Abstract
AKI is a clinical syndrome mainly manifested as a sharp decline in renal function, which is a common complication in the ICU and is characterized by high mortality and poor prognosis, and early diagnosis and treatment of AKI is important to save the patient’s life. When cells are stimulated by injury, the cell cycle cannot proceed normally and arrest at a certain stage. This phenomenon is called cell cycle arrest. Renal tubular epithelial cells of AKI patients usually have cell cycle arrest in G1 and/or G2 phases, which indicates that the expression changes of cell cycle arrest biomarkers can directly reflect the damage of renal tubular epithelial cells. Therefore, as a new standard for early prediction and diagnosis of AKI, the detection of cell cycle arrest biomarkers has become a current research hotspot.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
The research on cell cycle arrest biomarkers mainly focuses on the related fields of tumors and acute kidney injury (AKI). According to the admission criteria in the intensive care unit (ICU), the early diagnosis of tumors does not belong to the research scope in ICU, while AKI is characterized by high mortality and poor prognosis in ICU. Therefore, early diagnosis of AKI and provision of targeted treatment will be important to save the patient’s life and improve the prognosis. With the important role of cell cycle arrest in the pathogenesis of AKI widely recognized, tissue inhibitor of metalloproteinase-2 (TIMP-2) and insulin-like growth factor-binding protein 7 (IGFBP7), biomarkers of cell cycle arrest, have become the current research hotspots for early prediction of AKI in the ICU. In this paper, we will focus on cell cycle and cell cycle arrest, cell cycle arrest in AKI, AKI in ICU, and early prediction of AKI by cell cycle arrest biomarkers.
Cell Cycle and Cell Cycle Arrest
Cell Cycle
Cell cycle refers to the whole process experienced by cells from the end of the last mitosis to the completion of the next mitosis. A complete cell cycle is divided into DNA synthesis phase (S phase) and mitosis phase (M phase), and the two intermediate preparation phases (G1, G2 phases) (Nurse 2000). G1 phase, also known as presynthetic phase, mainly synthesizes ribosomes and RNA and other substances to prepare for the replication of DNA; S phase is the DNA synthesis phase, which synthesizes histones and various other enzymes in addition to DNA; G2 phase is the anaphase of synthesis, which is mainly the material conditions required for mitotic preparation; M phase is the mitotic phase. In addition, cells can also be in a state of stopping proliferation and entering quiescence, which is called G0 phase at this time (Vermeulen et al. 2003).
The cell cycle progresses orderly under the common regulation of a variety of cellular proteins, the most critical regulatory proteins of which are cyclin-dependent kinases (CDKs), cyclins, and cyclin-dependent kinase inhibitors(CKIs), which bind to cyclins to form complexes and promote cell cycle progression, while CKIs prevent the transition of the cell cycle to the next stage by disrupting their binding (Lim and Kaldis 2013). So far, 21 CDKs and 5 CDK-like genes have been identified, which can be mainly divided into two categories: (1) subfamilies that directly or indirectly regulate the cell cycle and (2) subfamilies that regulate transcription (Whittaker et al. 2017). Among them, in the process of regulating the cell cycle, CDK1, CDK2, CDK4, and CDK6 play a major role, and they regulate different cell cycle stages by binding to specific cyclins (Zhang et al. 2021) (Fig. 1).
Cell Cycle Arrest
There is a special set of regulatory mechanisms in the cell cycle, known as cell cycle checkpoints, which can be divided into four checkpoints according to the cell cycle. When there are problems such as abnormal cell morphology, DNA damage, and abnormal spindle assembly, cell cycle checkpoints are activated to prevent the progression of the cell cycle to the next stage, so that cells have time to repair damage, correct abnormalities or exit the cell cycle (Justman 2017). This phenomenon that the cell cycle cannot proceed smoothly due to intracellular and extracellular stress stimuli and arrests at a certain stage is called cell cycle arrest (Pack et al. 2019).
Depending on the cell cycle checkpoint, the cell cycle can be arrested at different stages, and the signaling pathways involved are mainly divided into the following aspects:
-
(1)
G1 arrest: In the classical cell cycle model, the G1 phase checkpoint is set at the end of G1 phase, through which cells will be allowed to enter S phase, and the cell cycle will be blocked in G1 phase when cells have factors such as lack of mitotic stimulation and/or DNA damage (Agami and Bernards 2002).
Normal mitotic stimulation can induce the expression of cyclin D. Cyclin D forms a complex with CDK4/6, and the cyclin-CDK complex enters the nucleus and is activated by CDK-activating kinase (CAK). The activated cyclin-CDK complex phosphorylates retinoblastoma protein (Rb); relieves the partial inhibition of E2F transcription factor family by Rb; promotes the expression of E2F target genes such as cyclin E, followed by the increase of cyclin E level; and activates CDK2. CyclE-CDK2 hyperphosphorylates Rb, which leads to increased release of E2F transcription factors, transcriptional initiation, and increased gene expression in S phase, and the cell cycle enters S phase from G1 phase (Goel et al. 2018; Ingham and Schwartz 2017; Yang et al. 2020). Cells are therefore unable to complete a normal G1/S phase transition when mitotic stimulation ceases or is lacking.
DNA damage caused by various endogenous or exogenous factors activates the ataxia-telangiectasia mutated (ATM) p53 signaling pathway; p53 acts as a transcription factor to activate the expression of the downstream protein p21, which, as a member of the CKI family, inhibits cyclin-CDK complex activity and prevents cells from entering S phase, thus providing time for DNA damage repair or induction of apoptosis (Georgakilas et al. 2017; Khoronenkova and Dianov 2015).
Thus, in the classical cell cycle model, hyperphosphorylation of Rb in late G1 becomes the molecular basis by which the cell cycle can enter S phase, so the G1 phase checkpoint is considered to be a limiting point located in late G1, after which cells will enter S phase. However, with the deepening of research, a new cell cycle model has been proposed in recent years, in which there are a total of three checkpoints to determine whether cells can enter S phase (Hume et al. 2020).
