi et al. 2011); as a result, progression of retinal as well as microvascular lesions has been reported (Ramsay et al. 1988) .
Current Status of Pancreatic Islet Transplantation
History of Islet Transplantation
The real father and pioneer of modern-day islet transplantation is Paul E. Lacy. He was the first to describe the method to isolate islets from rodent pancreata in 1969 and few years later carried out successful islet transplantations in rodents for the first time (Ballinger and Lacy 1972). The islet isolation technique developed in the rat by doctor Lacy prompted a surge of experimental studies in rodents. However, for several years the attempts to extend the Lacy isolation protocol to large animal pancreas (i.e., dog, nonhuman primate, and human) yielded poor results. A turning point for clinical islet transplantation was the introduction of the “automated method” of pancreas dissociation by Camillo Ricordi. The method consisted of a mechanically enhanced enzymatic digestion based on a dissociation/filtration chamber allowing pancreatic fragments and islets freed from the gland to be removed promptly from the system to avoid over-digestion while preserving cluster integrity. The method was first published in 1988 (Ricordi et al. 1988) and has represented ever since the gold standard for virtually all research centers working on human (Ricordi 2003) and large animal islets (Ricordi et al. 1990), besides its application for the isolation of other tissues (Vizzardelli et al. 2001). In 1990, the introduction of novel techniques to improve the efficiency of the isolation techniques resulting in high yields of pancreatic islets prompted the development of numerous clinical islet transplantation programs around the world. The first series of patients with sustained insulin independence was reported in nine patients undergoing excision of the liver and pancreas (that would result in surgery-induced diabetes) and receiving allogeneic liver and islet transplantation from the same cadaveric donor. The first clinical case of sustained insulin independence following allogeneic islet transplantation was a 15-year-old woman whose visceral organs were removed for cancer and who received a multi-visceral organ (liver, small bowel, and islet) transplantation (Tzakis et al. 1990; Ricordi et al. 1992). In 1990, doctors Scharp, Lacy, and colleagues at Washington University reported the first case of transient exogenous insulin independence following transplantation of 800,000 cultured allogeneic islets (pool of two allogeneic islet preparations), isolated using the automated method into a patient with T1D receiving Minnesota antilymphocyte serum, azathioprine and cyclosporine (Scharp et al. 1990). Ten days after transplantation, the patient achieved normoglycemia (albeit with residual glucose intolerance) and discontinued exogenous insulin for 2 weeks (Scharp et al. 1990). Insulin independence following islet transplantation from a single donor obtained using the automated method was reported by Dr. Carlo Socci and colleagues at the San Raffaele Institute in Milan (Italy) in a patient with T1D transplanted in April 1990 (Socci et al. 1991). Subsequently, insulin independence and/or consistent graft function after islet transplantation was reported across the world using cryopreserved (Warnock et al. 1991) along with fresh allogeneic islets, paving the way for the clinical application of cellular therapies to restore beta-cell function in patients with T1D (Hering et al. 1994; Secchi et al. 1997). Unfortunately, despite the advances in this field, between 1990 and 1998, only 8% of the patients receiving and islet transplant remained insulin-independent for more than 1 year (Bretzel 2001). A major advance occurred in 2000, when the University of Alberta group reported that with their protocol (known since then as the “Edmonton Protocol”), they were able to consistently achieve long-term insulin independence −100% at the end of the first year in seven patients with T1D (Shapiro et al. 2000). The Edmonton Protocol included two novel key elements that contributed to those successful results. The first consisted in the intraportal infusion of freshly isolated islets, followed by a second and sometimes a third infusion of additional islets from different donors, to achieve an islet mass [in their experience 10,000 islet equivalents per kilogram (IE/Kg)] necessary to achieve insulin independence. The second was the use of a steroid-free, rapamycin-based protocol of immunosuppression. The interest in islet transplantation was once more refueled, and several centers worldwide resumed their clinical programs (Shapiro et al. 2003). If we consider the 2007–2010 period, the islet graft survival (C-peptide ≥0.3 ng/mL) of 92% at 1 year and 83% at 3 years compares very favorably with whole-pancreas graft survival of 80% at 1 year and 61% at 3 years. In more recent years, these graft survival rates translate to an unconditional 44% insulin independence at 3 years, the highest long-term islet transplant success rate observed to date (Barton et al. 2012). For more information on the history in the field of islet cell transplantation to restore beta-cell function in patients with diabetes, see the recent review (Piemonti and Pileggi 2013).
Process of Islet Transplantation
The process of islet transplantation includes three different stages: (1) pancreas donation and retrieval, (2) islet isolation and culture, (3) islet transplantation.
Pancreas Donation and Retrieval
The selection of a donor pancreas for islet isolation is a key step in the transplantation procedure. Several studies have been conducted to identify the main donor characteristics required for successful islet isolation. Multivariate analyses suggest that donors >20 years of age, with a high body mass index (BMI) and normoglycemic (HbA1c < 6.0%), without hypotension or cardiac arrest and with a minimal inotropic support are optimal for islet isolation (Nano et al. 2005; Shapiro 2012; Balamurugan et al. 2014). However, the decision to allocate a pancreas to islet isolation is generally dependent on the possibility of using the pancreas for a whole-organ procedure, which is normally prioritized given the largest experience with this procedure (Berney and Johnson 2010). The surgical procedure for pancreas retrieval needs to be conducted meticulously. The maintenance of the integrity of the pancreatic capsule and duodenum is crucial for the digestion process later on. The duration of cold ischemia is also critical for a successful procedure as islets are particularly vulnerable to ischemia. It is generally recommended that cold ischemic time should not exceed 8 h (Mittal et al. 2014).
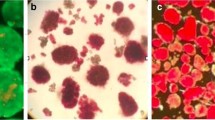
Islet Isolation
The aim of the islet isolation process is to extract the islets of Langerhans (approximately 1–2% of the pancreas) while removing the exocrine/acinar pancreatic tissue. It remains a challenging procedure requiring large expertise and is centrally performed by some highly specialized centers worldwide that generally provide islets for different implanting centers. Even in leading isolation centers, transplantable yields are only achieved in about 50% of pancreases. Islet isolation comprises two different steps: pancreas digestion and islet purification. Pancreas digestion is conducted as a combination of two procedures. Initially, the pancreas is disintegrated through enzymatic digestion by collagenase. Subsequently, a mechanical dissociation process of the already digested pancreas is performed by either manual or automated agitation within a digestion chamber. As a result, a suspension digest containing both the islets and the exocrine and ductal tissue is obtained. After digestion of the pancreas, the suspension digest undergoes purification to decrease transplanted tissue volume and prevent the activated pancreatic enzymes from being transplanted alongside the islet graft albeit with minimum loss of islet. This process is performed by density gradient purification, as islets are less dense than the exocrine and ductal tissue. Once the islets have been purified, they are counted and assessed for overall percentage purity and percentage viability (Johnson and Jones 2012). A minimal islet mass of 5,000 IEQ/kg is generally required for each transplant and >8,000 IEQ/kg for single-donor success (Shapiro 2012).
Islet Transplantation
The isolated pancreatic islets are subsequently infused into the hepatic portal system of the recipient by transhepatic cannulation of the portal vein with ultrasound and/or fluoroscopic guidance (Gaba et al. 2012). The infusion process lasts for about 1 h, and patients are generally discharged from the hospital within 48 h, once clinically stable and without complications. The initial few days following the islet infusion are critical for the final outcome of the islet transplantation process. Clinical and animal models show that up to 75% of the graft is lost during this period. It is suggested that islet graft loss is mainly related to an activation of the immune system of the recipient, to the ischemia reperfusion injury of the islets, and to relative ischemia in portal venules. Different approaches to improve engraftment are currently under investigation, including the use of anti-TNF agents, anti-IL-1 agents or glucagon-like-peptide 1 (GLP-1) analogues like exenatide.
Clinical Outcomes of Islet Transplantation
Islet transplantation is a minimally invasive treatment that has the potential to reverse diabetes thus resulting in an alternative to whole-pancreas transplantation in diabetic patients. It is estimated that over 1,400 islet transplants have been performed worldwide. Although islet transplantation is extensively considered an experimental procedure, several countries including Canada, the United Kingdom, France, Switzerland, Norway, Sweden, and other European countries fund the procedure as “non-research” standard clinical care. In the United States, major trials funded by the National Institutes of Health are being conducted to obtain a biological license application (BLA) by the Food and Drug Administration (FDA) (Markmann 2016). Islet transplantation may be performed alone (ITA), in simultaneously with renal transplantation (SIK), or following kidney transplantation (IAK). ITA is the most commonly used approach.
Patient and Graft Survival
The main goal of islet transplantation has historically been insulin independence; however, investigators are currently considering additional relevant outcomes, such as the reduction in the frequency of hypoglycemic episodes and the positive effects on complications and quality of life (Robertson 2010). Since the Edmonton Protocol breakthrough, the endocrine outcomes of islet transplantation have substantially improved, and according to the recent report of the Cell Islet Transplantation Registry, the rate of insulin independence after allogeneic islet infusion (ITA and IAK) is around 66% at 1 year and 44% at 3 years after last infusion (Barton et al. 2012), with 5-year insulin-independent normoglycemia achieved in >50% of patients at the most experienced centers (Bellin et al. 2008, 2012; Vantyghem et al. 2009, 2014a; Maffi et al. 2011; Shapiro et al. 2011). However, multiple infusions are generally required for transplant recipients to achieve insulin independence or to regain insulin independence, as the rate of insulin independence tends to decline over the years. Sixty-four percent of the patients included in the CITR have received more than one islet infusion (Barton et al. 2012). Furthermore, durability of islet graft function, as measured by fasting C-peptide ≥0.3 ng/mL regardless of insulin independence, has been improving significantly over the time, and work from several groups confirms that around 80% of islet-transplanted patients have persistent graft function at 4–5 years after last infusion (Ryan et al. 2005; Barton et al. 2012). Nearly all islet recipients had significant improvements in HbA1c and fasting blood glucose after islet transplantation. Importantly, the presence of insulin-dependent islet graft survival, defined by C-peptide >0.3 ng/mL, is document to protect from severe hypoglycemia (Johnson et al. 2004), and this effect persists even after the islet graft is lost. Available data on severe hypoglycemic events in islet recipients, regardless of graft function, shows that >90% of the patients remained free from severe hypoglycemic events during 5 years of follow-up (Johnson et al. 2004; Barton et al. 2012).
