Abstract
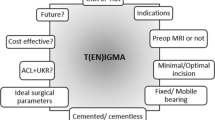
Minimally invasive (MIS) unicondylar knee arthroplasty (UKA) and total knee arthroplasty (TKA) each have specific indications and distinctive roles in the senior author’s algorithm for the treatment of knee osteoarthritis (OA). MIS UKA is not a substitute for TKA, which is the procedure of choice for treatment of advanced stages of OA. This philosophy is supported by Thornhill and Scott, who assert that UKA should be considered in the “continuum of surgical options for the treatment of the osteoarthritic patient” [1]. In cases of earlier, nonadvanced OA, the two procedures may act in conjunction with one another, with MIS UKA serving as a supplement to future TKA. Together, these devices may be considered as a “knee prosthetic system” [2].
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Knee prosthetic system
- Minimally invasive unicondylar knee arthroplasty (MIS UKA) program
- Ahlback classification
- Minimally invasive unicondylar knee arthroplasty (MIS UKA)
- Minimally invasive bone-sparing UKA technique
- Medial parapatellar capsular arthrotomy
- Medial unicompartmental osteoarthritis
- Repicci II unicondylar knee system
- Standard medial parapatellar approach
Minimally invasive (MIS) unicondylar knee arthroplasty (UKA) and total knee arthroplasty (TKA) each have specific indications and distinctive roles in the senior author’s algorithm for the treatment of knee osteoarthritis (OA). MIS UKA is not a substitute for TKA, which is the procedure of choice for treatment of advanced stages of OA. This philosophy is supported by Thornhill and Scott, who assert that UKA should be considered in the “continuum of surgical options for the treatment of the osteoarthritic patient” [1]. In cases of earlier, nonadvanced OA, the two procedures may act in conjunction with one another, with MIS UKA serving as a supplement to future TKA. Together, these devices may be considered as a “knee prosthetic system ” [2].
With the limited survivorship of TKA and the aging of the active baby boomer population, there is a need for a procedure in addition to TKA to address the treatment of earlier, nonadvanced stages of OA and to extend the survivability of knee prosthetics. Because knee prosthetics have a finite life span, a single device cannot encompass the entire spectrum of survivability necessary for many patients. Under the senior author’s serial replacement concept, a procedure such as MIS UKA performed at an earlier age, before TKA use and as a supplement to TKA, will absorb approximately 10 years of functional capacity so that when and if future arthroplasty is required, the survivability of the entire knee prosthetic system is lengthened [2, 3]. By following this philosophy, the use of MIS UKA in conjunction with a future TKA may increase the functional capacity of the entire knee prosthetic system to 20–30 years. The fundamental goal of this serial prosthetic replacement is to decrease the likelihood of a complex revision procedure in the patient’s lifetime.
Minimally Invasive UKA Program
A unique feature of this serial replacement philosophy is the MIS UKA program that was introduced by the senior author in 1992 [4]. This program is significantly different from simple use of a small incision or implementation of a MIS surgical approach. Instead, it combines the following MIS concepts into a single program.
Adjunct Use of Arthroscopy
This multipronged MIS approach begins with arthroscopic evaluation prior to arthroplasty, which allows assessment of the articular cartilage in the contralateral compartment and permits the evaluation of the contralateral meniscus. The contralateral meniscus cannot be visualized through traditional surgical exposure alone. If the contralateral compartment has advanced OA or if the contralateral meniscus is not intact, the preplanned MIS UKA procedure may be abandoned in favor of TKA.
Verification of a fully functioning, intact, contralateral meniscus is critical for successful UKA, as the load-bearing surface area and the stability of the knee joint are enhanced by intact menisci [5–11]. Due to the lower tibiofemoral contact area compared with TKA designs, a certain degree of cold flow is permissible in UKA designs, but an absent contralateral meniscus will result in an inadequate amount of tibiofemoral contact. If UKA is performed in spite of an absent contralateral meniscus, the continued osteoarthritic progression may hasten the rate of degeneration of the untreated contralateral side, possibly leading to early failure of the UKA device [12]. Thus, although eliminating overcorrection has reduced the incidence of UKA failures in recent years [1, 6, 12–25], contralateral compartment degeneration and early UKA failure remain a concern if the contralateral meniscus is not intact and the cruciate ligaments are not properly balanced.