-
(2)
S phase arrest: When cells have DNA replication stress factors such as abnormal replication origin excitation, DNA damage, or depletion of deoxyribonucleotide pools, the cell cycle cannot pass the S phase checkpoint and is arrested in S phase (Ciardo et al. 2019). In this process, endogenous or exogenous replication stress activates the ataxia telangiectasia and Rad3-related (ATR) and checkpoint kinase 1 (CHK1) signaling pathways, and ATR/CHK1-mediated phosphorylation events inhibit the activity of the CDK activator Cdc25, reduce CDK1/2 activity, and prevent the cell cycle from entering G2 phase (Giannattasio and Branzei 2017).
-
(3)
G2 arrest: When there are checkpoint defects such as p53 gene mutation, cells with DNA damage may enter G2 phase normally through the first two checkpoints, so the G2 phase checkpoint is essential for maintaining the integrity of the genome, and cells with DNA damage will be arrested in G2 phase for repair or selected for apoptosis and cannot enter M phase (Kastan and Bartek 2004). Similar to S phase, ATR-mediated damage repair is activated during DNA damage, and ATR/CHK1 activates the mitotic repressors WEE1 and MYT1, while inhibiting the expression of Cdc25, which inhibits the activity of cyclin B-CDK1 through these three pathways and halts the cell cycle in G2 phase (Gorecki et al. 2021; Schmidt et al. 2017).
However, some cells can overcome G2 phase cell cycle arrest and carry damaged DNA into mitosis, a phenomenon known as G2/M checkpoint adaptation. Of these, most of the cells die during mitosis, and a small proportion may survive due to changing the original genome during repair and adaptation, which may be associated with inactivation of CHK1 (Kalsbeek and Golsteyn 2017).
-
(4)
M phase arrest: When the spindle is not properly attached to the chromosome, the cell stops in M phase, so the M phase checkpoint is also called the spindle checkpoint (Musacchio 2015). After cells enter M phase, CDK1 releases APC/C from APC/C-CDH1 and phosphorylates APC/C, allowing it to disrupt the activity of cyclin B and securin, promote sister chromatid separation, and exit mitosis. When cells have abnormal chromosome segregation, however, the mitotic checkpoint complex will inhibit the activity of APC/C and maintain cells in M phase (Holder et al. 2019).
Recent studies have found that M phase may also have a DNA damage checkpoint due to the possible presence of persistent DNA replication defects, unrepaired pre-M phase DNA damage, and true M phase DNA damage, indicating that DNA damage can prolong M phase, which may be associated with ATM and the ATR cascade (Thompson et al. 2019).
Cell Cycle Arrest in AKI
Normally, the vast majority of renal tubular epithelial cells (TECs) are considered to be in the quiescent G0 stage, and less than 1% of cells are proliferating to balance cell physiological death or accidental loss from the basement membrane. When renal injury events such as ischemia-reperfusion, oxidative stress, and toxic injury occur, they will lead to necrosis and apoptosis of TECs, at which time surviving G0 phase TECs will reenter the cell cycle and replace necrotic and apoptotic cells by migration, proliferation, and differentiation to restore renal function (Moonen et al. 2018). AKI often also accompanies DNA damage in TECs (Yan et al. 2016; Zhu et al. 2015). Thus, when AKI occurs, TECs that enter the cell cycle are arrested at a certain cycle by activated cell cycle checkpoints.
In AKI, TECs cell cycle arrest mainly occurs in two stages: G1 and G2, of which G1 phase is mainly mediated by p21 signaling pathway, and early transient G1 arrest of TECs will facilitate cell repair injury, while continuous stay in G1 phase will lead to apoptosis. G2 phase is mainly mediated by the ATR/CHK1 signaling pathway, and G2/M-arrested TECs present a pro-fibrotic phenotype, while activating c-jun NH2 terminal kinase signaling pathway promotes the secretion of fibrotic factors, ultimately leading to the development of fibrosis and poor prognosis and even progression to chronic kidney disease (Andrade et al. 2018; Basile et al. 2015).
This seems to be a paradoxical phenomenon, and kidney injury stimulates cell proliferation and also leads to cell cycle arrest, but in fact, cell cycle arrest, as a protective mechanism, provides sufficient time for the repair of DNA damage to avoid genetic defects, cell necrosis, and other conditions that are not conducive to the recovery of kidney function during the proliferation and differentiation of TECs. Thus, AKI often undergoes cell cycle arrest in TECs in the early stage, and by detecting cell cycle arrest biomarkers, it is possible to detect whether TECs are damaged as early as possible, regardless of whether this damage is sufficient to lead to AKI, but this is the earliest detectable damage signal, so cell cycle arrest-related proteins are considered to be new biomarkers for predicting AKI.
Both TIMP-2 and IGFBP7 are closely associated with G1 arrest of TECs (Fig. 2) and can be detected in urine. When TECs are injured, both of them cause cell cycle arrest in TECs by autocrine and paracrine means, in which TIMP-2 stimulates p27 expression and IGFBP7 stimulates p21 and p53 expression, and these highly expressed p21, 27, and 53 inhibit the activity of cyclin D-CDK4 and cyclin E-CDK2 and arrest the cell cycle in G1 phase for repair (Kellum and Chawla 2015). Therefore, TIMP-2 and IGFBP7, as cell cycle arrest biomarkers, can indicate that TECs are damaged as early as possible and play an important role in the early prediction of AKI.
AKI in ICU
AKI is a clinical syndrome characterized by a sharp decline in renal function and is a common complication in ICUs, and a multinational study of more than 1800 patients in 97 ICUs pointed out that about 57% of patients will experience varying degrees of AKI within 1 week of admission (Hoste et al. 2015). AKI in the ICU appears primarily as a complication of several of the following conditions (Griffin et al. 2020):
-
(1)
Sepsis: Sepsis is the most important cause of AKI in the ICU, and sepsis-associated AKI (SA-AKI) occurs in 10%–20% of septic patients and 50%–70% of septic shock patients (Griffin et al. 2020), which accounts for 45%–70% of all AKI cases (Sun et al. 2019). The pathogenesis of SA-AKI has not been fully clarified. In the past, renal hypoperfusion and ischemia were considered to be the main causes of SA-AKI. However, recent studies have found that SA-AKI can also have normal or even increased renal blood flow. The classical renal hypoperfusion theory is not enough to explain the occurrence of SA-AKI. Therefore, a “unified theory” based on inflammation, oxidative stress, microvascular dysfunction, and endothelial dysfunction pointed out that tubular cells may adapt to these injurious and inflammatory danger signs caused by sepsis in a manner that sacrifices their own function, manifested as SA-AKI (Gomez et al. 2014; Poston and Koyner 2019).
