Abstract
In many clinical and biomechanical contexts of human motion analysis the model assumption of the foot as a single rigid segment is no longer acceptable. This has given rise to a large number of proposals for multi-segment foot models. The relevant experimental and analytical techniques differ for many aspects: the number of foot segments; the bony landmarks involved; the type of marker clusters; the definition of the anatomical frames; and the convention for the calculation of joint rotations. Different definitions of neutral reference posture have also been adopted, along with their utilization to offset kinematic data. Following previous partial review papers, the present chapter aims at introducing the current methodological studies for in vivo analysis of multi-segment foot kinematics. The survey has found more than 30 different techniques; however, only a limited number of these have reported convincing validation activities and have been exploited in a clinical context. A number of papers have also compared the experimental performance of different multi-segment foot models and highlighted the main advantages and disadvantages of each of them. Important biomechanical applications of musculoskeletal models for reliable estimation of biomechanical parameters are also discussed. In addition, we report on the feasibility and limitations of kinetic analysis applied to multi-segment foot models from ground reaction force data. The chapter ends with recommendations both for the selection of a most suitable technique from those already available, as well as for the design of an original one suitable to address the needs of the specific application.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Foot joint mobility
- 3D joint motion
- Multi-segment kinematics
- Ankle complex
- Chopart joint
- Lisfranc joint
- Metatarsophalangeal joint
- Foot arches
- Stereophotogrammetry
- Marker clusters
- Skin motion artifact
Introduction
In standard clinical gait analysis body segments are tracked in three-dimensions (3D) by a stereophotogrammetric system, while their relative positions are calculated to assess patterns of joint rotations during the execution of motor activities. Full-body gait analysis requires several passive reflective markers to be fixated to the trunk, pelvis, thigh, shank, and foot. Kinematics of segments are assessed with respect to the laboratory co-ordinate system, i.e., the absolute motion, and with respect to any adjoining segments for calculation of relative joint rotations. Frequently, motion of the trunk and pelvis is reported in the laboratory reference frame, in case with respect to the line of progression, together with hip, knee, and ankle joint motion. The moment of the external forces can also be calculated at these joints as the product of the joint center distance and the ground reaction force recorded by the force plate. Together with the spatiotemporal parameters (e.g., walking speed and stride length), these are the standard kinematic parameters necessary to assess, and characterize, most of the pathological conditions investigated in gait analysis. The use of skin-based reflective markers to track body segments comprised of single bones (e.g., the femur or the humerus) can result in a fairly accurate representation of their real motion. From a kinematic prospective, these segments can reasonably be assumed to move as rigid bodies, thus the position of at least three nonaligned points is required for their motion to be tracked in the 3D space. In gait analysis, these points are mostly palpable bony landmarks, the temporal position of which is tracked via reflective markers attached to the skin. With skin markers, however, the rigid body assumption is violated and accuracy is lower when multiple small bones are connected in a reduced volume (Nester et al. 2010). On the other hand, prospects to continuously track different segments are of particular relevance in the evaluation of pathologies regarding the shank and foot. Although the tibia and fibula bones present very small relative motion and thus can be considered reasonably as a single segment for kinematic analysis (Arndt et al. 2007), the foot is made up of 26 bones and several joints connecting them. Therefore, standard kinematic protocols based on three markers only appear inadequate in describing the complex foot biomechanics. In addition, foot bones are rather small and some of them, e.g., the talus, have no clear palpable landmarks, thus making it very difficult for those to be tracked in 3D space.
The importance of multi-segment foot models (MFMs) rather than single-segment foot tracking has been largely discussed in the literature. Benedetti et al. (2011) demonstrated the value of 3D motion analysis of the ankle joint in the clinical context. De Ridder et al. (2015) compared results from a MFM (“Ghent” in Table 1, by De Mits et al. 2012) and a single-segment foot model and showed the value of distal factors in chronic ankle instability, in particular the deviation in kinematics at the midfoot, which simply cannot be detected with a rigid foot model. Pothrat et al. (2015) reported significant differences and even opposite results for the same variables when the multi-segment Oxford Foot Model (OFM, see Table 2) and the Plug-in-Gait (modeling the foot as a single segment) were used to characterize normal and flat feet, concluding that the type of foot model strongly affects the measured ankle joint kinematics. Dixon et al. (2012) performed a similar study, i.e., OFM versus Plug-in-Gait albeit on kinetic data, and revealed that the latter overestimated ankle power by about 40% with respect to OFM and neglected the important midfoot loading. The authors of these papers shared the same recommendation of using caution when foot and ankle kinematics are measured with a single-segment foot model. Interestingly, the value of multi-segment foot kinematic analysis has been praised also in studies related to the analysis of more proximal lower limb joints (Arnold et al. 2014b). In 2003, a special technical session of the Gait and Clinical Movement Analysis Society (GCMAS) agreed on and recommended that shank, rearfoot, forefoot, and hallux are clinically meaningful foot segments to be tracked. These segments are in fact to be found in most of the multi-segment foot techniques reported in the literature.
Many basic foot biomechanic studies and clinical investigations employing various MFMs can be found in the literature. A number of relevant review papers have also been published, which represent valuable sources for an overview of foot modeling in kinematic analysis. Rankine et al. (2008) reported first a systematic analysis of 25 papers on foot kinematic modeling, thoroughly classified in terms of number of bony segments and joint rotations. All major technical and exploitation related issues were discussed systematically. Later, Deschamps et al. (2011) reported and assessed many of these techniques in relation to their exploitation in the clinical context. It was shown that whereas many foot joint rotations can be tracked in a consistent and repeatable way, some measures are still critical, and several of these techniques have yet to be used to address clinical problems. According to Bishop et al. (2012) this is the consequence of poorly described or flawed methodologies, preventing the readers from obtaining the same algorithms and programs to replicate the analysis. A minimum of five reporting standards were proposed in this paper; this aimed at guaranteeing full access to the most relevant modeling concepts and at providing a common platform for sharing and comparing foot kinematic data and as to improve their interpretation and usability. The association between foot posture and lower limb kinematics has been the objective of another interesting review analysis of twelve papers (Buldt et al. 2013). Evidence was found for increased frontal plane motion of the rearfoot during walking in individuals with pes planus. The latest review thus far by Novak et al. (2014) has highlighted the strengths and weaknesses of the most widely used and known MFMs, including an insight on their kinetic analyses.
While joint rotations have been thoroughly addressed in the literature, joint translations have been studied and discussed very rarely: generally these are within 2 mm (Bruening et al. 2012a) in any anatomical direction. Because this is in the order of magnitude of skin motion artifact, this topic would not be further discussed in this chapter. For foot joint kinematics reconstruction, also the so-called “global optimization” has been used recently (Arnold et al. 2013; Bishop et al. 2016). This basically entails with an iterative search of the best estimation of foot segment position and orientation, all together also called “pose”. This procedure starts from skin marker trajectories, but the optimal poses must be compatible also with predetermined kinematic models for all the joints, i.e. global, this according to an original technique for the lower limbs (Lu and O’Connor 1999).
The present chapter aims at introducing the current full series of methodological studies on this topic, in order to provide the basic knowledge for either the selection or the design of the most appropriate technique, according to the specific populations and hypotheses of the foot kinematic study to be performed.
