Abstract
Background
Epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs), such as gefitinib, have achieved good efficacy in EGFR mutation-positive non-small-cell lung cancer (NSCLC) patients, but eventual drug resistance is inevitable. Thus, new TKI-based combination therapies should be urgently explored to extend the overall survival time of these patients. CD8 + CD56+ natural killer T (NKT) cells are a natural and unique subset of lymphocytes in humans that present characteristics of T and NK cells and exert cytotoxicity on tumour cells in a granzyme B-dependent manner. The aim of this trial was to explore the efficacy and safety of CD8 + CD56+ NKT cell immunotherapy combined with gefitinib in patients with advanced EGFR-mutated NSCLC.
Methods
The study was designed as a prospective, randomized, controlled, open-label, phase I/II trial that includes 30 patients with EGFR mutation-positive stage III/IV NSCLC. All patients will be randomized in blocks at a 1:1 ratio and treated with gefitinib 250 mg/day monotherapy or combination therapy with allogeneic CD8 + CD56+ NKT cell infusions twice per month for 12 cycles or until disease progression occurs. The effectiveness of this treatment will be evaluated based on by progression-free survival (PFS), the time to progression (TTP), overall response rate (ORR), disease control rate (DCR) and overall survival (OS). The safety of the trail is being assessed based on adverse events (AEs). Recruitment and data collection, which started in December 2017, are ongoing.
Discussion
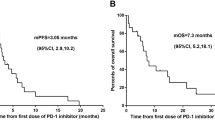
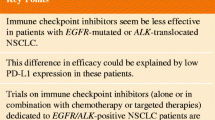
Although immunotherapy, including programmed death-1/programmed death-1 ligand (PD-1/PD-L1) immunotherapy, has been used for NSCLC treatment with or without EGFR-TKIs, its clear efficacy still has not been shown. Assessing the safety and therapeutic potential of allogeneic CD8 + CD56+ NKT killer cells in combination with EGFR-TKIs in NSCLC will be of great interest.
Trial registration
This trial (Phase I/II Trails of NKT Cell in Combination With Gefitinib For Non Small Cell Lung Cancer) was registered on 21 November 2017 with www.chictr.org.cn, ChiCTR-IIR-17013471.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
EGFR-TKI and NSCLC
According to a status report on the worldwide cancer burden in 2018, lung cancer remains the leading cause of cancer incidence and mortality [1]. Among the approximately 2 million new cases each year, 80–85% of new cases are non-small-cell lung cancer (NSCLC), such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, and 15–20% are small-cell lung cancer. Platinum chemotherapy has been the main systemic therapy for patients with advanced NSCLC over the past few decades [2]. In 2004, published data showed that somatic mutations in the epidermal growth factor receptor (EGFR) gene are detected in 30–40% of NSCLCs in Asian patients, and deletions in exon 19 and L858R in exon 21 account for 90% of these activating EGFR mutations [3]. Several epidermal growth factor receptor tyrosine kinase inhibitors (EGFR-TKIs), such as gefitinib, have shown a higher response rate and longer progression-free survival (PFS) than platinum chemotherapy in patients with EGFR mutations and have become a first-line treatment for advanced NSCLC [4, 5]. Thus, these key studies clarified the relationship between EGFR mutations and the efficacy of EGFR-TKI treatment, providing opportunities for the personalised treatment of advanced NSCLC. Though the majority of patients with mutation-positive NSCLC respond to treatment with EGFR-TKIs, the long-term use of EGFR-TKIs for approximately 9–12 months eventually leads to drug resistance, which limits their clinical benefits [6,7,8]. In addition, co-mutation is common in NSCLC patients with EGFR mutations, and the efficacy of first-line TKI monotherapy in NSCLC patients with EGFR co-mutations is significantly worse than that in patients without co-mutations [9]. Therefore, for EGFR mutation-positive patients, TKI-based combination therapy, especially with immunotherapy, needs to be further explored [10].
