Abstract
Hypoglycemia is a frequent occurrence for many patients with diabetes treated with insulin or insulin secretagogues. Episodes of hypoglycemia have significant morbidity and mortality and are the main limiting factor for achieving near optimal glycemic control. Risk factors including impaired glucose counterregulation and hypoglycemia unawareness are largely preventable and/or reversible. This chapter summarizes our current knowledge of the epidemiology, pathogenesis, risk factors, and complications of hypoglycemia in patients with diabetes and discusses prevention and treatment strategies.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
General Considerations
Normally, plasma glucose concentrations are maintained within a relatively narrow range throughout the day (usually between 55 and 165 mg/dl [~3.0 and 9.0 mM/L]) despite wide fluctuations in the delivery (e.g., meals) and removal (e.g., exercise) of glucose from the circulation. This is accomplished by a tightly linked balance between glucose production and glucose utilization regulated by complex mechanisms.
Because of limited availability of ketone bodies and amino acids and the limited transport of free fatty acids across the blood-brain barrier, glucose can be considered to be the sole source of energy for the brain except under conditions of prolonged fasting. In the latter situation ketone bodies increase severalfold so that these may be used as an alternative fuel [1].
The brain cannot store or produce glucose and therefore requires a continuous supply of glucose from the circulation. At physiological plasma glucose levels, phosphorylation of glucose is rate limiting for its utilization. However, because of the kinetics of glucose transfer across the blood-brain barrier, uptake becomes rate limiting as plasma glucose concentrations decrease below the normal range. Consequently maintenance of the plasma glucose concentration above some critical level is essential to the survival of the brain and thus the organism. It is therefore not surprising that a complex physiological mechanism exists to prevent or correct hypoglycemia (vide infra). Nevertheless for many patients with type 1 or type 2 diabetes hypoglycemia is a frequent occurrence. Because of its possible detrimental effects on the central nervous system and the fear thereof by patients and care givers, hypoglycemia is considered to be the main limiting factor for achieving near optimal glycemic control [2].
Definition and Classification of Diabetic Hypoglycemia
The American Diabetes Association and Endocrine Society workgroup on hypoglycemia defined hypoglycemia in patients with diabetes as all episodes of an abnormally low plasma glucose concentration that expose the patient to potential harm [3]. No single threshold value was assigned to define hypoglycemia since this value may differ among patients. An alert value of <70 mg/dL (<3.8 mM/L), however, was chosen to draw the attention of patients and caregivers and also for use as a cutoff value in the classification of hypoglycemia in diabetes as outlined in Table 1 [3].
Epidemiology of Hypoglycemia
The exact incidence and prevalence of hypoglycemia in patients with diabetes is difficult to define because mild to moderate hypoglycemia may go unnoticed or unreported. Additionally, hypoglycemia unawareness (the lack of appropriate autonomic warning signals of hypoglycemia before the development of neuroglycopenia – vide infra) can be found in 25% of patients with diabetes [4, 5]. The complete detection of chemical hypoglycemia would require continuous blood glucose measurements over prolonged periods. Studies using this approach have generally found that the frequency and duration of hypoglycemia, especially nocturnal hypoglycemia, are greater than what was previously thought [6, 7]. More reliable data are available from studies reporting severe hypoglycemia that is associated with loss of consciousness or requiring external assistance [3]. In general, the frequency of hypoglycemia is lower in people with T2DM than in those with T1DM [8–11]. For example, the UK Hypoglycemia Study Group reported severe hypoglycemia rates in patients with T2DM on insulin >2 years (10 episodes per 100 patient-year) to be far less than in patients with T1DM (<5 years disease duration, 110 episodes per 100 patient-year; >15 years disease duration, 320 episodes per 100 patient-year) [9].
Hypoglycemia occurs more often during intensified insulin therapy than during conventional insulin therapy. For example, during the 6.5 year follow-up in the DCCT trial [12], 35% of patients in the conventional treatment group and 65% of patients in the intensive treatment group had at least one episode of severe hypoglycemia.
Among patients with T2DM the frequency of hypoglycemia will vary by treatment modality. In patients treated with sulfonylureas the incidence of severe hypoglycemia has been reported to be approximately 1.5 episodes per 100 patient-years [13] and is more common with long-acting sulfonylureas such as glyburide [14]. Prandial insulins are associated with a greater frequency of hypoglycemia than are the long-acting so-called basal insulins [15]. Metformin, thiazolidinediones, dipeptidyl-peptidase-4 inhibitors, glucagon-like 1 mimetics, and sodium glucose cotransporter 2 inhibitors do not increase the risk of hypoglycemia when used without insulin or insulin secretagogues (sulfonylureas and meglitinides) [16].
Hypoglycemia Counterregulation
Normal Hypoglycemia Counterregulation and Hypoglycemia Awareness
Glucose counterregulation refers to the sum of the body’s defense mechanisms which prevent hypoglycemia from occurring and which restore euglycemia. Hypoglycemia awareness refers to the symptomatic responses to hypoglycemia that alert the patient to the declining blood glucose levels.
In normal postabsorptive individuals, i.e., after an overnight fast, the sum of glucose release by liver and kidney nearly equals systemic glucose utilization so that plasma glucose concentrations remain relatively stable. Since insulin suppresses both hepatic and renal glucose release [17, 18] and stimulates glucose uptake, in insulin-sensitive tissues such as muscles, excessive exogenous insulin administration can cause systemic glucose utilization to exceed systemic glucose release so that plasma glucose concentrations decrease.
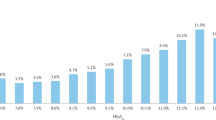
As the plasma glucose levels decrease there is a characteristic hierarchy of responses [19] (Fig. 1). Reduction of insulin secretion, the first in the cascade of hypoglycemia counterregulation [2, 4], derepresses glucose production and reduces glucose utilization. When plasma glucose levels decline to approximately 70 mg/dl (3.8 mM/L), there is an increase in the secretion of counterregulatory hormones (glucagon, epinephrine, growth hormone, cortisol) [19–22]. Glucagon and epinephrine have immediate effects on glucose kinetics whereas the effects of growth hormone and cortisol are delayed by several hours [23, 24] (Fig. 2).
