Abstract
Background
The purpose of this study was to evaluate the flexion-gap of the native knees in the normal population and to assess any gender-specific variations in the flexion gap of the knees.
Methods
A total of 50 normal asymptomatic volunteers with normal knee radiographs were selected for MRI of the knee. The left knee was scanned in an open MRI using a T1-weighted sequence. Imaging was performed in neutral, passive varus and valgus stress at 90° of knee flexion by placing custom-made blocks on a special board consecutively below the distal part of the leg.
Results
The study population consisted of 26 males and 24 females with a mean age of 25.77 years. Under varus stress, the mean lateral flexion gap increased to 9.28 ± 1.53 mm and under valgus stress, the mean medial flexion gap increased to 2.75 ± 1.22 mm from neutral. The increase in the flexion gap on the lateral side was 5.28 ± 1.79 mm, which was significantly higher compared to that on the medial side. In gender-specific analysis, the mean lateral flexion gap was 10.21 mm in females and 8.46 mm in males under varus stress.
Conclusion
The findings of the study indicate that the lateral soft tissues are more lax compared to the medial soft tissue structures and this laxity is higher in females as compared to males. The study provides evidence of the existing physiological variations of these soft tissue structures resulting in a trapezoidal flexion gap in the native knees rather than the recommended rectangular gap.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) has established itself as the treatment of choice for the degenerative diseases of the knee joint. The success of TKA is attributed to the restoration of the normal femorotibial mechanical axis. The collateral soft tissue balance has been implicated as an important factor affecting the weight-bearing alignment of the knee [1]. A high percentage of failures of TKA is attributed to improper alignment and soft tissue balancing. It is now accepted as a principle to have a well-balanced knee from 90° flexion to full extension [2]. The designs of the modern prostheses rely on creating such balanced and symmetrical flexion–extension gaps for deciding the thickness of the component [2,3,4]. The goal is to restore the alignment and soft-tissue balance to prevent undue stress on the components. However, recently there have been few reports suggesting that the shape of the flexion gap may be affected by the normal laxity of the ligaments creating an asymmetry [5, 6]. In the long-term, the effect of cyclical loading of the prosthesis in such knees might affect the durability of the prosthetic components and hence the overall outcomes in TKA.
In view of the emerging evidence, we asked the following questions:
-
1.
What is the normal flexion-gap of the knees in the normal Indian population?
-
2.
Does gender have any effect on the flexion gap in the population?
We obtained magnetic resonance imaging (MRI) imaging data, a readily accessible imaging tool, for assessing joint characteristics and quantified the anatomical variation in the medial and lateral joint opening under valgus or varus stresses at 90° of flexion.
Materials and Methods
Fifty normal asymptomatic volunteers with normal knee radiographs without any previous history of a knee injury, surgery, symptomatic knees, any malalignment problems, or ligamentous laxity were included for the study after informed consent. The study was approved by the Institutional Ethical Committee. To maintain uniformity only the left knee was chosen for MRI. The left knee was scanned in an open MRI (GE, 0.2 T) using a T1-weighted sequence (THR, TE, and the flip angle) using a neck coil around the knee joint. Consecutive coronal sections of 3.5 mm thickness were obtained across the knee joint. Imaging was performed in neutral, passive varus, and valgus stress at 90° of knee flexion.
A special board was fabricated on which the subjects were positioned for the imaging. It had the provision to strap the patient around the pelvis and thigh to prevent the change in position while imaging the knee. The varus or valgus stress was applied to the knee by placing custom-made blocks consecutively under the distal part of the leg just above the level of malleolus with a soft cushion on the top to prevent discomfort (Fig. 1). The method to apply the varus and valgus stress was demonstrated to the subjects before positioning them on the board to avoid any discomfort during the study.
Initially, for the neutral position, the subject was made to lie in the left lateral position (Fig. 2a). Later, for the varus and valgus stress, the subject was made to lie supine with unilateral cross-leg (Fig. 2b) or reverse cross-leg position (Fig. 2c), respectively. Most of the subjects found it difficult to lie in a complete unilateral reverse cross-leg position. However, they were able to lie down by turning 10–15° to the right. Once the patient was adequately positioned in each of these positions, the neck coil was passed over the knee and the knee was flexed to 90° as measured with a goniometer centered over the joint line. During stress testing, the custom-blocks were kept incrementally as described earlier until the patient felt stress at the knee and the imaging was done in this position.
