Abstract
Enterovirus infections are common in humans worldwide. Enteroviruses are excreted in feces during infection and can be detected from stool specimens by isolation in continuous laboratory cell lines. Characterization of enteroviruses is based on their antigenic and/or genetic properties.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
Four species of enteroviruses (Human enterovirus A to D, genus Enterovirus, family Picornaviridae) cause infections in humans. They include more than 100 antigenically or genetically defined serotypes or types [1]. Clinical manifestations differ from asymptomatic or mild respiratory infections to severe diseases of central nervous system . Typical enterovirus diseases include hand-foot-and-mouth disease and viral meningitis.
The golden standard for enterovirus diagnostics is the isolation of viruses in cell culture. Most of the enteroviruses multiply rapidly in several continuous cell lines routinely used in diagnostic laboratories. The obtained virus isolates have high titers (cell culture infectious doses, CCID50) and they can be further typed by either antigenic (neutralization with serotype-specific antisera) or genetic properties (capsid protein VP1 sequence identities determine the type of the virus). The results of these two typing assays correlate well [2, 3] and the choice of the method relies on the facilities available in the laboratory.
After the molecular typing method became available some years ago, it has been used increasingly because it overcomes some restrictions of the traditional neutralization assay . Type-specific antisera are not available for all of the recently described “new” enterovirus types. Besides, enteroviruses undergo continuous antigenic evolution and the currently circulating viruses may escape the neutralization by the antisera produced about 50 years ago. In addition, the genetic typing is based on the sequences obtained from the VP1 capsid protein coding region and these sequences can be used for molecular epidemiological analysis besides to the identification of the type of the virus.
Enteroviruses multiply in the human intestine and are excreted into feces in high concentrations. The stool specimens are considered the best choice for virus isolation. The number of viruses excreted in the feces may vary from day to day during the infection and so it is recommended that two samples taken at 1–2 days interval should be analyzed for each patient to increase the sensitivity of the assay [4]. Before inoculation into cell cultures, the stool samples are treated with chloroform in order to inactivate the bacteria always present in feces. In addition to the intestine, enteroviruses may infect many other organs and the virus isolation can be attempted also from other clinical specimens, like spinal fluid, respiratory samples, and swap samples from skin lesions. These specimens are collected according to the symptoms of the disease.
We describe here the traditional virus isolation from stool specimens [4], the antigenic typing assay [4] and the VP1 sequence-based type identification [5]. We assume that the readers have already good knowledge on the maintenance of laboratory cell lines, on working on the biosafety level 2 laboratories, and on the principles of the basic molecular biology methods, such as handling of RNA. In addition, the facilities for DNA sequencing and the software for sequence analysis are necessities.
2 Materials
2.1 Enterovirus Isolation
-
1.
Phosphate buffered saline (PBS) with calcium and magnesium ions, pH 7.2–7.4. Store at +4 °C. Supplement the PBS solution with antibiotics to a final concentration of 100 U/ml of penicillin G, 100 μg/ml of streptomycin sulfate, and 50 μg/ml of gentamicin. Store the PBS-antibiotics—solution at +4 °C for up to 1 week.
-
2.
Ethanol-stabilized chloroform (Merck). Store at room temperature, protected from light, in a fume hood.
-
3.
Continuous cell lines that support the growth of enteroviruses (see Note 1 ) seeded and grown in monolayer tube cultures (see Note 2 ).
-
4.
The maintenance media for cells. The media is cell-dependent; for RD(A) mix 100 ml Eagle’s MEM (GIBCO), 2 ml 1 M Hepes pH 7.4, 2 ml 1 M MgCl2, 2 ml heat-inactivated fetal bovine serum (Integro), 25 U/ml mycostatin, and the same antibiotics in the same final concentrations as in the PBS above.
2.2 Enterovirus Typing by Pools of Antisera
-
1.
Antisera pools for enterovirus typing (see Note 3 ). Dilute and store the pools according to the supplier’s instructions.
-
2.
The same cell lines and maintenance media used in the enterovirus isolation (see above). The cells should be seeded and grown in cell culture flasks.
-
3.
