Abstract
Background
High quality care for acute myocardial infarction (AMI) improves patient outcomes. Still, AMI patients are treated in hospitals with unequal access to percutaneous coronary intervention. The study compares changes in treatment and 30-day and 3-year mortality of AMI patients hospitalized into tertiary and secondary care hospitals in Estonia in 2001 and 2007.
Results
Final analysis included 423 cases in 2001 (210 from tertiary and 213 from secondary care hospitals) and 687 cases in 2007 (327 from tertiary and 360 from secondary care hospitals). The study sample in 2007 was older and had twice more often diabetes mellitus. The patients in the tertiary care hospitals underwent reperfusion for ST-elevation myocardial infarction, cardiac catheterization and revascularisation up to twice as often in 2007 as in 2001. In the secondary care, patient transfer for further invasive treatment into tertiary care hospitals increased (P < 0.001). Prescription rates of evidence-based medications for in-hospital and for outpatient use were higher in 2007 in both types of hospitals. However, better treatment did not improve significantly the short- and long-term mortality within a hospital type in crude and baseline-adjusted analysis. Still, in 2007 a mortality gap between the two hospital types was observed (P < 0.010).
Conclusions
AMI treatment improved in both types of hospitals, while the improvement was more pronounced in tertiary care. Still, better treatment did not result in a significantly lower mortality. Higher age and cardiovascular risk are posing a challenge for AMI treatment.
Similar content being viewed by others
Background
In the last decade, Estonia has reported one of the highest rates of mortality due to ischemic heart diseases in Europe [1]. At the same time, as in other East European countries, the health care system in Estonia has undergone considerable changes. Lead by the Estonian Society of Cardiology, much effort has been made to improve the quality of care for acute myocardial infarction (AMI) patients through better application of the diagnosis and treatment guidelines [2–7].
One of the main priorities has been to increase access to percutaneous coronary interventions (PCI) and to enable more ST-segment elevation AMI (STEMI) patients receive reperfusion, including primary PCI. According to a recent study, the rates of primary PCI in Estonia are now comparable to those in such Nordic countries as Norway and Denmark [8].
Previous studies have mainly focused on the overall changes in the treatment and mortality of AMI patients [9–14]. Changes in different types of hospitals with unequal availability of coronary intervention facilities have received little attention. Still, such information is crucial in a country with limited health care resources aiming to provide equal care for all AMI patients.
This study aimed to determine the changes in in-hospital treatment and 30-day mortality and 3-year mortality of AMI patients hospitalized into tertiary and secondary care hospitals in Estonia in 2001 and 2007.
Methods
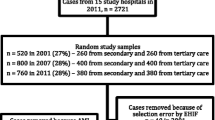
We conducted a retrospective cross-sectional study based on patient records. The formation of the study samples is presented in Figure 1. The list of AMI cases (main diagnosis code I21-I22 according to the International Statistical Classification of Diseases and Related Health Problems 10th revision [15]) hospitalized from January 1 to December 31, 2001 and 2007, was obtained from the database of the Estonian Health Insurance Fund (EHIF). The Estonian health insurance system is a social insurance relying on the principle of solidarity and of the 1.3 million inhabitants about 95% are insured. Consistency in reporting to the EHIF database and the validity of the data has been established [16].
The EHIF applied the following exclusion criteria for case selection: (1) patients who were not first hospitalized into one of the study hospitals; (2) patients who were re-admitted with AMI within 28 days of the first admission; (3) patients whose length of hospital stay was less than 3 days if they were discharged alive and were not transferred to another hospital, which made the diagnosis of AMI unlikely.
In 2001, according to the EHIF database, 2365 AMI cases were hospitalized during the study period in Estonia. Management of AMI patients was shared among 27 Estonian hospitals with a different number of beds. As we aimed to evaluate the management of AMI patients in hospitals that treat the major proportion of annual AMI cases, the study included 9 hospitals: 2 tertiary PCI-capable (only during working hours) and 7 secondary care hospitals. In the secondary care hospitals the number of annual AMI cases ranged from 7 to 165 cases and the tending physicians were mainly anesthesiologists or internists and in some hospitals also cardiologists. After the application of the exclusion criteria by the EHIF, 1955 cases remained, out of which a random sample of 520 cases (27%) was formed. The sampling was performed in clusters according to the hospitals involved.