After securing the position of the subject, a localizer run of around 42 s was used for getting the sagittal view from which the flexion angle was assessed. Later, standard slides showing intercondylar tibial eminence was obtained for every subject. For valgus position localizer was run twice to avoid conflict due to rotational malposition for getting the standard slides. After the final run of the MRI series, lasting for 4 min 8 s, primary screening was done to assess the quality of the acquired images, and if found satisfactory imaging was performed in other positions.
Method of Measurement
A special image analysis software—“Image J” from NIH was used for marking and assessing the slides. The slide which had the section of the lateral and medial epicondyles of the femur and /or longitudinal axis of the tibia was selected. Among the 150 image sequences obtained, 55 slides had the epicondyles and longitudinal axis of the tibia on the same slide. In the remaining 95 image slides, the epicondyles and the longitudinal axis of the tibia were in different slides. In such cases, two different slides were used and the mean of the two slides was taken.
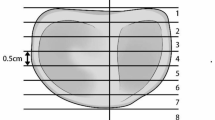
The shape and width of the flexion gap were assessed, based on four reference lines (2, 3, 4, and 5) and two points ‘P’ and ‘Q’ (Fig. 3). A pixel to millimeter-scale was set from the millimeter scale given in the slide before marking various lines.
Line 1 was defined as the longitudinal axis of the tibia, which was determined by connecting the midpoint of the width of tibial diaphysis at two levels. For sake of uniformity, the two levels for measuring the width were taken approximately 50 mm and 75 mm from the tibial intercondylar eminence. In slides with insufficient length of the tibia for marking these points, a minimum gap of 25 mm was maintained between the two points.
Line 2 was defined as the tibial osteotomy axis which was perpendicular to the longitudinal axis of tibia (Line 1). While marking the perpendicular line it was not always possible to get it exactly at 90°. In such cases, the marking was drawn to the nearest possible angle with a difference of less than 1°. However, while assessing the data, the tibial osteotomy axis was considered as perpendicular to the tibial longitudinal axis.
Line 3 was defined as the epicondylar axis connecting the lateral epicondylar prominence either to the medial sulcus (surgical epicondylar axis, SEA) or to the medial prominence (clinical epicondylar axis, CEA).
Line 4 was defined as the tibial articular axis which connected the proximal margins of the lateral and medial articular surfaces of the tibia.
Line 5 was made by connecting the posterior margins of the lateral and the medial femoral condyles.
The width of the medial and lateral joint gap was measured after marking points ‘P’ and ‘Q’ on medial and lateral femoral condyles respectively (marked at maximum convexity) and calculating the distance of point ‘P’ and ‘Q’ from line 4 i.e. tibial articular axis. The shape of the flexion gap in neutral and under varus and valgus stress was assessed by analyzing the angle between line 2 and line 3. This corresponds to the configuration of the flexion gap during the bone resection in the proximal tibia and posterior femoral condyles during the TKA. The angle between line 4 and line 5 was also determined as this represented the physiological separation of the tibiofemoral articular surfaces. The flexion angle was measured through sagittal images during the localizer series.
Statistical Analysis
The data was compiled and statistical analysis was done. The continuous variables were represented by the mean, median and standard deviation (SD). The independent sample t-test and Mann–Whitney U-test were used to analyze independent quantitative data and the difference between the groups. The results were considered statistically significant if the p-value was less than 0.05 (p < 0.05). All statistical analyses were performed using SPSS v22.0 for Windows (SPSS Inc., IL, USA).
Results
The study population consisted of 26 males and 24 females. The mean age of the participants was 25.77 ± 4.18 years and that of males and females was 25.81 ± 4.69 years and 25.71 ± 3.69 years respectively.
When no stress was applied, the lateral and medial femoral condyles were in contact with the tibial articular surface more on the medial side with a mean medial joint gap of 0.99 ± 0.57 mm (0–2.2 mm) and a lateral joint gap of 2.20 ± 0.89 mm (1.3–5.3 mm). The mean flexion angle was 87.7 ± 3.8° (82.3° to 95.8°) (Fig. 4a).