Effect of lack of glucagon, catecholamine (α- and ß-adrenergic blockade), growth hormone, and cortisol responses on insulin-induced hypoglycemia in nondiabetic volunteers studied with pituitary-adrenal-pancreatic clamp (From Gerich J. Glucose counterregulation and its impact on diabetes mellitus. Diabetes 37:1608–1617, 1988. Copyright © 1988 The American Diabetes Association. Used with permission)
Effect of lack of glucagon, catecholamine (α- and ß-adrenergic blockade), growth hormone, and cortisol responses on counterregulatory changes in glucose production and glucose utilization in nondiabetic volunteers studied with pituitary-adrenal-pancreatic clamp (From Gerich J. Glucose counterregulation and its impact on diabetes mellitus. Diabetes 37:1608–1617, 1988. Copyright © 1988 The American Diabetes Association. Used with permission)
Under normal physiological conditions, these responses prevent a further decrease in plasma glucose concentrations and restore normoglycemia. Decreases to ~60 mg/dl (3.4 mM/L) usually evoke the so-called autonomic warning symptoms [25, 26] (hunger, anxiety, palpitations, sweating, nausea) which if interpreted correctly lead a person to eat and prevent more serious hypoglycemia. However, clues of hypoglycemia may vary considerably from person to person [27]. If, for some reason, plasma glucose levels decrease to about 55 mg/dl (~3.0 mM/L), neuroglycopenic signs/symptoms of brain dysfunction (blurred vision, slurred speech, glassy-eyed appearance, confusion, difficulty in concentrating) would occur [25, 26]. Further decreases can produce coma and values below 30 mg/dl (~1.6 mM/L), if prolonged, can cause seizures, permanent neurological deficits, and death. However, it should be pointed out that in otherwise healthy/young (<45 years) individuals, glucose levels averaging 35 mg/dl (~2.0 mM/L) have been maintained for as long as 8 hours without any known long-term adverse effects [28] and chronic levels as low as 24 mg/dl (1.3 mM/L) in insulinoma patients have been observed in association with apparently normal cerebral function [29].
Hypoglycemia Counterregulation and Hypoglycemia Awareness in T1DM
In T1DM, the defense against hypoglycemia is markedly deranged. First, as endogenous insulin secretion becomes progressively deficient over the first few years of T1DM, the appearance of insulin in the circulation becomes unregulated since it relies on absorption from subcutaneous injection sites. Consequently, as plasma glucose levels are falling, insulin levels do not decrease. Second, glucagon responses to hypoglycemia are lost early in the course of T1DM [30, 31]. This defect coincides with the loss of insulin secretion and is therefore the rule in people with T1DM [32]. Nonetheless, glucose counterregulation appears to be adequate in such patients probably due to compensatory counterregulation by epinephrine [33]. After a few more years epinephrine responses to hypoglycemia are also commonly reduced [30, 34, 35]. When compared to patients with a defective glucagon response but normal epinephrine responses, patients with a combined defect in glucagon and epinephrine responses have at least a 25-fold increased risk for severe iatrogenic hypoglycemia [36, 37]. The combined defect in glucagon and epinephrine responses is therefore considered as the syndrome of impaired hypoglycemia counterregulation [2]. This is now known to be associated with impaired glucose production in both liver and kidney [38]. Pathophysiological mechanisms might be different when only glucagon responses are impaired and epinephrine responses are intact. Since glucagon affects exclusively the liver whereas epinephrine has a temporary effect on the liver but a sustained effect on the kidney, only hepatic glucose production might be decreased under these conditions.
In addition to impaired glucose counterregulation, people with T1DM often suffer from hypoglycemia unawareness. These patients no longer have autonomic warning symptoms of developing hypoglycemia which previously prompted them to take appropriate action (i.e., food intake before severe hypoglycemia with neuroglycopenia occurs). Hypoglycemia unawareness has been reported to occur in about 50% of patients with long-standing diabetes and estimated to affect 25% overall [39–42]. Hypoglycemia unawareness is associated with sixfold increased risk for severe hypoglycemia [40].
The mechanism of the loss of glucagon response is not completely understood. Recent evidence suggests that similar to insulin secretion from beta cells, glucagon secretion is influenced by ATP-regulated potassium (KATP) channels that are also present in glucagon-producing alpha cells [43, 44] and that glucose-induced closure of these channels leads to suppression of glucagon secretion. Abnormally increased channel activity found in patients with diabetes may explain the inverted glucose response and the loss of appropriate glucagon counterregulation [45]. The pathogenesis for impaired catecholamines and other hormone responses is also not entirely clear but may have been set in motion from recurrent hypoglycemia that (a) impairs glucose sensing in the ventromedial hypothalamus (a brain region that plays a major role in controlling the counterregulatory responses to hypoglycemia) and (b) leads to cellular adaptation which contributes to hypoglycemia unawareness and reduced adrenomedullary response to subsequent hypoglycemia [46]. Additionally there is impairment of beta-adrenergic sensitivity leading to impaired responsiveness to endogenous catecholamines which in turn contributes to hypoglycemia unawareness [47–49].
Hypoglycemia Counterregulation and Hypoglycemia Awareness in T2DM
In T2DM the hormonal glucose counterregulation is usually less impaired than in T1DM [50–52]. Nevertheless defects can be seen when patients become markedly insulin deficient [53]. One important factor for the nearly intact hormonal glucose counterregulation in T2DM may be some residual albeit abnormal insulin secretion. Since antecedent hypoglycemia is one of the main factors for impaired epinephrine responses to hypoglycemia and since hypoglycemia rarely occurs in people with T2DM because of their intact glucagon response, epinephrine responses usually also remain intact. Once patients with T2DM become markedly insulin deficient, glucagon responses are commonly impaired. However, in contrast to patients with T1DM, the epinephrine responses usually remain intact and in fact may partially compensate for the reduced glucagon responses to hypoglycemia [52, 54]. This may explain the reduced risk for severe hypoglycemia in patients with T2DM compared to patients with T1DM.
Risk Factors for Hypoglycemia
Table 2 summarizes important causes and risk factors for hypoglycemia. Treatment with insulin or insulin secretagogues (sulfonylureas and meglitinides) is the main cause for hypoglycemia in patients with diabetes. Factors that lead to absolute or relative insulin excess in patients who are treated with insulin or insulin secretagogues are summarized in Table 3 [55, 56].
Impaired glucose counterregulation and hypoglycemia unawareness significantly increase the risk of hypoglycemia in patients who are treated with insulin or insulin secretagogues. The risk of severe hypoglycemia is increased 25-fold in patients with impaired hypoglycemia counterregulation [36] and increased sixfold in those with hypoglycemia unawareness [40].
CKD with a GFR < 60 ml/min/1.73 m2 is found in up to 40% of people with diabetes. It is an independent risk factor for hypoglycemia and augments the risk for hypoglycemia that is already present in people with diabetes by adding multiple risk factors summarized in Table 3 [55].
Many nondiabetic pharmacological agents have also been implicated as a cause for hypoglycemia. Most of the evidence for that is from case reports or single cohort studies many of which have confounding factors such as concomitant use of insulin or sulfonylurea or presence of chronic kidney disease. A study that systematically reviewed the literature for reported drugs found 448 eligible studies describing nearly 2700 cases of hypoglycemia associated with 164 different drugs other than alcohol, insulin, or insulin secretagogues [57]. When taking into account the quality of evidence for the association between a particular drug and hypoglycemia (such as presence or absence of confounders, dose–response relationships, challenge/rechallenge designs, and randomized controlled trials of drug vs. placebo), none of the drugs had association supported by high-quality evidence and only seven were supported by moderate-quality evidence including cibenzoline, clinafloxacin, gatifloxacin, glucagon (when used as endoscopic premedication), indomethacin, pentamidine, and quinine. All other drugs had low or very low evidence supporting association with hypoglycemia. The most commonly cited drugs to be associated with hypoglycemia were quinolones, pentamidine, quinine, beta blockers, and angiotensin-converting enzyme inhibitors [57].