Minimally Invasive Surgical Approach Avoiding Patellar Dislocation
A distinction must be made between a MIS surgical approach and a “mini-incision,” which merely is a small hole and may result in significant distortion of soft tissue. A MIS surgical approach requires preservation of all possible tissues required for any future restoration, including the suprapatellar pouch, the quadriceps tendon, the patella, and the medial tibial buttress. The only UKA system meeting these criteria is the MIS bone-sparing UKA technique. By combining UKA with a MIS surgical approach, a reduction in postoperative morbidity and pain, a decrease in rehabilitation time without the need for formal physical therapy, and the ability to perform the procedure on a same-day or short-stay basis are possible [4, 26–31]. Compared with traditional open UKA, MIS UKA is associated with faster rates of recovery and earlier discharge [29, 30, 32]. In addition, equal reliability, without compromising proper component placement or long-term survivorship, has been demonstrated between a MIS surgical approach and a wide incision [26, 29, 32]. The diminished postoperative pain and decreased rehabilitation time associated with MIS UKA most likely are results of preservation of the quadriceps tendon and not the short skin incision itself [32].
Resurfacing UKA Design with Inlay Tibial Component
Another key feature of the senior author’s MIS UKA program is the use of a resurfacing UKA design with an inlay tibial component. A significant problem in the conversion of UKA to TKA is medial tibial bone loss [33, 34]. The use of an all-polyethylene inlay tibial component requires minimal bone resection and preserves the medial buttress and, therefore, is advantageous compared with use of their modular, saw-cut tibial counterparts, which are thicker and require significantly more bone resection. Due to the minimally invasive nature of the bone-sparing UKA technique, conversion to a TKA may be considered as a delayed primary TKA. An additional source of bone resection with other UKA systems is the full exposure often required for jig instrumentation. Finally, because many saw-cut tibial designs employ peg or fin fixation, the tibial bone is further compromised upon implant removal and may necessitate the use of bone grafts, special custom devices, or metal wedge tibial trays to stabilize the tibia during conversion to TKA [33–37].
Pain Management with Local Anesthetic and Without Use of Narcotics
Outpatient status is possible with the advocated MIS UKA program due to a structured pain management protocol. Spinal or general anesthesia is used in all cases. During surgery, 30-mg ketorolac tromethamine (15 mg for patients older than 65 years of age) is administered either intramuscularly or intravenously and is repeated after 5 h in patients with normal renal function. All incised tissues are infiltrated with long-acting local anesthetics to further pain relief. Additional components of the pain management protocol include patient education, avoidance of cerebral-depressing injectable narcotics, and the preemptive use of scheduled oral 400-mg ibuprofen every 4 h and oral 500-mg acetaminophen/5-mg hydrocodone bitartrate every 4 h for the first 3 days postoperatively.
As a result of this multimodal pain management program, patients are fully alert in the recovery room and have no local knee pain. Because pain is absent, the patients are able to perform straight leg raises and to actively participate in the postoperative rehabilitation process. The use of local anesthetic and avoidance of narcotics are credited for shortening the recovery and rehabilitation time, permitting the procedure to be performed on an outpatient basis.
Patient Selection
Proper patient selection is a significant factor contributing to the success of UKA for both MIS and traditional techniques. According to the senior author’s selection criteria, all patients between 50 and 90 years of age who are diagnosed with OA, have failed nonoperative treatment, present with weight-bearing pain that significantly impairs quality of life, and have weight-bearing radiographs with complete loss of medial joint space are considered candidates for MIS UKA. During the preoperative evaluation, radiographic assessment identifies pathological changes and establishes the extent of OA; physical examination determines the degree of pain, function, and deformity; and patient discussion divulges activities of daily living limitations, as well as occupational and functional demands, which are of particular importance in electing UKA [17, 38]. Although this preoperative evaluation assists in selecting potential UKA candidates, the decision to perform UKA may only be finalized at the time of surgery, at which point the status of the contralateral compartment and meniscus is evaluated.
A thorough radiographic analysis is critical to the patient selection process. In addition to obtaining weight-bearing anteroposterior, lateral, and patellofemoral radiographs, the Ahlback classification routinely is used to grade the progression of medial compartment OA [39]. The anatomic tibiofemoral alignment averages 6° varus for medial disease [40]. To qualify for UKA, OA must be confined to a single tibiofemoral compartment on weight-bearing radiograph. According to Sisto et al., the key to UKA success is being absolutely certain that OA is confined only to the involved compartment that is to be replaced [41]. Slight degenerative changes in the contralateral compartment, however, may be permissible and do not seem to adversely affect the results of UKA provided that the articular cartilage on the weight-bearing surface of the contralateral compartment appears adequate [15, 20, 21, 42, 43]. The presence of large osteophytes on the femoral condyle of the uninvolved compartment, however, may be indicative of bi- or tri-compartmental disease and, hence, is a contraindication to UKA [1, 20, 44].