-
(2)
Cardiac surgery: In the ICU patient population, cardiac surgery-associated AKI (CSA-AKI) is the second most common type of AKI after SA-AKI, with an incidence ranging from 5% to 42% in patients after cardiac surgery (Griffin et al. 2020). CSA-AKI can be classified as type I cardiorenal syndrome, that is, the dramatic deterioration of cardiac function leads to AKI, and its occurrence may involve several renal injury pathways such as renal hypoperfusion, ischemia-reperfusion injury, nephrotoxic drug stimulation, inflammation, and oxidative stress (Wang and Bellomo 2017).
-
(3)
Acute liver failure: Approximately 70% of patients with acute liver failure (ALF) will develop AKI during hospitalization, with acetaminophen-induced ALF and ischemic ALF having the highest incidence of AKI (Tujios et al. 2015). AKI during ALF may be caused by renal hypoperfusion, endogenous injury (e.g., tubular toxicity of acetaminophen), and other complications of ALF (e.g., sepsis) (Leventhal and Liu 2015).
-
(4)
Application of extracorporeal membrane oxygenation: Extracorporeal membrane oxygenation (ECMO) is widely used in the ICU, and the incidence of AKI is as high as 60%–70% in the ECMO patient population. ECMO can lead to the development of AKI through factors such as pulseless blood flow, coagulation disorders, and inflammatory response formed by cardiopulmonary bypass (Razo-Vazquez and Thornton 2016).
-
(5)
Other factors: A series of complex clinical syndromes such as cardiorenal syndrome and hepatorenal syndrome also trigger AKI, and the mechanism is closely related to factors such as hemodynamics (Gonwa and Wadei 2013; House 2018); intra-abdominal hypertension may also cause decreased perfusion and trigger AKI through increased renal venous and renal parenchymal pressure (Mohmand and Goldfarb 2011).
In conclusion, AKI is not only one of the common complications in the ICU, but also AKI acts as an independent risk factor for mortality in the ICU, and its severity is directly closely related to mortality (Hoste et al. 2015). In addition to death, survivors of AKI often face the threat of poor prognosis and progressive or persistent renal injury, which may progress to chronic kidney disease or end-stage renal disease (Forni et al. 2017). Therefore, diagnosing AKI as early as possible, with targeted intervention, will be important to save patients’ lives and improve prognosis.
Application of Cell Cycle Arrest Biomarkers in Predicting AKI
The diagnostic criteria for AKI have also not been uniform due to the lack of accepted definitions and grading criteria for AKI, and in this context, the Acute Dialysis Quality Initiative group proposed the RIFLE criteria in 2004 (Bellomo et al. 2004) AKI is divided into five stages: risk, injury, failure, loss, and end-stage renal disease, and is diagnosed by serum creatinine (Scr), glomerular filtration rate (GFR), and urine volume. Subsequently the AKIN improved the RIFLE criteria in 2007 (Mehta et al. 2007). GFR was canceled as the basis for the diagnosis of AKI, stages L and E were canceled, and AKI was classified into three grades based on the changes in Scr and urine volume. However, these diagnostic criteria still have some limitations, so in 2012 KDIGO synthesized the RIFLE criteria and AKIN criteria and released the first clinical practice guidelines (Kdigo.org.). KDIGO criteria followed the changes in Scr and urine volume in AKIN criteria as the diagnostic basis, modified and improved the diagnostic criteria for AKI 3 stage in the original criteria, and became the most applied AKI diagnostic criteria at present.
However, these diagnostic criteria have some problems; GFR and Scr baseline in RIFLE criteria are difficult to determine, while it is unknown whether the recommended MDRD formula is accurate in assessing GFR baseline under pathological conditions. Although AKIN and KDIGO improved the baseline problem and improved the sensitivity of Scr in the diagnosis of AKI, since Scr and urine volume are the embodiment of renal function and cannot visually reflect the renal injury, the changes of Scr and abnormal urine volume can be detected only when the renal function has been significantly impaired, which seriously hinders the early diagnosis of AKI and has a huge adverse impact on the prognosis of patients (Kashani et al. 2017). Changes in Scr are more suitable as a criterion rather than a diagnostic criterion for defining AKI, and in this context, the use of biomarkers produced during kidney injury as a new criterion for predicting and diagnosing AKI has become a hot topic of current research.
At present, the research on biomarkers of kidney injury mainly focuses on neutrophil gelatinase-associated lipocalin (NGAL), interleukin-18 (IL-18), kidney injury molecule-1 (KIM-1), L-type fatty acid-binding protein (L-FABP), TIMP-2, and IGFBP7. This article mainly introduces TIMP-2 and IGFBP7.
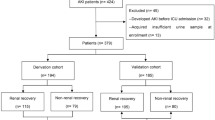
[TIMP-2] × [IGFBP7] Findings
The earliest important studies on TIMP-2 and IGFBP7 for predicting AKI can be pursued until 2010–2013, in order to find more appropriate AKI biomarkers. Kashani et al. (2013), based on various hypotheses of AKI pathophysiology (inflammation, apoptosis, necrosis, cell cycle, etc.), identified a total of 340 AKI related proteins including NGAL, IL-18, KIM-1, TIMP-2, and IGFBP7 as AKI candidate biomarkers and analyzed these 340 candidate biomarkers in combination with blood and urine samples from 3 ICU clinical bases. TIMP-2 and IGFBP7 performed the best in this process. Within 12–36 hours, according to RIFLE criteria, the AUC for predicting phase I/F was 0.75 (95% CI 0.70–0.80) and 0.77 (95% CI 0.71–0.82), respectively, which was more advantageous than other biomarkers such as urine NGAL, urine IL-18, and urine KIM-1. Subsequently, Kianoush et al. studied the performance of TIMP-2 and IGFBP7 in predicting AKI in 728 critically ill patients (Sapphire study). In this study, they found that the product of TIMP-2 and IGFBP7 had higher value in predicting AKI. When subjects developed moderate to severe AKI within 12 hours (KDIGO2-3 stage), the AUC of [TIMP-2] × [IGFBP7] was 0.80 (95% CI 0.75–0.84), while the AUC of TIMP-2 and IGFBP7 alone was 0.79 and 0.76, respectively. Meanwhile, the AUC of [TIMP-2] × [IGFBP7] was significantly higher than that of all other existing biomarkers. These evidences suggested that [TIMP-2] × [IGFBP7] may have obvious advantages in early prediction of AKI in clinical practice. Meanwhile, this study also proposed the use of [TIMP-2] × [IGFBP7] for AKI risk classification. When [TIMP-2] × [IGFBP7] > 0.3 (ng/mL)2/1000, the patient’s risk of AKI (KDIGO2-3 stage within 12 hours) and renal adverse events (death, dialysis, persistent renal insufficiency, etc.) increased dramatically; when [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000, the risk of AKI and renal adverse events increased to five times and two times, respectively.