Gastric bypass surgery is becoming more common as a treatment for morbid obesity. Many of these patients have T2DM. Hypoglycemia has been reported to occur in some patients usually in the second or third hour postprandially [58–61]. The exact mechanism is currently being investigated but could be multifactorial and related to the changes that follow surgery such as decreased caloric intake, weight loss, and a change in the nutrient composition, flora, and transit time in the gastrointestinal tract [62–64]. Studies have also shown decreased ghrelin secretion, exaggerated release of glucagon-like peptide-1 (GLP-1), and possibly other gastrointestinal hormone changes [65–69] that could enhance the release of insulin and/or inhibit the release of glucagon. Additionally, several severe cases of hyperinsulinemic hypoglycemia presenting as postprandial hypoglycemia after Roux-en-Y gastric bypass surgery have been published [70–72]. The mechanism by which this occurs is not entirely clear. Examination of pancreatic specimens obtained following partial pancreatectomy performed to treat these cases implicated nesidioblastosis or islet cell hyperplasia as a possible cause [70, 71]. A subsequent report, however, found no evidence of increased islet cell mass or neogenesis when some of these specimens were reexamined and compared with those of well-matched subjects [73]. The report suggests that hypoglycemia in these patients is related to a combination of gastric dumping and inappropriately increased insulin secretion due to either failure of beta cells to adapt to changes post gastric bypass or as an acquired phenomenon. It is also not clear whether patients with diabetes are more or less likely to suffer from post-gastric-bypass hypoglycemia when compared to other patients. Reversal of gastric bypass improved hypoglycemia in some [74, 75] but not all cases [76]. Experimentally, hypoglycemia following gastric bypass was corrected by administration of exendin-[9–39], a GLP-1 receptor antagonist [77].
Manifestations of Hypoglycemia
Manifestations of hypoglycemia are nonspecific and can sometimes be noted by observers rather than patients themselves. They can be categorized as autonomic (mostly due sympathetic neural activation) and neuroglycopenic (due to brain glucose deprivation) (Table 5). Autonomic manifestations precede neuroglycopenic and allow patients to recognize and self-treat hypoglycemia. Patients with hypoglycemia unawareness are likely to have hypoglycemia manifesting at an advanced stage with neuroglycopenic symptoms that may prevent self-treatment. Nocturnal hypoglycemia can manifest with disturbed sleep, nightmares, and “waking in sweat.” Acute severe hypoglycemia can present with a range of neurological and cardiovascular complications as detailed below.
Complications of Hypoglycemia
An episode of severe hypoglycemia can be detrimental or even fatal due to its effects on the central nervous system. At plasma glucose concentration of ~55 mg/dl (~3 mM/L), cognitive impairment and EEG changes are demonstrable. Decreases below 40 mg/dl (~2.5 mM/L) result in sleepiness and gross behavioral (e.g., combativeness) abnormalities. Further decreases can produce coma and values below 30 mg/dl (~1.6 mM/L) if prolonged can cause seizures, permanent neurological deficits, and death [78–80] (Fig. 3). It has also been suggested that repeated episodes of severe hypoglycemia may lead to subtle permanent cognitive dysfunction [81].
Hypoglycemia also affects the cardiovascular system creating cardiac repolarization abnormalities with lengthening of the QT interval and also ST wave changes, and increasing risk of arrhythmias induced by associated catecholamines response [82, 83]. Additionally, it is found to promote inflammatory and thrombotic responses and to impair endothelial function and has therefore been implicated in precipitating myocardial infarctions and strokes [83–86]. On the other hand, there is currently a suggestion that recurrent hypoglycemia, by attenuating the catecholamines response to future severe hypoglycemia, may have a positive (adaptive) aspect by reducing risk of lethal cardiac complications that could have otherwise been induced by severe catecholamines response [87]. This suggestion is based on the data demonstrating reduced risk of lethal cardiac arrhythmias induced by severe hypoglycemia in diabetic rats previously exposed to recurrent moderate hypoglycemia [88], and also reduced risk of death in T2DM patients on intensive treatment arm who experienced more hypoglycemia in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) and the Action in Diabetes and the Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) trials [89, 90].
In patients with underlying eye disease hypoglycemia has been shown to trigger retinal hemorrhages [91]. Hypoglycemia is also associated with more short-term disability and higher health care costs [92, 93]. Severe hypoglycemia has been reported to be at least a contributing factor to the cause of death in 3–13% of patients with T1DM which include motor vehicle accidents, injuries at work, etc. [94, 95]. Severe hypoglycemia due to sulfonylureas has been shown to have a mortality between 4% and 7% [96, 97].
In addition to its physical morbidity and mortality, recurrent hypoglycemia may be also associated with psychosocial morbidity. In fact many patients with diabetes are as much afraid of severe hypoglycemia as they are of blindness or renal failure [41].
Management of Hypoglycemia
Treatment
Treatment is aimed at restoring euglycemia, preventing recurrences and, if possible, alleviating the underlying cause.
In an insulin-taking diabetic patient with mild hypoglycemia due to a skipped meal, 15–20 g oral carbohydrate every 15–20 min until the blood glucose is above 80 mg/dl (4.5 mM/L) constitutes adequate treatment (Table 6) [98, 99]. Examples for oral carbohydrate source are presented in Table 7. In a patient with more severe hypoglycemia resulting in obtundation, where oral administration of carbohydrate might result in aspiration, 1 mg of glucagon administered subcutaneously or intramuscularly might be sufficient to raise the blood glucose and revive the patient so that oral carbohydrate may be given. Comatose patients should receive intravenous glucose (25 g bolus, followed by an infusion at an initial rate of 2 mg/kg/min, roughly 10 g/h) for as long as necessary for the insulin or sulfonylurea to wear off (Table 8). Sulfonylurea overdose can result in prolonged hypoglycemia requiring sustained intravenous glucose infusion aimed at keeping the blood glucose at ~80 mg/dl (~4.5 mM/L) to avoid hyperglycemia which would cause further stimulation of insulin secretion thus setting in motion a vicious cycle. Blood glucose levels should be monitored initially every 15–20 min and subsequently at 1–2 h intervals. Rarely diazoxide or a somatostatin analogue may be needed to inhibit insulin secretion [100]. Where other drugs may be involved, they should be discontinued if possible (i.e., sulfonamides in a patient with renal insufficiency). In other conditions, the underlying disorder should be treated (e.g., sepsis, heart failure, endocrine deficiency) and the blood glucose supported.
Prevention of Recurrences
Conventional Measures
For prevention of recurrences, it is important to determine whether hypoglycemia was an isolated event or whether it has occurred before. If so, how frequently? Is there any pattern to occurrences, i.e., always at night? For how long have the hypoglycemic episodes been occurring? Are they associated with hypoglycemic warning symptoms? If so, usually at what level of glycemia is hypoglycemia recognized? Are there any precipitating factors, i.e., exercise, skipped meal, erroneous insulin injection, alcohol ingestion, recent weight loss, or other precipitating factors (see above)? Did the patient spontaneously recover? What did the patient do to prevent recurrences or relieve symptoms? What is the patient’s occupation?