In 2007, 3251 AMI cases were hospitalized in Estonia. Due to the changes in the hospital network only 20 hospitals admitted AMI patients in 2007. The study included 16 hospitals that treated the major proportion of annual AMI cases: 2 tertiary 24/7 PCI-capable and 14 secondary care hospitals (one hospital had PCI availability during working hours). The tertiary care hospitals were the same in both time periods. In the secondary care hospitals the number of annual AMI cases ranged from 16 to 267 cases and the tending physicians were mainly anesthesiologists or internists and in some hospitals also cardiologists. After the application of the exclusion criteria by the EHIF, 2862 cases remained, out of which a random sample of 800 cases (28%) was formed. The sampling was performed in clusters according to the hospitals involved.
Data collection
Data from medical records were retrospectively abstracted by study experts according to a standardized data collection form. Most of the experts were certified cardiologists and all had received additional training on data collection for this study. Every case was reviewed by one expert. Data quality was monitored by random re-abstractions for determining the causes of discrepancies and followed by retraining of experts. The abstracted data included: (1) patient baseline characteristics; (2) time of symptom onset; (3) cardiac catheterization, revascularization, and non-invasive cardiac testing during index hospitalization; (4) in-hospital and discharge medications; (5) in-hospital mortality. The date of death during 3-year follow-up was obtained from the Estonian Population Register by the EHIF. The study was approved by the Research Ethics Committee of the University of Tartu (reference number 196/T-1).
As we aimed to assess the quality of care of the first hospital where the patient was hospitalized, the data collection stopped when the patients were transferred from a secondary care to a tertiary care hospital.
Statistical analysis
Categorical variables were expressed as frequencies and percentages, and continuous variables as means and standard deviations (SD), or as medians and interquartile ranges (IQR). To compare the patients admitted into the tertiary and secondary care hospitals in 2001 and 2007 in respect to baseline characteristics, in-hospital management and discharge prescription rates of medications, the Chi-Square or the Fisher's exact test for categorical variables and the t-test for two independent samples or the Wilcoxon-Mann-Whitney test for continuous variables were used.
The outcome was expressed as 30-day and 3-year mortality. The crude and baseline-adjusted [age, sex, AMI subtype (STEMI or non-STEMI), diabetes mellitus, arterial hypertension, previous AMI, previous heart failure] hazard ratios (HR) of mortality for patients admitted into the tertiary and secondary care hospitals in 2001 vs 2007 were estimated with Cox's proportional hazards regression. The ratio with the 95% confidence interval (CI) was presented as the ratio of the rate in 2007 to the rate in 2001 in the tertiary or secondary care hospitals.
The experts found that the documentation of smoking status and lipid profiles in medical records was incomplete in 2001 and 2007 (percentage of missing values ranged from 14.5-48.8) and those variables were not further analyzed in the patient characteristics of the results section.
Two-sided P values ≤ 0.05 were considered statistically significant. All analyses were performed using the Stata statistical software version 11.
Results
Out of the random study samples (n = 520 in 2001, n = 800 in 2007), 40 (7.8%) cases in 2001 and 62 (7.8%) cases in 2007 were excluded from the analysis because of selection errors that arose in the forming of the study population by the EHIF (the study sample included cases that were not first hospitalized into one of the study hospitals).
Among the remaining cases, the diagnosis of AMI was confirmed for the following patients: 93.3% in 2001 and 95.3% in 2007 (P = 0.304) in the tertiary care hospitals; 83.5% in 2001 and 91.1% in 2007 (P = 0.003) in the secondary care hospitals. The diagnosis of AMI in both study periods was based on the redefinition document of myocardial infarction published in 2000 [2].
The final study samples included 423 cases in 2001 (210 from the tertiary and 213 from the secondary care hospitals) and 687 cases in 2007 (327 from the tertiary and 360 from the secondary care hospitals).
Patient characteristics
In the study sample of the tertiary care hospitals, the proportion of men, patients with STEMI and diabetes mellitus was higher in 2007 compared to 2001 (Table 1). The patients of the study sample in the secondary care hospitals were considerably older, had more often diabetes mellitus, and hypertension in 2007 compared to 2001.