However, the Sapphire study still has some limitations, and in order to better apply the findings to clinical practice, Bihorac et al. (2014) validation was performed against the two proposed AKI Risk Grading cutoffs in the Sapphire study (Topaz study). A total of 408 critically ill patients were enrolled in this study, which investigated the sensitivity and specificity of two cutoffs, [TIMP-2] × [IGFBP7] > 0.3 (ng/mL)2/1000 and [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000, in predicting AKI, while clinical variables were introduced to investigate whether [TIMP-2] × [IGFBP7] remains a statistically significant biomarker for predicting AKI in a clinical model. In this study, the median value of [TIMP-2] × [IGFBP7] in critically ill patients diagnosed with AKI within 12 hours was 1.6 (0.7–2.8) (ng/mL)2/1000, significantly higher than the median value of 0.3 (0.2–0.8) (ng/mL)2/1000 in non-AKI critically ill patients, meanwhile, the AUC of [TIMP-2] × [IGFBP7] to predict AKI within 12 hours was 0.86 (95% CI 0.76–0.88) confirming the reliability and reproducibility of the AUC of [TIMP-2] × [IGFBP7] of 0.80 (95% CI 0.75–0.84) observed in the previous Sapphire study. The AUC of Scr determined in the same period was 0.63 (95% CI 0.56–0.70), indicating a significant advantage of [TIMP-2] × [IGFBP7] in early prediction of AKI. Compared with patients with [TIMP-2] × [IGFBP7] < 0.3 (ng/mL)2/1000, patients with [TIMP-2] × [IGFBP7] 0.3–2 (ng/mL) 2/1000 had a fivefold increased risk of AKI (95% CI3–17), and patients with [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000 had a 17-fold increased risk of AKI (95% CI9–54). Notably, when clinical variables were introduced, the AUC for the combined [TIMP-2] × [IGFBP7] and clinical model was 0.86 (95% CI 0.80 to 0.90), while the AUC for the clinical model alone was 0.70 (95% CI 0.63 to 0.76), a significant difference, indicating that [TIMP-2] × [IGFBP7] remains a strong biomarker for predicting AKI. In a subsequent cutoff study, [TIMP-2] × [IGFBP7] had the highest sensitivity of 92% (95% CI85–98) and specificity of 46% (95% CI41–52) at a cutoff of 0.3 (ng/mL)2/1000, and [TIMP-2] × [IGFBP7] had the highest specificity of 95% (95% CI93–97) and sensitivity of 37% (95% CI26–47) at a cutoff of 2 (ng/mL)2/1000. This is consistent with the conclusion of Hoste et al. (2014) that [TIMP-2] × [IGFBP7] had the highest sensitivity of 89% and NPV of 97% at a cutoff of 0.3 (ng/mL)2/1000 and [TIMP-2] × [IGFBP7] had the highest specificity of 95% and PPV of 49% at a cutoff of 2 (ng/mL)2/1000 in the Opal study of Eric et al. This identified a cutoff value of 0.3 (ng/mL)2/1000 for high sensitivity and 2 (ng/mL)2/1000 for high specificity in moderate-severe AKI, which is clinically important for identifying patients with AKI.
So far, the US Food and Drug Administration (FDA) has approved [TIMP-2] × [IGFBP7] for marketing as a biomarker for predicting the risk of AKI, NephroCheck® (NC) test. By quantitatively measuring the value of [TIMP-2] × [IGFBP7] in the patient’s urine, the test is compared with the clinical endpoint to provide a validated AKI risk index in prospective clinical trials. Since then, the clinical application of [TIMP-2] × [IGFBP7] has become a current research hotspot.
[TIMP-2] × [IGFBP7] to Predict Different Types of AKI
As AKI in ICU is mainly closely related to sepsis and cardiac surgery, [TIMP-2] × [IGFBP7] predicted that AKI was mainly concentrated in CSA-AKI and SA-AKI, as shown in Table 1.
CSA-AKI: Meersch et al. (2014) found that [TIMP-2] × [IGFBP7] is the best predictor in the process of predicting the risk of developing AKI after cardiac surgery, with high specificity and sensitivity. They enrolled 50 patients with a high risk of AKI who underwent cardiac surgery under cardiopulmonary bypass (CPB). Among them, 26 patients (52%) developed AKI after operation. In these patients, the value of [TIMP-2] × [IGFBP7] was significantly increased compared with that before CPB, and [TIMP-2] × [IGFBP7] increased from an average of 0.49 (SE 0.24) preoperatively to 1.51 (SE 0.57) at 4 hours after CPB, while AKI diagnosis according to traditional criteria occurred 1–3 days after CPB; the AUC of [TIMP-2] × [IGFBP7] at 4 hours after operation was 0.81 (95% CI 0.68–0.93), while the AUC of NGAL was 0.68 (95% CI 0.53–0.84), indicating that [TIMP-2] × [IGFBP7] has more important value in predicting the early risk of AKI after cardiac surgery. In particular, the specificity was 0.83, and the sensitivity was 0.80 using a cutoff value of 0.3 (ng/mL)2/1000, and the specificity was 0.81, and the sensitivity was 0.92 using a cutoff value of 0.5 (ng/mL)2/1000, indicating that the highest concentration of [TIMP-2] × [IGFBP7] at 4 hours after surgery is a specific and sensitive indicator for predicting the risk of postoperative AKI. Wang et al. (2017) subsequently validated the ability of [TIMP-2] × [IGFBP7] to predict the risk of AKI within 4 hours after surgery in a study of 57 cardiac surgery patients, with an AUC of 0.80 (95% CI 0.68–0.91), and the value of [TIMP-2] × [IGFBP7] was significantly higher in patients who developed AKI compared to those who did not. Oezkur et al. (2017) investigated the relationship between [TIMP-2] × [IGFBP7] at different time points after surgery and the risk of AKI in a study of 150 cardiac surgery patients, and they indicated that immediate postoperative measurement of [TIMP-2] × [IGFBP7] was the best time to predict the risk of AKI. Gist et al. (2017) investigated the ability of [TIMP-2] × [IGFBP7] to predict the risk of AKI in infants and newborns after cardiac surgery. The study found that the risk of AKI in patients with [TIMP-2] × [IGFBP7] ≥ 0.78 (ng/mL) 2/1000 was three times higher than that in patients with [TIMP-2] × [IGFBP7] < 0.78 (ng/mL) 2/1000. When combined with the clinical model, the AUC of [TIMP-2] × [IGFBP7] to predict AKI was 0.78 (95% CI 0.67–0.90). These studies showed that [TIMP-2] × [IGFBP7] also performed well in predicting the risk of AKI in infants, newborns, and children.