Immunotherapy and NSCLC
Immunotherapy is a novel, promising treatment for cancers that uses different effective elements of the immune system, such as cytokines, antibodies and effector immune cells. Currently, immune checkpoint inhibitors, anti-programmed death-1 (anti-PD-1) and anti-programmed death-1 ligand (anti-PD-L1), have shown promising effects for treating tumours [11]. Several combination trials of EGFR-TKIs and immune checkpoint inhibitors in NSCLC are also recruiting participants. Nevertheless, some evidence has shown that anti-PD-1 therapy has no additional effects with EGFR-TKI treatment because of the lower expression levels of PD-1 among EGFR-mutant NSCLC patients [12, 13]. Therefore, more evidence is needed on the actual synergistic effects of anti-PD-1 and anti-PD-L1 with EGFR-TKIs [14, 15].
Rationale
In the immune system, there are different types of killer cells that play roles in immune surveillance. Therefore, methods to isolate these cells from the blood, culture and expand them with or without gene editing in the laboratory, and finally infuse these killer cells into the body of patients to exert anti-tumour effects have also been designed for cancer immunotherapy. Currently, the types of killer cells used in cellular immunotherapy are CD8+ T cells including tumour-infiltrating lymphocytes (TILs) and chimeric antigen receptor T (CAR-T) cells, NK cells, and natural killer T (NKT) cells. NKT cells are a subset of CD1d-restricted T cells at the interface between the innate and adaptive immune systems and have characteristics of both conventional T cells and NK cells [16]. Classical NKT cells with invariant TCR α chains were first identified in mice in 1990 and subdivided into different subsets that have a variety of roles in cancer and other diseases [17, 18]. Nevertheless, in some studies, NKT cells have also been identified with flow cytometry analysis with the cell phenotype of CD3 + CD56+ or CD8 + CD56+ in humans and CD3 + NK1.1+ or CD8 + NK1.1+ in mice. Though the definition of these CD3+ subpopulations as NKT cells is still debatable, and they are even referred to as “NKT-like” cells, these cells show activity in innate immunity [19,20,21,22,23]. The work from Sergey S. Seregin showed that CD8 + NK1.1+ cells, not CD8 + NK1.1- cells, have the ability to provide a rapid innate immune response through Ag-independent IFN-γ production and granzyme B degranulation in pathogen infection [22, 23]. Our previous data also demonstrated that CD8 + NK1.1+ cells exerted NK- and CTL-like antitumour effects through the elimination of both tumour cells and myeloid-derived suppressor cells (MDSCs) in a granzyme B-dependent manner [24]. Moreover, we further proved that CD8 + CD56+ cells in humans have similar cytotoxicity to CD8 + NK1.1+ cells in mice and can be effectively expanded in vitro for tumour immunotherapy. However, it is unclear whether these CD8 + CD56+ NKT cells have synergistic effects with EGFR-TKIs, extend PFS and delay resistance to EGFR-TKIs in NSCLCs. Thus, a trial assessing the efficacy of CD8 + CD56+ NKT cells with gefitinib for patients with EGFR mutations is needed.
Methods
Objectives
The aim of this trial is to assess whether the proposed allogeneic NKT cell adoptive transfer, when given in combination with gefitinib, warrants further consideration based on its safety and efficacy for the treatment of advanced EGFR-mutant NSCLCs. Effectiveness is being evaluated by PFS, the time to progression (TTP), overall response rate(ORR), disease control rate (DCR) and overall survival (OS). Safety assessment is based on adverse events (AEs), vital signs, clinical laboratory tests, such as haematologic, blood biochemical and urine analysis, and electrocardiograms.
Trail design
The study protocol (Issue date: 9 September 2017, protocol amendment number: v1.2) was written in accordance with the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) 2013 Statement [25]. A SPIRIT checklist is provided in the supplementary material (Additional file 1: Table S1). This early exploratory phase I/II clinical trial was initiated by the investigators and supported by the key research and development special funding of the Jiangsu Science and Technology Bureau for social development. The affiliated Hospital of Jiangsu University is responsible for clinical research.
