Abstract
Background
Insulin resistance is considered to be an important factor in the progression of fibrosis and the enhancement of the risk of hepatocellular carcinoma (HCC) for chronic hepatitis C patients. The aim of this study was to assess the effect of insulin resistance on the development of HCC by non-cirrhotic chronic hepatitis C patients treated with pegylated interferon alpha-2b (PEG-IFNα2b) and ribavirin.
Methods
This retrospective study consisted of 474 Japanese non-cirrhotic patients with chronic hepatitis C. The cumulative incidence of HCC was estimated using the Kaplan-Meier method, according to insulin resistance by the homeostasis model assessment of insulin resistance (HOMA-IR) and treatment outcome.
Results
The overall sustained virological response (SVR) rate was 45.1 % (214/474, genotype 1: 35.4 % [129/364] and genotype 2: 77.3 % [85/110]). Twenty-one (4.4 %) patients developed HCC during the follow-up period. The 5-year cumulative incidence of HCC of the SVR group (2.6 %) was significantly lower than that of the non-SVR group (9.7 %) (log-rank test: P = 0.025). In multivariable logistic regression analysis, HOMA-IR (≥2.5) (hazard ratio [HR] 12.8, P = 0.0006), fibrosis status (F3) (HR 8.85, P < 0.0001), and post-treatment alanine aminotransferase (ALT) level (≥40 U/L) (HR 4.33, P = 0.036) were independently correlated to the development of HCC. Receiver operating characteristic analysis to determine the optimal threshold value of HOMA-IR for predicting the development of HCC in the non-SVR group showed that the areas under the curve was high (0.80, cutoff value: 3.0). Only three patients (1.4 %) who achieved SVR developed HCC. Two of them had severe insulin resistance and did not show improvement in HOMA-IR after achieving SVR.
Conclusions
Insulin resistance has a strong impact on the development of HCC by non-cirrhotic patients who have PEG-IFNα2b and ribavirin treatment failure.
Similar content being viewed by others
Background
Hepatitis C virus (HCV) is a major cause of chronic liver disease, including chronic hepatitis C, which often progresses to cirrhosis and hepatocellular carcinoma (HCC) [1, 2]. The aim of antiviral treatment with interferon (IFN) for HCV-infected patients is not only achievement of sustained viral eradication [3], but also prevention of HCC and liver-related death [4–9]. In spite of recent, marked advances in anti-HCV treatment, HCC is the fifth most common cancer and the third leading cause of cancer-related mortality worldwide [10]. Furthermore, the occurrence of HCC is increasing because of HCV infection, which has infected approximately 170 million people globally.
HCV-infected patients who obtain a sustained virological response (SVR) by IFN monotherapy or pegylated-IFN-alpha (PEG-IFNα) and ribavirin demonstrate significant improvement in liver fibrosis [11, 12] and a decrease in the occurrence of decompensated liver disease and HCC [4–9] compared with untreated or non-SVR patients. Furthermore, male, older age, cirrhosis, non-SVR, and alpha-fetoprotein (AFP) level were reported to be associated with the development of HCC [6, 7].
Among other factors related to the development of HCC, insulin resistance has been reported to be an important factor in fibrosis progression [13] and enhancing hapatocarcinogenesis through multiple pathways with branched-chain amino acid-induced inhibition [14] or oxidative/endoplasmic reticulum stress after postprandial hyperglycemia [15, 16]. Insulin resistance is usually measured clinically by the homeostasis model assessment of insulin resistance (HOMA-IR) [17]. Although we recently reported that insulin resistance undermined the efficacy of HCV clearance in PEG-IFNα2b and ribavirin treatment [18], no reports of the possible association of insulin resistance with the development of HCC after antiviral treatment for non-SVR patients have been provided. This information will be useful for prioritizing patients being considered for treatment with next generation direct-acting antivirals (DAA), especially for non-cirrhotic patients.
The aim of this retrospective study was to evaluate the impact of insulin resistance, by HOMA-IR, on HCC after PEG-IFNα2b and ribavirin treatment for non-cirrhotic patients, based on biopsy or transient elastography (FibroScan).