Obviously, if these questions reveal precipitating factors for hypoglycemia these should be eliminated (Table 9). However if careful testing does not reveal any apparent precipitating factors but reveals hypoglycemia unawareness instead, chances are relatively high that there is also impaired hypoglycemia counterregulation, especially in a patient with frequent hypoglycemic episodes. Consequently the question arises how to treat the affected patients.
The principles of intensive therapy – patient education, self-monitoring of blood glucose (SMBG), and an insulin regimen that provides basal insulin levels with prandial increments – still apply to the majority of patients who require insulin to control their diabetes. However, glycemic goals must be individualized according to the frequency of hypoglycemia. Since the prevention or correction of hypoglycemia normally involves dissipation of insulin and activation of counterregulatory hormones as discussed above, it follows that patients with impaired glucose counterregulation are extremely sensitive to very little insulin in excess of its requirement resulting in hypoglycemia. It is therefore generally accepted that normoglycemia is not a reasonable goal for such patients [101, 102]. American Diabetes Association most recent practice guidelines still recommend A1C goal for most adults to be <7% but also recognize that less stringent goals (such as <8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced complications, and comorbid conditions [103]. Approximately 25–35 mg/dL (1.5–2.0 mM/L) upward adjustment of SMBG goals is needed to increase in A1C by one percentage point.
Diabetes education in general and programs that focus on hypoglycemia have proven to be helpful and should be implemented to involve patients and their family or friends [104–106]. Patients need to learn basic skills such as the need to check blood glucose regularly, to carry supplies for treating hypoglycemia with them all the time, to have glucagon emergency kit available, to carry or wear medical alert identification, and to plan better for exercise. Advanced skills such as insulin dose adjustments and the use of continuous glucose monitors and/or insulin pumps can also be taught for many motivated and capable patients.
Substitution of preprandial short-acting (regular) insulin for rapid insulin (lispro, aspart, glulisine) may reduce the frequency of hypoglycemic episodes by reducing prolonged postprandial hyperinsulinemia [107]. Furthermore, substitution of intermediate-acting insulin (NPH) for long-acting insulin analogue (glargine or detemir) has been shown to reduce the frequency of hypoglycemia in patients with type 1 or type 2 diabetes [108–110]. In appropriate candidates, hypoglycemia can be reduced by insulin pump therapy despite the fact that glycemic control could actually improve with such therapy [111, 112]. Additionally, implementation of continuous glucose monitoring systems alone or in conjunction with insulin pump therapy has shown promising results in preventing hypoglycemia [113–115] and should be considered for appropriate patients.
If these measures result in strict avoidance of hypoglycemia, hypoglycemia awareness may be restored [116]. This might be due to an improvement in beta-adrenergic sensitivity [117]. Although strict avoidance of hypoglycemia does not improve glucagon responses to hypoglycemia in T1DM [116, 118–121], it does increase epinephrine responses [118, 121]. This however seems to be limited to patients with a diabetes duration of less than ~15 years. In patients with T1DM of more than 15 years’ duration, epinephrine responses may remain markedly impaired [116, 119]. Thus there is unfortunately no conventional therapy available to reverse impaired hypoglycemia counterregulation in such patients. Although the effects of avoidance of hypoglycemia have not been studied in patients with T2DM, it seems likely that these are similar to those in T1DM.
Pancreas/Islet Transplantation
Because of the irreversibly impaired hypoglycemia counterregulation in long-standing T1DM, pancreas or islet transplantation has been proposed as a possible treatment in patients who suffer from recurrent severe hypoglycemia despite all conventional measures [122–124]. Both procedures have been shown to lower the risk of hypoglycemia [125, 126]. Pancreatic transplantation is usually reserved for patients undergoing simultaneous kidney transplantation. It has been found to improve glucagon responses to hypoglycemia in most studies [127–133] and to improve or normalize epinephrine responses [129–131, 133–135]. Furthermore, it has been reported to improve hypoglycemia awareness in T1DM [125, 133].
Experience in the effects of islet transplantation on hypoglycemia counterregulation and awareness is limited and inconsistent [126]. Hypoglycemia awareness was found to improve in some studies [123, 136]. It seems that glucagon responses remain impaired after islet transplantation [122, 125, 137], However, epinephrine responses were reported to improve responses in some [123] but not all studies [137].
Although pancreas transplantation and islet transplantation may be promising alternatives for some patients with recurrent severe hypoglycemia, risk-benefit ratios should be very carefully analyzed because of the invasive nature of these forms of therapy and the necessity for potent lifelong immunosuppression.
Abbreviations
- CKD:
-
Chronic kidney disease
- T1DM:
-
Type 1 diabetes mellitus
- T2DM:
-
Type 2 diabetes mellitus
References
Owen O, Morgan A, Kemp H, Sullivan J, Herrera M, Cahill G. Brain metabolism during fasting. J Clin Invest. 1967;46:1589–95.
Cryer P. Banting Lecture: hypoglycemia, the limiting factor in the management of IDDM. Diabetes. 1994;43:1378–89.
Seaquist ER, Anderson J, Childs B, Cryer P, Dagogo-Jack S, Fish L, Heller SR, Rodriguez H, Rosenzweig J, Vigersky R. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36:1384–95.
Gerich J. Hypoglycemia and counterregulation in type 2 diabetes. Lancet. 2000;356(9246):19467.
Mokan M, Mitrakou M, Veneman T, Ryan C, Korytkowski M, Cryer P, Gerich J. Hypoglycemia unawareness in IDDM. Diabetes Care. 1994;17:1397–403.
Guillod L, Comte-Perret S, Monbaron D, Gaillard RC, Ruiz J. Nocturnal hypoglycaemias in type 1 diabetic patients: what can we learn with continuous glucose monitoring? Diabetes Metab. 2007;33:360–5.
Wentholt IM, Maran A, Masurel N, Heine RJ, Hoekstra JB, DeVries JH. Nocturnal hypoglycaemia in type 1 diabetic patients, assessed with continuous glucose monitoring: frequency, duration and associations. Diabet Med. 2007;24:527–32.
Leese GP, Wang J, Broomhall J, Kelly P, Marsden A, Morrison W, Frier BM, Morris AD. Frequency of severe hypoglycemia requiring emergency treatment in type 1 and type 2 diabetes: a population-based study of health service resource use. Diabetes Care. 2003;26:1176–80.
Hypoglycemia Study Group UK. Risk of hypoglycemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–7.
Akram K, Pedersen-Bjergaael U, Borch-Johnson K, Thorsteinsson B. Frequency and risk factors of severe hypoglycemia in insulin-treated type 2 diabetes: a literature survey. J Diabetes Complications. 2006;20:402–8.
Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycemia in type 2 diabetes. Diabet Med. 2008;25:245–54.