PBS without magnesium and calcium ions. Supplement with antibiotics to a final concentration of 100 U/ml of penicillin G, 100 μg/ml of streptomycin sulfate, and 50 μg/ml of gentamicin. Store the PBS-antibiotics—solution at +4 °C for up to 1 week.
-
4.
0.05 % trypsin solution. 0.5 g trypsin (DIFCO), 8.0 g NaCl, 0.4 g KCl, 0.35 g NaHCO3, 1.0 g d(+)-glucose, 0.005 g phenol red sodium salt, 0.2 g EDTA in 1000 ml purified water. Store at −20 °C.
2.3 Enterovirus Typing by Partial VP1 Sequencing
Store all reagents at room temperature unless indicated otherwise.
-
1.
RNeasy™ Mini Kit (Qiagen) for extraction of RNA from the virus isolates (see Note 4 ). Make the working solutions according to the manufacturer’s instructions.
-
2.
Oligonucleotide primers for the RT-PCR and sequencing reactions: 292-sense (5′-MIG CIG YIG ARA CNG G-3′) and 222-antisense (5′-CIC CIG GIG GIA YRW ACA T-3′) [5]. Store the stock solutions at −20 °C. Dilute to the 25 μM concentration for RT-PCR and to the 5 μM concentration for sequencing with RNase-free H2O (Sigma) and store at −20 °C.
-
3.
10× RT-PCR buffer. 670 ml 1 M Tris–HCl pH 8.8, 170 ml 1 M (NH4)2SO4, 0.120 ml 0.5 M EDTA pH 8.0, and 159.88 ml H2O. Store at −20 °C.
-
4.
Mixture of four dinucleotides (dATP, dCTP, dGTP, and dTTP; Roche). Make a solution, which has a 2 mM final concentration of each of the nucleotides in RNase-free H2O (Sigma). Store at −20 °C.
-
5.
25 mM MgCl2 (supplied with the Taq-polymerase, Integro BV). Store at −20 °C.
-
6.
Enzymes for RT-PCR reactions: AMV reverse transcriptase, 20 U/μl (Finnzymes), RNasin Inhibitor-enzyme, 40 U/μl (Promega), and Taq polymerase-enzyme, 5 U/μl (Integro BV). Store at −20 °C.
-
7.
Agarose powder (Lonza).
-
8.
Ethidium bromide (EtBr; BDH Prolabo). One drop from the EtBr bottle into 50 ml of the gel solution gives an EtBr concentration of 0.5 μg/ml.
-
9.
10×TBE-buffer. 61.83 g Tris (Merck), 121.1 g boric acid (ICN), and 7.44 g disodium salt (Titriplex III, Merck), adjust to 1000 ml with distilled H2O. Make the 1:10 (=1 × TBE) working solution with distilled water.
-
10.
100 bp DNA size marker ladder (Generuler, BDH Prolabo). The product is delivered with 6× loading buffer. Make the working dilution of the DNA marker according to the manufacturer’s instructions before use. Store at +4 °C.
-
11.
QIAquick Gel Extraction Kit (QIAGEN) (see Note 5 ). Add 200 ml 99.5 % ethanol into 50 ml of Buffer PE before use.
-
12.
PCR thermocycler, for example GeneAmp 9700 (Applied Biosystems), and tubes, strips, or 96-well plates for RT-PCR reactions, compatible with the PCR thermocycler (see Note 6 ).
-
13.
Equipment needed for preparing the agarose gels and for their electrophoresis. The ultraviolet light supply connected to a camera for viewing and taking pictures of the gel.
3 Methods
3.1 Enterovirus Isolation
-
1.
Add 10 ml PBS (supplemented with antibiotics), about 1 g glass beads (approx. 3 mm in diameter) and 1 ml chloroform to a 15 ml chloroform-resistant centrifuge tube. Transfer approximately 2 g of fecal specimen into the tube with a wooden spatula. Close the tube carefully and shake vigorously for 20 min either manually or using a mechanical shaker. Spin for 20 min at 1500 × g in a refrigerated (+4 °C) centrifuge. Transfer the supernatant (the stool extract) into a storage tube (see Note 7 ). Store at −20 °C.
