Abstract
Background
Determining the modifiable risk factors for postoperative complications is particularly significant in patients undergoing colorectal surgery since those are associated with worse long-term outcomes.
Methods
Consecutive newly diagnosed 104 colorectal cancer patients were prospectively included in this single-center observational study. Preoperative serum 25-OH vitamin D levels were measured and analyzed for infectious and postoperative complications.
Results
Serum 25-OH vitamin D levels were found to be < 20 ng/ml in 74 patients (71.2%) and ≥ 20 ng/ml in 30 patients (28.8%); and the mean serum 25-OH vitamin D level was 15.95 (± 9.08) ng/ml. In patients with surgical site infection and infectious complications, 25-OH vitamin D levels were significantly lower than patients without complications (p = 0.036 and p = 0.026). However, no significant difference was demonstrated in 25-OH vitamin D levels according to overall postoperative complications.
Conclusions
Our results suggest that vitamin D levels might be a potential risk factor for infectious complications in patients undergoing colorectal cancer surgery.
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the second cause of cancer-related mortality worldwide, and radical resection is still the treatment of choice [1]. Despite improvements in postoperative care, the rate of postoperative complication (PoC) is changed between 19 and 30% in patients undergoing elective colorectal surgery [2]. The most known factors related to PoC are nutritional status, comorbid diseases, and operation timing [3,4,5]. Inflammatory markers such as C-reactive protein (CRP), albumin, and procalcitonin have been widely used in clinical practice for early detection of complications [6,7,8,9]. As reported by numerous studies, PoC has a significant impact on not only short-term outcomes but also on overall survival in colorectal cancer patients [10,11,12].
25-hydroxy (OH) vitamin D levels have been inversely related to colorectal cancer risk by causing adenoma formation in colon epithelium [13,14,15,16]. 25-OH vitamin D levels have also been associated with long-term survival and increased response to oncological treatment; however, its effect on PoC has not been thoroughly investigated [17, 18].
The present study aimed to evaluate the association between serum 25-OH vitamin D levels and PoC and observe its effect on short-term outcomes in colorectal cancer patients.
Methods
This study was designed as an observational cohort study; and was approved by the Ethics Committee of Izmir Tepecik Training and Research Hospital, University of Health Sciences, Turkey. The study protocol is performed in accordance with the relevant guidelines. All patients' written informed consents were taken after oral and written explanations were made.
Patients' selection
We performed this study in patients undergoing colorectal cancer surgery between September 2017 and March 2019 at the department of General Surgery, Izmir Tepecik Training and Research Hospital, University of Health Sciences, Turkey. Consecutive patients who met the inclusion criteria were prospectively included in this study. The inclusion criteria were as follows: (1) histopathological evidence of colorectal cancer, (2) patients older than 18 years, (3) patients who underwent curative resection. The exclusion criteria were as follows: (1) unresectable disease, (2) systemic metastases, (3) patients who received neoadjuvant chemoradiotherapy, (4) patients who underwent an emergent operation or operated with palliative intent.
Data collection
The routine preoperative workup, including complete blood count, liver and kidney function tests, were done with an addition of preoperative serum levels of 25-OH vitamin D and carcinoembryonic antigen (CEA). Blood samples were taken in a week to the scheduled operation in all patients. Patients' nutritional status was evaluated using nutritional risk score-2002 (NRS), and comorbid diseases were classified according to the American Society of Anesthesiologists (ASA) [19, 20]. Patients' operative data were noted, and PoC occurring within 30 days of surgery were graded based on Clavien-Dindo classification [21]. Pathology results were also recorded, including histopathological grading and pathological tumor-node-metastasis (pTNM) staging [22].
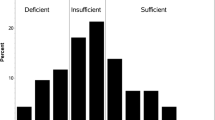
Preoperative 25-OH vitamin D levels were evaluated according to the guidelines of the American Endocrine Society [23]: severe deficiency (< 10 ng/ml), mild deficiency (10–20 ng/ml), level of insufficiency (20–30 ng/ml) and optimal levels (> 30 ng/ml).