Management during hospitalization
Prescription rates of evidence-based medications were higher in 2007 in both types of hospitals (Table 2).
The patients of the tertiary care hospitals underwent reperfusion for STEMI, cardiac catheterization and revascularisation up to twice as often in 2007 as in 2001. The reperfusion rates for STEMI did not change significantly in the secondary care hospitals.
Fourteen (6.6%) cases in 2001 and 74 (20.6%) cases in 2007 were transferred from a secondary to a tertiary care hospital for further management (P < 0.001).
Medications for outpatient use
In order to analyze the prescription rates of medications for outpatient use in the tertiary care hospitals, we excluded the patients who died during hospital stay [30 (14.3%) in 2001 and 37 (11.3%) in 2007]. In the secondary care hospitals, we excluded those who died during hospital stay [36 (16.9%) in 2001 and 62 (17.2%) in 2007], or were transferred into tertiary care hospitals [14 (6.6%) in 2001 and 74 (20.6%) in 2007].
The prescription rates of evidence-based medications for outpatient use increased in all studied drug groups in both hospital types in 2007 compared to 2001 (except for aspirin in the secondary care hospitals) (Table 3). At the same time, there was a decrease in the use of nitrates in both types of hospitals.
Mortality
In crude and baseline-adjusted analysis there were no significant differences in the 30-day mortality and 3-year mortality within the two hospital types in 2007 compared to 2001 (Table 4 and Figure 2).
Comparison of mortality between the two hospital types in 2001 showed no significant differences (results not presented). However, in 2007, the 30-day mortality was significantly lower in the tertiary care hospitals than in the secondary care hospitals in crude (HR 0.54; 95% CI 0.36-0.81) and baseline-adjusted analysis (HR 0.61; 95% CI 0.41-0.93). Also after 3 years mortality in the tertiary care hospitals remained lower in crude (HR 0.66; 95% CI 0.51-0.85) and baseline-adjusted analysis (HR 0.73; 95% CI 0.57-0.95).
Discussion
This country-wide study shows that between 2001 and 2007, the treatment of AMI patients improved in the tertiary and secondary care hospitals in Estonia, although the rates of reperfusion and revascularization increased mainly in the tertiary care setting. At the same time, improvements in the treatment did not translate into significantly lower mortality within the hospital types even after accounting of the differences in the baseline characteristics. Instead, in 2007, a marked mortality gap can be observed between the tertiary and the secondary care hospitals.
The positive trend in AMI treatment during hospitalization has also been reported by previous studies [9–14, 17–19]. The observed improvements in Estonia are probably connected to better access to coronary intervention facilities, the release of new European and Estonian guidelines during the study period, and the launching of several training programs by the Estonian Society of Cardiology [3–7].
Still, in 2007, the mean use of beta-blockers and ACEI/ARB during hospitalization and for outpatient use remained below 83%, while the rates in the secondary care hospitals were even lower. The use of statins in the secondary care hospitals causes even more concern as although the rates increased markedly during the study period, their use is still below 38%. The fact that the quality of care of AMI patients in the secondary care hospitals lags behind that in their tertiary care counterparts may be due to the known slower implementation of guideline-recommended medications in secondary care hospitals [20]. As the study demonstrated, patients in the secondary care hospitals tend to be older and have more co-morbidities, which may influence management decisions.
Better access to invasive coronary care facilities and recent research findings contributed to the wider use of PCI in the tertiary care hospitals. At the same time, in the secondary care hospitals transfer for further cardiac testing and revascularisation into tertiary care hospitals increased. Still, the transfer rates were low compared to previous studies [21, 22]. Although the mean age of transferred patients increased, transferred patients still tended to be younger than the non-transferred patients (data not presented).
While in the tertiary care hospitals reperfusion rates increased and primary PCI became the preferred method of reperfusion for STEMI patients, then in the secondary care hospitals reperfusion rates showed little change. It is possible that STEMI patients are usually transferred before receiving medical reperfusion. Still, a previous study revealed that the reasons for not receiving reperfusion may be unknown in up to 45% of cases [23].