-
2.
Use at least RD(A) cells for enterovirus isolation (see Note 8 ). Examine the cell cultures microscopically to be sure that the cells are healthy and the monolayer is confluent. Use two parallel cell monolayer tubes for one specimen. Use one tube of each cell type as a negative control. Remove the growth medium from the cells and replace it with 1 ml of warm maintenance medium (+36 °C). Inoculate each tube (excluding the negative control) with 0.2 ml of stool extract, close the caps, and incubate in the stationary position at +36 °C.
-
3.
Examine the cultures with a microscope for the appearance of cytopathic effect (CPE) at least at every 2–3 days. The characteristic enterovirus CPE (rounded cells, which detach from the surface of the tube) develops usually within 2–5 days. When 75–100 % of the cells are affected, freeze the tube at −20 °C. Thaw the tube and do the second passage in order to enrich the virus by inoculating 0.2 ml into a tube containing the same cell line that was used in the first inoculation and 1 ml of maintenance medium. When 100 % CPE is ready, store the tube at −20 °C. Use this second passage virus material for typing.
-
4.
If no CPE appears after 7 days of the first inoculation, perform a blind passage by inoculating 0.2 ml of the first passage into two cell culture tubes and continue examination for a further 7 days. If no CPE is seen, the specimen is recorded as negative in enterovirus isolation (see Note 9 ).
3.2 Enterovirus Typing by Pools of Antisera
Each enterovirus isolate is tested in two dilutions against the pooled enterovirus antisera. The titer of the virus should be approx. 100 CCID50, which is usually achieved by using 1:100 and 1:1000 dilutions of the virus. The exact procedure of the typing assay depends on the pools used; in principle, equal volumes of diluted virus and diluted antisera pools are mixed and incubated for neutralization. The cell suspension is added and the cells are incubated and observed microscopically. The specific antiserum prevents the growth of a given enterovirus and the absence of CPE is recorded as a positive result. The interpretation of the typing results is done according to the supplier’s instructions.
-
1.
Plan the pipetting schedule (antisera, virus dilutions, virus controls, cell controls, and virus titration) and label the 96-well flat-bottomed cell culture microtitre plate accordingly (see Note 10 ).
-
2.
Add 50 μl diluted antisera to the appropriate wells. Add 50 μl maintenance medium to virus control wells. Add 100 μl maintenance medium to cell control wells.
-
3.
Prepare 1:100 and 1:1000 dilutions of the unknown virus. Add 50 μl of either virus dilution to all wells containing antisera and to the virus control wells. Perform a titration of the virus on the same plate (see Note 11 ). Cover the plate with the lid and incubate for 1 h at +36 °C.
-
4.
Detach the cell monolayer from the cell culture flask by using the 0.05 % trypsin solution (see Note 12 ). Prepare a suspension of 100,000–200,000 cells per 1 ml maintenance medium. Distribute 100 μl cell suspension into all wells of the typing plate. Cover the plate with a sealer tape and incubate at +36 °C.
-
5.
Examine daily (or if not possible at 2 or 3 day intervals) by a microscope and record the CPE. Continue recording until 24 h after CPE in the virus control wells reaches 100 %. The virus is identified by the pattern of inhibition of CPE (negative wells have healthy cell monolayers) by antiserum pools (see Note 13 ).
3.3 Enterovirus Typing by Partial VP1 Sequencing
See first Note 14 for good laboratory techniques.
-
1.
Perform RNA extraction according to instructions given by the manufacturer of the extraction kit (see Note 15 ). If RNEasy (Qiagen) is used, elute the RNA into a volume of 40 μl (see Note 16 ). Store at −20 °C until used and at −70 °C for longer time.
-
2.