Because the joint line becomes elevated by several millimeters in the weight-bearing position, most patients with medial OA exhibit an altered patellofemoral compartment, which is not considered a contraindication for UKA [20, 21, 42]. UKA should not be an option, however, if the Merchant’s view demonstrates sclerosis with marked loss of lateral patellofemoral joint space [40].
Although the majority of patients selected for UKA demonstrate Ahlback stage 2 (absence of joint line) or stage 3 (minor bone attrition), the procedure may be considered in select cases with Ahlback stage 4 (moderate bone attrition) [40]. Patients with Ahlback stage 1 should be excluded from consideration, as the disease progression is in its early stages. Ahlback stage five patients have advanced OA with gross bone attrition, and, therefore, are more appropriately treated with TKA [40].
For Ahlback stage 2, 3, and 4 patients to be considered as UKA candidates, range of motion must be at least 10–90° [2, 3]. Instability, such as a compromised anterior cruciate ligament (ACL), is a relative contraindication to medial UKA [1–3, 23, 43, 45–47], but an absolute contraindication to lateral UKA [2, 3]. Rheumatoid arthritis, extensive avascular necrosis, and active or recent infection are absolute contraindications [2, 3]. As long as absolute indications are met, certain relative contraindications, including obesity and high activity, do not appear to significantly affect UKA survivorship [22, 25, 47].
Whereas other surgeons adhere to strict selection criteria [18, 48–50], concentrating on absolute indications and contraindications, the senior author follows a broad approach [3, 31], considering patient choice rather than definitive criteria. In accordance to the serial replacement concept, MIS UKA is used to treat patients with unicompartmental OA who wish to avoid or postpone TKA. If TKA is required in the future, the UKA may be converted to a primary TKA, which may survive the duration of the patient’s life.
In the senior author’s 25 years of offering MIS UKA, patients with unilateral OA readily accept the concept of a temporizing arthritis bypass to delay or prevent TKA. When presented with a choice between UKA and TKA, patients tend to opt for the less invasive procedure [3, 31]. In a study by Hawker et al. assessing the need for and willingness to undergo arthroplasty, less than 15 % of patients with severe arthritis were definitely willing to undergo arthroplasty, which led to the conclusion that patients’ preferences and surgical indications must be considered mutually when evaluating the need and appropriateness of arthroplasty [51]. Because most patients with unicompartmental OA are inconvenienced by pain, but remain involved in recreational or professional interests, UKA is an appealing alternative to TKA as a means of not only reducing symptoms but also allowing continued participation in their desired activities.
Preoperative Discussion and Informed Patient Consent
A comprehensive preoperative discussion is an integral component of this treatment approach. The serial replacement concept must be explained to the patient so that he or she understands that most knee prosthetics, including UKA and primary TKA devices, have a finite survivorship. If MIS UKA is selected, the patient must be aware that it may be the first component of a serial knee prosthetic system that will be used to treat knee OA. This is of particular importance to the young, heavier, or more active patient, who must be advised that the effectiveness of his or her UKA may be shorter than the 10-year duration experienced by the average UKA patient [31, 52, 53]. Conversely, UKA in an older or less active patient may function well beyond 10 years [31, 52]. Finally, the surgeon should explain that the most appropriate treatment option, UKA or TKA, will be determined at the time of surgery. Because of the possibility of performing TKA if OA is too advanced, all patients scheduled to undergo surgery should be encouraged to sign informed consents for both UKA and TKA [1, 54].
MIS Bone-Sparing UKA Surgical Technique
The MIS bone-sparing UKA surgical technique has been previously described [2, 4, 40, 55]. The technique for medial implantation is summarized below, as medial compartment OA is the most common indication for UKA. The goal of the procedure is to replace the medial tibiofemoral compartment and balance the forces so that body weight is equally dispersed between the replaced compartment and the opposite compartment.
Patient Preparation
General, spinal, or regional anesthesia may be employed; however, the anesthesia team must be cognizant of the goal for outpatient or short-stay rehabilitation, which requires walking within 2–4 h postsurgery. Patient preparation is performed per standard protocols, with patient placement in a supine position. A thigh holder with an arterial tourniquet set at 300 mmHg is used to secure the leg. A standard operating table is used, with the foot end of the table placed in a flexed position. The MIS surgical approach requires continuous repositioning of the knee to optimize visualization, as certain structures are better visualized at low or high degrees of flexion. Because knee positioning from 0° to 120° of flexion is necessary, the lower leg and knee are drape-free.
