Abstract
Post-traumatic stress disorder (PTSD) is an anxiety disorder that can develop following a traumatic event. Previous studies have found abnormal functional connectivity between the thalamus and other brain regions. However, the traditional functional connectivity method cannot investigate the directional flow of the influence in PTSD. In the present study, we used an effective connectivity method based on Granger causality to explore altered direction of causal information flow within a network associated with the thalamus in PTSD. Employing this method, we found that PTSD patients exhibited increased influence from thalamus to middle/inferior frontal gyrus and insula, and increased bidirectional influences between thalamus and medial prefrontal cortex compared to healthy controls. This is the first study to reveal a network of abnormal effective connectivity in PTSD. In addition, using the machine learning approach, we found that the altered functional measurements could differentiate patients from healthy controls. Our findings may have important implications for the pathophysiological basis underlying PTSD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Post-traumatic stress disorder (PTSD) is a prevalent anxiety disorder that can develop after exposure to a traumatic event. Motor vehicle accidents have been regarded as the common cause of PTSD (Silove et al. 2006). PTSD patients often suffer from a number of symptoms, including intrusive recollections of the trauma, hyperarousal and hypervigilance, and avoidance of trauma reminders (Blake et al. 1995). Although the symptoms of PTSD are familiar and readily identifiable, the effective connectivity relationship between brain regions underlying PTSD remains unclear.
Recently, resting-state functional magnetic resonance imaging (fMRI) has been considered to be an effective noninvasive technique for investigating pathophysiological basis of psychiatric and neurological disorders (Barkhof et al. 2014). Although several previous fMRI studies have found disrupted functional connectivity between thalamus and other brain regions in PTSD (Kennis et al. 2013; Yin et al. 2011), the directionality of the influence between separate brain regions remains unclear.
Exploration on directed pathways of information transfer between brain regions is a key issue and helps to advance our understanding of the abnormal brain function in psychiatric and neurological disorder. Granger causality (GC) was initially used to assess causal relationship between two time series of the economic sciences (Granger 1969). In our study, we applied GC method to fMRI data to investigate directed dynamical connectivity, which can provide novel information toward demonstrating the effective connectivity relationship between brain areas. It is a method based on multiple linear regression for exploring whether one time series could correctly predict another (Stephan and Roebroeck 2012). Compared with functional connectivity method that calculates intrinsic connections between spatially distinct brain regions, the GC method has the advantage of revealing both the direction and the strength of the information flow in brain circuits.
In the present study, we used the voxel-wise GC method and selected bilateral thalamus as seed regions to evaluate altered directional connectivity patterns from and to the thalamus in the resting-state in PTSD patients. In addition, we used the machine learning approach to examine brain-based predictors of PTSD patients. We hypothesized that effective connectivity networks of thalamus were disrupted in PTSD patients. These findings may have important implications for understanding of the pathophysiological basis underlying PTSD and provide the new evidence for the abnormal connectivity in this disorder.
Methods
Participants
Twenty PTSD patients with motor vehicle accidents and twenty age-, sex-, and education-matched healthy controls (HCs) were recruited (age 32.92 ± 8.48 years and 31.53 ± 7.43 years, respectively; gender 13 male/7 female and 14 male/6 female, respectively; education 11.20 ± 3.80 years and 13.00 ± 2.20 years, respectively). PTSD diagnosis was made using the Clinician-Administered PTSD Scale for DSM-IV (CAPS-DX). All participants had no history of psychiatric, neurological disorders and head injury.
MRI data acquisition
All images were obtained by a 3.0 T Siemens MRI scanner (Trio; Siemens Medical, Erlangen, Germany). Resting-state fMRI data were acquired using the echo-planar imaging (EPI) sequence with the following protocols: repetition time (TR) = 2000 ms, echo time (TE) = 30 ms, flip angle (FA) = 90°, matrix = 64 × 64, slice thickness = 3 mm, transverse slices = 36, and field of view (FOV) = 220 mm × 220 mm.