Prepare the RT-PCR reaction mix in a volume sufficient for all reactions (calculate the number of samples and positive and negative controls) by mixing all reagents in one tube on ice. For one reaction, use 5 μl 10× RT-PCR-buffer, 5 μl 2 mM mixture of dNTPs, 3 μl 25 mM MgCl2 , 2 μl 25 μM sense primer 292, 2 μl 25 μM antisense primer 222, 0.3 μl RNasin Inhibitor (40 U/μl), 0.2 μl AMV-reverse transcriptase (20 U/μl), 0.3 μl Thermoperfect DNA polymerase (5 U/μl), and 31 μl H2O. Mix thoroughly by pipetting up and down. Transfer 49 μl of the RT-PCR reaction mix into tubes or into wells of the PCR strip or plate.
-
3.
Add 1 μl sample RNA, 1 μl positive control RNA, or 1 μl water (negative control) into the tubes or wells containing the RT-PCR mix. Mix by pipetting several times up and down. Seal the caps or cover the plate with a foil.
-
4.
Start the RT-PCR program in the PCR thermocycler (+50 °C for 30 min, +94 °C for 3 min, 35 cycles of (+94 °C for 30 s, +42 °C for 30 s, and +72 °C for 60 s), +72 °C for 5 min, and +4 °C to hold). When the program has reached the first temperature (+50 °C), put the tubes or the strip into the PCR machine and let the program run until the final +4 °C temperature is reached.
-
5.
Visualize the RT-PCR amplicons by using an agarose gel electrophoresis . Assemble the gel casting tray and put the sample comb into its place. Prepare the agarose gel by mixing 4.0 g agarose powder and 200 ml 1× TBE-buffer. Heat in the microwave oven until the solution almost boils. Move it into the fume hood and let the solution cool by gently mixing the bottle until the solution is about +60 °C. Add 4 drops of ethidium bromide; the final concentration of ethidium bromide should be 0.5 μg/ml. Roll the bottle slowly to mix the red EtBr thoroughly into the solution. Pour the gel solution into the casting tray and let it solidify at room temperature for about 30 min. Remove the comb and transfer the gel with its container into the electrophoresis chamber, which contains 1× TBE buffer (see Note 16 ).
-
6.
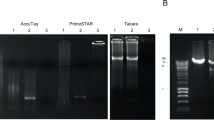
Prepare the samples by mixing 5 μl RT-PCR product and 2 μl 6× loading buffer. Mix by pipetting or vortexing. Pipet the samples into the wells of the agarose gel carefully, avoiding the formation of the air bubbles. Add 7 μl DNA ladder into the outermost wells of the gel. Run the gel at 140 mA for 20–60 min until the fastest color front has moved 3–4 cm from the sample wells. Stop the power supply. Remove the gel from the chamber and take a photo of the gel under the ultraviolet light. The expected size of the RT-PCR amplicon with the primers 292 and 222 is about 340 base pairs (see Note 17 ).
-
7.
Purify the RT-PCR amplicons before sequencing (see Note 18 ). If only one band with a correct size is visible in the gel, use QIAquick PCR purification procedure. If more bands are present, the band of a correct size must be sliced from the gel using the QIAquick Gel Extraction procedure. Perform the purification according to the protocol presented in the manufacturer’s handbook. The final volume of water in the DNA elution step is 40 μl.
-
8.
Sequencing of the purified DNA amplicons may be performed in several ways depending on the facilities available in the laboratory, but, importantly, two sequencing reactions, one with the sense primer and one with the antisense primer, should always be performed for each of the DNA amplicons. We use 3 μl purified DNA amplicon and 1.6 μl 5 μM sense primer for one reaction and 3 μl DNA and 1.6 μl 5 μM antisense primer for the second reaction and add 2.4 μl water into each reaction to reach the final volume of 7 μl. The following steps (the BigDye terminator cycle sequencing reactions, the purification of the amplicons and the analysis of the amplicons on an automated capillary sequencer) are purchased as a full-service from another laboratory.
-
9.
A software package (e.g., Geneious, created by Biomatters and available from www.geneious.com, or Sequencher from Gene Codes Corporation, available from www.genecodes.com ) is needed for analysis of the sequence files. Check carefully the quality of the raw sequence data: the chromatograms should consist of clearly distinguishable sharp calls for each of the four bases. Remove several of the first and the last base calls from the sequences; these are usually not of high quality enough. Assemble the sense and antisense sequences to a contig, check for and edit the ambiguous base calls sometimes seen between the two sequences, and, finally, save the sequence in a text format. Compare the sequence to the GenBank nucleotide data base with BLAST [6]. The enterovirus prototype sequence, which poses the highest nucleotide identity with the query sequence, determines the type of the enterovirus. This identity should be more than 75 % at the nucleotide level (see Note 19 ).