Diagnostic Arthroscopy
Prior to commencing MIS UKA, the preoperative diagnosis of unicompartmental OA is confirmed through arthroscopy using a medial portal. In addition to verifying that the contralateral compartment is unaffected, the status of the contralateral meniscus must be inspected, as it cannot be visualized through the flexion gap during the open procedure. The extent of medial compartment damage and the status of the ACL also should be noted.
The UKA procedure should proceed only if the OA is limited to one tibiofemoral compartment and the contralateral meniscus is functional. If the disease process is more progressive, the surgeon must be prepared to perform a TKA, the potential of which should be preoperatively discussed and consented to by the patient.
Exposure with Posterior Femoral Condyle Resection
To proceed with the MIS UKA, a limited 7- to 10-cm skin incision is developed from the superomedial edge of the patella to the proximal tibial region, incorporating the arthroscopic portal. A subcutaneous dissection, producing a 2- to 5-cm skin flap surrounding the entire incision, improves skin mobility and visualization.
A medial parapatellar capsular arthrotomy is created from the superior pole of the patella to the tibia. A 2-cm transverse release of the vastus medialis tendon further enhances visualization. If additional exposure to the femoral condyle is required, a 2- to 3-cm segment of the medial parapatellar osteophyte may be resected with a sagittal saw. This medial parapatellar capsular arthrotomy is fundamental to the MIS surgical technique, as it does not violate the extensor mechanism nor does it dislocate the patella. By avoiding patellar dislocation, the suprapatellar pouch remains intact and able to unfold the required four times in length during knee flexion to 90° [40, 55, 56]. On the contrary, during traditional open TKA or UKA procedures, the suprapatellar pouch is damaged when the patella is everted, necessitating extensive physical therapy to reverse the iatrogenic damage.
Because medial compartment OA is an extension gap disease (Fig. 1), with no defect in flexion gap, approximately 10 mm of space must be created in the flexion gap to accommodate the prosthesis. The first step in generating this space is a 5- to 8-mm resection of the posterior femoral condyle. The articular defect is located at the distal femur and the anterior tibia. An area of preserved articular cartilage, located by flexing the knee 90°, causing the femur to roll back onto the tibia, serves as an excellent reference point for reconstruction (Fig. 2).
Medial unicompartmental osteoarthritis is an extension gap disease. (a) No articular surface loss is present in the flexion gap. (b) In contrast, approximately 5 mm of articular surface is lost in the extension gap. This narrowingof the medial compartment joint space is evident on radiographic evaluation and is responsible for many of the clinical observations characteristic of medial unicompartmental osteoarthritis, including ACL and medial collateral ligament (MCL) laxity, lateral tibial thrust, or varus deformity, present in the extension gap and absent in the flexion gap
Distraction with Tibial Inlay Preparation and Resection
Curved distractor pins are inserted at the femoral and tibial levels to allow placement of a joint distractor, which improves visualization of the tibial plateau. At the posterior tibia, adjacent to the posterior tibial rim, a high-speed bur is buried 5 mm into normal cartilage to create the additional 4–5 mm of space in the flexion gap necessary for prosthetic insertion. In the anterior tibial region, corresponding to the area of articular cartilage loss and sclerotic bone formation, the medial tibial buttress is preserved by burying the bur at half-depth (3 mm). The bur holes are connected, creating a guide slot (Fig. 3).
During tibial resection, it also is critical to preserve a 2- to 3-mm circumferential rim, which aids in component stabilization. This entire resection process creates a bed for the all-polyethylene tibial inlay component. The natural location of femoral weight transfer at the anterior tibial level is indicated by the use of a crosshatch. The tibia inlay component then is fitted and adjusted as necessary.
Preservation of the layer of sclerotic bone creates a stable platform for the tibial component and minimizes medial tibial bone loss, which is a major cause of UKA revision [33, 34]. The importance of preserving this medial tibial buttress is analogous to the preservation of the posterior acetabular rim in total hip arthroplasty in that, if absent, future reconstruction is severely compromised. The use of resurfacing UKA designs with tibial inlay components is advantageous compared with the use of other UKA designs that require saw-cut resections and, hence, sacrifice the valuable layer of sclerotic bone, i.e., the medial tibial buttress (Fig. 4).
Femoral Preparation and Resection
Femoral preparation begins by creating a depth gauge using a 5.5-mm round bur drilled to a half-depth of 3 mm into the femoral extension gap surface (Figs. 2 and 5). An additional full depth of 5 mm is created at the junction with the previous saw cut and the distal femoral surface, which will allow the curved portion of the femoral component to set midway between the flexion and extension gaps (45° flexion position). Four 3-mm drill hole guides are created and bulk bone is resected to the guide depth (Fig. 6). This method of femoral resection allows adequate space for component insertion while preventing settling.