DCCT Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
van Staa T, Abenhaim L, Monette J. Rates of hypoglycemia in users of sulfonylureas. J Clin Epidemiol. 1997;50:735–41.
Gangji AS, Cukierman T, Gerstein HC, Goldsmith CH, Clase CM. A systematic review and meta-analysis of hypoglycemia and cardiovascular events: a comparison of glyburide with other secretagogues and with insulin. Diabetes Care. 2007;30:389–94.
Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, Keenan JF, Paul SK, 4-T Study Group. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–47.
Zammitt NN, Frier BM. Hypoglycemia in type 2 diabetes. Diabetes Care. 2005;28:2948–61.
Cersosimo E, Garlick P, Ferretti J. Renal glucose production during insulin-induced hypoglycemia in humans. Diabetes. 1999;48:261–6.
Meyer C, Dostou J, Gerich J. Role of the human kidney in glucose counterregulation. Diabetes. 1999;48:943–8.
Schwartz N, Clutter W, Shah S, Cryer P. The glycemic thresholds for activation of glucose counterregulatory systems are higher than the threshold for symptoms. J Clin Invest. 1987;79:777–81.
Meyer C, Grosmann R, Mitrakou A, Mahler R, Veneman T, Gerich J, Bretzel R. Effects of autonomic neuropathy on counterregulation and awareness of hypoglycemia in type 1 diabetic patients. Diabetes Care. 1998;21:1960–6.
Mitrakou A, Ryan C, Veneman T, Mokan M, Jenssen T, Kiss I, Durrant J, Cryer P, Gerich J. Hierarchy of glycemic thresholds for counterregulatory hormone secretion, symptoms, and cerebral dysfunction. Am J Physiol. 1991;260:E67–74.
Fanelli C, Pampanelli S, Epifano L, Rambotti A, Ciofetta M, Modarelli F, DiVincenzo A, Annibale B, Lepore M, Lalli C, DelSindaco P, Brunetti P, Bolli G. Relative roles of insulin and hypoglycemia on induction of neuroendocrine responses to, symptoms of, and deterioration of cognitive function in hypoglycemia in male and female humans. Diabetologia. 1994;37:797–807.
DeFeo P, Perriello G, Torlone E, Ventura M, Santeusanio F, Brunetti P, Gerich J, Bolli G. Demonstration of a role of growth hormone in glucose counterregulation. Am J Physiol. 1989;256:E835–43.
DeFeo P, Perriello G, Torlone E, Ventura M, Fanelli C, Santeusanio F, Brunetti P, Gerich J, Bolli G. Contribution of cortisol to glucose counterregulation in humans. Am J Physiol. 1989;257:E35–42.
Hepburn D, Deary I, Frier B, Patrick A, Quinn J, Fisher B. Symptoms of acute insulin-induced hypoglycemia in humans with and without IDDM. Factor-analysis approach. Diabetes Care. 1991;14:949–57.
Towler D, Havlin C, Craft S, Cryer P. Mechanism of awareness of hypoglycemia: perception of neurogenic (predominantly cholinergic) rather than neuroglycopenic symptoms. Diabetes. 1993;42:1791–8.
Cox D, Gonder-Frederick L, Antoun B, Cryer P, Clarke W. Perceived symptoms in the recognition of hypoglycemia. Diabetes Care. 1993;16:519–27.
Bolli G, DeFeo P, Perriello G, DeCosmo S, Ventura M, Campbell P, Brunetti P, Gerich J. Role of hepatic autoregulation in defense against hypoglycemia in humans. J Clin Invest. 1985;75:1623–31.
Mitrakou A, Fanelli C, Veneman T, Perriello G, Calderone S, Plantanisiotis D, Rambotti A, Raptis S, Brunetti P, Cryer P, Gerich J, Bolli G. Reversibility of unawareness of hypoglycemia in patients with insulinomas. N Engl J Med. 1993;329:834–9.
Bolli G, DeFeo P, Compagnucci P, Cartechini M, Angeletti G, Santeusanio F, Brunetti P, Gerich J. Abnormal glucose counterregulation in insulin-dependent diabetes mellitus: interaction of anti-insulin antibodies and impaired glucagon and epinephrine secretion. Diabetes. 1983;32:134–41.
Gerich J, Langlois M, Noacco C, Karam J, Forsham P. Lack of glucagon response to hypoglycemia in diabetes: evidence for an intrinsic pancreatic alpha-cell defect. Science. 1973;182:171–3.
Fukuda M, Tanaka A, Tahara Y, Ikegami H, Yamamoto Y, Kumahara Y, Shima K. Correlation between minimal secretory capacity of pancreatic ß-cells and stability of diabetic control. Diabetes. 1988;37:81–8.
Rizza R, Cryer P, Gerich J. Role of glucagon, epinephrine and growth hormone in glucose counterregulation. J Clin Invest. 1979;64:62–71.
Hirsch B, Shamoon H. Defective epinephrine and growth hormone responses in type I diabetes are stimulus specific. Diabetes. 1987;36:20–6.
Dagogo-Jack S, Craft S, Cryer P. Hypoglycemia-associated autonomic failure in insulin dependent diabetes mellitus. J Clin Invest. 1993;91:819–28.
White N, Skor D, Cryer P, Bier D, Levandoski L, Santiago J. Identification of type I diabetic patients at increased risk for hypoglycemia during intensive therapy. N Engl J Med. 1983;308:485–91.
Bolli G, DeFeo P, DeCosmo S, Perriello G, Ventura M, Benedetti M, Santeusanio F, Gerich J, Brunetti P. A reliable and reproducible test for adequate glucose counterregulation in type I diabetes mellitus. Diabetes. 1984;33:732–7.
Cersosimo E, Ferretti J, Sasvary D, Garlick P. Adrenergic stimulation of renal glucose release is impaired in type 1 diabetes. Diabetes. 2001;50 Suppl 2:A54.
Amiel S. R.D. Lawrence Lecture 1994. Limits of normality: the mechanisms of hypoglycemia unawareness. Diabet Med. 1994;11:918–24.
Gold A, MacLeod K, Frier B. Frequency of severe hypoglycemia in patients with type 1 diabetes with impaired awareness of hypoglycemia. Diabetes Care. 1994;17:697–703.
Pramming S, Thorsteinsson B, Bendtson I, Binder C. Symptomatic hypoglycemia in 411 type I diabetic patients. Diabet Med. 1991;8:217–22.
Hepburn D, Patrick A, Eadington D, Ewing D, Frier B. Unawareness of hypoglycemia in insulin-treated diabetic patients: prevalence and relationship to autonomic neuropathy. Diabet Med. 1990;7:711–7.
Macdonald PE, Marinis YZ, Ramracheya R, et al. A KATP channel-dependent pathway within alpha cells regulates glucagon release from both rodent and human islets of Langerhans. PLoS Biol. 2007;5, e143.
Munoz A, Hu M, Hussain K, Bryan J, Aguilar-Bryan L, Rajan AS. Regulation of glucagon secretion at low glucose concentrations: evidence for adenosine triphosphate-sensitive potassium channel involvement. Endocrinology. 2005;146:5514–21.