State of the Art
An extensive survey of the currently available multi-segment foot techniques and models is reported in Table 1. Several differences can be found between multi-segment foot techniques in the following factors:
-
Foot segments
-
Bony landmarks
-
Type of marker clusters
-
Definition of the anatomical frames
-
Joint convention – including 2D versus 3D measurements
-
Neutral reference posture
-
Offsets
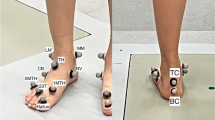
The major difference between MFMs is found in the number and selection of foot segments (Fig. 1). While tibia, rearfoot, and forefoot are tracked by most techniques, the hallux – or the first metatarso-phalangeal joint – is seldom tracked, and the midfoot is tracked only by few models (MacWilliams et al. 2003; Leardini et al. 2007; Rouhani et al. 2011; Portinaro et al. 2014). Medial and lateral forefoot subdivisions have also been proposed (MacWilliams et al. 2003; Hwang et al. 2004; Buczek et al. 2006; Rouhani et al. 2011). The current models available include up to 12 segments (Table 1); even a 26 segment foot model has been proposed (Oosterwaal et al. 2011, 2016), but its application is limited to advanced musculoskeletal modeling studies. The number and selection of foot segments to be tracked, somehow the resolution of the model, is usually defined according to the field of application, the clinical interest (Table 2), but also to the number, quality, and location of available cameras of the stereophotogrammetric system. While kinematic analysis of foot segments has been devised mostly for barefoot gait analysis, a number of techniques were explicitly designed for the analysis of shod feet (Wolf et al. 2008b; Cobb et al. 2009; Shultz et al. 2011b; Bishop et al. 2013). Moreover, the effect of foot and ankle orthoses has been investigated by established models (Lin et al. 2013; Leardini et al. 2014). The overall results, in terms of patterns of foot joint kinematics, can be confusing and difficult to interpret because of the differences mentioned above. Also, the varying populations analyzed, as highlighted in Table 2, in terms also of physical status, size, age, gender, etc., make it difficult to compare data across different studies.
The process to include and track a segment within a MFM for kinematic analysis requires a profound knowledge of foot biomechanics and of the limits and accuracy of the measuring system. For example, the actual joint motion to be recorded should be much larger than the accuracy of the stereophotogrammetric instrumentation used for the analysis and than any other source of error (particularly, the skin motion artifact). In addition to the known large rotations occurring at the tibiotalar and metatarso-phalangeal joints, and between metatarsus and calcaneus, in vivo and in vitro studies have demonstrated that significant and consistent rotations are experienced in normal feet also at the Chopart (talo-calcaneo-navicular and calcaneo-cuboid joints) and Lisfranc joints (tarso-metatarsal joints). These studies have confirmed that midfoot motion during gait is significant and its assessment should be included in relevant foot kinematic studies. The subtalar joint is also subjected to relatively large motion; however, this is very difficult to track in vivo with skin-based markers.
Both skin-based and plate-mounted marker clusters (Leardini et al. 1999; Carson et al. 2001; Houck et al. 2006; Hyslop et al. 2010; Nester et al. 2014; Raychoudhury et al. 2014; Souza et al. 2014; Buldt et al. 2015) on relevant foot and shank bony landmarks have been used to track foot segments. The differences between skin-markers and plate-mounted markers in measured joint motion were found to be small (Nester et al. 2007a). The markers used for motion analysis are usually passive, i.e., reflecting IR (infrared) light emitted by LEDS embedded in the motion cameras, or active, i.e., emitting IR light. While the latter usually provide a more accurate 3D location, they also require a wired external power which can result in uncomfortable setups also restraining the movement of the subject. The number of markers used in MFM can be as high as 35, as in Oosterwaal et al. (2011, 2016) and Raychoudhury et al. (2014). A compromise must always be found between the required degrees of freedom of the model, which is related also to the number of segments tracked in 2D or 3D, and the number, quality, and location of the available cameras. These are arranged usually to collect motion data for other anatomical districts and motor tasks in the same laboratory, and therefore compromising layouts must be found, as explicitly discussed for one widely used MFM (Leardini et al. 2007).
As mentioned above, at least three markers need to be fixated to each segment for a complete 3D representation of its motion. This setup is technically suitable for establishing a local reference frame on each segment and for calculation of triplanar joint rotations using the Euler or the Joint-Coordinate-System convention (Grood and Suntay 1983) (see typical results in Fig. 2). Anatomical landmarks are necessary to establish anatomical based reference frames. However, the paucity of bony landmarks and the small size of several foot bones limit the application of the three-marker tracking for foot segments kinematics. While most techniques for the kinematic analysis of foot segments use the 3D approach, i.e., three independent rotations about three different axes, 2D projection angles can also be used to measure relative rotations of a joint, with respect to anatomical planes. In the latter, line segments determined by the position of two markers are projected at each time sample onto an anatomical or other relevant planes, for the planar rotation to be calculated during motion (Simon et al. 2006; Leardini et al. 2007; Portinaro et al. 2014). 2D planar angles have been largely used to track motion of metatarsal bones, as well as for motion representations of the arches of the foot, particularly the medial longitudinal arch, and the varus/valgus inclination of the calcaneus. With this approach, however, very erroneous and misleading values can be obtained in extreme conditions, particularly in case of large ranges of joint motion and in case of large deviations between the line segment and the projection plane.
Typical mean (± one standard deviation) temporal profiles of foot joint rotations over the full gait cycle from a control population of normal subjects. In the left and right columns, respectively: motion of the calcaneus in the shank reference frame and of the metatarsals in the calcaneus reference frame. From top to bottom rows: rotations in the sagittal, frontal, and transverse anatomical planes
Another important question is whether to use a reference neutral position for the foot and ankle joints. Most frequently, a double leg standing posture is recorded to provide reference orientations of the foot and lower limb segments. The neutral orientation can be used as offset and subtracted from the corresponding temporal profile of joint rotation. The so-called “subtalar neutral” is also sought (Rao et al. 2009) to establish the correct initial alignment of the foot and ankle. Plaster molds have also been exploited to control the foot resting position (Saraswat et al. 2012, 2013), ensuring foot placement reproducibility and segment neutral orientation. This procedure is intended to compensate for differing anatomical frame definitions and foot static deformities, in order to establish a common “zero reference level” for inter-subject comparisons. The use of a neutral posture has the advantage of removing the bias associated to the anatomical frame definitions, thus allowing to focus the analysis and all relevant measurements on the “dynamic” pattern of the joint rotations. Unfortunately, it also removes any joint misalignments due to bone and/or joint deformity, which are frequently included in the clinical evidence of each patient and therefore should not be removed from the analysis. The choice of offsetting joint rotations by using a neutral posture is thus related to the specific study and its hypotheses and should take into consideration, for example, if there is any ongoing treatment to correct a foot deformity. Regardless of its application to offset the kinematic data, the inter-segmental orientations with the subject in the neutral posture represent extremely valuable information that should always be analyzed and assessed, in relation to the corresponding temporal profiles of joint rotations.
In order to help final users to identify which MFM is more reliable, repeatable, and/or best fitting the aims of their investigation, few studies have been published which compare the performance of the most popular MFM. Mahaffey et al. (2013) have used intra-class correlation coefficients to analyze the OFM, the Rizzoli Foot Model (RFM), and the Kinfoot (MacWilliams et al. 2003) in 17 children on two testing sessions. Although some variability has been found between segments, multi-segment foot kinematics were shown to be quite repeatable even in pediatric feet. A standard error of measurement greater than 5° was found in 26%, 15%, and 44% of the kinematic parameters, respectively, for the OFM, RFM, and the Kinfoot model. The latter showed the lowest repeatability and the highest errors. The OFM demonstrated moderate repeatability and reasonable errors in all segments except for the hindfoot in the transverse plane. The RFM resulted in moderate repeatability and reasonable test-retest error similar to that of the OFM, but with original additional data also on midfoot kinematics. In another paper by Powell et al. (2013), the OFM and RFM were assessed in the context of foot function and alignment as possible predisposition factors for overuse and traumatic injury in athletes. Both models helped detect significant differences in frontal plane motion between high- and low-arched footed athletes. However, the RFM was suggested to be the more appropriate because it allows to track also midfoot motion. While it was not the main scope of the study, a comparison between the Shriners Hospital for Children Greenville Foot Model (Davis et al. 2006) and the OFM can be found also in Maurer et al. (2013). The former model was shown to be more effective in quantifying the presence and severity of midfoot break deformity in the sagittal plane and in monitoring the progression over time. Di Marco et al. (2015a, b) performed the most comprehensive comparative analysis to date of the OFM, RFM, the Sawacha et al. (2009), and Saraswat et al. (2012) models. The best coefficient of multiple correlation between-sessions of the kinematic parameters during ground and treadmill walking was observed for the RFM (range 0.83–0.95).