Methods
Patients
This retrospective study consisted of 609 consecutive Japanese patients with chronic HCV infection aged 18 years or older treated with PEG-IFNα2b and ribavirin between December 2004 and November 2010. Patients were enrolled at Kyushu University Hospital, three affiliated hospitals, or one clinic in the northern Kyushu area of Japan (Mitsutake, Yokota, and Haradoi hospitals, and the Kyushu General Internal Medicine Clinic).
The exclusion criteria were: (1) liver cirrhosis measured by biopsy or transient elastography (FibroScan); (2) history of HCC; (3) HCC development during antiviral treatment; (4) PEG-IFNα2b and ribavirin treatment discontinuation; (5) anti-diabetic medication or insulin injection; (6) positivity for antibody to human immunodeficiency virus or positivity for hepatitis B surface antigen; (7) excessive active alcohol consumption (a daily intake of more than 60 g of ethanol) or drug abuse; or (8) other forms of liver disease (e.g. autoimmune hepatitis, primary biliary cholangitis, hemochromatosis). After exclusions, the data of 474 patients was available for analysis. The baseline characteristics of the patients are shown in Table 1. The median follow-up period after the end of treatment was 4.3 (range 0.5–7.2) years. The study was conducted in accordance with the ethical principles of the 2008 Declaration of Helsinki and was approved by the Ethics Committee of Kyushu University hospital.
Assessment of clinical and laboratory findings
Baseline clinical parameters included serum alanine aminotransferase (ALT), total cholesterol, plasma glucose, serum insulin, serum AFP, platelet count, and hemoglobin A1c (HbA1c), all measured by standard laboratory techniques at Kyushu University Hospital or a commercial laboratory (SRL Laboratory, Tokyo, Japan) within 1 week before the initiation of treatment. The Japan Diabetes Society (JDS) value of HbA1c was converted for use in this study to a National Glycohemoglobin Standardization Program (NGSP) assigned value by adding 0.4 % [19]. Body mass index was defined as the body mass divided by the square of the height, which is universally expressed in units of kg/m2. Clinical follow-up of HCV viremia was done by real-time reverse transcriptase PCR assay (COBAS TaqMan HCV assay) (Roche Diagnostics, Tokyo, Japan), with a lower limit of quantitation of 15 IU/mL and an outer limit of quantitation of 6.9X107 IU/mL (1.2 to 7.8 log IU/mL referred to log10 IU/mL) or COBAS Amplicor HCV Monitor Test v2.0 (Roche) using the 10-fold dilution method, with a lower limit of quantitation of 5,000 IU (5 kIU/mL) and an outer limit of quantitation of 5,100,000 IU (5,100 kIU/mL).
Assessment of insulin resistance
Insulin resistance was measured from fasting samples using HOMA-IR and calculated as fasting serum insulin (μU/mL) × fasting plasma glucose (mg/dL)/405 [17]. HOMA-IR was measured within 1 week before the initiation of treatment. Serum and plasma samples were collected at least 12 h after an overnight fast. Aliquots of fresh serum and plasma samples from each patient were immediately separated and sent at 4 °C to the hospital laboratory for the measurement of serum insulin and plasma glucose.
Assessment of liver fibrosis
Ultrasound-guided liver biopsy was done by experienced hepatologists within 1 month before initiation of antiviral therapy. The minimum length of the liver biopsy was 15 mm and at least 10 complete portal tracts were necessary for inclusion. For each specimen, the stage of fibrosis was established according to the METAVIR score [20]. The liver cirrhosis of patients with no liver biopsy was diagnosed by transient elastography (FibroScan value ≥14.9 kilopascal; the cutoff value that indicates a negative predictive value for cirrhosis is 100 %) [12].
Antiviral treatment and patient follow-up
All HCV genotype 1 patients received a combination treatment of PEG-IFNα2b (PEG-Intron; MSD K.K., Tokyo, Japan) and ribavirin (Rebetol; MSD) for 48–72 weeks: The same regimen was done for 24 weeks for genotype 2 patients. Successful treatment was an SVR, defined as undetectable HCV RNA at 24 weeks after the end of treatment. In order to investigate the post-treatment incidence of HCC, the length of the follow-up period was calculated from the end of antiviral treatment to the diagnosis of HCC or the last follow-up visit up to December 2012.