4 Notes
-
1.
Primarily, we use the wide-spectrum rhabdomyosarcoma, RD(A), cells and, if needed, increase the sensitivity of the assay with other cell lines such as HeLa, green monkey kidney (GMK), Vero, and/or CaCo-2. The ICAM-expressing HeLa cells are especially good for those species C enteroviruses that use ICAM-1 as their cellular receptor.
-
2.
The cells can be seeded, grown, and inoculated also in 6-, 12-, or 24-well plates, but be aware of the risk for cross-contamination when handling multiple specimens at the same time.
-
3.
The laboratories in the WHO Polio Laboratory Network use pooled horse antisera prepared at the National Institute of Public Health and the Environment (RIVM), Bilthoven, The Netherlands. This set of enterovirus typing antisera contains seven pools for the 20 most common echoviruses and Coxsackie virus A9, one pool for six Coxsackie B viruses and one trivalent pool for three poliovirus serotypes. Enterovirus typing pools are also commercially available. The compositions of antisera and thus the capability of typing the different enterovirus serotypes may vary in different pools. In addition, antisera for single enterovirus serotypes are available for example from the Swedish Institute for Infectious Disease Control (SMI).
-
4.
There are many other traditional and commercially available methods, which can be used for the extraction of viral RNA as well. Typically, the virus isolates obtained by propagation in cell cultures contain so large amount of viruses that the sensitivity of the RNA extraction method is not a limiting factor in the assay.
-
5.
The QIAQuick (Qiagen)-kit is used for purification of the RT-PCR products before sequencing. The corresponding methods are available from many manufacturers. We have good experience also on the PCR CheckIT gels from Elchrom Scientific.
-
6.
Any thermocycler with adjustable temperatures and incubation times can be used. Tubes, strips or 96-well plates should be compatible with the PCR machine. We use 96-well plates from Thermo-Fast and close the plates with foil seals from Abgene.
-
7.
Be careful not to take with the chloroform when pipetting the supernatant. The chloroform is toxic for the cells in the virus isolation step. If the supernatant is not clear after the centrifugation, repeat the chloroform treatment and the centrifugation.
-
8.
RD(A) cells support growth of most of the enteroviruses. The sensitivity of the virus isolation assay can be increased by using simultaneously more cell lines. However, the cell preferences of different enterovirus species, types or strains cannot be guaranteed. According to our experience, Coxsackie B viruses multiply rapidly and efficiently in HeLa cells, some but not all of the Coxsackie A viruses grow better in HeLa than in RD(A) cells, echoviruses grow well in RD(A) cells, but also in GMK and Vero cells , CaCo-2 cells support growth of many echoviruses, and enterovirus 71 multiplies slowly but still induces visible CPE both in Vero and in RD(A) cells. The L20B cells are more specific for polioviruses and they are used in the clinical (acute flaccid paralysis , AFP) surveillance for polioviruses.
-
9.
Some enterovirus strains may need longer incubation times than 7 days for the full CPE. For example, enterovirus 71 produces CPE slowly in Vero cells and the CPE should be monitored for up to 10 days. If the 75–100 % CPE is not achieved before the cells begin to degenerate due to their age, do the third passage in freshly seeded cells. Some enteroviruses do not infect/produce visible CPE in the laboratory cell lines. The clinical specimen may be positive in diagnostic enterovirus PCR while being negative in the virus isolation.
-
10.
You can find an example for the working chart from the Polio Laboratory Manual [4].
-
11.
The titer of the unknown virus should be about 100 CCID50/well. If the titer is lower, the negative result (no CPE) is not reliable. If the titer is higher, the amount of antisera may not be sufficient for total neutralization (CPE appears).
-
12.
The trypsinization time depends on the cell line; for RD(A) the time is approximately 30 s.