Rorsman P, Ramracheya R, Rorsman NJ, Zhang Q. ATP-regulated potassium channels and voltage-gated calcium channels in pancreatic alpha and beta cells: similar functions but reciprocal effects on secretion. Diabetologia. 2014;57(9):1749–61.
Reno CM, Litvin M, Clark AL, Fisher SJ. Defective counterregulation and hypoglycemia unawareness in diabetes: mechanisms and emerging treatments. Endocrinol Metab Clin North Am. 2013;42(1):15–38.
Korytkowski MT, Mokan M, Veneman TF, Mitrakou A, Cryer P, Gerich JE. Reduced beta-adrenergic sensitivity in patients with type 1 diabetes and hypoglycemia unawareness. Diabetes Care. 1998;21(11):1939–43.
Fritsche A, Stumvoll M, Grüb M, Sieslack S, Renn W, Schmülling RM, Häring HU, Gerich JE. Effect of hypoglycemia on beta-adrenergic sensitivity in normal and type 1 diabetic subjects. Diabetes Care. 1998;21(9):1505–10.
Trovik TS, Jaeger R, Jorde R, Sager G. Reduced beta-adrenergic sensitivity in healthy volunteers induced by hypoglycemia. Fundam Clin Pharmacol. 1995;9(2):181–6.
Heller S, MacDonald I, Tattersall R. Counterregulation in type 2 (noninsulin-dependent) diabetes mellitus: normal endocrine and glycemic responses, up to 10 years after diagnosis. Diabetologia. 1987;30:924–9.
Levy C, Kinsley B, Bajaj M, Simonson D. Effect of glycemic control on glucose counterregulation during hypoglycemia in NIDDM. Diabetes Care. 1998;21:1330–8.
Shamoon H, Friedman S, Canton C, Zacharowicz L, Hu M, Rossetti L. Increased epinephrine and skeletal muscle responses to hypoglycemia in non-insulin-dependent diabetes mellitus. J Clin Invest. 1994;93:2562–71.
Segel S, Paramore D, Cryer P. Hypoglycemia-associated autonomic failure in advanced type 2 diabetes. Diabetes. 2002;51:724–33.
Bolli G, Tsalikian E, Haymond M, Cryer P, Gerich J. Defective glucose counterregulation after subcutaneous insulin in noninsulin-dependent diabetes mellitus. J Clin Invest. 1984;73:1532–41.
Alsahli M, Gerich JE. Hypoglycemia in patients with renal disease. J Clin Med. 2015;4(5):948–64.
Alsahli M, Gerich JE. Hypoglycemia. Endocrinol Metab Clin North Am. 2013;42(4):657–76.
Murad MH, Coto-Yglesias F, Wang AT, Sheidaee N, Mullan RJ, Elamin MB, Erwin PJ, Montori VM. Drug-induced hypoglycmia: a systemic review. J Clin Endocrinol Metab. 2009;94:741–5.
Miholic J, Orskov C, Holst J, Kotzerke J, Meyer H. Emptying of the gastric substitute, glucagon-like peptide-1 (GLP-1), and reactive hypoglycemia after total gastrectomy. Dig Dis Sci. 1991;36:1361–70.
Wapnick S, Jones JJ. Changes in glucose tolerance and serum insulin following partial gastrectomy and intestinal resection. Gut. 1972;13:871–3.
Leichter S, Permutt M. Effect of adrenergic agents on postgastrectomy hypoglycemia. Diabetes. 1975;24:1005–10.
Shultz KT, Neelon FA, Nilsen LB, Lebovitz HE. Mechanism of postgastrectomy hypoglycemia. Arch Intern Med. 1971;128:240–6.
Guidone C, Manco M, Valera-Mora E, Iaconelli A, Gniuli D, Mari A, Nanni G, Castagneto M, Calvani M, Mingrone G. Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric surgery. Diabetes. 2006;55:2025–31.
Gumbs AA, Modlin IM, Ballantyne GH. Changes in insulin resistance following bariatric surgery: role of caloric restriction and weight loss. Obes Surg. 2005;15:462–73.
Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman HJ, Livingston EH, Nguyen NT, Li Z, Mojica WA, Hilton L, Rhodes S, Morton SC, Shekelle PG. Meta-analysis: surgical treatment of obesity. Ann Intern Med. 2005;142:547–59.
Gebhard B, Holst JJ, Biegelmayer C, Miholic J. Postprandial GLP-1, norepinephrine, and reactive hypoglycemia in dumping syndrome. Dig Dis Sci. 2001;46:1915–23.
Lawaetz O, Blackburn AM, Bloom SR, Aritas Y, Ralphs DN. Gut hormone profile and gastric emptying in the dumping syndrome. A hypothesis concerning the pathogenesis. Scand J Gastroenterol. 1983;18:73–80.
Dube PE, Brubaker PL. Nutrient, neural and endocrine control of glucagon-like peptide secretion. Horm Metab Res. 2004;36:755–60.
Kellum JM, Kuemmerle JF, O’Dorisio TM, Rayford P, Martin D, Engle K, Wolf L, Sugerman HJ. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg. 1990;211:763–70.
Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346:1623–30.
Patti ME, McMahon G, Mun EC, Bitton A, Holst JJ, Goldsmith J, Hanto DW, Callery M, Arky R, Nose V, Bonner-Weir S, Goldfine AB. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia. 2005;48:2236–40.
Service GJ, Thompson GB, Service FJ, Andrews JC, Collazo-Clavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med. 2005;353:249–54.
Won JG, Tseng HS, Yang AH, Tang KT, Jap TS, Lee CH, Lin HD, Burcus N, Pittenger G, Vinik A. Clinical features and morphological characterization of 10 patients with noninsulinoma pancreatogenous hypoglycaemia syndrome (NIPHS). Clin Endocrinol (Oxf). 2006;65:566–78.
Meier JJ, Butler AE, Galasso R, Butler PC. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased beta-cell turnover. Diabetes Care. 2006;29:1554–9.
McLaughlin T, Peck M, Holst J, Deacon C. Reversible hyperinsulinemic hypoglycemia after gastric bypass: a consequence of altered nutrient delivery. J Clin Endocrinol Metab. 2010;95(4):1851–5.
Campos GM, Ziemelis M, Paparodis R, Ahmed M, Davis DB. Laparoscopic reversal of Roux-en-Y gastric bypass: technique and utility for treatment of endocrine complications. Surg Obes Relat Dis. 2014;10(1):36.
Lee CJ, Brown T, Magnuson TH, Egan JM, Carlson O, Elahi D. Hormonal response to a mixed-meal challenge after reversal of gastric bypass for hypoglycemia. J Clin Endocrinol Metab. 2013;98(7):E1208–12.
Salehi M, Gatadelli A, D’Alessio DA. Blockade of glucagon-like peptide 1 receptor corrects postprandial hypoglycemia after gastric bypass. Gastroenterology. 2014;146(3):669–80.
Wredling R, Levander S, Adamson U, Lins P. Permanent neuropsychological impairment after recurrent episodes of severe hypoglycaemia in man. Diabetologia. 1990;33:152–7.