Postoperative AKI in other surgical procedures: In addition to cardiac surgery, other surgical procedures also have a higher risk of postoperative AKI. The study by Gocze et al. (2015) included 107 patients who underwent noncardiac surgery, and a total of 45 patients (42%) developed AKI within 48 hours after surgery, with an AUC of 0.85 (95% CI 0.78–0.93) for AKI 1 and 0.85 (95% CI 0.67–0.80) for AKI 2–3 according to the cutoff value of [TIMP-2] × [IGFBP7] > 0.3 (ng/mL)2/1000. Simultaneous, the AUC of 0.3 (ng/mL) 2/1000 as the cutoff value for predicting early application of RRT in patients was 0.83 (95% CI 0.75–0.92), and the AUC to predict 28-day mortality was 0.77 (95% CI 0.67–0.80), indicating that [TIMP-2] × [IGFBP7] can be used not only to predict the risk of AKI but also predict the prognosis of AKI and guide early renoprotective treatment. Gunnerson et al. (2016) also noted [TIMP-2] × [IGFBP7] to be a strong predictor of risk of AKI in patients after surgery in their analysis of critically ill surgical patients in the Sapphire study and Topaz study, with an AUC of 0.84 (95% CI 0.76–0.90).
SA-AKI: Honore et al. (2016) studied the probability of AKI in sepsis and non-sepsis patients predicted by [TIMP-2] × [IGFBP7] and found that AKI prediction by [TIMP-2] × [IGFBP7] was not affected by sepsis and AUC was 0.85 (95% CI 0.76–0.94) in patients with SOFA score > 7 in addition to renal score, while AUC was 0.84 (95% CI 0.73–0.92) in patients with ≤7, indicating [TIMP-2] × [IGFBP7] can still accurately predict AKI in septic patients. Cuartero et al. (2017) also verified this in subsequent studies, [TIMP-2] × [IGFBP7] was not affected by sepsis when predicting AKI, and its AUC was 0.80 (95%CI0.71–0.89), and these studies showed that [TIMP-2] × [IGFBP7] could be an independent predictor of AKI independent of sepsis interference. Maizel et al. (2019) found that the AUC of [TIMP-2] × [IGFBP7] for predicting progression to KDIGO3 stage within 24 hours in patients with septic shock was 0.83 (95% CI 0.75–0.90), which was superior to other predictors such as serum creatinine. When [TIMP-2] × [IGFBP7] > 1.92 (ng/mL)2/1000, the sensitivity and specificity for predicting AKI were 78% and 81%, respectively. In this study, [TIMP-2] × [IGFBP7] was only found to be clinically significant in predicting AKI in patients within 24 hours, but not 72 hours. When [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000, the risk of patients progressing to KDIGO3 stage within 24 hours will be increased by four times.
Other types of AKI: [TIMP-2] × [IGFBP7] predict the risk and prognosis of AKI in critically ill patients and is also widely used in general ICU wards. Fiorenza Ferrari et al. (2019) selected 442 ICU patients for observation. Among them, 188 patients (42.53%) developed AKI. The proportion of patients with [TIMP-2] × [IGFBP7] ≤ 0.3 (ng/mL)2/1000 and [TIMP-2] × [IGFBP7] > 0.3 (ng/mL)2/1000 was 31.9% and 68.1%, respectively. Meanwhile, the AUC of [TIMP-2] × [IGFBP7] for predicting AKI within 12 hours was 0.74 (95% CI 0.69–0.80), the AUC of AKI within 48 hours was 0.70 (95% CI 0.65–0.76), the AUC of AKI from 48 hours to 7 hours was 0.40 (95% CI 0.28–0.52), and [TIMP-2] × [IGFBP7] had the best prediction for severe AKI within 12 hours, with an AUC of 0.82 (95% CI 0.70–0.88). In addition, the risk of AKI increased by 2% for every 0.1(ng/mL)2/1000 units of [TIMP-2] × [IGFBP7] in Logistic regression model.
Applications to Prognosis
Koyner et al. (2014) found [TIMP-2] × [IGFBP7] also had a certain correlation with poor prognosis of AKI in secondary analysis of data after 9-month follow-up in Sapphire study. This study evaluated the value of [TIMP-2] × [IGFBP7] in predicting poor prognosis of AKI using Cox proportional hazard model with all-cause mortality or the need for renal replacement therapy as the composite endpoint. A total of 382 of these patients (55.2%) developed AKI within 72 hours of registration, and 217 patients (31.4%) met the composite endpoint. In univariate analysis, [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000 was associated with an increased risk of the composite endpoint, with a hazard ratio of 2.11 (95% CI 1.3–3.23), while [TIMP-2] × [IGFBP7] at 0.3–2 (ng/mL)2/1000 had a hazard ratio of 1.22 (95% CI 0.91–1.62), which was not significantly associated with an increased risk of the composite endpoint. In multivariable analysis adjusted for clinical model, [TIMP-2] × [IGFBP7] > 0.3 (ng/mL)2/1000 was only associated with a composite endpoint in patients who developed AKI, with adjusted hazard ratios of 1.44 (95% CI 1.00–2.06) for [TIMP-2] × [IGFBP7] at 0.3–2 (ng/mL)2/1000 and 2.16 (95% CI 1.32–3.53) for [TIMP-2] × [IGFBP7] > 2 (ng/mL)2/1000. These evidences suggest that early detection of [TIMP-2] × [IGFBP7] in critically ill patients can not only predict the occurrence of AKI but also have some significance for the prognosis of patients.