Serum ALT and AFP measurement and abdominal imaging (ultrasonographic examination, or computed tomography) were done every 3–6 months for each patient. The HCC diagnosis was confirmed by needle biopsy, histology of surgically resected specimens, or characteristic radiological findings.
Statistical analysis
Statistical analyses were conducted using SPSS Statistics version 22.0 (IBM SPSS Inc, Chicago, IL, USA). Baseline continuous data are expressed as median (first-third quartiles) and categorical variables are reported as frequencies and percentages. Univariate analyses were done using the Chi-square, Fisher’s Exact, or Mann-Whitney U test as appropriate. Variables with P < 0.10 in univariate analysis were evaluated using multivariate logistic regression to identify variables significantly associated with the incidence of HCC. The results are expressed as hazard ratios (HR) and their 95 % confidence interval (CI).
Receiver operating characteristic (ROC) curve analysis was done to evaluate the relationship between the HOMA-IR level and HCC development. The cutoff values were calculated from the ROC curve to maximize the total sensitivity and specificity. Cumulative incidence curves of HCC according to response to antiviral treatment or insulin resistance were plotted using the Kaplan-Meier method, and differences among groups were assessed using the log-rank test. The time frame for HCC incidence was defined as the time from the end of antiviral treatment to the diagnosis of HCC. A P value less than 0.05 was regarded as statistically significant in all analyses.
Results
Patient characteristics
Of the 474 patients enrolled, 364 (76.7 %) were infected with HCV genotype 1 and 110 (23.2 %) were genotype 2. The median age was 58, and 48.5 % of the patients were men. Almost all (88.8 %) received liver biopsy within the 2 weeks before the initiation of antiviral therapy, with the others diagnosed by FibroScan.
Of the studied patients, 214 (45.1 %) achieved SVR. The SVR rate of patients infected with HCV genotype 1 was 35.4 % (129/364), significantly lower than the 77.3 % (85/110) found for patients with genotype 2 (P < 0.0001).
Development of HCC
Twenty-one (4.4 %) patients developed HCC during the follow-up period. The baseline characteristics of these patients classified by the development of HCC are shown in Table 2. By univariate analysis, the development of HCC was associated with older age (≥60 years) (P = 0.0085), higher pre-treatment ALT level (≥40 U/L) (P = 0.042), higher post-treatment ALT level (≥40 U/L) (P < 0.0001), higher AFP level (≥10.0 ng/mL) (P = 0.0030), higher fasting serum insulin level (≥15.0 μU/mL) (P = 0.0033), higher HOMA-IR (≥2.5) (P < 0.0001), advanced fibrosis (METAVIR F3), and non-SVR (P < 0.0001). In multivariable logistic regression analysis, significant independently related factors of HCC were post-treatment ALT level (≥40 U/L) (HR 4.33, 95 % CI 1.09–24.8, P = 0.036), HOMA-IR (≥2.5) (HR 12.8, 95 % CI 2.81–93.0, P = 0.0006), and fibrosis status (F3) (HR 8.85, 95 % CI 2.99–29.3, P < 0.0001). For these non-cirrhotic patients, age and treatment outcome were not extracted as independent factors related to the development of HCC.
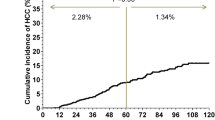
Overall cumulative incidence of HCC classified by treatment outcome
Of the 260 non-SVR patients, 19 (7.3 %) developed HCC, whereas only three (1.4 %) of the 214 patients with SVR did so. The 5-year cumulative incidence rate of HCC of the SVR (2.6 %) group was significantly lower than that of the non-SVR group (9.7 %) (log-rank test: P = 0.025) (Fig. 1).
ROC curve analysis of the effect of HOMA-IR on the development of HCC
ROC curve analysis was done to determine the optimal threshold values of the HOMA-IR levels for predicting the occurrence of HCC in the non-SVR group. The AUROC was 0.80 and the cut-off HOMA-IR level was 3.0 (sensitivity 90.5 %, specificity 73.1 %, positive predictive value 13.5 %, negative predictive value 99.4 %).