Femoral–Tibial Alignment
With the knee in full extension and flexion, methylene blue marks are created on the sclerotic tibial bone and on the corresponding area of the femoral condyle to indicate both the desired center of rotation, or contact point, of the femoral component in relation to the tibial component and the desired center point of the femoral component (Fig. 7). A femoral drill guide with a large central slot to visualize component alignment is inserted to assist in the creation of a center femoral drill hole. Referencing the methylene blue markings, a keel slot for the fin of the femoral component is created using a sagittal saw or side-cutting bur. The trial femoral component is placed using the femoral inserter.
Trial Reduction and Local Anesthetic Injection
Trial reduction is performed to evaluate range of motion through 115° of flexion and to assess soft tissue balancing. Lack of complete extension or flexion indicates inadequate tibial or femoral preparations. Insertion and proper alignment of appropriately sized implants should result in ligament balancing. If, however, the ligaments are tight only in the extension gap, tension may be adjusted by further bone removal at the distal femoral level. If tension is present in both the flexion and extension gaps, additional tibial bone may be resected, as previously described, in 1-mm increments until proper tension is achieved.
After satisfactory range of motion and proper soft tissue balancing are achieved, the trial components are removed, the joint is irrigated thoroughly, and a dry field is established. At this stage, both the femoral and tibial preparations are visible. Prior to component insertion, all incised tissues are infiltrated with anesthesia (0.25 % bupivacaine and 0.5 % epinephrine solution) for postoperative pain relief and hemostasis (Fig. 8).
Component Insertion and Final Preparation
After irrigation with pulse lavage and antibiotic solution, methyl methacrylate cement is used to insert all components into gauze-dried bone (Fig. 9). To dry the field and to aid in cement removal, sponge packs are placed in the suprapatellar pouch, posterior to the femoral condyle, and on the femoral and tibial surfaces. Excess cement is removed from the posterior recess and perimeter of the tibial component after insertion, but before femoral component placement, using a narrow nerve hook. After femoral component placement, excess cement is removed from the perimeter using a dental pick. Range of motion is performed following final prosthetic implantation to evaluate the flexion–extension gaps. Cement is cured with the knee in full extension. After the cement mantle has hardened, any remaining osteophytes should be removed. Patella contouring or notchplasty also may be performed, if necessary. As a final step, the joint is thoroughly irrigated with sterile saline.
The tourniquet is deflated and hemostasis is achieved with electrocautery. A tube drain is inserted into the contralateral component via a stab wound. Capsular closure is performed with size 0 Vicryl suture (Ethicon Company; Somerville, NJ). Subcuticular size 0 Prolene suture and sterile dressing are used for skin closure. Before exiting the operating room, a circumferential ice cuff, a pneumatic compression device, and an immobilizer are applied.
Surgical Technique for Conversion of MIS Bone-Sparing UKA to TKA
UKA Prosthesis Removal
The Repicci II unicondylar knee system (Biomet Inc., Warsaw, IN) is designed to extend the life of a natural knee while preserving the bone. As OA advances into the lateral femoral condyle, which may occur 10 years after the UKA procedure, conversion to TKA may be necessary. The MIS nature of this particular UKA design, along with the surgical technique described below for the removal of the UKA prosthetic system, results in minimal bone loss. Because resections equivalent to those performed in a primary TKA are produced, this conversion to a TKA may be considered as a delayed primary TKA.
Patient Preparation and Exposure
Anesthesia and patient preparation are performed per routine TKA protocols. A standard medial parapatellar approach is used, incorporating the previous UKA incision. The quadriceps tendon is split to the apex of the suprapatellar pouch. Four loops of size 0 Vicryl suture are placed at the apex to prevent tearing into the quadriceps muscle. A standard medial parapatellar approach is used to complete the exposure. The undersurface of the patella is resected to allow visualization with minimal soft tissue exposure.
Femoral Preparation
Overgrown bone is removed from the medial aspect of the femoral component. A drill hole is created in the distal femur for insertion of a standard intermedullary guide rod. A standard TKA distal femoral resection guide then is fixated into position. The femoral prosthesis should not be removed at this time. A standard, thick saw blade is used to resect the distal femur at the 9-mm level. It is important to resect all bone visible around the prosthetic system, taking caring to undermine the bone adjacent to the fin of the prosthesis (Fig. 10). A small saw blade is used to strip all remaining bone visible around the prosthetic system. A small osteotome then is used to remove the excess bone that has been previously undermined from the initial saw cut.