Complication
The procedure of islet transplantation has proven to be very safe, especially when compared with whole-pancreas transplantation (Ryan et al. 2004a; Maffi et al. 2011; Gaba et al. 2012). The incidence of (serious) adverse event related to islet infusions has declined, and the reporting of adverse events has improved over the years. For allogenic islet transplantation bleeding, either intraperitoneal or liver sub capsular is the most common procedure-related complication, occurring with an incidence as high as 13% (Villiger et al. 2005). The exact cause of bleeding in each case is often difficult to determine; however, independent risk factors for hemorrhagic complications include the cumulative number of transplant procedures and heparin dosage of 45 U/kg or more (Villiger et al. 2005). The use of fibrin tissue sealant and embolization coils in the hepatic catheter tract seems to effectively minimize the bleeding risk (Froud et al. 2004; Villiger et al. 2005). Partial portal vein thrombosis complicates fewer than 5% of islet infusion procedures (Ryan et al. 2005), and complete portal venous thrombosis is rare. The use of purer islet preparations, greater expertise in portal vein catheterization, and new radiological devices (catheters medicated with anticoagulation) will continue reducing the risk of portal vein thrombosis, although the risk is unlikely to be completely eliminated. Other complications of islet cell transplantation include transient liver enzyme elevation (50% incidence) (Barshes et al. 2005a), abdominal pain (50% incidence), focal hepatic steatosis (20% incidence) (Bhargava et al. 2004; Maffi et al. 2005), and severe hypoglycemia (<3% incidence). Another complication related to the intrahepatic islet transplantation procedure is portal hypertension that can occur acutely during the islet infusion, especially in the case of infusions other than the first one (Casey et al. 2002).The portal pressure generally normalizes after the acute phase of the procedure. Finally, severe hypoglycemia is a risk associated with the infusion of islets. Iatrogenic hypoglycemia in the immediate posttransplant period is a rare event. Frequent blood glucose monitoring immediately following islet transplantation is recommended to avoid severe unrecognized hypoglycemia in the early posttransplant period. Although islet allotransplantation is a relatively safe procedure, adverse events and serious adverse events are not infrequent. The Eighth Annual Report of the Collaborative Islet Transplant Registry (CITR) reported 1,878 adverse events on 496 out of 864 (57.4%) allograft recipients who underwent islet infusions between 1999 and 2014. The higher than expected incidence of adverse events is in part related to the fact that there is close follow-up of the patients and centers abiding to the strict rules of reporting imposed by the FDA. Moreover, many adverse events seen in this population (30% of recipients) are unrelated to islet transplantation but not unexpected in a cohort of older patients with T1D with significant comorbidity. In any case, many of these events were adjudicated by the investigator as possibly to definitely relate to either the infusion procedure or the immunosuppression. The Eighth Annual Report of the CITR reported that in the first 30 days following islet transplantation, about 31% of recipients experienced a reportable adverse event. Roughly half of these events were adjudicated as possibly or definitely related to either the infusion procedure or the immunosuppression. The vast majority was not unexpected, such as abnormal lymphocyte counts and increased transaminases. About 20% of all recipients experienced a serious adverse event in the first 30 days, which occurred about equally in IAK/SIK as in ITA, and have declined somewhat over the eras. In the first year after islet transplantation, about 48% of all recipients have experienced a reportable adverse event and about one-third have experienced a serious adverse event, with a significant decline in the most recent era. Overall, 16% of all recipients failed to recover completely from an adverse event. The incidence of life-threatening events has declined over time (from 23.9% in 1999–2002 to 3.9% in 2011–2014), and a total of 10.3% of the patients reporting (serious) adverse events in the 2011–2014 period resolved with sequelae. The need to implement antirejection therapy exposes transplant recipients to an increased risk of untoward side effects expected in any immunosuppressed subjects. Opportunistic infections of the urinary tract, upper respiratory tract, and skin are frequent, along with myelosuppressive and gastrointestinal effects of the immunosuppressive drugs. In the majority of the cases, these effects are not severe and resolve without sequelae with medical treatment. Direct organ toxicity of immunosuppressive drugs has been recognized. Symptoms associated with neuro- and/or nephrotoxicity are relatively frequent in subjects receiving chronic immunosuppressive agents currently in use in the clinical arena. In these cases, modification of the antirejection regimen is indicated, with dose reduction or conversion to a different combination of drugs. In the majority of cases, these changes resolve the symptoms without compromising graft survival. The risk of transmission of CMV disease from donor to recipient has been surprisingly low in recipients of islet allografts, particularly in the most recent period with routine use of purified islet preparations (140–144). As with any allogeneic transplant, islet transplant recipients may become sensitized to islet donor histocompatibility antigens (HLA), leading to the development of panel reactive alloantibodies (PRA). Data on the development of cytotoxic antibodies against donor HLA in islet allotransplant recipients with failing grafts have been reported from several islet transplant centers (148–152). A potential consequence of high PRA levels in recipients of a failed islet transplants is that if these individuals develop diabetic nephropathy in the future, a high PRA may increase their time on a transplant list for a suitable kidney graft. Nephrotoxicity from sirolimus and/or tacrolimus has been described in patients with T1D undergoing islet transplantation, particularly when kidney function is already impaired because of preexisting diabetic nephropathy (Andres et al. 2005; Maffi et al. 2007; Gala-Lopez et al. 2011). CITR ITA recipients exhibited a decline in eGFR of 12.4 ± 19.2 ml/min/1.73 m2, and IAK/SIK experienced a mean decline of 0.8 ± 32.3 ml/min/1.73 m2 in 5 years from their first islet infusion, compared to a mean decline of about 9 ml/min/1.73 m2 over the first 5 years in an age-unadjusted cohort of 1,141 patients with T1D followed by the DCCT and then by EDIC. A total of 41 instances of neoplasm have been reported in 32 of 864 islet transplant recipients during about 5,762 person-years of observed follow-up (0.007 neoplasms per person-year, CITR report). There were 21 instances in 17 patients of basal or squamous cell carcinoma of the skin. There were six instances of malignant ovarian cysts, four instances of breast cancer, two instances of lung cancer, two instances of thyroid cancer, and three instances of PTLD. Of the 14 recipients with non-skin cancer, 8 recovered, 2 recovered with sequelae, 5 have not recovered, and 1 died. Among islet allograft recipients, there have been 25 reports of death to the registry, i.e., a 2.4% crude mortality over a mean follow-up of 6.7 years. Causes of death were cardiovascular (n = 5), hemorrhage (n = 3), pneumonia (n = 2), diabetic ketoacidosis (n = 1), infection (n = 1), respiratory arrest (n = 1), acute toxicity (n = 1), pneumopathy (n = 1), multi-organ failure of unknown etiology (n = 1), lung carcinoma (n = 1), and viral meningitis (n = 1).
Immunosuppression
Preexisting and transplant-induced auto- and allo-specific cellular immune responses play a crucial role in the loss of islets and islet function infused in the liver (Campbell et al. 2007; Hilbrands et al. 2009; Piemonti et al. 2013) (Bertuzzi and Ricordi 2007) along with nonspecific immune responses predominantly mediated by innate inflammatory processes related to mechanics and site (Moberg et al. 2002; Matsuoka et al. 2010; Citro et al. 2012, 2013). Islet graft rejection occurs without clinical symptoms. Neither guidelines nor formal consensus on the “best” or “standard” immunosuppressive strategy for human islet transplantation is currently available. Multiple induction and maintenance agents are administered peri- and post-every infusion in the same recipient. According to the Collaborative Islet Transplant Registry (CITR) data (Barton et al. 2012), a substantial shift in immunosuppression strategies has been documented during the last 12 years. The 2000–2006 period was dominated by the Edmonton Protocol, which used an interleukin-2 receptor antagonist (e.g., daclizumab) for induction and a mammalian target of rapamycin (mTOR) inhibitor (e.g., sirolimus), together with a calcineurin inhibitor (CNI, e.g., tacrolimus) for maintenance immunosuppression (Shapiro et al. 2006). In the more recent years, there has been a shift toward the induction with a T-cell-depleting (TCD) antibody, with or without an inhibitor of tumor necrosis factor-α (TNF-α; e.g., etanercept) (Pileggi et al. 2004; Frank et al. 2005; Hering et al. 2005; Marzorati et al. 2007; Alejandro et al. 2008; Bellin et al. 2008; Froud et al. 2008; Gerber et al. 2008; Tan et al. 2008) and maintenance with an mTOR inhibitor or an inosine monophosphate dehydrogenase inhibitor (e.g., mycophenolic acid) combined with a CNI (Shapiro et al. 2000; Froud et al. 2005; Hering et al. 2005; Vantyghem et al. 2009). Moreover, the use of alemtuzumab induction therapy was recently reported and associated with encouraging longer-term function (Shapiro 2011; Nijhoff et al. 2015). New biologic agents with potentially lower islet cell and organ toxicity profiles are currently being evaluated in ongoing clinical trials. Among these are agents that target co-stimulation pathways in immune cells and/or adhesion molecules (CTLA4-Ig, LFA-1 PD-1/PD-L1 CD40) (Badell et al. 2010; Posselt et al. 2010a, b; Turgeon et al. 2010; Fotino and Pileggi 2011; Watanabe et al. 2013; Li et al. 2015) or chemokine receptors (CXCR1/2) (Citro et al. 2012, 2015). Finally, a calcineurin inhibitor-free immunosuppressive regimen was recently reported (Maffi et al. 2014).