Perhaps an overabundance of multi-segment foot techniques and models has been proposed to date. Some of these have been made available to the motion analysis community also via simple-to-use software codes. New users are free to choose the most appropriate model/technique for their needs according to the experimental conditions. In particular, the visibility and traceability of the relevant markers must be considered, both in relation to their dimension and location, together with its applicability on the clinical population under investigation, and to the motor activities to be analyzed. Moreover, foot and leg deformities should be carefully assessed before starting the data collection campaign. The advantages and disadvantages of existing techniques should be considered and analyzed before developing and validating a novel MFM suitable to the aims of the investigation.
Validation and Application of Foot Models
Validation Studies
New motion analysis procedures always require proper validation, but this is particularly challenging for the kinematic analysis of foot segments via skin-markers. Usually, MFMs are only assessed for repeatability of measurements (see Table 1) (Mahaffey et al. 2013; Di Marco et al. 2015a, b). Videofluoroscopy has been employed to estimate the error in the measurements due to the skin motion artifacts (Leardini et al. 2005; Wrbaskić and Dowling 2007; Shultz et al. 2011a). Skin motion artifacts were shown to be as large as 16 mm in very strenuous foot conditions. The largest errors were measured in the hindfoot and midfoot clusters at toe-off, likely because of the large deformations experienced by the foot bones and skin in this phase of stance. Still, the skin-to-bone relative motion at the foot was found to be smaller than that of typical markers on the shank and thigh (Leardini et al. 2005), thus it has been deemed sufficiently reliable for foot bone tracking. However, the most convincing evidence of skeletal motion is from in-vitro and in-vivo bone pins measurements. In vitro, robotic gait simulators are used to replicate the biomechanical conditions of the stance phase of walking on foot cadaver specimens (Whittaker et al. 2011; Peeters et al. 2013), and kinematics of foot bones can be accurately tracked via bone pins instrumented with markers. This data helped verify a promising consistency in foot joint kinematic patterns, for most of the foot joints, between skin-markers and bone pin measurements. Moreover, it has been possible to detect motion in a number of joints that are difficult to analyze in-vivo. In-vitro kinematic data should always be critically evaluated in relation to the fidelity of the replication of the real in-vivo conditions.
Validation of MFMs has been performed also by tracking real bone motion in-vivo (Nester et al. 2007a, b, 2010; Arndt et al. 2007; Lundgren et al. 2008; Wolf et al. 2008a; Okita et al. 2009). This required bone pins to be instrumented with marker clusters and fixated to a number of foot segments in volunteers under a small dose of local anesthesia. In this condition, the motion pattern of the main foot joints during walking and running can be established very accurately. It has been shown that the motion patterns with and without the inserted pins compare well, indicating that the subjects had little motion restriction due to such invasive intervention. Motion of major joints was revealed to be very complex, and that of small joints, such as the talo-navicular, to be larger than what expected – about 10° in the three anatomical planes – and also larger than that of the talo-calcaneal joint. Motion larger than 3°, therefore non negligible, was also measured between tibia and fibula. These studies also showed the kinematic differences between multibone segments, as measured by external skin clusters, and single bone pins. These experiments are limited by the small number of subjects and are hardly replicable for technical and ethical reasons. The relevant data published so far must serve as reference for other investigations on normal and pathological feet.
Musculoskeletal Multi-Segment Foot Modeling
MFMs can be used also to develop and validate complex musculoskeletal computer models for forward and inverse dynamic analysis. Typically, medical imaging is used to define geometrical models of the anatomical structures and in vivo recorded kinematics, whereas ground reaction forces provide the data to perform inverse-dynamics. This allows measurement of bone segment kinematics and estimes of loading conditions, at the joints, muscle-tendon units, and ligaments. These models are particularly valuable for an insight into pathological conditions, understanding disease mechanisms, and simulating the effects of possible treatments, whether surgical, pharmacological or physical. Saraswat et al. (2010) proposed a generic musculoskeletal model of an adult foot, including the intrinsic muscles and ligaments of the foot and ankle, configured and scaled by skin marker trajectories and an optimization routine. The predicted muscle activation patterns were assessed against corresponding EMG measurements from the literature. It was shown that small marker placement error may result in large differences in model outcomes. Another large investigation (Oosterwaal et al. 2011, 2016) has proposed a more complex musculoskeletal model which implies 26 segments and 26 idealized joints, either cylindrical, universal, or spherical, for a total of 39 degrees of freedom. The model geometry can be customized using CT and MRI data, and dynamic simulations can be performed by using bone kinematic data from the 34 skin markers. Both forward and inverse dynamic modeling were claimed to be exploitable, with the former integrating a multibody approach with FE analysis and the latter allowing to describe the interactions of the musculoskeletal structures. Computer models designed to estimate the mechanics of single structures in the foot, which can hardly be measured non invasively have also been developed and reported. One of these models has allowed to estimate the effect of walking speed on the tension in the plantar aponeurosis (Caravaggi et al. 2010).
A most recent study has exploited the modified OFM to develop a method for configuring personalized foot models to patients suffering of juvenile idiopathic arthritis (Prinold et al. 2016). This has highlighted the criticality of patient-specific definition of the ankle joint axes and the location of the Achilles tendon insertions. These models have great potential for the analysis of loading conditions in healthy and pathological feet, and is beneficial to predicting the effects, and thus improving the efficacy, of surgical treatments and foot and ankle orthoses. However: (a) the relevant data sets are hardly available or difficult to create, with real personalization nearly impossible; (b) the mechanical parameters of soft tissues (ligaments, tendons, retinacula, etc.) are difficult to attain and not fully available in the literature; (c) the external (so-called “boundary”) conditions depend on many factors not all measurable; and (d) the collection of relevant marker trajectories is demanding and requires a cameras setup with special arrangements. Confidence in interpretation diminishes because of the many unknowns and the relevant assumptions, optimization criteria, conventions, calculations, etc. The final concern is about validation, which is difficult to obtain for these bulky computational models.
Kinetic Analysis Including Foot Models
The moment and power at the ankle joint have been reported extensively in standard gait analysis with traditional single-segment foot models. However, MFMs offer specific insight also into muscle performance which would enlighten their function, particularly in physiological and pathological conditions. This assessment must take advantage of foot joint kinetics, where ground reaction force and joint center location are combined to obtain joint moment, work, and power. A number of studies (Dixon et al. 2012; MacWilliams et al. 2003) have demonstrated that the contribution of the midfoot to the overall power is important for forward propulsion during gait; power generation at rearfoot would instead be overestimated by a single-segment foot model. Detection of abnormal kinetic patterns, even prior to significant worsening of the prognosis, may help with the formulation of early specific interventions, aimed at reducing the progression of deformity and disability (DiLiberto et al. 2015).
In kinetic analysis, in addition to meaningful references associated to the segments of interest, the complete ground reaction forces, comprising normal and shear components, must be measured. The inertial properties of segments and the location of joint centers must also be determined. The latter is particularly critical at the Chopart and Lisfranc joints, but also at the metatarso-phalangeal joints since these encompass a number of anatomical articulations. Usually additional virtual points are defined on these joint lines, however these do not precisely represent the exact position of anatomical elements. Several attempts have been made to determine an optimum suitable technique for measuring reaction forces under each segment, i.e., subarea ground reaction. In order to estimate these regional forces, a miniature force platform, requiring the superposition of many targeted trials to create a full analysis (Scott and Winter 1991), and combined pressure and force plates with assumptions of proportionality between the two (Giacomozzi and Macellari 1997; MacWilliams et al. 2003; Giacomozzi et al. 2006) have been proposed.
Early kinetic measures of the foot (Scott and Winter 1991; MacWilliams et al. 2003) have been limited by intricate assumptions and equipment restrictions. The former was an 2D eight-joint model and relied on the superposition of multiple trials interacting with a small custom-built force sensor. The latter paper proposed a first 3D model with eight segments but implied many assumptions on joint motion, pressure, as well as force data for a final estimation of joint moments, which neglected the mediolateral component of the force. A theoretical extension of the MacWilliams model, addressing kinetic-based calculations, has been proposed a little later (Buczek et al. 2006).