Cumulative incidence of HCC for non-SVR patients, classified by HOMA-IR and post-treatment ALT level
The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with post-treatment ALT <40 U/L, classified by HOMA-IR using the 3.0 cut-off level, are shown in Fig. 2a. The 5-year cumulative incidence of HCC in the HOMA-IR ≥3.0 (6.2 %) group was higher, but not significantly, than that of the HOMA-IR <3.0 (0 %) group (log-rank test: P = 0.095). The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with post-treatment ALT ≥40 U/L, classified by HOMA-IR, are shown in Fig. 2b. The 5-year cumulative incidence of HCC in the HOMA-IR ≥3.0 (22.3 %) group was significantly higher than that of the HOMA-IR <3.0 (2.0 %) group (log-rank test: P = 0.0042).
Cumulative incidence of HCC according to insulin resistance (cut-off HOMA-IR 3.0) for non-SVR patients with a normal post-treatment ALT level (<40 U/L) and b high post-treatment ALT level (≥40 U/L). HCC, hepatocellular carcinoma; HOMA, homeostasis model assessment of insulin resistance; SVR, sustained virological response; ALT alanine aminotransferase
Cumulative incidence of HCC for non-SVR patients, classified by HOMA-IR and fibrosis
The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with F0-2, classified by HOMA-IR, are shown in Fig. 3a. The 5-year cumulative incidence of HCC in the HOMA-IR ≥3.0 (11.4 %) group was significantly higher than that of the HOMA-IR <3.0 (0 %) group (log-rank test: P = 0.025). The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with F3, classified by HOMA-IR, are shown in Fig. 3b. The 5-year cumulative incidence of HCC in the HOMA-IR ≥3.0 (32.2 %) group was significantly higher than that of the HOMA-IR <3.0 (4.6 %) group (log-rank test: P = 0.015).
Cumulative incidence of HCC for non-SVR patients, classified by HOMA-IR and AFP level
The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with AFP <10 ng/mL, classified by HOMA-IR, are shown in Fig. 4a. The 5-year cumulative incidence of HCC of the HOMA-IR ≥3.0 (13.4 %) group was significantly higher than that of the HOMA-IR <3.0 (1.3 %) group (log-rank test: P = 0.0079). The Kaplan Meyer curves for the estimation of the incidence of HCC by non-SVR patients with AFP ≥10 ng/mL, classified by HOMA-IR, are shown in Fig. 4b. The 5-year cumulative incidence of HCC in the HOMA-IR ≥3.0 (26.8 %) group was significantly higher than that of the HOMA-IR <3.0 (0 %) group (log-rank test: P = 0.032).
Cumulative incidence of HCC according to insulin resistance (cut-off HOMA-IR 3.0) for non-SVR patients with a low to moderate AFP level (<10 ng/mL) and b high AFP level (≥10 U/L). HCC, hepatocellular carcinoma; HOMA, homeostasis model assessment of insulin resistance; SVR, sustained virological response; AFP, alpha-fetoprotein
Development of HCC by SVR patients
Of the patients studied, three who achieved SVR developed HCC during the follow-up period, all of whom were infected with HCV genotype 1b treated with PEG-IFNα2b and ribavirin for 48 weeks, without discontinuation. Their fibrosis stage was F3 and two were overweight (BMI ≥25 kg/m2) and had severe insulin resistance (HOMA-IR 3.48 and 4.76). However, insulin resistance had not improved adequately at 6 months after achieving SVR (3.25 and 3.77, respectively), irrespective of normalization of the ALT level.
Discussion
This study of non-cirrhotic patients established important findings by demonstrating a significant association between severe insulin resistance and the development of HCC by non-SVR patients treated with PEG-IFNα2b and ribavirin. It is well known that SVR patients have little risk of HCC [6] and that patients with cirrhosis have the highest risk for the development of HCC. Our data, which show the importance of insulin resistance against HCC development, have clinically useful implications for the management of chronic hepatitis by physicians.
PEG-IFNα and ribavirin has been the standard anti-HCV regimen for the past decade. Although many studies concluded that non-SVR, older age, higher pre/post treatment ALT and AFP levels, and cirrhosis were associated with HCC occurrence, few reports focused on the relationship between insulin resistance and HCC occurrence, especially for non-cirrhotic patients. Indeed, diabetes mellitus enhanced the development of HCC after IFN treatment [21, 22] regardless of treatment outcome, probably because the hyperglycemia increases oxidative/endoplasmic reticulum stress. However, this study mainly consisted of non-diabetic patients (HbA1c median: 5.5 %, range: 4.4–6.8 %), thus, our results that severe insulin resistance, which was in the early stage of impaired glucose tolerance, had enhanced HCC development, irrespective of non-cirrhosis, provide useful information for making a decision on retreatment.