-
13.
Sometimes the typing assay fails to identify the analyzed virus. The virus may be newly discovered or new and thus the specific antiserum for a given virus is not included in the antisera pools. Alternatively, the virus may have drifted antigenically and the sera fail to identify it. The virus isolate may contain a mixture of two or more enterovirus types, which interferes with the interpretation of the results. The virus may be in an aggregated form which prevents the neutralization by specific antisera; in this case the isolate can be retested after dissolving the aggregates by the chloroform treatment.
-
14.
We use four separate laboratory rooms for the different phases of the procedure to avoid contamination. The virus RNA extraction is done in the biosafety level 2 laboratory; the reagents and mixtures for the RT-PCR are prepared in a clean pre-PCR laboratory, the RNA template is added in the third laboratory and, finally, the RT-PCR products are handled in the post-PCR laboratory. All laboratory safety cabins are cleaned thoroughly before and after work. The filter tips are used in all pipets. The most obvious contaminants are infectious viruses, which readily spread via aerosol, and RT-PCR products, which contain a lot of DNA and can be spread for example by aerosol or contaminated gloves.
-
15.
We always include a negative control (nuclease-free water) in the extraction step. This control is analyzed in the RT-PCR and it should not give any visible amplicons on an agarose gel.
-
16.
Be careful when extracting and handling RNA, because RNA is readily degraded by RNases. Be sure that all the reagents and plastic ware are RNase-free.
-
17.
The electrophoresis buffer should rise about 0.5 cm above the gel. The buffer should be changed once a week. If the wells contain air bubbles, remove them for example with the pipet tip.
-
18.
If no enterovirus amplicons (size of approx. 340 base pairs) are seen, reproduce the RT-PCR with a second set of pan-enterovirus primers, 040, 011, and 012 [7]. The enterovirus amplicon obtained with these primers has a size of approx. 450 base pairs.
-
19.
Because of the extensive genetic evolution some currently circulating enterovirus strains of species C may have less than 75 % nucleotide identities with the prototype strains [8]. In these cases, the typing can be based on the most closely matching enterovirus isolate sequences in the GenBank. If the query sequence is not closely related to any of the GenBank sequences (nucleotide identities <75 % and amino acid identities <85 %), you may have succeeded in isolating a new enterovirus not characterized before. If you suspect a new enterovirus type, please contact the Picornavirus Study Group (www.picornastudygroup.com) for further instructions.
References
Smura T, Savolainen-Kopra C, Roivainen M (2011) Evolution of newly described enteroviruses. Future Virol 6:109–131
Oberste MS, Maher K, Kilpatrick DR et al (1999) Molecular evolution of the human enteroviruses: correlation of serotype with VP1 sequence and application to picornavirus classification. J Virol 73:1941–1948
Blomqvist S, Paananen A, Savolainen-Kopra C et al (2008) Eight years of experience with molecular identification of human enteroviruses. J Clin Microbiol 46:2410–2413
World Health Organization (2004) Polio laboratory manual, 4th edn. WHO, Geneva, Switzerland
Oberste MS, Nix WA, Maher K et al (2003) Improved molecular identification of enteroviruses by RT-PCR and amplicon sequencing. J Clin Virol 26:375–377
Altschul SF, Gish W, Miller W et al (1990) Basic local alignment search tool. J Mol Biol 2215:403–410
Oberste MS, Maher K, Kilpatrick DR et al (1999) Typing of human enteroviruses by partial sequencing of VP1. J Clin Microbiol 37:1288–1293
Brown BA, Maher K, Flemister MR et al (2009) Resolving ambiguities in genetic typing of human enterovirus species C clinical isolates and identification of enterovirus 96, 99 and 102. J Gen Virol 90:1713–1723
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Blomqvist, S., Roivainen, M. (2016). Isolation and Characterization of Enteroviruses from Clinical Samples. In: Martín, J. (eds) Poliovirus. Methods in Molecular Biology, vol 1387. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3292-4_3
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3292-4_3
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3291-7
Online ISBN: 978-1-4939-3292-4
eBook Packages: Springer Protocols