An extensive investigation undergone in a clinical and research setting (Bruening et al. 2012a, b), involving respectively 17 and 10 healthy pediatric subjects, explicitly aimed at exploiting the feasibility and relevance of a proposed technique for kinetic analysis applied to a MFM. A three-segment kinetic model was first characterized and assessed. In the second paper, kinetic parameters, joint moments and powers during level walking were reported. Three submodels of the shank and foot complex were created and two adjacent force platforms employed for calculation of rotation, net moment, and total power at the ankle, midtarsal, and 1st metatarso-phalangeal joints. Unfortunately, the protocol required visual targeting of the force platforms, whose confounding contribution, together with that of the inertial parameters, was assessed separately. The study confirmed that not only sagittal plane motion but also generated peak power are generally overestimated at the ankle (35% on average) when using a single-segment, rather than a MFM. This “split force platform approach” can be an alternative to ad-hoc hardware, but it is critical when applied to pathological populations for the special targeting of the force plates.
DiLiberto et al. (2015) have reported, for the first time, multi-joint foot kinetics in subjects with diabetes mellitus, peripheral neuropathy, and in a healthy adult control group, by using an electromagnetic sensor motion capture system. The model consisted of the tibia, rearfoot, and forefoot, with ideal hinge joints connecting the segments. It has been shown that (i) positive peak power and work of the forefoot with respect to rearfoot was smaller in the patients group with respect to the control, (ii) negative peak powers of both the forefoot to rearfoot and rearfoot to tibia was larger, and (iii) a greater proportion of negative work was present at both these joints.
While, the value of joint kinematics from MFMs has been repeatedly demonstrated, relevant joint kinetics are still controversial because motion occurs at multiple articulations between bony segments (Nester et al. 2007a), particularly for the critical estimation of position and orientation of the axes of rotation, which would significantly affect kinetic measurements.
It is no doubt that kinetic measurements can increase the knowledge of foot and ankle function, as well as influence the evolution of MFMs. Though some preliminary attempts in this direction might have been too complex (Wang et al. 2016), the currently available simple representations here discussed seem a good compromise between comprehensiveness of foot kinetics and comprehension of the results for clinical use. These techniques, however, are hardly exploitable by the large scientific community, due to the modeling and the implementation issues.
Summary
Stereophotogrammetry has made enormous progress in the last few years, with cheaper motion analysis systems achieving high performance in markers tracking. Today, multi-segment foot kinematic analysis is easier than what it was years ago. A large number of multi-segment foot techniques for in vivo gait analysis based on stereophotogrammetric systems have been published over the last three decades. The large variety of currently available marker sets and protocols is of great value for anyone interested in the analysis of foot motion in normal or pathological conditions, following treatments, in the evaluation of sport performance, etc. Following this long survey of the current techniques for kinematic analysis of foot segments, the reader interested in the application of an existing MFM, or in the design of a new one suitable to the aims of his/her specific investigation, shall find valuable recommendations for either options here below.
In case of selection of an existing MFM, the researcher must be careful in deciding on the most appropriate model from the literature; this must be done according to the number of segments and degrees of freedom, the technique used for the calculation of joint rotations, the position and visibility of the markers, etc. As far as the latter, the number of cameras and their positions should be checked against the motor tasks analyzed. Using a camera setup closer to the acquisition volume, and better optics, normally will result in a better quality of the measurements. However, the cameras are often arranged for full body gait analysis, and the necessary frequent changes in the cameras configuration can be a tedious operation requiring repeated calibrations. The consistency with existing single-segment foot and lower limb models should also be discussed with the motion analysis team. First of all the user must comprehend which segments should be tracked for the study, thus excluding unnecessarily complex marker sets. Another important decision regards the reference neutral orientation and whether this shall be used as an off-set to compensate for anatomical frame definitions and foot deformities. As already stated above, the decision should be taken according to the scope of the study and the population analyzed. Relevant literature supporting the model should also be sought, in particular in relation to the repeatability of measurements and the validation against gold standards. Calculation and analysis of foot joint rotations can be supported by commercial software or freeware. While this allows users to save time and resources in writing ad-hoc analysis programs, the consistency of the calculations should always be assessed against corresponding data published by the authors. Unfortunately, many papers do not provide complete instructions on exact marker mounting, marker trajectory smoothing, anatomical frame definition, joint conventions, etc. (Bishop et al. 2012); even small changes to the original definitions may affect the final measurements. The involvement of experienced operators is therefore recommended, and a program of continuous training activities should be implemented. Software tools which have been developed and/or verified by the original model designers are preferable.
In case it is required to design new specific models, a consistent and careful identification of specific single or combined bony segments, which are originally tracked according to the aims of the study, must be performed. From a theoretical perspective, an extremely large number of models can be devised and formalized simply by mixing and matching the 26 foot bones. As long as a reference system is clearly defined and a sufficient number of markers can be fixated to each segment, the model can be considered original and reproducible. However, many of the papers reported here have failed to properly describe the relevant details of the model, including origin and orientation of the reference frames. Moreover, some of these allegedly novel MFMs are merely a subset or small variations of previously existing models, whereby a fewer number of segments has been tracked and/or only minor modifications to the location of the markers have been implemented. In this respect, we recommend that for a new, in vivo multi-segment technique for kinematic analysis of the foot to be considered as a novel model, the following criteria should be followed:
-
(1)
The rationale for proposing a new segmentation of the foot for kinematic analysis should be explicit and clear, e.g., for biomechanical or clinical purposes. The authors should be able to address the question: why any of the existing MFMs is not appropriate to address the aims of my study?
-
(2)
The description of the new model should be exhaustive as far as the following information: foot segments; relevant anatomical landmarks; position and orientation of the local reference co-ordinate system; and number and location of the skin markers for motion tracking.
-
(3)
A validation study should be performed – possibly by a different research group – to demonstrate that the repeatability of the kinematic outcome is comparable or better than that of the current most common and widely used foot models.
-
(4)
At least one clinical or biomechanical application of the model should be reported to demonstrate the value and efficacy of the new model.
If the proposed criteria were strictly followed, only a few of the foot segmentation techniques found in the literature and here reported could be considered as appropriate MFMs. In fact, even following these criteria would not necessarily guarantee the new model to become popular in everyday gait analyses and to be widely used. Many other factors influence the “popularity” and diffusion of gait analysis protocols in the scientific and clinical contexts, such as their comprehension (as far as the basic concepts, its application, the data processing and reporting), their usability and utility, the availability of relevant processing software, the support provided by the inventors, the distribution and actions of motion capture systems vendors, etc. The scientific community of human motion analysis would however be pleased to welcome any such robust contribution in the discipline.
Future Directions
While foot kinematics can now be described with multiple degrees of freedom foot models, a number of issues still remain to be addressed in the future, particularly for in vivo studies. The complex procedures for validation of the models and the unavoidable bias from the soft tissue artifacts are known to affect these measures (Leardini et al. 2005). Nevertheless single or plate-mounted skin markers are necessary, the alternatives in routine clinical analyses having several limitations. While videofluoroscopy and bone pins provide more accurate measures of foot joints motion, these are also excessively invasive for patients. Inertial sensors (Rouhani et al. 2012, 2014) and marker-less dynamic 3D scanning (Van den Herrewegen et al. 2014) are definitely less invasive, but accuracy and anatomical based analysis fall short.
Due to the variety of motion analysis systems and protocols for data acquisition, a normative database for foot kinematic data should be available in every single gait analysis facility (Deschamps et al. 2012a). Moreover, kinematic analysis of foot joints is highly sensitive to errors in marker placement due to the small size of foot bones in comparison to other body segments. Even a small deviation from the recommended marker location can result in a large error within the position and orientation of the reference co-ordinate system. In order to decrease the error rate and improve the protocol repeatability, only experienced operators with extensive knowledge of foot anatomy and practice in multi-segment foot analysis should be in charge of mounting the markers (Caravaggi et al. 2011; Deschamps et al. 2012a).