Impact of Islet Transplantation on Metabolic Control and Diabetes Complication
Recent clinical trials demonstrated that the effects of islet transplantation on metabolic control are quite reproducible in subjects with unstable type 1 diabetes (Barton et al. 2012). Exogenous insulin requirements needed to attain optimal metabolic control are dramatically reduced immediately after islet transplantation, with a reduction of mean amplitude of glycemic excursions (MAGE) throughout the day and normalization of A1c <6.5% (Shapiro et al. 2000; Froud et al. 2005). Since the main indications for islet transplantation in subjects with type 1 diabetes are unstable control and frequent severe hypoglycemic episodes, the most remarkable effect of the transplant is the abrogation of severe hypoglycemia (Johnson et al. 2004; Poggioli et al. 2006; Leitao et al. 2008; Tharavanij et al. 2008). Using HYPO score and Lability Index to longitudinally assess islet transplant recipients, a significant reduction in the incidence of severe hypoglycemia over a 4-year follow-up period was demonstrated, a finding suggesting that the intervention can support a better and more physiological metabolic control than medical therapy (Ryan et al. 2004b, 2005). It is noteworthy that the prevention of severe hypoglycemia persists long-term and even in subjects requiring exogenous insulin to maintain optimal glycemic control (such as after implantation of a suboptimal islet mass or after development of graft dysfunction) as far as C-peptide is measurable (Pileggi et al. 2004; Alejandro et al. 2008). Following islet transplantation, the restoration of beta-cell responses to secretagogue stimulation is observed, with improved insulin secretion (“first phase”) in response to intravenous glucose, as well as increased C-peptide secretion in response to oral glucose. Normalization of the glycemic threshold triggering the release of counter-regulatory hormones can be demonstrated during hypoglycemic clamp studies, albeit without reaching normalization of the magnitude of the vegetative response. Furthermore, quasi-normal glucagon secretion in response to hypoglycemia can be observed (Paty et al. 2002, 2006; Rickels et al. 2005a, b, 2007). These observations may, at least in part, explain the significant improvement in metabolic control and recovery of hypoglycemia awareness observed after islet transplantation, which persists after development of graft dysfunction and even several months after graft failure (and loss of detectable C-peptide) (Johnson et al. 2004; Barton et al. 2012). Quality of life dramatically improves after islet transplantation. Improvements include greater satisfaction with life and health, more feelings of control and independence, and perceptions of better physical, mental, and social health and function. T1D patients with insulin independence or partial graft function similarly report reduction of hypoglycemic episodes (Radosevich et al. 2013), improvement of symptom awareness, and the rediscovering of reliability and independence (Barshes et al. 2005b; Poggioli et al. 2006; Toso et al. 2007; Cure et al. 2008; Tharavanij et al. 2008; Benhamou et al. 2009). After transplantation of an adequate islet mass obtained from one or more donor pancreata (estimated ≥10.000 islet equivalents (IEq)/kg of recipient’s body weight), insulin independence can be reproducibly achieved. By combining donor selection criteria with improved isolation techniques and adequate immunomodulation of the recipient, insulin independence after single-donor islet preparation is becoming more reproducibly possible to achieve. Islet preparations obtained from more than one donor pancreas can be transplanted at once after pooling them or sequentially based on the metabolic needs of each subject. Data from the Clinical Islet Transplant Registry and independent trial reports have shown that insulin independence at 1 year from completion of the transplant is up to 70% with virtually 100% of the subjects maintaining graft function (C-peptide) if adequately immunosuppressed (Alejandro et al. 2008; Barton et al. 2012). A progressive loss of insulin independence with approximately 90% of subjects requiring reintroduction of exogenous insulin at 5 years (most of them with detectable C-peptide) has been reported in clinical trials based on the “Edmonton Protocol” (induction with anti-IL2R antibody; maintenance with sirolimus and tacrolimus) and some variants of it (Shapiro et al. 2000; Hering et al. 2005; Ryan et al. 2005; Shapiro et al. 2006; Vantyghem et al. 2009). More recent trials using more potent lymphodepletion (i.e., thymoglobulin, anti-CD3, or anti-CD52 antibodies) and/or biologics (anti-IL2R, anti-TNF, anti-LFA-1 antibody or CTLA4Ig) have shown great promise with approximately 50% insulin independence at 5 years after islet transplantation (Bellin et al. 2008, 2012; Vantyghem et al. 2009, 2014a; Maffi et al. 2011; Shapiro 2011), which is comparable to some of the data in whole-pancreas transplantation in subjects with type 1 diabetes (Froud et al. 2008; Tan et al. 2008; Vantyghem et al. 2009; Posselt et al. 2010a, b). In light of the results of the last decade of clinical islet transplant trials, achievement of insulin independence, although desirable, no longer should be considered the main goal of islet transplantation. The sizable improvement of metabolic control in the absence of severe hypoglycemic events, the amelioration of diabetes complications, and the achievement of sustained better quality of life, which are quite cumbersome to reproduce by the means of medical treatment, justify the risks associated with the islet transplant procedure and immunosuppression in this high-risk population of subjects with unstable diabetes. Encouraging results have been reported in recent years on the multiple beneficial effects of islet transplantation on progression of diabetes complications [reviewed in (Bassi and Fiorina 2011)]. Although based on nonrandomized pilot studies, which should be cautiously evaluated, they provide the proof of concept of the importance of restoring beta-cell function in patients with diabetes. In particular, improvement of micro- and macroangiopathy (main causes of diabetic nephropathy) (Fiorina et al. 2003c, 2005b; Toso et al. 2006; Fung et al. 2007; Maffi et al. 2007; Senior et al. 2007; Cure et al. 2008; Gerber et al. 2008; Leitao et al. 2009; Thompson et al. 2011; Gillard et al. 2014) and stabilization/reduced progression of retinopathy (Lee et al. 2005; Venturini et al. 2006; Warnock et al. 2008; Thompson et al. 2011) and neuropathy (Lee et al. 2005; Del Carro et al. 2007; D’Addio et al. 2014; Vantyghem et al. 2014b) have been described. Amelioration of cardiovascular and endothelial dysfunction and reduction of atherothrombotic profile, paralleled by reduced incidence of cardiovascular accidents and higher survival rates, were reported in IAK recipients (Fiorina et al. 2003a, b, c, 2005a, b; Del Carro et al. 2007; Danielson et al. 2013; D’Addio et al. 2014). Furthermore, significantly improved longevity of a renal transplant was observed after islet transplantation (Fiorina et al. 2005b). It is likely that these benefits are the consequence of improved metabolic control conferred by the islet transplant. In addition, a contribution of restored C-peptide secretion and its effects on multiple targets has been proposed (Hansen et al. 2002) .
Current Challenges in Islet Transplantation
While significant progress has been made in the islet transplantation field, several obstacles remain precluding its widespread use. The clinical experience of islet transplantation has been developed almost exclusively using the intrahepatic infusion through the portal vein (Shapiro et al. 2006). It has been suggested that the loss of as many as 50–75% of islets during engraftment is the reason why a very large number of islets are needed to achieve normoglycemia (Cantarelli and Piemonti 2011; Citro et al. 2013). Moreover, two additional important limitations are the currently inadequate immunosuppression for preventing islet rejection (Piemonti et al. 2013) and the limited oxygen supply to the islet in the engraftment site (Barkai et al. 2013; Lo et al. 2013). Current immunosuppressive regimens are capable of preventing islet failure for months to years, but the agents used in these treatments may increase the risk for specific malignancies and opportunistic infections. In addition the most commonly used agents (like calcineurin inhibitors and rapamycin) are also known to impair normal islet function and/or insulin action. Furthermore, like all medications, these agents have other associated toxicities, including the harmful effect of certain widely employed immunosuppressive agents on renal function. The second very significant factor for early and late loss of islet mass is the critical lack of immediate vascularization and chronic hypoxygenation. Physiological supply of oxygen and nutrients in native islets is maintained by a tight capillary network, destroyed by the islet isolation procedure, restricting supply to diffusion from the portal vein and hepatic arterial capillaries until the revascularization process is completed. Oxygen tension in the liver parenchyma decreases from approximately 40 to 5 mmHg, eightfold lower compared to the intrapancreatic levels, leading to severe hypoxia and β-cell death. Revascularization of the islet graft in rodent transplant requires 10–14 days and much longer in nonhuman primates and human recipients. Even after the revascularization of the islets is completed, the capillary’ density is significantly lower compared to the physiological intrapancreatic situation. The proof of concept for cellular replacement therapy in diabetes has been firmly established with islet transplantation. It represents an extremely promising therapy, but it needs to be improved and made more widely available .
Future Developments in Beta-Cell Replacement Therapies
The field of beta-cell replacement has evolved significantly over the last three decades thanks to the incredible efforts of the research community worldwide with continuous improvements in islet manufacturing process and pancreas transplantation techniques, coupled with better patient management and the development of more effective induction and maintenance immunosuppressive protocols. In addition, islet transplantation represents an excellent platform toward the development of cellular therapies aimed at the restoration of β-cell function using alternative sources of β-cells like xenogeneic islets or insulin-producing cells derived from the differentiation of stem cells. While a wide range of improvements may be implemented in the donor selection and organ allocation scheme to increase pancreas utilization for transplantation, there is increasing new excitement for the use of unlimited alternative sources of transplantable islets, such as xenogeneic (i.e., obtained from other species such as porcine islets) [reviewed in (Marigliano et al. 2011)] or derived from human stem cells (Kroon et al. 2008; Schulz et al. 2012; Pagliuca et al. 2014; Rezania et al. 2014). Currently, the most significant advances come from the stem cell field; in fact it has been described that human ESC and iPSC are able to generate pancreatic progenitors and/or functional β-cells in vitro that can treat diabetic mice, and a clinical trial with ESC-derived cells is ongoing in T1D patients. Moreover, the stem cell approach may synergize well with other developing innovations such as the generation of immune isolating and retrievable devices, fundamental to allow cell therapy without immunosuppression and to overcome the safety concerns about tumorigenic cells. It is likely that altogether, these experiences will change the way we treat T1D and lead to new therapeutic options for patients with diabetes.