[TIMP-2] × [IGFBP7] Disadvantage in Predicting AKI
However, with the deepening of research, many evidences question the value of [TIMP-2] × [IGFBP7] in predicting the risk and prognosis of AKI. Fiorenza Ferrari et al.’s (2019) study stated that the traditional cutoff point for severe AKI was not confirmed in their study, while [TIMP-2] × [IGFBP7] was only optimal in predicting AKI within 12 hours. Bojan et al. (2020) also observed that the use of [TIMP-2] × [IGFBP7] in predicting AKI risk in infants and neonates undergoing cardiac surgery was not significant at 1 hour or 1 to 3 hours after surgery. Zaouter et al.’s (2018) study failed to demonstrate that [TIMP-2] × [IGFBP7] predicted the risk of AKI within 24 hours, within 1 week after cardiac surgery, and only predicted the risk of AKI within 12 hours, with an AUC of 0.65 (95% CI 0.53–0.84). In addition, Titeca-Beauport et al. (2020) found that [TIMP-2] × [IGFBP7] could not be used to accurately distinguish sepsis-related transient and persistent AKI, while other clinical prediction models such as serum creatinine and urine volume had better prediction effect for persistent AKI. These evidences suggest that [TIMP-2] × [IGFBP7], although it is currently an excellent new biomarker for predicting AKI with high specificity and sensitivity, it still faces many challenges, and more clinical studies are needed to validate its ability to predict AKI risk.
Conclusion
As a common clinical syndrome in ICU, early detection, diagnosis, and provision of early renoprotective therapy are important for patients to sustain their lives and improve their prognosis. Cell cycle arrest plays an important role in the occurrence and development of AKI. Cell cycle arrest biomarkers TIMP-2 and IGFBP7 are expected to play a role in clinical practice as biomarkers for early prediction of AKI, but their clinical effects have not been confirmed. Therefore, to explore the clinical effects of [TIMP-2] × [IGFBP7] and study the application of [TIMP-2] × [IGFBP7] in different clinical settings, different pathogenic factors and different patient populations will provide great help for the clinical application of [TIMP-2] × [IGFBP7].
Mini-Dictionary of Terms
-
Acute kidney injury . Acute kidney injury is defined as a clinical syndrome arising from a dramatic decrease in renal function caused by a variety of etiologies and is particularly common in the ICU.
-
Biomarker. Biomarkers refer to the indicator substances reflecting disease changes or therapeutic effects through detecting the proteins, genes, and other substances contained in the human blood, urine, and other body fluids or tissues.
-
Cell cycle arrest . When the cell is stimulated by injury, the cell cycle cannot proceed normally and is blocked at a certain stage, which is called cell cycle arrest.
-
ICU. The concept of ICU is often considered to have originated in the polio epidemic in Copenhagen in 1952 and is a place to provide higher quality medical services for acutely ill patients by concentrating manpower, strengthening equipment allocation, and treating and managing them.
-
[TIMP-2] × [IGFBP7] . Also known as NephroCheck® (NC) test, it was approved by FDA for marketing in 2014. Predict the risk index of AKI in patients by quantitatively measuring the value of [TIMP-2] × [IGFBP7] in urine of patients.
Key Facts of AKI
-
AKI is a clinical syndrome characterized by a dramatic decrease in renal function.
-
AKI is a common complication in ICU. About 57% patients will develop different degrees of AKI within 1 week after admission.
-
Sepsis is the most important cause of AKI in the ICU, and SA-AKI accounts for 45%–70% of all AKI cases.
-
Scr and urine volume are both embodiments of renal function and do not intuitively reflect renal injury and are not conducive to the early diagnosis of AKI.
-
The related studies of [TIMP-2] × [IGFBP7] in predicting AKI in ICU mainly focused on CSA-AKI and SA-AKI.
Key Facts of Cell Cycle Arrest
-
The cell cycle refers to the entire process that cells undergo from the end of the last mitosis to the completion of the next mitosis.
-
The normal cell cycle is regulated by cell cycle checkpoints, and when stimulated by stress, the cell cycle arrests at a certain stage for repair.
-
Transient cell cycle arrest facilitates damage repair, and sustained cell cycle arrest may lead to apoptosis and necrosis.
-
When AKI occurs, the cell cycle of tubular epithelial cells is mainly arrested in G1 and/or G2 phases.
-
Both TIMP-2 and IGFBP7, as cell cycle arrest biomarkers, are closely associated with G1 arrest of TECs and can be detected in urine.
Summary Points
-
Cell cycle arrest biomarkers are mainly used to predict AKI early in the ICU; AKI is a common complication in the ICU, with high mortality and poor prognosis; and early intervention is beneficial to improve prognosis.
-
Both TIMP-2 and IGFBP7 are associated with G1 arrest in renal tubular epithelial cells and can be detected in urine, and the product of TIMP-2 and IGFBP7 has a higher value in predicting AKI.
-
The existing diagnostic criteria do not indicate the occurrence of AKI as early as possible, so the search for biomarkers during early renal injury as novel biomarkers to predict AKI has become a hot topic in current research.
-
[TIMP-2] × [IGFBP7] can not only predict the risk of AKI but also predict the prognosis of AKI patients.
-
Although [TIMP-2] × [IGFBP7] is an excellent AKI biomarker, there are still some problems that need to be verified by more clinical studies.