To ensure for an increased and coherent use of these techniques, standardization of the references shall be sought, in terms of anatomical landmark and frame definitions. In this respect, another fundamental step forward would imply establishing a common terminology, which can avoid confusion and inconsistency. The utilization of these models is still critical in the presence of shoes or foot orthotics (Lin et al. 2013; Bishop et al. 2013; Leardini et al. 2014; Bishop et al. 2015; Halstead et al. 2016), hence the limitation of available literature currently. All these issues perhaps can account for the limited number of relevant clinical applications (Deschamps et al. 2011).
Cross-References
-
Integration of Foot Pressure and Foot Kinematics Measurements for Medical Applications
-
Interpreting Spatiotemporal Parameters, Symmetry, and Variability in Clinical Gait Analysis
-
Three-Dimensional Human Kinematic Estimation Using Magneto-Inertial Measurement Units
-
Three-Dimensional Reconstruction of the Human Skeleton in Motion
-
Variations of Marker Sets and Models for Standard Gait Analysis
References
Alonso-Vázquez A, Villarroya MA, Franco MA, Asín J, Calvo B (2009) Kinematic assessment of paediatric forefoot varus. Gait Posture 29(2):214–219
Arampatzis A, Brüggemann GP, Klapsing GM (2002) A three-dimensional shank-foot model to determine the foot motion during landings. Med Sci Sports Exerc 34(1):130–138
Arndt A, Wolf P, Liu A, Nester C, Stacoff A, Jones R, Lundgren P, Lundberg A (2007) Intrinsic foot kinematics measured in vivo during the stance phase of slow running. J Biomech 40(12):2672–2678
Arnold JB, Mackintosh S, Jones S, Thewlis D (2013) Repeatability of stance phase kinematics from a multi-segment foot model in people aged 50 years and older. Gait Posture 38(2):349–351
Arnold JB, Mackintosh S, Jones S, Thewlis D (2014a) Differences in foot kinematics between young and older adults during walking. Gait Posture 39(2):689–694
Arnold J, Mackintosh S, Jones S, Thewlis D (2014b) Altered dynamic foot kinematics in people with medial knee osteoarthritis during walking: a cross-sectional study. Knee 21(6):1101–1106
Atkinson HD, Daniels TR, Klejman S, Pinsker E, Houck JR, Singer S (2010) Pre- and post-operative gait analysis following conversion of tibiotalocalcaneal fusion to total ankle arthroplasty. Foot Ankle Int 31(10):927–932
Barton CJ, Levinger P, Crossley KM, Webster KE, Menz HB (2011a) Relationships between the Foot Posture Index and foot kinematics during gait in individuals with and without patellofemoral pain syndrome. J Foot Ankle Res 4:10
Barton CJ, Levinger P, Webster KE, Menz HB (2011b) Walking kinematics in individuals with patellofemoral pain syndrome: a case–control study. Gait Posture 33(2):286–289
Barton CJ, Menz HB, Levinger P, Webster KE, Crossley KM (2011c) Greater peak rearfoot eversion predicts foot orthoses efficacy in individuals with patellofemoral pain syndrome. Br J Sports Med 5(9):697–701
Benedetti MG, Manca M, Ferraresi G, Boschi M, Leardini A (2011) A new protocol for 3D assessment of foot during gait: application on patients with equinovarus foot. Clin Biomech 26(10):1033–1038
Bishop C, Paul G, Thewlis D (2012) Recommendations for the reporting of foot and ankle models. J Biomech 45(13):2185–2194
Bishop C, Paul G, Thewlis D (2013) The reliability, accuracy and minimal detectable difference of a multi-segment kinematic model of the foot-shoe complex. Gait Posture 37(4):552–557
Bishop C, Arnold JB, Fraysse F, Thewlis D (2015) A method to investigate the effect of shoe-hole size on surface marker movement when describing in-shoe joint kinematics using a multi-segment foot model. Gait Posture 41(1):295–299
Bishop C, Arnold JB, May T (2016) Effects of taping and orthoses on foot biomechanics in adults with flat arched feet. Med Sci Sports Exerc 48(4):689–696
Brodsky JW, Charlick DA, Coleman SC, Pollo FE, Royer CT (2009) Hindfoot motion following reconstruction for posterior tibial tendon dysfunction. Foot Ankle Int 30(7):613–618
Bruening DA, Cooney KM, Buczek FL (2012a) Analysis of a kinetic multi-segment foot model. Part I: model repeatability and kinematic validity. Gait Posture 35(4):529–534
Bruening DA, Cooney KM, Buczek FL (2012b) Analysis of a kinetic multi-segment foot model. Part II: kinetics and clinical implications. Gait Posture 35(4):535–540
Buczek FL, Walker MR, Rainbow MJ, Cooney KM, Sanders JO (2006) Impact of mediolateral segmentation on a multi-segment foot model. Gait Posture 23(4):519–522
Buldt AK, Murley GS, Butterworth P, Levinger P, Menz HB, Landorf KB (2013) The relationship between foot posture and lower limb kinematics during walking: a systematic review. Gait Posture 38(3):363–372
Buldt AK, Levinger P, Murley GS, Menz HB, Nester CJ, Landorf KB (2015) Foot posture is associated with kinematics of the foot during gait: a comparison of normal, planus and cavus feet. Gait Posture 42(1):42–48
Canseco K, Long J, Marks R, Khazzam M, Harris G (2008) Quantitative characterization of gait kinematics in patients with hallux rigidus using the Milwaukee foot model. J Orthop Res 26(4):419–427
Canseco K, Long J, Marks R, Khazzam M, Harris G (2009) Quantitative motion analysis in patients with hallux rigidus before and after cheilectomy. J Orthop Res 7(1):128–134
Canseco K, Long J, Smedberg T, Tarima S, Marks RM, Harris GF (2012) Multisegmental foot and ankle motion analysis after hallux valgus surgery. Foot Ankle Int 33(2):141–147
Caravaggi P, Pataky T, Gunther M et al (2010) Dynamics of longitudinal arch support in relation to walking speed: contribution of the plantar aponeurosis. J Anat 217:254–261
Caravaggi P, Benedetti MG, Berti L, Leardini A (2011) Repeatability of a multi-segment foot protocol in adult subjects. Gait Posture 33(1):133–135
Carson MC, Harrington ME, Thompson N, O’Connor JJ, Theologis TN (2001) Kinematic analysis of a multi-segment foot model for research and clinical applications: a repeatability analysis. J Biomech 34(10):1299–1307
Carty CP, Walsh HP, Gillett JG (2015) Sensitivity of the Oxford foot model to marker misplacement: a systematic single-case investigation. Gait Posture 42(3):398–401
Chang R, Van Emmerik R, Hamill J (2008) Quantifying rearfoot-forefoot coordination in human walking. J Biomech 41(14):3101–3105
Chang R, Rodrigues PA, Van Emmerik RE, Hamill J (2014) Multi-segment foot kinematics and ground reaction forces during gait of individuals with plantar fasciitis. J Biomech 47(11):2571–2577
Cobb SC, Tis LL, Johnson JT, Wang YT, Geil MD, McCarty FA (2009) The effect of low-mobile foot posture on multi-segment medial foot model gait kinematics. Gait Posture 30(3):334–339
Cornwall MW, McPoil TG (1999a) Effect of ankle dorsiflexion range of motion on rearfoot motion during walking. J Am Podiatr Med Assoc 89(6):272–277
Cornwall MW, McPoil TG (1999b) Three-dimensional movement of the foot during the stance phase of walking. J Am Podiatr Med Assoc 89(2):56–66
Cornwall MW, McPoil TG (2002) Motion of the calcaneus, navicular, and first metatarsal during the stance phase of walking. J Am Podiatr Med Assoc 92(2):67–76