References
Alejandro R, Barton FB, et al. 2008 Update from the collaborative islet transplant registry. Transplantation. 2008;86(12):1783–8.
Andres A, Toso C, et al. Impairment of renal function after islet transplant alone or islet-after-kidney transplantation using a sirolimus/tacrolimus-based immunosuppressive regimen. Transpl Int. 2005;18(11):1226–30.
Badell IR, Russell MC, et al. LFA-1-specific therapy prolongs allograft survival in rhesus macaques. J Clin Invest. 2010;120(12):4520–31.
Baghurst PA. Calculating the mean amplitude of glycemic excursion from continuous glucose monitoring data: an automated algorithm. Diabetes Technol Ther. 2011;13(3):296–302.
Balamurugan AN, Naziruddin B, et al. Islet product characteristics and factors related to successful human islet transplantation from the collaborative islet transplant registry (CITR) 1999–2010. Am J Transplant. 2014;14(11):2595–606.
Ballinger WF, Lacy PE. Transplantation of intact pancreatic islets in rats. Surgery. 1972;72(2):175–86.
Barkai U, Weir GC, et al. Enhanced oxygen supply improves islet viability in a new bioartificial pancreas. Cell Transplant. 2013;22(8):1463–76.
Barshes NR, Lee TC, et al. Transaminitis after pancreatic islet transplantation. J Am Coll Surg. 2005a;200(3):353–61.
Barshes NR, Vanatta JM, et al. Health-related quality of life after pancreatic islet transplantation: a longitudinal study. Transplantation. 2005b;79(12):1727–30.
Barton FB, Rickels MR, et al. Improvement in outcomes of clinical islet transplantation: 1999–2010. Diabetes Care. 2012;35(7):1436–45.
Bassi R, Fiorina P. Impact of islet transplantation on diabetes complications and quality of life. Curr Diab Rep. 2011;11(5):355–63.
Bazerbachi F, Selzner M, et al. Portal venous versus systemic venous drainage of pancreas grafts: impact on long-term results. Am J Transplant. 2012;12(1):226–32.
Becker BN, Brazy PC, et al. Simultaneous pancreas-kidney transplantation reduces excess mortality in type 1 diabetic patients with end-stage renal disease. Kidney Int. 2000;57(5):2129–35.
Bellin MD, Kandaswamy R, et al. Prolonged insulin independence after islet allotransplants in recipients with type 1 diabetes. Am J Transplant. 2008;8(11):2463–70.
Bellin MD, Barton FB, et al. Potent induction immunotherapy promotes long-term insulin independence after islet transplantation in type 1 diabetes. Am J Transplant. 2012;12(6):1576–83.
Benhamou PY, Milliat-Guittard L, et al. Quality of life after islet transplantation: data from the GRAGIL 1 and 2 trials. Diabet Med. 2009;26(6):617–21.
Bergenstal RM, Tamborlane WV, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 2010;363(4):311–20.
Bergenstal RM, Klonoff DC, et al. Threshold-based insulin-pump interruption for reduction of hypoglycemia. N Engl J Med. 2013;369(3):224–32.
Berney T, Johnson PR. Donor pancreata: evolving approaches to organ allocation for whole pancreas versus islet transplantation. Transplantation. 2010;90(3):238–43.
Bertuzzi F, Ricordi C. Beta-cell replacement in immunosuppressed recipients: old and new clinical indications. Acta Diabetol. 2007;44(4):171–6.
Bertuzzi F, Verzaro R, et al. Brittle type 1 diabetes mellitus. Curr Med Chem. 2007;14(16):1739–44.
Bhargava R, Senior PA, et al. Prevalence of hepatic steatosis after islet transplantation and its relation to graft function. Diabetes. 2004;53(5):1311–7.
Biesenbach G, Konigsrainer A, et al. Progression of macrovascular diseases is reduced in type 1 diabetic patients after more than 5 years successful combined pancreas-kidney transplantation in comparison to kidney transplantation alone. Transpl Int. 2005;18(9):1054–60.
Bode BW, Schwartz S, et al. Glycemic characteristics in continuously monitored patients with type 1 and type 2 diabetes: normative values. Diabetes Care. 2005;28(10):2361–6.
Boggi U, Vistoli F, et al. Results of pancreas transplantation alone with special attention to native kidney function and proteinuria in type 1 diabetes patients. Rev Diabet Stud. 2011;8(2):259–67.
Bonfanti R, Lepore G, et al. Survey on the use of insulin pumps in Italy: comparison between pediatric and adult age groups (IMITA study). Acta Diabetol. 2015;53:403.
Bretzel R, Brendel M, Hering B. International islet transplant registry. Newsletter #9. 2001;8:1.
Campbell PM, Salam A, et al. Pretransplant HLA antibodies are associated with reduced graft survival after clinical islet transplantation. Am J Transplant. 2007;7(5):1242–8.
Campistol JM, de Fijter JW, et al. mTOR inhibitor-associated dermatologic and mucosal problems. Clin Transpl. 2010;24(2):149–56.
Cantarelli E, Piemonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011;11(5):364–74.
Cartwright A, Wallymahmed M, et al. The outcome of brittle type 1 diabetes – a 20 year study. QJM. 2011;104(7):575–9.
Casey JJ, Lakey JR, et al. Portal venous pressure changes after sequential clinical islet transplantation. Transplantation. 2002;74(7):913–5.
Chiang JL, Kirkman MS, et al. Type 1 diabetes through the life span: a position statement of the American diabetes association. Diabetes Care. 2014;37(7):2034–54.
Choudhary P, Geddes J, et al. Frequency of biochemical hypoglycaemia in adults with Type 1 diabetes with and without impaired awareness of hypoglycaemia: no identifiable differences using continuous glucose monitoring. Diabet Med. 2010;27(6):666–72.
Choudhary P, Rickels MR, et al. Evidence-informed clinical practice recommendations for treatment of type 1 diabetes complicated by problematic hypoglycemia. Diabetes Care. 2015;38(6):1016–29.
Citro A, Cantarelli E, et al. CXCR1/2 inhibition enhances pancreatic islet survival after transplantation. J Clin Invest. 2012;122(10):3647–51.
Citro A, Cantarelli E, et al. Anti-inflammatory strategies to enhance islet engraftment and survival. Curr Diab Rep. 2013;13(5):733–44.
Citro A, Cantarelli E, et al. The CXCR1/2 pathway: involvement in diabetes pathophysiology and potential target for T1D interventions. Curr Diab Rep. 2015;15(10):638.
Clarke WL, Cox DJ, et al. Reduced awareness of hypoglycemia in adults with IDDM. A prospective study of hypoglycemic frequency and associated symptoms. Diabetes Care. 1995;18(4):517–22.
Cook K, Sollinger HW, et al. Pancreaticocystostomy: an alternative method for exocrine drainage of segmental pancreatic allografts. Transplantation. 1983;35(6):634–6.
Coppelli A, Giannarelli R, et al. Pancreas transplant alone determines early improvement of cardiovascular risk factors and cardiac function in type 1 diabetic patients. Transplantation. 2003;76(6):974–6.
Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2013;369(4):362–72.
Cure P, Pileggi A, et al. Improved metabolic control and quality of life in seven patients with type 1 diabetes following islet after kidney transplantation. Transplantation. 2008;85(6):801–12.
D’Addio F, Maffi P, et al. Islet transplantation stabilizes hemostatic abnormalities and cerebral metabolism in individuals with type 1 diabetes. Diabetes Care. 2014;37(1):267–76.
Danielson KK, Hatipoglu B, et al. Reduction in carotid intima-media thickness after pancreatic islet transplantation in patients with type 1 diabetes. Diabetes Care. 2013;36(2):450–6.
de Mattos AM, Olyaei AJ, et al. Nephrotoxicity of immunosuppressive drugs: long-term consequences and challenges for the future. Am J Kidney Dis. 2000;35(2):333–46.
Del Carro U, Fiorina P, et al. Evaluation of polyneuropathy markers in type 1 diabetic kidney transplant patients and effects of islet transplantation: neurophysiological and skin biopsy longitudinal analysis. Diabetes Care. 2007;30(12):3063–9.
Dew MA, Switzer GE, et al. Psychosocial assessments and outcomes in organ transplantation. Prog Transplant. 2000;10(4):239–59; quiz 260–231.
Dieterle CD, Arbogast H, et al. Metabolic follow-up after long-term pancreas graft survival. Eur J Endocrinol. 2007;156(5):603–10.
Dubernard JM, Traeger J, et al. A new method of preparation of segmental pancreatic grafts for transplantation: trials in dogs and in man. Surgery. 1978;84(5):633–9.
Fatourechi MM, Kudva YC, et al. Clinical review: hypoglycemia with intensive insulin therapy: a systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. J Clin Endocrinol Metab. 2009;94(3):729–40.
Feldmeyer L, Hofbauer GF, et al. Mammalian target of rapamycin (mTOR) inhibitors slow skin carcinogenesis, but impair wound healing. Br J Dermatol. 2012;166(2):422–4.
Feltbower RG, Bodansky HJ, et al. Acute complications and drug misuse are important causes of death for children and young adults with type 1 diabetes: results from the Yorkshire register of diabetes in children and young adults. Diabetes Care. 2008;31(5):922–6.
Fioretto P, Steffes MW, et al. Reversal of lesions of diabetic nephropathy after pancreas transplantation. N Engl J Med. 1998;339(2):69–75.
Fioretto P, Sutherland DE, et al. Remodeling of renal interstitial and tubular lesions in pancreas transplant recipients. Kidney Int. 2006;69(5):907–12.
Fiorina P, La Rocca E, et al. Reversal of left ventricular diastolic dysfunction after kidney-pancreas transplantation in type 1 diabetic uremic patients. Diabetes Care. 2000;23(12):1804–10.