Patrick A, Campbell I. Fatal hypoglycaemia in insulin-treated diabetes mellitus: clinical features and neuropathological changes. Diabet Med. 1990;7:349–54.
Perros P, Frier B. The long-term sequelae of severe hypoglycemia on the brain in insulin-dependent diabetes mellitus. Horm Metab Res. 1997;29:197–202.
Deary I, Crawford J, Hepburn D, Langan S, Blackmore L, Frier B. Severe hypoglycemia and intelligence in adult patients with insulin-treated diabetes. Diabetes. 1993;42:341–4.
Reno CM, Daphna-Iken D, Chen YS, VanderWeele J, Jethi K, Fisher SJ. Severe hypoglycemia–induced lethal cardiac arrhythmias are mediated by sympathoadrenal activation. Diabetes. 2013;62(10):3570–81.
Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nat Rev Endocrinol. 2014;10:711–22.
Fisher B, Quin J, Rumley A, Lennie S, Small M, MacCuish A, Lowe G. Effects of acute insulin-induced hypoglycaemia on haemostasis, fibrinolysis and haemorheology in insulin-dependent diabetic patients and control subjects. Clin Sci. 1991;80:525–31.
Joy NG, Tate DB, Younk LM, Davis SN. Effects of acute and antecedent hypoglycemia on endothelial function and markers of atherothrombotic balance in healthy humans. Diabetes. 2015;64:2571–80.
Duh E, Feinglos M. Hypoglycemia-induced angina pectoris in a patient with diabetes mellitus. Ann Intern Med. 1994;121:945–6.
Cryer PE. Hypoglycemia-Associated Autonomic Failure in diabetes: maladaptive, adaptive, or both? Diabetes. 2015;64(7):2322–3.
VanderWeele JJ, Daphna-Iken D, Chen YS, Hoffman RS, Clark AL, Fisher SJ. Antecedent recurrent hypoglycemia reduces lethal cardiac arrhythmias induced by severe hypoglycemia in diabetic rats. Diabetes. 2014;53 Suppl 1:A39.
Gerstein HC, Miller ME, Byington RP, Goff Jr DC, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm Jr RH, Probstfield JL, Simons-Morton DG, Friedewald WT, Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358:2545–59.
Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F, ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Kohner E, McLeod D, Marshall J. Complications of diabetes. London: Edward Arnold; 1982.
Rhoads GG, Orsini LS, Crown W, Wang S, Getahun D, Zhang Q. Contribution of hypoglycemia to medical care expenditures and short-term disability in employees with diabetes. J Occup Environ Med. 2005;47:447–52.
Curkendall SM, Natoli JL, Alexander CM, Nathanson BH, Haidar T, Dubois RW. Economic and clinical impact of inpatient diabetic hypoglycemia. Endocr Pract. 2009;15:302–12.
Paz-Guevara A, Hsu T-H, White P. Juvenile diabetes mellitus after forty years. Diabetes. 1975;24:559–65.
Nabarro J, Mustaffa B, Morris D, Walport M, Kurtz A. Insulin deficient diabetes. Contrasts with other endocrine deficiencies. Diabetologia. 1979;16:5–12.
Seltzer H. Severe drug-induced hypoglycemia: a review. Compr Ther. 1979;5:21–9.
Berger W, Caduff F, Pasquel M, Rump A. Die relative haufigkeit der schweren Sulfonylharnstoff- hypoglykamie in den letzten 25 Jahren in der Schweiz. Schwerz Med Wschr. 1986;116:145–51.
Gaston S. Outcomes of hypoglycemia treated by standardized protocol in a community hospital. Diabetes Educ. 1992;18:491–4.
Slama G, Traynard P, Desplanque N, Pudar H, Dhunputh I, Letanoux M, Bornet F, Tchobroutsky G. The search for an optimized treatment of hypoglycemia. Carbohydrates in tablets, solution, or gel for the correction of insulin reactions. Arch Intern Med. 1990;150:589–93.
Palatnick W, Meatherall R, Tenenbein M. Clinical spectrum of sulfonylurea overdose and experience with diazoxide therapy. Arch Intern Med. 1991;151:1859–62.
Cryer P, Gerich J. Glucose counterregulation, hypoglycemia, and intensive insulin therapy in diabetes mellitus. N Engl J Med. 1985;313:232–41.
Bolli G. How to ameliorate the problem of hypoglycemia in intensive as well as nonintensive treatment of type 1 diabetes. Diabetes Care. 1999;22 Suppl 2:B43–52.
American Diabetes Association. Standards of medical care in diabetes 2015. Diabetes Care. 2015;38 Suppl 1:S58–66.
Cox D, Ritterband L, Magee J, Clarke W, Gonder-Frederick L. Blood glucose awareness training delivered over the internet. Diabetes Care. 2008;31(8):1527–8.
Samann A, Muhlhauser I, Bender R, Kloos C, Muller UA. Glycaemic control and severe hypoglycaemia following training in flexible, intensive insulin therapy to enable dietary freedom in people with type 1 diabetes: a prospective implementation study. Diabetologia. 2005;48:1965–70.
The DAFNE Study Group. Training in flexible intensive insulin management to enable dietary freedom in people with type 1 diabetes: dose adjustment for normal eating (DAFNE) randomized controlled trial. BMJ. 2002;325:746–52.
Brunelle R, Llewelyn J, Anderson J, Gale E, Koivisto V. Meta-analysis of the effect of insulin lispro on severe hypoglycemia in patients with type 1 diabetes. Diabetes Care. 1998;21:1726–31.
Home P, Bartley P, Russell-Jones D, Hanaire-Broutin H, Heeg JE, Abrams P, Landin-Olsson M, Hylleberg B, Lang H, Draeger E. Insulin detemir offers improved glycemic control compared with NPH insulin in people with type 1 diabetes: a randomized clinical trial. Diabetes Care. 2004;27:1081–7.
Rosenstock J, Dailey G, Massi-Benedetti M, Fritsche A, Lin Z, Salzman A. Reduced hypoglycemia risk with insulin glargine: a meta-analysis comparing insulin glargine with human NPH insulin in type 2 diabetes. Diabetes Care. 2005;28:950–5.
Hermansen K, Davies M, Derezinski T, Martinez RG, Clauson P, Home P. A 26-week, randomized, parallel, treat-to-target trial comparing insulin detemir with NPH insulin as add-on therapy to oral glucose-lowering drugs in insulin-naive people with type 2 diabetes. Diabetes Care. 2006;29:1269–74.
Boland E, Grey M, Oesterle A, Fredrickson L, Tamborlane W. Continuous subcutaneous insulin infusion. A new way to lower risk of severe hypoglycemia, improve metabolic control, and enhance coping in adolescents with type 1 diabetes. Diabetes Care. 1999;22:1779–84.
Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in type 1 diabetes: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med. 2008;25:765–74.
Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Effectiveness of continuous glucose monitoring in a clinical care environment: evidence from the Juvenile Diabetes Research Foundation Continuous Glucose Monitoring (JDRF-CGM) trial. N Engl J Med. 2010;363:311–20.