Curtis DJ, Bencke J, Stebbins JA, Stansfield B (2009) Intra-rater repeatability of the Oxford foot model in healthy children in different stages of the foot roll over process during gait. Gait Posture 30(1):118–121
Davis RB, Eugene G, Jameson E, Davids JR, Christopher LM, Benjamin M, Rogozinski B, Anderson JP (2008) The design, development, and initial evaluation of a multi-segment foot model for routine clinical gait analysis. In: Harris GF, Smith PA, Marks RM (eds) Foot and ankle motion analysis: clinical treatment and technology. CRC Press, Taylor and Francis Group, pp 425–444
De Mits S, Segers V, Woodburn J, Elewaut D, De Clercq D, Roosen P (2012) A clinically applicable six-segmented foot model. J Orthop Res 30(4):655–661
De Ridder R, Willems T, Vanrenterghem J, Robinson MA, Palmans T, Roosen P (2015) Multi-segment foot landing kinematics in subjects with chronic ankle instability. Clin Biomech 30(6):585–592
Deschamps K, Birch I, Desloovere K, Matricali GA (2010) The impact of hallux valgus on foot kinematics: a cross-sectional, comparative study. Gait Posture 32(1):102–106
Deschamps K, Staes F, Roosen P, Nobels F, Desloovere K, Bruyninckx H, Matricali GA (2011) Body of evidence supporting the clinical use of 3D multi-segment foot models: a systematic review. Gait Posture 33(3):338–349
Deschamps K, Staes F, Bruyninckx H, Busschots E, Jaspers E, Atre A, Desloovere K (2012a) Repeatability in the assessment of multi-segment foot kinematics. Gait Posture 35(2):255–260
Deschamps K, Staes F, Bruyninckx H, Busschots E, Matricali GA, Spaepen P, Meyer C, Desloovere K (2012b) Repeatability of a 3D multi-segment foot model protocol in presence of foot deformities. Gait Posture 36(3):635–638
Deschamps K, Matricali GA, Roosen P, Nobels F, Tits J, Desloovere K, Bruyninckx H, Flour M, Deleu PA, Verhoeven W, Staes F (2013) Comparison of foot segmental mobility and coupling during gait between patients with diabetes mellitus with and without neuropathy and adults without diabetes. Clin Biomech 28(7):813–819
Deschamps K, Dingenen B, Pans F, Van Bavel I, Matricali GA, Staes F (2016) Effect of taping on foot kinematics in persons with chronic ankle instability. J Sci Med Sport 19(7):541–546
Di Marco R, Rossi S, Racic V, Cappa P, Mazzà C (2015a) A comparison between four foot model protocols: the effect of walking on a treadmill. Conference paper 2015: XXV congress of the international society of biomechanics, Glasgow
Di Marco R, Rossi S, Racic V, Cappa P, Mazzà C (2015b) Concurrent reliability assessment of four foot models for gait analysis. Conference paper 2016: XVI congress of the Società Italiana di Analisi del Movimento in Clinica, Padova
DiLiberto FE, Tome J, Baumhauer JF, Quinn JR, Houck J, Nawoczenski DA (2015) Multi-joint foot kinetics during walking in people with diabetes mellitus and peripheral neuropathy. J Biomech 48(13):3679–3684
Dixon PC, Böhm H, Döderlein L (2012) Ankle and midfoot kinetics during normal gait: a multi-segment approach. J Biomech 45(6):1011–1016
Dubbeldam R, Nester C, Nene A, Hermens H, Buurke J (2013) Kinematic coupling relationships exist between non-adjacent segments of the foot and ankle of healthy subjects. Gait Posture 37:159–164
Giacomozzi C, Macellari V (1997) Piezo-dynamometric platform for a more complete analysis of foot-to-floor interaction. IEEE Trans Rehabil Eng 5(4):322–330
Giacomozzi C, Benedetti MG, Leardini A, Macellari V, Giannini S (2006) Gait analysis with an integrated system for functional assessment of talocalcaneal coalition. J Am Podiatr Med Assoc 96(2):107–115
Graff A, Hassani S, Krzak J, Long J, Caudill A, Flanagan A, Eastwood D, Kuo KN, Harris G, Smith P (2010) Long-term outcome evaluation in young adults following clubfoot surgical release. J Pediatr Orthop 30(4):379–385
Grood ES, Suntay WJ (1983) A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 105(2):136–144
Halstead J, Keenan AM, Chapman GJ, Redmond AC (2016) The feasibility of a modified shoe for multi-segment foot motion analysis: a preliminary study. J Foot Ankle Res 9:7
Hetsroni I, Nyska M, Ben-Sira D, Arnson Y, Buksbaum C, Aliev E, Mann G, Massarwe S, Rozenfeld G, Ayalon M (2011) Analysis of foot and ankle kinematics after operative reduction of high-grade intra-articular fractures of the calcaneus. J Trauma 70(5):1234–1240
Hösl M, Böhm H, Multerer C, Döderlein L (2014) Does excessive flatfoot deformity affect function? A comparison between symptomatic and asymptomatic flatfeet using the Oxford foot model. Gait Posture 39(1):23–28
Houck JR, Tome JM, Nawozensky DA (2006) Subtalar neutral position as an offset for a kinematic model of the foot during walking. Gait Analy 28:29–37
Houck JR, Neville C, Tome J, Flemister AS (2009) Foot kinematics during a bilateral heel rise test in participants with stage II posterior tibial tendon dysfunction. J Orthop Sports Phys Ther 39(8):593–603
Houdijk H, Doets HC, van Middelkoop M, DirkjanVeeger HE (2008) Joint stiffness of the ankle during walking after successful mobile-bearing total ankle replacement. Gait Posture 27(1):115–119
Hsu WH, Lewis CL, Monaghan GM, Saltzman E, Hamill J, Holt KG (2014) Orthoses posted in both the forefoot and rearfoot reduce moments and angular impulses on lower extremity joints during walking. J Biomech 47(11):2618–2625
Hunt AE, Smith RM, Torode M (2001) Extrinsic muscle activity, foot motion and ankle joint moments during the stance phase of walking. Foot Ankle Int 22(1):31–41
Hwang SJ, Choi HS, Kim YH (2004) Motion analysis based on a multi-segment foot model in normal walking. Conf Proc IEEE Eng Med Biol Soc 7:5104–5106
Hyslop E, Woodburn J, McInnes IB, Semple R, Newcombe L, Hendry G, Rafferty D, De Mits S, Turner DE (2010) A reliability study of biomechanical foot function in psoriatic arthritis based on a novel multi-segmented foot model. Gait Posture 32(4):619–626
Jenkyn TR, Nicol AC (2007) A multi-segment kinematic model of the foot with a novel definition of forefoot motion for use in clinical gait analysis during walking. J Biomech 40(14):3271–3278
Jenkyn TR, Shultz R, Giffin JR, Birmingham TB (2010) A comparison of subtalar joint motion during anticipated medial cutting turns and level walking using a multi-segment foot model. Gait Posture 31(2):153–158
Kalkum E, van Drongelen S, Mussler J, Wolf SI, Kuni B (2016) A marker placement laser device for improving repeatability in 3D-foot motion analysis. Gait Posture 44:227–230
Kelly LA, Cresswell AG, Racinais S, Whiteley R, Lichtwark G (2014) Intrinsic foot muscles have the capacity to control deformation of the longitudinal arch. J R Soc Interface 11(93):20131188
Kepple TM, Stanhope SJ, Lohmann KN, Roman NL (1990) A video-based technique for measuring ankle-subtalar motion during stance. J Biomed Eng 12(4):273–280
Khazzam M, Long JT, Marks RM, Harris GF (2007) Kinematic changes of the foot and ankle in patients with systemic rheumatoid arthritis and forefoot deformity. J Orthop Res 25(3):319–329
Kidder SM, Abuzzahab FS Jr, Harris GF, Johnson JE (1996) A system for the analysis of foot and ankle kinematics during gait. IEEE Trans Rehabil Eng 4(1):25–32
Kitaoka HB, Crevoisier XM, Hansen D, Katajarvi B, Harbst K, Kaufman KR (2006) Foot and ankle kinematics and ground reaction forces during ambulation. Foot Ankle Int 27(10):808–813