Study outcomes
Our study's primary outcome was to demonstrate the relation between 25-OH vitamin D levels and postoperative complications. The secondary outcome was to evaluate its relationship with histopathological grading and pTNM staging.
Statistical analysis
The data was recorded and analyzed with IBM SPSS Statistics 24.0.0.0. Categorical variables were presented as frequency distributions and continuous variables as mean values ± standard deviation (median; min–max). Shapiro–Wilk test was performed to confirm the normal distribution of continuous variables. Categorical variables were analyzed using Chi-square and Fischer's exact tests. The Student t-test or Mann–Whitney-U test were used for analyses involving binary categorical subgroups, and One-way ANOVA and Kruskal–Wallis tests for analyses involving three or more categorical subgroups.
Logistic regression analysis in backward stepwise (likelihood ratio) fashion was performed to demonstrate independent risk factors for infectious complications. Selected co-variates were, including gender, age, ASA, NRS, serum levels of albumin, CEA, 25-OH vitamin D and WBC, type of procedure, T and N stages, and histopathological grade.
p value < 0.05 was accepted as significant for each test.
Results
The study population consisted of 104 patients; 64 males (61.5%) and 40 females (38.5%); the mean age was found to be 62.71 (± 12.41) years. The mean serum 25-OH vitamin D level was 15.95 (± 9.08) ng/ml, which corresponds to the cohort's vitamin D deficiency. Serum vitamin D levels were found to be < 20 ng/ml in 74 patients (71.2%) and ≥ 20 ng/ml in 30 patients (28.8%). Patients' demographic and clinical characteristics are shown in Table 1.
Vitamin D levels were found to be 15.7 ± 8.3 (13.7; 4.5–60.1) ng/ml in males and 16.4 ± 10.3 (13.5; 5–54.7) ng/ml in females (U = 1237.500, p = 0.776). There was no significant association between 25-OH vitamin D levels and serum CEA, albumin, hemoglobin, and WBC levels. Most of the patients scored ASA-2 (53.8%); patients with higher vitamin D levels were found to have higher ASA scores (p = 0.043).
However, 25-OH vitamin D levels were measured as 18.9 ± 7.4 (20.9; 5–30.4) ng/ml in ASA-1 patients, 15.3 ± 8.7(13.2;4.5–54.7) ng/ml in ASA-2 patients, and 15.5 ± 10.5 (13.15; 5.6–60.1) in ASA-3 patients (x2 = 4.485, p = 0.106).
Tumor location was demonstrated as a colon in 74 patients (71.2%) and rectum in 30 patients (28.8%). Metachronous colon tumor was found in 1 patient and synchronous colon tumors in 2 patients. Serum 25-OH vitamin D levels were found to be significantly lower in patients with rectal cancer (13 ± 7.5 (10.3; 4.5–31.7) ng/ml) compared to patients with colon cancer (17.1 ± 9.5 (15.2; 5–60.1) ng/ml) (U = 755.000, p = 0.011). The most common operative procedure performed was low anterior resection (37.5%) followed by right hemicolectomy (19.2%). The laparoscopic approach was chosen in 9 patients, and laparotomy was performed in 95 patients. There were no significant differences observed in vitamin D levels according to the type of operative procedures.
Patients' histopathological results confirmed the diagnosis of carcinoma-in-situ in 2 patients, adenocarcinoma in 88 patients, mucinous adenocarcinoma in 12 patients, signet cell carcinoma in 2 patients, and malignant fibrous histiocytoma in 1 patient. Most of the patients were staged as pTNM stage IIa (33.7%) and IIIb (25%), and a statistically significant difference was found in vitamin D levels for pTNM staging (p = 0.036).