The femoral prosthesis is 3 mm in thickness and the femoral cutting guide is set at 9 mm; therefore, 5–6 mm of fin and post are exposed by this technique, with the surface of the femoral prosthesis sitting 5–6 mm proud of the distal femoral surface cut (Fig. 11). The remaining exposed bone is removed from the fin and the posterior aspect of the femoral prosthesis with a small saw blade. The saw is placed posteriorly along the posterior aspect of the femoral condyle to ensure that the bony interface has been properly exposed.
At this time, any attempt to drive the femoral prosthesis off the femur risks the development of a serious fracture or loss of a significant portion of the femoral condyle. The surface of the prosthesis, therefore, is tapped into the distal femur with a hammer. The post of the prosthesis acts as a punch and is driven somewhat into the bone. The fin serves as an osteotome, allowing disruption of the bone–cement interface without damage to the condyles or bone loss (Fig. 12). The femoral prosthesis then is grasped and removed from the femoral condyle without bone loss.
Tibial Preparation
The all-polyethylene inlay tibial component is 6.5 mm in thickness. The standard TKA tibial cutting guide is set at 10 mm for 10 mm of resection. It is not necessary to remove the prosthesis. By simply cutting below it, the medial tibial buttress is preserved, which allows adequate bone support for TKA (Fig. 13). This step is performed prior to the final femoral resection to allow adequate space for insertion of the distal femoral resection guide.
Final Femoral Preparation
The distal femoral resection guide is applied using Whiteside’s anteroposterior (AP) axis line as a mid-guide due to the defect in the posterior aspect of the femoral condyle. Standard saw cuts are used to create the necessary distal surfaces. As when performing a standard TKA, it is important to remove the posterior femoral osteophytes.
At this point, the UKA prosthetic system has been removed with minimal bone loss, and the appropriate femoral and tibial preparations are complete (Fig. 14). The TKA may proceed with insertion of the desired TKA prosthetic design per standard procedures.
Results
This MIS UKA approach with medial inlay preparation was utilized in a retrospective study comprised of 136 patients classified with Ahlback stages 2, 3, or 4 OA [31]. A resurfacing UKA design, the Repicci II unicondylar knee system, was used in all cases. All patients ambulated with a walker within 4 h after surgery, and most (98 %) were discharged from the hospital within 23 h. The overall revision rate to TKA was 7 % at 8 years. Primary TKA designs were used in the eight cases requiring revision, with good (25 %) or excellent (75 %) Knee Society clinical ratings at follow-up. These results support the safety and efficacy of this MIS UKA technique, illustrate its decreased recovery and rehabilitation time, and substantiate the relative ease of conversion to TKA, if required.
Conclusion
The senior author’s multipronged MIS UKA program results in minimal interference in physiology, lifestyle, and future treatment options. The thorough preoperative clinical and radiographic evaluation, which is corroborated by diagnostic arthroscopy, assists in excluding patients with more advanced stages of OA, for whom TKA is the more appropriate treatment choice, thereby reducing morbidity and increasing survivorship of MIS UKA. Because the MIS surgical approach avoids patellar dislocation and nonessential tissue dissection, interference in physiology is averted, which results in lower morbidity and rapid rehabilitation. The resurfacing UKA design diminishes bone resection compared with other UKA designs and, consequently, does not limit future treatment options. Therefore, this MIS UKA may be used in a broader range of patients, including younger, heavier, or more active patients. Combined with the structured pain management program, MIS UKA may be performed on an outpatient basis, with full independence achieved within 4 h postoperatively. The resulting rapid rehabilitation and return to activities of daily living address patient desire to minimize lifestyle interference, thereby enhancing patient satisfaction.
The long-term survivorship of MIS UKA is variable and dependent on many factors, including the stage of OA at insertion, the amount of tibial bone support, and material limitations, such as polyethylene deformity and wear. However, because the single most important factor affecting UKA survivorship, regardless of design or use of a MIS approach, is precise surgical technique, proper instructional training is critical in ensuring the surgical expertise required for a successful UKA. Although combining a MIS approach with UKA is appealing, due to lower morbidity and decreased rehabilitation, it adds a significant variable to an already demanding surgical procedure. Proper component positioning and accurate cement removal in the face of decreased visualization is essential. However, once the technique is mastered, this UKA bone-sparing technique combined with the multipronged MIS program is a highly desirable treatment option for patients suffering from unicompartmental OA and has a distinctive role in the orthopedic surgeon’s knee prosthetic armamentarium.