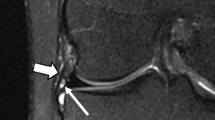
When varus stress was applied, the mean lateral flexion gap increased to 9.28 ± 1.53 mm (6.46 mm to 11.6 mm) and the medial tibial and femoral joint surfaces were in contact obliterating the medial joint gap (Fig. 4b). The effective increase in the lateral flexion gap from the neutral stress position was 7.05 ± 1.88 mm. The mean flexion angle was 88.2 ± 6.3° (76.3° to 98.8°).
On applying the valgus stress, the mean medial flexion gap increased to 2.75 ± 1.22 mm (0.82–5.86) and the lateral tibial and femoral joint surfaces were in contact with a mean flexion angle of 87.2 ± 4.1° (79.2–92.6) (Fig. 4c). The effective change in the mean medial flexion gap from the neutral stress position was 1.76 ± 0.99 mm. The increase in the flexion gap on the lateral side was 5.28 ± 1.79 mm, which was significantly higher compared to that on the medial side (p < 0.001) (Fig. 5).
In the gender-specific analysis, we found that the collateral ligament laxity was variable among individuals, and ligaments laxity was more in females than males. The mean medial flexion gap when under no stress in females was 0.92 ± 0.54 mm (0 to 2.1) and that in men was 1.05 ± 0.60 mm (0–2.2 mm) and the mean lateral flexion gap was 2.25 ± 0.81 mm in females and 2.22 ± 0.97 mm (1.3–5.3 mm) in males. Under varus stress, the mean lateral flexion gap was 10.21 ± 1.14 mm (7.59–11.60 mm) in women and 8.46 ± 1.36 mm (6.46 m to 10.69 mm) in men (Fig. 6). Whereas under the valgus stress the mean medial joint gap was 2.93 ± 1.38 mm (1.2 mm to 5.86 mm) in females and 2.60 ± 1.08 mm (0.82–4.6 mm) in males. The change in the lateral flexion gap was significantly larger in females compared to males (p-value = 0.02).
On paired angle measurements for flexion gap between line 2 and line 3 under varus stress, the mean angle was 10.18 ± 2.12° (5.2° to 14.2°) and that under valgus stress was 0.88 ± 2.88° (− 5.8° to 4.6°). The mean asymmetry between lines 2 and 3 was 9.24 ± 3.84°. When the paired angles were measured between the line 4 and 5, the mean asymmetry was calculated to be 12.18 ± 2.95° with the angles measuring 1.24 ± 0.96° (− 0.15° to 3.10°) in neutral and 8.86 ± 2.80° (3.5° to 13.6°) and − 3.31 ± 1.16° (− 4.60 to − 0.08) under varus and valgus stress respectively (Table 1).
Discussion
The knee joint is an inherently unstable joint and the remarkable stability is a function of the soft tissues around the knee [2]. The soft tissues on the medial and lateral aspects of the knee joint play a significant role in the biomechanics of the knee. They maintain the tibiofemoral alignment, an important factor determining the distribution of the load on the two tibial plateaus. It is thus considered imperative to achieve a balanced knee during a total knee replacement. Traditionally, a neutral alignment with a rectangular gap in flexion and extension has been recommended as ideal to achieve an optimum balancing of the soft tissues and maximize the survival of the implant [7].
The recommendations for the rectangular flexion gap ignore some of the intrinsic factors. The concepts have been described for an unloaded knee, which has different biomechanics than a loaded knee. Since the soft tissues around the knee are dynamic structures, the rectangular gap in flexion and extension might be affected by the loading of the knee, which might not be apparent during surgery. Recently, several clinical and anatomical studies have shown that there is a difference in the laxity of the medial and the lateral soft tissues resulting in the differential opening of the joint under varus and valgus stress [5, 6, 8, 9]. Physiologically, the lateral collateral ligament is laxer compared to the opposite side. This enables the knee joint to pivot over the medial condyle around which axial tibiofemoral rotation, the ‘screw-home mechanism’, occurs [2, 10]. Additionally, as suggested by Thomine et al. [11] the coronal alignment might be affected by several individual-specific factors like the extrinsic varus offset of the knee, based on the weight and pelvic width of an individual.