Infectious complications were seen in 18 patients (17.3%), including wound infection, anastomotic leak, intra-abdominal abscess, and pneumonia (Table 2). The anastomotic leak occurred in 7 patients (6.73%): on postoperative day-5 in 1 patient, day-6 in 4 patients, and day-8 in 2 patients. Non-operative management was chosen in 2 patients, and the Hartmann procedure was performed in 5 patients. No significant differences in vitamin D levels were observed according to Clavien-Dindo scores (p = 0.75).
The study population was evaluated for the association between 25-OH vitamin D levels and infectious complications (Table 3). In patients with surgical site infection and infectious complications, 25-OH vitamin D levels were significantly lower than patients without complications (p = 0.036 and p = 0.026). However, no significant difference was demonstrated in 25-OH vitamin D levels according to overall PoC.
Logistic regression analysis was conducted to evaluate the predictive competence of the preoperative factors for infectious complications (Table 4). Although lower vitamin D levels were associated with infectious complications on univariate analysis, the exact correlation was not shown on multivariate analysis. The type of operative procedure was found to be the only independent risk factor for infectious complications.
Discussion
PoC related to colorectal cancer surgery remain a significant problem; infectious complications represent the most of those and have been associated with decreased long-term survival in colorectal cancer patients [24, 25]. Therefore, determining the modifiable risk factors for preoperative complications is particularly significant in patients undergoing colorectal surgery.
In recent years, an increasing number of studies have investigated the effect of 25-OH vitamin D on progression-free survival and overall survival in patients with colorectal cancer [26,27,28]. It has also been revealed that infectious complications are increased in hospitalized patients with vitamin D deficiency because of its decreased immunomodulatory effects [29, 30]. The effects of vitamin D on the immune system are mainly based on the presence of vitamin D receptors on B and T lymphocytes and macrophages, and promoting chemotaxis, autophagy, and phagolysosomal function in innate immune cells. Vitamin D is also found to be responsible for the barrier function of the intestinal epithelium and the modulation of the bowel system [31].
In line with these findings, preoperative 25-OH vitamin D levels were inversely related to surgical site infections in patients undergoing cardiac surgery and total knee arthroplasty [32, 33]. Quraishi et al. have also reported that hospital-acquired infections are associated with low preoperative 25-OH vitamin D levels in patients following bariatric surgery [34].
To better demonstrate the relation between vitamin D deficiency and PoC, we excluded the patients who were operated on in an emergency setting and received neoadjuvant chemoradiotherapy. To that end, the study cohort was relatively small, consisting of 104 patients with a mean 25-OH vitamin D value of 15.95 (± 9.08) ng/ml. In line with previous studies' findings, patients with surgical site infection and infectious complications had significantly lower 25-OH vitamin D levels compared to patients without complications. However, we did not observe any association between vitamin D levels and overall PoC.
A recent study conducted in hepatobiliary surgery patients revealed that preoperative 25-OH vitamin D levels were related to hospital-acquired infections and in-hospital outcomes [35]. There were also significant differences observed in vitamin D levels according to gender, ASA, and Clavien-Dindo scores. However, there was no significant association between vitamin D levels, gender, ASA, and Clavien-Dindo scores in our study. We suggest that these findings result from the sample size and study cohort, which has a high prevalence (94%) of vitamin D deficiency.
Our secondary outcome was to evaluate the effect of 25-OH vitamin D levels on histopathological grading and pTNM staging based on the fact that decreased 25-OH vitamin D levels are linked with poor survival in colorectal cancer patients [36]. Vitamin D levels were not related to histopathological grading in our study. Värynen et al. revealed that 25-OH vitamin D levels were lower in pTNM stage II-IV colorectal cancer patients than pTNM stage I colorectal cancer patients [16]. Similar to their results, we observed a significant difference in pTNM staging according to vitamin D levels. Moreover, patients with rectal cancer were found to have significantly lower vitamin D levels in the present study. Rectal cancer has also been associated with an increased risk of PoC [24]. Our findings may also suggest a possible relationship between vitamin D levels and PoC.