Fiorina P, Folli F, et al. Long-term beneficial effect of islet transplantation on diabetic macro-/microangiopathy in type 1 diabetic kidney-transplanted patients. Diabetes Care. 2003a;26(4):1129–36.
Fiorina P, Folli F, et al. Islet transplantation improves vascular diabetic complications in patients with diabetes who underwent kidney transplantation: a comparison between kidney-pancreas and kidney-alone transplantation. Transplantation. 2003b;75(8):1296–301.
Fiorina P, Folli F, et al. Islet transplantation is associated with improvement of renal function among uremic patients with type I diabetes mellitus and kidney transplants. J Am Soc Nephrol. 2003c;14(8):2150–8.
Fiorina P, Gremizzi C, et al. Islet transplantation is associated with an improvement of cardiovascular function in type 1 diabetic kidney transplant patients. Diabetes Care. 2005a;28(6):1358–65.
Fiorina P, Venturini M, et al. Natural history of kidney graft survival, hypertrophy, and vascular function in end-stage renal disease type 1 diabetic kidney-transplanted patients: beneficial impact of pancreas and successful islet cotransplantation. Diabetes Care. 2005b;28(6):1303–10.
Fiorina P, Perseghin G, et al. Altered kidney graft high-energy phosphate metabolism in kidney-transplanted end-stage renal disease type 1 diabetic patients: a cross-sectional analysis of the effect of kidney alone and kidney-pancreas transplantation. Diabetes Care. 2007;30(3):597–603.
Fiorina P, Vezzulli P, et al. Near normalization of metabolic and functional features of the central nervous system in type 1 diabetic patients with end-stage renal disease after kidney-pancreas transplantation. Diabetes Care. 2012;35(2):367–74.
Floyd B, Chandra P, et al. Comparative analysis of the efficacy of continuous glucose monitoring and self-monitoring of blood glucose in type 1 diabetes mellitus. J Diabetes Sci Technol. 2012;6(5):1094–102.
Folli F, Guzzi V, et al. Proteomics reveals novel oxidative and glycolytic mechanisms in type 1 diabetic patients’ skin which are normalized by kidney-pancreas transplantation. PLoS One. 2010;5(3):e9923.
Fotino C, Pileggi A. Blockade of leukocyte function antigen-1 (LFA-1) in clinical islet transplantation. Curr Diab Rep. 2011;11(5):337–44.
Franco OH, Steyerberg EW, et al. Associations of diabetes mellitus with total life expectancy and life expectancy with and without cardiovascular disease. Arch Intern Med. 2007;167(11):1145–51.
Frank AM, Barker CF, et al. Comparison of whole organ pancreas and isolated islet transplantation for type 1 diabetes. Adv Surg. 2005;39:137–63.
Freckmann G, Hagenlocher S, et al. Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals. J Diabetes Sci Technol. 2007;1(5):695–703.
Frier BM. Morbidity of hypoglycemia in type 1 diabetes. Diabetes Res Clin Pract. 2004;65(Suppl 1):S47–52.
Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol. 2014;10(12):711–22.
Froud T, Yrizarry JM, et al. Use of D-STAT to prevent bleeding following percutaneous transhepatic intraportal islet transplantation. Cell Transplant. 2004;13(1):55–9.
Froud T, Ricordi C, et al. Islet transplantation in type 1 diabetes mellitus using cultured islets and steroid-free immunosuppression: Miami experience. Am J Transplant. 2005;5(8):2037–46.
Froud T, Baidal DA, et al. Islet transplantation with alemtuzumab induction and calcineurin-free maintenance immunosuppression results in improved short- and long-term outcomes. Transplantation. 2008;86(12):1695–701.
Fung MA, Warnock GL, et al. The effect of medical therapy and islet cell transplantation on diabetic nephropathy: an interim report. Transplantation. 2007;84(1):17–22.
Gaba RC, Garcia-Roca R, et al. Pancreatic islet cell transplantation: an update for interventional radiologists. J Vasc Interv Radiol. 2012;23(5):583–94; quiz 594.
Gaber AO, Oxley D, et al. Changes in gastric emptying in recipients of successful combined pancreas-kidney transplants. Dig Dis. 1991;9(6):437–43.
Gaber AO, el-Gebely S, et al. Early improvement in cardiac function occurs for pancreas-kidney but not diabetic kidney-alone transplant recipients. Transplantation. 1995a;59(8):1105–12.
Gaber AO, Shokouh-Amiri MH, et al. Results of pancreas transplantation with portal venous and enteric drainage. Ann Surg. 1995b;221(6):613–22; discussion 622–614.
Gala-Lopez BL, Senior PA, et al. Late cytomegalovirus transmission and impact of T-depletion in clinical islet transplantation. Am J Transplant. 2011;11(12):2708–14.
Garg S, Zisser H, et al. Improvement in glycemic excursions with a transcutaneous, real-time continuous glucose sensor: a randomized controlled trial. Diabetes Care. 2006;29(1):44–50.
Geddes J, Schopman JE, et al. Prevalence of impaired awareness of hypoglycaemia in adults with type 1 diabetes. Diabet Med. 2008;25(4):501–4.
Geissler EK. Post-transplantation malignancies: here today, gone tomorrow? Nat Rev Clin Oncol. 2015;12(12):705–17.
Gerber PA, Pavlicek V, et al. Simultaneous islet-kidney vs pancreas-kidney transplantation in type 1 diabetes mellitus: a 5 year single centre follow-up. Diabetologia. 2008;51(1):110–9.
Giannarelli R, Coppelli A, et al. Effects of pancreas-kidney transplantation on diabetic retinopathy. Transpl Int. 2005;18(5):619–22.
Giannarelli R, Coppelli A, et al. Pancreas transplant alone has beneficial effects on retinopathy in type 1 diabetic patients. Diabetologia. 2006;49(12):2977–82.
Gill GV. The spectrum of brittle diabetes. J R Soc Med. 1992;85(5):259–61.
Gill GV, Lucas S, et al. Prevalence and characteristics of brittle diabetes in Britain. QJM. 1996;89(11):839–43.
Gillard P, Rustandi M, et al. Early alteration of kidney function in nonuremic type 1 diabetic islet transplant recipients under tacrolimus-mycophenolate therapy. Transplantation. 2014;98:451.
Giorda CB, Ozzello A, et al. Incidence and risk factors for severe and symptomatic hypoglycemia in type 1 diabetes. Results of the HYPOS-1 study. Acta Diabetol. 2015;52(5):845–53.
Girman P, Lipar K, et al. Neoplasm incidence in simultaneous pancreas and kidney transplantation: a single-center analysis. Transplant Proc. 2011;43(9):3288–91.
Gliedman ML, Gold M, et al. Clinical segmental pancreatic transplantation with ureter-pancreatic duct anastomosis for exocrine drainage. Surgery. 1973;74(2):171–80.
Gold AE, MacLeod KM, et al. Frequency of severe hypoglycemia in patients with type I diabetes with impaired awareness of hypoglycemia. Diabetes Care. 1994;17(7):697–703.
Golden SH, Sapir T. Methods for insulin delivery and glucose monitoring in diabetes: summary of a comparative effectiveness review. J Manag Care Pharm. 2012;18(6 Suppl):S1–17.
Graveling AJ, Frier BM. Impaired awareness of hypoglycaemia: a review. Diabetes Metab. 2010;36(Suppl 3):S64–74.
Gregg EW, Li Y, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23.
Gross CR, Zehrer CL. Health-related quality of life outcomes of pancreas transplant recipients. Clin Transpl. 1992;6(3 part 1):165–71.
Gruden G, Barutta F, et al. Severe hypoglycemia and cardiovascular disease incidence in type 1 diabetes: the EURODIAB prospective complications study. Diabetes Care. 2012;35(7):1598–604.
Gruessner AC. 2011 update on pancreas transplantation: comprehensive trend analysis of 25,000 cases followed up over the course of twenty-four years at the international pancreas transplant registry (IPTR). Rev Diabet Stud. 2011;8(1):6–16.
Gruessner AC, Gruessner RW. Pancreas transplant outcomes for United States and non United States cases as reported to the united network for organ sharing and the international pancreas transplant registry as of December 2011. Clin Transpl. 2012:23–40. PMID: 23721008.
Gruessner RW, Gruessner AC. The current state of pancreas transplantation. Nat Rev Endocrinol. 2013a;9(9):555–62.
Gruessner RW, Gruessner AC. Pancreas transplant alone: a procedure coming of age. Diabetes Care. 2013b;36(8):2440–7.
Gruessner AC, Gruessner RW. Declining numbers of pancreas transplantations but significant improvements in outcome. Transplant Proc. 2014;46(6):1936–7.
Gruessner AC, Sutherland DE. Pancreas transplant outcomes for United States (US) cases reported to the united network for organ sharing (UNOS) and non-US cases reported to the international pancreas transplant registry (IPTR) as of October, 2000. Clin Transpl. 2000:45–72. PMID: 11512358.
Gruessner RW, Sutherland DE, et al. Mortality assessment for pancreas transplants. Am J Transplant. 2004;4(12):2018–26.
Han DJ, Sutherland DE. Pancreas transplantation. Gut Liver. 2010;4(4):450–65.
Hansen A, Johansson BL, et al. C-peptide exerts beneficial effects on myocardial blood flow and function in patients with type 1 diabetes. Diabetes. 2002;51(10):3077–82.
Hao WJ, Zong HT, et al. The efficacy and safety of alemtuzumab and daclizumab versus antithymocyte globulin during organ transplantation: a meta-analysis. Transplant Proc. 2012;44(10):2955–60.
Hasskarl J. Everolimus. Recent Results Cancer Res. 2014;201:373–92.
Helfrich M, Ison MG. Opportunistic infections complicating solid organ transplantation with alemtuzumab induction. Transpl Infect Dis. 2015;17(5):627–36.