Data preprocessing
All fMRI data were preprocessed using Data Processing Assistant for Resting-State fMRI (DPARSF) (Yan and Zang 2010). The first ten volumes were discarded for equilibrium. Then slice-timing correction and realignment for head motion correction were performed. No translation or rotation parameters in any participants exceeded 3 mm or 3°. In addition, the imagings were further spatially normalized to the Montreal Neurological Institute EPI template image, and each voxel was resampled to 3 × 3 × 3 mm3. Then, the data were spatially smoothed using Gaussian kernel of 6 mm FWHW and detrended to abandon linear trend. After this, several sources of spurious variance were then removed from the data using linear regression, including Friston-24 head motion parameters, white matter signal, and cerebrospinal fluid. Finally, the data were temporally band-pass filtered (0.01–0.08 Hz) to reduce the effects of low-frequency drift and high-frequency noise.
Granger causality method
The bilateral thalamus of the automated anatomical labeling template was selected as the region of interest for the effective connectivity analysis. GC was used to describe the effective connectivity analysis between the seed regions and all other brain regions. The averaged time series of the seed region was defined as the seed time series X, and the time series Y represents the time series of voxels within the whole brain. The linear direct effect of X on Y (F x→y ) and the linear direct effect of Y on X (F y→x ) were calculated voxel by voxel within the whole brain. Therefore, two GC maps for each participant were obtained.
The calculation of GC method value was based on the Geweke’s feedback model (Geweke 1982).
The autoregressive representation:
The joint regressive representation:
Finally,
where X t is the seed region signal and Y t is the other voxels signal, ɛ t and \(\varepsilon_{t}^{{\prime }}\) are the residuals of autoregression, \(\mu_{\text{t}}\) and \(\mu_{t}^{{\prime }}\) are residuals, and Z t is the covariate. F x→y represents directional influence from the time series X to Y. F y→x represents directional influence from the time series from Y to X.
Statistical analysis
Mean values of F x→y and F y→x maps were calculated. The two-sample t test was conducted on the GC method data in SPM8 to test the group differences between the PTSD patients and HCs. The multiple comparison correction was conducted using the AlphaSim program in the REST software (http://resting-fmri.sourceforge.net). The significance levels were set at p < 0.05.
The pattern classification
Pattern classification was included to address the potential effects related to group difference in more detail. The support vector machine (SVM) was applied to the GC, which found significant difference through statistical analysis. Therefore, the SVM, based on the LIBSVM implementation with linear kernel and default parameter, was applied using a leave-one-out cross-validation procedure. Furthermore, the statistical significance of pattern classification was assessed using permutation testing.
Results
In the present study, the F x→y represents strength of the directed information flow from the thalamus to the other brain regions. The F y→x represents strength of the directed information flow from the other brain regions to the thalamus. We found altered F x→y and F y→x of bilateral thalamus in the PTSD patients relative to the HCs using the two-sample t test.
Effective Connectivity from and to the Left Thalamus
Compared with HCs, PTSD patients exhibited significantly increased effective connectivity from the left thalamus to left inferior frontal gyrus and insula (left thalamus with F x→y ), and increased effective connectivity from the medial prefrontal cortex (MPFC) to left thalamus (left thalamus with F y→x ) (p < 0.05, AlphaSim corrected) (shown in Table 1; Fig. 1).
Between-group differences of effective connectivity from and to the left thalamus. a represents the effective connectivity from the left thalamus to other brain regions. b represents the effective connectivity from other brain regions to left thalamus. The red color represents the brain regions that show significantly increased effective connectivity
Effective connectivity from and to the right thalamus
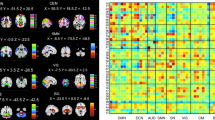
Compared with HCs, PTSD patients also exhibited significantly increased effective connectivity from the right thalamus to left middle frontal gyrus and MPFC, (right thalamus with F x→y ) and significantly increased effective connectivity from the MPFC to right thalamus (right thalamus with F y→x ) (p < 0.05, AlphaSim corrected) (shown in Table 2; Fig. 2).
Between-group differences of effective connectivity from and to the right thalamus. a represents the effective connectivity from the right thalamus to other brain regions. b represents the effective connectivity from other brain regions to right thalamus. The red color represents the brain regions that show significantly increased effective connectivity
Overall classifier performance
The classification analysis showed a correct classification rate of 77.5% (p < 0.001) with sensitivity of 70.0% and specificity of 85.0%. Taking each subject’s discriminative score as a threshold, the receiver operating characteristic (ROC) curve of the classifier was yielded (Fig. 3). The area under the ROC curve (AUC) was 0.895, indicating a good classification power.