Abdehgah et al. reported that preoperative 25-OH vitamin D levels were found to be independent predictors of surgical site infections in addition to the length of hospital stay [37]. On multivariate analysis, we could not demonstrate the effect of vitamin D on infectious complications; the only independent risk factor was the type of operative procedure. It should be emphasized that Abdehgah et al. conducted their study in a heterogeneous cohort undergoing varied types of gastrointestinal tract, hepatobiliary, thoracic, and vascular operations. Also, the prevalence of vitamin D deficiency was only 39% in the study cohort.
The major limitation of this observational study was the retrospective analysis of a small sample size with a significantly high prevalence of vitamin D deficiency (94%). Therefore, we could not draw firm results for associations between vitamin D levels and PoC, and Clavien-Dindo scores. Furthermore, dose–response analysis of vitamin D levels for infectious complications could not be performed in this study.
Conclusions
In summary, vitamin D levels might be a potential risk factor for infectious complications in patients undergoing colorectal cancer surgery. We need prospective randomized controlled studies to draw firm conclusions for the relation of preoperative 25-OH vitamin D levels and PoC and to investigate whether vitamin D levels should be optimized to improve short-term outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424.
Zhuang CL, Ye XZ, Zhang XD, Chen BC, Yu Z. Enhanced recovery after surgery programs versus traditional care for colorectal surgery; a meta-analysis of randomized controlled trials. Dis Colon Rectum. 2013;56:667–78.
Schiesser M, Kirchhoff P, Müller MK, Schäfer M, Clavien PA. The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery. 2009;145(5):519–26.
Hendry PO, Hausel J, Nygren J, Lassen K, Dejong CH, Ljungqvist O, Fearon KC, Enhanced Recovery After Surgery Study Group. Determinants of outcome after colorectal resection within an enhanced recovery programme. Br J Surg. 2009;96(2):197–205.
Lee CHA, Kong JCH, Heriot AG, et al. Short-term outcome of emergency colorectal cancer surgery: results from Bi-National Colorectal Cancer Audit. Int J Colorectal Dis. 2019;34:63–9. https://doi.org/10.1007/s00384-018-3169-5.
McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102(5):462–79.
McSorley ST, Khor BY, MacKay GJ, Horgan PG, McMillan DC. Examination of a CRP first approach for the detection of postoperative complications in patients undergoing surgery for colorectal cancer: a pragmatic study. Medicine (Baltimore). 2017;96(7):e6133.
Montomoli J, Erichsen R, Antonsen S, et al. Impact of preoperative serum albumin on 30-day mortality following surgery for colorectal cancer: a population-based cohort study. BMJ Open Gastroenterol. 2015;2:e000047.
Domínguez-Comesaña E, Estevez-Fernández SM, López-Gómez V, Ballinas-Miranda J, Domínguez-Fernández R. Procalcitonin and C-reactive protein as early markers of postoperative intra-abdominal infection in patients operated on colorectal cancer. Int J Colorectal Dis. 2017;32(12):1771–4.
McSorley ST, Horgan PG, McMillan DC. The impact of the type and severity of postoperative complications on long-term outcomes following surgery for colorectal cancer: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2016;97:168–77.
Artinyan A, Orcutt ST, Anaya DA, Richardson P, Chen GJ, Berger DH. Infectious postoperative complications decrease long-term survival in patients undergoing curative surgery for colorectal cancer: a study of 12,075 patients. Ann Surg. 2015;261(3):497–505.
Odermatt M, Miskovic D, Flashman K, Khan J, Senapati A, O’Leary D, Thompson M, Parvaiz A. Major postoperative complications following elective resection for colorectal cancer decrease long-term survival but not the time to recurrence. Colorectal Dis. 2015;17(2):141–9.