Krzak JJ, Corcos DM, Damiano DL, Graf A, Hedeker D, Smith PA, Harris GF (2015) Kinematic foot types in youth with equinovarus secondary to hemiplegia. Gait Posture 41(2):402–408
Leardini A, Benedetti MG, Catani F, Simoncini L, Giannini S (1999) An anatomically based protocol for the description of foot segment kinematics during gait. Clin Biomech 14(8):528–536
Leardini A, Chiari L, Della Croce U, Cappozzo A (2005) Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation. Gait Posture 21(2):212–225
Leardini A, Benedetti MG, Berti L, Bettinelli D, Nativo R, Giannini S (2007) Rear-foot, mid-foot and fore-foot motion during the stance phase of gait. Gait Posture 25(3):453–462
Leardini A, Aquila A, Caravaggi P, Ferraresi C, Giannini S (2014) Multi-segment foot mobility in a hinged ankle-foot orthosis: the effect of rotation axis position. Gait Posture 40(1):274–277
Levinger P, Murley GS, Barton CJ, Cotchett MP, McSweene SR, Menz HB (2010) A comparison of foot kinematics in people with normal- and flat-arched feet using the Oxford foot model. Gait Posture 32:519–523
Lin SC, Chen CP, Tang SF, Wong AM, Hsieh JH, Chen WP (2013) Changes in windlass effect in response to different shoe and insole designs during walking. Gait Posture 37(2):235–241
Long JT, Eastwood DC, Graf AR, Smith PA, Harris GF (2010) Repeatability and sources of variability in multi-center assessment of segmental foot kinematics in normal adults. Gait Posture 31(1):32–36
Lu TW, O’Connor JJ (1999) Bone position estimation from skin marker co-ordinates using global optimisation with joint constraints. J Biomech 32(2):129–134
Lucareli PR, Contani LB, Lima B, Rabelo ND, Ferreira CL, Lima FP, Correa JC, Politti F (2016) Repeatability of a 3D multi-segment foot model during anterior and lateral step down tests. Gait Posture 43:9–16
Lundgren P, Nester C, Liu A, Arndt A, Jones R, Stacoff A, Wolf P, Lundberg A (2008) Invasive in vivo measurement of rear-, mid- and forefoot motion during walking. Gait Posture 28(1):93–100
MacWilliams BA, Cowley M, Nicholson DE (2003) Foot kinematics and kinetics during adolescent gait. Gait Posture 17(3):214–224
Mahaffey R, Morrison SC, Drechsler WI, Cramp MCJ (2013) Evaluation of multi-segmental kinematic modelling in the paediatric foot using three concurrent foot models. J Foot Ankle Res 6(1):43
Marks RM, Long JT, Ness ME, Khazzam M, Harris GF (2009) Surgical reconstruction of posterior tibial tendon dysfunction: prospective comparison of flexor digitorumlongus substitution combined with lateral column lengthening or medial displacement calcaneal osteotomy. Gait Posture 29(1):17–22
Maurer JD, Ward V, Mayson TA, Davies KR, Alvarez CM, Beauchamp RD, Black AH (2013) A kinematic description of dynamic midfoot break in children using a multi-segment foot model. Gait Posture 38(2):287–292
Merker J, Hartmann M, Kreuzpointner F, Schwirtz A, Haas JP (2015) Pathophysiology of juvenile idiopathic arthritis induced pesplanovalgus in static and walking condition: a functional view using 3D gait analysis. J Pediatr Rheumatol Online 13:21
Milner CE, Brindle RA (2016) Reliability and minimal detectable difference in multi-segment foot kinematics during shod walking and running. Gait Posture 43:192–197
Moseley L, Hunt A, Grant R (1996) Three-dimensional kinematics of the rearfoot during the stance phase of walking in normal young adult males. Clin Biomech 11(1):39–45
Myers KA, Wang M, Marks RM, Harris GF (2004) Validation of a multi-segment foot and ankle kinematic model for pediatric gait. IEEE Trans Neural Syst Rehabil Eng 12(1):122–130
Nawoczenski DA, Ketz J, Baumhauer JF (2008) Dynamic kinematic and plantar pressure changes following cheilectomy for hallux rigidus: a mid-term followup. Foot Ankle Int 29(3):265–272
Ness ME, Long J, Marks R, Harris G (2008) Foot and ankle kinematics in patients with posterior tibial tendon dysfunction. Gait Posture 27(2):331–339
Nester C, Jones RK, Liu A, Howard D, Lundberg A, Arndt A, Lundgren P, Stacoff A, Wolf P (2007a) Foot kinematics during walking measured using bone and surface mounted markers. J Biomech 40(15):3412–3423
Nester CJ, Liu AM, Ward E, Howard D, Cocheba J, Derrick T, Patterson P (2007b) In vitro study of foot kinematics using a dynamic walking cadaver model. J Biomech 40(9):1927–1937
Nester CJ, Liu AM, Ward E, Howard D, Cocheba J, Derrick T (2010) Error in the description of foot kinematics due to violation of rigid body assumptions. J Biomech 43(4):666–672
Nester CJ, Jarvis HL, Jones RK, Bowden PD, Liu A (2014) Movement of the human foot in 100 pain free individuals aged 18–45: implications for understanding normal foot function. J Foot Ankle Res 7(1):51
Neville C, Flemister AS, Houck JR (2009) Effects of the AirLift PTTD brace on foot kinematics in subjects with stage II posterior tibial tendon dysfunction. J Orthop Sports Phys Ther 39(3):201–209
Novak AC, Mayich DJ, Perry SD, Daniels TR, Brodsky JW (2014) Gait analysis for foot and ankle surgeons – topical review, part 2: approaches to multi-segment modeling of the foot. Foot Ankle Int 35(2):178–191
Okita N, Meyers SA, Challis JH, Sharkey NA (2009) An objective evaluation of a segmented foot model. Gait Posture 30(1):27–34
Oosterwaal M, Telfer S, Torholm S, Carbes S, van Rhijn LW, Macduff R, Meijer K, Woodburn J (2011) Generation of subject-specific, dynamic, multi-segment ankle and foot models to improve orthotic design: a feasibility study. BMC Musculoskelet Disord 12:256
Oosterwaal M, Carbes S, Telfer S, Woodburn J, Tørholm S, Al-Munajjed A, van Rhijn L, Meijer K (2016) The Glasgow-Maastricht foot model, evaluation of a 26 segment kinematic model of the foot. J Foot Ankle Res 9:19
Peeters K, Natsakis T, Burg J, Spaepen P, Jonkers I, Dereymaeker G, Vander Sloten J (2013) An in vitro approach to the evaluation of foot-ankle kinematics: performance evaluation of a custom-built gait simulator. Proc Inst Mech Eng H 227(9):955–967
Pohl MB, Messenger N, Buckley JG (2006) Changes in foot and lower limb coupling due to systematic variations in step width. Clin Biomech 21(2):175–183
Portinaro N, Leardini A, Panou A, Monzani V, Caravaggi P (2014) Modifying the Rizzoli foot model to improve the diagnosis of pes-planus: application to kinematics of feet in teenagers. J Foot Ankle Res 7(1):754
Pothrat C, Authier G, Viehweger E, Berton E, Rao G (2015) One- and multi-segment foot models lead to opposite results on ankle joint kinematics during gait: implications for clinical assessment. Clin Biomech 30(5):493–499
Powell DW, Williams DS, Butler RJ (2013) A comparison of two multi-segment foot models in high-and low-arched athletes. J Am Podiatr Med Assoc 103(2):99–105
Prinold JA, Mazzà C, Di Marco R, Hannah I, Malattia C, Magni-Manzoni S, Petrarca M, Ronchetti AB, Tanturri de Horatio L, van Dijkhuizen EH, Wesarg S, Viceconti M, MD-PAEDIGREE Consortium Ann (2016) A patient-specific foot model for the estimate of ankle joint forces in patients with juvenile idiopathic arthritis. Ann Biomed Eng 44(1):247–257
Rankine L, Long J, Canseco K, Harris GF (2008) Multisegmental foot modeling: a review. Crit Rev Biomed Eng 36(2–3):127–181