References
Thornhill TS, Scott RD. Unicompartmental total knee arthroplasty. Orthop Clin N Am. 1989;20(2):245–56.
Repicci JA, Hartman JF. Minimally invasive unicondylar knee arthroplasty for the treatment of unicompartmental osteoarthritis: an outpatient arthritic bypass procedure. Orthop Clin N Am. 2004;35:201–16.
Repicci JA, Hartman JF. Unicondylar knee replacement: the American experience. In: Fu FH, Browner BD, editors. Management of osteoarthritis of the knee: an international consensus. 1st ed. Rosemont: American Academy of Orthopaedic Surgeons; 2003. p. 67–79.
Repicci JA, Eberle RW. Minimally invasive surgical technique for unicondylar knee arthroplasty. J South Orthop Assoc. 1999;8(1):20–7.
Fithian DC, Kelly MA, Mow VC. Material properties and structure function relationships in the menisci. Clin Orthop Relat Res. 1990;252:19–31.
Grelsamer RP. Current concepts review. Unicompartmental osteoarthrosis of the knee. J Bone Joint Surg Am. 1995;77(2):278–92.
Ihn JC, Kim SJ, Park IH. In vitro study of contact area and pressure distribution in the human knee after partial and total meniscectomy. Int Orthop. 1993;17(4):214–8.
Johnson RJ, Kettelkamp DB, Clark W, et al. Factors affecting late results after meniscectomy. J Bone Joint Surg Am. 1974;56(4):719–29.
Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;149:283–90.
Shrive NG, O’Connor JJ, Goodfellow JW. Load-bearing in the knee joint. Clin Orthop Relat Res. 1978;131:279–87.
Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–92.
Marmor L. Results of single compartment arthroplasty with acrylic cement fixation. A minimum follow–up of two years. Clin Orthop Relat Res. 1977;122:181–8.
Bohm I, Landsiedl F. Revision surgery after failed unicompartmental knee arthroplasty. A study of 35 cases. J Arthroplasty. 2000;15(8):982–9.
Goodfellow JW, Kershaw CJ, Benson MK, et al. The Oxford knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg (Br). 1988;70(5):692–701.
Goodfellow JW, Tibrewal SB, Sherman KP, et al. Unicompartmental Oxford meniscal knee arthroplasty. J Arthroplasty. 1987;2(1):1–9.
Kennedy WR, White RP. Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin Orthop Relat Res. 1987;221:278–85.
Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am. 1989;71(1):145–50.
Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am. 1978;60(2):182–5.
Marmor L. Marmor modular knee in unicompartmental disease. Minimum four year follow-up. J Bone Joint Surg Am. 1979;61(3):347–53.
Marmor L. Unicompartmental knee arthroplasty. Ten- to 13-year follow-up study. Clin Orthop Relat Res. 1988;226:14–20.
Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg (Br). 1998;80(6):983–9.
Squire MW, Callaghan JJ, Goetz DD, et al. Unicompartmental knee replacement. A minimum 15 year follow-up study. Clin Orthop Relat Res. 1999;367:61–72.
Stockelman RE, Pohl KP. The long-term efficacy of unicompartmental arthroplasty of the knee. Clin Orthop Relat Res. 1991;271:88–95.
Swank M, Stulberg SD, Jiganti J, et al. The natural history of unicompartmental arthroplasty. An eight-year follow-up study with survival analysis. Clin Orthop Relat Res. 1993;286:130–42.
Tabor Jr OB, Tabor OB. Unicompartmental arthroplasty: a long-term follow-up study. J Arthroplasty. 1998;13(4):373–9.
Brown A. The Oxford unicompartmental knee replacement for osteoarthritis. Issues Emerg Health Technol. 2001;23:1–4.
Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clin Orthop Relat Res. 2001;392:272–8.
Keys GW. Reduced invasive approach for Oxford II medial unicompartmental knee replacement-a preliminary study. Knee. 1999;6(3):193–6.
Murray DW. Unicompartmental knee replacement: now or never? Orthopedics. 2000;23(9):979–80.
Price A, Webb J, Topf H, et al. Oxford unicompartmental knee replacement with a minimally invasive technique. J Bone Joint Surg (Br). 2000;82 Suppl 1:24.
Romanowski MR, Repicci JA. Minimally invasive unicondylar arthroplasty. Eight-year follow-up. Am J Knee Surg. 2002;15(1):17–22.
Price AJ, Webb J, Topf H, Dodd CA, Goodfellow JW, Murray DW. Rapid recovery after Oxford unicompartmental arthroplasty through a short incision. J Arthroplasty. 2001;16(8):970–6.