Insulin resistance is usually the main pathology of metabolic syndrome, which is represented by overweight/obesity and a lack of exercise. In contrast, the mechanism of the insulin resistance of patients with chronic HCV infection has been reported to be the harmful effect of HCV core protein [23, 24]. The diversity of the HCV core region has been correlated with ALT elevation and HCC development [25, 26]. In addition, HCV core protein can cause the downregulation of insulin receptor substrate-1 (IRS-1) signaling [23], the elevation of inflammatory cytokine [27], and hepatic steatosis due to impaired secretion of very low lipoprotein cholesterol or decreased fatty acid beta-oxidation [28]. According to a recent report, NS3 and NS5A proteins were significantly associated with the development of HCC [29]. Hyperinsulinemia may play a crucial role as an important factor in the onset or progression of HCC through up-regulation of insulin signal cascades. This could promote fibrogenesis by stimulating the release of connective tissue growth factor, a fibrogenic growth factor from hepatic stellate cells [14]. Moreover, the secretion of various adipokines, such as tumor necrosis factor α (TNFα), interleukin-6 (IL-6), and adiponectin may play a role in the relation between insulin resistance and the development of HCC. Increased production of pro-inflammatory cytokines such as TNFα and IL-6 has been reported to be associated with insulin resistance [30, 31]. On the other hand, adiponectin, which possesses anti-inflammatory and insulin-sensitizing properties, has been positively correlated with the development of HCC [32, 33]. A possible explanation is that adiponectin levels may be increased in cirrhosis and with increasing stages of fibrosis [34]. In any case, the role of adiponectin in chronic hepatitis C is not well understood and the relation between adiponectin and the development of HCC remains controversial.
Based on this study of non-cirrhotic patients, pre-treatment HOMA-IR level, post-treatment ALT level, and fibrosis were independent factors for the development of HCC by patients treated with PEG-IFNα2b and ribavirin. Of note, insulin resistance was more closely related to the development of HCC by non-cirrhotic patients than was treatment outcome. We may need to consider early retreatment to avoid increasing the risk of HCC development, especially for patients with insulin resistance and a high post-treatment ALT level, irrespective of the fibrosis status. Interestingly, some cohort studies have shown that metformin, an oral drug widely used for the treatment of type 2 diabetes that improves insulin resistance, can reduce the risk of HCC [35, 36]. Furthermore, Juan et al. recently reported that metformin appeared to have a direct anti-HCC effect in animal models [37].
Our goal is for all patients with chronic hepatitis C to eventually achieve SVR to antiviral treatment. Since 2011, various DAAs have become available for use in the clinical practice setting [38], and DAA only regimens will be the first-line HCV treatment worldwide in the near future. However, waiting for many years for the new DAAs to become available will lead to an increased risk of progressed fibrosis and HCC, especially for patients with insulin resistance. Patients who are at high risk for HCC have the greatest need for antiviral treatment, and it needs to be carried out in as timely a manner as possible.
This study has some limitations. We used HOMA-IR to assess insulin resistance. Although HOMA-IR is one of the most commonly used models for estimating insulin resistance, misclassification is possible when interpreting the results. Among chronic hepatitis C patients without diabetes mellitus, the most commonly cited HOMA-IR cut-off values for insulin resistance (3.0) were reported to have possible misclassification [39]. Particularly, the degree of obesity may have an influence on the overestimation of insulin resistance, with overweight patients (BMI 25.0–29.9 kg/m2) likely to be misclassified because of higher odds of false positivity for insulin resistance compared to normal weight patients (BMI <25.0 kg/m2), irrespective of ethnicity. Furthermore, obesity itself has been related to increased endogenous insulin secretion, decreased insulin clearance, and increased insulin resistance. The second limitation is the lack of post-treatment HOMA-IR data. According to a previous report that studied mainly Caucasian patients, SVR by HCV genotype 1 patients was associated with reduced insulin resistance (HOMA-IR), but non-SVR was not [40]. However, decreased body weight during IFN treatment is a common adverse effect due to general malaise or a depressive state, especially for elderly Japanese patients [41]. This would have an effect on HOMA-IR values and make it difficult to evaluate the true insulin resistance.