Abbreviations
- AKI:
-
acute kidney injury
- ALI:
-
acute liver failure
- ATM:
-
activates the ataxia-telangiectasia mutated
- ATR :
-
ataxia telangiectasia and Rad3-related
- CAK:
-
CDK-activating kinase
- CDKs:
-
cyclin-dependent kinases
- CHK1:
-
checkpoint kinase 1
- CKIs:
-
Cdk inhibitors
- CPB :
-
cardiopulmonary bypass
- CSA-AKI:
-
cardiac surgery-associated AKI
- ECMO:
-
extracorporeal membrane oxygenation
- GFR:
-
glomerular filtration rate
- ICU:
-
intensive care unit
- IGFBP7 :
-
insulin-like growth factor-binding protein 7
- IL-18:
-
interleukin-18
- KIM-1:
-
kidney injury molecule-1
- L-FABP:
-
L-type fatty acid-binding protein
- NGAL:
-
neutrophil gelatinase-associated lipocalin
- Rb :
-
Retinoblastoma protein
- SA-AKI:
-
sepsis-associated AKI
- Scr:
-
serum creatinine
- TECs:
-
renal tubular epithelial cells
- TIMP-2:
-
tissue inhibitor of metalloproteinase-2
References
Agami R, Bernards R. Convergence of mitogenic and DNA damage signaling in the G1 phase of the cell cycle. Cancer Lett. 2002;177(2):111–8.
Andrade L, Rodrigues C, Gomes S, et al. Acute kidney injury as a condition of renal senescence. Cell Transplant. 2018;27(5):739–53.
Basile D, Bonventre J, Mehta R, et al. Progression after AKI: understanding maladaptive repair processes to predict and identify therapeutic treatments. J Am Soc Nephrol. 2015;27(3):687–97.
Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute dialysis quality initiative (ADQI) group. Crit Care. 2004;8(4):1–9.
Bihorac A, Chawla LS, Shaw AD, et al. Validation of cell-cycle arrest biomarkers for acute kidney injury using clinical adjudication. Am J Respir Crit Care Med. 2014;189(8):932–9.
Bojan M, Pieroni L, Semeraro M, et al. Cell-Cycle Arrest Biomarkers: Usefulness for Cardiac Surgery-Related Acute Kidney Injury in Neonates and Infants*. Pediatr Crit Care Med. 2020;21(6):563–70.
Ciardo D, Goldar A, Marheineke K. On the Interplay of the DNA Replication Program and the Intra-S Phase Checkpoint Pathway. Genes. 2019;10(2):94.
Cuartero M, Ballús J, Sabater J, et al. Cell-cycle arrest biomarkers in urine to predict acute kidney injury in septic and non-septic critically ill patients. Ann Intensive Care. 2017;7(1)
Ferrari F, Romero-González G, Topete L, et al. Routine Adoption of Urinary [IGFBP7]∙[TIMP-2] to Assess Acute Kidney Injury at Any Stage 12 hours After Intensive Care Unit Admission: a Prospective Cohort Study. Sci Rep. 2019;9(1)
Forni LG, Darmon M, Ostermann M, et al. Renal recovery after acute kidney injury. Intensive Care Med. 2017;43(6):855–66.
Georgakilas A, Martin O, Bonner W. p21: a two-faced genome guardian. Trends Mol Med. 2017;23(4):310–9.
Giannattasio M, Branzei D. S-phase checkpoint regulations that preserve replication and chromosome integrity upon dNTP depletion. Cell Mol Life Sci. 2017;74(13):2361–80.
Gist K, Goldstein S, Wrona J, et al. Kinetics of the cell cycle arrest biomarkers (TIMP-2*IGFBP-7) for prediction of acute kidney injury in infants after cardiac surgery. Pediatr Nephrol. 2017;32(9):1611–9.
Gocze I, Koch M, Renner P, et al. Urinary biomarkers TIMP-2 and IGFBP7 early predict acute kidney injury after major surgery. PLoS One. 2015;10(3):e0120863.
Goel S, DeCristo M, McAllister S, et al. CDK4/6 inhibition in cancer: beyond cell cycle arrest. Trends Cell Biol. 2018;28(11):911–25.
Gomez H, Ince C, De Backer D, et al. A unified theory of sepsis-induced acute kidney injury. Shock. 2014;41(1):3–11.
Gonwa T, Wadei H. Kidney disease in the setting of liver failure: core curriculum 2013. Am J Kidney Dis. 2013;62(6):1198–212.
Gorecki L, Andrs M, Korabecny J. Clinical candidates targeting the ATR–CHK1–WEE1 Axis in cancer. Cancers. 2021;13(4):795.
Griffin B, Liu K, Teixeira J. Critical care nephrology: core curriculum 2020. Am J Kidney Dis. 2020;75(3):435–52.
Gunnerson K, Shaw A, Chawla L, et al. TIMP2•IGFBP7 biomarker panel accurately predicts acute kidney injury in high-risk surgical patients. J Trauma Acute Care Surg. 2016;80(2):243–9.
Holder J, Poser E, Barr F. Getting out of mitosis: spatial and temporal control of mitotic exit and cytokinesis byPP1 andPP2A. FEBS Lett. 2019;593(20):2908–24.
Honore P, Nguyen H, Gong M, et al. Urinary Tissue Inhibitor of Metalloproteinase-2 and Insulin-Like Growth Factor-Binding Protein 7 for Risk Stratification of Acute Kidney Injury in Patients with Sepsis. Crit Care Med. 2016;44(10):1851–60.
Hoste E, McCullough P, Kashani K, et al. Derivation and validation of cutoffs for clinical use of cell cycle arrest biomarkers. Nephrol Dial Transplant. 2014;29(11):2054–61.
Hoste E, Bagshaw S, Bellomo R, et al. Epidemiology of acute kidney injury in critically ill patients: the multinational AKI-EPI study. Intensive Care Med. 2015;41(8):1411–23.
House A. Management of heart failure in advancing CKD: core curriculum 2018. Am J Kidney Dis. 2018;72(2):284–95.
Hume S, Dianov G, Ramadan K. A unified model for the G1/S cell cycle transition. Nucleic Acids Res. 2020;48(22):12483–501.
Ingham M, Schwartz G. Cell-cycle therapeutics come of age. J Clin Oncol. 2017;35(25):2949–59.
Justman Q. Looking beyond the stop sign: cell-cycle checkpoints reconsidered. Cell Syst. 2017;5(5):438–40.
Kalsbeek D, Golsteyn R. G2/M-phase checkpoint adaptation and micronuclei formation as mechanisms that contribute to genomic instability in human cells. Int J Mol Sci. 2017;18(11):2344.
Kashani K, Al-Khafaji A, Ardiles T, et al. Discovery and validation of cell cycle arrest biomarkers in human acute kidney injury. Crit Care. 2013;17(1):1–12.