McCullough ML, Zoltick ES, Weinstein SJ, Fedirko V, Wang M, Cook NR, Eliassen AH, Zeleniuch-Jacquotte A, Agnoli C, Albanes D, Barnett MJ, Buring JE, Campbell PT, Clendenen TV, Freedman ND, Gapstur SM, Giovannucci EL, Goodman GG, Haiman CA, Ho GYF, Horst RL, Hou T, Huang WY, Jenab M, Jones ME, Joshu CE, Krogh V, Lee IM, Lee JE, Männistö S, Le Marchand L, Mondul AM, Neuhouser ML, Platz EA, Purdue MP, Riboli E, Robsahm TE, Rohan TE, Sasazuki S, Schoemaker MJ, Sieri S, Stampfer MJ, Swerdlow AJ, Thomson CA, Tretli S, Tsugane S, Ursin G, Visvanathan K, White KK, Wu K, Yaun SS, Zhang X, Willett WC, Gail MH, Ziegler RG, Smith-Warner SA. Circulating vitamin D and colorectal cancer risk: an international pooling project of 17 cohorts. J Natl Cancer Inst. 2018. https://doi.org/10.1093/jnci/djy087.
Dimitrakopoulou VI, Tsilidis KK, Haycock PC, et al. Circulating vitamin D concentration and risk of seven cancers: mendelian randomisation study. BMJ. 2017;359:j4761.
Gibbs DC, Fedirko V, Um C, Gross MD, Thyagarajan B, Bostick RM. Associations of circulating 25-hydroxyvitamin D3 concentrations with incident, sporadic colorectal adenoma risk according to common vitamin d binding protein isoforms. Am J Epidemiol. 2018;187:1923.
Väyrynen JP, Mutt SJ, Herzig KH, Väyrynen SA, Kantola T, Karhu T, Karttunen TJ, Klintrup K, Mäkelä J, Mäkinen MJ, Tuomisto A. Decreased preoperative serum 25-Hydroxyvitamin D levels in colorectal cancer are associated with systemic inflammation and serrated morphology. Sci Rep. 2016;6:36519.
Maalmi H, Walter V, Jansen L, Boakye D, Schöttker B, Hoffmeister M, Brenner H. Association between blood 25-hydroxyvitamin D levels and survival in colorectal cancer patients: an updated systematic review and meta-analysis. Nutrients. 2018;10(7):896.
Yang L, Chen H, Zhao M, Peng P. Prognostic value of circulating vitamin D binding protein, total, free and bioavailable 25-hydroxy vitamin D in patients with colorectal cancer. Oncotarget. 2017;8(25):40214–21.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–36. https://doi.org/10.1016/s0261-5614(02)00214-5.
Hurwitz EE, Simon M, Vinta SR, et al. Adding examples to the ASA-Physical Status classification improves correct assignments to patients. Anesthesiology. 2017;126:614–22.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th Edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010. https://doi.org/10.1245/s10434-010-0985-4.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, Murad MH, Weaver CM, Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–30.
Miyamoto Y, Hiyoshi Y, Tokunaga R, Akiyama T, Daitoku N, Sakamoto Y, Yoshida N, Baba H. Postoperative complications are associated with poor survival outcome after curative resection for colorectal cancer: a propensity-score analysis. J Surg Oncol. 2020;122(2):344–9. https://doi.org/10.1002/jso.25961 (Epub 2020 Apr 28).
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P. Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg. 2011;253(5):890–9. https://doi.org/10.1097/SLA.0b013e3182128929.
Maalmi H, Ordonez-Mena JM, Schottker B, Brenner H. Serum 25-hydroxyvitamin D levels and survival in colorectal and breast cancer patients: systematic review and meta-analysis of prospective cohort studies. Eur J Cancer. 2014;50(8):1510–21.
Abrahamsson H, Porojnicu AC, Lindstrøm JC, Dueland S, Flatmark K, Hole KH, et al. High level of circulating vitamin D during neoadjuvant therapy may lower risk of metastatic progression in high-risk rectal cancer. BMC Cancer. 2019;19(1):488. https://doi.org/10.1186/s12885-019-5724-z.