Conclusion
In conclusion, insulin resistance has a strong impact on the development of HCC. Our findings show that HOMA-IR is a simple and practical biomarker for predicting the development of HCC, particular for non-cirrhotic patients, irrespective of treatment outcome, serum ALT, or AFP level. Our findings will be useful for helping physicians make decisions on the appropriate timing and priority of retreatment.
Abbreviations
- HCV:
-
Hepatitis C virus
- HCC:
-
Hepatocellular carcinoma
- PEG-IFNα:
-
Pegylated interferon-alpha
- SVR:
-
Sustained virological response
- AFP:
-
Alpha-fetoprotein
- HOMA-IR:
-
Homeostasis model assessment of insulin resistance
- DAA:
-
Direct-acting antiviral
- ALT:
-
Alanine aminotransferase
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
- ROC:
-
Receiver operating characteristic
References
Hayashi J, Furusyo N, Ariyama I, Sawayama Y, Etoh Y, Kashiwagi S. A relationship between the evolution of hepatitis C virus variants, liver damage, and hepatocellular carcinoma in patients with hepatitis C viremia. J Infect Dis. 2000;181:1523–7.
Fattovich G, Stroffolini T, Zagni I, Donato F. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology. 2004;127:S35–50.
Hayashi J, Kishihara Y, Ueno K, Yamaji K, Kawakami Y, Furusyo N, et al. Age-related response to interferon alfa treatment in women vs men with chronic hepatitis C virus infection. Arch Intern Med. 1998;26:177–81.
Morgan TR, Ghany MG, Kim HY, Snow KK, Shiffman ML, De Santo JL, et al. Outcome of sustained virological responders with histologically advanced chronic hepatitis C. Hepatology. 2010;52:833–44.
van der Meer AJ, Veldt BJ, Feld JJ, Wedemeyer H, Dufour JF, Lammert F, et al. Association between sustained virological response and all-cause mortality among patients with chronic hepatitis C and advanced hepatic fibrosis. JAMA. 2012;308:2584–93.
Ogawa E, Furusyo N, Kajiwara E, Takahashi K, Nomura H, Maruyama T, et al. Efficacy of pegylated interferon alpha-2b and ribavirin treatment on the risk of hepatocellular carcinoma in patients with chronic hepatitis C: a prospective, multicenter study. J Hepatol. 2013;58:495–501.
Asahina Y, Tsuchiya K, Nishimura T, Muraoka M, Suzuki Y, Tamaki N, et al. α-fetoprotein levels after interferon therapy and risk of hepatocarcinogenesis in chronic hepatitis C. Hepatology. 2013;58:1253–62.
Yoshida H, Shiratori Y, Moriyama M, Arakawa Y, Ide T, Sata M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. Ann Intern Med. 1999;131:174–81.
Bruno S, Stroffolini T, Colombo M, Bollani S, Benvegnù L, Mazzella G, et al. Sustained virological response to interferon-alpha is associated with improved outcome in HCV-related cirrhosis: a retrospective study. Hepatology. 2007;45:579–87.
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132:2557–76.
Shiratori Y, Imazeki F, Moriyama M, Yano M, Arakawa Y, Yokosuka O, et al. Histologic improvement of fibrosis in patients with hepatitis C who have sustained response to interferon therapy. Ann Intern Med. 2000;132:517–24.
Ogawa E, Furusyo N, Toyoda K, Takeoka H, Maeda S, Hayashi J. The longitudinal quantitative assessment by transient elastography of chronic hepatitis C patients treated with pegylated interferon alpha-2b and ribavirin. Antiviral Res. 2009;83:127–34.
Fartoux L, Poujol-Robert A, Guéchot J, Wendum D, Poupon R, Serfaty L. Insulin resistance is a cause of steatosis and fibrosis progression in chronic hepatitis C. Gut. 2005;54:1003–8.