In the present study, the lateral flexion gap was measured to be 2.2 mm when no stress was applied, which was higher compared to the medial flexion gap of 0.99 mm, indicating a greater residual laxity of the ligaments on the lateral side compared to the medial side. Under the varus and valgus stress, this difference became much more pronounced with a mean change of 5.31 ± 1.79 mm more on the lateral side compared to the medial side. The asymmetry between the medial and lateral side was found to be 9.24 ± 3.84°. Previously, Jae Chul Yoo et al. [12] tried to quantify the difference between the medial and lateral joint gaps with a custom-made device by applying a manual varus and valgus stress at 20° of flexion. There was a positive difference of 4.5 mm in the lateral joint opening compared to the medial side. Okazaki et al. [9] had studied the effects of varus and valgus loading of the knee on plain radiographs. The mean angle in varus and valgus stress was 4.8° and 1.7° respectively, corroborating our findings. However, radiographs do not accurately represent the change in the joint space, as they are affected by changes in the thickness of articular cartilage which is not well demonstrated on X-ray film.
The magnetic resonance imaging has the benefit of delineating the articular cartilage as well, thus providing accurate measurements of the true changes in the joint space. In studies done by Tokuhara and his colleagues, the flexion gap was measured with both MRI [6] and radiography [5]. In the MRI study, the authors had used the weight of the individual’s leg to apply a varus and valgus force after flexion of the knee to 90° and a difference of 4.6 mm between the two sides and a tilt of 5° was noted. In the radiographic analysis, the authors had loaded the knee joint in a sitting position by applying a weight of 1.5 kg to the ankle with legs hanging by the table. The authors had reported an asymmetry in the flexion gap by 5.1° between the two sides. The results had a strong correlation with those obtained by MRI. In our study, a custom-made board which blocked pelvic rotation, and obtained maximum physiological passive varus-valgus stress by using height blocks were used which was not the case in the previous study. Also, while assessing and marking the tibial axis we standardized the points (50–75 mm from tibial eminence) which acted as a reference for the tibial axis. While assessing slides the neutral position was not taken as reference (0° for lines 4 and 5) as done by a previous study showing the physiological space occupied by normal cartilage tissue and some knees having more lateral space in a neutral position. Recently, Kamal Deep [8] attempted to quantify the laxity using a computer navigation system and a varus and valgus stress of 10-Nm in 0° and 15° of flexion, which corroborated with our findings.
There was also a significant difference between the genders in the laxity of the ligaments. The lateral joint gap of 10.21 ± 1.14 mm in women was significantly higher compared to the 8.52 ± 1.31 mm in males (p < 0.001). A similar observation was reported by Jae Chul Yoo et al. [12] who had reported a mean lateral joint opening of 7.2° in females compared to 5.9° in males, indicating a higher laxity in females.
In addition to these findings, it is imperative to understand that squatting and sitting cross-legged are two functions unique to the Asian, Middle Eastern, Japanese, and South Asian populations for a variety of social & religious needs and habits. It is also observed that these functions and a greater range of flexion have been achieved postoperatively more in this population group than in the Caucasian group [13, 14]. Whether this due to some racial variations in tissue properties or because these activities are incorporated into Activities of Daily Living (ADL) right from the beginning is open to debate and discussion.
The findings in the present study demonstrate lateral stress accommodated under loading to the tune of 5–6 mm. This physiologic laxity is probably exploited by individuals who can effortlessly do these maneuvers without a tinge of pain or discomfort within the limits of physiological tolerance. These functions of deep bend, squatting and sitting cross-legged do accentuate the forces on the lateral joint structures. The surface geometry of most modern designs of the prosthesis in use does not resemble the native geometry of the cartilage surface, though in the recent past attempts are being made to replicate these and enable a medial pivot mechanics. Kinematic studies show only 65% of the PS designs demonstrate a medial pivot [15,16,17]. The emphasis is always on a balanced symmetrical flexion gap. Theoretically, in this scenario, the functions of deep squat or cross-legged sitting would place abnormal load and tension on the lateral supporting structures. This probably explains the discomfort experienced by the subjects while performing these acts.