Several studies have demonstrated that closer adherence to published guidelines for AMI management results in improved short-and long-term outcomes and this even despite the growing prevalence of risk factors (older age, history of hyperlipidaemia and diabetes mellitus) at presentation [10–14, 16, 24–26]. Although our study demonstrates a marked improvement in the treatment quality for AMI patients in 2007 compared to 2001, especially in tertiary care hospitals, it fails to show a significant decrease in 30-day and 3-year mortality. As the study sample of the secondary care hospitals demonstrated, this may largely be due to the higher age and cardiovascular risk among the study samples in 2007. For instance, the rates of diabetes had almost doubled in both types of hospitals. In order to further clarify this issue, we performed a sub-analysis to compare the baseline characteristics, quality of care provided, and mortality separately among patients < 75 and ≥ 75 years in 2001 and 2007 in tertiary care hospitals (data not presented). On the basis of this analysis we may hypothesize that in tertiary care hospitals the reason why short-and long-term mortality has not improved despite better overall quality of care is that firstly the improvement is more targeting those younger and healthier and secondly the rate of patients over 75 years with more co-morbidities has increased.
Interesting findings of the study were the differences in short and long-term mortality between the two hospital types in 2007. This can probably be explained by a combined effect of improved management possibilities in the tertiary care hospitals and different patient baseline characteristics in the two hospital types. The patients admitted to the secondary care hospitals are more likely to be older and have a higher cardiovascular risk. Moreover, as the elderly often present with atypical symptoms and have a greater burden of cardiac and non-cardiac co-morbidities, physicians are more reluctant to treat them aggressively, the more so when the outcomes of interventions and surgery may be poorer [27, 28].
Limitations
Firstly, this study includes only random study samples which may not represent the true patient populations. As a consequence, the practice patterns observed in the present study may not be representative of the general AMI patient population. Secondly, the sample of 2007 included patients from seven secondary care hospitals that were not included in 2001 (accounting for 25% of the cases from the secondary care hospitals). This corresponds to the study principle of including hospitals that treat the major proportion of annual AMI cases. Limiting the analysis to only those secondary care hospitals that participated both in 2001 and 2007 produced similar treatment and mortality results (data not presented). Thirdly, the study did not capture information on co-morbid conditions such as chronic kidney disease and cancer, which may have precluded the use of certain pharmacologic and interventional treatments. Fourthly, owing to the study design, we were not fully able to collect information on smoking and lipid profiles and hence we could not account for these variables in mortality analysis.
Conclusions
In Estonia, both types of hospitals underwent considerable improvement in AMI treatment between 2001 and 2007. Still, changes were more pronounced in the tertiary care setting, especially with respect to the use of reperfusion and revascularisation. Low rates of reperfusion and transfer for PCI clearly need to be addressed in the secondary care hospitals. The improvement in treatment did not result in a significant change in short-and long-term mortality in either hospital type. Higher age and cardiovascular risk are posing a challenge for AMI management.
In addition to addressing the gaps in the quality of AMI treatment across Estonian hospitals, there is a need for high-quality data from a prospective nationwide acute myocardial infarction register for continuous follow-up of AMI treatment and outcomes.
Authors' information
MB, TA, TM, and JE are the members of the working group of Acute Coronary Syndromes of the Estonian Society of Cardiology as well as the members of the Scientific Board of the Estonian Myocardial Infarction Registry.
References
European Statistical Office. [http://epp.eurostat.ec.europa.eu/portal/page/portal/health/public_health]
Alpert JS, Thygesen K, Antman E, Bassand JP: Myocardial infarction redefined--a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000, 36: 959-969. 10.1016/S0735-1097(00)00804-4.
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, Ornato JP: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004, 44: E1-E211. 10.1016/j.jacc.2004.07.014.
Bertrand ME, Simoons ML, Fox KA, Wallentin LC, Hamm CW, McFadden E, De Feyter PJ, Specchia G, Ruzyllo W: Management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2004, 23: 1809-1840.
Braunwald E, Antman EM, Beasley JW, Califf RM, Cheitlin MD, Hochman JS, Jones RH, Kereiakes D, Kupersmith J, Levin TN, Pepine CJ, Schaeffer JW, Smith EE, Steward DE, Theroux P, Gibbons RJ, Alpert JS, Faxon DP, Fuster V, Gregoratos G, Hiratzka LF, Jacobs AK, Smith SC: ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction-summary article: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients with Unstable Angina). J Am Coll Cardiol. 2002, 40: 1366-1374. 10.1016/S0735-1097(02)02336-7.