Kawaguchi T, Izumi N, Charlton MR, Sata M. Branched-chain amino acids as pharmacological nutrients in chronic liver disease. Hepatology. 2011;54:1063–70.
Moriya K, Nakagawa K, Santa T, Shintani Y, Fujie H, Miyoshi H, et al. Oxidative stress in the absence of inflammation in a mouse model for hepatitis C virus-associated hepatocarcinogenesis. Cancer Res. 2001;61:4365–70.
Shuda M, Kondoh N, Imazeki N, Tanaka K, Okada T, Mori K, et al. Activation of the ATF6, XBP1 and grp78 genes in human hepatocellular carcinoma: a possible involvement of the ER stress pathway in hepatocarcinogenesis. J Hepatol. 2003;38:605–14.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Ogawa E, Furusyo N, Murata M, Ikezaki H, Ihara T, Hayashi T, et al. Insulin resistance undermines the advantages of IL28B polymorphism in the pegylated interferon alpha-2b and ribavirin treatment of chronic hepatitis C patients with genotype 1. J Hepatol. 2012;57:534–40.
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus, Seino Y, Nanjo K, Tajima N, Kadowaki T, Kashiwagi A, et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. J Diabetes Invest. 2010;1:212–28.
The French METAVIR Cooperative Study Group. Intraobserver and interobserver variations in liver biopsy interpretation in patients with chronic hepatitis C. Hepatology. 1994;20:15–20.
Hung CH, Lee CM, Wang JH, Hu TH, Chen CH, Lin CY, et al. Impact of diabetes mellitus on incidence of hepatocellular carcinoma in chronic hepatitis C patients treated with interferon-based antiviral therapy. Int J Cancer. 2011;128:2344–52.
Arase Y, Kobayashi M, Suzuki F, Suzuki Y, Kawamura Y, Akuta N, et al. Effect of type 2 diabetes on risk for malignancies includes hepatocellular carcinoma in chronic hepatitis C. Hepatology. 2013;57:964–73.
Pazienza V, Clément S, Pugnale P, Conzelman S, Foti M, Mangia A, et al. The hepatitis C virus core protein of genotypes 3a and 1b downregulates insulin receptor substrate 1 through genotype-specific mechanisms. Hepatology. 2007;45:1164–71.
Akuta N, Suzuki F, Hirakawa M, Kawamura Y, Yatsuji H, Sezaki H, et al. Amino acid substitutions in the hepatitis C virus core region of genotype 1b are the important predictor of severe insulin resistance in patients without cirrhosis and diabetes mellitus. J Med Virol. 2009;81:1032–9.
Hayashi J, Kishihara Y, Yamaji K, Furusyo N, Yamamoto T, Pae Y, et al. Hepatitis C viral quasispecies and liver damage in patients with chronic hepatitis C virus infection. Hepatology. 1997;25:697–701.
Akuta N, Suzuki F, Kawamura Y, Yatsuji H, Sezaki H, Suzuki Y, et al. Amino acid substitutions in the hepatitis C virus core region are the important predictor of hepatocarcinogenesis. Hepatology. 2007;46:1357–64.
Dolganiuc A, Kodys K, Kopasz A, Marshall C, Do T, Romics Jr L, et al. Hepatitis C virus core and nonstructural protein 3 proteins induce pro- and anti-inflammatory cytokines and inhibit dendritic cell differentiation. J Immunol. 2003;170:5615–24.
Negro F, Sanyal AJ. Hepatitis C virus, steatosis and lipid abnormalities: clinical and pathogenic data. Liver Int. 2009;29:26–37.
El-Shamy A, Shindo M, Shoji I, Deng L, Okuno T, Hotta H. Polymorphisms of the core, NS3, and NS5A proteins of hepatitis C virus genotype 1b associate with development of hepatocellular carcinoma. Hepatology. 2013;58:555–63.
Bertoletti A, D’Elios MM, Boni C, De Carli M, Zignego AL, Durazzo M, et al. Different cytokine profiles of intraphepatic T cells in chronic hepatitis B and hepatitis C virus infections. Gastroenterology. 1997;112:193–9.
Durante-Mangoni E, Zampino R, Marrone A, Tripodi MF, Rinaldi L, Restivo L, et al. Hepatic steatosis and insulin resistance are associated with serum imbalance of adiponectin/tumour necrosis factor-alpha in chronic hepatitis C patients. Aliment Pharmacol Ther. 2006;24:1349–57.