Barrett WP, Scott RD. Revision of failed unicondylar unicompartmental knee arthroplasty. J Bone Joint Surg Am. 1987;69(9):1328–35.
Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am. 1991;73(2):186–90.
Insall J, Dethmers DA. Revision of total knee arthroplasty. Clin Orthop Relat Res. 1982;170:123–30.
Lai CH, Rand JA. Revision of failed unicompartmental total knee arthroplasty. Clin Orthop Relat Res. 1993;287:193–201.
Rand JA, Bryan RS. Results of revision total knee arthroplasties using condylar prostheses. A review of fifty knees. J Bone Joint Surg Am. 1988;70(5):738–45.
Kozinn SC, Scott RD. Surgical treatment of unicompartmental degenerative arthritis of the knee. Rheum Dis Clin N Am. 1988;14(3):545–64.
Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn. 1968;277(Suppl):7–72.
Romanowski MR, Repicci JA. Unicondylar knee surgery: development of the minimally invasive surgical approach. In: Scuderi GR, Tria Jr AJ, editors. MIS of the hip and the knee: a clinical prospective. New York: Springer; 2004. p. 123–51.
Sisto DJ, Blazina ME, Heskiaoff D, et al. Unicompartmental arthroplasty for osteoarthrosis of the knee. Clin Orthop Relat Res. 1993;286:149–53.
Carr A, Keyes G, Miller R, et al. Medial unicompartmental arthroplasty. A survival study of the Oxford meniscal knee. Clin Orthop Relat Res. 1993;295:205–13.
Jackson RW. Surgical treatment. Osteotomy and unicompartmental arthroplasty. Am J Knee Surg. 1998;11(1):55–7.
Marmor L. Unicompartmental knee arthroplasty of the knee with a minimum ten-year follow-up period. Clin Orthop Relat Res. 1988;228:171–7.
Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery. 10-year minimum follow-up period. J Arthroplasty. 1996;11(7):782–8.
Christensen NO. Unicompartmental prosthesis for gonarthrosis. A nine-year series of 575 knees from a Swedish hospital. Clin Orthop Relat Res. 1991;273:165–9.
Voss F, Sheinkop MB, Galante JO, et al. Miller-Galante unicompartmental knee arthroplasty at 2- to 5-year follow-up evaluations. J Arthroplasty. 1995;10(6):764–71.
Berger RA, Nedeff DD, Barden RM, et al. Unicompartmental knee arthroplasty. Clinical experience at 6- to 10-year follow-up. Clin Orthop Relat Res. 1999;367:50–60.
Bert JM. 10-year survivorship of metal-backed, unicompartmental arthroplasty. J Arthroplasty. 1998;13(8):901–5.
Capra Jr SW, Fehring TK. Unicondylar arthroplasty. A survivorship analysis. J Arthroplasty. 1992;7(3):247–51.
Hawker GA, Wright JG, Coyte PC, et al. Determining the need for hip and knee arthroplasty: the role of clinical severity and patients’ preferences. Med Care. 2001;39:206–16.
Knutson K, Lewold S, Robertsson O, et al. The Swedish knee arthroplasty register. A nation-wide study of 30,003 knees 1976–1992. Acta Orthop Scand. 1994;65:375–86.
Scott RD, Cobb AG, McQueary FG, et al. Unicompartmental knee arthroplasty. Eight- to 12-year follow-up evaluation with survivorship analysis. Clin Orthop Relat Res. 1991;271:96–100.
Keblish PA. The case for unicompartmental knee arthroplasty. Orthopedics. 1994;17:853–5.
Repicci JA, Hartman JF. Minimally invasive surgery for unicondylar knee arthroplasty: the bone-sparing technique. In: Scuderi GR, Tria Jr AJ, Berger RA, editors. MIS techniques in orthopedics. New York: Springer Science + Business Media; 2006. p. 193–213.
Kapandji IA. The physiology of the joints, vol. 2. 5th ed. New York: Churchill Livingstone; 1987.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this entry
Cite this entry
Repicci, J.A., Hartman, J.F. (2016). MIS Unicondylar Arthroplasty: The Bone-Sparing Technique. In: Scuderi, G., Tria, A. (eds) Minimally Invasive Surgery in Orthopedics. Springer, Cham. https://doi.org/10.1007/978-3-319-34109-5_50
Download citation
DOI: https://doi.org/10.1007/978-3-319-34109-5_50
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-34107-1
Online ISBN: 978-3-319-34109-5
eBook Packages: MedicineReference Module Medicine