Van de Werf F, Bax J, Betriu A, Blomstrom-Lundqvist C, Crea F, Falk V, Filippatos G, Fox K, Huber K, Kastrati A, Rosengren A, Steg PG, Tubaro M, Verheugt F, Weidinger F, Weis M: Management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2003, 24: 28-66.
Soopold U, Marandi T, Ainla T, Liiver A, Elmet M, Laanoja J, Peeba M, Ristimae T: Estonian guidelines for the management of patients with ST-elevation myocardial infarction. Eesti Arst. 2004, 2: (Suppl 1):2-48 (in Estonian).
Widimsky P, Wijns W, Fajadet J, de Belder M, Knot J, Aaberge L, Andrikopoulos G, Baz JA, Betriu A, Claeys M, Danchin N, Djambazov S, Erne P, Hartikainen J, Huber K, Kala P, Klinceva M, Kristensen SD, Ludman P, Ferre JM, Merkely B, Milicic D, Morais J, Noc M, Opolski G, Ostojic M, Radovanovic D, De Servi S, Stenestrand U, Studencan M, Tubaro M, Vasiljevic Z, Weidinger F, Witkowski A, Zeymer U: Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J. 2010, 31: 943-957. 10.1093/eurheartj/ehp492.
Goodman SG, Huang W, Yan AT, Budaj A, Kennelly BM, Gore JM, Fox KA, Goldberg RJ, Anderson FA: The expanded Global Registry of Acute Coronary Events: baseline characteristics, management practices, and hospital outcomes of patients with acute coronary syndromes. Am Heart J. 2009, 158: 193-201. 10.1016/j.ahj.2009.06.003.
Peterson ED, Shah BR, Parsons L, Pollack CV, French WJ, Canto JG, Gibson CM, Rogers WJ: Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008, 156: 1045-1055. 10.1016/j.ahj.2008.07.028.
Mandelzweig L, Battler A, Boyko V, Bueno H, Danchin N, Filippatos G, Gitt A, Hasdai D, Hasin Y, Marrugat J, Van de Werf F, Wallentin L, Behar S: The second Euro Heart Survey on acute coronary syndromes: characteristics, treatment, and outcome of patients with ACS in Europe and the Mediterranean Basin in 2004. Eur Heart J. 2006, 27: 2285-2293. 10.1093/eurheartj/ehl196.
Stolt Steiger V, Goy JJ, Stauffer JC, Radovanovic D, Duvoisin N, Urban P, Bertel O, Erne P: Significant decrease in in-hospital mortality and major adverse cardiac events in Swiss STEMI patients between 2000 and December 2007. Swiss Med Wkly. 2009, 139: 453-457.
Janion M, Polewczyk A, Gasior M, Polonski L: Progress in the management of ST-segment elevation myocardial infarction during economic transition in Poland between 1992 and 2006. Int J Cardiol. 2009, 135: 263-265. 10.1016/j.ijcard.2008.03.059.
Monhart Z, Grunfeldova H, Jansky P, Zvarova J, Faltus V: Pilot register of acute myocardial infarction--a 5-year evaluation of quality of care in non-PCI hospitals. Vnitr Lek. 2010, 56: 21-29 (in Czech).
World Health Organization: International Statistical Classification of Diseases and Related Health Problems. 2004, Geneva: World Health Organization, revision, 10
Comparative analysis of morbidity information on the basis of annual statistical reports and the database of Estonian Health Insurance Fund. [http://ee.euro.who.int/Haigestumusinfo_vordlus%20SoM_HK.pdf]
Gibson CM, Pride YB, Frederick PD, Pollack CV, Canto JG, Tiefenbrunn AJ, Weaver WD, Lambrew CT, French WJ, Peterson ED, Rogers WJ: Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008, 156: 1035-1044. 10.1016/j.ahj.2008.07.029.
Fang J, Alderman MH, Keenan NL, Ayala C: Acute myocardial infarction hospitalization in the United States, 1979 to 2005. Am J Medicine. 2010, 123: 259-266. 10.1016/j.amjmed.2009.08.018.