The study was designed as a prospective, randomized, open-label, controlled phase I/II parallel-group trial to explore the efficacy and safety of NKT cell infusion immunotherapy combined with gefitinib versus gefitinib monotherapy in patients with advanced EGFR-mutated NSCLC (Fig. 1). This study will recruit 30 participants with advanced NSCLC who meet the inclusion/exclusion criteria and individually randomize them at a 1:1 ratio based on the trial schedule (Fig. 1). The two arms of the trial are as follows (Table 1):
-
Experimental group (Arm A): 250 mg gefitinib orally once daily. After being effectively treated with gefitinib for 8 weeks, allogeneic NKT cell transfer treatment will be added every 4 weeks, with a total cell number of 1 × 1010 ± 15% divided into two infusions with an interval of 3 days. This process will be repeated for a total of 16 weeks, which is defined as one-cell therapy cycle, and then NKT cell infusion treatment will be suspended for 4 weeks. After that, this cycle will be continually repeated three times (total of 60 weeks) or stopped when disease progression/unacceptable toxicity/participant choice occurs (Table 1).
-
Control group (Arm B): 250 mg gefitinib orally once daily until disease progression/unacceptable toxicity/participant choice occurs.
Study population
The main participant inclusion and exclusion criteria are shown in Table 2. This trial aims to include only patients with advanced NSCLC (III/IV) harbouring mutated EGFR (exon 19 deletion or exon 21 Leu858 Arg point mutation) who can be effectively treated with gefitinib.
This is also an exploratory study to test the safety and efficacy of the intravenous infusion of CD8 + CD56+ NKT cells, which replicates a planned larger study in at a smaller scale. Some authors have put forward suggestions on the sample size of pilot trials, specifically, 10 [26], 12 [27], or 15 [28] per group and a total of at least 20 participants [29]. According to a sample size “rule of thumb” of 30, the number of patients was designated as 15 patients in the experimental group and 15 patients in the control group, with a total sample size of 30 patients in this study. Although the power of this study is inadequate for evaluating clinical efficacy, the estimation of the efficacy of NKT cell immunotherapy combined with gefitinib and gefitinib alone will enable follow-up studies to calculate the efficacy more accurately.
Randomization
After the subjects are registered (and before any trial treatment), the subjects will be randomly assigned to the experimental group (Arm A) or the control group (Arm B) at a proportion of 1:1. The method of block randomization will be used to randomize the subjects into the groups. The random number table will be generated by statistics experts.
Preparation and administration of NKT cells
In this study, healthy immediate family members of the patient will be selected as donors for peripheral blood of nuclear cell (PBMC) collection and NKT cell preparation. PBMCs of the donor will be collected by an automatic blood cell separator and then frozen in liquid nitrogen. In the treatment phase of the study, PBMCs will be thawed, cultured and expanded with NKT complete medium with a protocol specially developed by the Institute of Cell Therapy, Tsinghua University, China. Prior to cell infusion, the quality of expanded NKT cells will be tested based on the cell number, purity, viability and sterility. The criteria of the tested cells included viability ≥90%, CD8+ ≥60%, and a minimum of 20% CD8 + CD56+ NKT cells. Along with gefitinib treatment in both Arms A and B, all patients in Arm A will intravenously receive 1 × 1010 expanded cells over 1 month with an interval of 3 days according to the schedule in Table 1. At the end of the cell transfusion, the subject will lie still and will be observed for 1 h, and their normal activities can be resumed if there is no discomfort or other adverse reactions.
Assessments
A schedule of procedures and assessments is shown in Additional file 2: Table S2.
Several assessments will be used for the evaluation of therapeutic effects, including tumour lesion measurements, patient quality of life scores, and the detection of serum tumour markers, such as CEA. For tumour lesion detection, according to the Response Evaluation Criteria in Solid Tumors version 1.1 (RECIST Version 1.1), computed tomography (CT) will be used to measure the size of solid tumours during screening, treatment and follow-up in the study. All baseline assessments of the tumour focus size should be completed as close to the start of treatment as possible. Additionally, the KPS score and EORTC QLQ-C30-LC13 score will be evaluated to assess the quality of life of patients with lung cancer in all stages.