Hering BJ, Bretzel RG, et al. New protocol toward prevention of early human islet allograft failure. Transplant Proc. 1994;26(2):570–1.
Hering BJ, Kandaswamy R, et al. Single-donor, marginal-dose islet transplantation in patients with type 1 diabetes. JAMA. 2005;293(7):830–5.
Hilbrands R, Huurman VA, et al. Differences in baseline lymphocyte counts and autoreactivity are associated with differences in outcome of islet cell transplantation in type 1 diabetic patients. Diabetes. 2009;58(10):2267–76.
Hoi-Hansen T, Pedersen-Bjergaard U, et al. Classification of hypoglycemia awareness in people with type 1 diabetes in clinical practice. J Diabetes Complicat. 2010;24(6):392–7.
Hopkins D, Lawrence I, et al. Improved biomedical and psychological outcomes 1 year after structured education in flexible insulin therapy for people with type 1 diabetes: the U.K. DAFNE experience. Diabetes Care. 2012;35(8):1638–42.
Hu FB, Stampfer MJ, et al. The impact of diabetes mellitus on mortality from all causes and coronary heart disease in women: 20 years of follow-up. Arch Intern Med. 2001;161(14):1717–23.
Isla Pera P, Moncho Vasallo J, et al. Quality of life in simultaneous pancreas-kidney transplant recipients. Clin Transpl. 2009;23(5):600–5.
Jahansouz C, Kumer SC, et al. Evolution of beta-cell replacement therapy in diabetes mellitus: pancreas transplantation. Diabetes Technol Ther. 2011;13(3):395–418.
Johnson PR, Jones KE. Pancreatic islet transplantation. Semin Pediatr Surg. 2012;21(3):272–80. https://doi.org/10.1053/j.sempedsurg.2012.05.012. PMID: 22800980 [Indexed for MEDLINE]
Johnson JA, Kotovych M, et al. Reduced fear of hypoglycemia in successful islet transplantation. Diabetes Care. 2004;27(2):624–5.
Johnston O, Rose CL, et al. Sirolimus is associated with new-onset diabetes in kidney transplant recipients. J Am Soc Nephrol. 2008;19(7):1411–8.
Jukema JW, Smets YF, et al. Impact of simultaneous pancreas and kidney transplantation on progression of coronary atherosclerosis in patients with end-stage renal failure due to type 1 diabetes. Diabetes Care. 2002;25(5):906–11.
Kandaswamy R, Skeans MA, et al. OPTN/SRTR 2013 annual data report: pancreas. Am J Transplant. 2015;15(Suppl 2):1–20.
Kandaswamy R, Skeans MA, et al. Pancreas. Am J Transplant. 2016;16(Suppl 2):47–68.
Kelly WD, Lillehei RC, et al. Allotransplantation of the pancreas and duodenum along with the kidney in diabetic nephropathy. Surgery. 1967;61(6):827–37.
Kennedy WR, Navarro X, et al. Effects of pancreatic transplantation on diabetic neuropathy. N Engl J Med. 1990;322(15):1031–7.
Kent LA, Gill GV, et al. Mortality and outcome of patients with brittle diabetes and recurrent ketoacidosis. Lancet. 1994;344(8925):778–81.
Kleinclauss F, Fauda M, et al. Pancreas after living donor kidney transplants in diabetic patients: impact on long-term kidney graft function. Clin Transpl. 2009;23(4):437–46.
Kovatchev BP, Cox DJ, et al. Assessment of risk for severe hypoglycemia among adults with IDDM: validation of the low blood glucose index. Diabetes Care. 1998;21(11):1870–5.
Koznarova R, Saudek F, et al. Beneficial effect of pancreas and kidney transplantation on advanced diabetic retinopathy. Cell Transplant. 2000;9(6):903–8.
Kroon E, Martinson LA, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–52.
La Rocca E, Minicucci F, et al. Evolution of carotid vascular lesions in kidney-pancreas and kidney-alone transplanted insulin-dependent diabetic patients. Transplant Proc. 1995;27(6):3072.
La Rocca E, Fiorina P, et al. Cardiovascular outcomes after kidney-pancreas and kidney-alone transplantation. Kidney Int. 2001;60(5):1964–71.
Larsen JL, Ratanasuwan T, et al. Carotid intima media thickness decreases after pancreas transplantation. Transplantation. 2002;73(6):936–40.
Larsen JL, Colling CW, et al. Pancreas transplantation improves vascular disease in patients with type 1 diabetes. Diabetes Care. 2004;27(7):1706–11.
Larsen CP, Pearson TC, et al. Rational development of LEA29Y (belatacept), a high-affinity variant of CTLA4-Ig with potent immunosuppressive properties. Am J Transplant. 2005;5(3):443–53.
Lee TC, Barshes NR, et al. The effect of pancreatic islet transplantation on progression of diabetic retinopathy and neuropathy. Transplant Proc. 2005;37(5):2263–5.
Lehmann R, Graziano J, et al. Glycemic control in simultaneous islet-kidney versus pancreas-kidney transplantation in type 1 diabetes: a prospective 13-year follow-up. Diabetes Care. 2015;38(5):752–9.
Leitao CB, Tharavanij T, et al. Restoration of hypoglycemia awareness after islet transplantation. Diabetes Care. 2008;31(11):2113–5.
Leitao CB, Cure P, et al. Stable renal function after islet transplantation: importance of patient selection and aggressive clinical management. Transplantation. 2009;87(5):681–8.
Letavernier E, Legendre C. mToR inhibitors-induced proteinuria: mechanisms, significance, and management. Transplant Rev (Orlando). 2008;22(2):125–30.
Li T, Ma R, et al. PD-1/PD-L1 costimulatory pathway-induced mouse islet transplantation immune tolerance. Transplant Proc. 2015;47(1):165–70.
Lind M, Svensson AM, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014;371(21):1972–82.
Livingstone SJ, Levin D, et al. Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008–2010. JAMA. 2015;313(1):37–44.
Lo JF, Wang Y, et al. Quantitative and temporal control of oxygen microenvironment at the single islet level. J Vis Exp. 2013;(81):e50616. https://doi.org/10.3791/50616.
Maahs DM, Calhoun P, et al. A randomized trial of a home system to reduce nocturnal hypoglycemia in type 1 diabetes. Diabetes Care. 2014;37(7):1885–91.
Maffi P, Angeli E, et al. Minimal focal steatosis of liver after islet transplantation in humans: a long-term study. Cell Transplant. 2005;14(10):727–33.
Maffi P, Bertuzzi F, et al. Kidney function after islet transplant alone in type 1 diabetes: impact of immunosuppressive therapy on progression of diabetic nephropathy. Diabetes Care. 2007;30(5):1150–5.
Maffi P, Scavini M, et al. Risks and benefits of transplantation in the cure of type 1 diabetes: whole pancreas versus islet transplantation. A single center study. Rev Diabet Stud. 2011;8(1):44–50.
Maffi P, Berney T, et al. Calcineurin inhibitor-free immunosuppressive regimen in type 1 diabetes patients receiving islet transplantation: single-group phase 1/2 trial. Transplantation. 2014;98(12):1301–9.
Mannucci E, Monami M, et al. Achieving HbA1c targets in clinical trials and in the real world: a systematic review and meta-analysis. J Endocrinol Investig. 2014;37(5):477–95.
Marigliano M, Bertera S, et al. Pig-to-nonhuman primates pancreatic islet xenotransplantation: an overview. Curr Diab Rep. 2011;11(5):402–12.
Markmann JF. Isolated pancreatic islet transplantation: a coming of age. Am J Transplant. 2016;16(2):381–2.
Martinenghi S, Comi G, et al. Amelioration of nerve conduction velocity following simultaneous kidney/pancreas transplantation is due to the glycaemic control provided by the pancreas. Diabetologia. 1997;40(9):1110–2.
Marzorati S, Pileggi A, et al. Allogeneic islet transplantation. Expert Opin Biol Ther. 2007;7(11):1627–45.
Matsuoka N, Itoh T, et al. High-mobility group box 1 is involved in the initial events of early loss of transplanted islets in mice. J Clin Invest. 2010;120(3):735–43.
McAlister VC, Gao Z, et al. Sirolimus-tacrolimus combination immunosuppression. Lancet. 2000;355(9201):376–7.
McCoy RG, Van Houten HK, et al. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care. 2012;35(9):1897–901.
McDonnell CM, Donath SM, et al. A novel approach to continuous glucose analysis utilizing glycemic variation. Diabetes Technol Ther. 2005;7(2):253–63.
McKnight JA, Wild SH, et al. Glycaemic control of type 1 diabetes in clinical practice early in the 21st century: an international comparison. Diabet Med. 2015;32(8):1036–50.
Merkel FK, Ryan WG, et al. Pancreatic transplantation for diabetes mellitus. IMJ Ill Med J. 1973;144(5):477–9 passim.
Miller KM, Foster NC, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D exchange clinic registry. Diabetes Care. 2015;38(6):971–8.
Mittal S, Gough SC. Pancreas transplantation: a treatment option for people with diabetes. Diabet Med. 2014;31(5):512–21.
Mittal S, Johnson P, et al. Pancreas transplantation: solid organ and islet. Cold Spring Harb Perspect Med. 2014;4(4):a015610.
Moassesfar S, Masharani U, et al. A comparative analysis of the safety, efficacy, and cost of islet versus pancreas transplantation in nonuremic patients with type 1 diabetes. Am J Transplant. 2016;16(2):518–26.
Moberg L, Johansson H, et al. Production of tissue factor by pancreatic islet cells as a trigger of detrimental thrombotic reactions in clinical islet transplantation. Lancet. 2002;360(9350):2039–45.
Mohan P, Safi K, et al. Improved patient survival in recipients of simultaneous pancreas-kidney transplant compared with kidney transplant alone in patients with type 1 diabetes mellitus and end-stage renal disease. Br J Surg. 2003;90(9):1137–41.
Morath C, Zeier M, et al. Metabolic control improves long-term renal allograft and patient survival in type 1 diabetes. J Am Soc Nephrol. 2008;19(8):1557–63.