Rao S, Saltzman C, Yack HY (2006) Segmental foot mobility in individuals with and without diabetes and neuropathy. Clin Biomech 22:464–471
Rao S, Baumhauer JF, Tome J, Nawoczenski DA (2009) Comparison of in vivo segmental foot motion during walking and step descent in patients with midfoot arthritis and matched asymptomatic control subjects. J Biomech 42(8):1054–1060
Rattanaprasert U, Smith R, Sullivan M, Gilleard W (1999) Three-dimensional kinematics of the forefoot, rearfoot, and leg without the function of tibialis posterior in comparison with normals during stance phase of walking. Clin Biomech 14(1):14–23
Raychoudhury S, Hu D, Ren L (2014) Three-dimensional kinematics of the human metatarsophalangeal joint during level walking. Front Bioeng Biotechnol 2:73
Rouhani H, Favre J, Crevoisier X, Jolles BM, Aminian K (2011) Segmentation of foot and ankle complex based on kinematic criteria. Comput Methods Biomech Biomed Engin 4(9):773–781
Rouhani H, Favre J, Aminian K, Crevoisier X (2012) Multi-segment foot kinematics after total ankle replacement and ankle arthrodesis during relatively long-distance gait. Gait Posture 36(3):561–566
Rouhani H, Favre J, Crevoisier X, Aminian K (2014) A wearable system for multi-segment foot kinetics measurement. J Biomech 47(7):1704–1711
Saraswat P, Andersen MS, MacWilliams BA (2010) A musculoskeletal foot model for clinical gait analysis. J Biomech 43:1645–1652
Saraswat P, MacWilliams BA, Davis RB (2012) A multi-segment foot model based on anatomically registered technical coordinate systems: method repeatability in pediatric feet. Gait Posture 35(4):547–555
Saraswat P, MacWilliams BA, Davis RB, D’Astous JL (2013) A multi-segment foot model based on anatomically registered technical coordinate systems: method repeatability and sensitivity in pediatric planovalgus feet. Gait Posture 37(1):121–125
Sawacha Z, Cristoferi G, Guarneri G, Corazza S, Donà G, Denti P, Facchinetti A, Avogaro A, Cobelli C (2009) Characterizing multi-segment foot kinematics during gait in diabetic foot patients. J Neuroeng Rehabil 6:37
Scott SH, Winter DA (1991) Talocrural and talocalcaneal joint kinematics and kinetics during the stance phase of walking. J Biomech 24(8):743–752
Seo SG, Lee DY, Moon HJ, Kim SJ, Kim J, Lee KM, Chung CY, Choi IH (2014) Repeatability of a multi-segment foot model with a 15-marker set in healthy adults. J Foot Ankle Res 7:24
Shultz R, Kedgley AE, Jenkyn TR (2011a) Quantifying skin motion artifact error of the hindfoot and forefoot marker clusters with the optical tracking of a multi-segment foot model using single-plane fluoroscopy. Gait Posture 34(1):44–48
Shultz R, Birmingham TB, Jenkyn TR (2011b) Differences in neutral foot positions when measured barefoot compared to in shoes with varying stiffnesses. Med Eng Phys 33(10):1309–1313
Simon J, Doederlein L, McIntosh AS, Metaxiotis D, Bock HG, Wolf SI (2006) The Heidelberg foot measurement method: development, description and assessment. Gait Posture 23(4):411–424
Souza TR, Fonseca HL, Vaz AC, Antero JS, Marinho CS, Fonseca ST (2014) Between-day reliability of a cluster-based method for multi-segment kinematic analysis of the foot-ankle complex. J Am Podiatr Med Assoc 104(6):601–609
Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T (2006) Repeatability of a model for measuring multi-segment foot kinematics in children. Gait Posture 23(4):401–410
Stebbins J, Harrington M, Thompson N, Zavatsky A, Theologis T (2010) Gait compensations caused by foot deformity in cerebral palsy. Gait Posture 32(2):226–230
Theologis TN, Harrington ME, Thompson N, Benson MK (2003) Dynamic foot movement in children treated for congenital talipesequinovarus. J Bone Joint Surg Br 85(4):572–577
Tome J, Nawoczenski DA, Flemister A, Houck J (2006) Comparison of foot kinematics between subjects with posterior tibialis tendon dysfunction and healthy controls. J Orthop Sports Phys Ther 36(9):635–644
Turner DE, Helliwell PS, Emery P, Woodburn J (2006) The impact of rheumatoid arthritis on foot function in the early stages of disease: a clinical case series. BMC Musculoskelet Disord 7:102
Turner DE, Woodburn J (2008) Characterising the clinical and biomechanical features of severely deformed feet in rheumatoid arthritis. Gait Posture 28(4):574–580
Twomey D, McIntosh AS, Simon J, Lowe K, Wolf SI (2010) Kinematic differences between normal and low arched feet in children using the Heidelberg foot measurement method. Gait Posture 32(1):1–5
Van den Herrewegen I, Cuppens K, Broeckx M, Barisch-Fritz B, Vander Sloten J, Leardini A, Peeraer L (2014) Dynamic 3D scanning as a markerless method to calculate multi-segment foot kinematics during stance phase: methodology and first application. J Biomech 47(11):2531–2539
vanHoeve S, de Vos J, Weijers P, Verbruggen J, Willems P, Poeze M, Meijer K (2015) Repeatability of the Oxford foot model for kinematic gait analysis of the foot and ankle. Clin Res Foot Ankle 3:171
Wang R, Thur CK, Gutierrez-Farewik EM, Wretenberg P, Broström E (2010) One year follow-up after operative ankle fractures: a prospective gait analysis study with a multi-segment foot model. Gait Posture 31(2):234–240
Wang Y, Wong DW, Zhang M (2016) Computational models of the foot and ankle for pathomechanics and clinical applications: a review. Ann Biomed Eng 44(1):213–221
Whittaker EC, Aubin PM, Ledoux WR (2011) Foot bone kinematics as measured in a cadaveric robotic gait simulator. Gait Posture 33(4):645–650
Wolf P, Stacoff A, Liu A, Nester C, Arndt A, Lundberg A, Stuessi E (2008a) Functional units of the human foot. Gait Posture 28(3):434–441
Wolf S, Simon J, Patikas D, Schuster W, Armbrust P, Döderlein L (2008b) Foot motion in children shoes: a comparison of barefoot walking with shod walking in conventional and flexible shoes. Gait Posture 27(1):51–59
Woodburn J, Turner DE, Helliwell PS, Barker S (1999) A preliminary study determining the feasibility of electromagnetic tracking for kinematics at the ankle joint complex. Rheumatology (Oxford) 38(12):1260–1268
Woodburn J, Nelson KM, Siegel KL, Kepple TM, Gerber LH (2004) Multisegment foot motion during gait: proof of concept in rheumatoid arthritis. J Rheumatol 31(10):1918–1927
Wrbaskić N, Dowling JJ (2007) An investigation into the deformable characteristics of the human foot using fluoroscopic imaging. Clin Biomech 22(2):230–238
Wright CJ, Arnold BL, Coffey TG, Pidcoe PE (2011) Repeatability of the modified Oxford foot model during gait in healthy adults. Gait Posture 33(1):108–112
Wu WL, Su FC, Cheng YM, Huang PJ, Chou YL, Chou CK (2000) Gait analysis after ankle arthrodesis. Gait Posture 11(1):54–61
Author information
Authors and Affiliations
Corresponding author
Section Editor information
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this entry
Cite this entry
Leardini, A., Caravaggi, P. (2018). Kinematic Foot Models for Instrumented Gait Analysis. In: Handbook of Human Motion. Springer, Cham. https://doi.org/10.1007/978-3-319-14418-4_28
Download citation
DOI: https://doi.org/10.1007/978-3-319-14418-4_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14417-7
Online ISBN: 978-3-319-14418-4
eBook Packages: EngineeringReference Module Computer Science and Engineering