Bergenstal RM, Tamborlane WV, Ahmann A, Buse JB, Dailey G, Davis SN, Joyce C, Peoples T, Perkins BA, Welsh JB, Willi SM, Wood MA, STAR 3 Study Group. Effectiveness of sensor augmented insulin-pump therapy in type 1 diabetes. N Engl J Med. 2010;363:311–20.
Battelino T, Phillip M, Bratina N, Nimri R, Oskarsson P, Bolinder J. Effect of continuous glucose monitoring on hypoglycemia in type 1 diabetes. Diabetes Care. 2011;34(4):795–800.
Dagogo-Jack S, Rattarason C, Cryer P. Reversal of hypoglycemia unawareness, but not defective glucose counterregulation in IDDM. Diabetes. 1994;43:1426–34.
Fritsche A, Stumvoll M, Haring H, Gerich J. Reversal of hypoglycemia unawareness in a long-term type 1 diabetic patient by improvement of beta-adrenergic sensitivity after prevention of hypoglycemia. J Clin Endocrinol Metab. 2000;85:523–5.
Fanelli C, Epifano L, Rambotti A, Pampanelli S, Di Vincenzo A, Modarelli F, Lepore M, Annibale B, Ciofetta M, Bottini P, Porcellati F, Scionti L, Santeusanio F, Brunetti P, Bolli G. Meticulous prevention of hypoglycemia normalizes the glycemic thresholds and magnitude of most of neuroendocrine responses to, symptoms of, and cognitive function during hypoglycemia in intensively treated patients with short-term IDDM. Diabetes. 1993;42:1683–9.
Fanelli C, Pampanelli S, Epifano L, Rambotti A, Vincenzo A, Modarelli F, Ciofetta M, Lepore M, Annibale B, Torlone E, Perriello G, DeFeo P, Santeusano F, Brunetti P, Bolli G. Long-term recovery from unawareness, deficient counterregulation and lack of cognitive dysfunction during hypoglycemia, following institution of rational, intensive insulin therapy in IDDM. Diabetologia. 1994;37:1265–76.
Cranston I, Lomas J, Maran A, MacDonald I, Amiel S. Restoration of hypoglycemia unawareness in patients with long- duration insulin-dependent diabetes. Lancet. 1994;344:283–7.
Davis M, Mellman M, Friedman S, Chang C, Shamoon H. Recovery of epinephrire response but not hypoglycemic symptom threshold after intensive therapy in type 1 diabetes. Am J Med. 1994;97:535–42.
Kendall D, Teuscher A, Robertson R. Defective glucagon secretion during sustained hypoglycemia following successful islet allo- and autotransplantation in humans. Diabetes. 1997;46:23–7.
Meyer C, Hering B, Grosmann R, Brandhorst H, Brandhorst D, Gerich J, Federlin K, Bretzel R. Improved glucose counterregulation and autonomic symptoms after intraportal islet transplants alone in patients with long-standing type I diabetes mellitus. Transplantation. 1998;66:233–40.
Federlin K, Pozza G. Indications for clinical islet transplantation today and in the foreseeable future-the diabetologist's point of view. J Mol Med. 1999;77:148–52.
Choudhary RMR, Vantyghem M, Maffi P, Kay TW, Keymeulen B, Inagaki N, Saudek F, Lehmann R, Hering BJ. Evidence-informed clinical practice recommendations for treatment of type 1 diabetes complicated by problematic hypoglycemia. Diabetes Care. 2015;38:1016–29.
Robertson RP. Islet transplantation for type 1 diabetes, 2015: what have we learned from alloislet and autoislet successes? Diabetes Care. 2015;38:1030–5.
Bosi E, Piatti P, Secchi A, Monti L, Traeger J, Dubernard J, Pozza G. Response of glucagon and insulin secretion to insulin-induced hypoglycemia in diabetic patients after pancreatic transplantation. Diab Nutr Metab. 1988;1:21–7.
Diem P, Redman J, Abid M, Moran A, Sutherland D, Halter J, Robertson R. Glucagon, catecholamine, and pancreatic polypeptide secretion in type I diabetic recipients of pancreas allografts. J Clin Invest. 1990;86:2008–13.
Bolinder J, Wahrenberg H, Persson A, Linde B, Tyden G, Groth C, Ostman J. Effect of pancreas transplantation on glucose counterregulation in insulin-dependent diabetic patients prone to severe hypoglycaemia. J Intern Med. 1991;230:527–33.
Bolinder J, Wahrenberg H, Linde B, Tyden G, Groth C, Ostman J. Improved glucose counterregulation after pancreas transplantation in diabetic patients with unawareness of hypoglycemia. Transplant Proc. 1991;23:1667–9.
Landgraf R, Nusser J, Riepl R, Fiedler F, Illner W, Abendroth D, Land W. Metabolic and hormonal studies of type 1 (insulin-dependent) diabetic patients after successful pancreas and kidney transplantation. Diabetologia. 1991;34 Suppl 1:S61–7.
Barrou Z, Seaquist E, Robertson R. Pancreas transplantation in diabetic humans normalizes hepatic glucose production during hypoglycemia. Diabetes. 1994;43:661–6.
Kendall D, Rooney D, Smets Y, Bolding L, Robertson R. Pancreas transplantation restores epinephrine response and symptom recognition during hypoglycemia in patients with long-standing type 1 diabetes and autonomic neuropathy. Diabetes. 1997;46:249–57.
Luzi L, Battezzati A, Perseghin G, Bianchi E, Vergani S, Secchi A, La Rocca E, Staudacher C, Spotti D, Ferrari G, Di Carlo V, Pozza G. Lack of feedback inhibition of insulin secretion in denervated human pancreas. Diabetes. 1992;41:1632–9.
Battezzati A, Luzi L, Perseghin G, Bianchi E, Spotti D, Secchi A, Vergani S, Di Carlo V, Pozza G. Persistence of counter-regulatory abnormalities in insulin-dependent diabetes mellitus after pancreas transplantation. Eur J Clin Invest. 1994;24:751–8.
Leitão CB, Tharavanij T, Cure P, Pileggi A, Baidal DA, Ricordi C, Alejandro R. Restoration of hypoglycemia awareness after islet transplantation. Diabetes Care. 2008;31(11):2113–5.
Paty BW, Ryan EA, Shapiro AM, Lakey JR, Robertson RP. Intrahepatic islet transplantation in type 1 diabetic patients does not restore hypoglycemic hormonal counterregulation or symptom recognition after insulin independence. Diabetes. 2002;51:3428–34.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this entry
Cite this entry
Alsahli, M., Gerich, J.E. (2017). Hypoglycemia in Diabetes Mellitus. In: Poretsky, L. (eds) Principles of Diabetes Mellitus. Springer, Cham. https://doi.org/10.1007/978-3-319-18741-9_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-18741-9_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-18740-2
Online ISBN: 978-3-319-18741-9
eBook Packages: MedicineReference Module Medicine