Morrissey PE, Shaffer D, et al. Peripheral vascular disease after kidney-pancreas transplantation in diabetic patients with end-stage renal disease. Arch Surg. 1997;132(4):358–61; discussion 361–352.
Mujtaba MA, Sharfuddin AA, et al. Conversion from tacrolimus to belatacept to prevent the progression of chronic kidney disease in pancreas transplantation: case report of two patients. Am J Transplant. 2014;14(11):2657–61.
Nakache R, Tyden G, et al. Long-term quality of life in diabetic patients after combined pancreas-kidney transplantation or kidney transplantation. Transplant Proc. 1994;26(2):510–1.
Nano R, Clissi B, et al. Islet isolation for allotransplantation: variables associated with successful islet yield and graft function. Diabetologia. 2005;48(5):906–12.
Nath DS, Gruessner A, et al. Late anastomotic leaks in pancreas transplant recipients – clinical characteristics and predisposing factors. Clin Transpl. 2005;19(2):220–4.
Navarro X, Sutherland DE, et al. Long-term effects of pancreatic transplantation on diabetic neuropathy. Ann Neurol. 1997;42(5):727–36.
Nghiem DD, Corry RJ. Technique of simultaneous renal pancreatoduodenal transplantation with urinary drainage of pancreatic secretion. Am J Surg. 1987;153(4):405–6.
Nijhoff MF, Engelse MA, et al. Glycemic stability through islet-after-kidney transplantation using an Alemtuzumab-based induction regimen and long-term triple-maintenance immunosuppression. Am J Transplant. 2015;16:246.
Norman SP, Kommareddi M, et al. Early pancreas graft failure is associated with inferior late clinical outcomes after simultaneous kidney-pancreas transplantation. Transplantation. 2011;92(7):796–801.
Ogundipe OO, Geddes J, et al. Impaired hypoglycaemia awareness and employment in people with type 1 diabetes. Occup Med (Lond). 2011;61(4):241–6.
Ojo AO, Meier-Kriesche HU, et al. The impact of simultaneous pancreas-kidney transplantation on long-term patient survival. Transplantation. 2001;71(1):82–90.
Olsen SE, Asvold BO, et al. Hypoglycaemia symptoms and impaired awareness of hypoglycaemia in adults with type 1 diabetes: the association with diabetes duration. Diabet Med. 2014;31(10):1210–7.
Pagliuca FW, Millman JR, et al. Generation of functional human pancreatic beta cells in vitro. Cell. 2014;159(2):428–39.
Paty BW, Ryan EA, et al. Intrahepatic islet transplantation in type 1 diabetic patients does not restore hypoglycemic hormonal counterregulation or symptom recognition after insulin independence. Diabetes. 2002;51(12):3428–34.
Paty BW, Senior PA, et al. Assessment of glycemic control after islet transplantation using the continuous glucose monitor in insulin-independent versus insulin-requiring type 1 diabetes subjects. Diabetes Technol Ther. 2006;8(2):165–73.
Pedersen-Bjergaard U, Pramming S, et al. Recall of severe hypoglycaemia and self-estimated state of awareness in type 1 diabetes. Diabetes Metab Res Rev. 2003;19(3):232–40.
Pedersen-Bjergaard U, Pramming S, et al. Severe hypoglycaemia in 1076 adult patients with type 1 diabetes: influence of risk markers and selection. Diabetes Metab Res Rev. 2004;20(6):479–86.
Phillip M, Battelino T, et al. Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med. 2013;368(9):824–33.
Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in type 1 diabetes: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med. 2008;25(7):765–74.
Piemonti L, Pileggi A. 25 years of the Ricordi automated method for islet isolation. CellR4. 2013;1(1):e128.
Piemonti L, Everly MJ, et al. Alloantibody and autoantibody monitoring predicts islet transplantation outcome in human type 1 diabetes. Diabetes. 2013;62(5):1656–64.
Pileggi A, Ricordi C, et al. Twenty years of clinical islet transplantation at the Diabetes Research Institute – University of Miami. Clin Transpl. 2004:177–204.
Poggioli R, Faradji RN, et al. Quality of life after islet transplantation. Am J Transplant. 2006;6(2):371–8.
Port FK, Wolfe RA, et al. Comparison of survival probabilities for dialysis patients vs cadaveric renal transplant recipients. JAMA. 1993;270(11):1339–43.
Posselt AM, Bellin MD, et al. Islet transplantation in type 1 diabetics using an immunosuppressive protocol based on the anti-LFA-1 antibody efalizumab. Am J Transplant. 2010a;10(8):1870–80.
Posselt AM, Szot GL, et al. Islet transplantation in type 1 diabetic patients using calcineurin inhibitor-free immunosuppressive protocols based on T-cell adhesion or costimulation blockade. Transplantation. 2010b;90(12):1595–601.
Pozza G, Traeger J, et al. Endocrine responses of type 1 (insulin-dependent) diabetic patients following successful pancreas transplantation. Diabetologia. 1983;24(4):244–8.
Prieto M, Sutherland DE, et al. Pancreas transplant results according to the technique of duct management: bladder versus enteric drainage. Surgery. 1987;102(4):680–91.
Radosevich DM, Jevne R, et al. Comprehensive health assessment and five-yr follow-up of allogeneic islet transplant recipients. Clin Transpl. 2013;27(6):E715–24.
Ramsay RC, Goetz FC, et al. Progression of diabetic retinopathy after pancreas transplantation for insulin-dependent diabetes mellitus. N Engl J Med. 1988;318(4):208–14.
Rana A, Gruessner A, et al. Survival benefit of solid-organ transplant in the United States. JAMA Surg. 2015;150(3):252–9.
Rangel EB. Tacrolimus in pancreas transplant: a focus on toxicity, diabetogenic effect and drug-drug interactions. Expert Opin Drug Metab Toxicol. 2014;10(11):1585–605.
Rayhill SC, D’Alessandro AM, et al. Simultaneous pancreas-kidney transplantation and living related donor renal transplantation in patients with diabetes: is there a difference in survival? Ann Surg. 2000;231(3):417–23.
Reddy KS, Stablein D, et al. Long-term survival following simultaneous kidney-pancreas transplantation versus kidney transplantation alone in patients with type 1 diabetes mellitus and renal failure. Am J Kidney Dis. 2003;41(2):464–70.
Rezania A, Bruin JE, et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat Biotechnol. 2014;32(11):1121–33.
Rickels MR. Recovery of endocrine function after islet and pancreas transplantation. Curr Diab Rep. 2012;12(5):587–96.
Rickels MR, Schutta MH, et al. {beta}-cell function following human islet transplantation for type 1 diabetes. Diabetes. 2005a;54(1):100–6.
Rickels MR, Schutta MH, et al. Islet cell hormonal responses to hypoglycemia after human islet transplantation for type 1 diabetes. Diabetes. 2005b;54(11):3205–11.
Rickels MR, Naji A, et al. Acute insulin responses to glucose and arginine as predictors of beta-cell secretory capacity in human islet transplantation. Transplantation. 2007;84(10):1357–60.
Ricordi C. Islet transplantation: a brave new world. Diabetes. 2003;52(7):1595–603.
Ricordi C, Lacy PE, et al. Automated method for isolation of human pancreatic islets. Diabetes. 1988;37(4):413–20.
Ricordi C, Socci C, et al. Isolation of the elusive pig islet. Surgery. 1990;107(6):688–94.
Ricordi C, Tzakis AG, et al. Human islet isolation and allotransplantation in 22 consecutive cases. Transplantation. 1992;53(2):407–14.
Robertson RP. Islet transplantation a decade later and strategies for filling a half-full glass. Diabetes. 2010;59(6):1285–91.
Robertson P, Davis C, et al. Pancreas transplantation in type 1 diabetes. Diabetes Care. 2004;27(Suppl 1):S105.
Robertson RP, Davis C, et al. Pancreas and islet transplantation in type 1 diabetes. Diabetes Care. 2006;29(4):935.
Rosenlof LK, Earnhardt RC, et al. Pancreas transplantation. An initial experience with systemic and portal drainage of pancreatic allografts. Ann Surg. 1992;215(6):586–95; discussion 596–587.
Ross PL, Milburn J, et al. Clinical review: insulin pump-associated adverse events in adults and children. Acta Diabetol. 2015;52(6):1017–24.
Rostambeigi N, Kudva YC, et al. Epidemiology of infections requiring hospitalization during long-term follow-up of pancreas transplantation. Transplantation. 2010;89(9):1126–33.
Russell SJ, El-Khatib FH, et al. Outpatient glycemic control with a bionic pancreas in type 1 diabetes. N Engl J Med. 2014;371(4):313–25.
Ryan EA, Paty BW, et al. Risks and side effects of islet transplantation. Curr Diab Rep. 2004a;4(4):304–9.
Ryan EA, Shandro T, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes. 2004b;53(4):955–62.
Ryan EA, Paty BW, et al. Five-year follow-up after clinical islet transplantation. Diabetes. 2005;54(7):2060–9.
Salonia A, D’Addio F, et al. Kidney-pancreas transplantation is associated with near-normal sexual function in uremic type 1 diabetic patients. Transplantation. 2011;92(7):802–8.
Salvalaggio PR, Dzebisashvili N, et al. Incremental value of the pancreas allograft to the survival of simultaneous pancreas-kidney transplant recipients. Diabetes Care. 2009;32(4):600–2.
Scharp DW, Lacy PE, et al. Insulin independence after islet transplantation into type I diabetic patient. Diabetes. 1990;39(4):515–8.
Schmidt S, Norgaard K. Bolus calculators. J Diabetes Sci Technol. 2014;8(5):1035–41.
Schulz TC, Young HY, et al. A scalable system for production of functional pancreatic progenitors from human embryonic stem cells. PLoS One. 2012;7(5):e37004.
Seaquist ER, Anderson J, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36(5):1384–95.