Kashani K, Cheungpasitporn W, Ronco C. Biomarkers of acute kidney injury: the pathway from discovery to clinical adoption. Clin Chem Lab Med (CCLM). 2017;55(8):1074–89.
Kastan M, Bartek J. Cell-cycle checkpoints and cancer. Nature. 2004;432(7015):316–23.
Kdigo.org. 2021. [online] Available at: https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf. Accessed 31 Oct 2021.
Kellum J, Chawla L. Cell-cycle arrest and acute kidney injury: the light and the dark sides. Nephrol Dial Transplant. 2015;31(1):16–22.
Khoronenkova S, Dianov G. ATM prevents DSB formation by coordinating SSB repair and cell cycle progression. Proc Natl Acad Sci. 2015;112(13):3997–4002.
Koyner J, Shaw A, Chawla L, et al. Tissue inhibitor metalloproteinase-2 (TIMP-2)·IGF-binding protein-7 (IGFBP7) levels are associated with adverse long-term outcomes in patients with AKI. J Am Soc Nephrol. 2014;26(7):1747–54.
Leventhal T, Liu K. What a nephrologist needs to know about acute liver failure. Adv Chronic Kidney Dis. 2015;22(5):376–81.
Lim S, Kaldis P. Cdks, cyclins and CKIs: roles beyond cell cycle regulation. Development. 2013;140(15):3079–93.
Maizel J, Daubin D, Vong L, et al. Urinary TIMP2 and IGFBP7 Identifies High Risk Patients of Short-Term Progression from Mild and Moderate to Severe Acute Kidney Injury during Septic Shock: A Prospective Cohort Study. Dis Markers. 2019;2019:1–8.
Meersch M, Schmidt C, Van Aken H, et al. Urinary TIMP-2 and IGFBP7 as early biomarkers of acute kidney injury and renal recovery following cardiac surgery. PLoS One. 2014;9(3):e93460.
Mehta R, Kellum J, Shah S, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31.
Mohmand H, Goldfarb S. Renal dysfunction associated with intra-abdominal hypertension and the abdominal compartment syndrome: table 1. J Am Soc Nephrol. 2011;22(4):615–21.
Moonen L, D’Haese P, Vervaet B. Epithelial cell cycle behaviour in the injured kidney. Int J Mol Sci. 2018;19(7):2038.
Musacchio A. The molecular biology of spindle assembly checkpoint signaling dynamics. Curr Biol. 2015;25(22):3017.
Nurse P. A long twentieth century of the cell cycle and beyond. Cell. 2000;100(1):71–8.
Oezkur M, Magyar A, Thomas P, et al. TIMP-2*IGFBP7 (Nephrocheck®) measurements at intensive care unit admission after cardiac surgery are predictive for acute kidney injury within 48 hours. Kidney Blood Press Res. 2017;42(3):456–67.
Pack L, Daigh L, Meyer T. Putting the brakes on the cell cycle: mechanisms of cellular growth arrest. Curr Opin Cell Biol. 2019;60:106–13.
Poston J, Koyner J. Sepsis associated acute kidney injury. BMJ. 2019:k4891.
Razo-Vazquez A, Thornton K. Extracorporeal membrane oxygenation—what the nephrologist needs to know. Adv Chronic Kidney Dis. 2016;23(3):146–51.
Schmidt M, Rohe A, Platzer C, et al. Regulation of G2/M transition by inhibition of WEE1 and PKMYT1 kinases. Molecules. 2017;22(12):2045.
Sun J, Zhang J, Tian J, et al. Mitochondria in sepsis-induced AKI. J Am Soc Nephrol. 2019;30(7):1151–61.
Thompson R, Gatenby R, Sidi S. How cells handle DNA breaks during mitosis: detection, signaling, repair, and fate choice. Cell. 2019;8(9):1049.
Titeca-Beauport D, Daubin D, Van Vong L, et al. Correction to: urine cell cycle arrest biomarkers distinguish poorly between transient and persistent AKI in early septic shock: a prospective, multicenter study. Crit Care. 2020;24(1)
Tujios S, Hynan L, Vazquez M, et al. Risk factors and outcomes of acute kidney injury in patients with acute liver failure. Clin Gastroenterol Hepatol. 2015;13(2):352–9.
Vermeulen K, Van Bockstaele D, Berneman Z. The cell cycle: a review of regulation, deregulation and therapeutic targets in cancer. Cell Prolif. 2003;36(3):131–49.
Wang Y, Bellomo R. Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment. Nat Rev Nephrol. 2017;13(11):697–711.
Wang Y, Zou Z, Jin J, et al. Urinary TIMP-2 and IGFBP7 for the prediction of acute kidney injury following cardiac surgery. BMC Nephrol. 2017;18(1)
Whittaker S, Mallinger A, Workman P, et al. Inhibitors of cyclin-dependent kinases as cancer therapeutics. Pharmacol Ther. 2017;173:83–105.
Yan M, Tang C, Ma Z, et al. DNA damage response in nephrotoxic and ischemic kidney injury. Toxicol Appl Pharmacol. 2016;313:104–8.
Yang Y, Luo J, Chen X, et al. CDK4/6 inhibitors: a novel strategy for tumor radiosensitization. J Exp Clin Cancer Res. 2020;39(1)
Zaouter C, Potvin J, Bats M, et al. A combined approach for the early recognition of acute kidney injury after adult cardiac surgery. Anaesth Crit Care; Pain Med. 2018;37(4):335–41.
Zhang M, Zhang L, Hei R, et al. Cdk inhibitors in cancer therapy, an overview of recent development. Am J Cancer Res. 2021;11(5):1913–35.
Zhu S, Pabla N, Tang C, et al. DNA damage response in cisplatin-induced nephrotoxicity. Arch Toxicol. 2015;89(12):2197–205.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this entry
Cite this entry
Zhou, Zj., Yang, B. (2023). Cell Cycle Arrest Biomarkers in the Intensive Care Unit. In: Rajendram, R., Preedy, V.R., Patel, V.B. (eds) Biomarkers in Trauma, Injury and Critical Care. Biomarkers in Disease: Methods, Discoveries and Applications. Springer, Cham. https://doi.org/10.1007/978-3-031-07395-3_10
Download citation
DOI: https://doi.org/10.1007/978-3-031-07395-3_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-07394-6
Online ISBN: 978-3-031-07395-3
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences