Abstract
Respiratory failure from severe asthma is a potentially reversible, life-threatening condition. Poor outcome in this setting is frequently a result of the development of gas-trapping. This condition can arise in any mechanically ventilated patient, but those with severe airflow limitation have a predisposition. It is important that clinicians managing these types of patients understand that the use of mechanical ventilation can lead to or worsen gas-trapping. In this review we discuss the development of this complication during mechanical ventilation, techniques to measure it and strategies to limit its severity. We hope that by understanding such concepts clinicians will be able to reduce further the poor outcomes occasionally related to severe asthma.
Similar content being viewed by others
Introduction
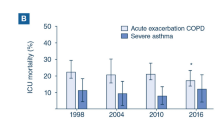
Asthma continues to inflict significant morbidity and mortality worldwide. Despite advances in therapy and in our understanding of its pathophysiology, the prevalence of asthma is increasing [1–3], although there is significant age and geographic variation [4]. While the prevalence of asthma has increased, outcomes of severe asthma appear to be improving, with lower complication rates and fewer in-hospital deaths [3]. Nonetheless, it is estimated that about 10% of individuals admitted to hospital for asthma go to the intensive care unit, with 2% of all admitted patients being intubated [5]. Not surprisingly, admission to the intensive care unit and need for mechanical ventilation are associated with mortality [1, 2]. When death does occur it is most commonly a result of one of the complications of severe gas-trapping. These complications include barotrauma, hypotension and refractory respiratory acidosis. If the morbidity and mortality associated with severe asthma is to continue to decrease, then it is imperative that clinicians caring for such patients have a clear understanding of how gas-trapping can occur and of how it may be recognized/measured and limited.
This article reviews the principles of mechanical ventilation in severe asthma, giving particular attention to the development of gas-trapping as well as how to measure and limit it. Specific details on pharmacological management and prevention of future episodes of severe asthma are beyond the scope of this review but can be found elsewhere [6, 7].
Rationale for mechanical ventilation in severe asthma
When a patient with severe asthma does not respond adequately to medical therapy, prompt intervention in an effort to provide adequate oxygenation and ventilation by means of noninvasive positive pressure ventilation (NPPV) or invasive positive pressure mechanical ventilation is frequently life saving. Given that these patients have a propensity to develop severe airflow limitation, making it difficult to exhale all of their inspired gas, gas-trapping (which leads to dynamic hyperinflation and is also referred to as intrinsic positive end-expiratory pressure [PEEP] and auto-PEEP) frequently occurs. As a result, one of the most important principles of mechanical ventilation in this setting is to utilize a strategy aimed at reducing the likelihood that this complication will occur.
Noninvasive positive pressure ventilation
It is possible that in some patients with severe asthma NPPV may be preferential to intubation. However, to date only two small, prospective, randomized trials have been completed that evaluated the use of NPPV in patients with severe asthma: one in children [8] and a pilot study in adults [9]. Both of those studies suggested that, in selected patients with severe asthma, NPPV could improve lung function and possibly reduce the need for hospitalization. There are also some observational studies, which yielded consistent results [10, 11]. In chronic obstructive pulmonary disease – another condition frequently associated with severe airflow limitation – a number of prospective randomized trials have shown that noninvasive ventilation reduces the need for endotracheal intubation, length of hospital stay and in-hospital mortality rate, and even that it improves long-term survival [12–16]. The degree to which these data can be applied to the asthmatic population is debatable.
Even though NPPV requires further investigation in severe asthma, it is currently being used as an initial alternative to mechanical ventilation in some centres. As is the case in other conditions, the success of NPPV depends on a variety of factors including clinician experience [17], patient selection and interfaces [16], and that it is not used in patients with any known contraindications [18, 19]. It is particularly important to be very cautious in using NPPV in paediatric patients, in whom the margins of safety are narrow, and a low threshold for intubation when required should be maintained in these patients. The commonly accepted contraindications to NPPV are as follows: cardiac/respiratory arrest, severe encephalopathy, haemodynamic instability, facial surgery/deformity, high risk for aspiration, non-respiratory organ failure, severe upper gastrointestinal bleeding, unstable arrhythmia, and upper airway obstruction.
The decision to intubate
The decision to intubate should be based mainly on clinical judgement. Markers of deterioration include rising carbon dioxide levels (including normalization in a previously hypocapnic patient), exhaustion, mental status depression, haemodynamic instability and refractory hypoxaemia [20]. Clinical judgement is crucial because many patients presenting with hypercapnia do not require intubation [21], and thus the decision should not be based solely on blood gases.
Development of gas-trapping
Severe airflow limitation is always associated with severe asthma exacerbation and occurs as a result of broncho-constriction, airway oedema and/or mucous plugging. Consequently, the work of breathing is significantly increased. Increased work occurs because the normally passive process of expiration becomes active in an attempt by the patient to force the inspired gas out of their lungs. In addition, there is increased inspiratory work caused by high airway resistance and hyperinflation. This hyperinflation causes the lungs and chest wall to operate on a suboptimal portion of their pressure–volume curves (i.e. they are overstretched), resulting in increased work to stretch them further in an attempt to ventilate adequately. Gas-trapping occurs because the low expiratory flow rates mandate long expiratory times if the entire inspired volume is to be exhaled. If the next breath interrupts exhalation, then gas-trapping results (Fig. 1). Because gas is trapped in the lungs there is additional pressure at the end of expiration (auto-PEEP or intrinsic PEEP) above applied PEEP, which leads to dynamic hyperinflation. Auto-PEEP, intrinsic PEEP and dynamic hyperinflation are terms that are frequently used interchangeably.
Dynamic hyperinflation has been defined as failure of the lung to return to its relaxed volume or functional residual capacity at end-exhalation [22–24]. Of note, some refer to gas-trapping as the component of hyperinflation that is due to airway occlusion, and is therefore potentially less amenable to ventilator manipulation (in some situations, the dominant component of total hyperinflation in severe asthma [25]). Hyperinflation can be adaptive in that with higher lung volumes the increase in airway diameter and elastic recoil pressure enhances expiratory flow; however, excessive dynamic hyperinflation has been shown to predict the development of hypotension and barotrauma during mechanical ventilation of severe asthma [25]. These developments are the usual causes of excess morbidity and mortality.
Measuring gas-trapping
Gas-trapping can be measured a variety of ways involving volume, pressure, or flow of gas. Estimating gas-trapping using volume measures can be done by collecting the total exhaled volume during 20–60 s of apnoea in a paralyzed patient. Tuxen and coworkers [25, 26] described this volume as 'VEI', or the volume of gas at end-inspiration above functional residual capacity (Fig. 2). Tuxen and Lane [25] also showed that a VEI above 20 ml/kg predicted complications of hypotension and barotrauma in mechanically ventilated patients with severe asthma. Prospective studies involving larger patient numbers are needed to validate the predictive value of VEI. Another way to estimate gas-trapping is to measure end-expiratory pressure in the lungs. If the expiratory port of the ventilator is occluded at end-expiration, then the proximal airway pressure will equilibrate with alveolar pressure and permit measurement of auto-PEEP (end-expiratory pressure above applied PEEP) at the airway opening (Fig. 3). Expiratory muscle contraction can elevate auto-PEEP without adding to dynamic hyperinflation, and therefore for accurate measurement of auto-PEEP the patient should be relaxed. Auto-PEEP measured in this manner has not yet been shown to correlate with complications [27]. Another way to look for gas-trapping is to observe the flow versus time graphics on the ventilator. If inspiratory flow begins before expiratory flow ends, then gas must be trapped in the lungs.
Each of the measures of gas-trapping described thus far rely on the assumption that the airways all remain in communication with the proximal airway throughout expiration because pressure, flow, or gas volume cannot be measured from a noncommunicating airway. Frequently, all of the airways may not be in communication with the proximal airway in severe asthma. For example, it has been noted (perhaps as a result of complete airway closure) that there may at times be 'unmeasured' or 'occult' auto-PEEP [23]. This occult auto-PEEP has all of the untoward effects of the measurable auto-PEEP, but it cannot be quantified using the usual approaches [23]. As a result, exercising good clinical judgement is important. When assessing dynamic hyperinflation/gas-trapping in mechanically ventilated patients with severe asthma, clinicians should question low auto-PEEP measurements in clinical situations that suggest otherwise.
One such clinical situation would be increasing plateau airway pressure (Pplat) unexplained by decreases in respiratory system compliance during volume-cycled ventilation. Pplat can be determined by stopping flow at end-inspiration utilizing an end-inspiratory pause (typically 0.4 s). During this pause, airway opening pressure falls from peak pressure (the sum of static and resistive pressures) to Pplat (static pressure alone) as resistive pressure falls to zero (Fig. 4). Patients must be paralyzed or heavily sedated to obtain reliable measurements. Because alveolar pressure increases as lung volume increases, measurement of Pplat should reflect gas-trapping (again assuming that there is no other explanation, such as adjustments to the ventilator or changes in respiratory system compliance). Some have pointed out that if Pplat is kept at less than 30 cmH2O then complications appear to be rare [28], although no studies have yet shown Pplat to be a reliable predictor of complications. Similarly, when using pressure cycled ventilation, decreasing tidal volumes may indicate gas-trapping. Other situations in which clinicians should suspect gas-trapping include increasing chest wall girth, hyperinflation on chest imaging, reduced efficiency of ventilation, increased patient effort, unexplained patient agitation, development of barotrauma, haemodynamic compromise and missed respiratory efforts (as patients attempt to trigger the ventilator but cannot generate enough pressure to overcome the auto-PEEP that has developed) [22].
Limiting gas-trapping
Because gas-trapping is potentially associated with significant adverse events in severe asthma, clinicians must be vigilant for its development and employ strategies to limit it. Understanding how gas-trapping occurs is the first step in developing such strategies. These strategies include controlled hypoventilation (reduced tidal volumes [less gas to exhale] and reduced respiratory rates [longer expiratory time]), relieving expiratory flow resistance (frequent airway suctioning if necessary, bronchodilators, steroids, large-bore endotracheal tube), reducing inspiratory time by increasing the inspiratory flow rate or incorporating nondistensible tubing, and reducing the need for high minute ventilation by decreasing carbon dioxide production (e.g. sedation/paralysis, controlling fever/pain). The application of external PEEP in severe asthma remains a controversial topic. It could theoretically decrease the work of breathing and hence carbon dioxide production, while limiting gas-trapping by splinting the airways open [29, 30]; however, in practice there are situations in which the application of external PEEP may increase total PEEP and worsen gas-trapping.
Assuming that appropriate medical therapy to alleviate airflow obstruction has been administered (i.e. inhaled beta agonists, inhaled ipratroprium bromide, steroids, with/without intravenous magnesium sulphate, etc.), by far the most effective method of decreasing dynamic hyperinflation/gas-trapping is to reduce the minute ventilation [31, 32]. Reducing the minute ventilation by adjusting the tidal volume, frequency, or set pressure on the ventilator may result in carbon dioxide retention. In this setting the controlled use of 'permissive hypercapnia' is generally considered well tolerated [33, 34]. Permissive hypercapnia that maintains a pH above 7.20 or an arterial carbon dioxide tension below 90 mmHg has gained widespread acceptance [27, 34–36]. Permissive hypercapnia has been used successfully in mechanically ventilated patients with status asthmaticus [33].
Expiratory time can be lengthened by using higher inspiratory flow settings (70–100 l/min) during volume cycled ventilation, using a shorter inspiratory time fraction, reducing respiratory rate, and eliminating any inspiratory pause. Prolongation of expiratory time has been shown to decrease dynamic hyperinflation in patients with severe asthma, as is evident by decreased plateau pressures [37]. The magnitude of this effect becomes relatively modest when the baseline minute ventilation is 10 l/min or less and when the baseline respiratory rate is low [37]. It should be emphasized that while modifying the I/E ratio is important in fine tuning the amount of gas-trapping, the single most effective way is by reducing minute ventilation [6, 7].
Applying adequate sedation and analgesia is a fundamental step in lowering the production of carbon dioxide and subsequently ventilatory requirements. Sedation and/or paralysis may also allow the clinician to avoid patient–ventilator dysynchrony and facilitate strategies to limit gas-trapping in the most severe of cases. It is beyond the scope of this review to recommend which agents or protocols are best for this. The use of neuromuscular blocking agents should be limited to short periods of time and only when absolutely necessary in patients with severe asthma who are not achieving synchrony with other agents. Although neuromuscular blocking agents effectively promote synchrony, lower the risk for barotrauma, reduce lactate accumulation [38] and reduce oxygen consumption and carbon dioxide production, their prolonged use, particularly when combined with steroids, can lead to prolonged paralysis and/or myopathy [39, 40].
The addition of extrinsic PEEP in the setting of auto-PEEP may reduce work of breathing and possibly even prevent gas-trapping by splinting the airways open [29]. In terms of reducing the work of breathing, the addition of extrinsic PEEP in patients with dynamic hyperinflation would theoretically reduce the inspiratory muscle effort required to overcome auto-PEEP and initiate an inspiration. It has been demonstrated that in patients with chronic obstructive pulmonary disease more than 40% of inspiratory muscle effort can be expended to overcome auto-PEEP [41, 42], and that adding extrinsic PEEP can attenuate the inspiratory muscle effort needed to trigger inspiration and improve patient–ventilator interaction. In these patients extrinsic PEEP must be titrated individually, with an average of 80% of the auto-PEEP being tolerated before the plateau pressures and total PEEP begin to increase. Such an approach is only useful in those patients who are breathing spontaneously and capable of triggering the ventilator. In addition, extrinsic PEEP may prevent airway collapse (which could lead to occult auto-PEEP) by splinting the airways open. If this is the case then extrinsic PEEP would be most useful only in the most severe of cases, including those patients who are not spontaneously breathing. It should be noted that extrinsic PEEP has also been shown to be effective at preventing ventilator-induced lung injury in other forms of lung injury and hence may be of added benefit in this situation. In practice, however, adding extrinsic PEEP in some patients with severe asthma has been shown to worsen auto-PEEP [43]. As mentioned above, it is occasionally difficult to measure auto-PEEP reliably, and if the extrinsic PEEP is greater than the auto-PEEP then gas-trapping will likely worsen. This has led some to recommend minimizing the use of extrinsic PEEP or not using it at all [35, 36] in the ventilation of patients with severe asthma. If extrinsic PEEP is to be used, then careful bedside observation with a clear understanding of how the benefits (reductions in auto-PEEP) and adverse effects (worsening gas-trapping) would manifest is mandatory.
Considerations for initial ventilator settings in patients with severe asthma
There have been a number of review articles recommending initial ventilator settings and algorithmic approaches to mechanical ventilation in severe asthma [6, 7]. The fine details of the ventilator settings are not as crucial as close attention to the basic principles of ventilating patients with severe asthma: employ low tidal volumes and respiratory rate; prolong expiratory time as much as possible; shorten inspiratory time as much as possible; and monitor for the development of dynamic hyperinflation.
As a starting point for ventilating patients with severe asthma, we recommend that the ventilator initially be used in pressure control mode, setting the pressure to achieve a tidal volume of 6–8 ml/kg, respiratory rate of 11–14 breaths/min and PEEP at 0–5 cmH2O. We use these settings with a goal of obtaining a pH, in general, above 7.2 and a Pplat under 30 cmH2O. If a Pplat under 30 cmH2O cannot be maintained, then the patient must be evaluated for causes of decreased respiratory system compliance (i.e. pneumothorax, misplaced endotracheal tube, pulmonary oedema, etc.) beyond the development of dynamic hyperinflation. If no such causes are evident then efforts to limit gas-trapping further must be considered. If permissive hypercapnia results in a pH below 7.2, then the same type of evaluation needs to occur, including consideration of increased sedation/paralysis and methods of decreasing carbon dioxide production (i.e. reducing fever, preventing over-feeding, decreasing patient effort, etc.). In addition to these examples, administration of sodium bicarbonate to maintain a pH of 7.2 during controlled hypoventilation has been investigated in patients with status asthmaticus [44]; however, no studies have demonstrated any benefit associated with bicarbonate infusion. Decisions regarding ongoing ventilator management must be based on the principles outlined in this review.
Adjuncts to mechanical ventilation
A large variety of unproven therapies that clinicians may need to consider in an emergent situation have been proposed, including intravenous magnesium sulphate, general anaesthesia, bronchoscopic lavage, heliox and extracorporeal membrane oxygenation.
Intravenous magnesium sulphate has bronchodilating properties and has been shown in limited studies to improve pulmonary function in patients with severe asthma [45, 46], at least in the short term. Several inhalation anaesthetic agents have intrinsic bronchodilator properties [47, 48] and there are reports of successful use of these agents in refractory status asthmaticus [49, 50]. The special equipment and personnel needed for inhalation anaesthesia and the significant haemodynamic complications associated with these agents make their use problematic. Ketamine is an intravenous agent that has analgesic and bronchodilating properties [51]. There are limited clinical data available regarding the use of ketamine in status asthmaticus [52, 53], and its side effects of tachycardia, hypertension, delirium and lowering the seizure threshold should always be taken into account.
In patients with status asthmaticus and severe mucous impaction, it has been suggested that bronchoscopic examination of the airways and removal of secretions may be beneficial [54]. As the presence of the bronchoscope may worsen lung hyperinflation and increase the risk for pneumothorax [55], we do not recommend this technique.
Heliox is a blend of helium and oxygen (usually at a 70 : 30 ratio), which is less dense than air, theoretically permitting higher flow rates through a given airway segment for the same driving pressure, thereby alleviating dynamic hyperinflation. Several small studies have shown heliox to reduce peak inspiratory pressure and arterial carbon dioxide tension, and to improve oxygenation in mechanically ventilated patients [56, 57]. That heliox is expensive, has a limited concentration of oxygen and has conflicting results in the literature [58–61] make it a somewhat controversial therapy, and at this time we cannot recommend it for routine use in severe asthma.
Extracorporeal membrane oxygenation is another expensive modality that has been successfully used in patients with severe refractory asthma [62, 63]. The use of these second-line therapies should be on a case-by-case basis, carefully weighing the risks and benefits.
Conclusion
Severe asthma exacerbation causing respiratory failure has not yet been eliminated, and remains a potentially reversible, life-threatening condition that imposes significant morbidity and mortality. When mechanical ventilation is required in severe asthma, it is important that clinicians managing these patients understand why gas-trapping occurs, how to measure it and how to limit its severity. We hope that by understanding such concepts clinicians will be able to reduce further the number of poor outcomes that are occasionally associated with severe asthma.
Abbreviations
- NPPV:
-
noninvasive positive pressure ventilation
- PEEP:
-
positive end-expiratory pressure
- Pplat:
-
plateau airway pressure
- VEI:
-
volume of gas at end-inspiration above functional residual capacity.
References
Richards GN, Kolbe J, Fenwick J, Rea HH: Demographic characteristics of patients with severe life threatening asthma: comparison with asthma deaths. Thorax 1993, 48: 1105-1109.
Turner MO, Noertjojo K, Vedal S, Bai T, Crump S, Fitzgerald JM: Risk factors for near-fatal asthma. A case-control study in hospitalized patients with asthma. Am J Respir Crit Care Med 1998, 157: 1804-1809.
Kearney SE, Graham DR, Atherton ST: Acute severe asthma treated by mechanical ventilation: a comparison of the changing characteristics over a 17 yr period. Respir Med 1998, 92: 716-721. 10.1016/S0954-6111(98)90001-4
Manfreda J, Sears MR, Becklake MR, Chan-Yeung M, Dimich-Ward H, Siersted HC, Ernst P, Sweet L, Van Til L, Bowie DM, et al.: Geographic and gender variability in the prevalence of bronchial responsiveness in Canada. Chest 2004, 125: 1657-1664. 10.1378/chest.125.5.1657
Pendergraft TB, Stanford RH, Beasley R, Stempel DA, Roberts C, McLaughlin T: Rates and characterisitics of intensive care unit admissions and intubations among asthma-related hospitalizations. Ann Allergy Asthma Immunol 2004, 93: 29-35.
Corbridge TC, Hall JB: The assessment and management of adults with status asthmaticus. Am J Respir Crit Care Med 1995, 151: 1296-1316.
Levy BD, Kitch B, Fanta CH: Medical and ventilatory management of status asthmaticus. Intensive Care Med 1998, 24: 105-117. 10.1007/s001340050530
Thill PJ, McGuire JK, Baden HP, Green TP, Checchia PA: Noninvasive positive-pressure ventilation in children with lower airway obstruction. Pediatr Crit Care Med 2004, 5: 337-342. 10.1097/01.PCC.0000128670.36435.83
Soroksky A, Stav D, Shpirer I: A pilot prospective, randomized, placebo-controlled trial of bilevel positive airway pressure in acute asthma attack. Chest 2003, 123: 1018-1025. 10.1378/chest.123.4.1018
Fernandez MM, Villagra A, Blanch L, Fernandez R: Non-invasive mechanical ventilation in status asthmaticus. Intensive Care Med 2001, 27: 486-492. 10.1007/s001340100853
Keenan SO, Gregor J, Sibbald WJ, Cook D, Gafni A: Noninvasive positive pressure ventilation in status asthmaticus. Chest 1996, 110: 767-774.
Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simonneau G, Benito S, Gasparetto A, Lemaire F, et al.: Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Eng J Med 1995, 333: 817-822. 10.1056/NEJM199509283331301
Plant PK, Owen JL: Early use of non-invasive positive pressure ventilation in the setting of severe, acute exacerbations of chronic obstructive pulmonary disease on general respiratory wards: a multicenter randomized controlled trial. Lancet 2000, 355: 1941-1935. 10.1016/S0140-6736(00)02323-0
Plant PK, Owen JL, Elliott MW: Non-invasive ventilation in acute exacerbations of chronic obstructive lung disease: long term survival and predictors of in-hospital outcome. Lancet 2001, 56: 708-712.
Confalonieri M, Parigi P, Scartabellati A, Aiolfi S, Scorsetti S, Nava S, Gandola L: Noninvasive mechanical ventilation imporves the immediate and long-term outcome of COPD patients with acute respiratory failure. Eur Respir J 1996, 9: 422-430. 10.1183/09031936.96.09030422
Soo Hoo GW, Santiago S, Williams A: Nasal mechanical ventilation for hypercapnic respiratory failure in chronic obstructive pulmonary disease: determinants of success and failure. Crit Care Med 1994, 22: 1253-1261.
Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS: Randomized, prospective trial of noninvasive positive pressure ventilaiton in acute respiratory failure. Am J Resp Crit Care Med 1995, 151: 1799-1806.
Sinuff T, Keenan SP: Clinical practice guideline for the use of noninvasive positive pressure ventilation in COPD patients with acute respiratory failure. J Crit Care 2004, 19: 82-91. 10.1016/j.jcrc.2004.04.006
Evans TW, Albert RK, Angus DC, Bion JF, Chiche J-D, Epstein SK, Fagon JY, Ranieri M, Sznajder JI, Torres A, Walley KR: International consensus conferences in intensive care medicine: noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med 2001, 163: 283-291.
National Heart, Lung and Blood Institute: Guidelines for the Diagnosis and Management of Asthma, Expert Panel Report 2. Publication number 97-4051. Bethesda: National Institutes of Health; 1997.
Mountain RD, Sahn S: Clinical features and outcomes in patients with acute asthma presenting with hypercapnia. Am Rev Respir Dis 1988, 138: 535-539.
Stewart TE, Slutsky AS: Occult, occult auto-PEEP in status asthmaticus. Crit Care Med 1996, 24: 379-380. 10.1097/00003246-199603000-00003
Leatherman JW, Ravenscraft SA: Low measured auto-positive end-expiratory pressure during mechanical ventilation of patients with severe asthma: hidden auto-positive end-expiratory pressure. Crit Care Med 1996, 24: 541-546. 10.1097/00003246-199603000-00028
Pepe PE, Marini JJ: Occult positive end-expiratory pressure in mechanically ventilated paitents with airflow obstruction. The auto-PEEP effect. Am Rev Resp Dis 1982, 126: 166-170.
Tuxen DV, Lane S: The effects of ventilatory pattern on hyperinflation, airway pressures, and circulation in mechanical ventilation of patients with severe air-flow obtruction. Am Rev Respir Dis 1987, 136: 872-879.
Tuxen DV, Williams TJ, Scheinkestel CD, Czarny D, Bowes G: Use of a measurement of pulmonary hyperinflation to control the level of mechanical ventilation in patients with acute severe asthma. Am Rev Respir Dis 1992, 146: 1136-1142.
Phipps P, Gerrard CS: The pulmonary physician in critical care: acute severe asthma in the intensive care unit. Thorax 2003, 58: 81-88. 10.1136/thorax.58.1.81
Leatherman J: Life-threatening asthma. Clin Chest Med 1994, 15: 453-479.
Kondili E, Alexopoulou C, Prinianakis G, Xirouchaki N, Georgopoulos D: Pattern of lung emptying and expiratory resistance in mechanically ventilated patients with chronic obstructive pulmonary disease. Intensive Care Med 2004, 30: 1311-1318.
Kondili E, Prinianakis G, Athanasakis D, Georgopoulos D: Lung emptying in patients with acute respiratory distress syndrome: effects of positive end-expiratory pressure. Eur Respir J 2002, 19: 811-819. 10.1183/09031936.02.00255102
Williams TJ, Tuxen DV, Scheinkestel CD, Czarny D, Bowes G: Risk factors for morbidity in mechanically ventilated patients with acute severe asthma. Am Rev Respir Dis 1992, 146: 607-615.
Bellomo R, McLaughlin P, Tai E, Parkin G: Asthma requiring mechanical ventilation. A low morbidity approach. Chest 1994, 105: 891-896.
Darioli R, Perret C: Mechanical controlled hypoventilation in status asthmaticus. Am Rev Respir Dis 1984, 129: 385-387.
Bigatello LM, Patroniti N, Sangalli F: Permissive hypercapnia. Curr Opin Crit Care 2001, 7: 34-40. 10.1097/00075198-200102000-00006
Peigang Y, Marini JJ: Ventilation of patients with asthma and chronic obstructive pulmonary disease. Curr Opin Crit Care 2002, 8: 70-76. 10.1097/00075198-200202000-00011
Rodrigo GJ, Rodrigo C, Hall JB: Acute asthma in adults: a review. Chest 2004, 125: 1081-1102. 10.1378/chest.125.3.1081
Leatherman JW, McArthur C, Shapiro RS: Effect of prolongation of expiratory time on dynamic hyperinflation in mechanically ventilated paitents with severe asthma. Crit Care Med 2004, 32: 1542-1545. 10.1097/01.CCM.0000130993.43076.20
Papiris S, Kotanidou A, Malagari K, Roussos C: Clinical review: Severe asthma. Crit Care 2002, 6: 30-44. 10.1186/cc1451
Leatherman JW, Fluegel WL, David WS, Davies SF, Iber C: Muscle weakness in mechanically ventilated patients with severe asthma. Am J Respir Crit Car Med 1996, 153: 1686-1690.
Behbehani NA, Al-Mane F, D'yachkova Y, Pare P, FitzGerald JM: Myopathy following mechanical ventilation for acute severe asthma: the role of muscle relaxants and corticosteroids. Chest 1999, 115: 1627-1631. 10.1378/chest.115.6.1627
Appendini L, Purro A, Patessio A, Zanaboni S, Carone M, Spada E, Donner CF, Rossi A: Partitioning of inspiratory muscle workload and pressure assistance in ventilator-dependent COPD patients. Am J Respir Crit Care Med 1996, 154: 1301-1309.
Guerin C, Milic-Emili J, Fournier G: Effect of PEEP on work of breathing in mechanically ventilated COPD patients. Intensive Care Med 2000, 26: 1207-1214. 10.1007/s001340051339
Tuxen DV: Detrimental effects of positive end-expiratory pressure during controlled mechanical ventilation of patients with severe airflow obstruction. Am Rev Respir Dis 1989, 140: 5-10.
Menitove SM, Goldring RM: Combined ventilator and bicarbonate strategy in the management of status asthmaticus. Am J Med 1983, 74: 898-901. 10.1016/0002-9343(83)91082-3
Rowe BH, Bretzlaff JA, Bourdon C, Bota GW, Camargo CA Jr: Intravenous magnesium sulfate treatment for acute asthma in the emergency department: a systematic review of the literature. Ann Emerg Med 2000, 36: 181-190. 10.1067/mem.2000.105659
Silverman RA, Osborn H, Runge J, Gallagher EJ, Chiang W, Feldman J, Gaeta T, Freeman K, Levin B, Mancherje N, et al.: IV magnesium sulfate in the treatment of acute severe asthma: a multicenter randomized controlled trial. Chest 2002, 122: 489-497. 10.1378/chest.122.2.489
Rooke GA, Choi JH, Bishop M: The effect of isofluorane, halothane, sevoflurane, and thiopental/nitrous oxide on respiratory system resistance after tracheal intubation. Anesthesiol 1997, 86: 1294-1299. 10.1097/00000542-199706000-00010
Maltais F, Sovilj M, Goldberg P, Gottfried SB: Respiratory mechanics in status asthmaticus. Effects of inhalational anesthesia. Chest 1994, 116: 296-300.
Otte RW, Fireman P: Isoflurane anesthesia for the treatment of refractory status asthmaticus. Ann Allergy 1991, 66: 305-309.
Bierman MI, Brown M, Muren O, Keenan RL, Glauser FL: Prolonged isoflurane anesthesia in status asthmaticus. Crit Care Med 1986, 14: 832-833.
Corseen G, Guitierrez J, Reves JG, Huber FC: Ketamine in the anesthetic management of asthmatic patients. Anesth Analg 1972, 51: 588-596.
Sarma V: Use of ketamine in acute severe asthma. Acta Anaesthesiol Scand 1992, 36: 106-107.
Hemmingsen C, Nielsen PK, Odorico J: Ketamine in the treatment of bronchospasm during mechanical ventilation. Am J Emerg Med 1994, 12: 417-420. 10.1016/0735-6757(94)90051-5
Henke CA, Hertz M, Gustafson P: Combined bronchoscopy and mucolytic therapy for patients with severe refractory status asthmaticus on mechanical ventilation: a case report and review of the literature. Crit Care Med 1994, 22: 1880-1883.
Luksza AR, Smith P, Coakley J, Gordan IJ, Atherton ST: Acute severe asthma treated by mechanical ventilation: 10 years' experience from a district general hospital. Thorax 1986, 41: 459-463.
Gluck EH, Onorato DJ, Castriotta R: Helium-oxygen mixtures in intubated patients with status asthmaticus and respiratory acidosis. Chest 1990, 98: 693-698.
Schaeffer EM, Pohlman A, Morgan S, Hall JB: Oxygenation in status asthmaticus improves during ventilation with helium-oxygen. Crit Care Med 1999, 27: 2666-2670. 10.1097/00003246-199912000-00010
Kass JE, Terregino CA: The effect of heliox in acute severe asthma: a randomized controlled trial. Chest 1999, 116: 296-300. 10.1378/chest.116.2.296
Tassaux D, Jolliet P, Roeseler J, Chevrolet JC: Effects of helium-oxygen on intrinsic Positive end-expiratory pressure in intubated and mechanically ventilated patients with severe chronic obstructive pulmonary disease. Crit Care Med 2000, 28: 2721-2728. 10.1097/00003246-200008000-00006
Carter LER, Webb CCR, Moffitt CER: Evaluation of heliox in children hospitalized with acute severe asthma: a randomized crossover trial. Chest 1996, 109: 1256-1261.
Henderson SO, Acharya P, Kilaghbian T, Perez J, Korn CS, Chan LS: Use of heliox-driven nebulizer therapy in the treatment of acute asthma. Ann Emerg Med 1999, 33: 141-146. 10.1016/S0196-0644(99)70386-0
Kukita I, Okamoto K, Sato T, Shibata Y, Taki K, Kurose M, Terasaki H, Kohrogi H, Ando M: Emergency extracorporeal life support for patients with near-fatal status asthmaticus. Am J Emerg Med 1997, 15: 566-569. 10.1016/S0735-6757(97)90158-3
Shapiro MB, Kleaveland AC, Bartlett RH: Extracorporeal life support for status asthmaticus. Chest 1993, 103: 1651-1654.
Corbridge TC, Hall JB: Status asthmaticus. In Principles of Critical Care. Edited by: Hall JB, Schmidt GA, Wood LD. McGraw Hill; 1998:579-595.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Stather, D.R., Stewart, T.E. Clinical review: Mechanical ventilation in severe asthma. Crit Care 9, 581 (2005). https://doi.org/10.1186/cc3733
Published:
DOI: https://doi.org/10.1186/cc3733