Discussion
To the best of our knowledge, this is the first study using GC method to examine effective connectivity network associated with the thalamus in PTSD patients. We found that PTSD patients exhibited abnormal directionality of influence both from and to the thalamus.
GC method is a valuable tool to explore effective functional connectivity in psychiatric and neurological disorders, and it can supply information about the dynamics and directionality of BOLD (blood oxygenation level-dependent) signal in brain circuits. In the present study, an autoregressive model was applied for data analyzing. We used F value based on the decrease of the variance of residual to explore effective connectivity in participants. Using the GC method, we can detect the abnormalities in directional flow of the influence in PTSD patients. We found increased influence from the left thalamus to the left inferior frontal gyrus and insula, from the right thalamus to the left middle frontal gyrus, and mutual increased influences between MPFC and thalamus. The prefrontal cortex has been thought to be involved in encoding and retrieval of memories and emotional processing (Etkin et al. 2011). The insula plays a key role in emotional processing and cognitional processing (Gu et al. 2013; Menon and Uddin 2010). Thus, the findings in our study may suggest the abnormal emotional processing and cognitive processing in PTSD patients. One limitation is that the small sample size in our study should be noticed. Future studies will require larger sample size and divide the patients into subgroups according to their illness duration to confirm our findings.
Conclusion
In this study, we firstly found abnormal effective connectives in several thalamus-related pathways, which were involved in emotional processing and cognitive processing. In addition, employing the machine learning approach, we found that the abnormal functional measurements could differentiate PTSD patients from HCs. Our findings added important insights into understanding the effective connectivity networks and neural circuitry underlying PTSD.
References
Barkhof F, Haller S, Rombouts SA (2014) Resting-state functional MR imaging: a new window to the brain. Radiology 272:29–49
Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM (1995) The development of a clinician-administered PTSD scale. J Trauma Stress 8:75–90
Etkin A, Egner T, Kalisch R (2011) Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cognit Sci 15:85–93
Geweke J (1982) Measurement of linear dependence and feedback between multiple time series. J Am Stat Assoc 77:304–313
Granger CW (1969) Investigating causal relations by econometric models and cross-spectral methods. Econom J Econom Soc 37:424–438
Gu X, Hof PR, Friston KJ, Fan J (2013) Anterior insular cortex and emotional awareness. J Comp Neurol 521:3371–3388
Kennis, M, Rademaker, A.R, van Rooij, S J, Kahn, R S, Geuze, E (2013) Altered functional connectivity in posttraumatic stress disorder with versus without comorbid major depressive disorder: a resting state fMRI study. F1000Research 2:289. doi:10.12688/f1000research.2-289.v2
Menon V, Uddin LQ (2010) Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 214:655–667
Silove D, Brooks R, Steel Z, Blaszczynski A, Hillman K, Tyndall K (2006) Can structured interviews for posttraumatic stress disorder assist clinical decision-making after motor vehicle accidents? An exploratory analysis. Compr Psychiatry 47:194–200
Stephan KE, Roebroeck A (2012) A short history of causal modeling of fMRI data. Neuroimage 62:856–863
Yan C, Zang Y (2010) DPARSF: a MATLAB toolbox for “pipeline” data analysis of resting-state fMRI. Front Syst Neurosci 14:421–438
Yin Y, Jin C, Hu X, Duan L, Li Z, Song M, Chen H, Feng B, Jiang T, Jin H (2011) Altered resting-state functional connectivity of thalamus in earthquake-induced posttraumatic stress disorder: a functional magnetic resonance imaging study. Brain Res 1411:98–107
Authors’ contributions
HC and YZ designed the study. YZ, HC, and ZL analyzed the imaging data. YZ, QC, and HC wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The work is supported by the National High Technology Research and Development Program of China (863 Program) (2015AA020505), the Natural Science Foundation of China (61533006 and 31400901), the Fundamental Research Funds for the Central Universities (ZYGX2013Z004).
Competing interests
The authors declare that they have no competing interests.
Declarations
There are ethical restrictions on the data, and the authors do not have ethical approval to make the data publicly available. Please send requests via email to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Zhang, Y., Chen, H., Long, Z. et al. Altered effective connectivity network of the thalamus in post-traumatic stress disorder: a resting-state FMRI study with granger causality method. Appl Inform 3, 8 (2016). https://doi.org/10.1186/s40535-016-0025-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40535-016-0025-y