Given these findings and the available evidence in the literature, it is thus evident that the flexion gap is trapezoidal and not rectangular. Thus, the notion of maintaining a rectangular flexion gap during a total knee replacement may need a careful reconsideration. The effect of such an asymmetrical flexion gap on the longevity of the implant is not yet adequately studied. McEwen et al. [18] tried to address the problem by performing kinematic total knee arthroplasty (KTKA) where the asymmetrical balance of the normal knee was considered for component placement instead of the traditional rectangular gap. There were significantly better outcomes in the patient-reported outcomes measures (PROMs) with the lateral ligament laxity. Conversely, Azukinawa et al. [19] had reported that an intraoperative medial flexion gap of ≥ 4 mm at 90° flexion negatively affected the functional outcome. Hungerford and Krackow [20] even recommended to position the tibial component in slight varus to make the joint line oblique, so that the increased valgus at the femoral component was compensated to make the joint line parallel to ground. It is also known that an unbalanced load distribution between the two tibial plateaus affects the wear characteristics of the implant. Studies have shown that a knee with more than 5° of malalignment leads to loss of implant thickness at the rate of 0.11 mm per year [21].
The attempts to restore the joint line, preserving the soft tissue structures, the placement of the components, and many such factors are all attempts at restoring the tissue and ligament isometry during the surgery with which one hopes to stay within the zone of homeostasis so that painless comfortable range of a function is maximized without undue loading of the joint structures. Hence, it cannot be overemphasized that there is a need for further evaluating the effect of the physiological asymmetric flexion gap on the biomechanics of the post-TKA knee and wear characteristics of the implant. It is thus essential to revisit the previous concepts with a fresh perspective for the Indian population considering the unique needs and lifestyle of the region.
Some of the limitations of the present study included the inability to quantify the amount of varus and valgus stress applied, which may vary between individuals depending on the pain tolerance and the inherent laxity of the ligaments. It was not always possible to obtain the soft tissue images in the same scanning plane in the three positions to accurately identify the anatomical points for measurements.
Conclusion
The success of TKR remains in restoring the mechanical alignment ensuring near-physiological loading of the surfaces resembling the normal joint. The soft tissue structures around the knee joint play a vital role in providing a painless functional knee to the patients. The study provides evidence of the existing physiological variations of these soft tissue structures. With an increasing number of Indians undergoing knee replacement surgeries accompanied by varied lifestyle needs, the role of the lateral ligamentous laxity in implant biomechanics, and subsequent failed TKR may need to be assessed more thoroughly.
Data availability
The manuscript data can be made available on request.
References
Willcox, N. M. J., Clarke, J. V., Smith, B. R. K., Deakin, A. H., & Deep, K. (2012). A comparison of radiological and computer navigation measurements of lower limb coronal alignment before and after total knee replacement. The Journal of Bone and Joint Surgery Series B, 94, 1234–1240. https://doi.org/10.1302/0301-620X.94B9.28250
Scott, W. N. (2017). Insall & Scott surgery of the knee. (6th ed.). Churchill Livingstone/Elsevier.
Scuderi, G., & Insall, J. (1989). The posterior stabilized knee prosthesis. Orthopedic Clinics of North America, 20, 71–78
Beverland D. E. (2009). Soft-tissue balance in total knee arthroplasty. In European instructional lectures. Springer Berlin Heidelberg. pp. 213–8.