AEs, vital signs and safety laboratory examinations will be used for safety evaluation. The severity of AEs will be graded using a modified version of The Common Terminology Criteria for AEs (CTCAE v5.0), reported and addressed at any time during the course of the study. Nevertheless, vital signs, including blood pressure, body temperature, respiration and heart rate, will be monitored during all visits, and routine safety laboratory examinations are detailed in Table S2.
Outcomes
Primary effectiveness endpoint
The efficacy will be evaluated based on PFS, which is defined as the time from randomization to the first recording of disease progression (as defined by RECIST v1.1) or the death of the patient. Patients who are still alive and have no progression as of the date of analysis will be recorded as the date of their last imaging evaluation.
Secondary effectiveness endpoints
TPP: the length of time from the date of randomization to tumour progression based on RECIST v1.1 criteria.
ORR: the proportion of participants with complete remission and partial remission, as judged by RECIST v1.1.
DCR: the proportion of participants with an objective response and stable disease, as defined by RECIST v1.1.
OS: defined as the time from the beginning of randomization to death from any cause. For patients who are still alive on the date of analysis, the date of their last contact will be recorded as the endpoint.
Security endpoints
Safety and toxicity assessment will be calculated based on AEs, vital signs, clinical laboratory tests, and electrocardiograms. Each AE will be monitored during the study, and its nature, intensity and relationship with treatment will be evaluated.
Statistical analysis
A full analysis set will be used to analyse the primary and secondary efficacy indicators. The full analysis set refers to the ideal subject set, which is as close as possible to intention-to-treat principles (the main analysis should include all subjects). For missing value estimation of the main variables, the last observation carried forward (LOCF) method will be used to carry forward the missing data of the study, and the number of subjects whose efficacy is evaluated at the endpoint will be consistent with that at the beginning of the study. The safety set is the main group of safety evaluations in this study. All groups with at least one study drug (cell preparation) and at least one safety assessment record will constitute the safety set of this study.
All statistical tests will be conducted using unilateral tests, and P < 0.05 will be considered to be statistically significant (except when specifically stated). Measurement data will be statistically described by the mean, median, standard deviation, maximum, minimum, and 25 and 75% quantiles; counting data or grade data will be expressed as the frequency. FPS, TTP and OS will be estimated by the Kaplan-Meier method and compared between groups with an unstratified log-rank test. Greenwood’s formula will be used to calculate 95% CIs. Fisher’s exact probability method will be used to compare the incidence of ORR, DCR and AEs between the two groups. The Wilcoxon rank-sum test will be used to compare the significant differences between the two groups for adverse reactions of different degrees. Changes in laboratory test results and quality of life assessments during the study will be summarized in tables and graphs. In addition, the relationship between abnormal changes and cell preparation will be further analysed.
Discussion
The ideal combination of immunotherapy with EGFR-TKIs should target different mechanisms of tumour-induced immunosuppression in the microenvironment [30]. Different types of killer cells combined with surgery and chemoradiotherapy have been explored for immunotherapy in NSCLC, including TILs and dendritic cell-cytokine induced killer (DC-CIK) cells [31,32,33]. Gefitinib prevents the proliferation of mutant EGFR-dependent cells, enhances the presentation of tumour antigens, and promotes the apoptosis of tumour cells without affecting biological functions of immune effector cells. However, as described in previous publications, the efficacy of autologous killer cell infusion in the clinic still needs to be improved [34]. In this study, we used allogeneic CD8 + CD56+ killer cells combined with gefitinib to treat NSCLC with EGFR mutations. Compared with previous studies, there are several different properties of this clinical design. First, the cells we used in this protocol are different from previously reported DC-CIK cells, which are rich in CD8 + CD56+ NKT cells. The biological properties of CD8 + CD56+ cells in humans and their equivalent subset, CD8 + NK1.1+ cells, in mice have been analysed in the lab, and the data showed that these CD8+ NKT subsets might have innate and adaptive immune functions and exhibit stronger cytotoxicity functions than conventional CD8-CD56+ NK and CTL cells; additionally, more granzyme particles were found in their cytoplasm [26]. Second, based on the higher cell proliferation rate in the NKT culture medium that we established, more killer cells can be easily expanded from a small number of seeded PBMCs. Thus, a large number of cells can be used for each transfer treatment. In this protocol, the total cell number of transferred cells in this trial was 1 × 1010 cells per week with two transfers, which was significantly greater than the cell numbers in previous studies, which were generally 109 per week or even lower. The safety test data of previous studies in a mouse model (CD8 + NK1.1+ cells), preclinical study and primary clinical safety trial (CD8 + CD56+ cells) in humans showed that this number of CD8 + CD56+ NKT cells caused no obvious adverse reactions or cytotoxicity in recipients (data not shown). Thus, in this study, we continued to use this dose of transferred cells in EGFR-TKI gefitinib combination therapy to further evaluate its safety and efficiency.
The tumour microenvironment in the patient promotes immune suppression and induces anergy and exhaustion in endogenous and transferred immune cells through different mechanisms [35]. Immune checkpoint blockades with anti-PD-1 mAbs successfully reinvigorate TILs and provide clinical benefits to patients with advanced cancer [36]. Unfortunately, published data has shown that anti-PD-1 was not associated with a significantly longer PFS than chemotherapy in NSCLC patients with low PD-L1 expression [37]. Thus, effectively reversing immune suppression in patients with NSCLC is a key factor for successful immunotherapy. Accumulating data on allogeneic transplantation showed that allogeneic human leukocyte antigens (HLAs) induced a T cell response with extraordinary strength and diversity of the alloreactive repertoire compared with classic antigens. These allorecognition-activated alloimmune T cells are the backbone of adaptive immune responses to transplants from donors or to the host, which, respectively cause graft rejection and graft-versus host disease (GVHD) [38, 39]. In this trial, we prepared allogeneic CD8 + CD56+ NKT cells from PBMCs for NSCLC treatment. After transfer, in addition to the direct cellular-mediated cytotoxicity to tumour cells, allogeneic CD8 + CD56+ NKT cells also provide mismatched donor HLA peptide for alloimmune T cell activation in recipients through the allorecognition pathway. Generally, graft-versus-host disease occurs in immune-deficient recipients who undergo immune organ transplantation, such as bone marrow and thymus [40]. However, in this case, there are two points that are dramatically different from haematopoietic stem cells (HSCs) or T cell progenitor transfer treatment. First, transferred allogeneic CD8 + CD56+ NKT cells in this study are mature cells without potential differentiation capability, which stem cells and progenitor cells have. Next, the participants in the trial were immunocompetent, which was different from the patients accepting bone marrow transplantation. Thus, these transferred allogeneic CD8 + CD56+ NKT cells can effectively prime alloimmune T cells of patients to activate cells and reverse tumour microenvironment-induced immune suppression without inducing GVHD. We did not observe any clinical GVHD as an adverse reaction in preclinical and primary clinical studies.
In summary, we developed this clinical trial using allogeneic CD8 + CD56+ NKT cells combined with gefitinib for patients with advanced NSCLC with EGFR mutations to address gefitinib acquired resistance and extend PFS in these patients. Although the sample size is small in this exploratory trial, the success of this approach will help expand the testing scale, extending to other EGFR-TKIs and a variety of other tumours.
Availability of data and materials
Not applicable – data collection is still ongoing.
Abbreviations
- AE:
-
Adverse event
- Anti-PD-1:
-
Anti-programmed death-1
- Anti-PD-L1:
-
Anti-programmed death-1 ligand
- CAR-T:
-
Chimeric antigen receptor t
- DC-CIK:
-
Dendritic cell-cytokine induced killer
- CT:
-
Computed tomography
- CTCAE:
-
Common Terminology Criteria for AEs
- DCR:
-
Disease control rate
- EGFR:
-
Epidermal growth factor receptor
- EGFR-TKIs:
-
Epidermal growth factor receptor tyrosine kinase inhibitors
- GVHD:
-
Graft-versus host disease
- HSCs:
-
Haematopoietic stem cells
- HLAs:
-
Human leukocyte antigens
- LOCF:
-
Last observation carried forward
- MDSCs:
-
Myeloid-derived suppressor cells
- NKT:
-
Natural killer T
- NSCLC:
-
Non-small-cell lung cancer
- ORR:
-
Overall response rate
- OS:
-
Overall survival
- PBMCs:
-
Peripheral blood mononuclear cells
- PFS:
-
Progression-free survival
- RECIST:
-
Response Evaluation Criteria In Solid Tumors
- SPIRIT:
-
Standard Protocol Items: Recommendations for Interventional Trials
- TTP:
-
Time to progression
- TILs:
-
Tumour-infiltrating lymphocytes
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. https://doi.org/10.3322/caac.21492.
Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, et al. Eastern cooperative oncology G. comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346(2):92–8. https://doi.org/10.1056/NEJMoa011954.
Lynch T, Bell D, Sordella R, Gurubhagavatula S, Okimoto R, Brannigan B, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350(21):2129–39. https://doi.org/10.1056/NEJMoa040938.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med. 2009;361(10):947–57. https://doi.org/10.1056/NEJMoa0810699.
Maemondo M, Inoue A, Kobayashi K, Sugawara S, Oizumi S, Isobe H, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362(25):2380–8. https://doi.org/10.1056/NEJMoa0909530.
Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–42. https://doi.org/10.1016/S1470-2045(11)70184-X.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–8. https://doi.org/10.1016/S1470-2045(09)70364-X.
Stirrups R. Osimertinib improves progression-free survival in NSCLC. Lancet Oncol. 2018;19(1):e10. https://doi.org/10.1016/S1470-2045(17)30893-8.
Barnet MB, O'Toole S, Horvath LG, Selinger C, Yu B, Ng CC, et al. EGFR-co-mutated advanced NSCLC and response to EGFR tyrosine kinase inhibitors. J Thorac Oncol. 2017;12(3):585–90. https://doi.org/10.1016/j.jtho.2016.09.001.
Saito H, Fukuhara T, Furuya N, Watanabe K, Sugawara S, Iwasawa S, et al. Erlotinib plus bevacizumab versus erlotinib alone in patients with EGFR-positive advanced non-squamous non-small-cell lung cancer (NEJ026): interim analysis of an open-label, randomised, multicentre, phase 3 trial. Lancet Oncol. 2019;20(5):625–35. https://doi.org/10.1016/S1470-2045(19)30035-X.
Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–54. https://doi.org/10.1056/NEJMoa1200690.
Gainor JF, Shaw AT, Sequist LV, Fu X, Azzoli CG, Piotrowska Z, et al. EGFR mutations and ALK rearrangements are associated with low response rates to PD-1 pathway blockade in non-small cell lung Cancer: a retrospective analysis. Clin Cancer Res. 2016;22(18):4585–93. https://doi.org/10.1158/1078-0432.CCR-15-3101.
Mazzaschi G, Madeddu D, Falco A, Bocchialini G, Goldoni M, Sogni F, et al. Low PD-1 expression in cytotoxic CD8(+) tumor-infiltrating lymphocytes confers an immune-privileged tissue microenvironment in NSCLC with a prognostic and predictive value. Clin Cancer Res. 2018;24(2):407–19. https://doi.org/10.1158/1078-0432.CCR-17-2156.
Creelan BC, Yeh TC, Kim SW, Nogami N, Kim DW, Chow LQM, et al. A phase 1 study of gefitinib combined with durvalumab in EGFR TKI-naive patients with EGFR mutation-positive locally advanced/metastatic non-small-cell lung cancer. Br J Cancer. 2021;124:383-90. https://doi.org/10.1038/s41416-020-01099-7.
Yang JC, Gadgeel SM, Sequist LV, Wu CL, Papadimitrakopoulou VA, Su WC, et al. Pembrolizumab in combination with Erlotinib or Gefitinib as first-line therapy for advanced NSCLC with sensitizing EGFR mutation. J Thorac Oncol. 2019;14(3):553–9. https://doi.org/10.1016/j.jtho.2018.11.028.
Godfrey DI, Stankovic S, Baxter AG. Raising the NKT cell family. Nat Immunol. 2010;11(3):197–206. https://doi.org/10.1038/ni.1841.