Ng K, Nimeiri HS, McCleary NJ, Abrams TA, Yurgelun MB, Cleary JM, et al. Effect of high-dose vs standard-dose vitamin d3 supplementation on progression-free survival among patients with advanced or metastatic colorectal cancer: the SUNSHINE randomized clinical trial. JAMA. 2019;321(14):1370–9.
Toubi E, Shoenfeld Y. The role of vitamin D in regulating immune responses. Isr Med Assoc J. 2010;12:174–5.
Youssef DA, Ranasinghe T, Grant WB, Peiris AN. Vitamin D’s potential to reduce the risk of hospital-acquired infections. Derm Endocrinol. 2012;4:167e175.
Sassi F, Tamone C, D’Amelio P. Vitamin D: nutrient, hormone, and immunomodulator. Nutrients. 2018;10(11):1656. https://doi.org/10.3390/nu10111656.
Zittermann A, Kuhn J, Ernst JB, Becker T, Larisch J, Dreier J, Knabbe C, Börgermann J, Gummert JF. Circulating 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentrations and postoperative infections in cardiac surgical patients: the CALCITOP-study. PLoS ONE. 2016;11(6): e0158532. https://doi.org/10.1371/journal.pone.0158532.
Hegde V, Arshi A, Wang C, Buser Z, Wang JC, Jensen AR, Adams JS, Zeegen EN, Bernthal NM. Preoperative vitamin D deficiency is associated with higher postoperative complication rates in total knee arthroplasty. Orthopedics. 2018;41(4):e489–95. https://doi.org/10.3928/01477447-20180424-04 (Epub 2018 Apr 30).
Quraishi SA, Bittner EA, Blum L, Hutter MM, Camargo CA Jr. Association between preoperative 25-hydroxyvitamin D level and hospital-acquired infections following Roux-en-Y gastric bypass surgery. JAMA Surg. 2014;149(2):112–8. https://doi.org/10.1001/jamasurg.2013.3176.
Laviano E, Sanchez Rubio M, González-Nicolás MT, Palacian MP, López J, et al. Association between preoperative levels of 25-hydroxyvitamin D and hospital-acquired infections after hepatobiliary surgery: a prospective study in a third-level hospital. PLoS ONE. 2020;15(3): e0230336. https://doi.org/10.1371/journal.pone.0230336.
Wu G, Xue M, Zhao Y, Han Y, Zhang S, Zhang J, Li C, Xu J. Low circulating 25-hydroxyvitamin D level is associated with increased colorectal cancer mortality: a systematic review and dose-response meta-analysis. Biosci Rep. 2020;40(7):BSR20201008. https://doi.org/10.1042/BSR20201008.
Abdehgah AG, Monshizadeh A, Tehrani MM, Afhami S, Molavi B, Jafari M, Nasiri S, Soroush A. Relationship between preoperative 25-hydroxy vitamin D and surgical site infection. J Surg Res. 2020;245:338–43. https://doi.org/10.1016/j.jss.2019.07.036 (Epub 2019 Aug 16).
Acknowledgements
Special thanks to Dr. Ali Eba Demirbag for his contributions to this study in statistical analysis.
Funding
No grants or fundings were received for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, BB and BC; literature review, BB and GK; data collection, BB and GK, writing—original draft preparation, BB; writing—review and editing, CA and BC; supervision, CA. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This observational study was conducted prospectively and approved by the Ethics Committee of Izmir Tepecik Training and Research Hospital, University of Health Sciences, Turkey. The study protocol is performed in accordance with the relevant guidelines. All patients' written informed consents were taken after oral and written explanations were made.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Balci, B., Kilinc, G., Calik, B. et al. The association between preoperative 25-OH vitamin D levels and postoperative complications in patients undergoing colorectal cancer surgery. BMC Surg 21, 369 (2021). https://doi.org/10.1186/s12893-021-01369-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-021-01369-y