Tatu-Chitoiu G, Cinteza M, Dorobantu M, Udeanu M, Manfrini O, Pizzi C, Vintila M, Ionescu DD, Craiu E, Burghina D, Bugiardini R: In-hospital case fatality rates for acute myocardial infarction in Romania. CMAJ. 2009, 180: 1207-1213. 10.1503/cmaj.081227.
Dorsch MF, Lawrance RA, Sapsford RJ, Durham N, Das R, Jackson BM, Morrell C, Ball SG, Robinson MB, Hall AS: An evaluation of the relationship between specialist training in cardiology and implementation of evidence-based care of patients following acute myocardial infarction. Int J Cardiol. 2004, 96: 335-340. 10.1016/j.ijcard.2003.05.038.
Labarere J, Belle L, Fourny M, Genes N, Lablanche JM, Blanchard D, Cambou JP, Danchin N: Outcomes of myocardial infarction in hospitals with percutaneous coronary intervention facilities. Arch Intern Med. 2007, 167: 913-920. 10.1001/archinte.167.9.913.
Radovanovic D, Urban P, Simon R, Schmidli M, Maggiorini M, Rickli H, Stauffer JC, Seifert B, Gutzwiller F, Erne P: Outcome of patients with acute coronary syndrome in hospitals of different sizes. A report from the AMIS Plus Registry. Swiss Med Wkly. 2010, 140: 314-322.
Blondal M, Ainla T, Marandi T, Baburin A, Rahu M, Eha J: Better outcomes for acute myocardial infarction patients first admitted to PCI hospitals in Estonia. Acta Cardiol. 2010, 65: 541-548.
Fox KA, Steg PG, Eagle KA, Goodman SG, Anderson FA, Granger CB, Budaj A, Quill A, Gore JM: Decline in rates of death and heart failure in acute coronary syndromes, 1999-2006. JAMA. 2007, 297: 1892-1900. 10.1001/jama.297.17.1892.
Krumholz HM, Wang Y, Chen J, Drye EE, Spertus JA, Ross JS, Curtis JP, Nallamothu BK, Lichtman JH, Havranek EP, Masoudi FA, Radford MJ, Han LF, Rapp MT, Straube BM, Normand SL: Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995-2006. JAMA. 2009, 302: 767-773. 10.1001/jama.2009.1178.
Rogers WJ, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, Pollack CV, Gore JM, Chandra-Strobos N, Peterson ED, French WJ: Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008, 156: 1026-1034. 10.1016/j.ahj.2008.07.030.
Alexander KP, Roe MT, Chen AY, Lytle BL, Pollack CV, Foody JM, Boden WE, Smith SC, Gibler WB, Ohman EM, Peterson ED: Evolution in cardiovascular care for elderly patients with non-ST-segment elevation acute coronary syndromes: results from the CRUSADE National Quality Improvement Initiative. J Am Coll Cardiol. 2005, 46: 1479-1487. 10.1016/j.jacc.2005.05.084.
Bridges CR, Edwards FH, Peterson ED, Coombs LP, Ferguson TB: Cardiac surgery in nonagenarians and centenarians. J Am Coll Surg. 2003, 197: 347-356, discussion 356-357. 10.1016/S1072-7515(03)00384-3.
Acknowledgements
We thank the Estonian Health Insurance Fund for supplying the list of hospitalized AMI cases and data on follow-up. We also thank the experts who participated in abstraction of the data form medical records.
The research of MB, TA, TM, JE was supported by the Estonian Ministry of Education and Research (target funding SF0180001s07) and by the grant of the Estonian Science Foundation (No ETF8903 and ETF8273). The research of AB was supported by the Estonian Ministry of Education and Research (target funding SF0940026s07).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MB, TA, TM, AB, and JE participated in the design of the study and in writing the manuscript. MB and AB performed the statistical analysis. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Blöndal, M., Ainla, T., Marandi, T. et al. Changes in treatment and mortality of acute myocardial infarction in Estonian tertiary and secondary care hospitals in 2001 and 2007. BMC Res Notes 5, 71 (2012). https://doi.org/10.1186/1756-0500-5-71
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-0500-5-71