Arano T, Nakagawa H, Tateishi R, Ikeda H, Uchino K, Enooku K, et al. Serum level of adiponectin and the risk of liver cancer development in chronic hepatitis C patients. Int J Cancer. 2011;129:2226–35.
Aleksandrova K, Boeing H, Nöthlings U, Jenab M, Fedirko V, Kaaks R, et al. Inflammatory and metabolic biomarkers and risk of liver and biliary tract cancer. Hepatology. 2014;60:858–71.
Tacke F, Wüstefeld T, Horn R, Luedde T, Srinivas Rao A, Manns MP, et al. High adiponectin in chronic liver disease and cholestasis suggests biliary route of adiponectin excretion in vivo. J Hepatol. 2005;42:666–73.
Chen HP, Shieh JJ, Chang CC, Chen TT, Lin JT, Wu MS, et al. Metformin decreases hepatocellular carcinoma risk in a dose-dependent manner: population-based and in vitro studies. Gut. 2013;62:606–15.
Lai SW, Chen PC, Liao KF, Muo CH, Lin CC, Sung FC. Risk of hepatocellular carcinoma in diabetic patients and risk reduction associated with anti-diabetic therapy: a population-based cohort study. Am J Gastroenterol. 2012;107:46–52.
Li J, Hernanda PY, Bramer WM, Peppelenbosch MP, van Luijk J, Pan Q. Anti-tumor effects of metformin in animal models of hepatocellular carcinoma: a systematic review and meta-analysis. PLoS One. 2015;10:e0127967.
Furusyo N, Ogawa E, Nakamuta M, Kajiwara E, Nomura H, Dohmen K, et al. Telaprevir can be successfully and safely used to treat older patients with genotype 1b chronic hepatitis C. J Hepatol. 2013;59:205–12.
Lam KD, Bacchetti P, Abbasi F, Ayala CE, Loeb SM, Shah V, et al. Comparison of surrogate and direct measurement of insulin resistance in chronic hepatitis C virus infection: impact of obesity and ethnicity. Hepatology. 2010;52:38–46.
Thompson AJ, Patel K, Chuang WL, Lawitz EJ, Rodriguez-Torres M, Rustgi VK, et al. Viral clearance is associated with improved insulin resistance in genotype 1 chronic hepatitis C but not genotype 2/3. Gut. 2012;61:128–34.
Ogawa E, Furusyo N, Kajiwara E, Takahashi K, Nomura H, Tanabe Y, et al. Evaluation of the adverse effect of premature discontinuation of pegylated interferon α-2b and ribavirin treatment for chronic hepatitis C virus infection: results from Kyushu University Liver Disease Study. J Gastroenterol Hepatol. 2012;27:1233–40.
Acknowledgements
We are grateful to Drs. Mosaburo Kainuma, Kazuhiro Toyoda, Motohiro Shimizu, Hiroaki Ikezaki, Takeshi Ihara, Satoshi Hiramine, Fujiko Mitsumoto-Kaseida, Koji Takayama, Kazuya Ura, Rinne Takeda, Sho Yamasaki, Yoshifumi Kato, Yuuki Tanaka and Masaru Sakiyama from the Department of General Internal Medicine, Kyushu University Hospital for their assistance with this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Norihiro Furusyo has received grants from Taisho Toyama Pharmaceutical Co., Ltd., Daiichi Sankyo Co., Ltd., and Bristol-Myers Squibb. The remaining authors declare that they have no conflicts of interest. This work was supported by a research grant from the Japanese Society of Hospital General Medicine.
Authors’ contributions
TH participated in the design of the study and collecting data, performed the statistical analysis and drafted the manuscript. EO helped draft the manuscript, perform the statistical analysis, and participated in the design of the study and collection of data. NF, MM, and JH critically revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hayashi, T., Ogawa, E., Furusyo, N. et al. Influence of insulin resistance on the development of hepatocellular carcinoma after antiviral treatment for non-cirrhotic patients with chronic hepatitis C. Infect Agents Cancer 11, 9 (2016). https://doi.org/10.1186/s13027-016-0056-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13027-016-0056-y