Secchi A, Socci C, et al. Islet transplantation in IDDM patients. Diabetologia. 1997;40(2):225–31.
Senior PA, Zeman M, et al. Changes in renal function after clinical islet transplantation: four-year observational study. Am J Transplant. 2007;7(1):91–8.
Shapiro AM. Strategies toward single-donor islets of Langerhans transplantation. Curr Opin Organ Transplant. 2011;16(6):627–31.
Shapiro AM. Islet transplantation in type 1 diabetes: ongoing challenges, refined procedures, and long-term outcome. Rev Diabet Stud. 2012;9(4):385–406.
Shapiro AM, Lakey JR, et al. Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med. 2000;343(4):230–8.
Shapiro AM, Ricordi C, et al. Edmonton’s islet success has indeed been replicated elsewhere. Lancet. 2003;362(9391):1242.
Shapiro AM, Ricordi C, et al. International trial of the Edmonton protocol for islet transplantation. N Engl J Med. 2006;355(13):1318–30.
Shapiro AT, C, Imes S, Koh A, Kin T, O’Gorman D, Malcolm A, Dinyari P, Owen R, Kneteman RN, Bigam DL, Calne RY, Senior PA, Roep BO. Five-year results of islet-alone transplantation match pancreas-alone transplantation with Alemtuzumab, Tac/MMF, with strong suppression of auto and alloreactivity. In: 13th world congress of the international pancreas and islet transplant association (IPITA), Prague; 2011.
Siskind E, Maloney C, et al. An analysis of pancreas transplantation outcomes based on age groupings – an update of the UNOS database. Clin Transpl. 2014;28(9):990–4.
Skrivarhaug T, Bangstad HJ, et al. Long-term mortality in a nationwide cohort of childhood-onset type 1 diabetic patients in Norway. Diabetologia. 2006;49(2):298–305.
Smets YF, Westendorp RG, et al. Effect of simultaneous pancreas-kidney transplantation on mortality of patients with type-1 diabetes mellitus and end-stage renal failure. Lancet. 1999;353(9168):1915–9.
Smith GC, Trauer T, et al. Prospective quality-of-life monitoring of simultaneous pancreas and kidney transplant recipients using the 36-item short form health survey. Am J Kidney Dis. 2010;55(4):698–707.
Socci C, Falqui L, et al. Fresh human islet transplantation to replace pancreatic endocrine function in type 1 diabetic patients. Report of six cases. Acta Diabetol. 1991;28(2):151–7.
Sollinger HW, Odorico JS, et al. One thousand simultaneous pancreas-kidney transplants at a single center with 22-year follow-up. Ann Surg. 2009;250(4):618–30.
Speight J, Reaney MD, et al. Patient-reported outcomes following islet cell or pancreas transplantation (alone or after kidney) in type 1 diabetes: a systematic review. Diabet Med. 2010;27(7):812–22.
Stadler M, Anderwald C, et al. Chronic peripheral hyperinsulinemia in type 1 diabetic patients after successful combined pancreas-kidney transplantation does not affect ectopic lipid accumulation in skeletal muscle and liver. Diabetes. 2010;59(1):215–8.
Starzl TE, Iwatsuki S, et al. Pancreaticoduodenal transplantation in humans. Surg Gynecol Obstet. 1984;159(3):265–72.
Stratta RJ. Cardiovascular disease and neoplasms after pancreas transplantation. Lancet. 1998;352(9121):65–6.
Stratta RJ. Surgical nuances in pancreas transplantation. Transplant Proc. 2005;37(2):1291–3.
Sutherland DE, Goetz FC, et al. Living-related donor segmental pancreatectomy for transplantation. Transplant Proc. 1980;12(4 Suppl 2):19–25.
Sutherland DE, Gruessner RW, et al. Lessons learned from more than 1,000 pancreas transplants at a single institution. Ann Surg. 2001;233(4):463–501.
Tan J, Yang S, et al. Simultaneous islet and kidney transplantation in seven patients with type 1 diabetes and end-stage renal disease using a glucocorticoid-free immunosuppressive regimen with alemtuzumab induction. Diabetes. 2008;57(10):2666–71.
Tangri N, Grams ME, et al. Multinational assessment of accuracy of equations for predicting risk of kidney failure: a meta-analysis. JAMA. 2016;315(2):164–74.
Tattersall RB. Brittle diabetes revisited: the third Arnold Bloom memorial lecture. Diabet Med. 1997;14(2):99–110.
Tattersall R, Gregory R, et al. Course of brittle diabetes: 12 year follow up. BMJ. 1991;302(6787):1240–3.
Tharavanij T, Betancourt A, et al. Improved long-term health-related quality of life after islet transplantation. Transplantation. 2008;86(9):1161–7.
Thompson DM, Meloche M, et al. Reduced progression of diabetic microvascular complications with islet cell transplantation compared with intensive medical therapy. Transplantation. 2011;91(3):373–8.
Toso C, Baertschiger R, et al. Sequential kidney/islet transplantation: efficacy and safety assessment of a steroid-free immunosuppression protocol. Am J Transplant. 2006;6(5 Pt 1):1049–58.
Toso C, Shapiro AM, et al. Quality of life after islet transplant: impact of the number of islet infusions and metabolic outcome. Transplantation. 2007;84(5):664–6.
Turgeon NA, Avila JG, et al. Experience with a novel efalizumab-based immunosuppressive regimen to facilitate single donor islet cell transplantation. Am J Transplant. 2010;10(9):2082–91.
Tyden G, Bolinder J, et al. Improved survival in patients with insulin-dependent diabetes mellitus and end-stage diabetic nephropathy 10 years after combined pancreas and kidney transplantation. Transplantation. 1999;67(5):645–8.
Tzakis AG, Ricordi C, et al. Pancreatic islet transplantation after upper abdominal exenteration and liver replacement. Lancet. 1990;336(8712):402–5.
UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50(6):1140–7.
van Dellen D, Worthington J, et al. Mortality in diabetes: pancreas transplantation is associated with significant survival benefit. Nephrol Dial Transplant. 2013;28(5):1315–22.
Vantyghem MC, Press M. Management strategies for brittle diabetes. Ann Endocrinol (Paris). 2006;67(4):287–96.
Vantyghem MC, Kerr-Conte J, et al. Primary graft function, metabolic control, and graft survival after islet transplantation. Diabetes Care. 2009;32(8):1473–8.
Vantyghem MC, Defrance F, et al. Treating diabetes with islet transplantation: lessons from the past decade in Lille. Diabetes Metab. 2014a;40(2):108–19.
Vantyghem MC, Quintin D, et al. Improvement of electrophysiological neuropathy after islet transplantation for type 1 diabetes: a 5-year prospective study. Diabetes Care. 2014b;37(6):e141–2.
Venstrom JM, McBride MA, et al. Survival after pancreas transplantation in patients with diabetes and preserved kidney function. JAMA. 2003;290(21):2817–23.
Venturini M, Fiorina P, et al. Early increase of retinal arterial and venous blood flow velocities at color Doppler imaging in brittle type 1 diabetes after islet transplant alone. Transplantation. 2006;81(9):1274–7.
Vigersky RA. The benefits, limitations, and cost-effectiveness of advanced technologies in the management of patients with diabetes mellitus. J Diabetes Sci Technol. 2015;9(2):320–30.
Villiger P, Ryan EA, et al. Prevention of bleeding after islet transplantation: lessons learned from a multivariate analysis of 132 cases at a single institution. Am J Transplant. 2005;5(12):2992–8.
Vizzardelli C, Potter ED, et al. Automated method for isolation of adrenal medullary chromaffin cells from neonatal porcine glands. Cell Transplant. 2001;10(8):689–96.
Voulgari C, Tentolouris N. Brittle diabetes: a contemporary review of the myth and its realization. In: Rigobelo EC, editor. Diabetes – damages and treatments. In: Everlon Cid Rigobelo. Tech; 2011, Janeza Trdine 9, 51000 Rijeka, Croatia. Chapters.
Voulgari C, Pagoni S, et al. ‘Brittleness’ in diabetes: easier spoken than broken. Diabetes Technol Ther. 2012;14(9):835–48.
Warnock GL, Kneteman NM, et al. Normoglycaemia after transplantation of freshly isolated and cryopreserved pancreatic islets in type 1 (insulin-dependent) diabetes mellitus. Diabetologia. 1991;34(1):55–8.
Warnock GL, Thompson DM, et al. A multi-year analysis of islet transplantation compared with intensive medical therapy on progression of complications in type 1 diabetes. Transplantation. 2008;86(12):1762–6.
Watanabe M, Yamashita K, et al. ASKP1240, a fully human anti-CD40 monoclonal antibody, prolongs pancreatic islet allograft survival in nonhuman primates. Am J Transplant. 2013;13(8):1976–88.
Weinstock RS, Xing D, et al. Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange clinic registry. J Clin Endocrinol Metab. 2013;98(8):3411–9.
Weiss AS, Smits G, et al. Twelve-month pancreas graft function significantly influences survival following simultaneous pancreas-kidney transplantation. Clin J Am Soc Nephrol. 2009;4(5):988–95.
White SA, Shaw JA, et al. Pancreas transplantation. Lancet. 2009;373(9677):1808–17.
Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28(5):1245–9.
Ziaja J, Bozek-Pajak D, et al. Impact of pancreas transplantation on the quality of life of diabetic renal transplant recipients. Transplant Proc. 2009;41(8):3156–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this entry
Cite this entry
Piemonti, L., Socci, C., Nano, R., Maffi, P., Secchi, A. (2018). Islet Cell or Pancreas Transplantation. In: Bonora, E., DeFronzo, R. (eds) Diabetes Epidemiology, Genetics, Pathogenesis, Diagnosis, Prevention, and Treatment . Endocrinology. Springer, Cham. https://doi.org/10.1007/978-3-319-45015-5_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-45015-5_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-45014-8
Online ISBN: 978-3-319-45015-5
eBook Packages: MedicineReference Module Medicine