Porcelli S, Yockey CE, Brenner MB, Balk SP. Analysis of T cell antigen receptor (TCR) expression by human peripheral blood CD4-8- alpha/beta T cells demonstrates preferential use of several V beta genes and an invariant TCR alpha chain. J Exp Med. 1993;178(1):1–16. https://doi.org/10.1084/jem.178.1.1.
Terabe M, Berzofsky JA. The immunoregulatory role of type I and type II NKT cells in cancer and other diseases. Cancer Immunol Immunother. 2014;63(3):199–213. https://doi.org/10.1007/s00262-013-1509-4.
Chan WK, Rujkijyanont P, Neale G, Yang J, Bari R, Das Gupta N, et al. Multiplex and genome-wide analyses reveal distinctive properties of KIR+ and CD56+ T cells in human blood. J Immunol. 2013;191(4):1625–36. https://doi.org/10.4049/jimmunol.1300111.
Campbell JJ, Qin S, Unutmaz D, Soler D, Murphy KE, Hodge MR, et al. Unique subpopulations of CD56+ NK and NK-T peripheral blood lymphocytes identified by chemokine receptor expression repertoire. J Immunol. 2001;166(11):6477–82. https://doi.org/10.4049/jimmunol.166.11.6477.
van den Heuvel MJ, Peralta CG, Hatta K, Han VK, Clark DA. Decline in number of elevated blood CD3(+) CD56(+) NKT cells in response to intravenous immunoglobulin treatment correlates with successful pregnancy. Am J Reprod Immunol. 2007;58(5):447–59. https://doi.org/10.1111/j.1600-0897.2007.00529.x.
Seregin S, Chen G, Laouar Y. Dissecting CD8+ NKT cell responses to Listeria infection reveals a component of innate resistance. J Immunol (Baltimore, Md: 1950). 2015;195(3):1112–20. https://doi.org/10.4049/jimmunol.1500084.
Ruiz A, Soudja S, Deceneux C, Lauvau G, Marie J. NK1.1+ CD8+ T cells escape TGF-β control and contribute to early microbial pathogen response. Nat Commun. 2014;5:5150. https://doi.org/10.1038/ncomms6150.
Li Z, Wu Y, Wang C, Zhang M. Mouse CD8NKT-like cells exert dual cytotoxicity against mouse tumor cells and myeloid-derived suppressor cells. Cancer Immunol Immunother. 2019;68(8):1303–15. https://doi.org/10.1007/s00262-019-02363-3.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gotzsche PC, Krleza-Jeric K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158(3):200–7. https://doi.org/10.7326/0003-4819-158-3-201302050-00583.
Birkett MA, Day SJ. Internal pilot studies for estimating sample size. Stat Med. 1994;13(23–24):2455–63. https://doi.org/10.1002/sim.4780132309.
Julious SA. Sample size of 12 per group rule of thumb for a pilot study. Pharm Stat. 2010;4(4):287–91. https://doi.org/10.1002/pst.185.
Browne RH. On the use of a pilot sample for sample size determination. Stat Med. 1995;14(17):1933–40. https://doi.org/10.1002/sim.4780141709.
Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol. 2012;65(3):301–8. https://doi.org/10.1016/j.jclinepi.2011.07.011.
Sharma P, Allison JP. Immune checkpoint targeting in cancer therapy: toward combination strategies with curative potential. Cell. 2015;161(2):205–14. https://doi.org/10.1016/j.cell.2015.03.030.
Ratto G, Zino P, Mirabelli S, Minuti P, Aquilina R, Fantino G, et al. A randomized trial of adoptive immunotherapy with tumor-infiltrating lymphocytes and interleukin-2 versus standard therapy in the postoperative treatment of resected nonsmall cell lung carcinoma. Cancer. 1996;78(2):244–51. https://doi.org/10.1002/(SICI)1097-0142(19960715)78:2<244::AID-CNCR9>3.0.CO;2-L.
Kimura H, Matsui Y, Ishikawa A, Nakajima T, Yoshino M, Sakairi Y. Randomized controlled phase III trial of adjuvant chemo-immunotherapy with activated killer T cells and dendritic cells in patients with resected primary lung cancer. Cancer Immunol Immunother. 2015;64(1):51–9. https://doi.org/10.1007/s00262-014-1613-0.