Tokuhara, Y., Kadoya, Y., Kanekasu, K., Kondo, M., Kobayashi, A., & Takaoka, K. (2006). Evaluation of the flexion gap by axial radiography of the distal femur. The Journal of Bone and Joint Surgery Series B, 88, 1327–1330. https://doi.org/10.1302/0301-620X.88B1017793
Tokuhara, Y., Kadoya, Y., Nakagawa, S., Kobayashi, A., Takaoka, K., & Surgeon, O. (2004). The flexion gap in normal knees AN MRI STUDY. The Journal of Bone and Joint Surgery [British Volume], 86, 1133–1139. https://doi.org/10.1302/0301-620X.86B8
Matsuda, S., & Ito, H. (2015). Ligament balancing in total knee arthroplasty—Medial stabilizing technique. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, 2, 108–113. https://doi.org/10.1016/j.asmart.2015.07.002
Deep, K. (2014). Collateral ligament laxity in knees: what is normal? Clinical Orthopaedics and Related Research, 472, 3426–3431. https://doi.org/10.1007/s11999-014-3865-6
Okazaki, K., Miura, H., Matsuda, S., Takeuchi, N., Mawatari, T., Hashizume, M., et al. (2006). Asymmetry of mediolateral laxity of the normal knee. Journal of Orthopaedic Science, 11, 264–266. https://doi.org/10.1007/s00776-006-1009-x
Rajendran, K. (1985). Mechanism of locking at the knee joint. Journal of Anatomy, 143, 189–194
Thomine, J. M., Boudjemaa, A., Gibon, Y., & Biga, N. (1981). Varizing axial distances in osteoarthrosis of the knee (author’s transl). Revue de Chirurgie Orthopedique et Reparatrice de l’Appareil Moteur, 67, 319–327
Yoo, J. C., Ahn, J. H., Sung, K. S., Wang, J. H., Lee, S. H., Bae, S. W., et al. (2006). Measurement and comparison of the difference in normal medial and lateral knee joint opening. Knee Surgery, Sport Traumatology, Arthroscopy, 14, 1238–1244. https://doi.org/10.1007/s00167-006-0095-9
Ahlberg, A., Moussa, M., & Al-Nahdi, M. (1988). On geographical variations in the normal range of joint motion. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-198809000-00040
Mulholland, S. J., & Wyss, U. P. (2001). Activities of daily living in non-Western cultures: Range of motion requirements for hip and knee joint implants. International Journal of Rehabilitation Research, 24, 191–198. https://doi.org/10.1097/00004356-200109000-00004
Dennis, D. A., Komistek, R. D., Walker, S. A., Cheal, E. J., & Stiehl, J. B. (2001). Femoral condylar lift-off in vivo in total knee arthroplasty. The Journal of Bone and Joint Surgery. British Volume, 83, 33
Dennis, D. A., Komistek, R. D., Mahfouz, M. R., Haas, B. D., & Stiehl, J. B. (2003). Multicenter determination of in vivo kinematics after total knee arthroplasty. Clinical Orthopaedics & Related Research, 416, 37–57. https://doi.org/10.1097/01.blo.0000092986.12414.b5
Dennis, D. A., Komistek, R. D., Stiehl, J. B., Walker, S. A., & Dennis, K. N. (1998). Range of motion after total knee arthroplasty: The effect of implant design and weight-bearing conditions. Journal of Arthroplasty, 13, 748–752. https://doi.org/10.1016/S0883-5403(98)90025-0
McEwen, P., Balendra, G., & Doma, K. (2019). Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. The Bone & Joint Journal, 101, 331–339. https://doi.org/10.1302/0301-620X.101B3.BJJ-2018-0544.R1
Azukizawa, M., Kuriyama, S., Nakamura, S., Nishitani, K., Lyman, S., Morita, Y., et al. (2018). Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery, 138, 1143–1150. https://doi.org/10.1007/s00402-018-2965-2
Hungerford, D. S., & Krackow, K. A. (1985). Total joint arthroplasty of the knee. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-198501000-00004
Massin, P. (2017). How does total knee replacement technique influence polyethylene wear? Orthopaedics & Traumatology, Surgery & Research, 103, S21–S27. https://doi.org/10.1016/j.otsr.2016.06.024
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SKP: manuscript preparation, manuscript editing; MS: data collection, subject allocation, manuscript preparation; AAS: supervision, manuscript editing, statistical analysis; PT: manuscript editing, statistical analysis, data collection; RKG: manuscript editing, data collection; RA: data collection and analysis. JC: manuscript editing, statistical analysis. AS: data collection, manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pathak, S.K., Sethi, M., Salunke, A.A. et al. Is Flexion Gap Rectangular in Native Indian Knees? Results of an MRI Study. JOIO 55, 1127–1134 (2021). https://doi.org/10.1007/s43465-021-00418-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00418-1