Ben-Avi R, Farhi R, Ben-Nun A, Gorodner M, Greenberg E, Markel G, et al. Establishment of adoptive cell therapy with tumor infiltrating lymphocytes for non-small cell lung cancer patients. Cancer Immunol Immunother. 2018;67(8):1221–30. https://doi.org/10.1007/s00262-018-2174-4.
Xiao Z, Wang CQ, Feng JH, Zhou MH, Wang YZ, Li NN, et al. Effectiveness and safety of chemotherapy with cytokine-induced killer cells in non-small cell lung cancer: a systematic review and meta-analysis of 32 randomized controlled trials. Cytotherapy. 2019;21(2):125–47. https://doi.org/10.1016/j.jcyt.2018.10.011.
Crespo J, Sun H, Welling TH, Tian Z, Zou W. T cell anergy, exhaustion, senescence, and stemness in the tumor microenvironment. Curr Opin Immunol. 2013;25(2):214–21. https://doi.org/10.1016/j.coi.2012.12.003.
Zarour HM. Reversing T-cell dysfunction and exhaustion in Cancer. Clin Cancer Res. 2016;22(8):1856–64. https://doi.org/10.1158/1078-0432.CCR-15-1849.
Carbone DP, Reck M, Paz-Ares L, Creelan B, Horn L, Steins M, et al. First-line Nivolumab in stage IV or recurrent non-small-cell lung Cancer. N Engl J Med. 2017;376(25):2415–26. https://doi.org/10.1056/NEJMoa1613493.
DeWolf S, Sykes M. Alloimmune T cells in transplantation. J Clin Invest. 2017;127(7):2473–81. https://doi.org/10.1172/JCI90595.
van den Heuvel H, Heidt S, Roelen DL, Claas FH. T-cell alloreactivity and transplantation outcome: a budding role for heterologous immunity? Curr Opin Organ Transplant. 2015;20(4):454–60. https://doi.org/10.1097/MOT.0000000000000218.
Ghimire S, Weber D, Mavin E, Wang XN, Dickinson AM, Holler E. Pathophysiology of GvHD and other HSCT-related major complications. Front Immunol. 2017;8:79. https://doi.org/10.3389/fimmu.2017.00079.
Acknowledgements
We thank all the patients who participated in this trial, all investigators who devote their time and passion in the implementation of this study.
Funding
This study was funded by Jiangsu Provincial Key Research and Development Program (Grant no. BE2017696). The funding source has no role in study design, data collection, analysis, interpretation, the writing of the manuscript, and the decision to submit results. This study protocol manuscript was peer reviewed by the funding body.
Author information
Authors and Affiliations
Contributions
SX and DYC was responsible for initiating, applying, organizing, funding and monitoring this clinical study; MHZ, ZHG and HZA provided key technical support for the preparation of NKT cells; CMM supervised the conduct of the study; JRL provided statistical analysis and statistical expertise in clinical trial design; WJY draft the manuscript, SX and ZHG revised the manuscript; FY and YX enrolled participants, assigned participants to interventions and coordinated with other members; XQL, LJ, CHD, FHQ and DQW are members of the endpoint adjudication committee and they played an important role in the recruitment of subjects and the diagnosis and treatment of diseases; WJY and YLM managed data on the ResMan clinical trial management public platform; XJF and YPZ worked in PBMCs collection from the patients. All authors read study protocol and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Institutional review board approval was obtained for the trial from the Biomedical Research Ethics Committee of affiliated hospital of Jiangsu University (Approved No. of ethic committee: SWYXLL20170904). This Trial was registered on 21 November, 2017 with www.chictr.org.cn, ChiCTR-IIR-17013471. Written informed consent is obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
SPIRIT Checklist.
Additional file 2: Table S2.
Schedule of Procedures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, W., Ye, F., Yuan, X. et al. A phase I/II clinical trial on the efficacy and safety of NKT cells combined with gefitinib for advanced EGFR-mutated non-small-cell lung cancer. BMC Cancer 21, 877 (2021). https://doi.org/10.1186/s12885-021-08590-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-021-08590-1